#Medical coding professional
Explore tagged Tumblr posts
Note
10 for smoke and mirrors? 😼
Heatwave stares at the bags he's packed.
The room is still just as full without his stuff, which doesn't make him feel any better about this. His guardians assured him that they weren't going to replace him as soon as he left, that they're done taking in sparklings, even with the extra space now.
The thought is nice, but Heatwave doesn't believe them, because he's heard that line too many times without any evidence backing it up. Which he doesn't really hold against them, he loves everyone that lives in his home, it's just...
It's not just regular jitters- sure, this is his first time leaving home, his first time alone, of course he's going to be nervous.
But he's not nervous. He's scared.
Heatwave really should bring up the strange hallucinations he’s been having with his guardians.
His tanks will oddly cramp, he’ll see things in the corners of his optics, or his visual input will suddenly become shimmery and swirly, as he watches events play out before they do.
Now, Heatwave has heard of outliers before. He’s not stupid. But he never thought…
Yet all the signs are there. He’s able to do something no one else can, or rather, something happens to him that doesn’t happen to anyone else. He overproduces coolant and runs hotter than any other mech.
He shouldn’t tell anyone. Outliers are required to be documented by the government, and Heatwave has heard too many stories of mechs being whisked away to government facilities never to be seen again, as their abilities are exhausted while the government tries to turn them into some sort of weapon.
So no, he’s not telling anyone.
“Heatwave!”
Snapdragon’s voice floats to his audials from downstairs.
“Coming!” He shouts back, leaving his stuff laid on his berth.
The living room is the center of a rare moment of peace- the sparklings are all down for naps, while the older mechs are all out and about. He can see the twins bickering quietly in the kitchen, though.
Snapdragon is standing next to the couch, while Hard Drive, his other guardian, leans on it towards her.
They’re both tall and bulky mechs, bigger than Heatwave. He hates feeling small, but it doesn’t feel so bad when he’s next to them.
“C’mere, kiddo,” Hard Drive says, grinning with badly disguised excitement. “We gotcha somethin’!”
Snapdragon produces a little box and with a grin to match Hard Drive’s, shoves it into Heatwave’s hands. “Go on, open it!” she encourages.
He does, keeping his field tight to his frame so his guardians don’t pick up on the feeling of foreboding he can’t seem to shake.
It’s a universal translator. Heatwave’s tanks drop.
“It was a while of savin’ up,” Snapdragon starts to explain, clapping her hands together with glee. “But so worth it. Our little Heatwave’s gonna be a Rescue Bot!”
Seemingly oblivious to his inner turmoil, both Heatwave’s guardians sweep him up into a crushing hug.
Primus. I can’t tell them I don’t want to go now!
Heatwave worries his lip between his fangs, but returns the hug. “Thank you,” he murmurs.
I have to… I have to at least try.
#heatwave’s good at slipping through the cracks when it comes to medical professionals#when you have something to hide you have to be#but he also has dormant coding even he doesn’t know about#but yeah#he is very much older middle child in giant family#he just like me fr!!!!!#well my family isn’t as big as his but still#and of course he’s nervous he’s leaving home for the first time and can apparently see the future now. I wouldn’t want to leave either#it ends up being a good thing of course#but one can’t help but wonder what would’ve happened if he’d stayed#I’ll go over more what happened to Kaon and heatwave’s family in the tags of a different ask#there are actually some familiar faces in heatwave’s family#but we’ll get to them later#but I am planning on fleshing out every square inch of this universe#maccadam#transformers#transformers rescue bots#woosh answers#thanks for the ask!!#rescue bots au#tfrb heatwave#smoke and mirrors au#academy s&m ask game#ask game
27 notes
·
View notes
Text
random thing bc im watching forensic files;
when DNA samples or things like finger prints, are found at a scene. They check through the existing database of local/state prisons first, before going to the public. (however i think they hardly go asking for DNA donations to the public, unless it's for unknown remains and its to match the living family)
This is one possible reason, why a case can run cold. The existing DNA, cannot be paired with existing DNA in databases.
