#I went to a specialist 5 years ago and my symptoms were NOTHING compared to now
Text
I hate dentists.
#might need oral surgery ✌️#I'll be damned if I ever go back to a dentist though#most evil people I've met#my mom and I just had a conversation about all of our dental experiences and it just reignited my intense hatred#I always repress those memories for a reason#but yeah I'm researching oral surgeons rn because my jaw is a problem!! I need to go back to a professional#I went to a specialist 5 years ago and my symptoms were NOTHING compared to now#now it's like dire but I still refuse to go to a dentist#if I need a recommendation to get into a surgeon's office I'm going to get it from my old orthodontist that I haven't seen in a year#this is a dentist hate blog#ashley rambles
5 notes
·
View notes
Text
424
A health survey. Must be fun.
What health problems do you have right now?
Well my back is a bitch 24/7; my joints hurt when it gets cold; I have scoliosis; and mentally speaking I’m not very stable either. I sound 60.
Are you in chronic pain?
Never been diagnosed with such, no.
What do you take medications for?
I don’t. I probably need to, but the state of mental health care in the Philippines is just so inaccessible: it’s expensive, available services are few and far between, and anyone younger than 21 needs to get written consent from their parents, which can be difficult if someone’s parents don’t actually believe in mental health issues. There is a lot of work to be done.
What are some health issues you have had in the past?
My lactose intolerance was a problem when I was an infant. My family didn’t know I had it, so they kept panicking when I would just poop out all the milk they fed me all day and when my stomach would end up storing nothing. It got critical and I had to be sent to the hospital, but it turned out well after.
Do you have allergies?
Nope. Free to eat and be in contact with anything.
If so, what are you allergic to?
Have you ever been to an allergist?
No, never had to.
Have you ever been to the ER?
Mmm nope, never been in an emergency situation.
Have you ever been treated poorly in the ER?
Have you ever been told your symptoms were anxiety, when they weren't?
I haven’t been tested for that. When I was doing my health exam for university though, they did review my mental health and suspected me of having depression, but they didn’t declare symptoms or formally diagnose me or anything.
What is the most physically painful thing you've ever experienced?
Probably scraping and kicking my feet against coral reefs when I went snorkeling back in ‘09. I had no flippers and I was panicking (I wasn’t used to using the snorkeling mask to breathe) so I was thrashing my legs around in the water. I knew I was hitting the coral reefs and they were fucking sharp, but I was panicking so I powered through even though it meant I had to hit them every time I kicked. It was painful while I was swimming and even more painful in the weeks that followed. It was the worst infected wound I’ve ever had. Just imagine kicking a razor-sharp boulder with your bare feet.
How many surgeries have you had?
Zero. I hope I never need any, the thought of surgery terrifies me.
What types of surgery have you had?
Have you always recovered well from surgery?
Have you ever been treated poorly by a doctor?
YES!!! The ones in my university’s health service are horrible. Case in point, my health exam for admission to UP: I know it’s part of a doctor’s job, but the doctor assigned to me back then touched my breasts very hastily to check for suspicious bumps. It would have helped tons if 1) she gave me a heads-up beforehand and 2) asked permission, but this lady just told me to lie down and went ahead to stick her hand under my shirt. As someone who had only been fresh out of Catholic school at that point, it was the perfect opportunity to panic. Same doctor was the one who suspected I was depressed after reviewing my mental health form, but instead of being helpful she DEMANDED reasons why I felt that way. I was already uncomfortable with the boob incident by then and was too stunned to speak, so I just kept saying I was fine and that I was mentally stable. In reality I just wanted to get out from that nasty old bitch.
Have you ever had a doctor tried to kill you?
Oh well that’s just taking it a million times further. No.
Is your primary care doctor a man or a woman?
I don’t have one.
Have you had the same primary care doctor your whole life?
We don’t have a family doctor.
Are you happy with your current doctor?
Have you ever seen a specialist for anything?
X-ray technicians. I had trips to see them the most when we found out I had scoliosis.
What is the most itchiest thing you have ever experienced?
I had weird rashes on my legs one time in high school, and since I was stubborn I kept scratching them until they turned into nasty black and blue wounds/bruises and cuts. I still have no idea where they came from.
Have you ever had a severe itch, that you'd rate a 10?
^ That.
On a scale of 1-10, what's the worst physical pain you've ever been in?
The coral reef incident is an easy 20.
Have you ever passed out from pain?
Noooooo. Passing out from pain is one of my greatest fears. I avoid encountering anything painful as much as I can just because I’m scared of the thought of passing out because of pain.
Have you ever thrown up from pain?
Nope. Just from drinking and expired barbecue lmfao.
Do you have any food intolerances? If so, to what?
It’s not official, but I hate fruits. Like, I can immediately tell if something has fruit in it and I will spit it out accordingly. That and raisins.
Do you have any food sensitivities? If so, to what?
Nope.
What medications are you allergic to?
Do you have acne?
A small pimple shows up every now and then (mostly when I’m stressed or if my face gets oily) but it’s never been a full-on breakout. I’ve been lucky when it comes to acne.
Do you take birth control pills?
I don’t. I want to take them just because I heard it makes your breasts get bigger hahahahahaha but Gab is adamant about not letting me take them.
Are your hormones screwed up?
Mm no, they’re not that bad. Obviously they act up when I’m nearing or on my period e.g. cravings, crying all the time, being sensitive about everything, but not to the point that my period is irregular or gives me severe dysmenorrhea.
Do you have bad withdrawals from medications?
I don’t take meds to begin with.
What are some withdrawal symptoms you've had?
What are some bad side effects of medications that you've had?
Have you ever gained weight from a medication? If so, how much?
Have you ever had to take Prednisone?
Never even heard of it.
If so, did it make you gain weight and make your face puff up?
Looks like I’m skipping lots of questions.
How many hours a sleep do you need?
Don’t adults need 8 hours, in general?
How many hours a sleep do you get?
I try to make it to 8, but I’ve been really busy for this semester that it ends up being 5-7 hours instead.
Do you exercise enough?
I don’t at all, haaaaaaaaaaah.
Do you eat healthy?
I do like vegetables and will happily eat salads and sandwiches with veggies packed in them, but I tend to balance it out with grossly unhealthy food anyway, so you decide if this still counts as healthy.
Are you on a special diet for your health?
No, I don’t think I need to be.
Are you trying to lose weight or gain weight?
Gain, which I’m on the way to doing. I’m a little chubbier now compared to high school.
Are you a healthy weight?
I’m 90 lbs. the last time I checked. Relative to my height, that’s underweight.
Are you happy with your weight?
Sure, but gaining a few pounds wouldn’t hurt either.
How often do you wash your hair?
Everyday if I’m in school; every other day if I’m on summer break.
Do you take showers or baths?
Showers.
How often do you shower or bathe?
^ Same thing.
Do you take vitamins? If so, which ones?
I used to take two vitamin syrups everyday when I was younger: one for vitamin C and the other to help me grow taller. When I got a little older my mom changed our usual syrups to these cute vitamin C gummy bears, then after a while I just stopped taking.
What bones have you broken?
Haven’t broken any, fortunately.
What's the worst physical injury you've had?
Aside from my icky foot infection, I had a bad fall in school a few months ago and my ankle got sprained pretty bad. I don’t think I gave it A+ treatment so it never really fully healed. I know this because the same foot still hurts whenever it’s in an odd position or when I shift too much of my weight on it.
Do you have sensitive skin?
Yes. It eventually gets itchy when my skin is out in the open. In high school, I often had a hard time walking from point A to B because my skin would always get irritated, but I couldn’t scratch it because I was wearing a skirt.
What chemicals make you sick?
Toxic ones, I would assume? Haha.
What time of year do you usually get sick?
I never get sick.
What's the highest fever you've ever had?
40ºC. It was a dengue scare.
Have you ever had the flu?
Sure, a few times here and there.
Have you ever had bronchitis?
Nope.
Have you ever had an ear infection?
I don’t remember having one.
Do you snore?
Only when I’m so tired that I’m 130% passed out.
What pain reliever do you use for cramps?
My menstrual cramps never get that bad.
If you're female, what symptoms do you get when on your period?
My pelvis area and legs hurt; I cry over everything; I’m sensitive when people are angry; I will essentially take everything personally; my cravings either change every 5 minutes or I just want one food and I will murder to get such craving; I get very poopy; and sometimes I’ll get very drowsy.
Do you have regular periods?
Pretty much, yes. Sometimes they’ll be a few days early or late but very rarely does it go completely irregular.
Are you afraid of shots?
Deathly afraid. Like I would do everything to avoid having to take them.
Have you ever donated blood?
No. Even if I wanted to, I’m not allowed to (underweight). Plus you have to be pricked for that, which is a Huge No-No for me.
Do you do well with shots?
If I absolutely have to have a shot, I can manage albeit with a lot of fidgeting. What I’m terrible with is IV. I had a huge meltdown the one and only time I needed to have a needle injected onto my wrist. I was a 12 year old grown ass person thrashing around in the hospital room lol.
What x-rays have you had?
Just my spine.
Have you ever gotten a pill or a piece of food stuck in your throat?
Pill-stuck-in-throat sensation happens sometimes, but it’s never been anything serious.
What method of birth control do you use, if applicable?
Do you take birth control to control hormones, or to prevent pregnancy?
As mentioned, I don’t take it.
How often does your hair need to be washed?
I don’t know about need, but I wash it everyday or every other day so that it doesn’t get oily, which feels irritating.
What do you keep on hand for emergencies?
I don’t really keep stuff for emergency, just money hahaha.
Have you ever had a severe allergic reaction?
Nopes.
If so, what were your symptoms?
Have you ever used an epi pen?
I have not.
Have you ever been to the ER for a severe allergic reaction?
Negative.
What's the worst burn you've ever had?
When I was 7, I wanted to do something daring so I touched a clothes iron that was plugged in and was in use (by my grandma, but she left to attend to something at the time). My index finger rightfully had a tiny blister for the next two weeks. My dumbass definitely deserved it.
What's the worst allergic reaction you've ever had?
No allergies.
Have you had any health-related embarrassing moments?
I don’t think anything bad enough has happened yet.
If so, what happened? (if you want to share)
Do you use tampons or pads?
Pads. I’m scared of tampons.
Do you sweat a lot?
I don’t, actually. I drink a lot of water, but I guess I just don’t sweat much.
Do you get nosebleeds?
I’ve never experienced a nosebleed and am also too scared to get one.
Do you get motion sickness?
Pretty easily, especially if I’m riding an unfamiliar car.
Do you have acne?
I get a pimple every now and then but it’s not a big issue.
Do you have scars?
Sure. There’s one on my fourth right toe and the other one on my left eyebrow.
What are some of your scars from?
Toe scar is from when my toes got stuck in my bike’s blades (something like that, anyway); eyebrow scar is from a stupid cousin smashing a small glass bottle towards my face.
Do you have a birthmark? If so, what color is it?
I have a brown one behind my left shoulder. I also have one near my elbow; it used to be blue/green but now it’s a faint black-ish shade.
What makes your eyes itch?
Uh, dirt? I also know if I’ve been spending too much time in front of the computer when my eyes start feeling irritated. That’s usually my signal to go to bed or to have a break.
Are you ticklish?
Very. I can’t be tickled on any part of my body.
Do you have a sweet tooth?
I have my moods, but overly sweet food isn’t really a favorite of mine.
Do you ever crave chocolate?
Never, actually. I can crave sweet stuff like brownies and cookies, but never chocolate bars.
Do you ever crave cheese?
No. Lactose intolerance makes me wary of cheese so I never really ~crave it.
What else, if anything, do you get cravings for?
I usually crave for cuisines in general or specific restaurants.
Do you drink enough water?
Yeah I’m pretty sure I do.
Do you comfort eat when stressed?
