#Introduction to RCM
Explore tagged Tumblr posts
Text
Revenue Cycle Management (RCM) is not a one-size-fits-all solution; it's a complex tapestry of essential components working together seamlessly to achieve financial stability and success for healthcare organizations. Let's explore the three key components of an effective RCM strategy in more detail.
0 notes
Text



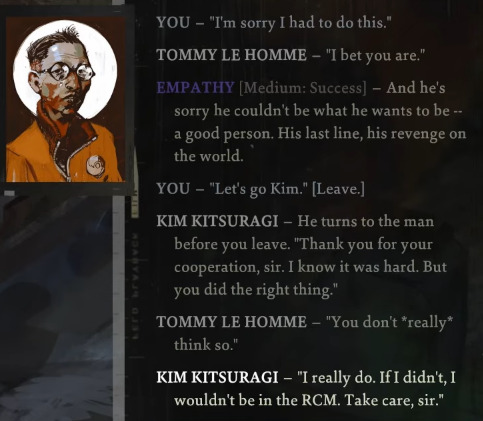


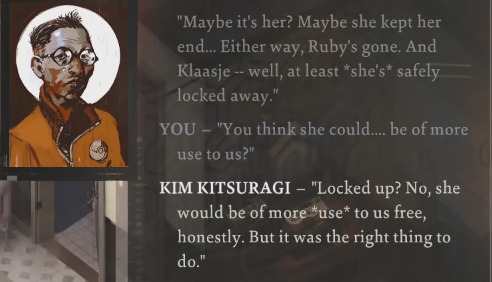

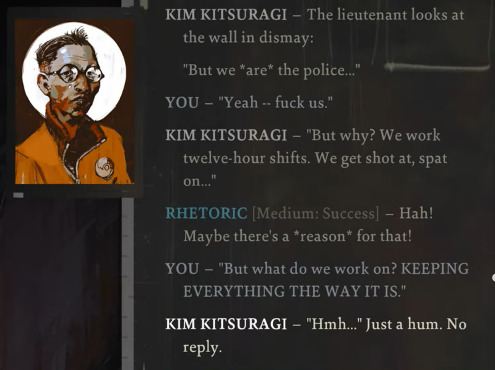

The radicalization of Kim Kitsuragi
#disox Elysium#kim kitsuragi#harry du bois#de#de meta#his radicalization through the game is so subtle and quiet but it's there... a man finally looking at the ground he built his whole life on#< posted this tag on a kim quote a few days ago and it seemed to resonate with people.. and i thought id make a compilation to point it out#i think a huge part of kim's arc is the introduction of doubt into his life via harry and his amnesia. suddenly kim- the image of certainty#and purpose- the one who always knows the right thing to do- mister i believe in the rcm- is invited to question everything. and the ground#shakes beneath him. rattling his carefully constructed life. not an earthquake- but for the first time in a long time he starts to believe#that real change is possible. and it is. IT'S COMING.#juha.txt#🏺
637 notes
·
View notes
Text
I’m fascinated by how variations of Sea Power's “Want to Be Free (Remix)” provide a musical theme for death and endings that follows Harry and his foils throughout Disco Elysium.
The first place you hear it is as “The Field Autopsy” while inspecting the Hanged Man’s body. It's barely recognizable as the original song, though. It's sluggish and muddy and bilious. The piano melody has been lowered and sustained to an ominous funereal organ and combined with deep strings. A lilting viola line in the lush layers of the original "Want to Be Free" is isolated here and contrasts with the low organ, rising like the stench off a corpse. If you do the autopsy first thing as Kim suggests, Harry – freshly, grotesquely awakened from his apocalyptic bender – is not in a much better state than a corpse himself.
The music underscores a visceral scene of death and decay, our introduction to the Hanged Man, the first of Harry's foils. Both Harry and Lely are agents of state-sponsored violence as a cop and mercenary, respectively. They bear similar physical scars from the neglect of the systems they grew up in. They both desperately want to escape the horrorshow of their lives, using drugs and dark fantasies to cope with the terrible things they see and do but finding little more than self-destruction in the nihilism. The Bloated Corpse of a Drunk taking the Hanged Man's place in Harry's first night dream makes their connection explicit: you should be dead, Harry. This may as well have been you.
The next place you hear a variant of "Want to Be Free" is in the washerwoman's shack in the fishing village. “Live With Me” is wistful and melancholic. The gentle piano and cooing vocals evoke the wind and waves on the bay, an escape calling outside the salt-rimed shack. But this is a place of death, or at least its potential, as the return of the high viola from "The Field Autopsy" reminds us. This is where Ruby hid when Harry's arrival made her fear for her life, where she contemplated killing herself if things got even worse. This is where Harry can end up if no one vouches for him at the RCM tribunal finale, where his wounds will grow infected without medical care, where there is little left to do but return to drinking and wait to die.
But true to the song title, the shack also offers Harry the possibility of learning to with himself as he emerges from his bender. Here is a mirror free from the damage and trauma of attempting to destroy himself where he can reflect on who he was and who he wants to become. He can choose to keep or let go of his past coping/defense mechanisms like his facial hair and The Expression. He can choose to embrace or reject the self-defeating fantasy of fascism. The shack marks a midpoint of the game, when the hangover has worn off but before the case is closed. So "Live With Me" scores the balance between potential endings: abandonment or acceptance, relapse or recovery, death or life. Harry breathes in the sea air, breathes it back out, and takes another step.
I didn’t realize this until a recent replay, but “Live With Me” also plays when you visit the Working Class Woman to notify her of her husband’s death. Since this is an optional sidequest, I understand why they didn't create original music for it. But they didn't reuse "Rue de Saint-Gislaine", the song for the rest of the Capeside Apartments (including the Smoker on the Balcony's apartment when you talk to the Sunday Friend). The Working Class Husband is another mirror for Harry who has met his end, and "Live With Me" plays to mourn him.
Victor Méjean died from an accident while inebriated, a fate that also could have befallen Harry on a previous drinking binge. The striking thing about Victor's death is how easily he could have been overlooked and forgotten. He died at the end of a pier in a fenced off, abandoned part of town. His wife wasn't concerned about his days-long absence. It's only by virtue of Can Opening and Jamrock Shuffling that Harry will know about or find him. Victor literally and figuratively died slipping through the cracks – of the rotted boardwalk, yes, but also of any sort of social safety net. This is what happens to alcoholics in Revachol. This is what will happen to Harry if he continues drinking and hasn't built his own personal safety net with Kim or Cuno to prevent the RCM from abandoning him. As Harry informs Billie of her husband's death, it's only natural for him to think of his own possible endings, and the soundtrack reflects that.
The final version of the song you hear is “Burn, Baby, Burn” blasting from Sad FM on the boat ride to the Sea Fortress to find the Hanged Man's killer and Harry's last dark reflection: Dros, The Deserter. Dros shares Harry's penchant for clinging to political ideology to give meaning to his life and obsessing over women he can't be with. He lives in bitter isolation, refusing to move beyond the failures of the past, his personal shortcomings and the evils of the world alike. He's emblematic of yet another possible outcome for Harry: not literal death, but despair-induced stagnation that leaves one living like a ghost in the mortal realm.
