#RCM Overview
Explore tagged Tumblr posts
Text
Revenue Cycle Management (RCM) is not a one-size-fits-all solution; it's a complex tapestry of essential components working together seamlessly to achieve financial stability and success for healthcare organizations. Let's explore the three key components of an effective RCM strategy in more detail.
0 notes
Text
jean vicquemare skillset
half-assed, very brief overview of jean’s skills i constructed for this oneshot i wrote:
https://archiveofourown.org/works/66613924
I didn’t end up using some of them, but i might for future stuff… who’s to say.
(imo the average person would not have the amount of skills harry has — he is an exceptional case — but for the sake of keeping things even, i’ve maintained six skills per category. some of them aren’t new because i believe harry has some skills universal enough that jean would have them too. everything else is based off bits of canon, speculation, or just purely made up for funsies. enjoy!)
INTELLECT
1. Logic
- The ability to piece together clues, detect inconsistencies, think rationally about things, etc. As per Harry’s version in canon (though arguably a bit more refined).
2. Retort
- Broadly speaking this is Jean’s capacity to create witty/dry/harsh/whatever-the-situation-calls-for comebacks. Usually manifests in the form of sarcasm but can be quite funny when he wants to be.
3. Parlé
- Distinct from Retort in that this is purely Jean’s ability to argue, convince, and converse. Basically Rhetoric.
4. Investigation
- Jean’s ability to be a good detective. Less of the praxis side of things and more concerned with being methodical (in some sense, it is an amalgam of all Intellect skills but specifically focuses on the RCM side of it; i.e. looking deeper into evidence, interrogating suspects etc.)
5. Labyrinth
- A more pragmatic version of Shivers. Knowing all the nooks and crannies of Jamrock (and Revachol in general); where to go, who knows what. Understanding the city like the back of one’s hand.
6. Masquerade
- Drama, essentially; the ability to play a role, act, lie, be whatever the situation needs him to be (case in point: showing up to the Whirling-in-Rags for three days in a wig. That sort of thing).
PSYCHE
1. Willpower
- Jean’s Volition. This is will to keep going in spite of all signs suggesting otherwise. The mental fortitude he has to possess to get through the day, to stay steady and vigilant and alive. This can sometimes result in him coming off as a bit too aloof if he keeps his walls up too high.
2. Isle of Man
- Man is an island when he is alone. This is simultaneously Jean’s feelings of being isolated from others, and isolating himself from them. Useful in terms of temporary self-preservation, but definitely not sustainable in the long run.
3. The Next World
- Hope. Belief. Optimism. Things which do not exist in this world, but are possible for the next. Jean is fundamentally a very hopeful person; this is exemplified by him continuing to look out for Harry despite everything, and ‘the Next World Mural’ case. He believes that things can and will get better — not necessarily for him, but for others. Has some elements of Inland Empire (i.e. imagination).
4. Anomaly
- Clinical depression. Named after that one line where he says the doctors call it an ‘anomaly’. There is nothing positive about this skill in any way, really; it is inherently numb, life-sucking, fearful, hateful, and occasionally contains some suicide ideation. A counterbalance to both Willpower and the Next World.
5. Saviour
- Jean’s version of Empathy, but much more intense. The desire to save people, even when they cannot be saved. I H/C that this used to just be Empathy, but his brain renamed it as Saviour without him really knowing when or why (cough cough it would happen as Harry begins to decline cough cou). This can be a very good skill when used in the right way, but can easily have a detrimental effect on him.
6. Esprit de corps
- Understanding cop culture. He’d lack the aspect Harry has to know exactly what an officer is doing at a certain point in a different time/location, but generally Jean would have an understanding of how his fellow officers are feeling, their attitudes in a workplace/field context, etc.
PHYSIQUE
1. Adrenaline
- The ability to threaten and feel threatened. The body taking control to prepare Jean for a stressful, violent, or any other similar situation. Basically flight-or-fight, basically Half-Light.
2. Musculature
- Brute power and strength. Using his muscles, body, strength, all that to intimidate others (he’s mentioned as being ‘buff’ by like three different people in canon so.)
3. Paramour
- Feelings of love and romance, often shrouded in secrecy and shame (linked to the Next World, somewhat supported by his potential feelings towards Judit as indicated in canon — in general, though, he seems like the type of guy who would harbour uncomfortable feelings about letting himself love and be loved back).
4. Masochist
- Simultaneously the opposite and complimentary skill to Paramour; this is the desire to be hurt by others. The angry part of Jean that seeks pain and punishment.
5. Junkie
- Jean’s inclination for drugs (sometimes alcohol, but mostly drugs — amphetamines and occasionally ketamine). Despite the name, he still maintains some sense of self-control here.
6. Constellation
- Jean’s insecurities, mostly the physical ones. H/C that once during a night out with Harry, while very, very drunk and feeling very, very sorry for himself, he’d made some sort of stupid comment about his pockmarks looking like constellations in an attempt to be charming. Something like that. The sort of thing to shift Jean’s worldview, to the point of still retaining this certain deeply rooted anger about himself but giving it a new name (much like Empathy/Saviour. A lot of his identity is tied to Harry, and this would be no different — but that is more writing for another time).
MOTORICS
1. Sharpshooter
- Hand/eye coordination but predominantly for firearms. All other H/E checks would probably fall under this too tbh.
2. Equestrian
- Affinity for horses #horsegirljeantruther
The rest of Jean’s Motorics skills — Perception, Pain threshold, Reaction Speed, and Composure — are just as per what’s canon for Harry. Honestly I only redid this category so I could shoehorn that Equestrian skill in there.
25 notes
·
View notes
Text
X7 Narrative Overview Transcripts and Notes: Acts IV-V, Analysis, & Endings Sections
Be warned, this is very long. You can scratch off my "I'm not gonna squint" comment from the last one, I ended up squinting so hard that now mermaid people are canon in DE, I guess?
Read my Acts 1, 2 and 3 transcripts here.
Once again, this does not include the first "Summary" slides of acts IV and V, which I already transcribed like yonks ago.
Act IV: The Doubt

me doubting my decisions
Location
Top box: "2 nautical miles to Hämärä Maa"
Blue sticky note: "Another Locust Dream... Visuals TBD"
Bottom of slide: "[...] and clearly all the inmates have much more freedom than they would in a more traditional prison. At the same time the cost of living and the low income has forced some of the guards to [...] and sometimes it can cause a friction. Imagine coming home from the [...] and watching a [...] guard on the [...] He's sorry [...] kicked him out, he just needs a place to crash for four days. Overall there's a beautiful [...] in the [...] sincerity in the Tréville. ([...] about taking [...] don't you?)"
Characters


Supporting: Gang of Girls
Purple box: "Philippe Constance Rhöne" Grey-ish box: "Middle Man" Blue box: "Family Friend" Bottom olive box: "Girl gang" Two blue stickies: "Horse thief?" "Siamese Twins?"
Plot details
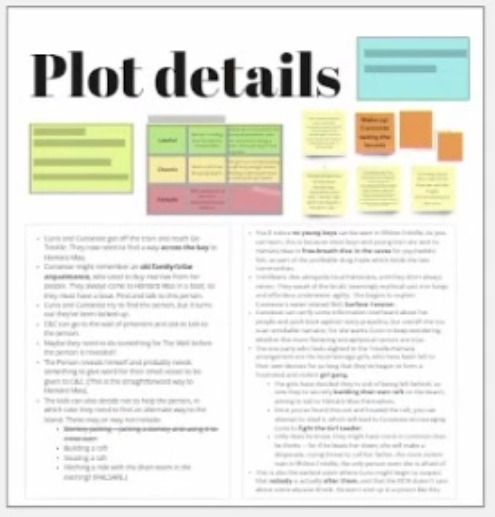

Bottom box:
Cuno and Cunoesse get off the train and reach the Tréville. They start seeking a way across the bay to Hämärä Maa.
Cunoesse might remember an old family/tribe acquaintance, who used to buy marrow from her people. They always came to Hämärä Maa in a boat, so they must have a boat. Find and talk to this person.
Cuno and Cunoesse try to find the person, but it turns out they've been locked up.
C&C can go to the wall of prisoners, and ask to talk to the person.
Maybe they need to do something for The Wall before the person is revealed?
The Person reveals himself and probably wants something to [...] for their small vessel to be given to C&C. (This is the straightforward way to Hämärä Maa.)
The kids can also decide not to help the person, in which case they need to find an alternate way to the island. These may or may not include: Donkey-jacking -- jacking a donkey and using it to cross over; Building a raft; Stealing a raft; Hitching a ride with the diver-beam in the evening? (FAILSAFE) [A/N: confident this one is correct, how are they crossing over on a donkey???]
[...] prison boys [...]
[...] Skill, Surface Tension.
[...]
[...] girl gang.
Subpoint: [...] they've been secretly building their own raft on the beach, aiming to sail to Hämärä Maa themselves.
Subpoint: Once you've found this out and located the raft, you can attempt to steal it, which will lead to Cunoesse encouraging Cuno to fight the Girl Leader.
Subpoint: Little does he know, they might have more in common than he thinks -- for if he takes her down, she will make a desperate, crying threat to call her father, the most violent man in Rhöne-Tréville, the only person even she is afraid of.
This is also the earliest point where Cuno might begin to connect that nobody is actually after them, and that the RCM doesn't care about some abusive drunk. He won't end up in a prison like this.
Tasks

Critical tasks:
Find a way across the strait to Hämärä Maa:
Jack the raft
Swarm evolves
Side tasks:
"More like *dread* raft" - Dress the raft up, make it pretty.
Make the warden look like a fool.
"What would a real Rhöne do" with Philippe Constance Rhöne.
Win The Wall's respect.
Set up an enterprise, Cuno's little Shit Show.
Reactivity/Outcomes:
Swarm variations
Items

Maybe: Book; Prison photo [...]; Magazine
Thoughts, Special Assets
Cuno thought: "I am Cuno"
Systems asset: "Leave the area by boat/raft.
Relationship Beats
Cunoesse vs. Her Kind; Cuno vs. The Unfamiliar
Act V: The Arrival