It varies. Sometimes I’ll rely on eating, but other times I’ll lose my appetite and wouldn’t want to be anywhere near food.
How old were you when you started your period?
I was 9 but was about to turn 10.
How old were you when you started going through puberty?
I am guessing the same age when I had my period, but everything sped up only when I was 10/11.
What was the first sign of puberty for you?
...My period?
Did your hair change when you went through puberty?
Hair started to grow in places, but as for changes, not really.
At what time of day do you normally feel your best?
I don’t really keep track lol.
Are you naturally optimistic or pessimistic?
Um both, depending on my mood for the day. It never stays constant.
Are you naturally energetic?
I’m naturally un-energetic. Looking at extroverts exhausts me.
Does your mind wander a lot?
Only when I’m bored at something, like in a certain class. I can generally focus well.
Do you know your blood type?
I don’t actually hah.
Have you ever been taken to the hospital against your will?
Nope.
Any final thoughts?
Cool survey. It’s different.
3 notes
·
View notes
Text
Postpartum depression on the rise, especially for women of color, during COVID-19 pandemic
New Post has been published on https://depression-md.com/postpartum-depression-on-the-rise-especially-for-women-of-color-during-covid-19-pandemic/
Postpartum depression on the rise, especially for women of color, during COVID-19 pandemic

Los Angeles — When Altagracia Mejía learned she was going to be a mother, happiness flooded her heart.
She picked out a crib. She took photos of her growing belly and redecorated her bedroom. She held a gender-reveal party on Zoom.
But her bliss didn’t last long.
Perplexing feelings of anxiety and doubts that she ever could be a fit mother for her baby crept into her head during pregnancy while living in her small one-bedroom apartment. And while the Panorama City resident tried to brush away her uneasiness, those feelings seized her again after she gave birth to her daughter, Alexa, in the middle of the pandemic, on Sept. 8, 2020.
By the time Mejía’s daughter was around 2 months old, the 26-year-old mother’s episodes of anxiety and irritability had darkened into thoughts of suicide.
“In my most lucid moments, I ask myself over and over again what is happening to me,” said Mejía, who immigrated to the United States from El Salvador four years ago in hopes of putting the poverty and violence of her homeland behind her. “I am supposed to be happy, resplendent and full of energy, but nothing is as they paint it on television or social networks.
“For society, especially for Latinos,” she continued, “it is unforgivable for a woman to feel sad or have thoughts of death at this moment that is supposed to be the happiest of her life.”

Mejía suffers from postpartum depression, a severe form of clinical depression related to pregnancy and childbirth. Symptoms include severe mood swings and deep despondency as well as impulses that can impel a mother to harm herself or her child.
Last week, Sandra Chico, the 28-year-old mother of three children found dead in an East Los Angeles home, was arrested on suspicion of murder and is being held on $2-million bail, L.A. County Sheriff’s Department officials said Tuesday.
In an interview with the Times, Elizabeth Chico said her younger sister had exhibited symptoms of postpartum depression following the birth of her youngest child about a month ago. “All that stress, all that anxiety, it takes over you,” she said.
Although the California Department of Public Health has not released figures on the number of women with postpartum depression since 2018, experts say that an increase in calls from women asking for help from local nonprofit organizations, along with lengthening hospital waiting lists, indicate that postpartum depression cases may have increased dramatically over the course of the COVID-19 pandemic.
Women of color continue to be among the most affected, in part because many do not have health insurance or their insurance covers little or no therapy, said Misty Richards, one of the directors of the Maternal Outpatient Mental Health Services program at UCLA. Evidence suggests that some Latina mothers may hesitate to seek help because of stigmas associated with mental illness, as well as cultural expectations surrounding motherhood and the traditional roles of women in Latin societies.
In addition, many of those afflicted are not being screened for postpartum depression, despite California’s maternal mental health bill, AB 2193, which went into effect on July 1, 2019, and requires that obstetricians and gynecologists screen mothers for these conditions during and after pregnancy and ensure that they get any needed treatment.
The most recent available CDPH statistics, from 2018, indicated that 1 in 5 California women suffered from postpartum depression during or after giving birth, which translated to 100,000 cases a year. The report also states that: “Black and Latina women experience the highest percentage of depressive symptoms of all racial/ethnic groups during both the prenatal and postpartum periods.”
According to the CDPH: “Disparities are particularly evident for prenatal symptoms of depression, which are twice as common for Black (19.9%) and Latina (17.1%) women compared to white (9.5%) and Asian/Pacific Islander (10.3%) women.”
Richards, of the UCLA clinic, said that she has seen a 30% increase in postpartum depression cases since the pandemic started. She expressed particular concern for low-income women of color who are disappearing into the cracks of an inaccessible healthcare system.
She estimates that she sees 15 women a week, or about 700 cases a year. If the clinic is full, as has been the case since the beginning of the pandemic, she refers mothers to other affordable clinics and nonprofit organizations.
“A single 90-minute visit to the reproductive psychiatrist in California costs $500 to $800 if you don’t have health insurance,” said Richards, who currently has a 15-day waiting list for treating patients. “That money cannot be paid by a low-income person.”
Responding to the pandemic, the California Department of Health Care Services implemented a Provisional Postpartum Care Extension programon Aug. 1, 2020, that allows Medi-Cal eligible mothers who are diagnosed with a maternal mental health condition to remain eligible for assistance for up to one year after giving birth — 10 months longer than the normal 60-day period of post-pregnancy care.
However, in order to get help, mothers must be diagnosed with postpartum depression, and many health experts are not even aware of the existence of the program, which will expire Dec. 31.
Medi-Cal, the service that pays for more than 50% of all births in California, would have covered mental aid assistance for Mejía, but her condition was never detected, she said.
“In my clinic, I filled out forms about how I felt, and even though they knew I had depression, they never gave me a positive diagnosis even after giving birth,” she said.
While trying to navigate the labyrinthine U.S. medical system, Mejía felt isolated from friends and family. Fear of catching COVID-19, and shame over what she felt were her failures as a mother, kept her from seeking out others for comfort and support.
“Since I came to this country four years ago, I have worked as a babysitter,” she said. “It was not possible to share that I could take care of other children, and not even be able to breastfeed my own daughter.”
Because she couldn’t afford a private specialist, Mejía, along with her husband of three years, Walberto Gochez, a maintenance worker, and her father, Marco Antonio Mejía, had to seek help on their own from Maternal Mental Health Now, a nonprofit that advocates for screening and treatment of prenatal and postpartum depression in Los Angeles County.
Eynav Accortt, a clinical psychologist at Cedars-Sinai Hospital, who treats women with anxiety and depression during pregnancy and postpartum (known as perinatal mood and anxiety disorders), said the pandemic has added a layer of complexity and isolation that could substantially increase rates of such cases.
“Women have been under more stress from the pandemic,” she said. “They fear getting sick or their babies getting sick, they can’t have home visits and this adds to the worries of the day, even if they aren’t low-income.”
According to Accortt, the Cedars-Sinai Reproductive Psychology Clinic received twice as many calls from women seeking help between January and April of this year, as it did during the entire previous year.
“About 11 patients who could have seen me for individual therapy, because I am in the network with their insurance company, were referred to other community providers, many of whom were already full,” she said. “Right now, I have a three-week waiting list for a client to start individual therapy with me.”
In 2020, about 6,500 women were screened for postpartum depression at Cedars-Sinai, and 300 to 500 who were at risk for perinatal mood and anxiety disorders were referred to local organizations for help. In addition, 150 other women obtained direct services such as individual therapy or support group aid from the Cedars-Sinai Reproductive Psychology Clinic.
Alondra Espinoza, 36, of East Los Angeles, is among those women whose postpartum depression was exacerbated by the pandemic. She was shocked after learning she was pregnant for the third time, in 2019, while raising her daughter, Jocelyn, now 15, and son, Isaiah, 11.
“During my pregnancy, I didn’t want people to see me, I thought I was too old to start caring for a baby again,” she said. “I started crying all the time and feeling irritated at the same time. As the months went by, I started to feel lonely, frustrated and desperate about what my future was going to be like. “
In January 2020, three months before giving birth, she had to stop working as a teacher’s assistant because she suffers from sciatica.
In April 2020, Espinoza gave birth to Lexi, and by June, postpartum depression hit her harder when she learned that her husband, Jezreel, a building demolition worker, would have to return to work out of state.
“During the pandemic I couldn’t go out, I was afraid that we would catch [the coronavirus] and I didn’t know who to turn to,” Espinoza said.
“My girl cried all the time, and I felt useless next to her,” she continued. “I felt like she was freaking out. … I wanted to get out of the house and run aimlessly, I wanted to disappear.”
Like Mejía, Espinoza said, she was never diagnosed with postpartum depression despite filling out several forms at Garfield Medical Center in Monterey Park, where she gave birth.
“It took me about two months after giving birth to seek help on my own because I thought that asking for assistance was wrong,” she said. “I believed that people would think that I am not a good mother and then social services would take away my children.”
An employee of Garfield Medical Center, who did not want to be identified, said that since November 2019, the center has been screening all mothers before they return home with their newborns. “And if they screen high risk for postpartum depression, a social worker refers them to different resources,” the employee said.
Regarding Espinoza’s case, the employee said that there might have been a communication issue or “most likely she did not meet the criteria for high-risk postpartum.”
“We only see the mothers for a short period of time, about four days, after the delivery,” the employee said. “If they do not speak to us, we cannot catch them, we do not have a chance to help.”
Emily C. Dossett, clinical assistant professor of psychiatry and behavioral sciences at USC’s Keck School of Medicine, maintains that even though screening women for postpartum depression is now encoded in state law, “there is still a lack of resources available to do so, which puts doctors in a bad situation.”
“If health experts are not aware of the postpartum screening laws or the [Provisional Postpartum Care Extension] law, and if there are not enough staff to refer women or therapists, there will always be mothers who will disappear into the cracks without any treatment,” said Dossett, who since the pandemic began has seen a 25% increase in referrals from mothers in need of therapy.
“Postpartum depression can occur shortly after delivery or even up to a year later,” Dossett continued. “That’s why we need more affordable support services because in my experience I believe that 80% of women with postpartum depression can be treated with therapies.”
Norwalk resident Adriana Rangel did not have postpartum depression until two months after giving birth to Ivana on Nov. 13, 2020.
“As if there was a switch in my brain, suddenly I began to feel sad, exhausted, I did not want to eat, I did not even want to take off my pajamas,” said Rangel, 31. “I was no longer the talkative, cheerful and outgoing woman that people knew.”
When her mother died of COVID-19 in February, Rangel plunged further into depression and feared getting sick or making her daughter sick.
She subsequently was able to get help for her condition. She has private health insurance and pays $25 out of pocket for each weekly appointment to see a psychologist at Providence St. Joseph Hospital.
Mike Sherbun, executive director of the Providence Mental Health Clinical Institute, which is made up of 11 hospitals in Orange and Los Angeles counties, said that cases of postpartum depression have risen as much as 25% during the pandemic. He fears those figures are undercounted and may keep rising because they don’t include women who don’t seek help.
“These increases are just the tip of a mental health crisis in California,” he said. “So our institute is in the process of opening more outpatient programs that can assist mothers with postpartum depression in Torrance and Tarzana.”
Sherbun stressed that more laws are needed in California to cover all mothers, while current laws need to be enforced.
In the case of E.R., who asked not to disclose her full name, her OB/GYN did not tell her that she suffered from depression during pregnancy or after delivery until she, too, sought help on her own, she said. The Los Angeles resident, who gave birth in January, began to suffer from anxiety almost three months after her pregnancy began.
“I worked as a mental health case manager and even though I was scared of getting sick with COVID-19, I didn’t want to stop working,” E.R. said. “I heard from so many people who lost their jobs and couldn’t pay their rent and didn’t want to be in that situation. At the same time, I began to be scared by my future, the safety and stability of the baby, so I decided to work until the very moment I gave birth.