#any other forensic ppl who are like#more knowledge in this can correct or clarify#as i had lost my train of thought immediately and worded shit badly#except i dont know a way to word it correctly because i keep loosing my train of thought#im also not a professional#i'm gonna attempt to study it when going to collage#but im also intrested in aviation/aviation forensics#locomotive/locomotive forensics#cooking#fire science/fire fighting#EMT/Medical#and coding/computer shit#why are the tags separated i hate tumblr tags somtimes oml#shadow gens rambling#-Illusion Steve/Digital | 🌀🟦
4 notes
·
View notes
Text
Me: *Trying to go about my day like a normal person *
My brain: “What if we made a TADC OC that’s basically a slime monster girl, but she’s based on the kind of toy slime that has a bunch of cutesy objects in it?? And when she was a human she was a highly skilled and respected Intensivist working at an ICU?? And as a doctor, she was known for being gentle and compassionate to all her patients, and she treasured the staff members working under he?? And she saw all her staff as members of her family, and was fiercely protective of them?? But also while she always appeared extremely confident and well put together, deep inside she struggled daily with a massive inferiority complex and imposter syndrome?? Because she never believed she deserved any of the praise she received despite her work, and constantly felt the need to prove herself by going above and beyond in her work?? And all the plays into why she’s a slime girl now, because even though she always appeared as strong and confident in the surface, inside she’s soft and anxious??
And while she doesn’t remember her life prior to entering the Digital World, during times of crisis or when someone’s injured or at high risk of abstracting, suddenly doctor mode activates?? She quite literally pulls herself together and becomes completely solid like plastic, and gives off a strong aura of confidence and authority?? Thoughts, terminology, and emotions that are foreign yet seem SO familiar surge through her, and without really thinking about it she talking and acting just like she did as an ICU doctor; leading her to quickly take control of the situation with firm confidence before gently tending to the injured/abstracting individual. She doesn’t understand how she knows any of what she’s saying as she gently tends to, and or talks the individual back down from the edge, but it feels so natural to her! It’s like she was MADE to do this, and had actually done it many times before despite having no recollection of doing anything like this previously?? And as she slowly helps the individual ground themselves in reality once more, she’s still maintaining a perfect composure during the whole ordeal, not once showing just how afraid she really was and instead just remaining laser focused on helping the “patient” in front of her??
And it’s only when her “patient” has finally stabilized somewhat that she finally notices everyone staring at her in awe, and then she starts barking orders to everyone to get the “patient” back to their room so they can be admitted into the hospital for surveillance, and that she wants a full blood panel and PHQ-9 assessment completed while she fills out an incident report for the hospital’s records. And everyone is so taken aback/still in shock that they just kinda go along with it because she sounds so sure of herself no one knows how to argue otherwise.
It’s only when someone breaks out of their stupor enough to ask her how she did all that/what the heck happened that she snaps out of it, and she softens into her goopy self again as she tries to clumsily explain she has no clue what happened but was just overwhelmed by these sudden thoughts and emotions, and despite not knowing where any of it was coming from it felt like she just instinctively knew what to do and how to do it.
Someone points out to her that she looked and sounded just like a doctor back there, and that maybe that’s who she was prior to entering the Digital Circus. She doesn’t believe it, insisting that there’s no way someone like her could be a doctor, but everyone insists that she absolutely could be and that what she did was incredible?? And now she’s kinda the unofficial doctor of the circus despite still not believing she was, or could ever be, a doctor??”