Location
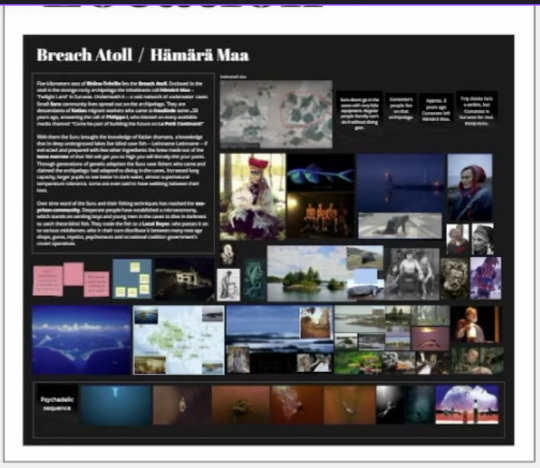
Breach Atoll / Hämärä Maa
Top left box: "Five kilometers west of Rhöne-Tréville lies the Breach Atoll. Erected in the atoll is the strange rocky-archipelago the inhabitants call Hämärä Maa - "Twilight Land" in Suruese. Underneath it -- a vast network of underwater caves. Small Suru-community lives, spread out on the archipelago. They are descendants of the Katlan migrant workers who came to Insulinde some ~50 years ago, answering the call of Phillippe I, who broadcast on every available media channel. "Come be part of building the future on Le Petit Continent!"
[...]-there, the Suru brought the knowledge of Katlan shamans, a knowledge that in deep underground lakes live blind-cave fish -- Latinname Latinname -- if distracted and prepared with few other ingredients, the brine made out of the bone marrow of that fish will get you so high you will literally shit your pants. Through generations of genetic adaptation the Suru cave fishers who came and claimed the archipelago had adapted to diving in the caves. Increased lung capacity, larger pupils to see better in dark water, almost supernatural [...], some are even [...]
Over time word of the Suru and their fishing techniques has reached the exo-prison community. Desperate people have established a microeconomy, which stands on sending boys and young men in the caves to dive in darkness to catch these blind fish. They trade the fish to a Local Buyer, who passes it on to serious middlemen, who in their town distribute it between many new age shops, gurus, mystics, psychonauts and occasional coalition government's covert operatives."
Top right stickies: "Cave divers go in the caves with very little equipment. Regular people literally can't do it without diving gear." "Cunoesse's people live on that archipelago." "Approx. 3 years ago Cunoesse left Hämärä Maa." "Trip thinks he's [...], but Cunoesse is [...]."
Characters
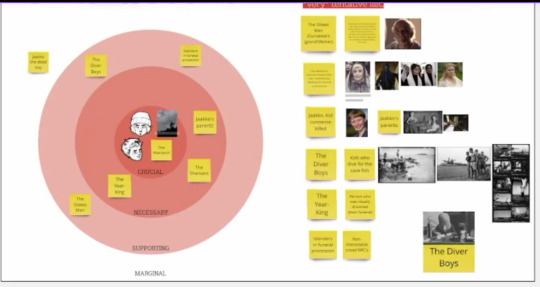
Character bubble: Crucial: Cuno, Cunoesse, [...], The Matriarch Necessary: Jaakko's parents, The Shamans, The Year-King Supporting: The Diver Boys, Islanders in funeral procession, The Oldest Man Marginal: Jaakko, the dead boy
Character list: Note on top reads: "*very* tentative list." Row 1: The Oldest Man (Cunoesse's grandfather); [too small to read] Row 2: The Matriarch (current head of the [...] / community, leading the funeral procession) Row 3: Jaakko, Kid cunoesse killed; Jaakko's parents Row 4: The Diver Boys; Kids who dive for the cave fish Row 5: The Year-King; Person who was ritually drowned (their funeral) Row 6: Islanders in funeral procession; Non-interactable crowd NPCs; The Diver Boys
Plot Details

Box 1: So what *is* Cunoesse's story?
Cunoesse has brought Cuno to Hämärä Maa as a replacement for a kid she drowned three years ago.
Cuno and Jaakko -- the drowned kid -- don't have a lot in common. Both are/were boys with red hair, and about the same build but that's about it. Only a child's mind would come up with a plan to replace the dead kid with an 'identical' one so she'd be accepted back in her tribe.
But Cuno can't just be like Jaakko, he has to *become* Jaakko.
The Suru have a coming of age rite that involves drinking a brew made of the bone marrow of a blind underwater cave fish. This experience has sometimes profound, sometimes devastating effect on one's consciousness.
Subpoint: Perhaps this "Naming Ceremony" doesn't happen until the Hämäräns are 11 years old, so that's why Cunoesse never got her name, and this is the pretense under which she lures Cuno into the ceremony -- a name for herself (but Cuno doesn't know it's also going to be a new name for him.)
Cunoesse believes that if she subjects Cuno to this ceremony and "spirit guides" him through this process Cuno might actually *become* Jaakko. Or at least accept he's Jaakko now. She's been laying foundation for this transformation throughout this whole journey.
Cunoesse's people thought her dead, drowned with the boy. Hardly anyone could recognize her at first sight.
Subpoint: Maybe Cunoesse hid the body |under a rock in one of the caves| before she fled Hämärä Maa, so in her mind no-one can definitely claim the kid she brought back isn't Jaakko.
Box 2: Psychedelic Sequence
We want this to be a visually memorable and spectacular setpiece, where we can bend the rules of everything we visually do with dialogue and visuals and apply dream-logic.
The entire underwater showdown will be in FELD.
We can depart from / play with the isometric perspective, switching from a side-view showing the vastness of the dark ocean, with C&C small figures, sinking.
Experiment with overlays, filters as well as painted and/or 3D modeled additions to the scene, showing people, motifs and iconic elements from their journey. There can be lots of reactivity here, with the visual elements reflecting decisions the player had made throughout the game.
Competitive Red Checks are the key new feature we want to test here, to create unique playthroughs and the impression of truly "fighting yourself" as the rolled value of Cuno or Cunoesse's Red Checks affects the difficulty of the other's counter-attack.
For the first time Skills may break the barrier and commune with each other.
Cunoesse comes out of the trip with +1 Psyche if she lives.
Stickies: Multiple life/death outcomes. Swarm / Locust City side-plot reaches its conclusion. End of Evangelion style psychedelic underwater fight sequence. New Home for Locusts Funeral cultural event.
Tasks

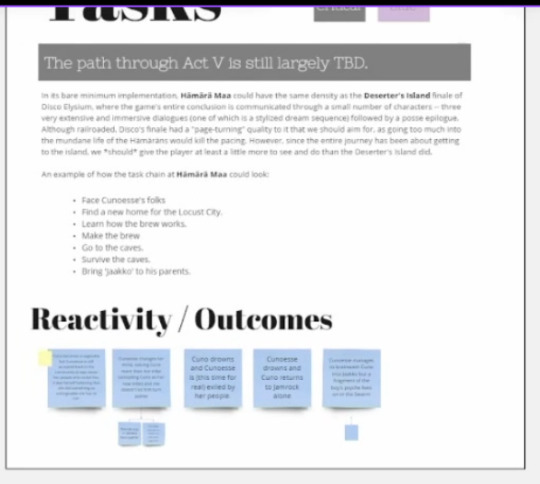
Note on slide reads "needs work"
Critical: "The path through Act V is still largely TBD." "In its bare minimum implementation, Hämärä Maa could have the same density as the Deserter's Island finale of Disco Elysium, where the game's entire conclusion is communicated through a small number of characters -- three very extensive and immersive dialogues (one of which is a stylized dream sequence) followed by a posse epilogue. Although railroaded, Disco's finale had a *page-turning* quality to it that we should aim for, as going too much into the mundane life of the Hämäräns would kill the pacing. However, since the entire journey has been about getting to the island, we *should* give the player at least a little more to see and do than the Deserter's island did.
An example of how the task chain at Hämärä Maa could look:
Face Cunoesse's folks
Find a new home for the Locust City.
Learn how the brew works.
Make the brew
Go to the caves.
Survive the caves.
Bring 'Jaakko' to his parents."
Reactivity/Outcomes: [...] Cunoesse changes her mind, valuing Cuno more than her tribe (accepting Cuno as her new tribe and she doesn't let him [...] Jaakko) [Two sub-stickies, illegible] Cuno drowns and Cunoesse is (this time for real) exiled by her people. Cunoesse drowns and Cuno returns to Jamrock alone Cunoesse manages to brainwash Cuno into Jaakko [...] fragment of the boy's psyche lives on in the depths [One sub-sticky , illegible]
Items
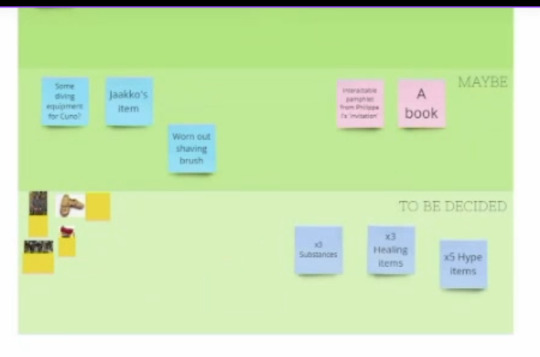
Definitely: Interactable: The blind cave-fish
Maybe: Other: Some diving equipment for Cuno?; Jaakko's item; Worn-out shaving brush Interactable: Interactable pamphlet from Philippe I's 'invitation'; A book
To be decided: Consumable: x3 Substances; x3 Healing items; x5 Hype items
Thoughts

Cunoesse: Jaakko drowning [+5 blank Thought diamonds] Cuno: Dark jungle; If not *trust* then...? [+4 blank Thought diamonds]
Special Assets
Systems: Arrive by boat/raft; Sailing of [...] (has been cut); [...] Art: Area map; Location splash screen; Hämärän Culture Design; Cultural [...]; Psychedelic dream sequence Audio: Psychedelic dream sequence; The [...] of Hämärä Maa
Relationship Beats
Cunoesse vs. Cuno
Analysis
(Note: This section is EXCLUSIVELY production-related. If you're just here for lore, scroll down to the endings. I will keep the screenshots here much more sparse.)

Total map size: approx. ~1 Martinaise. (Act 2 = the right side of the Traffic Jam zone; Act 3 = the length of the Traffic Jam zone; Act 4 = the entirety of the Church peninsula; Act 5 = Whirling-in-Rags, part of dock, the Capeside Apartments)
Total characters per Tier Tier system explanation (and Disco Elysium analogies)
Crucial (5 characters) - Characters required for the minimum viable path from the first scene to the ending of an Act. (Klaasje, Titus, Ruby, Deserter, Hanged Man, Jean Vicquemare.)
Necessary (16 characters) - Characters who affect the main story significantly, requied[sic] for an enjoyable player experience. (Everart[sic], Joyce, Measurehead, Garte, Station Radio, Sylvie, Lillienne, Dora, Lena and Morrell.)
Supporting (10 characters) - Smaller NPC's who have information affecting the main story, but are skippable. (Cuno, Idiot Doom Spiral, Rosemary, Paledriver, Roy, The Pigs, The Gardener).
Marginal (7 characters) - Additional folks with very little to no bearing on the main story, but with side-tasks of their own. (Working Class Woman, Annette, Dicemaker, Easy Leo, Mega Rich Light Bending Guy, the Ravers, PIss & Fuck, Mañana.)
Total: 38 (characters with portraits & VO (barking NPC's not included))
Character Matrix: "Considering the discrepancy in subjective story significance of a character vs. their actual mechanical importance (e.g. Cuno in Tier 3, Jean in Tier 1), another dimension needs to be added in order to provide the full picture: the expected word count, quantifying how much a character has to say to you over the course of the game.