“I think working helped me a little bit not to think about depression and anxiety. However, once I had my baby, my mental health declined faster. I cried all the time. I fought with my husband.
“Part of my depression was also due to being isolated from my family and close friends. I come from a Latino family where we celebrate everything, and this time we couldn’t because of the pandemic.”
In the moments when she couldn’t sleep, thoughts of ending her own life, or her child’s, closed in on her.
“I thought that if she was dead, things would be better,” she said. “What happens if I throw myself into a car or throw myself off a building?”
E.R. didn’t confide in her family for fear that they would think she was crazy or that they would take her baby from her.
“In my family, with a mother from Mexico and a father from El Salvador, it is not normal for a mother to feel this way, or you just solve it yourself or you approach the priest to give you advice,” she said.
E. R. asked her husband to accompany her to therapy groups, but he refused, wary of the stigma around mental health issues.
“Fortunately, he understands that I need help and has become more patient,” E.R. said. “He also takes the baby with him when I have felt like I want a break. Having him on my side has helped me a lot.”
Gabrielle Kaufman, clinical director of Maternal Mental Health Now, an organization that helps women with postpartum depression and advocates creating laws that benefit them, said there is still a lot to do at the state level.
“A couple of laws have been passed in the last three years to help this sector, but the pandemic has once again stalled us,” she said. “If as health experts we do not follow current laws and do not advocate for more laws that protect mothers, we will have a mental health crisis that is going to leave a dent in the future.”
Assemblyman Brian Maienschein (D-San Diego), the creator of the law to screen women for postpartum depression, acknowledges that new mothers need to be more aware of their rights .
“We want to remind [mothers] that experts should do postpartum screenings, and that they can ask for them if their providers don’t,” Maienschein said.
He added that “there is also a supplier problem. So a new law that I introduced to the Legislature in February will expand that group. After the diagnosis comes the next step, directing the mothers to the expert for treatment.”
AB 935, the Mothers and Children Mental Health Support Act, would provide the consultation service through telehealth from private insurers and managed care organizations such as Medi-Cal to close gaps when there is a shortage of providers.
However, the bill will not be discussed until 2022.
For now, Mejía and Espinoza attend Maternal Mental Health Now groups. Rangel sees a psychologist at St. Joseph Heritage Hospital every week through her private health insurance. E. R. gets help in free therapy groups at Downtown Women’s Center in Los Angeles.
“No mother has to suffer from postpartum depression alone,” Mejía said. “Families must support their mothers so that there are no suicides, and in worse cases, even homicides. This mood disorder is real.”
Source link
0 notes
Text
I just finished watching Jennifer Brea’s incredible documentary Unrest on Netflix. Watch it now. Everyone should.
My story.
I became ill suddenly, and severely, in September (I think) of 2016. I had just moved to Providence in August from San Francisco, without my partner of 10+ years, to take a teaching job at Brown University. I was teaching a poetry workshop for Frequency Writers, a community writing group, as well as a class I developed for Brown’s Literary Arts department, Experimental Poets of Color. Providence is a city I love, and even though the gig was adjunct (i.e. no job security, no health insurance, etc.) I wanted to be in Providence, and I wanted to be teaching in my fiend. I had health insurance through the ACA at the time, and though I had been diagnosed with several mental illnesses many years before (major depression and general and social anxiety disorders) I felt that my hearth was well managed with the medication I was on.
I was so happy to be back in Providence, I would walk for hours around the city, sometimes 7 miles in one stretch, listening to music and books. I was thrilled to be teaching the class I desperately wish I had been able to take at any point in my education (which includes three masters degrees), and to be nearer to my friends and family who live in Boston and the surrounding areas. I missed my partner, but we’ve been long distance for much of our relationship (the price of being an artist in academia), and it seemed like he was getting ready to leave San Francisco and head back east himself.
It was the second meeting, I think, of the Frequency open poetry workshop. It was Wednesday night. I walked to the community gallery space on Carpenter St. where we held our meetings early, unlocked the doors, and made myself some tea. It was a normal night. At some point during the workshop I started to feel exhausted, sick, like I was getting a cold. I pushed through, but took a Lyft home. I woke up the next day and still felt bad. Worse, even. I cancelled that day’s class and stayed in bed. By the next week I still wasn’t feeling any better. I went to the CVS clinic to see if I had the flu, which was going around and apparently quite bad that year. I didn’t, I was told it was just a bad cold, and to take some cough suppressant for the bad cough.
I thought maybe I wasn’t sleeping well - I was tired all the time - and maybe that was making the cold last longer than normal. I had had (undiagnosed) chronic pain for years which had started in 2007 in my first year in grad school. It was especially bad in my neck and lower back, so I had spent years and a lot of money finding a really good mattress. But I had housemates that were young, noisy, up late, so I invested in an eye mask, noise-cancelling headphones that I slept in, and a white noise machine. I had to teach my classes, but I would show up, teach, and come immediately back home and stay in bed until I had to teach the next class. I spent several weeks like this, thinking it was just a cold, until someone pointed out that colds, even very bad ones, don’t last for several weeks.
I made an appointment with my primary care doctor in Boston. I’ve struggled finding doctors that take me seriously, like most women and non binary people I imagine, especially with chronic and challenging illnesses. This doctor listened to me, and was gentle, and that was pretty much all I could hope for. He examined me, and tested me for mono, strep, walking pneumonia (which I’d had before, and which was basically the closest comparable experience I had). I had none of them. Then we tested my thyroid, my B12 levels, and my immune functions. He found nothing wrong with me.
A digression on chronic pain, including a digression on trauma.
I had gone down a diagnostic wormhole several years ago when I’d first started getting tests to see if we could find an underlying cause for my chronic pain. It started in Iowa City, where I did my second graduate degree, and included MRIs, x-rays, testing for immunological disorders, cancers, and basically anything they could think of. Eventually I was referred to a psychologist, because they determined my pain might be a physical manifestation of trauma. And I’d had my share of trauma.
A digression on trauma. I grew up with an emotionally abusive mother who, though never diagnosed, meets all of the criteria for narcissistic personality disorder. I ran away from home as a teenager, living on the streets for most of a year, before re-establishing a relationship with my family, primarily my father who helped me get an apartment, back into school, and eventually into college. At that point my mother re-entered the picture, and my father stopped helping me pay for college, so I worked sometimes as many as 5 jobs while completing my undergraduate degree. I met my partner in undergrad, and he has been an immense help for me in recovering from my trauma, but like so many who were experienced long-term abuse as children, I probably will never be un-affected by my experiences.
So the trauma angle seemed at least plausible to me, and I went to a year’s worth of sessions with two different people, one a psychologist who specialized in and studied the manifestation of trauma as physical pain, and another who practiced CBT and meditative mindfulness therapy. Both helped immensely with my emotional state, but my pain persisted. So when I moved away for my third graduate degree (my first move to Providence) I transferred care and we started the diagnostics all over again. This time I saved all my records - I have my MRIs and my X-rays still in some box somewhere. We did CAT scans and I went to scores of specialists including an orthopedic surgeon who recommended surgery; a chiropractor who works with the Boston Ballet Company who diagnosed me as hyper-flexible and gave me strengthening exercises to do that actually seemed to help somewhat; and a neurologist who found nothing wrong with me at all. After four years of referrals and diagnostics, I found a integrative care physician who listened to me break down in her office, prescribed an anti-depressant that is also a sedative to help me fall asleep, and helped me come up with a plan to manage the pain. Massage, chiropractor, walking and stretching, the anti-depressants, 800mg Ibuprofen when I needed it, and Vicodin when nothing else helped.
After all of this, I wasn’t eager to go down another diagnostic chase.
Back to 2016.
By this point it was the middle of November. I was so sick that I couldn’t feed myself, I couldn’t do laundry, I couldn’t leave the house except for to teach, and then I spent the next 24-48 hours recovering mostly in bed from the fatigue it caused me. I was experiencing sever cognitive deficiencies, most notably my ability to process and retain information, and my ability to speak. It felt like I had dementia, or what I imagine dementia to feel like. I would read the same sentence over and over again and not understand it, or not remember it when I started the next one. I would fight to get up to go into the kitchen, only to forget what I was there for. Did I need water? Had I fed the cat? Did I need to use the bathroom? My father and brother were taking turns coming down to my house to prepare food for me for the week, and to get my groceries, and to do my laundry. I needed help with everything. I could do one, maybe two things in a given day. Those things included brushing my teeth and feeding the cat.
I couldn’t even research my condition, given my cognitive symptoms. I was angry, and many days I felt like it would be better to die. I couldn’t read or write, so I took up embroidery as a way to try to keep my life worth living, a way to keep making art.
In January, 2017 when my partner came to visit for his winter break, we went to my doctor together. I couldn’t remember the questions he wanted me to ask, and I couldn’t have remembered the answers anyway, and I certainly couldn’t get myself there and back without help, so him coming was the only way I was going to get there. I don’t remember much of the appointment, but I do remember my doctor suggested that I might be experiencing a severe prolonged depressive episode. Based on my previous diagnosis of depression. Based on the fact that there seemed to be nothing wrong with me, physically.
My partner didn’t buy it. I sort of did, or at least I didn’t have the energy to dispute it. My partner started researching, aggressively, and a few months later he came up with something. Maybe, he said, it was my copper IUD. Maybe I had copper toxicity. My doctor said that was impossible, that the IUD can’t cause copper toxicity, but my symptoms aligned, and there are thousands of women on the internet who have experienced copper poisoning from their IUD. So one day in April, my best friend took me to the hospital and I had mine removed. The next day, I felt better. Not 100% better, but maybe 40% better. The next day my partner and I went for a walk, the first time in almost a year I had felt able to do that.
I kept feeling better. Not getting better, but I stayed feeling about 40% better. A few days I felt almost entirely myself, but then the next day I would be exhausted again. I could do things, but if I pushed too hard, I would collapse and pay for it for days. I learned about spoons, and disability culture and activism. I learned about setting my limits, and prioritizing. I said no to almost everything, because almost nothing was worth the risk of incapacitation for me.
My brain started to recover too - I could read. I started writing in my journal, not poetry but at least writing of some sort. I felt hopeful that I was recovering. We bought a house, a big old Victorian that needs TLC, and I moved in there with 4 other queer artist friends. I didn’t get the tenure-track job at Brown, but I did get another adjunct offer to teach Book Arts, and I accepted - something I definitely couldn’t have done at my sickest, given that it’s a 15-hr a week studio course.
But now, a year post-removal, my memory is still a problem. And I still get exhausted a lot. A lot more than I used to, before I got sick. But the anecdotal evidence on the copper IUD detox forums says that it could take years to fully process the toxicity out of your system. The most severe days might be attributed to “dumps” - when the body releases stored copper all at once - and those days feel like my worst ones did when I was at my sickest. I had thought that when I felt better, I would start to do things again, go to poetry readings, have dinner with friends, go for walks, be part of the community I’d moved here because I loved. But I still say no to most things, or write them down in my calendar and don’t go. I know that if I push too hard, I’ll pay for it for days. And “too hard” is a moving target - it changes seemingly randomly, and I don’t know when I’m approaching it until it’s too late. Then I’m in bed for days.
I’ve been having an especially bad few days. Maybe a week. Maybe more. My memory, my brain isn’t good at sequence anymore, or keeping track of time. It’s frustrating, because I can’t keep track of my own symptoms. Sometimes I remember to write them down, and sometimes I forget, or am too tired. And there’s no one here to watch me, or help me - my partner doesn’t move here until June. Today, for example, I got up at 11 and I fed the cats. And I was so tired that I lay down, and just...passed out. I don’t remember falling back asleep, but then I woke up at 6 pm. I fed the cats again, and then had to go back to bed. The last week has been similar: do just what is necessary, then back to bed. It feels like I’m sick all over again.