By the time Harry gets in the boat to the island, his fate at the end of the game is set. The RCM (specifically Jean) has all they need to decide whether to accept or abandon their prodigal lieutenant-yefreitor. Should his former partners leave him, Harry can return to the shack and the circle of drunks who have also given up on life. Or he can return to the island, where he would take Dros' place as the creepy old man haunting the fortress, scaring children, and staring at the mainland with longing and resentment. But even if Harry returns with his unit to Jamrock, simply resuming his old life will not keep him from returning to the depths of despair. The RCM broke him; the RCM will not save him. Neither outcome helps Harry become a person he truly wants to live with.
"Want to be free/It will last forever/Eternally," croons the boombox on the boat. The lyrics echo the self destruction that Harry sought before the game's events: freedom forever from pain, the ultimate release of death. At least that's what the Ancient Reptilian Brain would see in those words. But there's tension in the lyrics as the desire for freedom and exhortations to "burn, baby, burn" repeat. The bridge offers an alternative vision of verdure not consumed by the disco inferno: "And the trees are green and overhanging/Feather-light, free, and everlasting." Perhaps a less moribund future exists for Harry, even if only in the next world, as a new person.
#disco elysium#disco elysium spoilers#disco elysium meta#disco elucidations#sea power#i know tommy le homme sings lyrics from “want to be free” but i wanted to focus on the soundtrack here#someone else can do that analysis lol#music is not my bailiwick so please correct me if i got any instruments or terms wrong#god this took me forever to write#and i have a whole nother different music and de post still in drafts too#whoopsie doo#my disco posting is never done
198 notes
·
View notes
Text
Another thing is when you call 41 to report your badge missing, there’s a bit of dialogue where you can ask “who’s that” when Jean goes off in the background
Jules goes what, you mean your partner
And then Jean asks wtf did he say
Jules tells him Harry’s asking who he is
“IM HIS GOD DAMN PARTNER” yes Jules already told Harry that
And then Jules tells Harry its satellite officer Jean Vicquemare
So basically Jean instead of identifying himself with his name title position like most officers do, first thing comes to his mind THIS IS WHAT I AM TO YOU, THIS
Later if Kim goes to hospital, Jean pops up in the ward and goes hi sir I wanna ask about the Lieutenant-Yefreitor, IM HIS PARTNER
So he knows to address harry by his proper title to people, but not his own title
Which again, for anyone else working at RCM, unusual behaviour
Also at that point he knows Kim already has that information, with high enough espirt the game tells you Kim literally figured out Jean’s from 41 the moment Harry talked to Jean. It really didn’t take a genius to figure out Jean is Harry’s partner by the tone he told Harry that they were partners in an AU at Whirling. but no the guy feels the need to reiterate that as a formal introduction. And then after all that he still isn’t gonna mention his own name and title
If the first time calling in is the game trying to give the player some quick basic facts about him, at this point close to game ending this is about the person that he is. It’s like he feels like that’s his most important identity, any time he introduces himself to anyone he goes “I’m Harry du bois’s partner, now you know all about me”
#I mean fair plays when you’d assume that any partner of Harry’s wouldn’t voluntarily admit to that#and there jean goes owning it#with no shame /jk#de#disco elysium#jean vicquemare#harry du bois#jules pidieu
163 notes
·
View notes
Text
You know something that I can't stop thinking about, regarding Disco Elysium? The morning of Day 3. Because it is wild, if you think about it.
You come downstairs, and very obviously within view of each other are Kim, the Man with Sunglasses (MwS) and the Horse-Faced Woman (HFW). All of them are very obviously RCM officers. MwS and HFW are in uniform, even! And they aren't talking to one another.
Is there some combination of stats that gives you more insight into this moment? Because I've never encountered any, and, again, it is wild that these 3 people are all in the same room and apparently haven't said a single thing to one another.
Wouldn't it make so much sense for Kim to approach them? It would be very easy for him to assume they're from the 41st. "Oh, thank god, your colleague is having a serious medical emergency, and this place is a tinderbox."
But, also, wouldn't it make sense for them to approach Kim? They know who he is, at least by reputation, and MwS at least doesn't seem like he could handle the idea of you embarrassing the 41st as much as he assumes you currently are. "Oh, Lt. Kitsuragi -- I hope that drunk asshole hasn't been causing you problems the last three days."
Did they do so? And then, for some reason, split up again? Or did they all just very awkwardly identify each other and then not say anything?
Did Kim, perhaps as a result of overhearing your radio call about your badge, decide it was best not to interact with them? He walks right past them! Did he somehow come to the conclusion that working alone with the amnesiac undergoing drug withdrawal was better than seeking support from these others? Or did they, perhaps out of embarrassment (?) or some sense of rank (?), think they shouldn't talk to him until you were there to make the introduction? How weird is that! MwS continues on with his whole hilarious "I'm wearing a wig" joke, even when he knows that a representative from another precinct is right there!
I just want answers. What were the twenty minutes before you woke up like? I just want to know!
12 notes
·
View notes
Note
You're married to your work and dating Harry, how cute
Exactly, yes. Then again, Harry often is my work, since we are partners at the RCM. So I’m dating Harry, but married to my work, which in a way means I am married to Harry.
It’s confusing, but it does make introductions much simpler. Whether in a professional or social setting, I always say, “This is my partner, Harry.”
4 notes
·
View notes
Text
Why Accurate Medical Coding Service Is Critical for Healthcare Revenue Cycle Success

Introduction
In today’s healthcare landscape, the need for operational efficiency and financial accuracy has never been more important. At the core of this system lies the medical coding service, an often overlooked yet critical component of the healthcare revenue cycle management (RCM) process. From translating complex clinical documentation into standardized codes to ensuring clean claim submissions, medical coding is the bridge that connects care delivery to financial reimbursement.
In this blog, we’ll explore what medical coding service involves, why it is vital to the RCM process, and how outsourcing or enhancing this function can significantly improve your organization’s bottom line.
What Is Medical Coding Service in Healthcare?
Medical coding involves converting patient diagnosis, treatments, procedures, and medical equipment into universal alphanumeric codes. These codes—such as ICD-10, CPT, and HCPCS—are used for billing and insurance claims.
A medical coding service ensures this process is handled accurately and efficiently, either by an in-house team or a third-party provider. Coders must interpret medical records and assign the correct codes, playing a crucial role in minimizing claim denials and ensuring timely reimbursement.
How Medical Coding Ties into Healthcare RCM
Revenue Cycle Management (RCM) is the financial process that healthcare facilities use to track patient care episodes from registration and appointment scheduling to the final payment of a balance. Within this complex cycle, coding is pivotal in these areas:
Claim Generation: Accurate coding ensures that claims sent to payers reflect the services provided.
Reimbursement Accuracy: Mistakes in coding can lead to underpayments or overpayments, both of which can hurt your cash flow.
Denial Management: Incorrect or incomplete codes are among the top reasons for claim rejections.
An effective medical coding service streamlines these steps, improving the efficiency of the entire RCM process.