Downscoping approaches: "Should the scope need to be adjusted, there are two diretions we can take. The trade-off between the number of locations and the distribution of the character population will be a fine balancing act to ensure the locations aren't too barren, nor that the supporting characters cast balloons out of scope. We believe the current number and population of acts are optimal to tell the story we want to tell. More discussion is need on how we should approach scoping each location as well as the story in total; the two most orthogonal approaches are depicted below."
Scenario 1: High location variety; Low character stratification Keep five distinct Locations/Acts, but remove marginal characters and cut down on supporting cast.
PROS:
Keeps the maps fresh & simple, not too long in any one place
Maintains the "road story" vibe
Sense of traveling large distance
A new and unexpected direction for a Disco-like cRPG.
CONS:
Loses the layered richness of the Disco world
Characters in the world only exist to prop up the main story
Hard to ensure each map has enough meaningful content with too few characters
Scenario 2: Low location variety; High character stratification Reduce the number of Locations/Acts, but maintain a higher number of characters in each.
PROS:
The world of Disco is rich because of its supporting cast
Less need to "cram" into a few characters
Easier to populate map with content & reactivity
CONS:
Trouble maintaining the central conceit of a journey
Locations become more complex
Extensive plot reworks needed
Lower art cost, but higher writing & casting cost.
Endings

Summary
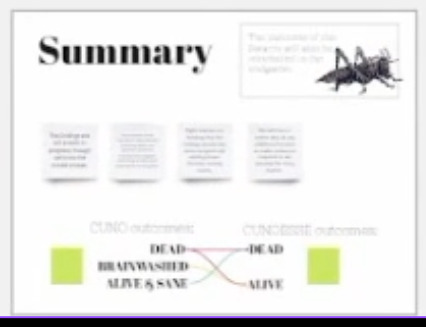
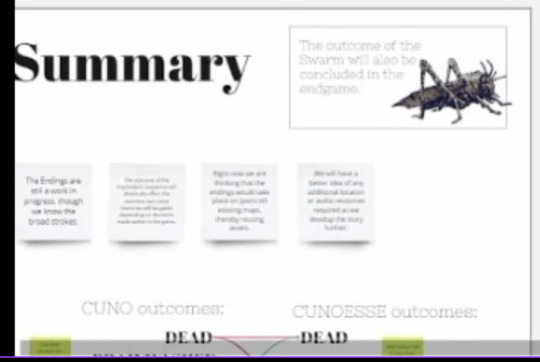
Top right box: "The outcome of the Swarm will also be concluded in the endgame."
Stickies: "The Endings are still a work in progress, though we know the broad strokes." "The outcome of the psychedelic sequence will dramatically affect the [...], [...] will be [...] depending on the choices made earlier in the game. "Right now we are thinking that the endings would take place in (part of) existing maps, thereby reusing assets." "We will have a better idea of any additional location or audio resources required as we develop the story further."
Cuno potential outcomes: Dead; Brainwashed; Alive & Sane Cunoesse potential outcomes: Dead; Alive Potential endings: Cuno dead and Cunoesse dead; Cuno dead and Cunoesse alive; Cuno brainwashed and Cunoesse alive; Cuno alive & sane and Cunoesse dead [Two sticky notes, illegible]
Ending 1: Jaakko Ending
Cunoesse alive, Cuno brainwashed Location: Hämärä Maa
Sticky notes: "Cunoesse's manipulation worked. Cuno has fully internalized Jaakko." "The scene closes with Cuno diving dead-eyed among the Hämärän boys. He's one of them now." "Loss of identity. No more Cuno-sentences.
Ending 2: Pale Ending
Cunoesse dead, Cuno alive Location: Tréville, deserted
Sticky notes: "With Cunoesse dead, Hämärä Maa holds nothing for Cuno anymore. He turns back, aimless." "He lands back in Tréville and finds it deserted. The prison has finally moved." "One prisoner has been left behind. They've forgotten him. He could go anywhere, but he [...] "Surely they'll come back for me, won't they?"" "Cuno sits with him. With Cunoesse's death, Cuno's prison has left him too. The thing about freedom is that no one tells you where to go." "Cuno waits with the prisoner indefinitely. We fade to white and roll credits."
Ending 3: Bad Ending
Cuno dead, Cunoesse dead Location: ?
Ending 4: Cycle Ending
Cunoesse alive, Cuno dead Location: ?
Sticky notes: "With Cuno dead and her plan foiled, Cunoesse must exile herself from Hämärä Maa. Again." [...] "[...] has irrevocably closed. In [...], Cunoesse finds that she is bleeding the only blood not of violence. [...]" "The Interval Skill announces: "A new epoch of timekeeping is beginning."" "She goes into another Murder Hangover, back to sleep and hibernation."
Ending 5?: New Tribe Ending
Cunoesse alive, Cuno alive Location: ?
#not par art#disco elysium#locust city#i'll make one final post after this for Miro board stuff (probably just the “major systems” bit)#(the minor systems one is just a rehash of DE stuff and is mostly unreadable)#(and the swarm one was already transcribed by someone else lol)#i'll see what other text is strewn throughout the video too maybe
13 notes
·
View notes
Text
The Regions of Kishetal

Pictured Above: An environmental map of the land of Kishetal

Pictured Above: A map of the 7 Kishic Regions

Pictured Above: A map of the Kishic City-States and their territories

Pictured Above: A map of Significant Stable Forestfolk Populations
Here is a quick overview of the regions of Kishetal, the homeland of Narul and Ninma. And some good ol' maps. I'll be posting in the future about some of the creatures and forestfolk mentioned below!
As always send questions please!
Continues below the cut!
The Regions of Kishetal
1. The Red Cedar Mountains

Pictured Above: The Red Cedar Mountains near Kepfis
The Red Cedar Mountains stretch from the Shabalic Sea in the north nearly to the Sea of Agitu in the south. The Red Cedar Mountains were formed in ancient times having already been present in the Age of Metal and Glass. However, the Red Cedar Mountains are not among the eleven “Chains of Sanctuary,” those mountain ranges around the planet in which humanity sheltered from the wrath of the gods during the Calamity. The predominant underlying stone of the RCM is limestone, with occasional but significant areas and deposits of serpentinite, basalt, and dolerite. The region experiences warm summers and cold winters, often with considerable snow and rainfall, particularly at higher elevations. The Mountains surround Lake Shebali, which acts as an inland sea and a source of food and transport for much of eastern Kishetal. At lower elevations, such as Labisa, the predominant vegetation is juniper and oak. Forests of black pine, cedar, and fir are dominant and common at higher elevations. The highest peaks are home to alpine meadows. Wild grapes, figs, and olives are all abundant in this region alongside their domesticated cousins.
Some fauna include wolves, jackals, wild goats, giant minks, wild bulls(aurochs), leopards, kishic lions, kishic tigers, caracals, roe deer, gazelle, wild boar, eagles, storks, horned rabbits, kishic brown bears, lynxes, and kishic ibex.
Very rarely found is the Kishic Elephant, actually a species of mammoth, these tiny pachyderms are about the same size as the average dairy cow. Only about 100 still survive in sheltered valleys to the north.
Examples of monstrous and magical Fauna including Flesh-eating deer, kiriki, dorasi, and the kutiri. While there are rumors of larger monsters such as dragons, these are mostly little more than legends and folklore. Though there is no telling what creatures could be hiding in the many caves and tunnels which dot the mountains.
There are numerous small forestfolk tribes which live in isolated areas.
(I will post more about that later)
2. The Felic Plain

Pictured Above: The Felic Plain north of Boshalum
The Felic Plains primarily consist of grassland with occasional patches of deciduous forest. The area is famed for its almond trees and its many wildflowers, including wild roses and hasir flowers. During the fall, great patches of the plains turn red with the blooming of hasir flowers.
The region experiences hot summers and mild but wet winters, which makes the region ideal for farming. As such, the Felic Plains act as the bread-basket of Kishetal. The region is split by the Aratshin River, which extends from Lake Shebali to the Green Sea. The plains are disrupted by an especially dense forested area known as the Garden. All attempts to settle the Garden have failed.
Fauna include, wolves, jackals, gazelles, wild bulls, kishic lions, deer, eagles, storks, horned rabbits, kishic brown bears, foxes, wild goats, polecats( which are popular pets), felic falcons, and hyenas.
The plains are home to several monstrous/magical species, including Flesh-eating deer, garudu, takmek, and the Unturu Serpent.
There are a handul of forestfolk tribes as well as a single hillfolk tribe in this region.
3. The Western Coast

Pictured Above: The Western Coast near the city-state of Chibal
The Western Coast borders the Green Sea stretching from Bura in the north to Bisabal in the south. The ecoregion has a warm semi-tropical climate akin to a Mediterranean climate. Winter is the wettest season, and summer is the driest.
The Western coast consists primarily of three biomes. The deciduous forests in the north consist primarily of hornbeams, oaks, maples, cedar, and black pine. The central marshlands surrounding Udur have heavy concentrations of reeds, papyrus, poplar, and willow. The southern plains are similar to the Felic plain region though typically arider. Bay, olive, carob, and sweetgum are all common in this region. The Green Sea and its coast are home to many kinds of edible seaweed which form an essential part of the Chibalic and Buric diets.
Fauna include wild boars, foxes, jackals, wolves, badgers, wildcats, coastal brown bears, gazelles, deer, wild bulls, wild goats, and storks. Marine life includes dolphins, seals, whales, sea turtles, and many species of fish.
Monstrous fauna include bulari, sea-dragons, serpents, krinari, and ramitalek.
Aside from Ikopeshi's there are no surviving forestfolk tribes in this region.
4. The Northern Coast/Sheprian Forest

Pictured Above: The Sheprian Forest near Shepra
The Sheprian forest in the northern part of Kishetal is primarily composed of deciduous trees with occasional conifer patches at areas with higher elevations. Common trees include oak, chestnut, birch, hornbeam, black pine, cedar, and beech.
The climate is temperate with warm dry summers and cold wet winters. The north is typically thought of as the wildest region, with most city-states and settlements, including Shepra, clinging to the Corin river. Sheprian poetry is a unique variety of poetry, similar to the Japanese haiku, which originates from the forest festivals of the northern coast.
Fauna include wolves, jackals, gazelles, wild bulls, kishic lions, deer, eagles, storks, horned rabbits, kishic brown bears, foxes, wild goats, giant minks, horned rabbits, wild sheep, eagles, and kishic leopards.
Monstrous fauna include flesh-eating deer, garudu, kiriki, dorasi, and winged tigers.
This region contains the second highest concentration of forestfolk after the Red Cedar Mountains.
5. The Southern coast