I have had my period, which can be associated with copper dumps. I’m not saying it’s not copper “dumps,” or that it’s isn’t related to copper poisoning. But I watched Unrest and thought: “maybe this is what I have, too?” So many of those scenes were heartbreakingly familiar. I wept through most of it, because Jennifer was saying the things that I’d been feeling. About feeling like it was a good day when all I had done was survived it. About feeling like my life had ended, and that I had a new one now, one that sometimes didn’t feel like a life at all, but one that I still didn’t want to give up. About not being listened to, about not being believed. I wept at the thought of having a diagnosis, after all this time. Of maybe finally at least knowing what is wrong with me. Maybe.
But I don’t know how to find out. I don’t currently have health insurance, because the premium on my ACA policy from last year went up by 50% and I couldn’t afford it anymore, and adjuncts at Brown who teach fewer than 4 classes a year don’t get health insurance, and I’m only teaching 3, and I am barely able to do that; this semester teaching 2 classes took every bit of energy I had. I will get health insurance starting in September when my partner starts his new job in Providence, and maybe then I can get some answers. If I have the energy for it.
My story doesn’t have an ending yet. I’m in bed, as I have been all day. Writing this was the most writing I’ve done since I got sick. I’m grateful for that. It feels like, thanks to the work that Jennifer has done, an important story is at least starting to be told. Not just mine, but one that is shared by millions.
#chronic fatigue#chronically ill#m.e.#m.e./cfs#me/cfs#unrest#millionsmissing#iud copper toxicity#copper toxicity#spoonie#chronic illness#meaction#disability
6 notes
·
View notes
Photo

New Post has been published on https://techcrunchapp.com/more-parents-seek-adhd-diagnosis-and-drugs-for-kids-to-manage-remote-learning/
More parents seek ADHD diagnosis and drugs for kids to manage remote learning

Susan McLaughlin’s 12-year-old daughter, Isabela, was a straight-A student before the pandemic. Isabela, who lives in a suburb of Columbus, Ohio, excelled at science and math and was already getting high school credit for algebra.
But when her school shut down in March and classes shifted to Zoom, Isabela’s grades took a nosedive. She signed on for her virtual class from a desk piled high with books, papers and stuffed animals and then spent hours trying to clean her room instead of focusing on schoolwork. She found herself “paralyzed” by assignments, McLaughlin said, but she wouldn’t tell the teacher over email that she was struggling, as she would have done in person.
“It was meltdown after meltdown after meltdown,” said McLaughlin, 53, a mother of three from Delaware, Ohio, who works in a high school with chronically truant children.


McLaughlin recalls one time in April when Isabela, who was already diagnosed with severe anxiety, was given a language arts assignment and “fell to pieces.”
“She was crying and screaming and hyperventilating and started to get some tics, moving her head and flapping her arms. She had never had them before. That’s when we started to consider that it might be ADHD.”
McLaughlin spent months trying to bring more structure to Isabela’s day by writing lists, schedules, timelines and checkboxes. But as someone who was diagnosed with attention deficit hyperactivity disorder herself a decade ago, McLaughlin realized that she was seeing the same behaviors in Isabela. She thought, “I’ve got to nip this in the bud.”
Isabela is being evaluated by a psychiatrist, a process that takes several hours and requires her teachers to fill out questionnaires about her behavior. McLaughlin hopes that with an ADHD diagnosis, Isabela will be able to get a prescription for a stimulant medication — such as Ritalin, Adderall or Vyvanse — to alleviate her symptoms.
“I know it’s super controversial sometimes. But I’ve been medicated for a long time, and I can’t function without taking it,” McLaughlin said. “If I don’t take my medication, I see an immediate difference in my ability to manage complex tasks, clean the house, get up and cook dinner. So I’m hoping it will have the same effect on her.”
Susan McLaughlin and Isabela Burgeson do schoolwork.Maddie McGarvey
Growing problems
McLaughlin isn’t alone in seeking an ADHD assessment for her child during the pandemic. Two dozen children, pediatricians, psychiatrists, psychologists and researchers all described a crisis among children suffering from inattention and tanking school performance.
Data from specialists involved with diagnosing and treating ADHD show just how much parents are struggling to get help: They are flooding an ADHD support line with questions, and ADHD diagnoses and prescriptions for related medications have soared.
“Covid has been a tipping point that has pushed some families to get help,” said Dr. Melvin Oatis of the American Academy of Child and Adolescent Psychiatry, who said the stress of the pandemic, the shift to remote learning and social isolation have created “anxiety-provoking” conditions that affect students’ attention.
Experts warn that children who appear to have symptoms of ADHD should have thorough evaluations to rule out other conditions or stresses related to the pandemic before they seek medication.
“Our concern is that pediatricians and families be very careful to not simply list the symptoms of ADHD, but to look at the child’s history and use differential diagnosis to make sure we have the best possible explanation for the symptoms,” said Dr. Arthur Lavin, a Cleveland-based pediatrician who has served on several national committees of the American Academy of Pediatrics.
Related
In the meantime, parents are seeking any help they can find. The number of parents calling a help line set up by CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder), a nonprofit that supports people with ADHD, rose by 62 percent since the pandemic started, the organization said. Traffic to its website last year grew by 77 percent compared to 2019.
“We’re getting a lot of calls from caregivers who are working at home alongside their children and starting to see more issues with their behavior than they did before,” said April Gower-Getz, CHADD’s chief operating officer.
They’re certainly trying to get their children evaluated more frequently. The Child Mind Institute, a New York-based nonprofit that helps children with mental health disorders and their families, recorded a 20 percent increase in the number of appointments to discuss medication last year compared to 2019. The “lion’s share” of the appointments were to discuss medication for ADHD, said Dr. Harold Koplewicz, the institute’s founder.
And more parents are getting their children diagnosed and treated with medication for ADHD.
Athenahealth, a technology company that creates practice management software for health care providers, published research in May, drawing on data from its customers, that showed an increase in patients ages 13 to 17 who received new diagnoses of ADHD. From the week of March 9 to the week of March 30, the proportion of visits by teenagers that involved first-time ADHD diagnoses rose by 67 percent. There was a similar spike among teenagers — particularly boys — who received prescriptions for ADHD medicines for the first time.
The cases also seem to have picked up in recent months, said psychologist Keith Sutton, director of the Bay Area Center for ADD/ADHD. He said he had a “sharp increase” in inquiries during the fall.
“Before the summer, everyone was just trying to get through those months,” Sutton said. “Then, in October, when grades were coming back, parents were thinking we’re in it for the long run, something is going on here and we need help.”
Isabela Burgeson thrives with in-person schooling but has been struggling during virtual learning.Maddie McGarvey / for NBC News
Why now?
Experts attribute the increase in inquiries to a variety of factors, including the loss of structure and accommodations in the classroom setting.
Parents are also seeing their children’s troubles during school hours firsthand. Dr. Devang Patel, a family medicine physician in Illinois who specializes in ADHD, is one of several clinicians who said he is fielding more requests from parents for medication for their children.
“When the problem was in front of the teachers, it wasn’t really the parents’ concern,” Patel said. “But now they are at home trying to make their kid sit still for just half an hour and seeing how difficult that is.”
Children also miss the school environment, which helped ameliorate such issues. Dr. Jenny Radesky, a Michigan-based developmental behavioral pediatrician, said she has started prescribing stimulants for children as young as 5 and 6 this year. Their ADHD symptoms were manageable in supportive classrooms with flexible teachers, sensory tools and clear routines. But when those structures went away in March, their symptoms flared up.
“I’m watching kids who used to love school become unenthused and unmotivated,” said Radesky, who said she was worried about the long-term impact of virtual learning. “They need the social environment at school to learn how to regulate themselves. Without that, they are really struggling.”
Related
Parenting challenges
Sasha Harris-Cronin’s 8-year-old son, Z (he chose his own name when he was 6), who is in the third grade, was diagnosed with ADHD in 2019 but didn’t start medication until last August.
Before the pandemic, Z’s school provided accommodations, like seating him directly in front of the teacher, where he wouldn’t be distracted, and making sure he ran around outside during recess.
Harris-Cronin said the shift to Zoom for Z was “awful.”
“It was so difficult. There were so many tears,” she said. Z missed the structure of school and couldn’t focus on Zoom classes. He would take an hour to write four words of a writing assignment. Days would go by when he got “absolutely nothing” done.
When she and Z realized that they were “looking down the barrel of another year like this,” they visited a psychiatrist, who prescribed Ritalin and Metadate.
“It was mind-blowing,” Harris-Cronin said. “He wrote a poem the first day. It’s not a miracle cure. But boy, is it an effective tool.”
Finding relief
Jahkim Hendrix, 18, of Atherton, California, suspected that he had ADHD for many years. But he didn’t get formally evaluated until late last year, during his senior year of high school. He had been falling behind academically the previous year, and when the schools closed in March, it didn’t take long for him to “give up completely.”
“The teacher would be speaking and I’d go blank,” he said, adding that students objected to putting their cameras on for their teachers, which made them — and him — even less accountable. “I would mute my teacher and go on TikTok and stay there for hours. That’s what sustained my attention.”
He barely passed his junior year of high school, and his grades slid from Ds to Fs as he started his senior year last fall. He and his mom, who was also diagnosed with ADHD as a child, decided it was time to seek help. It took two months to get an appointment with a psychiatrist, who evaluated him for over five hours in mid-December.
In late January, he was diagnosed with ADHD.
“I cried with relief,” he said. “I have always been told I have high potential but low performance, and I didn’t know why. Now I have a name to the thing that I’m facing, as well as tools and resources to help me.”
Worried doctors
Many experts said parents and clinicians need to be extra cautious about diagnosing ADHD during a pandemic because a child might show more signs that meet the criteria for the disorder. A diagnosis simply needs six or more symptoms listed in the Diagnostic and Statistical Manual of Mental Disorders, the book of mental disorders recognized by the American Psychiatric Association. They include making careless mistakes, struggling to stay focused on tasks, having trouble organizing activities, not following through on instructions, avoiding schoolwork, losing items and being easily distracted.
“The pandemic has substantially disrupted the routines of every family, and that is going to make a good number of children feel like they can’t pay attention so well,” said Lavin, the Cleveland pediatrician. “ADHD might be one of the explanations, but only one. But the stress of a pandemic may also cause inattention.”
Medical experts say someone with ADHD was very likely to show signs before the pandemic began. Both the American Academy of Pediatrics and the American Academy of Child and Adolescent Psychiatry recommend lengthy evaluations that take in children’s full developmental histories, surveys parents and teachers and compares symptoms to peers their own ages and genders.
A 15-minute office visit with a pediatrician isn’t long enough to rule out other causes of inattention, such as anxiety, depression and problems at home, said Sutton of the Bay Area Center for ADD/ADHD.
Susan McLaughlin and her daughter, Isabela Burgeson.Maddie McGarvey / for NBC News
Lengthy dependence
As many schools remain closed, some experts said they were concerned about the long-term impact of remote learning for young people with ADHD, particularly teenagers.
Maggie Sibley, a psychologist and researcher at the University of Washington and Seattle Children’s Hospital, has written a research paper, accepted by the Journal of Psychiatric Research, showing that symptoms are worsening and stress levels are skyrocketing among adolescents and young adults with ADHD during the pandemic. That has prompted numerous problems, including social isolation and disengagement from class.
“A person with ADHD typically has fewer friends and less social activities in their calendar,” she said. “A lot are getting their only social interactions at school.”
Students with ADHD were at particular risk of depression and dropping out of school, the study concluded.