Top Benefits of a Reliable Medical Coding Service
1. Improved Claim Accuracy
Accurate coding reduces the risk of claim denials and rework. A reliable coding service ensures that every code matches the clinical documentation and payer guidelines.
2. Faster Reimbursements
Timely and correct code submissions lead to quicker claim approvals and faster cash flow. This is especially important for practices and hospitals operating on tight budgets.
3. Regulatory Compliance
A professional medical coding service helps your facility stay compliant with healthcare regulations such as HIPAA, ICD-10 updates, and payer-specific rules, thereby reducing legal risks.
4. Reduced Administrative Burden
Outsourcing medical coding allows in-house staff to focus on patient care and strategic financial planning rather than coding audits and error corrections.
5. Scalability and Flexibility
As your practice grows, so does the complexity of coding. A dedicated medical coding service provides scalable support, enabling you to adapt quickly to increased workloads without compromising accuracy.
Common Challenges in Medical Coding and How to Overcome Them
Even the best coding professionals face obstacles. Here are common challenges and ways a robust coding service can address them:
Challenge
Solution Offered by Coding Services
Frequent Code Updates
Regular training and upskilling to stay current
Incomplete Clinical Documentation
Integrated CDI (Clinical Documentation Improvement) support
High Denial Rates
Automated denial analysis and coding audits
Staff Shortages
Access to certified and experienced remote coders
Payer-Specific Requirements
Custom coding workflows based on payer rules
Outsourcing Medical Coding: Is It Right for You?
Many healthcare providers now outsource their medical coding services to trusted vendors. Here’s why it makes sense:
Cost-effective: No need to hire, train, and manage a large internal team.
Expertise on Demand: Access to certified coders (CPC, CCS, etc.) across various specialties.
Advanced Technology: Outsourcing companies often leverage AI-assisted coding and automation for better accuracy and speed.
Performance Metrics: Outsourced services typically come with detailed reporting and KPI tracking to ensure transparency.
However, choosing the right partner is key. Look for a provider with healthcare RCM expertise, robust data security practices, and a proven track record in your specialty.
How to Measure the Impact of a Medical Coding Service
Tracking the effectiveness of your medical coding service involves monitoring several key performance indicators (KPIs), including:
First-pass claim acceptance rate
Coding accuracy rate
Claim denial rate
Average reimbursement time
Compliance audit score
Regular audits and performance reviews will help you identify areas for improvement and ensure you're getting maximum ROI from your coding investment.
Conclusion
A high-quality medical coding service isn’t just a back-office function—it’s a revenue enabler. By ensuring the accuracy, compliance, and timeliness of your coding processes, you can dramatically improve your healthcare revenue cycle management. Whether you’re running a small clinic or a large hospital network, investing in better medical coding practices is a strategic move that pays off in both efficiency and profitability.
If you're facing challenges in managing your coding workflow or denial rates are affecting your cash flow, it might be time to explore a professional medical coding solution tailored to your needs.
0 notes
Text
Leading Benefits of Online Medical Billing Software for Healthcare Providers in 2024
Top Benefits of Online Medical Billing Software for Healthcare Providers in 2024
In teh rapidly evolving healthcare industry of 2024, technology continues to reshape how providers deliver services, manage administrative tasks, and enhance patient care. Among these technological innovations, online medical billing software stands out as a game-changer. It streamlines billing processes, reduces errors, and boosts revenue cycle management, helping healthcare providers operate more efficiently and focus more on patient health. This comprehensive guide explores the top benefits of online medical billing software for healthcare providers in 2024.
Introduction
Medical billing is a complex, time-consuming process that involves coding, claims submission, payment processing, and follow-up. Traditionally performed manually or with outdated software, it often led to billing errors, delayed reimbursements, and increased administrative overhead. Thankfully, online medical billing software offers a modern, cloud-based solution designed to address these challenges. As we step into 2024, embracing this technology is not just beneficial but essential for healthcare practices seeking growth, compliance, and efficiency.
What is Online Medical Billing Software?
Online medical billing software is a cloud-based platform that automates and simplifies the billing and coding process for healthcare providers. it integrates seamlessly with electronic health records (EHR) systems, facilitates electronic claims submission, manages patient data, and provides real-time analytics. Unlike traditional desktop software, online billing solutions offer accessibility from any device with an internet connection, ensuring flexible and efficient management of billing operations.
Top Benefits of Online Medical Billing Software in 2024
1. enhanced Billing Accuracy and Reduced Errors
Manual data entry and complex coding processes are prone to errors which can delay payments or cause claim denials. Online medical billing software automates coding, validation, and claim submission processes, drastically reducing human error. Accurate billing ensures faster reimbursements and improves cash flow.
2. Accelerated Claims Processing and Faster Payments
With integrated electronic claim submission and automatic validation checks, online billing software speeds up the entire billing cycle.real-time claim tracking and instant rejection alerts enable speedy corrections, minimizing delays and increasing the likelihood of timely reimbursements.
3. Improved Revenue Cycle Management (RCM)
Effective revenue cycle management is vital for practice sustainability.Online billing solutions provide comprehensive dashboards and analytics that help monitor claims, denials, and collections. Some platforms even suggest revenue optimization strategies based on payment patterns, enabling healthcare providers to maximize profitability.
4. Increased Compliance with Regulations
Staying compliant with evolving healthcare regulations like HIPAA, CMS guidelines, and ICD-10 coding standards is crucial. Online medical billing software is regularly updated to adhere to current regulations,reducing the risk of penalties and audits.
5. Enhanced Data Security and Privacy
security is paramount in healthcare. Cloud-based billing solutions employ robust encryption, user access controls, and audit trails to safeguard sensitive patient data. This ensures compliance with data protection laws and peace of mind for providers and patients alike.
6. Seamless integration with EHR and Practice Management Systems
Integration with Electronic Health Records (EHR) and other practice management tools allows for automatic data synchronization, eliminating redundancy and minimizing discrepancies. This interoperability streamlines workflows and enhances overall operational efficiency.
7. Cost Savings and Operational Efficiency
Transitioning to online billing software reduces reliance on paper, minimizes billing staff workload, and decreases administrative overhead. These cost savings enable healthcare providers to allocate resources elsewhere, such as patient care or practice expansion.
8. Accessibility and Flexibility
Being cloud-based, online medical billing software offers access from multiple devices and locations.This flexibility supports remote work and allows billing staff to operate efficiently outside the traditional office setting, especially important amidst remote work trends in 2024.
Practical tips for Choosing the Right Online Medical Billing Software
Evaluate integration capabilities with your existing EHR and practice management systems.
Prioritize data security features to ensure compliance and protect sensitive data.
Consider automation features such as automatic claim rejection alerts or payment posting.
Check for real-time reporting and analytics tools to monitor financial performance.
Assess customer support and training options to maximize software benefits.