Placed Above: The Southern Coast near Bisabal
The Southern Coast consists of three regions; the southern deciduous forest, the scrubland, and the plains. The climate in the south is quite warm, with summers being hot and dry and winters mild in both temperature and rainfall. On rare occasions, the southern coast may experience heavy snowfall.
Major cities are sparse however, many villages dot the southern coast, many of these villages rely on piracy, preying primarily on Apunian and Jezaani ships traveling to and from the Western Coast.
Limestone plateaus and outcroppings are near the border of the southern coast, and the desert are said to be the remains of ancient buildings though this is not true.
Poplar, olive, bay, carob, almond, oaks, and umbrella pine are all common.
Fauna includes wolves, jackals, gazelles, wild bulls, kishic lions, deer, eagles, storks, horned rabbits, kishic brown bears, foxes, wild goats, polecats, felic falcons, kishic leopards, and hyenas.
The south is home to relatively few monstrous/magical species though it is home to the largest population of kiriki in Kishetal.
There are only two forestfolk populations in this region.
6. The Kipsian Desert

Pictured Above: The limestone formations of the Kipsian desert south east of Kipsu.
The Kipsian desert is the least populated region of Kishetal as the arid environment is not conducive to agriculture. Ruins of older civilizations suggest that the area may have once been more hospitable.
Plant life is sparse and largely limited to hardy shrubs and grasses. The region is famous for its carob and the candies and sweets produced from the carob by its inhabitants. Mesa, plateaus, pillars, and other stone structures are common; foreign visitors often visit the region seeking religious or spiritual enlightenment amongst the arches and columns. Many never leave.
Fauna include jackals, gazelles, kishic lions, deer, gazelle, wild asses, and hyenas. The Kipsian desert is also the only region in Kishetal in which the kishic ostrich and oryx survive.
Monstrous fauna include Flesh-eating deer, takmek, sikara, kiriki, and giant lions.
There are no forestfolk populations here.
7. The Makurian Steppe

Pictured Above: The Makurian Steppe north of Shebal
The Makurian steppe is massive, spreading over most of western Masia. Only a tiny sliver of that vast extent falls in Kishetal. Trees are almost entirely absent. Vast expanses of grass-covered hills define the area. To the north of the steppe is the Shabalic forest, and to the south is the Jezaaic desert.
The heavy presence of sagebrush, sedges, and grasses and the relatively dry climate have led to a preference for a nomadic and pastoralist lifestyle. Makurian tribes regularly raid and intrude in the region, with their westward pushes typically being halted by the mountains.
Fauna include wild horses, wild asses, wild bulls, jackals, gazelle, deer, mountain sheep, macuri lions, and leopards.
Monstrous fauna include the tomob and the wulut.
There are only 3 native forestfolk populations in this region.
As always ask questions! Anything! And if y'all like this I might do this with some other regions.
@patternwelded-quill @flaneurarbiter @skyderman @blackblooms @roach-pizza @illarian-rambling @dezerex @theocticscribe @axl-ul, @persnickety-peahen @angie-j-kay
@surroundedbypearls I was looking through my intro post and I just realized I've been completely forgetting to put you in the taglist! Sorry about that!
#writeblr#writing#fantasy#worldbuilding#writer#fantasy writing#queer fantasy#fantasy world#testamentsofthegreensea#fantasy map#fantasy novel#fantasy worldbuilding#world building#narul#writblr
61 notes
·
View notes
Text
Medical Service Provider: A Complete Overview
In today’s fast-evolving healthcare industry, the term medical service provider has gained immense importance. These providers form the backbone of the healthcare system by delivering essential medical services — from clinical care and diagnostics to administrative support and medical billing.
What is a Medical Service Provider?
A medical service provider refers to any individual or organization that offers medical-related services to patients or healthcare institutions. These services can be clinical (like treatment or diagnosis) or non-clinical (like billing, coding, or telemedicine support).
Common examples include:
Hospitals & clinics
Physicians & specialists
Diagnostic labs & imaging centers
Medical billing & RCM companies
Telehealth platforms
Home healthcare providers
Types of Medical Services Offered
Clinical Services
General consultation
Emergency care
Surgical procedures
Specialized treatments (cardiology, neurology, etc.)
Diagnostic Services
Blood tests
X-rays, MRIs, and CT scans
Pathology and genetic testing
Support Services
Medical billing and coding
Health information management
Revenue cycle management (RCM)
Insurance verification and claims handling
Digital Healthcare Services
Telemedicine consultations
Remote patient monitoring
e-Prescriptions and digital health records
Why Medical Service Providers Are Important
Medical service providers play a critical role in:
Ensuring Timely Care: Quick and reliable services help improve patient outcomes.
Improving Healthcare Access: Through telemedicine and mobile clinics, services reach remote areas.
Streamlining Operations: Backend services like billing and RCM allow doctors to focus on patient care.
Maintaining Compliance: Trained providers ensure adherence to healthcare laws and data privacy (e.g., HIPAA).
Qualities of a Good Medical Service Provider
A top-tier provider should offer:
Skilled professionals and specialists
Transparent and secure systems
Reliable service delivery with timely support
Scalable solutions for clinics or hospitals
Data security and HIPAA compliance
Virtual Oplossing – Your Trusted Medical Service Provider
At Virtual Oplossing, we specialize in offering advanced medical support services including medical billing, coding, revenue cycle management, and digital health solutions. With a focus on accuracy, efficiency, and compliance, we help healthcare providers deliver better care while improving their financial outcomes.
Our Key Services:
Medical Billing & Coding
RCM Solutions
Telehealth Support
Data Management & Reporting
Conclusion
A reliable medical service provider helps bridge the gap between patient care and healthcare operations. Whether clinical or administrative, choosing the right partner can enhance efficiency, compliance, and patient satisfaction. As the industry continues to evolve, providers like Virtual Oplossing are leading the way in modern, tech-enabled healthcare support.
0 notes
Text
Is Payment Posting the Right RCM Career for You?

RCM is essential for helping healthcare providers receive accurate and timely payments for the care they deliver. Among these roles, payment posting stands out as both vital and rewarding. For those exploring medical billing jobs, becoming a payment posting specialist can be a promising career path. But how do you know if this is the right fit for you?
Let’s explore what a career in payment posting involves, its significance in the RCM process, and the qualities you need to thrive in this role.
What Is Payment Posting in RCM?
Payment posting is the process of recording payments received from insurance companies and patients into the medical billing system. It is a critical step in the revenue cycle, helping ensure that the healthcare provider’s financial records accurately reflect incoming payments.
There are typically two types of payment posting:
Manual Posting – Data entry professionals manually input payment details from Explanation of Benefits (EOBs).
Electronic Remittance Advice (ERA) Posting – An automated method that processes electronic payment files.
Regardless of the method, accuracy and speed are crucial. Errors at this stage can lead to claim discrepancies, patient dissatisfaction, or revenue loss.
Why Consider Payment Posting Specialist Jobs?
If you’re looking at jobs with long-term growth and stability, payment posting are a strong choice. Here’s why:
Foundational Role in the RCM Process
Payment posting is more than just entering data—it provides insights into the financial health of a healthcare practice. By analyzing denials, underpayments, and trends, payment posters help identify and prevent revenue leakage.
High Demand and Job Security
As the healthcare industry grows, so does the demand for skilled RCM professionals. Payment posting is a specialized skill, and many providers prefer dedicated staff or outsourced teams to manage this task efficiently. This creates a steady stream of opportunities for skilled candidates.
Entry-Level Access with Career Advancement
Many payment posting jobs are open to candidates with basic training in medical billing or healthcare administration. Over time, professionals in this role can advance to senior billing positions, denial management, or even RCM leadership roles.
Skills Needed to Succeed in Payment Posting
Before diving into this career, it’s important to assess whether your skills and interests align with the role. Successful payment posters typically possess:
Attention to Detail: Accuracy is non-negotiable when entering payment data.
Familiarity with EOBs/ERAs: Understanding various formats of payment documentation is key.
Analytical Thinking: Spotting patterns in denials or short payments can help identify systemic issues.
Time Management: Handling high volumes of data within tight deadlines is a daily task.
Basic Software Proficiency: Knowledge of billing software and spreadsheets is a plus.
If these strengths resonate with you, then payment posting may be a perfect entry into the world of medical billing jobs.
Day in the Life of a Payment Posting Specialist
Wondering what a typical day looks like? Here’s a brief overview:
Log into the billing software and retrieve ERAs or scan EOBs.
Post insurance payments and patient payments into the system.
Adjust claims based on contracted rates, write-offs, or denials.
Flag discrepancies and notify the denial management team.
Maintain logs and generate reports for daily transactions.
It’s a role that combines routine with responsibility, offering stability and the satisfaction of keeping the revenue cycle moving smoothly.
Is Payment Posting Right for You?
To decide if payment posting are a good fit for you, consider the following:
Do you enjoy administrative tasks and working with numbers?
Are you patient, organized, and deadline-driven?
Are you looking for a healthcare role without direct patient interaction?
Do you aspire to build a long-term career in medical billing jobs?
If you answered "yes" to most of these, then payment posting could be your ideal starting point in the RCM industry.
How RCM HIRE Can Help
At RCM HIRE, we specialize in connecting talented professionals with the right opportunities in the medical coding and billing field. Whether you’re a fresher looking to start your career or an experienced professional aiming to switch roles, we help you find the best fit in the growing world of RCM.
Final Thoughts
Payment posting may seem like a behind-the-scenes role, but its impact on a healthcare organization’s revenue cycle is massive. It’s an excellent opportunity for those seeking structured work, career stability, and a chance to contribute to healthcare operations without being on the clinical frontlines.
#medical billing services#medical coding services#rcm services#revenue cycle management#payment posting
0 notes
Text
Comparing Traditional vs. AI-Powered Revenue Cycle Management Technologies
In the evolving landscape of healthcare, revenue cycle management technology plays a pivotal role in ensuring the financial health of medical institutions. Traditionally, medical billing solutions relied heavily on manual processes, leading to inefficiencies and errors. However, the advent of Artificial Intelligence (AI) has revolutionized these systems, offering enhanced accuracy and efficiency. This article delves into a comparative analysis of traditional and AI-powered revenue cycle management (RCM) technologies, highlighting their impacts on healthcare operations.