“If you are in a situation where you are experiencing chronic boredom, getting poor grades in school, socially isolated and stuck in a house, it’s a recipe for depression,” Sibley said. While suicide isn’t an inevitable result, “we have to be vigilant down the road, especially since we know from research that when people with ADHD get depressed, they are more likely to make suicidal gestures because of their impulsivity.”
Susan McLaughlin will find out whether Isabela has ADHD at a follow-up appointment with the psychiatrist on Tuesday. While they wait, Isabela continues to battle with her assignments, particularly on Thursdays and Fridays, when class is entirely self-directed.
“I just want her to be everything she can be, a happy, well-adjusted 12-year-old — or as well-adjusted as anyone can be at this point.”
0 notes
Text
(PotDA 11) The Professional Patient

It has been a year since my upper teeth were ripped out. While some of the updates to my life are good, there are plenty more issues that rise up. Specifically in how much I feel I need to do before and while I continue to try and get my teeth removed. Though, at this point, it is bringing myself to actually make the appointment. The machismo from the adrenaline has worn off, and I find myself terrified of another go. While the pain was not spread over a weak like the torment I am used to, the agony of the removal of my teeth sticks with me. While I can take comfort in it as inspiration for horror plots and ponderings that hopefully will become the horror stories to define my legacy one day, but the terror of another go holds me back. Like it did in writing this.
I suppose, at this point, you could clearly call my focus on the health care system a bit of an obsession. Though, I personally do not know how I should otherwise approach a situation as I have experienced. The years go by, and still, I have more to write and ramble about. Still, I have more that makes my mind throb with conflicting emotions of manic outrage and debilitating depression. All the while the buzz of anxiety add to the haze, while the ADHD warps me completely. Fuels the fire of the rest by being the name for a peculiarity in my mind I had since I was born, I’d imagine, as I was diagnosed with it at the age of 5. However, I’ll get to the bumblefuck that was my ADHD treatment (or lack thereof for the past decade) in the next ramble. This one is to bridge the gap I mentioned in the last one.
As a brief recap, on March 23, 2018, I went in to have all of my teeth removed. This was required as a lifetime of one of my disease’s flare-ups mixed with a decade (around 16-20 to a week ago. More on that later.) of the issues of suddenly taken off medicine for your ADHD and forced to stay off it no matter how many damn doctors/shrinks/pill-shrinks you see explaining your symptoms causing the stress to increase and the flare-ups to become more frequent. The constant vomiting exacerbated an issue a sugary diet may have caused and utterly demolished my teeth little by little. However, thanks to complications from how infected these teeth had become (having been unable to do anything due to co-pay costs, then not having insurance, then Medicaid being a headache to find anyone to be able to get it fixed) which lead to a few hours of pulling, waiting, pulling, blah blah… I was referred to an oral surgeon.
Which is where the Health Insurance Shenanigans begins. I am quite familiar with these shenanigans, as they have been happening since I started. You see, the many different Nevada Medicaid healthcare providers who have insured me will have a list of the different doctors that will take your insurance. It sometimes might even claim to be able to tell you if they accept patients. This would be highly convenient if it did as it said. Instead, whenever I wanted to find a doctor, I would have to go down the list and call them one at a time. The moment Medicaid is mentioned, their tone sours ever so slightly. They tell you that, regardless of what the list on my provider’s own list says, they do not take Medicaid. The other constant was that if they DID, they were full on patients. If the did and they had openings, it is months down the line. When you need to find multiple specialists to deal with multiple issues caused by the same illness, this gets highly agitating. Frustrating as the ones I believed I could complain to like to assure me they understand it as. Why I do not believe them is they also seem surprised at how FUCKING PISSED OFF fucking up my health makes me.
Remember these shenanigans, I will be bringing them up often.
On March 6th, 2018 I received a letter from the allergist, who had been (poorly) helping me with my HAE care, that my care with them has suddenly been terminated. Now, I had only a few months prior FINALLY received from this doctor a pair of highly useful medications. In between the belittling, lecturing, and talking down to I got more than treatment, I finally was prescribed HAEGARDA and FIRAZYR. The first being a medication I WAS taking twice a week. It was rather painful for 15 minutes upon injection, but that cleared up quickly. The other was to be used in the event of swelling, injected like an Epipen (WHICH IT GOD DAMN ISN’T) might be at the moment of attack. With these two medicines, I had been comfortable enough to make my appointment with the dentist in the first place, which after a few appointments before I received the letter had been set for March 23rd.
Suddenly I received that letter, which was soon followed by the provider of the two medicines telling me my YEAR LONG PRESCRIPTIONS with them had suddenly been pulled. Something they were confused about, MUCH LIKE IS WAS. Upon calling my allergist’s office, I learned that the reason had been APPARENTLY I wasn’t taking it. Which is confusing, as I had been, and had only missed the one appointment before the letter thanks to the INFECTION IN MY GUMS I NEEDED REMOVED along with all the other damn issues I was having and trying to mix making me have troubles sleeping and making an early morning appointment. Something that I apparently need to suck up.
This reasoning SHOULD have been easily refuted by the constant deliveries of the medicine TO MY DOOR. The nurse that had come and taught me to use these medicines, THEIR APPROVAL THAT I KNEW WHAT I WAS DOING. As well me having sharps container with plenty of the injection needles I used. They did not wish for any of this, and after angry demands given I HAD A SURGERY APPOINTMENT for my teeth which has a DAMN HISTORY of causing swelling of the throat. So they extended it for 30 days, a bridge period, after constant calls that now just sit in my head like an angry flurry. Mixing them up, but the point is I had to FIGHT to make sure I had enough of the medicine for my blood disease so I could go through the dental procedure with the lost chance of a POSSIBLY FATAL flare-up. Fun.
So, once I was healed up after the dental appointment so I could start calling and get the bottoms removed… The Healthcare Shuffle appeared! This is when I tried to call the Oral Surgeon I was referred to, they said they never received it. I call the Dentist who sent it and they said they sent it to my insurance. I call my insurance and they first said they haven’t received it. Later say they do and sent it but the Oral Surgeon never got it. WHILE all this was happening, a far more problematic issue arose. Keep in mind, this is all happening as I am still getting over the fact I now have these annoying dentures that I am STILL angry over.
The medicine ran out. So, of course, I had to find someone new to prescribe me it. This had the issue of me needing to FIND someone who would do this. The Primary Care Physician that I had was uncertain himself and kept telling me he knew nothing about the disease. After explaining, he referred me to a Hematologist and Allergist… IN VEGAS. (This is 8 hours away from me on a good day or requires an hour and a half plane trip for something I likely need to do multiple times. I live in a city, not a small town. That has MANY ALLERGISTS AND HEMATOLOGISTS.)
Annoyed by this, and after Medicaid Shenanigans, I eventually got an Allergist and a Hematologist referral. Upon calling the Hematologist, they refused! I was highly confused, as they kept repeating that I should go to an allergist. They don’t treat allergies. Hereditary Angioedema is a blood disease. NOT an allergy. Apparently, nothing can be done and I have still yet to see a hematologist. Joy. The reason? Even though I explained extensively this was a genetic blood disease and the symptoms only could be COMPARED to an allergy to stress. IT DOES NOT REACT TO ALLERGY MEDS. An epipen makes the area I inject just swell up yet give me the energy for my skeleton to feel like it wants to run around the block without the rest of me.
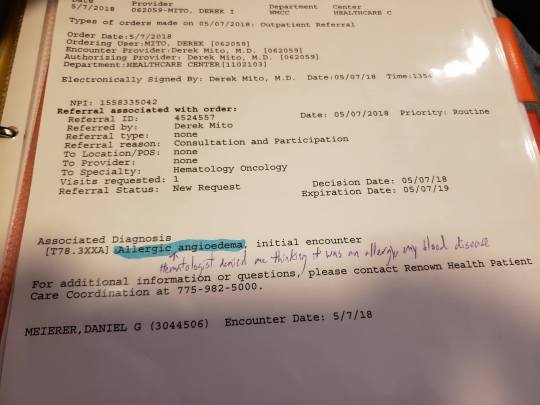
So, not surprising, this caused a lot of issues with swelling. Inevitably, I had an episode involving my gastrointestinal system. This time, it was bad enough I couldn’t seem to use medical marijuana to cover the symptoms until I was well and had water in me. So one Ambulance ride later I am in a hospital bed… Oh, wait, no, I am at the front desk of the emergency room waiting for a bed for a bit. Until I puke enough to be a disturbance. However it still takes quite a while before I get the main thing I want and have been kept from thanks to my body violently puking it up. I wanted an IV with something to hydrate me. The drugs could wait untiul the doctor, but as time went by and it felt like an eternity, I kept being told by all the people checking on me that I had to wait for a doctor to get my damn liquid.
All the while my fiance and my father are both helping explain that this was, without any doubt, an attack from my blood disease. It was an hereditary angioedema attack, blah blah… My discharge papers (useful in tracking my disorder and proving problems.) instead say it is some ‘unspecified vomiting type’ instead of maybe ‘blood disease triggered vomiting’ or ‘HAE triggered vomiting’, ‘genetic disorder triggered vomiting’. Think you get the point, more something that proved the medical staff were actually listening to my concerns. Attempts to fix this so I had proof with disability was met with them saying once that is written down it is permanent.
Then, five months later, it happened again.

Luckily, the Allergist I eventually found turned out to actually have heard and seen a couple others who had this disorder. He knew of medicines and, instead of feeling like I needed to teach my doctors… I was given hope! I was given a vial of Firazyr. He said it was extending an olive branch, and I feel this will be what I remember when I try to think of the emotions needed to write a scene similar. I have never felt hope like I have then. Hope that likes to come and go, but at least I have one doctor at-bat for me.
Until a couple of months ago as of March 20th, 2019, I FINALLY was put on a new medication. Tahkzyro which I take twice a month. HOWEVER, I am still getting push back when it comes to getting the Firazyr, which would help me with my anxiety over the next surgery to remove my bottoms. Which, now that I have Tahkzyro, I once more have to take on HealthCare shenanigans to try and figure out who gets the god damned honor of removing my teeth. As the ones I was referred to HAVE the damn referral… But they don’t take Medicaid. SEEMS THE INFECTION IN MY BOTTOM TEETH GETS TO STAY! Just get to keep draining that thing myself. GUESS WE ARE FRIENDS FOREVER, ME AND THIS INFECTED TOOTH! Though it is crumbling away like the rest. It is down to the gums now. Though, I would like the Firazyr so I can inject myself IMMEDIATELY upon noticing my throat swelling. Never been asphyxiated but something tells me it ISN’T ALL THE FUN AN END! Especially at twenty fucking eight. So you can see my troubles. That doctor is still great, and makes a good point, I just think I need to make myself a bit clearer.
The years feel like they become less and less about me finding my place in this world, healing, and learning but instead more and more about me working as quality control for a broken system with no desire to fix itself. With every passing event involving them, I feel less like a patient and more like the data point I clearly am. With articles full of professionals professionally talking about diseases and medicines without much mention or care for the patients. The ones who that was made for.
For patients like me to heal. Not for people to make money. That is a side-effect of the job they signed up for. To fucking CARE for your goddamn patients. Not be coerced into giving meds left and right (or taking them away as a debate on whether or not ADHD FUCKING EXISTS goes on) or whether you believe the name given to the collection of symptoms I show. My disorders are not Cryptids. I have blood tests, medical papers, and diagnoses. Not blurry pictures of my blood viewed through a slide where fragments of the disease are seen peeking over their shoulder as they rush into a forest of red blood cells.
My particular disorders that I had since birth (ADHD and HAE) were caused by my body’s INABILITY to produce something. So if someone who CAN produce it takes it (least in the sense of ADHD as I doubt anyone else will benefit from a c1-inhibitor. No more than insulin if they aren’t in need of it like a diabetic) then of COURSE something different will happen. Of course, they might get high. That is not my fault as the patient it was made for.