Case Study: Success Story of a Mid-Sized Healthcare Practice in 2024
Practice Type
Challenge
Solution Implemented
Results Achieved
Multi-specialty clinic
High claim rejection rates and slow payment turnaround
Adopted cloud-based medical billing software with automated claim verification
Reduced rejection rate by 35%, sped up payment cycle by 20 days
First-Hand Experience: Why We Switched to Online Medical Billing Software
As a healthcare provider, we found manual billing processes time-consuming and error-prone. After switching to a reputable online medical billing platform in 2024, our practice experienced a meaningful boost in revenue, compliance, and staff productivity. With real-time dashboards and automated claim handling, we could focus more on patient care while the billing remained accurate and clear. This firsthand experience highlights how online solutions are essential for modern practices aiming for growth and efficiency.
Conclusion
In 2024, online medical billing software is transforming healthcare practices by making billing processes more efficient, accurate, and secure. From speeding up claims and payments to ensuring regulatory compliance and reducing operational costs,the top benefits of this technology are undeniable. Healthcare providers who embrace these digital solutions gain a competitive edge, improve cash flow, and enhance patient satisfaction. As the industry continues to evolve, investing in reliable online medical billing software is a strategic move towards a more streamlined and profitable practice.
Whether you’re a small practice or a large hospital system, leveraging the power of cloud-based billing solutions can unlock new levels of operational excellence. stay ahead of the curve in 2024 by choosing the right software tailored to your needs-your practice’s financial health depends on it.
https://medicalcodingandbillingclasses.net/leading-benefits-of-online-medical-billing-software-for-healthcare-providers-in-2024/
0 notes
Text
Top Medical Billing Practices to Boost Revenue & Ensure Compliance in Healthcare
Top Medical Billing Practices to Boost Revenue & Ensure Compliance in Healthcare
Introduction
in the ever-evolving landscape of healthcare, a robust medical billing process is vital for ensuring financial stability, maximizing revenue, and maintaining regulatory compliance. Proper medical billing practices not only streamline cash flow but also help avoid costly audits and penalties. Whether you’re a healthcare provider, billing specialist, or practise manager, understanding the top strategies for effective medical billing is essential. This comprehensive guide explores proven practices, practical tips, benefits, real-world case studies, and expert insights to help you optimize your billing workflow and achieve enduring growth.
why Effective Medical Billing Practices Matter
Efficient medical billing is the backbone of a profitable healthcare practice. It directly impacts revenue cycle management,patient satisfaction,and compliance with federal and state regulations. Poor billing practices can result in delayed payments, denied claims, revenue loss, and legal complications. Thus, adopting best practices is crucial for fiscal health and operational excellence.
Key Medical billing Practices to Boost Revenue & Ensure Compliance
1. Accurate Data Entry & Documentation
One of the most foundational aspects of successful medical billing is ensuring accuracy in patient data and documentation. Mistakes in demographic info, insurance details, or clinical documentation can lead to claim rejections.
Double-check patient information during registration
Ensure thorough and precise clinical documentation
use integrated electronic health records (EHR) systems for automatic data syncing
2. Staying Updated with Coding & Regulations
Medical coding standards-such as ICD-10, CPT, and HCPCS-stand at the core of insurance reimbursements. Outdated or incorrect codes can cause claim denials or audits.
Regularly train billing staff on coding updates
Utilize coding software with built-in guidelines
stay informed about healthcare billing regulations like HIPAA and Medicare policies
3. Robust Claim Submission & Follow-up Process
Automating claim submission and implementing diligent follow-up procedures enhance the chances of timely reimbursement. Use electronic claim submission (EDI) systems to reduce errors and accelerate processing.
Step
Action
Benefits
1
Automatic claim submission via EHR
Faster processing
2
Regular claim status review
Early detection of issues
3
Prompt appeal of denied claims
Increased revenue recovery
4. Effective Denial Management
Handling claim denials proactively can save considerable revenue and prevent cash flow disruptions.Establish a denial management team or process for rapid resolution.
Analyze denial reasons systematically
Correct errors promptly and resubmit claims
Implement denial tracking tools for continuous enhancement
5. Regular Staff Training & Education
Healthcare billing regulations and coding standards evolve frequently. Continuous education ensures your team remains compliant and efficient.
Schedule quarterly training sessions
Leverage online courses and certifications
Promote a culture of compliance and accuracy
6. Integrate Revenue cycle Management (RCM) Technology
Investing in comprehensive RCM software can automate many billing tasks, from patient registration to collections. This integration leads to reduced errors and faster reimbursements.
Popular tools include:
Automated claim scrubbing
Real-time eligibility verification
Advanced analytics dashboards
Benefits of Implementing Top Medical Billing Practices
Benefit
Description
Increased Revenue
Faster and accurate reimbursements boost your practice’s cash flow.
Improved Compliance
Minimize legal risks by adhering to regulations and standards.
Reduced Claim Denials
Efficient processes lead to fewer rejected claims, saving time and resources.
Enhanced Patient Satisfaction
Clear billing processes and obvious interaction improve patient trust.
Operational Efficiency
Automation and staff training streamline workflows for better productivity.
Practical Tips for Optimizing Your Medical Billing Process
Use Technology: Invest in reliable billing and practice management software that integrates with EHR systems.
Monitor KPIs: Track metrics such as days in accounts receivable, claim rejection rate, and denial reasons for continuous improvement.
Establish Clear policies: Develop standardized procedures for billing,denials,and collections to ensure consistency.
Maintain Open Communication: Foster collaboration between clinical, administrative, and billing teams for seamless workflows.
Perform Regular Audits: Conduct periodic audits to identify vulnerabilities and rectify inconsistencies early.
Case Study: Transforming Billing Efficiency at HealthyCare Clinic
Background: HealthyCare Clinic faced recurring claim rejections and delayed reimbursements, impacting their revenue cycle. They decided to overhaul their billing practices.
Approach: By implementing automated billing software, retraining staff, and establishing a denial management team, HealthyCare substantially enhanced their billing operations.
Aspect
Before
After
Claim Rejection Rate
15%
4%
Average Days in Accounts Receivable
45 days
25 days
Revenue Growth
Flat
15% increase annually
Result: Streamlined billing led to faster collections, fewer rejected claims, and increased revenue-highlighting the power of adopting top medical billing practices.
First-Hand Experience: My Recommendations
Having worked with various healthcare providers, I recommend prioritizing technological integration and staff training. Align billing practices with evolving regulations to stay compliant and optimize revenue. Consistent review and improvement ensure your practice remains resilient against common billing pitfalls.
Conclusion
Implementing top medical billing practices is key to boosting revenue,ensuring compliance,and fostering a smooth healthcare operation. From accurate documentation and staying current with coding standards to leveraging automation and continuous staff education, these strategies can transform your billing process into a powerful tool for growth.Remember, proactive denial management and regular audits are essential for maintaining financial health. By adopting these proven practices, healthcare providers can achieve operational excellence, enhance patient satisfaction, and secure long-term success.