Traditional Revenue Cycle Management: An Overview
Traditional revenue cycle management technology encompasses a series of manual processes, including patient registration, insurance verification, charge capture, claim submission, payment posting, and collections. These methods often involve:
Manual Data Entry: Leading to potential errors and inconsistencies.
Delayed Processing: Resulting in slower reimbursements and cash flow issues.
Limited Analytics: Hindering the ability to forecast and strategize effectively.
Such limitations can adversely affect the financial stability of healthcare providers, emphasizing the need for more efficient medical billing solutions.
Emergence of AI-Powered Revenue Cycle Management
AI-powered revenue cycle management technology integrates machine learning algorithms and automation to streamline billing processes. Key features include:
Automated Data Entry: Reducing human errors and expediting processing times.
Predictive Analytics: Allowing for better forecasting and decision-making.
Real-Time Monitoring: Facilitating immediate identification and resolution of issues.
These advancements in medical billing solutions enhance operational efficiency and financial performance.
Comparative Analysis: Traditional vs. AI-Powered RCM
AspectTraditional RCMAI-Powered RCMData EntryManual, error-proneAutomated, accurateProcessing TimeSlower due to manual tasksFaster through automationAnalyticsLimited capabilitiesAdvanced predictive analyticsError RateHigher due to human involvementLower with machine learningCost EfficiencyHigher operational costsReduced costs through automation
The integration of AI in revenue cycle management technology significantly enhances the efficiency and accuracy of medical billing solutions, leading to improved financial outcomes.
Benefits of AI-Powered Revenue Cycle Management
Enhanced Accuracy: AI algorithms minimize errors in billing and coding.
Improved Cash Flow: Faster processing leads to quicker reimbursements.
Resource Optimization: Automation allows staff to focus on patient care.
Scalability: AI systems can adapt to increasing workloads without compromising performance.
Compliance: Ensures adherence to regulatory standards through consistent monitoring.
These benefits underscore the transformative impact of AI on revenue cycle management technology.
Challenges in Implementing AI-Powered RCM
While AI offers numerous advantages, its implementation in medical billing solutions presents challenges:
Initial Investment: High upfront costs for technology acquisition and training.
Data Security: Ensuring patient data privacy and compliance with regulations.
Integration: Aligning new AI systems with existing infrastructure.
Addressing these challenges is crucial for the successful adoption of AI in revenue cycle management technology.
Case Studies: Real-World Applications
Several healthcare institutions have successfully transitioned to AI-powered medical billing solutions, witnessing:
Reduction in Claim Denials: Due to improved accuracy in billing.
Increased Revenue: Through efficient processing and reduced delays.
Enhanced Patient Satisfaction: As a result of streamlined billing procedures.
These case studies highlight the tangible benefits of integrating AI into revenue cycle management technology.
Future Outlook
The future of revenue cycle management technology lies in the continued integration of AI, with anticipated developments such as:
Advanced Predictive Modeling: For better financial forecasting.
Natural Language Processing: To interpret unstructured data efficiently.
Robotic Process Automation: Further reducing manual intervention.
As medical billing solutions evolve, embracing AI will be essential for healthcare providers aiming to optimize their revenue cycles.
Conclusion
The comparison between traditional and AI-powered revenue cycle management technology reveals a clear shift towards automation and efficiency. While traditional methods have served the industry for years, the integration of AI in medical billing solutions offers unparalleled advantages in accuracy, speed, and financial performance. Healthcare providers must consider these advancements to remain competitive and ensure sustainable operations.
0 notes
Text
U.S. Revenue Cycle Management Market: The Impact of Value-Based Care on Revenue Strategies
U.S. Revenue Cycle Management Industry Overview
The U.S. Revenue Cycle Management Market, valued at approximately $172.24 billion in 2024, is projected to grow at a CAGR of 10.1% from 2025 to 2030. The swiftly evolving healthcare landscape, marked by increasing digitalization, has created opportunities for the adoption of healthcare IT services, including revenue cycle management (RCM) systems. These systems aim to organize and streamline healthcare organization workflows through synchronized management software solutions. RCM solutions integrate payment models, reimbursement guidelines, codes, and interactions with third-party payers. The complexities inherent in billing and ensuring accurate payment for medical services are anticipated to drive the demand for innovative RCM solutions.
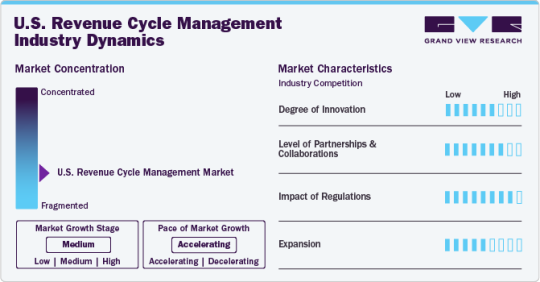
The practice of U.S. healthcare entities outsourcing RCM is gaining momentum due to its increasing advantages. The market is expected to experience substantial growth as a result of the intricate and labor-intensive nature of RCM processes, a shortage of qualified healthcare professionals, the necessity for cost-effective solutions, and the challenges presented by strict regulations, financial constraints, and staff shortages within the healthcare sector. Consequently, healthcare providers are increasingly choosing to outsource RCM tasks to specialized companies to optimize processes, decrease expenses, enhance accuracy, and prioritize patient care over administrative duties. This trend is likely to persist as providers seek efficient cash flow, cost reductions, and improved value-based care delivery.
Detailed Segmentation:
Component Insights
The software segment is anticipated to grow significantly during the forecast period, owing to a growing demand for digitalization and streamlining of operational workflows to improve patient care. The growing amount of unorganized data generated from multiple healthcare functionalities requires centralization and consolidation, which is anticipated to drive the software segment over the forecast period.
Product Insights
The integrated segment dominated the market in 2024 with a market share of over 71.84% and is anticipated to grow at the fastest rate during the forecast period. This is attributed to the constant technological advancements and rapid adoption of integrated RCM solutions by healthcare organizations. Furthermore, integrated solutions provide a synchronized and streamlined platform for financial activities with a standardized data collection and analysis process, which is expected to drive the market over the forecast period.
Delivery Mode Insights
The web-based segment dominated the market in 2024 with a market share of over 56.76%. Web-based solutions are being increasingly implemented since these solutions are to be installed off-site and do not require additional hardware or storage. Affordability and rapid deployment are some of the benefits offered by web-based solutions. athernaOne, e-Hospital Systems, Simplex HIMES, and Advanced HIMS are examples of web-based practice management solutions. The cloud-based segment is anticipated to grow at the fastest rate during the forecast period.
Specialty Insights
The cardiology segment held a significant share of 7.15% in 2024 and is expected to grow at the fastest rate during the forecast period. Cardiology treatments are expensive procedures requiring RCM services; these services help enhance the procedure's effectiveness & patient care and seamlessly manage medical billing. According to an Elsevier, Inc. paper in September 2023, approximately 6.7 million U.S. adults aged 20 years and above had heart failure, and the prevalence is projected to reach 8.5 million by 2030. The rising prevalence of cardiovascular diseases directly increases the workload burden on healthcare providers and healthcare payers, which is expected to drive the segment.
Sourcing Insights
The in-house segment dominated the market in 2024 and accounted for a revenue share of over 70.82%. The segment growth is attributed to associated benefits, such as complete control of coding operations, patient information confidentiality, and accessibility of in-house medical billers. One of the major challenges in-house RCM services face is the requirement of a large medical staff to handle the patient’s medical data. Healthcare providers need to employ trained billers and coders, which can result in backlogs if one of them is ineffective, jeopardizing the entire revenue cycle.
End-use Insights
The hospitals segment is expected to grow at the fastest rate during the forecast period. This is attributed to the growing presence of renowned and well-established hospitals in the U.S. and the rising number of patient care regulatory reforms & guidelines introduced by regulatory agencies. Hospitals are focusing on implementing innovative RCM solutions by collaborating with vendors to transform the reimbursement scenario, which is anticipated to boost segment growth. Moreover, the growing demand to optimize hospitals’ workflow to improve efficiency and productivity is expected to boost the adoption of integrated RCM systems in hospitals.
Function Insights
The claims management segment dominated the market in 2024 with a market share of over 52.78%. This is attributed to the swiftly expanding patient pool, the rising geriatric population, and the introduction of advantageous government programs related to medical insurance coverage. In addition, the adoption of risk- or value-based reimbursement models is boosting the implementation of enhanced supervision and revenue cycle prediction, particularly for high-risk & vulnerable patient groups.
Gather more insights about the market drivers, restraints, and growth of the U.S. Revenue Cycle Management Market
Key Companies & Market Share Insights
Some emerging companies in the market are Aidéo Technologies, Access Healthcare, TELCOR, CorroHealth, and others. Key players' strategies to strengthen their market presence include new product launches, partnerships & collaborations, mergers & acquisitions, and geographical expansion.
Key U.S. Revenue Cycle Management Companies:
athenahealth, Inc.
Cerner Corporation
eClinicalWorks
Epic Systems Corporation
McKesson Corporation
NXGN Management, LLC
Oncospark, Inc.
R1 RCM, Inc.
The SSI Group, Inc.
Veradigm LLC (Allscripts Healthcare LLC)
Order a free sample PDF of the Market Intelligence Study, published by Grand View Research.
Recent Developments
In January 2025, Access Healthcare received a strategic investment from New Mountain Capital, LLC. This investment is noteworthy because it originates from a reputable, growth-focused firm that manages around USD 55 billion in assets. The partnership intends to enhance Access Healthcare's capabilities and support its expansion into new markets.