As the point I am trying to make is that I do not feel I have been treated as a patient, I feel I am given more paperwork and calls than a cubicle worker. I feel I have to study more about the laws and practices to keep myself from being further burned. In between the Madness. The Pain. The Suffering that ALL OF THIS has inflicted on me. In between the new disorders this has caused me, particularly my obsession.
All I can think of is how to fix this. How I keep seeing articles, posts, and websites full of cries for help at a broken system. Of people fucked over, lacking their medicine, and the only ones getting the fucking attention are the dipshits who thought that taking someone else’s necessity would be a good way to get high. A good way to ‘focus’. To ‘relax’. While you use that as a fucking excuse to let people like me suffer, and further excuse it by brushing us into a group of people who just ‘slipped through the cracks’.
This obsession has grown now. Especially from the subject of the next article, ADHD meds from the perspective of someone who was one them from the age of 5, had them taken somewhere between the ages of 16 and 20 (my memory is incredibly hazy in this period thanks to the damn medicine being taken away) and getting only mild relief from marijuana replenishing my Dopamine… But that isn’t all Marijuana does nor all ADHD needs. I FINALLY am being treated, though it is just beginning. Still need to find MY medicine. It only took a decade for them to admit they were screwing with me. The lengths of my rage, again, is the subject of the next article.
This one was about how this madness turned me into someone who believes his job is to be a Professional Patient. Being talked into long commutes, long waits waiting for a doctor who will drop you for being late when they are constantly 45 to an hour late. Constantly filling out paperwork and debating about the fact my problems EXIST. Being treated as too young to be suffering. To the point, I don’t know what else to do. When you are too fucked up to work, explained in an earlier article, too fucked around for college, and the only thing you can apparently do is smash your rage against a keyboard and hope spreading your story around for no one to read will get something done.
If not? Then no matter what happens. If I die from malpractice or my disease, if I am killed, if I am silenced. My words on how this bullshit has made me feel will be, hopefully, somewhere.
The internet is notorious for being difficult to clean thoroughly, after all. If you do a little light digital legwork with the intention of being annoying as all hell. Especially since I got denied for disability again. Next time, I have to go to federal court apparently. JOLLY GEE GOODIE.
#nonfiction#Medicaid#Hereditary Angioedema#genetics and heredity#disability#us healthcare#us health insurance#reno#renown#suffering#blood disease#disease#rant#medical malpractice
1 note
·
View note
Text
I Had 6 Months of Therapy, and Now I’m Ready to Tell You How People Slowly Go Crazy
New Post has been published on http://www.infolibrary.net/i-had-6-months-of-therapy-and-now-im-ready-to-tell-you-how-people-slowly-go-crazy/
I Had 6 Months of Therapy, and Now I’m Ready to Tell You How People Slowly Go Crazy
Hello, my name is Katya, and today I will tell you about my experience of visiting a psychotherapist. Spoiler alert: I did not hear any mysterious voices in my head and I didn’t think there was some kind of a world conspiracy. It’s just that at a certain time in my life, I couldn’t figure out the point of living or find pleasure in my life anymore and I couldn’t navigate through these feelings on my own.
I will share my psychotherapy adventures with Bright Side readers and I hope that my story will help someone to find peace with themselves. Or at least this story can help you take your first steps toward a normal life.
How I ended up going to a psychotherapist
This is what I looked like before I was sad all the time.
In 2012, at the age of 28, I became a widow. Nothing could have predicted what happened. We were a regular family raising a boy and I was pregnant with my second child. But in just several days, my life changed completely: my young husband got ill and died in just one week. So, there I was, 9 months pregnant and alone with a 3-year-old child.
Nothing changed around me: the sun was still there, the birds were still singing, and people went to work. I didn’t think I would be depressed — just because I had to be strong.
Of course, I was in mourning, I was shocked: how could something like this even happen to me? But now, 7 years later, I realize that I was sort of in a spacesuit: all the feelings I was having were kind of blunt because I wouldn’t let myself relax. I closed my heart to pain, I learned not to cry, and, as I found out later, I shouldn’t have.
This was me when I was depressed. Where are my cheeks?
Depression caught up with me when I thought I had already overcome my loss. I lost 45 pounds in one year — I just didn’t want to eat. And once, I thought that I had cancer or some other terminal disease. I became obsessed: I started looking for the “suitable” symptoms online, I went to doctors, but they couldn’t find any diseases. I was absolutely sure that I had something terrible and that I would die any day, so I took my temperature like 5 times a day, I looked for rashes or other spots on my skin, I even constantly checked my lymph nodes.
Once I felt like my heart was beating so fast that it was going to break my ribs. I was sweating, my hands were shaking, and I wanted to run somewhere. I thought something terrible was about to happen and I did not realize that this was my first panic attack.
My body kept screaming, “I’m hurt,” and I was breaking apart, but I didn’t want to acknowledge it and I thought it all would go away. And it was only when my clothes became several sizes bigger and I couldn’t get out of bed in the morning that I realized I needed a shrink.
I started searching for a good doctor online. Actually, psychotherapists are very expensive, but at a local hospital there was a specialist I could visit for free. Anyway, I had nothing to lose, so I decided to go and this was the start of my path to healing.
I visited the specialist for several months. Together, we found out that I had a reactive depression. This is a kind of depression, but it’s different from others. Usually depression is based on something that a person had in childhood, and this disorder is the brain’s response to a traumatizing experience.
I hoped that the doctor would just prescribe some antidepressants and let me go, but this is not how therapy works. In order to get rid of depression, you need to work on it.
This is what I realized after 6 months of therapy:
1. Realize that you’ll need more than pills to help you.
There is no such thing as a magic pill. There just isn’t. There is no pill that can make you happy. My therapist compared antidepressants with crutches. When a person breaks a leg, they have a bandage and crutches in order to be able to move. But this is a temporary solution: sooner or later they will have to ditch the crutches and learn to walk again.
The same goes for pills: they can remove the symptoms (like anxiety and fear), they can help you get through the darkest days, but they won’t heal you. Without the right therapy, you can take pills for years. Seriously, I have met people who are like foodies, they know all the different types of antidepressants. In order to get rid of depression, you need to do a lot of work.
2. Sometimes it hurts.
During my first sessions, I realized that I didn’t want to live. I didn’t have any plans for more than a couple of days. Why? We all will die one way or another… I didn’t see the point of doing a renovation or go to a hairstylist. Even taking a shower didn’t seem like a necessary procedure.
I had to learn to want to live. I had to. My therapist and I made lists of plans, I drew what I planned to do in the future. And also, I had to learn to control my negative thoughts. This can be really hard and really painful.
3. Only trust someone who is a medical expert.
It is best to trust a medical specialist who has a special education — a doctor can help you find the reasons for your problems and recommend the right treatment. Depression is a multi-faceted beast: sometimes it’s the hormones, sometimes the brain lacks serotonin, and sometimes, it’s about traumatizing experiences. A doctor can get to the bottom of it and find the best approach.
And most importantly — when someone has panic attacks or depression, they need to have a full medical examination like with an ECG, a neurologist and an endocrinologist, and they need to have their lungs checked. It is amazing how some diseases can pretend to be depression. So, while you are wasting time on the therapy, your health may be getting even worse.
4. People around you won’t get it.
Most people around me thought that all of my suffering was caused by the fact that I had nothing to do. Only lazy people have depression. “Drink some mint tea, get some good sleep, buy some new shoes and your depression will go away,” everyone around me said.
I’m glad I didn’t listen to them. Nothing made me happy and I was afraid of getting out of bed in the morning, I had panic attacks — and all of this was caused by laziness? And then I realized something, in order to admit that you are weak, you have to be brave. And in order to start treatment, you need to be 100 times braver. Don’t listen to anyone. And don’t follow their advice.
5. Recovery can be extremely slow.
Some of the recommendations from your doctor can seem completely silly. A psychotherapist might recommend that you start a diary, make a plan 3 years in advance, or draw a picture. I thought, “How is this supposed to help? Give me some pills and I’ll just go home.”
The thing is, all of these things really work, you just don’t notice it. The next morning, or a week later, I didn’t feel better. I didn’t understand that I was doing better until months later. I think that even the specialist didn’t know if it was going to work or not.
6. Setbacks are a part of the treatment.
Sometimes, it gets worse. “How can this be? I do visit the doctor, I do follow the recommendations, and I still don’t feel like laughing…” It’s okay to have setbacks. It is totally normal. You can’t do something big in just several days. You have to be patient and persistent.
7. A specialist won’t think you are insane.
People are often scared of visiting psychotherapists because they think it makes them “crazy” or something like that. Well, it doesn’t. It only makes them strong enough to realize that they have a problem and are willing to solve it.
8. It may be unpleasant to find out who you really are as a person.
Psychotherapy is your chance to get to know yourself better, but you might not like what you find out. I realized that my depression was based on anger and aggression. I was angry with my husband who died and left me alone with my children. I was angry with women who had husbands and children who had fathers. I was definitely the most unhappy woman in the world and I thought nobody could understand me.
9. Depression can come back. And it most likely will.
Just like drug and alcohol addiction, depression can return. Psychotherapists are not wizards, they can’t make you a totally different person, but they can give you the tools and the skills to overcome these situations.
There is no way you can become a superhuman who is never sad and doesn’t have any psychological problems. But you can learn to live in peace with yourself, deal with your problems, and explain certain things to yourself if you have to.
10. A sense of humor helps sometimes.
You should not “worship” your depression. Yes, it is a disease and it has to be treated. Don’t let it conquer your life. When you have a cold, you don’t pay much attention to it. When you have a problem, you need to solve it — that’s it. Don’t get desperate.
My sense of humor helped me tremendously. Sometimes I thought I was losing my mind. But I kept thinking, “Okay, I’m going to a mental hospital, at least I won’t have to do any cleaning, laundry, or other things.” Sometimes sarcasm is really healthy.
The conclusion
I visited a psychotherapist 6 years ago and I regret nothing. His recommendations helped me get out of a very difficult place and now I know how to avoid desperation. My experience was very positive, so when someone I know has signs of depression, anxiety, and other problems, I recommend that they see a specialist.
It is amazing how many people try to ignore these problems just because they think they might seem “crazy” to others. And some people are scared of psychotherapists and think that they’re going to put them into a hospital and inject them with tranquilizers or something like that.
Don’t be afraid of asking for help!
function runAnalytics() []; _comscore.push( c1: "2", c2: "19962933" ); (function() var s = document.createElement("script"), el = document.getElementsByTagName("script")[0]; s.async = true; s.src = (document.location.protocol == "https:" ? "https://sb" : "http://b") + ".scorecardresearch.com/beacon.js"; el.parentNode.insertBefore(s, el); )();
Source link
0 notes
Text
My Journey To Diagnosis
Endometriosis is a chronic, systemic inflammatory disease that doesn’t have a cure. 1 in 10 women have endometriosis, yet it is one of the least researched and understood diseases. Average time of proper diagnosis is 7 – 10 years. I began experiencing symptoms of Endo when I was 13, yet didn’t get a diagnosis until I was 27.
Endometriosis acts like a cancer as in the cells rapidly divide, grow and invade any surrounding tissues and organs. This causes a lot of internal bleeding and severe damage to organs accompanied by unbearable pain.
I went through this pain for more than 10 years before I was diagnosed with Stage 4 Endometriosis. Every month I would take 2 – 3 days off from school during my cycle. Curl myself in bed, unable to eat anything and if I did eat something, I will vomit which makes the pain worse. I have a twin sister who have normal periods. My mum would always compare the two of us and give extra attention and care for me. Years passed by and my pain was getting worse. I was rushed into A&E several times during college and uni days. I’ve been to so many hospitals and seen countless number of doctors. Every doctor concluded the case with just a ‘bad period’.