Ready to revolutionize your medical billing? Contact us today for expert guidance and tailored solutions to maximize your healthcare practice’s revenue and compliance!
https://medicalbillingcodingcourses.net/top-medical-billing-practices-to-boost-revenue-ensure-compliance-in-healthcare/
0 notes
Text
How an Automated EMR Patient Eligibility Verification System Transforms Physician Revenue Cycles

Introduction
In today’s complex healthcare environment, ensuring accurate and timely patient eligibility verification is critical to maintaining a healthy revenue cycle. For physicians and medical practices, denied claims due to eligibility issues can cause significant financial losses, administrative burden, and frustration. This is where an Automated EMR Patient Eligibility Verification System becomes a game-changer.
This blog explores how integrating automated eligibility verification within your Electronic Medical Record (EMR) system can significantly enhance operational efficiency, reduce claim denials, and ultimately benefit physicians in the healthcare RCM landscape.
The Need for Accurate Eligibility Verification
Patient eligibility verification is the first and arguably most important step in the revenue cycle. It involves confirming a patient’s insurance coverage, policy status, co-pay, deductible, and service authorization before care is delivered. A single error or oversight can lead to:
Claim denials or rejections
Delayed reimbursements
Increased A/R days
Loss of patient trust
Physicians are often burdened with administrative tasks that take time away from patient care. Manual eligibility checks using payer portals or phone calls can be inefficient, error-prone, and inconsistent.
What is an Automated EMR Patient Eligibility Verification System?
An Automated EMR Patient Eligibility Verification System is an integrated software solution that checks insurance eligibility in real-time or batch mode directly within the EMR. It eliminates the need for manual data entry and reduces the risk of human error.
These systems automatically verify:
Active insurance coverage
Plan-specific benefits
Deductibles and co-pays
Referral or authorization requirements
Coverage for specific services or procedures
Automation ensures that practices have the correct insurance details before the patient arrives, leading to faster billing cycles and fewer surprises.
Key Benefits for Physicians
Let’s explore the various ways in which physicians benefit directly from using an automated eligibility verification system:
1. Reduces Claim Denials and Rework
Denied claims often stem from eligibility issues. With an automated system, physicians can significantly reduce denials by verifying patient insurance information ahead of time. This proactive approach ensures:
Fewer billing errors
Decreased rework for the billing team
Faster reimbursements from payers
By avoiding denials, physicians can maintain consistent cash flow and reduce delays in payments.
2. Improves Front-Office Efficiency
Automation lightens the administrative load on front-desk staff, allowing them to focus more on patient engagement and less on navigating payer websites. Eligibility checks that once took several minutes per patient are now completed in seconds.
This efficiency is especially important during busy clinic hours or in high-volume practices.
3. Enhances Patient Experience
Patients appreciate transparency. When their benefits, out-of-pocket costs, and co-pays are accurately known before the visit, it reduces confusion and builds trust.
Physicians benefit from better-informed patients who are more likely to pay at the time of service, which contributes to:
Higher point-of-service collections
Fewer patient disputes
Improved satisfaction scores
4. Supports Accurate Pre-Authorization
Certain procedures and treatments require prior authorization. An automated system flags these requirements early, helping providers avoid performing non-covered services.
By staying compliant with payer rules, physicians minimize the risk of non-payment and protect their practice from audits or penalties.
5. Streamlines Scheduling and Workflows
With integrated eligibility verification, scheduling systems can check patient coverage at the time of booking. This ensures that only eligible appointments are confirmed, reducing no-shows and last-minute cancellations.
For physicians, this leads to:
Better use of clinical time
More predictable revenue streams
Improved staff coordination
6. Real-Time and Batch Verification
Physicians benefit from the flexibility to verify patient eligibility either in real time (for walk-ins or urgent cases) or in batches (for scheduled appointments). This dual mode ensures full coverage without adding complexity.
Batch verification the night before appointments allows staff to resolve issues before the patient arrives.
How it Works: A Quick Workflow Example
Patient schedules an appointment
EMR system triggers automatic eligibility check
System retrieves payer data and updates EMR
Staff reviews any issues (inactive coverage, referrals needed)
Patient notified if action is required
Physician proceeds with visit knowing eligibility is verified
This seamless workflow eliminates last-minute surprises and strengthens the entire revenue cycle.
Integrating with Your Current EMR System
Most modern EMRs now offer eligibility verification as a native or add-on feature. Integration is straightforward and often supported by:
HL7 or FHIR-based APIs
Clearinghouses or third-party RCM platforms
Direct payer connections
Choosing a solution that supports real-time eligibility checks with major insurance providers ensures broader coverage and fewer gaps.
Real-World Impact: A Case Study
Dr. Patel, an independent cardiologist in Texas, implemented an Automated EMR Patient Eligibility Verification System and saw the following results within 90 days:
27% reduction in claim denials
40% less time spent on insurance calls
Improved patient collections by 18%
Increased overall staff satisfaction
The automation allowed his team to shift focus from troubleshooting to patient engagement, ultimately driving practice growth.
Final Thoughts
Physicians today are under immense pressure to balance patient care with practice profitability. By adopting an Automated EMR Patient Eligibility Verification System, they can streamline one of the most critical steps in the revenue cycle.
Whether you run a solo practice or a multi-provider clinic, eligibility automation enhances accuracy, reduces denials, and frees up valuable time for what matters most—caring for patients.
0 notes
Text
Top 17 Revenue Cycle Management Trends Shaping the Future of Healthcare

The Revenue Cycle Management field experiences substantial transformation due to technological developments along with changing patient demands and regulatory modifications.
Healthcare organizations must understand the new patterns emerging in RCM to better manage efficiency improvements and cost reductions while delivering superior patient outcomes.
The RCM field will experience multiple transformative developments in the next five years which will present new challenges and opportunities to providers.
1. Integration of Artificial Intelligence and Automation
The future of RCM processes and rcm services for medical or any sector will be transformed through the implementation of Artificial Intelligence and automation. Healthcare providers can eliminate administrative burdens and reduce errors by automating routine tasks like patient registration and claims processing. Artificial intelligence tools examine massive datasets to detect patterns while predicting denials and improving revenue cycle operations. Implementing AI leads to improved operational efficiency while enabling employees to dedicate their time to high-value complex tasks.
2. Emphasis on Patient-Centric Billing
Billing practices are now evolving to support patient-centered care models. Modern patients require billing processes that provide clear transparency as well as convenient and flexible financial transactions. Healthcare organizations respond to patient demands for financial transparency and convenience by offering billing platforms which provide clear charge explanations and real-time account access together with multiple payment options. Improving patient financial interactions leads to better patient satisfaction while also speeding up payment processing and decreasing bad debt amounts.
3. Expansion of Telehealth Services
Telehealth's swift integration has led to increased complexities in Revenue Cycle Management. Accurate coding and knowledge of payer policies along with adherence to changing regulations are essential for billing virtual visits. Healthcare providers need to update their RCM systems to support telehealth services while maintaining smooth operations with current workflows. With the expansion of telehealth services financial stability relies on efficient handling of revenue cycle components.
4. Transition to Value-Based Care Models
The healthcare sector is shifting away from fee-for-service reimbursement towards value-based care frameworks that emphasize patient results and efficiency. The shift to value-based care requires RCM strategies to adapt through the introduction of new metrics alongside risk adjustment approaches and performance-based payments. To track quality measures and demonstrate value to payers healthcare organizations need to invest in data analytics and reporting tools.