In September 2024, CorroHealth, completed the acquisition of the Xtend healthcare revenue cycle management business from Navient. This strategic move is significant for several reasons, which will be explored in detail below. As part of this transaction, over 925 employees from Xtend have joined CorroHealth’s workforce. This addition not only expands CorroHealth’s team but also brings in valuable expertise that can enhance their operational capabilities.
0 notes
Text
A Comprehensive Overview of North America And Europe Medical Technology Market Landscape
North America and Europe medical technology market size is expected to reach USD 647.1 billion by 2028, according to a new report by Grand View Research, Inc. The market is expected to expand at a CAGR of 11.5% from 2021 to 2028. The growing patient population at healthcare facilities, ineffective hospital service management, rising healthcare expenditure, growing geriatric population coupled with rising prevalence of chronic diseases, increasing healthcare workforce shortage, and overburdened health systems is driving the digitalization and automation of the healthcare industry. These digital health solutions enhance patient-provider engagement and improve the quality of patient care. The improving internet connectivity and rising smartphone penetration is boosting the adoption of digital health solutions across North American and European markets.
The growing potential of the medical technology industry is attracting both public and private investors to support the development of innovative digital health solutions. The ongoing Covid-19 pandemic exposed the downfalls and shortcomings of the existing overburdened health systems and reaffirmed the need to adopt digitalization and automation of healthcare services. The laid down travel restrictions and lockdowns imposed by government bodies, restricted the patients to adopting virtual care solutions such as telemedicine and teleconsultation. Various industry participants and consultants witnessed a significant surge in adoption rates of virtual care and digital health solutions post the outbreak of the pandemic.
The market is expected to witness a boost in revenue growth over the forecast period and would follow an upward projected technology life cycle trajectory. The services segment dominated the market due to the prevailing trend of outsourcing digital health services from third-party vendors since healthcare facilities lack the required expertise and technology skillset. Rapid advancements and innovative upgradations in software solutions have contributed to the growth of the services segment. These services could vary from installations, implementation, education and training, and upgradation, and are either availed as a complete package or partially in the form of long-term contracts.
The Revenue Cycle Management (RCM) segment dominated the market owing to multiple functions of RCM such as product development, member engagement, network management, care management, claim management, and risks and compliance. The growing trend of automating the claim processing, reimbursement, denial process, and risk and compliance is driving the need for RCM solutions. The others segment dominated the market due to the growing investment in digitalization of healthcare services and to reduce rising healthcare costs. Growing awareness of smartphone healthcare solutions, medication management, and imminent healthcare are also some of the factors driving the others segment. North America dominated due to the presence of key market players, high digital literacy, advancements in IT infrastructure, rising health IT expenditure, and rapid adoption of digital health solutions.
Request Free Sample PDF of North America And Europe Medical Technology Market Size, Share, And Trends Analysis Report
North America And Europe Medical Technology Market Highlights
• The market size is expected to be valued at USD 647.1 billion by 2028, due to the digitalization and automation of the healthcare industry
• In the type segment, services dominated the market in 2020, due to the prevailing trend of outsourcing these services since healthcare organizations lack the required personnel and skill sets
• In the application segment, the revenue cycle management segment dominated the market in 2020, owing to automation of claim management, reimbursement, and risk and compliance functions
• The others segment held the largest market share in 2020 due to the growing demand to reduce diagnostic costs and reduce machine downtime
• North America dominated in 2020 due to the availability of advanced infrastructure, high digital literacy, presence of key market players, increasing health IT spending, and rapid adoption rates
North America And Europe Medical Technology Market Segmentation
Grand View Research, has segmented the North America and Europe medical technology market on the basis of type, application, end use, and region:
North America And Europe Medical Technology Type Outlook (Revenue, USD Million, 2016 - 2028)
• Hardware
• Software
• Service
North America And Europe Medical Technology Application Outlook (Revenue, USD Million, 2016 - 2028)
• Telemedicine
• Electronic Health Records
• mHealth Apps
• Revenue Cycle Management
• Enterprise Resource Planning
• Healthcare Consulting
• Wearables
North America And Europe Medical Technology End-use Outlook (Revenue, USD Million, 2016 - 2028)
• Hospitals
• Ambulatory Surgery Centers/ Clinics
• Others
North America And Europe Medical Technology Regional Outlook (Revenue, USD Million, 2016 - 2028)
• North America
o U.S.
o Canada
• Europe
o Germany
o U.K.
o France
o Italy
o Spain
o Russia
List of Key Players of North America And Europe Medical Technology Market
• Allscripts Healthcare Solutions
• eClinical Works
• Athenahealth, Inc.
• Carestream Health
• e-MDS Incorporation
• American Well
• Teladoc Health
• MDLive Inc.
• AdvancedMD Inc.
• Qualcomm Technologies Inc.
• Greenway Health LLC
• CureMD Healthcare
• DXC Technology Company
�� HealthTap Inc
• Doctor On Demand, Inc.
Order a free sample PDF of the North America And Europe Medical Technology Market Intelligence Study, published by Grand View Research.
#North America And Europe Medical Technology Market#North America And Europe Medical Technology Market Size#North America And Europe Medical Technology Market Share#North America And Europe Medical Technology Market Analysis#North America And Europe Medical Technology Market Growth
0 notes
Text
VAT in Saudi Arabia: A Quick Guide for Businesses
Value Added Tax (VAT) is a crucial part of Saudi Arabia’s tax system, impacting businesses across all sectors. Since its implementation in January 2018, VAT has undergone changes, affecting pricing, compliance, and financial management for businesses operating in the Kingdom.
With the standard VAT rate at 15%, businesses must look after registration, invoicing, reporting, and compliance requirements while strategizing VAT optimization and recovery.
This post provides an in-depth overview of VAT in Saudi Arabia, including who needs to register, key compliance obligations, penalties, and best practices to manage VAT efficiently.
What is VAT?
Value Added Tax (VAT) is a consumption tax applied at each stage of the supply chain, ultimately borne by the end consumer. Businesses collect VAT on sales (output VAT) and pay VAT on purchases (input VAT), remitting the difference to the Zakat, Tax, and Customs Authority (ZATCA).
Saudi Arabia introduced VAT as part of the Gulf Cooperation Council (GCC) VAT Agreement, an economic reform initiative to reduce reliance on oil revenue and diversify income sources.
Current VAT Rate in Saudi Arabia
Standard VAT rate: 15% (increased from 5% in July 2020)
Zero-rated supplies: 0% VAT (applies to certain exports and essential services)
Exempt supplies: No VAT charged (specific financial services, residential rental properties, etc.)
(Source: ZATCA – Saudi Arabia’s Tax Authority, 2024)
Who Needs to Register for VAT in Saudi Arabia?
1. Mandatory VAT Registration
Businesses must register for VAT if their annual taxable turnover exceeds SAR 375,000 ($100,000). This applies to:
- Local businesses selling goods or services in Saudi Arabia. - Foreign businesses providing taxable supplies within Saudi Arabia. - E-commerce businesses selling digital goods or services.
2. Voluntary VAT Registration
Businesses with annual taxable turnover between SAR 187,500 ($50,000) and SAR 375,000 ($100,000) may voluntarily register to reclaim VAT on expenses.
Exemptions from VAT Registration
- Businesses with a turnover below SAR 187,500 ($50,000). - Entities engaged only in VAT-exempt activities (like certain financial services).
- VAT Compliance & Reporting Requirements
1. VAT Invoicing
Businesses must issue tax invoices with the following details:
Supplier & buyer details (name, address, VAT number).
Invoice date & VAT rate (15% or zero-rated).
VAT amount and total price including VAT.
Invoices must be issued within 15 days of the month following a sale.
2. VAT Filing & Payment Deadlines
Businesses with annual revenue above SAR 40 million: Monthly VAT filing.
Businesses with annual revenue below SAR 40 million: Quarterly VAT filing.
VAT returns must be filed and paid within 30 days after the tax period ends.
3. VAT Record Keeping
Businesses must maintain VAT records for at least six years, including:
Tax invoices & receipts.
VAT returns filed with ZATCA.
Import/export documentation.
4. VAT Exemptions & Zero-Rated Supplies
Zero-Rated VAT (0%)
- Exports of goods & services to non-GCC countries. - International transport services (e.g., airlines). - Certain medical & educational services (as per ZATCA guidelines).
VAT-Exempt Supplies
- Financial services (e.g., interest on loans, insurance). - Residential property leases. - Local transport services.
(Source: ZATCA, 2024 VAT Guidelines)
VAT for Foreign Businesses & E-Commerce Companies
- Reverse Charge Mechanism (RCM)
Foreign businesses providing taxable services to Saudi customers must comply with the Reverse Charge Mechanism (RCM), where the recipient accounts for VAT instead of the supplier.
- VAT on Digital Services (E-Commerce VAT)
Foreign e-commerce platforms selling digital goods & services (e-books, streaming, software, etc.) must register for VAT in Saudi Arabia, even without a physical presence.
(Source: GCC VAT Framework, 2024)
Optimizing VAT Recovery
1. Claiming Input VAT Deductions
Businesses can reclaim VAT paid on business expenses, including: ✔ Rent & utilities for commercial premises. ✔ Raw materials & production costs. ✔ IT & business consulting services.
2. Avoiding VAT Leakage
✔ Ensure proper VAT invoicing to claim deductions. ✔ Conduct regular VAT audits to identify overpayments. ✔ Use automated accounting software for VAT tracking.
Why Businesses Must Stay VAT Compliant in the KSA?