Me: *Sitting on the couch letting my brain hyperfixate* 👁️👄👁️
#this…this ended up being WAY longer than i intended#but my brain has literally been CONSUMED by this idea#that trope of ‘amnesiac somehow instinctively knows how to do the the thing because they did it previously’ is a fav of mine#she might not remember her old life but the caregiver instincts and knowledge is still very much ingrained into her#and it comes out full force when someone is in need of medical attention#she orders caine to go prepare a hospital bed and he’s like ‘yes ma’am!’ before taking off to do that#he makes it 2/3s down the hall before realizing what just happened and poofing back#in his defense she was so confident and authoritative his coding went ‘ah a doctor. you should always listen to medical professional.’#shitpost#tadc#long post#the amazing digital circus#tadc oc#haven’t quite figured out a name for her yet#but i’m tryna name her in a way that would allow the nickname ‘squish’ to be acceptable#because squish as a nickname for a slime lady makes me laugh
14 notes
·
View notes
Text
idk if I have any people following me who make a living on their art alone, but if you have any tax and legal tips (e.g. what's one thing you wish you knew before you started?), I am all ears
#fine art#sole proprietorship#professional artist#artrepreneur#entrepreneur#I live in Texas so I won't have state income tax but I will have sales tax#for which I'll need a permit#idk if there are other taxes to which artists are usually subject that TX forgoes#x#my long-term goal is to be making the median income of the area in which I live by 2030#(not to name numbers but let's just say I'm a pauper in a princess town)#my immediate goal is to pay for my medical needs ~ so I have no choice but to be serious about it#and my biggest fear is running into unforeseen financial barriers or violating some obscure legal code that brings it all tumbling down#bc I obviously can't afford any advisors rn
4 notes
·
View notes
Text
Medical Billing Services in Charleston, South Carolina (SC) - 24/7 Medical Billing Services
Leading Medical Billing Services provider in Charleston, South Carolina (SC). 12+ years of expert Medical Billing Services. Call 888-502-0537 now!
#Medical Billing Charleston#Medical Billing and Coding Charleston#Medical Billing Company Charleston#Medical Billing Services Charleston#top Medical Billing Services Charleston#Leading Medical Billing Services Charleston#Medical Billing Agency Charleston#Top Medical Billing Agency Charleston#Top Medical Billing Specialist Company Charleston#Medical Billing Management company Charleston#Best Medical Billing service Company Charleston#Professional Medical Billing Company Charleston#Cheap Medical Billing Company Charleston#Cheap Medical Billing services provider Charleston#Cheap Medical Billing services Specialists#Outsourcing Medical Billing Charleston#Top Outsourcing Medical Billing Charleston#Best Outsourcing Medical Billing Charleston#Outsourcing Medical Billing Services Charleston#Medical Billing Services provider Charleston#Best Medical Billing Service Experts Charleston#Medical Billing Company Experts Charleston#Best Medical Billing Company Experts Charleston#Professional Medical Billing Company#Outsourcing Medical Billing#Top Medical Billing Company Charleston#remote Medical billing Charleston#Medical Billing#Medical Coding#Medical Coding Charleston
0 notes
Text
How a Medical Coding Institute Can Propel Your Career in Healthcare
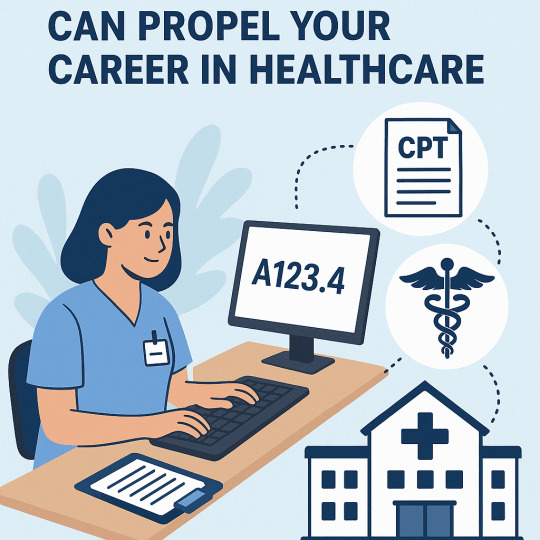
In the ever-evolving world of healthcare, the demand for skilled professionals who can manage and interpret complex medical data has skyrocketed. Among the most sought-after careers is medical coding, a vital function that connects healthcare services with accurate billing and insurance processes. If you're considering a rewarding and future-proof career path, enrolling in a Medical Coding Institute can be your first powerful step. But what makes medical coding such a promising option, and how does a reputable institute prepare you for this role?
In this blog, we’ll explore the growing importance of medical coding, the benefits of enrolling in a specialised institute, and how this career can open up a world of opportunities in the healthcare industry.
What Is Medical Coding?