5. Adoption of Blockchain Technology
Blockchain technology shows great potential for improving transparency as well as security and operational efficiency in RCM systems. Blockchain enables claims adjudication and payment reconciliation processes and patient consent management through its decentralized and immutable ledger system. The use of blockchain technology helps eliminate fraudulent activities and duplicate processes while establishing trust among all involved parties. As blockchain technology advances its implementation in RCM systems will grow more common.
6. Focus on Data Analytics and Predictive Modeling
Through the application of data analytics and predictive modeling healthcare providers can actively oversee their revenue cycles. Through historical data analysis organizations become capable of recognizing trends and predicting cash flows while identifying emerging problems early on. Predictive analytics help organizations optimize resource allocation while also strengthening patient engagement strategies and boosting financial performance. Robust analytics capabilities have become essential tools for making informed decisions.
7. Outsourcing of RCM Functions
Specialized vendors take on RCM functions for healthcare organizations because these organizations face staffing shortages and need to minimize operational costs. Through outsourcing healthcare organizations gain access to specialized knowledge along with advanced technological resources and scalable solutions. Healthcare organizations can prioritize core clinical functions by partnering with outside RCM providers which helps maintain efficient revenue cycle operations. Providers will keep pursuing this approach to improve their operational agility and resilience.
8. Strengthening Cybersecurity Measures
The digitization surge in healthcare data has made cybersecurity a top priority within RCM systems. To defend sensitive patient information against breaches and cyberattacks effective security protocols must be combined with routine risk assessments and proper staff training. Data integrity protection and HIPAA compliance necessitate the deployment of advanced encryption, multi-factor authentication and intrusion detection systems.
9. Implementation of Interoperable Systems
Effective RCM processes depend on interoperability between different healthcare systems to enable seamless data exchange. By connecting electronic health records (EHRs) with billing systems and payer platforms healthcare providers can instantly share information which eliminates duplicate efforts and boosts care coordination. Using standardized data formats alongside interoperable technologies leads to better revenue cycle outcomes through smoother workflow processes.
10. Embracing Remote Work Models
Healthcare adopted remote work practices more quickly because of the COVID-19 pandemic which included remote revenue cycle management operations. Organizations have implemented permanent remote work policies through cloud-based systems while maintaining secure data access. The remote work arrangement provides employees with flexible schedules while broadening access to diverse talent pools and offering potential savings on operational costs. To maintain productivity and compliance in remote work environments organizations must invest in strong communication tools alongside performance monitoring and cybersecurity initiatives.
11. Enhancing Prior Authorization Processes
The need for prior authorization presents a major obstacle within RCM processes because it causes administrative delays and increased workload. Healthcare providers implement electronic prior authorization systems to automate request submissions while integrating these systems with EHRs and offering real-time decision-making support. Streamlining prior authorization workflows increases operational efficiency and speeds up patient treatment access while minimizing denial rates.
12. Leveraging Robotic Process Automation (RPA)
The healthcare industry sees increasing adoption of Robotic Process Automation (RPA) within Revenue Cycle Management (RCM) for streamlining routine tasks that follow specific rules. RPA bots demonstrate exceptional precision and rapid processing capabilities in executing tasks like data entry and payment postings as well as claims submissions. RPA enables staff members to concentrate on strategic tasks while reducing error rates and boosting revenue cycle effectiveness by diminishing manual workload demands.
13. Addressing Social Determinants of Health (SDOH)
Healthcare organizations are now integrating social determinants of health data into their revenue cycle management strategies because these factors affect both patient outcomes and financial performance. When healthcare providers detect patient barriers like transportation challenges and housing instability they can link patients with needed resources while decreasing missed appointments and ensuring better treatment adherence. The implementation of SDOH elements within RCM frameworks delivers comprehensive patient care while strengthening revenue security.
14. Preparing for Regulatory Changes
Healthcare regulatory changes happen all the time which impacts RCM practices through new policies. Healthcare professionals need to keep updated on billing code modifications alongside new reimbursement methods and compliance obligations. To manage regulatory changes efficiently healthcare organizations need to provide continuous staff training and system updates along with proactive payer communication.
15. Promoting Financial Literacy Among Patients
Patient education about healthcare costs, insurance coverage and payment options enables them to make knowledgeable choices while actively participating in managing their financial obligations. Organizations that deliver transparent cost estimates and financial counseling together with clear explanations establish trust and achieve better collection outcomes. Patient-centered RCM strategies depend on promoting financial literacy among patients.
16. Utilizing Cloud-Based RCM Solutions
RCM platforms running on the cloud deliver scalable solutions that provide flexible access to data in real-time. These solutions enhance remote work capabilities while promoting interoperability between systems and allowing quick update deployments. Healthcare organizations achieve better operational efficiency and lower IT infrastructure costs while strengthening their disaster recovery capabilities through adoption of cloud-based systems.
17. Emphasizing Revenue Integrity Programs
Revenue integrity programs work to maintain precise documentation practices along with proper coding and billing techniques. These programs align clinical and financial processes which helps to protect revenue streams while minimizing compliance risks and improving reimbursement rates. Organizations must establish strong revenue integrity initiatives to maintain financial stability and meet regulatory standards.
Conclusion
Over the coming five years Revenue Cycle Management will experience fundamental changes because of technological advancements alongside shifts in patient expectations and the introduction of new regulations. To deliver value-based care while ensuring compliance and improving efficiency healthcare organizations need to proactively adjust to new trends.
0 notes
Text
Compliance and Regulations Impacting Revenue Cycle Management Structure

Introduction
In today’s healthcare landscape, Revenue Cycle Management (RCM) is more than just a back-end function. It plays a central role in maintaining the financial stability of healthcare organizations. However, as the industry continues to evolve, so do the regulatory and compliance requirements that govern it. Navigating this complex environment demands not only robust systems but also an adaptable and compliant RCM structure.
The Importance of Compliance in Revenue Cycle Management
Healthcare regulations are designed to ensure transparency, protect patient data, and prevent fraud and abuse. RCM involves all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue. Compliance with federal and state regulations is critical to maintain credibility, avoid penalties, and ensure seamless reimbursement processes.
For healthcare providers, a compliant RCM structure ensures that billing practices are ethical, accurate, and in line with current legislation. This is particularly important given the increased scrutiny from regulatory bodies such as the Centers for Medicare & Medicaid Services (CMS), the Office of Inspector General (OIG), and the Health Insurance Portability and Accountability Act (HIPAA).
One of the foundational elements of a compliant revenue cycle is conducting a Practice Assessment. This involves evaluating the entire revenue cycle process to identify gaps, inefficiencies, and risks. A comprehensive assessment ensures that the organization adheres to best practices and complies with evolving regulations.
Key Regulatory Influences on RCM
HIPAA and Data Security
The Health Insurance Portability and Accountability Act (HIPAA) sets national standards for protecting sensitive patient data. Any healthcare entity involved in billing, coding, or recordkeeping must ensure that all information is stored and transmitted securely. Non-compliance can lead to heavy fines and reputational damage. RCM structures must incorporate encryption protocols, access controls, and employee training to comply with HIPAA requirements.