Saudi Arabia takes compliance seriously and to ensure seamless business operations within the region, businesses must do the same. With Saudi Arabia’s VAT regime firmly in place, businesses must register on time to avoid penalties.
They should issue compliant tax invoices and maintain accurate records and file VAT returns & payments on time to stay compliant.
For complete and proper understanding of Saudi Arabia’s VAT landscape, it’s wise to engage in professional tax advisory and accounting services. Understanding VAT obligations ensures smooth operations, financial compliance, and cost-saving opportunities.
0 notes
Text
10 Essential Medical Billing Images: Visual Guides for Streamlining Your Practice
10 Essential Medical Billing Images: Visual Guides for Streamlining Your Practice
In the fast-paced world of healthcare, efficient medical billing is crucial for the sustainability of any practice. Utilizing visual guides can considerably streamline processes, enhance understanding, and reduce errors in billing and coding. In this article, we will explore ten essential medical billing images that can help transform your practice. whether you are a medical biller, coder, or practice manager, these visual assets will enhance your workflow and accuracy.
The importance of Visual Guides in Medical Billing
Visual guides serve as rapid references that aid in the understanding and execution of complex medical billing tasks. Here are a few reasons why visual aids are invaluable in this industry:
Enhanced Understanding: Images facilitate quicker comprehension of intricate coding processes.
Error Reduction: Visual guides can minimize mistakes by providing clear examples of correct procedures.
Training Tool: New staff members can use visuals to grasp concepts more rapidly, streamlining the onboarding process.
1. Medical Coding Process Flowchart
A flowchart illustrating the medical coding process is essential. It highlights the various stages, from patient encounter to claims submission, ensuring all steps are followed in order. this visual guide can significantly reduce errors in the billing cycle.
2. Explanation of CPT Codes
Understanding Current Procedural Terminology (CPT) codes is vital for accurate billing. An image that lists common CPT codes, along with descriptions and common uses, helps ensure coders select the correct codes for procedures.
CPT Code
Description
Common Use
99213
Established patient visit
Routine office visit
93000
Electrocardiogram
Heart health assessment
20610
Arthrocentesis
Joint aspiration
3. ICD-10 Coding Guide
providing a visual chart of common ICD-10 (International Classification of Diseases) codes is beneficial for quick reference during patient diagnosis and billing. This guide simplifies complex code structures and ensures accurate billing.
4. Patient Insurance Verification Checklist
An image showcasing a checklist for patient insurance verification can be invaluable to front-office staff.This ensures that all necessary details is collected before an appointment, reducing claim denials later.
5. Denial Management Workflow
Denial management is crucial for cash flow in medical practices. A visual guide that outlines the denial management process can help practices respond to claims denials effectively and efficiently.
6. Claims Submission Process Diagram
A diagram depicting the claims submission process helps coders and billers understand each stage,including the documentation needed for clean claims submission. This reduces the time and resources spent on resubmissions.
7. Common Billing Errors Chart
A visual chart showcasing the most common billing errors can serve as a training tool for billers. Knowing common pitfalls can lead to improved accuracy in claims submission.
8. Timely Filing Limits Reference
Each insurance company has different timely filing limits for claims.A visual guide that lists these limits for various insurers can help practices avoid late submissions and denials.
9. Electronic Health Record (EHR) Integration Tips
For practices using Electronic Health Records, an infographic illustrating tips for effective billing integration can enhance workflow and patient data management.
10. Revenue Cycle Management (RCM) Overview
A complete overview of Revenue Cycle Management visually lays out the components necessary for financial success in a healthcare setting.This guide is pivotal for understanding the financial flow within a practice.
Benefits of Using Visual Guides in Medical Billing
Incorporating visual aids into the billing process yields several advantages:
Improved Efficiency: Visuals reduce the time needed to locate information, thus speeding up billing tasks.
Training and Growth: New hires can use visual aids as a learning tool,fostering quicker adaptation.
Enhanced Communication: Visuals can bridge gaps between clinical and administrative staff, ensuring everyone is on the same page.
Practical Tips for Implementing Visual Guides
Here are a few practical tips to effectively implement these images in your medical billing practice:
Make Them Accessible: Ensure that all staff can easily access visual guides online or in physical format.
Regularly Update Content: The medical billing field changes frequently; ensure visuals reflect the latest information.
Encourage Participation: Involve staff in creating or suggesting additional visuals that can aid in their daily tasks.
Conclusion
Utilizing these 10 essential medical billing images can significantly enhance the efficiency and accuracy of your practice. Visual guides serve as powerful tools that simplify complex processes, aid in training, and reduce errors in medical billing. By integrating these images into your workflows, you not only streamline your operations but also foster a more informed and productive habitat. Make these resources a part of your practice today, and witness a transformative improvement in your medical billing processes.
youtube
https://medicalcodingandbillingclasses.net/10-essential-medical-billing-images-visual-guides-for-streamlining-your-practice/
0 notes
Text
Global Medical Billing Market Size, Growth Outlook 2035
The medical billing market Size was valued at USD 15.88 billion in 2023 and is projected to grow from USD 17.76 Billion in 2024 to USD 32.79 billion by 2032
Summary
The global medical billing market is experiencing rapid expansion due to the increasing need for streamlined revenue cycle management (RCM) in healthcare. With the growing complexity of medical billing and coding procedures, hospitals, physician offices, and diagnostic centers are turning to automated and outsourced billing solutions to optimize their administrative and financial operations. The transition from traditional paper-based billing systems to cloud-based and AI-driven solutions has significantly improved efficiency, minimized billing errors, and enhanced reimbursement processes. Additionally, government initiatives promoting electronic health records (EHRs) and digital billing solutions are further accelerating market growth. However, the market faces challenges such as data security concerns, regulatory complexities, and the high cost of implementation. Despite these obstacles, advancements in AI, blockchain, and automation are expected to drive innovation in medical billing systems, ensuring sustained market growth.
Market Overview
Medical billing is a crucial component of healthcare administration, ensuring that healthcare providers receive payments for their services from insurance companies, patients, and government healthcare programs. The market has evolved significantly, integrating automated claim processing, real-time patient billing, and AI-powered coding assistance to reduce human errors and increase operational efficiency. With the increasing burden of medical debt and insurance reimbursement challenges, healthcare organizations are investing in robust billing solutions to optimize revenue cycles. The outsourcing of medical billing services is also gaining popularity, as third-party service providers offer cost-effective solutions while ensuring compliance with evolving healthcare regulations.
Market Size and Growth Analysis
The medical billing market Size was valued at USD 15.88 billion in 2023 and is projected to grow from USD 17.76 Billion in 2024 to USD 32.79 billion by 2032, exhibiting a compound annual growth rate (CAGR) of 12.14% during the forecast period (2024 - 2032). The rise in healthcare expenditure, regulatory mandates for digital healthcare solutions, and increasing adoption of cloud-based billing platforms are key contributors to this growth.
Market Dynamics
Growth Drivers
The increasing complexity of medical billing and the need for efficient revenue cycle management solutions are primary drivers of market growth. The adoption of electronic health records (EHRs) and practice management software has streamlined billing processes, reducing administrative burdens on healthcare providers. Additionally, government regulations supporting healthcare digitization, such as the Health Insurance Portability and Accountability Act (HIPAA) in the U.S., are encouraging hospitals and clinics to implement secure and compliant billing systems. The growing trend of outsourcing medical billing services is also driving market expansion, as healthcare organizations seek cost-effective and error-free billing solutions.
Challenges and Restraints
Despite the market's rapid growth, challenges such as data security risks, regulatory compliance complexities, and high initial investment costs pose significant hurdles. Medical billing systems must adhere to stringent regulations to ensure patient data privacy and avoid legal penalties. Moreover, the lack of skilled personnel and resistance to adopting new technologies in certain regions further restrains market growth.
Regional Analysis
The North American region dominates the global medical billing market, with the United States being the key contributor due to its advanced healthcare IT infrastructure and stringent regulatory mandates for digital billing. Europe follows closely, driven by government initiatives promoting digital healthcare solutions. Asia-Pacific is expected to witness the highest growth rate, with countries such as India, China, and Japan increasingly investing in healthcare IT and billing automation. The Middle East & Africa and Latin America are gradually adopting digital billing solutions, but infrastructure challenges continue to limit rapid expansion.
Market Segmentation
By Component:
Software – Includes cloud-based and AI-driven billing platforms
Services – Outsourced billing services and consulting
By Mode of Deployment:
Cloud-based solutions – Increasingly preferred due to scalability and cost-efficiency
On-premise solutions – Offers greater security and customization options
By End-User:
Hospitals & Healthcare Providers – Major adopters of automated billing software
Diagnostic Centers & Laboratories – Require streamlined claims processing solutions
Outsourced Billing Companies – Provide end-to-end revenue cycle management services
Key Market Players
Several companies are actively shaping the medical billing landscape, including:
Accenture (US)
AGS Health (India)
TCS (India),
Cognizant Technology Solutions (US)
Genpact (US)
GeBBS Healthcare (US)
INFINIT Healthcare
Recent Developments
The medical billing market has seen notable advancements in recent years, including the integration of AI-driven coding systems, blockchain-based secure billing solutions, and real-time claim adjudication technologies. Mergers and acquisitions among key market players have strengthened the industry, enhancing technological capabilities and service offerings. Governments worldwide are also introducing new policies for medical billing transparency, further shaping the market landscape.
Future Outlook and Opportunities
The future of the medical billing market looks promising, with ongoing innovations in AI, machine learning, and automation revolutionizing revenue cycle management. The adoption of predictive analytics in billing processes is expected to reduce claim denials and improve financial performance for healthcare providers. Additionally, as telehealth and remote patient monitoring services continue to rise, the demand for digital billing solutions will further expand. However, overcoming data security risks and regulatory challenges will be crucial to ensuring sustained growth in this evolving industry.
For more information, please visit @marketresearchfuture
#Global Medical Billing Market Size#Global Medical Billing Market Share#Global Medical Billing Market Growth#Global Medical Billing Market Analysis#Global Medical Billing Market Trends#Global Medical Billing Market Forecast#Global Medical Billing Market Segments
0 notes
Text
Mastering Florida Medical Billing: Essential Tips for Streamlined Revenue Cycle Management
Mastering Florida Medical Billing: Essential Tips for Streamlined revenue Cycle Management
In the ever-evolving landscape of healthcare, efficient medical billing is crucial to the success of medical practices in Florida. The process encompasses various aspects of patient care, from scheduling appointments to receiving payment for services rendered. mastering Florida medical billing not only accelerates cash flow but also reduces denials and enhances patient satisfaction. In this article, we will explore essential tips for streamlining revenue cycle management that every medical practice should know.
Understanding the Revenue Cycle Management Process
The revenue cycle management (RCM) process involves tracking patient care events from registration to final payment. Here’s a brief overview:
Registration: Collect patient demographics and insurance data.
Eligibility Verification: Check patient insurance benefits before services.
Coding: Assign medical codes for services rendered.
Billing: Generate and submit claims to payers.
Payment Posting: Record payments received from patients and insurers.
Follow-up: Manage outstanding claims and denials.
Benefits of Streamlined Medical Billing
Effective medical billing saves time, reduces errors, and enhances cash flow. Key benefits include:
Benefit
Description
Increased Revenue
Improves collection rates and reduces days in accounts receivable.
Enhanced accuracy
Minimizes billing errors and reduces claim rejections.
Improved Patient Satisfaction
Streamlines the billing process, leading to clearer patient communications.
Time Efficiency
Automates repetitive tasks, allowing staff to focus on patient care.
Essential Tips for Mastering Florida Medical Billing
1. Stay Updated on Florida healthcare Regulations