Medical coding is the process of translating healthcare diagnoses, procedures, medical services, and equipment into standardised alphanumeric codes. These codes are derived from various classification systems such as ICD (International Classification of Diseases), CPT (Current Procedural Terminology), and HCPCS (Healthcare Common Procedure Coding System). They are essential for medical billing and ensuring healthcare providers are reimbursed accurately and efficiently by insurance companies.
A certified medical coder must have a keen eye for detail, comprehensive knowledge of medical terminology, and a strong understanding of anatomy and physiology. This is where a Medical Coding Institute plays a crucial role.
The Growing Demand for Medical Coders
The healthcare sector is expanding rapidly, and with it, the need for accurate documentation and billing. Governments and insurance companies are enforcing stricter compliance regulations, making skilled medical coders indispensable.
According to labour market projections, employment for medical records and health information technicians, including medical coders, is expected to grow faster than average in the coming years. With the rise of telemedicine, electronic health records (EHRs), and data-driven healthcare, this demand is only set to increase.
Why Choose a Medical Coding Institute?
A Medical Coding Institute offers specialised training that equips students with the technical knowledge and hands-on experience required to thrive in the industry. Here are several compelling reasons to pursue your training through a dedicated institute:
1. Structured Curriculum
Medical coding isn’t something you can learn casually. A professional institute offers a well-structured curriculum that covers all essential areas, such as:
Anatomy and physiology
Medical terminology
Coding systems (ICD, CPT, HCPCS)
Healthcare laws and regulations
Ethical practices in coding
2. Hands-on Training
A good institute doesn't just focus on theory. Practical training, coding simulations, and real-world case studies help students understand how to apply code accurately in clinical scenarios.
3. Preparation for Certification Exams
Most healthcare employers prefer or require certified coders. Reputable institutes prepare students for industry-recognised certification exams, increasing their employability and salary prospects.
4. Expert Instructors
Learning from experienced instructors with a background in healthcare and coding ensures students gain insights from real-world challenges and best practices.
5. Placement Assistance
Many institutes offer job placement support through career counselling, resume-building workshops, and partnerships with healthcare providers.
Career Opportunities After Medical Coding Training
Graduating from a Medical Coding Institute opens the door to various career paths in the healthcare sector. Some of the job roles you can pursue include:
Medical Coder: Assign accurate codes to procedures and diagnoses.
Medical Billing Specialist: Process and submit claims to insurance companies.
Health Information Technician: Manage and analyse patient data.
Compliance Auditor: Ensure that healthcare providers meet regulatory standards.
Clinical Data Analyst: Interpret medical data for research and improvement of healthcare services.
These roles can be found in a variety of settings, including hospitals, clinics, insurance companies, and third-party billing organisations. Some roles also offer remote working opportunities, making it an ideal career for those seeking flexibility.
Benefits of a Career in Medical Coding
Opting for a career in medical coding through a specialised institute brings numerous advantages:
Job Stability: The healthcare industry is recession-resistant, offering consistent demand for coding professionals.
Attractive Salary: Certified coders often enjoy competitive salaries with room for advancement.
Career Progression: With experience and further certifications, professionals can move into auditing, consulting, or management roles.
Work-Life Balance: Many coding positions offer standard working hours or remote options.
Choosing the Right Medical Coding Institute
When selecting a Medical Coding Institute, consider the following:
Accreditation: Ensure the institute is recognised by relevant educational or healthcare authorities.
Curriculum: The program should align with industry standards and prepare you for certification.
Faculty: Look for experienced instructors with healthcare or coding backgrounds.
Reviews and Testimonials: Check student feedback to gauge the quality of training and support.
Career Services: Strong placement support can significantly enhance your job prospects post-training.
Final Thoughts
Medical coding is more than just a clerical job—it's a critical function in the healthcare system that ensures proper patient care documentation and accurate financial reimbursement. As the healthcare industry grows, so does the need for skilled coders. A Medical Coding Institute provides you with the knowledge, training, and credentials necessary to succeed in this dynamic field.
Whether you're a recent graduate, a professional looking to switch careers, or someone seeking a stable, rewarding job, medical coding could be the path forward. With the right training, your future in healthcare is not just possible—it’s promising.