The Affordable Care Act (ACA)
The ACA has significantly impacted healthcare billing and reimbursement structures. It introduced new models of care, such as value-based payment systems, which reward healthcare providers for quality over quantity. As a result, RCM systems had to evolve to handle performance metrics, patient outcomes, and preventive care billing. This shift has forced healthcare providers to adapt their revenue cycle operations accordingly.
CMS Rules and Reimbursement Guidelines
The Centers for Medicare & Medicaid Services constantly update rules regarding billing codes, reimbursement rates, and documentation requirements. A minor error in coding or billing can result in claim denials or delayed payments. Hence, continuous education and system updates are necessary to maintain compliance with CMS regulations. This has led to a more dynamic RCM structure that must stay aligned with policy changes.
Structuring the RCM for Compliance
Integrated Technology Solutions
To stay compliant, many healthcare organizations are turning to integrated software solutions that offer real-time updates on regulatory changes. These platforms can automate eligibility checks, ensure correct coding, and flag potential compliance issues before claims are submitted. They also generate audit trails that support transparency and accountability.
Staff Training and Development
An effective RCM structure depends on the competency of the staff handling it. Frequent training sessions on regulatory updates, fraud prevention, and data security are essential. Teams must understand the implications of compliance violations and be equipped to adapt to changes swiftly.
Internal Auditing and Monitoring
Ongoing auditing processes are crucial for maintaining compliance. Internal audits help identify discrepancies, patterns of errors, or potential compliance breaches before they become liabilities. Regular monitoring ensures that policies are being followed and corrective actions are taken when necessary.
Penalties and Risks of Non-Compliance
The risks associated with non-compliance are both financial and operational. Penalties for violating HIPAA rules, for instance, can range from thousands to millions of dollars depending on the severity. Incorrect billing can trigger investigations, lead to reimbursement clawbacks, or even cause legal action. Beyond the financial implications, non-compliance can harm a provider’s reputation and patient trust.
Building a Culture of Compliance
Compliance is not a one-time effort but a continuous process. Healthcare organizations need to foster a culture where compliance is prioritized at every level—from front-desk staff to billing teams and administrators. This involves transparent communication, clearly defined roles, and accountability systems.
Leadership must emphasize the importance of staying informed about regulatory changes and encourage cross-functional collaboration to address compliance issues holistically.
Conclusion
Compliance and regulations are inextricably linked to the structure and efficiency of Revenue Cycle Management. As healthcare regulations grow more complex, it becomes increasingly important for healthcare organizations to structure their RCM systems around compliance, security, and adaptability. By investing in technology, training, and regular Practice Assessment, organizations can not only mitigate risk but also enhance operational efficiency and financial performance.
In a rapidly changing regulatory environment, staying ahead of compliance requirements is not just about avoiding penalties—it’s a strategic imperative that supports long-term sustainability and quality patient care.
0 notes
Text
UAE Precious Metals VAT Changes - Shuraa Tax

The United Arab Emirates (UAE) is renowned for its vibrant trade in precious metals and stones, with Dubai often called the “City of Gold.” In 2018, the UAE introduced a 5% Value Added Tax (VAT) on most goods and services, including precious metals and stones. To support and enhance this vital sector, the government has recently announced UAE Precious Metals VAT Changes. A notable change is the introduction of the Reverse Charge Mechanism (RCM) through Cabinet Decision No. (127) of 2024, which shifts the responsibility of reporting VAT from the seller to the buyer in certain transactions. This update aims to simplify tax procedures and improve cash flow for businesses. For businesses and investors in this sector, understanding these changes is crucial to ensure compliance and optimize financial operations. At Shuraa Tax, we make VAT easy for you. Whether you need help with VAT registration, filing, or understanding the new rules, our experts are here to guide you. Get in touch with us today for hassle-free VAT solutions and keep your business running smoothly.
#UAE Precious Metals VAT#UAE VAT Changes on Precious Metals#Dubai Precious Metals VAT Changes#VAT in the UAE
0 notes
Text
Spring, ‘32, Grand Couron, Revachol
Harry du bois, gym teacher and substitute coach for regional high school games: Calling off a match between two schools when a pox-scarred kid was pushed to the ground and trampled by both teams in the middle of the game.
Later in the week he got a phone call from the kid, clearly forced by his parents to call and grumpily thanked Harry for saving him from breaking all 4 limbs. Dora jokingly commented that Harry upheld justice- he’d make a good RCM officer.
Spring ‘48, Jamrock, Revachol
Harry du bois, RCM officer, customarily drunk, pausing at his new partner’s self introduction: “I uh- recognise your voice from somewhere.”
His new partner, dryly: “You don’t say?”
Harry du bois, trying to stifle a hiccup and see straight at the same time: “There was this- From- *hiccup* Uh. *tapping forehead* No, it’s gone. Bad memory- 2 bottles of whisky.”
His new partner, nodding stiffly. “Probably a coincidence. People sound alike.”
Harry du bois, bleary-eyed: “huh. What-“
His new partner, whose name Harry already forgot: “The voice thing. It’s just a coincidence. You are drunk. You should run along.”
#Harry joined the RCM at age 26. a year ago he’s 25 being a highschool gym teacher. when jean was 15. a highschooler#what if they already met before#what if that meeting changed the trajectories of both of their lives#more or less quarter baked thoughts. I’ll need to come back to it when I get a few seconds free time#I didn’t say it was rugby but I also didn’t say it wasn’t rugby#my sports knowledge is limited to ‘have you seen that ludicrous display last night’#if you get that reference… I gently clasp you by the shoulder with tears in my eyes#de headcanon#harry du bois#jean vicquemare#de#disco elysium
19 notes
·
View notes
Text
Key Steps to Optimize Revenue Cycle Management in Healthcare

Key Steps to Optimize Revenue Cycle Management in Healthcare
Introduction
Financial stability, like the quality of patient care, is essential for the operation of a health care facility, yet it is often undermined by revenue cycle inefficiency, claim denial, and delay in reimbursement. Revenue Cycle Management (RCM) refers to efficient and effective collection efforts from providers to bring cash into the organization in compliance with regulations. On the other hand, RCM is more than cash flow; it covers an end-to-end technology-enabled process in every step-from patient registration to collection of payments at the endpoint. In this guide, we will discuss the steps that need to be undertaken to refine RCM processes for an improved bottom line to healthcare providers.
Learning About Revenue Cycle Management
What is RCM?
Revenue Cycle Management (RCM) consists of the financial processes used by organizations within healthcare to manage billing, claims processing, and payment collection. This process begins with the scheduling of a patient and thus continues until the final payment is made. An optimized revenue cycle management might reap smaller revenue leakage and faster reimbursement.
The Purposes of RCM
Building an effective RCM strategy for providers must involve the following concepts:
Patient progression in the registration and insurance verification: entry error avoidance for billing errors.
Medical coding and billing: Proper CPT, ICD-10, and HCPCS coding ensures acceptance from Payers.
Claim submission and processing- Timely submission to claim less denial.