Florida’s healthcare regulations are constantly evolving. Ensure compliance by staying informed about changes in billing codes and payer guidelines. Regular training for your billing staff is essential.
2.Leverage Technology
Investing in billing software can dramatically enhance efficiency. Consider systems that offer:
Automated coding suggestions
Claim tracking functionalities
Patient portals for easy access to billing statements
3. Implement a Robust Verification Process
prior to appointments, verify patient insurance coverage. This step helps to avoid claim denials due to eligibility issues. Utilizing Electronic Data Interchange (EDI) can facilitate real-time verification.
4. Focus on Accurate Medical Coding
Proper coding is basic in medical billing. Ensure your coding staff is well-trained in the latest ICD-10, CPT, and HCPCS codes. Consider regular audits of coding practices to maintain accuracy.
5. Optimize Claims Submission
Submit claims as soon as possible after services are rendered. Utilize batch submissions to increase efficiency, and keep detailed records of submitted claims for follow-up.
6. Monitor Accounts Receivable
Regularly review accounts receivable reports to identify trends and areas for improvement. Set clear goals for reducing days in accounts receivable and implement procedures for timely follow-ups on outstanding claims.
7.Train Staff Continuously
Provide ongoing education and training for your billing team. encourage them to stay up-to-date with coding changes, payer policies, and best practices in medical billing.
8. Foster Patient Communication
Transparent communication with patients about their billing will enhance trust.Implement clear billing statements and offer assistance regarding payment plans and financial policies.
Case Study: Success Through Streamlined billing
consider the experience of a Florida-based orthopedic practice that faced important cash flow issues due to frequent claim denials. By implementing a dedicated revenue cycle management strategy,including training staff on coding and adopting an advanced billing software system,the practice improved it’s claim acceptance rate from 75% to 95% within six months. Consequently, their average collection period decreased from 60 days to 30 days, substantially enhancing cash flow and allowing the practice to expand.
First-hand Experience in Florida Medical Billing
Having worked directly in the medical billing field for several years, I can attest to the importance of meticulous attention to detail. One of the most beneficial changes I implemented at a prior workplace was establishing a weekly review meeting for billing staff to discuss claim denials and brainstorm potential solutions. This collaborative approach fostered an habitat of accountability and continuous improvement, ultimately leading to significant reductions in follow-up time on unpaid claims.
Conclusion
Mastering Florida medical billing is essential for ensuring a smooth revenue cycle management process. By implementing the tips outlined above, including staying informed about regulatory changes, leveraging technology, and maintaining open lines of communication with patients, healthcare practices can improve their billing efficiency significantly. The ultimate goal is not just to collect payments promptly but to establish robust financial health for the practice while enhancing the patient experience. Remember, a streamlined billing process is the foundation of a thriving medical practice.
youtube
https://medicalbillingcodingcourses.net/mastering-florida-medical-billing-essential-tips-for-streamlined-revenue-cycle-management/
0 notes
Text
Opening Success in Medical Billing: Top Strategies to Maximize Revenue and Minimize Denials
Unlocking Success in Medical Billing: Top Strategies to Maximize Revenue and Minimize Denials
in the ever-evolving landscape of healthcare, maximizing revenue and minimizing denials in medical billing has become paramount for healthcare providers. With the right strategies in place, organizations can streamline processes, optimize collections, and ensure the financial health of their practice. This complete guide uncovers the top strategies for achieving success in medical billing, offering actionable insights and practical tips.
Understanding Medical Billing and Its Importance
Medical billing involves submitting and following up on claims with health insurance companies to receive payment for services rendered by healthcare providers. It is a crucial element of the revenue cycle management (RCM) process, directly impacting the financial stability of a practice.
Key Challenges in Medical Billing
Complex regulations and compliance requirements
frequent changes in insurance policies
High rates of claim denials
Data entry errors and inaccuracies
Top Strategies to Maximize Revenue in Medical billing
1. Invest in Training and Education
Providing continuous education and training for billing staff ensures they are up-to-date with the latest coding practices and compliance guidelines. Regular workshops and webinars can enhance their skills and knowledge.
2. Leverage Advanced Technology
Utilizing billing software that integrates with Electronic Health Records (EHR) can significantly reduce errors and streamline the billing process. Consider software with AI capabilities to automate repetitive tasks and improve accuracy.
3. Ensure Accurate Coding
Proper coding is essential to prevent claim denials. Implement a thorough review process to double-check codes and ensure they are aligned with the services provided. Regularly auditing claims can definitely help catch errors before submission.
4. Establish Clear Billing Policies
Clear billing policies help both staff and patients understand the financial responsibilities associated with healthcare services. Ensure that these policies are communicated effectively to avoid confusion and discontent.
5. Monitor Key Performance Indicators (KPIs)
Establish KPIs that gauge the performance of your billing processes. Key metrics to track include:
Days in Accounts Receivable (AR)
Claim denial rates
Patient collections success rates
Benefits of Optimizing Medical Billing Processes
Enhancing your medical billing process offers numerous benefits, including:
Increased cash flow
Improved patient satisfaction
Better compliance with regulations
Reduced administrative workload
Common Reasons for Claim Denials
Reason for Denial
Solution
Incorrect patient information
Validate patient ID and insurance information at check-in.
Missing prior authorization
Ensure proper verification and secure necessary authorizations.
Late filing of claims
Implement a timely filing system to track deadlines.
Inaccurate coding
Regular training and audits to ensure coding accuracy.
Case Studies: Real-World Success in Medical Billing
Case study analysis can provide a clear understanding of strategies that work. Here’s a brief overview of a healthcare provider who optimized their billing processes:
Case study: XYZ Medical Centre
XYZ Medical Center faced high denial rates and extensive days in Accounts Receivable. By investing in staff training, upgrading their billing software, and refining their coding practices, they reduced denials by 30% over the span of a year. Their accounts receivable days decreased from 60 to 30, significantly improving cash flow.
Frequently Asked Questions (FAQs)
What is the role of medical billing in healthcare?
Medical billing is essential for the reimbursement process in healthcare. It ensures that providers are compensated for their services through accurate claim submissions and follow-ups.
How can technology improve medical billing processes?
Technology streamlines billing tasks, reduces human errors, and facilitates better tracking of claims and payments. Automation tools can also enhance the speed and accuracy of the billing process.
Conclusion
Unlocking success in medical billing requires a multi-faceted approach focusing on education, technology, and process optimization. By implementing the strategies discussed in this article, healthcare providers can significantly maximize their revenue while minimizing claim denials, thereby ensuring a healthier financial ecosystem for their practice. Take the next step in transforming your medical billing processes today!
youtube
https://schoolsformedicalbilling.org/opening-success-in-medical-billing-top-strategies-to-maximize-revenue-and-minimize-denials/
0 notes
Text
Top Medical Billing Companies in NY: Streamline Your Revenue Cycle Today!
Top Medical Billing Companies in NY: Streamline Your Revenue Cycle Today!
In the healthcare industry, efficient medical billing is crucial for ensuring that healthcare providers receive timely payments for their services.As the demands of billing adn coding evolve, healthcare providers in New York are increasingly turning to specialized medical billing companies to manage their revenue cycles. This article will provide a comprehensive overview of the top medical billing companies in New York,along with practical tips for selecting the best fit for your practice.
Understanding Medical Billing and Its Importance
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for services rendered. A streamlined revenue cycle not only increases cash flow but also minimizes errors that can lead to delays in payments. Here are some key reasons why medical billing is essential:
Improved Cash flow
Reduced Administrative Costs
Enhanced Focus on Patient Care
Minimized Billing Errors
Benefits of Outsourcing Medical Billing
Outsourcing medical billing to professional companies can offer several advantages:
Expertise: Medical billing companies have expertise in the latest coding standards and reimbursement processes.
Cost-Effective: Businesses save money by avoiding hiring, training, and maintaining an in-house billing team.
Scalability: Medical billing companies can handle fluctuations in volume, ensuring that practices can focus on growth.
Technology: These companies often use advanced software solutions to streamline processes and enhance accuracy.
Top Medical Billing companies in New York
Here is a list of some of the top medical billing companies in New York that can definitely help streamline your revenue cycle:
Company name
Services Offered
Website
AdvancedMD
Medical Billing, RCM, EHR
advancedmd.com
Optimum Billing
Claims Processing, Denial Management
optimumbilling.com
MedBillingExperts
Billing Services, Coding, consulting
medbillingexperts.com
CareCloud
Revenue Cycle Management, EHR
carecloud.com
eCatalyst Healthcare Solutions
billing, Coding, Consulting
ecatalysths.com
Case Studies: Prosperous Implementation of Medical Billing Services
To understand the impact of outsourcing medical billing,let’s take a look at two case studies.
Case Study 1: A Growing Dermatology Practice
A dermatology practice in New York was struggling with billing delays, resulting in cash flow issues. By outsourcing its medical billing to a specialized firm, the practice saw a 30% increase in collections within the first six months. The billing company’s expertise in handling dermatological codes increased the accuracy of claims.
Case Study 2: Multi-Specialty Medical Group
A multi-specialty medical group was facing challenges with claim denials and slow reimbursements. After partnering with a leading medical billing company,the group experienced a 25% reduction in denial rates within three months. The company’s effective denial management strategies played a crucial role in this success.
Practical tips for Choosing a Medical Billing Company
Choosing the right medical billing company can be daunting. Here are some practical tips to help you make an informed decision:
Evaluate Experience: Look for companies with experience in your specialty to ensure they understand the specific billing codes and requirements.
check Reviews and Testimonials: Research online reviews and case studies to gauge the company’s reputation and performance.
Assess Technology: Inquire about the technology and software they use, as an efficient system can substantially impact billing accuracy.
Understand Fee Structures: Be clear on how the company charges for services; some may charge a percentage of collections, while others may have a flat fee.
Seek Communication: Ensure that the company communicates effectively and provides regular updates on your practice’s revenue cycle.
Conclusion
Streamlining your revenue cycle is essential for the financial health of any healthcare practice. By partnering with one of the top medical billing companies in NY, you can alleviate the challenges associated with billing and coding, improve your cash flow, and ultimately enhance patient care.
Remember to assess your specific needs, conduct thorough research, and choose a medical billing partner that aligns with your practice’s vision. The right company can transform your billing process and significantly boost your practiceS profitability. Start your journey towards a more efficient revenue cycle today!
youtube
https://medicalbillingcertificationprograms.org/top-medical-billing-companies-in-ny-streamline-your-revenue-cycle-today/
0 notes
Video
youtube
GSTR-9 Annual Return FY 2023 24| पूरी जानकारी एक ही वीडियो में| How to file GSTR 9| CA Devesh Thakur
📌GSTR-9 Annual Return FY 2023-24 | पूरी जानकारी एक ही वीडियो में | How to File GSTR-9
👉Welcome to cadeveshthakur ! In this comprehensive video, I explain everything you need to know about filing your GSTR-9 Annual Return for FY 2023-24. Whether you're filing online or offline, this video has got you covered with a step-by-step guide.
📌In this video, I cover:
📍How to file GSTR-9: Detailed procedures for both online and offline modes. 📍Downloading & Filling Offline Utility Form: Complete guidance on downloading the form and filling it correctly. 📍Conditions for Filing GSTR-9: Eligibility requirements and who must file. 📍Due Dates & Consequences: Important deadlines and what happens if GSTR-9 is not filed on time. 📍Important Notifications and Sections: Including Notification No. 14/2014, Section 35, and Rule 56. 📍GST Returns Overview: Understanding GSTR-3B, GSTR-1, and claiming Input Tax Credit (ITC). 📍Documents to Maintain: Outward register, export/import register, reversal of ITC, RCM, advance register, and stock register. 📍Filing GSTR-9 as NIL Return: Who is eligible and the necessary conditions. 📍Implications of a Cancelled GSTIN: Steps and considerations if your GSTIN has been canceled. ✒️💡 Don't miss out on the handwritten notes for GSTR-9! Leave your email ID in the comments, and I'll share them with you.
🔗Make sure to like, subscribe, and hit the bell icon for more insightful GST and accounting content. Feel free to drop any questions or feedback in the comments!
0 notes