#Cigma Medical Coding Academy#Transcription Courses in Kochi#Medical Coding Courses in Kochi#Medical Billing Courses in Kochi#Billing Certificate Program in Kochi#Medical Coding Certificate Program in Kerala#Transcription Certificate Program in Kochi#Medical Coding Academy#Australian Clinical Coding Training#Certificate Program in Medical Billing Kerala#Certificate Program in Medical Transcription Kochi#Medical Transcription Course Kochi#Medical Coding Institute#Best Medical Coding Institute in Kerala#Medical Coding Course in Kerala#Best medical coding academy in Kerala#Medical Coding Auditing training in Kochi#AM coding training in Kochi#Clinical Coding training Kerala#Dental Coding training India#Health information Management courses in Kerala#Saudi Coding training in Kerala#Post graduate program in Health information management in Kochi#CPMA Training in Kerala#Medical coding Training Kerala#Professional Medical Coding Courses in Kerala#medical coding programs in Kochi#medical coding certification courses Kerala#AAPC institute of Medical Coding Kochi#Transcription Courses in Mangalore
0 notes
Text
Mastering Domain II of the RHIT Exam: Access, Disclosure, Privacy, and Security
Mastering Domain II of the RHIT Exam: Access, Disclosure, Privacy, and Security
Earning your Registered Health Information Technician (RHIT) credential is a big achievement. It shows you have the knowledge and skills to handle health information with care; making sure it’s accurate, secure, and confidential. One of the most important parts of the RHIT exam is Domain II: Access, Disclosure, Privacy, and Security. In today’s healthcare world, where so much information is stored digitally and privacy rules are more complex than ever, this domain tests not just what you know but how well you can apply it to real situations.
What Is Domain II?
Domain II is all about understanding how health information is accessed, shared, and protected. It covers the laws, policies, and procedures designed to keep patient information safe while making sure the right people can access it when needed. This includes important topics like HIPAA regulations, how to properly release information, ways to protect data, how to respond if there’s a breach, and how to ethically handle sensitive patient information (Sayles, 2020).
In today’s world of electronic health records (EHRs), telehealth services, and health data sharing across systems, keeping information secure and private is more important than ever. Mistakes or breaches can put patient trust at risk and even lead to legal trouble. That’s why Domain II is designed to make sure you’re ready to protect patient information in both paper and electronic formats, no matter where you work (Sayles, 2020).
Key Focus Areas
1. Legal and Regulatory Requirements
Understanding the laws around health information is the foundation of this domain. You’ll need to know the ins and outs of HIPAA, especially the Privacy and Security Rules, which govern how protected health information (PHI) can be used and shared. The HITECH Act also plays a big role, expanding HIPAA’s reach and adding breach notification rules. Since state laws sometimes have stricter privacy requirements than federal ones, you’ll also need to know how to handle those differences. And don’t forget patient rights patients have the right to see, amend, or limit access to their health records. Finally, you should understand how to deal with legal requests like subpoenas or court orders properly (Sayles, 2020).
2. Access and Disclosure Policies
This section covers how you control who gets to see health information and under what conditions. You’ll learn when patient authorization is necessary and how to document it correctly. You’ll also need to understand the Release of Information (ROI) process, knowing who can receive information and how to track those requests carefully. The Minimum Necessary Standard is key here; it means only sharing the smallest amount of information needed for a specific purpose, reducing unnecessary exposure. Special care is needed when dealing with sensitive records like mental health, substance abuse, reproductive health, or HIV/AIDS data, as these often require extra protection (Sayles, 2020).
3. Health Information Security
Protecting health data isn’t just about rules it’s also about putting the right safeguards in place. This part dives into administrative safeguards like policies and procedures that show how an organization follows HIPAA’s security requirements. You’ll also study technical safeguards such as passwords, role-based access controls, audit logs, and encryption, tools that keep electronic health records secure. Physical safeguards are just as important; these include things like controlling who can enter facilities, securing workstations, and properly disposing of paper records. Regular security training helps staff stay aware of risks and best practices, reducing mistakes that could lead to breaches. Finally, you’ll learn how to handle incidents like data breaches, including how to report and respond to them quickly and effectively (Sayles, 2020).