After graduating in BA Accounting and Finance, I got my first job as an Accounting Assistant. I didn’t want this horrible illness to interfere with my new job so I managed to get some temporary medication to balance my hormones. My GP prescribed me with contraceptive pills which is a temporary cure to help with the pain. Even though it had several side effects such as migraines, mood changes, nausea, night sweats, etc, I managed to adjust to it.
Three years passed by, I was almost 25 and was getting ready to get married and move in with my childhood sweetheart. I’ve been with my husband since school days, for more than 15 years now. Both our parents accepted our relationship early which made things easier for us. We both agreed on starting our family as soon as we get married as we had no reason to wait. So, a year prior to our wedding, I decided to come off the contraceptive pills to bring my hormone levels back to normal and prepare my body to conceive. I had to go through several months of painful periods without the pill, in hope that I will be able to conceive as soon I get married and I will have a break from periods while I am pregnant. However, things did not go that way. I was rushed into A&E several times between this time when I have severe pain. I had to take time off from work frequently but was unable to explain the actual reason at work as I was not diagnosed then.
I went through depression because I was unable to lead a normal life and had no idea what was going on with my body. I was unable to continue my job as I was going through this unexplainable pain and confusion. To divert my mind from all this I decided to quit my job and take on my passion and started this Makeup Artist journey 2 years ago in March 2017. The reason I chose this job is because it does not hold a schedule the way that most other careers do. Every job has it’s own call time. Some may be in the middle of the night and some could be in the middle of the day. I love being able to set a schedule of my choosing. You can accept the jobs that coincide with the life you are living and refuse the ones that are not. In other words, you will be working to live around your schedule, not living to work around someone else’s, which was totally convenient for me. One good thing about my periods were that my dates were pretty regular. So, I avoid taking bookings around those dates. Even then, I had two awful experiences where I had to work in pain as my dates messed up.
One occasion was when I was booked for a Bridal Saree draping job in Central London. Total cost for this job was only £100 including travel since I was new to the wedding industry. I usually drive to my jobs but in this case since I was unable to drive due to the pain, therefore I had to take a cab to the venue and back home, which cost me over £150. I didn’t eat or drink anything that morning because I usually throw up when I’m in pain. Even then I brought a couple of carrier bags with me in case I threw up in the car but thank god I didn’t. I had no other choice because I respect my job and I cannot let my client down on the day of the event and break the trust.
Later on another occasion, I was booked for a pre-wedding photo shoot in Cornwall, which is roughly 5 hours drive from my place. I didn’t want to travel alone as I had to stay over for a night so my husband accompanied me on this trip. I was looking forward to this job since it was my first job far from home and to make it more special, my husband was with me. But the happiness didn’t last long at all! On our way to Cornwall we took a break in-between to have lunch. When I went to refresh myself, all my excitement was flushed away in the toilet as my period came a week early.
Luckily, we were next to a petrol station, so I managed to get hold of sanitary pads and painkillers. I was praying to God to give me strength to bare the pain for the next couple of days.
First Pre-wedding look was scheduled to be shot that evening so once we arrived at the hotel, I unpacked my kit and got the bride-to-be ready. The pain was bearable, so I managed to do my job with less trouble. But the pain was increasing slowly and I had a sleepless night in fear worrying about the next day. The following day I was scheduled to do two different looks, one in the morning and one in the afternoon and head home in the evening. The pain was unbearable in the morning. I had to take several breaks in between to vomit because that’s one of the worst parts of my severe period pain.
More than the pain, it was extremely embarrassing in front of the new people I just met and I couldn’t explain the name for my illness because it was just a ‘bad period’ like the doctors named it. Never the less, I managed to complete my job and my client was happy with the looks I created which gave a satisfaction before I left to head home.
That 5-hour car journey home with my husband is the most unforgettable journey in my life.
I wanted to cry out all the pain I was holding that I couldn’t show in front of everyone. The pain was intolerable, and I was crying through out the journey. At one point, my husband lost his patience and began to get frustrated with me. Like every other person, my husband trusted the doctor’s words that there is nothing wrong me and it’s just a bad period. So, he assumed my pain is normal like his sister’s and every other girl’s but I’m exaggerating and making a drama. That’s the day I felt the meaning to ‘Words hurt more than actions. Actions hurts our body, but words hurt our soul.’
Initially he was very supportive when I decided to quit my Accounting job and was happy to support me financially as it would take time for me to grow in the wedding industry before I can start doing bridal jobs. But watching me go through pain during my job, he assumed I’m not even able to do that simple job. He shouted ‘Stop crying and overdramatising, It’s better for you to quit everything and sit at home and do nothing because that’s all you’re capable of doing. Your voice is irritating me, if you don’t stop crying, I will get off the car and walk home.’ I had no strength to respond since I was mentally and physically drained out.
We finally reached home. My husband opened the house door for me and left. I filled a hot water bottle to ease my pain and curled myself in bed. I really wanted to get some sleep to rest my mind and body but all I could hear in my mind was my husband’s words repeating how useless I was.
I began to judge myself through everyone else’s eyes. I started to doubt myself whether my pain is real or am I over reacting. The one and only person I wished who would trust me and give all the love and support even doubts my pain, this led me into making wrong decisions. I couldn’t imagine living with this pain for the rest of my life, so I decided to take my own life. I took the 12 pain killers that were left in the new pack I bought the previous day and went to sleep in hope that I will not wake up the following day. But little did I know that my body was strong enough that exceeding the stated dose does nothing to my body. I was perfectly fine the next morning. I sat my husband down and told him how hurt I was by his words and it led into taking the tablets last night. He felt extremely bad about what he did and apologised. Soon things were back to normal between us.
Never in a million years did infertility cross my mind so after several months of trying to conceive, without any positive results I began to have serious concerns. I explained the situation to a new gynaecologist at my GP surgery, who was also an endometriosis specialist. After a scan, I learnt I had a large cyst on my left ovary that needs to be removed (laparoscopic) surgery which could increase my chances of getting pregnant, but I was told I may lose an ovary. My husband and I decided to do it as it would also help my pain.
Following my operation, my surgeon explained she had removed the cyst, managed to keep my ovaries intact, remove my left fallopian tube which was totally damaged and there was much more than that. I was diagnosed with Stage 4 endometriosis!
There are four stages of endometriosis: minimal, mild, moderate, or severe endometriosis.
Minimal endometriosis also called stage 1 endometriosis and is characterized by isolated implants and no significant adhesions.
Mild endometriosis (stage 2) is characterized by superficial implants that measure less than 5 cm in diameter without significant adhesions.
Moderate endometriosis (stage 3) involves multiple deep implants, small cysts on one or both ovaries, and the presence of flimsy adhesions.
Severe endometriosis (stage 4) this is the final stage. consists of multiple deep implants, large cysts on one or both ovaries, and thick adhesions. In addition, infertility is likely with stage 4 endo.
I was given pictures of how a normal women’s reproductive system would look and how my one looked from the pictures they took during the surgery. Everything was explained clearly and all my questions were answered. But there was something that I was not ready for. I had to wait 6 months to heal from this surgery and would need to under go another surgery to remove the rest of the endometriosis. My surgeon also confirmed that I will not be able to conceive naturally due to the damages caused by endometriosis so our only option is IVF. But there is only less than 0.8% chance of success.
I felt a slight relief after the surgery having more knowledge about my illness and was preparing myself for surgery number two. I was told having normal periods between the two surgery could cause more pain and damage to my organs, therefore I was on an injection called ‘zoladex’ to stop my periods are prepare my body for the next surgery which is much more complicated compared to the previous one. There are several side effects related to this painful injection: hot flashes, sweating, migraine, dizziness, mood changes, bone pain, nausea, vomiting, diarrhoea, loss of appetite, sleep problems (insomnia), and much more. I managed to overcome all this and currently recovering from my second surgery...
0 notes
Text
Interview #7
14/3/19
Tell me about a time where you started feeling symptoms. What did you do? How did you feel in that moment?
I started feeling symptoms at work and I went to the doctor the next day
I felt concerned cause my foot hurt (ran over with a trolley)
I was stressed cause I had to take time off work but was also happy cause I get time off work *laughs*
I was just annoyed mostly, it was a hassle
How important is it to you to get symptoms checked out?
Only if they’re debilitating, you can’t walk or function, it’s actually causing you issue outside the issue
If it’s minor I ignore it till it goes away. Don’t wanna spend money on a minor injury
Longest I’d wait is a week
I try to wait for it to get better
Can you tell me about your healthcare provider?
Doctor by appointment
I haven’t thought about whether they’re a GP? Hasn’t come up whether they’re a doctor or a GP. I don’t know what the difference is. I thought a GP is just a doctor
There would be specialist doctors then a GP would be all-encompassing. You see a GP then they refer you to a specialist
Booking an appointment process
I just call them up and say I wanna book an appointment for e.g. Friday, they say we have these times available and I just pick a time and it’s done
The time is always early morning (not close to when I’d wanna be seen)
Wait time to be seen
At least half an hour but usually half an hour. It kinda depends on the day
Importance of seeing one doctor for all checkups
No, they’re all the same to me
I’ve never had ongoing issues that you need the same doctor to know about
They don’t ask me about much
Most recent GP visit, what were you thinking? How were you feeling?
Driving to doctor: I was very stressed because it was down Lincoln road (busy) I had to be there by 9:30, I left at 8:30 didn’t get there till after 9:30
Motorway was blocked, all other routes were blocked. Took me ages to get there
Got to the clinic: I was a bit relieved. I was only 15 minutes late and I only had to sit down for about 10 minutes before the doctor was there but that was cause it was already booked. For A&E you wait half an hour at least
If I got there on time it would’ve been pretty much instant
Got into the doctor’s room: It was pretty good cause he just talked me through how my injury was feeling, showed me how it was and told me when I could go back to work. But this was more of like a follow-up
What about the first time you went there for you injury?
A&E and it was middle of the day (but 9:30 that I got there)
Packed, a lot of other people
Took an hour for me to be seen, another hour for an x-ray and then about 20 minutes after that to be seen again
Took a really long time and they don’t give you painkillers
Reception service
Accomodating, was good
Duration of check-up
Follow up was a lot quicker, was just an x-ray and no one was there
If it was busy it would’ve taken ages but it was smooth
How well does the doctor explain solutions/what to do from there? Were you able to clearly understand?
They were really thorough, told me not to walk and use crutches
Anything you might have forgotten to bring up?
Nah
Was the doctor able to explain clearly the side effects that could be involved in taking medication?
Yeah, they told me not to take more than 2 codeines cause it makes you drowsy and take Ibuprofen with food as it can give you digestive problems
They were really thorough
Significant clinical experience
Nah, there’s nothing
Every doctor visit is just the same
You just go in, wait for ages, you see the doctor, and then you say “this is wrong with me” and doctor goes “yeah that thing is wrong with you” and then they’ll give you medicine and that’s it
I’ve never needed to go for repeated visits, just check-ups and if I’m injured but in that case it’s all sort of done for you
What’s the ideal doctor for you?
One that asks questions, knows what to ask and knows your medical history well
Are you open to your doctor and honest? Naturally talk a lot?
I need them to ask me questions. I only ever tell them about the injury I’m there for I don’t bring up anything else that could be an issue
Cautious with medication?
I don’t really ask them because they tell you side effects but I do research online to see what other people say - broader
Sometimes what the doctor thinks what the side effects could be aren’t what you might have, you could have different symptoms
This is after I take it home and I look it up
They prescribe it to you so you can’t say “no I don’t want the prescription”
They’ll tell you whether or not it’s good for you
I don’t have a normal GP
Quality of care versus cost
Extremely expensive and check-ups aren’t that great
There’s one doctor who’s pretty good and easy to talk to
But the other doctor I got was so dismissive, didn’t seem like they cared about what I wanted them to see me for
Made me feel like I was wasting my money
Paying $90 to be told nothing’s wrong with me when I have an issue
I don’t complain
I have considered going to a cheaper doctor but not tried to look
I’ve heard about others and that makes me wanna go see them instead
Factors for choosing a doctor
Price and how close they are
Family GP?