Payment collections- Patient financial responsibility education increases collections.
The new compliance and audits: Keeping abreast of rules and regulations limits financial risks.
Financial Reporting and Analytics: Data-driven decisions lead to revenue efficiency.
Key Steps to Optimize RCM
1. Ensure Accurate Patient Registration and Insurance Verification
Mistakes in patient registration are among the most critical reasons for claim denials. Capturing proper demographic and insurance information from the first instance will prevent billing issues. Automated insurance verification tools help reduce manual errors and improve claims acceptance rates.
2. Advanced Medical Billing and Coding
Medical coding inaccuracies lead to rejection of his claims and delays in payment. Healthcare providers should:
Regularly train coders on the latest CPT and ICD-10 updates.
Periodically conduct coding audits to identify and correct errors.
Use coding software for improved efficiency and accuracy.
3. Claims Submission and Follow Up: Simplified
Claim submission is the most vital thing to keep the cash flow at a steady stream. Denied claims must be followed up with a very strong follow-up process which ensures revenue recovery lost to the provider. Aside from such imperatives:
Claims are submitted within the timeline set by the insurer.
Status of claims tracked by RCM software.
Resolving denied claims within the shortest possible time to improve reimbursement rates.
4. Implement Efficient Payment Collection Methods
Most providers find it difficult to collect payments from patients. Improve the collection of patient payments by giving different methods of paying and educating patients about their financial responsibility. Here are some best practices:
Easy to understand the billing statement.
Multiple payment channels: Online portals, mobile applications.
Train staff to communicate financial policies.
5. Use Technology for Automation
Transformation, be it in the form of optimizing RCM through technology, is another reason to automate billing and claims processing. Healthcare providers can now:
minimize manual error and administrator burden.
conduct revenue cycle tracking in real time using RCM software.
detect revenue leakage with AI-enhanced analytics.
6. Compliance with Healthcare Regulations
An important aspect of RCM that every healthcare provider must adhere to is compliance. Updated regular changes prevent penalties and claim denials. Providers, for instance, should:
Be informed of ICD-10, HIPAA, and payer specific requirements.
Conduct routine internal audits.
Ensure compliance training programs for staff.
7. Better Patient Engagement and Communication
Healthcare providers should keep clear lines of transparent patient billing and proactive patient communications because they drive collections:
provide pricing transparency so fees do not come as a surprise.
Real-time access to bills and payment options made available through patient portals. Automate reminders for payments due.
8. Training and Development for Staff
An efficient revenue cycle requires a well-trained workforce. In-house training periodically will ensure that the billing team stays abreast with the latest:
Medical coding and documentation guidelines.
Claim management best practices.
Regulatory changes affecting reimbursement.
RCM Optimization-Evaluating Success
The measurement of the RCM effectiveness is well-kent by application of key performance indicators. Some of the most valuable KPI include the following:
Decrease in claim denial rates – This means that there are few problematic claims.
Accounts Receivable Cycle – Shorter AR- A sign that payments are received quickly.
Clean claim rate = A high rate shows an efficient submission technique.
Patient payment collection rate – More collections means stronger, survivable finances.
Ongoing Improvement Techniques
RCM optimization is not a single-time activity. It should include:
Assessment of performance on a regular basis.
Automate where applicable.
Be innovative to meet payer policies and government regulations as they come.
Optimum RCM with Expert ICS
RCM efficiency requires garnered experience, relevant technology, and strategic perspective. Info Hub Consultancy Services (ICS) brings an array of specialized revenue cycle solutions applicable to the unique needs of different healthcare organizations. From certified billing and coding professionals, ICS clients are assured of processing and compliance ways across various medical specialties.
What We Offer to ICS Partnership
World-Class Expertise – More than 40 specialties are delivered with perfection billing services by ICS.
Integration of Advanced Softwares – Integrative with proficiency in more than one billing platform at at great ease.
Maximized Revenue – Proven strategies to enhance reimbursement rates and reduce claim denials.
Cost-effective RCM– FTE model minimizes operational costs at just $7.5 per hour.
Reliable Support– Proactive customer support to ensure reliable workflow management.
Conclusion
When it comes to ensuring the financial sustainability of a healthcare organization, revenue cycle optimization is extremely important. Automated processes, accurate coding, claim tracking, and compliance can help reduce denials and enhance collections. Partnering with experienced outsourced medical coding and billing service providers like ICS will create further efficiencies, ensuring seamless operations and long-term financial viability. Partner with Info Hub Consultancy Services today to optimize RCM and maximize profits.
#Revenue_cycle_management#Outsource Medical Billing#Medical Billing Company#Best Outsource Medical Billing and coding Company
0 notes
Text
What is GST Course? A Detailed Introduction for Freshers
What is a GST Course?

A GST course is a professional training course aimed at teaching people about the complexities of GST laws, regulations, and procedures. The courses are offline and online and can be undertaken by students, working professionals, and entrepreneurs. The course material includes the basics of GST, tax computation, registration, filing of returns, input tax credit, and compliances.
Who Should Take a GST Course?
A GST course is useful for:
Accounting and finance professionals
Entrepreneurs and business owners
Tax lawyers and advisors
Commerce and finance students
All those who are interested in taxation and finance
Important Points Discussed in a GST Course
A good GST course covers the following points:
Introduction to GST: Goods and Services Tax basics, history, and goals.
GST Registration: Business process and eligibility.
Tax Structure and Rate: CGST, SGST, IGST, and more than one tax slabs.
GST Returns and Filing: GSTR-1, GSTR-3B, annual return, and filing process.
Input Tax Credit (ITC): What, who is eligible, and the limitations.
GST Invoicing and Documenting: Format, compliance, and e-invoicing.
Reverse Charge Mechanism (RCM): When to use and how.
GST Compliance and Auditing: Rules, penalties, and audits.
GST on E-commerce and Exports: Special rules and exemptions.
Recent Amendments and Updates: Keeping up with new developments in GST laws.

Advantages of Enrolling for a GST Course
Increased Knowledge: Achieve full knowledge regarding GST and its effects on businesses.
Career Opportunity: Offer career opportunities in taxation, accounting, and compliance positions.
Increased Business Compliance: Facilitates business owners to file GST and escape penalties.
Freelance and Consultancy Opportunities: Offer services as a GST consultant and help businesses comply.
Career Opportunities After a GST Course
A GST course can offer the following few career opportunities:
GST Consultant
Taxation Executive
GST Compliance Manager
Accountant with GST specialization
Business Advisor
How to Select the Best GST Course
Course curriculum and coverage of topics
Certification and accreditation
Method of learning (offline/online)
Faculty expertise and industry relevance
Reviews and ratings by alumni
Conclusion
A GST course is a good investment for anybody who wants to gain more knowledge in taxation and bring his or her career to the next level. As a student, a professional, or an entrepreneur, you can learn GST and get the skills needed to optimize the tax process. If you want to skill up, enrolling in a GST course may be the ideal next move.
#gst course in delhi#gst certification course in delhi#tally gst course in delhi#gst course duration#gst course fee#what is gst course#gst practitioner course in hindi
0 notes