4. Data Integrity and Confidentiality
Keeping records accurate and trustworthy throughout their lifecycle is essential. You’ll explore how to handle amendments and changes in a way that maintains data integrity. Regular data audits help spot unauthorized access and keep things transparent. Strong confidentiality policies ensure only authorized personnel can access PHI, and conducting risk assessments helps identify weak points and plan for better protection (Sayles, 2020).
5. Professional Ethics and Responsibilities
Being an HIM professional means more than just following rules, it means living up to high ethical standards guided by the AHIMA Code of Ethics. This code highlights the importance of advocating for patients, protecting their rights and dignity every step of the way. It also stresses honesty and integrity you should never do anything that might compromise the confidentiality or accuracy of patient information. Good professional judgment is crucial, especially when facing tough or unclear situations. And finally, managing conflicts of interest means making sure your personal or financial interests never get in the way of your professional responsibilities (Sayles, 2020).
Tips for Studying Domain II
Mastering Domain II isn’t just about memorizing facts it’s about thinking like a compliance officer, a privacy advocate, and a leader in health information management. Here are some tips to help you prepare:
Use case-based learning: Work through real-life scenarios, like handling information requests from family members or law enforcement, to see how the rules apply in practice.
Create flowcharts: Visualize complex processes such as release of information, breach response steps, or who can access different levels of PHI.
Take practice exams regularly: This will sharpen your recall and help you develop the reasoning skills needed for tricky questions.
Stay current: HIPAA and healthcare privacy laws evolve, especially with the rise of telehealth and new security threats. Keep up with changes so your knowledge stays fresh and relevant
Final Thoughts
Mastering Domain II of the RHIT exam is about more than passing a test it’s about becoming a trusted guardian of patient privacy and health data security. When you’re well-trained, aware, and ethical, you help build a safer, more effective healthcare system for everyone.
Remember, every policy you learn and every scenario you practice impacts real people. Patients count on professionals like you to handle their information with care, competence, and respect. Take that responsibility seriously, and you’ll be well on your way to success not just on the exam, but in your career as a Health Information Technician.
References
American Health Information Management Association. (2023). RHIT certification exam content outline. AHIMA. https://www.ahima.org/media/x3opwug4/rhit_contentoutline_09_2023_final-1.pdf
Sayles, W. L. (2020). Health information management technology: An applied approach (5th ed.). Elsevier.
#RHIT exam#health information management#HIM study#HIPAA#HIM student#HIT career#medical coding#data privacy#healthcare compliance#health IT#studyblr#exam prep#study tips#future RHIT#digital health#release of information#patient privacy#HIM professional#career in healthcare#AHIMA
0 notes
Text
Understanding the Foundation of DRGs: A Guide for Smarter Medical Billing

Understanding the Foundation of DRGs: A Guide for Smarter Medical Billing
Imagine two patients walking into different hospitals — one in New York City and another in a small rural town in Texas. Both have the same condition, i.e., a broken hip.
Despite being treated in entirely different locations, with different staff and facilities, the hospital receives a fixed payment for each patient’s care. No breakdown of every X-ray, painkiller, or overnight stay, just one bundled payment for the whole case.
Sounds simple, right?
But behind that single payment is a complex system that is quietly reshaping how hospitals operate, doctors document care, and insurers reimburse providers. That system is called DRG-based billing which has changed hospital payments from long lists of individual charges to a more streamlined, diagnosis-based payment.
In this blog, we will understand about the foundation of DRGs as an important factor for offshore medical billing and coding services in India.
What are DRG-Based Payments?
Diagnostic-Related Groups (DRGs) are a technique mainly used by Medicare to reimburse hospitals for inpatient care services. Rather than getting billed for each individual supply or service, DRGs provide a set payment for each diagnosis, treatment plan, and applicable clinical factors of the patient. This model simplifies billing and encourages more cost-effective care.