Every single one of us were at the same medical centre up until 5 years ago
We all switched once we became adults
Student support for healthcare
I did not know about these
I feel like I’m getting swindled not having known
I think it needs to be made more explicit if you can get it cheaper
Make it known. I’ve never heard of it
If I haven’t heard it how can everyone else?
Satisfaction
4 out of 10, it’s very expensive
Thoughts on NZ healthcare system
It’s really hard to find a compassionate doctor, one who’s interested in helping you
A lot of the time you go in and it feels systematic, “here’s my symptoms”
This is what’s wrong, here you go then you leave
Never feels like they want to figure out what’s wrong with you, they just want you to tell them what’s wrong with you and they prescribe the medication
Personal reflection: Again, this interview was a bit shorter and the interviewee would finish answering quickly and wouldn’t naturally elaborate on his statements. I had to poke and prod to get more insights and in doing so, I found out that this interviewee had more negative experiences with their healthcare provider in the past which I will use to compare and cluster with what others said.
0 notes
Text
Asclepius the God
It is a long time since I last posted here. I have to find some flow again, so please forgive me if the following is a bit disjointed. It also starts with a physical ailment, which is uninspiring (and elderly), but it is merely a way in…
I have, for some time now, been suffering from lower back pain. It’s nothing dramatic, just a constant dull ache. But it is enough to kill my enthusiasm, in a very general way. Taking the dog for a walk, watering a plant… they become an effort rather than a pleasure.

There are different theories about the etiology of lower back pain. Some people say it is stress related (and, in my case, it came on at a time when I felt very tense). A friend of mine who is a practitioner of Traditional Chinese Medicine was more precise: it is specifically related to money trouble. The spine specialist in London was true to his scientific roots and diagnosed, with the help of an MRI, ‘mild joint effusions at L 4 – 5’. I asked him about the effects of stress. He said that stress and tension could make a problem worse, but that they could not be the cause of it.
I saw a chiropractor and an acupuncturist, neither of whom were able to effect any lasting improvement. In the end, the spine specialist prescribed painkillers, anti-inflammatories, and a course of physiotherapy. I followed this conscientiously over a period of months, also to no avail. Eventually, I went for an expensive cortisone and anaesthetic injection into the spine. The symptoms went away for a month, but as soon as those chemicals were no longer present in my back, the pain returned. I began to feel that I would just have to live with it; manageable, but joyless.
Here in Athens, a friend told me about about an ‘energy healer’ who had helped her a lot, and who was in any case an interesting individual. I thought to myself that I had nothing to lose, and I asked her for the healer’s contact details.
A week later, on a cold and drizzly February morning, I rang Iannis’ doorbell on a street in Pangrati - a comparatively quiet area of central Athens. Iannis came to let me in. He was a diminutive, smiling man in his late sixties or early seventies, with a lively, engaging manner.
We went into his apartment which was small, modern, and perfectly ordinary. On the walls were a few of those tricksy landscape paintings that are sold by street artists. I was about to launch into a description and history of my complaint, which so far I had not told him anything about, when he stopped me by holding up his hand. ‘Let me diagnose you,’ he said.
I then stood in silence, fully clothed, in front of Iannis, while he put his hands lightly on my shoulders for a few minutes. Eventually he said, ‘You have lower back pain, a problem around vertebra 04, and you have had trouble with your right knee in the past.’
I was blown away by this. He was right about the knee too, it was a rugby injury that had plagued me for about 2 years. While driving, the pain used to force me to stop the car every half hour to stretch my leg. But that was more than ten years ago, and since then I have not had any knee trouble.
‘Do you also sometimes feel that your heart beats irregularly?’ he asked. ‘No,’ I replied truthfully, and my belief in his omniscience diminished a little, though it is possible that he is right and I am not aware of it. He then said that my lungs were not breathing properly, owing to a problem some time ago. This is also true, I got pneumonia a few years back. He seemed to think that this was the more serious problem, since it affected the amount of oxygen in my brain and therefore also my general mood. But he thought that he would be able to treat all of these problems. When I asked how many sessions would be necessary, he blithely replied, ‘Just one.’
Iannis told me that he used a form of energy manipulation. ‘Like Reiki?’ I asked. ‘A bit like Reiki,’ he said, ‘but this is an ancient Greek technique, in the tradition of Asclepius, the God of medicine and healing. It is not written down anywhere. It has been passed down through generations of practitioners, but there are not many of us these days.’
Iannis told me to lie down on my back on his sofa with my eyes closed while he performed the energy manipulation above me. He told me to report anything I saw or felt, particularly any colours I saw. It lasted for about half an hour. Frankly, I did not see or feel a lot. Perhaps some warmth in my hands, and a slight vibration in my solar plexus. I saw a few greens and reds, but I could never be quite sure that I wasn’t imagining them, or willing them into being. But each time I reported a colour or a sensation, Iannis would respond with an encouraging, ‘Yes, very good.’
The treatment ended with the painful massaging of three pressure points, two on my left foot, and one near my heart. Then he asked me to stand up and walk around the apartment. I did feel a lot better, though the pain from my back had not gone completely.
I asked Iannis how he had performed the initial diagnosis. He said that it was by knowing himself very well, and then by sensing the energy of another person through various sense modalities, including sound and smell. He said that it was not so much a gift as the result of single-minded dedication over a lifetime. He reiterated that what is absolutely fundamental is self-knowledge; only on that basis can one come to know others. That is rather what I think about psychotherapy.
I paid 70 Euros and left his apartment. It was still raining outside, so I decided to wait it out and treat myself to a coffee. As I sat in the café, the ache in my lower back returned, as persistent as it had ever been.
*
Some months later, I felt I needed to escape the summer heat of Athens. I got on my motorbike for a weekend trip to visit some of the Mycenaean sites in the Peloponnese. The Mycenaean culture was dominant from about 1600 - 1100 BC; it consisted of a number of small independent kingdoms – Mycenae, Sparta, Argos, Pylos, Tiryns, Midea, Thebes, Athens and a few others. This was the period subsequently made famous by Homer in the Iliad and the Odyssey. It is the factual basis for the myths and legends that he committed to paper between 500 and 1000 years later, and also the period that saw the birth of the first attested form of written Greek (called ‘Linear B’), which predated the Greek alphabet by several centuries.
I crossed the Corinth canal and then followed the small country roads down to ancient Epidauros. This was once a sanctuary of Asclepius - a site of pilgimage and the most famous healing centre in the ancient world. It comprised the temple of Asclepius, a hospital, a 160 room guesthouse, a bathing complex, a 14,000 seat theatre with near-perfect acoustics, and a sports stadium used for quadrennial games.

The 14,000 seat theatre at Epidauros.
There were few other visitors that afternoon and it felt like a magical place. The pine trees appeared to pulsate with health. Beside the Temple of Asclepius are the remains of the rectangular Abaton; patients used to sleep in this building in expectation of a visitation, in their dreams, from Asclepius the healing God, commonly believed to take the form of a serpent. The God would advise them what they had to do to regain their health.
Beside the Abaton was the circular Tholos, the foundation walls of which formed a labyrinth that was used as a snake pit, full of harmless snakes. The pit may have served as a primitive form of shock therapy for the mentally ill. The afflicted would have crawled in darkness through the maze-like structure, guided by a crack of light towards the middle, where they would find themselves surrounded by writhing reptiles. One would need a very strong constitution not to find that shocking.
In the museum there was a sculpture of Asclepius holding a staff with a snake wrapped around it. This is the famous ‘Rod of Asclepius’ – the symbol of medicine and healing arts that is still used around the world today (it should not be confused with the caduceus, the staff of Hermes, which has two entwining snakes and is more properly associated with commerce). Asclepius is also often depicted with a dog by his side, and some healing temples used sacred dogs to lick the wounds of sick petitioners.

Asclepius and his snake-entwined rod.
Wandering around this peaceful temple complex, I wondered about the role of snakes in healing. It is a major theme in Amazonian shamanism. Snakes are probably the most common motif in Ayahuasca visions, and they play a significant role in the cosmologies and mythologies of many indigenous cultures. And indeed in our Western mythology too, going back to the serpent in the garden of Eden. Why are snakes so significant, and why are they associated with medicine and healing across cultures? I would like to know (there is an interesting theory in Jeremy Narby’s Cosmic Serpent, to do with the double helix of DNA, though it would seem to apply more accurately to two entwined snakes, rather than just one).
There was an area of shade at the back of the rectangular Abaton. Hanging on the wall was a photo of a relief sculpture from another Asclepian sanctuary (at Piraeus), depicting the kind of healing that may have gone on in this building. A patient was lying on a couch, and a healer, or perhaps Asclepius himself, seemed to be performing some kind of energy manipulation above him. It could have been me on Iannis’ couch.
Relief sculpture from the sanctuary of Asclepius at Piraeus
*
From Epidauros I drove to Nafplio. For 13 years, this small seaside town was the first capital of modern Greece, from the start of the Greek War of Independence in 1821 until 1834. At that time, as photos attest, Athens consisted of little more than ruins surrounded by a few farmhouses.
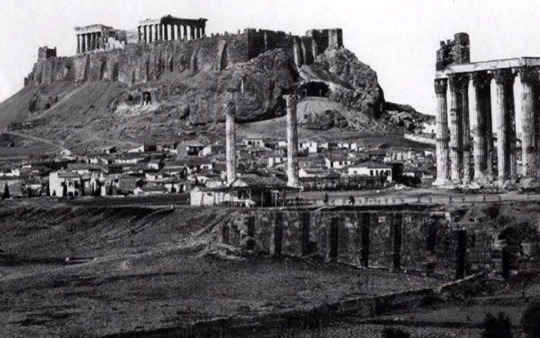
I spent the night in Nafplio, then visited the site of ancient Argos the following morning. It is on the outskirts of town, rather hard to find. Entry is free and the theatre is impressive, but less so than Epidauros. Then I pushed on to Sparta, down to Kalamata, and finally up into the foothills of Arcadia.
In the early evening I passed through modern Megalopolis; it is a nowhere sort of place – an empty main street, a series of traffic lights, and strong winds - but in ancient times there was a huge city here. From the road a few miles outside the modern town, I saw three Ionic columns standing unremarked in the tall grass of a tawny field, and behind them a flock of sheep and their shepherd. Who placed them there, and why? What were they once a part of? Which God was worshipped there?

I spent that night in the hillside village of Karitena. The night was blissfully cool after the sultry nights in Athens. The following morning I had to wait for the mist to clear, then I followed small, winding roads into the forested hills of Arcadia. I crossed the river Alpheus on an small stone bridge – Alpheus was probably the basis of Alph, the ‘sacred river’ that Coleridge glimpsed in his opium-inspired reverie, and whose ready-formed verses he subsequently committed to paper as the poem Kubla Khan.
I thought of the resonance of Arcadia, the traditional precinct of the nature god Pan. For later Roman poets, Arcadia was linked to the Golden Age - a time of innocence and primordial bliss, before the rot set in. Virgil claims Arcadia as his own in the climax to his Eclogues.
Arcadia came to be known as ‘Arkady’ in English, though Evelyn Waugh reverted to ‘Arcadia’ for the title of Book One of Brideshead Revisited: ‘Et in Arcadia Ego’. This is a memento mori in which Death is warning us that he will find us even in Paradise – the skull is forever grinning in at the banquet. But, one has to wonder, is that not what gives the meal its relish?
My GPS ceased to function on these tiny roads, and I was soon lost and had to retrace my route. But it was a beautiful drive and I felt profoundly grateful to live in Greece.
0 notes