Benefits of the DRG System
Introduced in 1982 by the Centers for Medicare and Medicaid Services, DRGs replaced the previously used cost-based reimbursement system. In this earlier model, hospitals were reimbursed for the actual cost of providing care, often resulting in higher healthcare costs. The DRG model aimed to control these costs while maintaining quality care. The following are the benefits of DRG-based payments:
Fair Reimbursement: A standardized rate ensures that treatment for the same condition receives consistent payment across hospitals (with local cost adjustments).
Reduced Administrative Burden: DRGs eliminate the need for itemized bills, making documentation and offshore medical billing and coding services in India more efficient.
Efficiency and Quality of Care: Since payment is fixed, hospitals are encouraged to avoid unnecessary testing or prolonged hospital stays.
Different Types of DRG
Outsourcing medical billing and coding services providers in India and healthcare providers needs to be aware for the following DRGs types to ensure accurate billing and coding:
1. Pediatric DRGs
Pediatric DRGs are meant exclusively for children and deal with children’s specific diagnostic and treatment patterns prevalent in pediatric medicine. These groupings help adjust payments to reflect the specialized care children often require.
2. Surgical DRGs
Surgical DRGs categorize patients as per the clinical procedures they undergo during their stay in the hospital. These categories assure that the complexity and expense of surgical procedures are accurately accounted for in reimbursement.
3. Major Diagnostic Category (MDC) DRGs
These DRGs classify patients into wide categories of diagnoses that correspond to particular organ systems or medical specialties. MDCs form the underlying framework for DRG classification, grouping patients with related conditions and anticipated similar healthcare resources.
4. Condition-Specific DRGs
These DRG codes are specifically designed for clinical conditions, such as mental disorders, HIV/AIDS, or severe trauma. Such specialized categories allow hospitals to receive appropriate reimbursement for handling cases that are too complex and resource-intensive.
5. Transfer DRGs
These DRGs are applied if a patient is transferred from one facility to another for further treatment. As the full course of treatment is split between facilities, Transfer DRGs adjust payments to reflect the shared responsibility and cost.
How do DRGs Work in Medical Billing?
DRGs form the backbone of inpatient billing under Medicare and many other healthcare systems. Instead of billing separately for every test, treatment, or day of stay, DRGs offer a payment model that bundles services and standardizes and simplifies reimbursement. Here is how the process works:
1. Categorizing the Patient
Each inpatient hospital admission is given a unique DRG code. This classification is based on several factors:
Primary diagnosis
Procedures performed
Patient’s age and sex
Presence of complications or comorbidities
Hospitals assign each individual to one of more than 700 distinct DRGs, with the aim of grouping together similar cases into similar groups clinically and expected to require similar levels of hospital resources.
2. Setting the Payment Amount
Once the DRG code is assigned, it automatically establishes the bundled payment that will be paid to the hospital for the case. This payment is fixed, no matter how long the patient remains or how many services are rendered. However, several adjustments are applied to ensure fairness:
Geographic adjustments: Hospitals in high-cost areas (like major cities) receive higher payments than rural facilities.
Hospital characteristics: Teaching hospitals or facilities that handle especially complex cases may receive additional compensation.
Case complexity: If the patient has serious comorbidities (e.g., diabetes or heart failure), the payment increases to account for the extra care required.
3. The Efficiency Game
Since the payment is fixed for every DRG, hospitals have financial incentives to treat patients in a diligent manner. The ultimate aim is to provide quality care without unnecessary delays, tests, or longer hospital stays. This results in less avoidable readmission, quicker coordinated care, and the transition from volume-based to value-based care.
For instance, two patients with pneumonia may differ in the duration of stay, but as long as they are classified under the same DRG, the hospital gets the same reimbursement. Thus, it is encouraged that hospitals optimize care pathways and eliminate wastage but keep clinical outcomes in check.
Challenges in DRG-Based Hospital Billing
Though the DRG system has made hospital billing and reimbursement easier, it also poses a number of issues that healthcare providers have to closely monitor. One of the biggest obstacles is coding accuracy. Incomplete or inaccurate coding can result in denied claims or decreased payments, consequently impacting a hospital’s financial performance and revenue directly.
Another key determinant is the Case Mix Index (CMI), a measure that indicates the case complexity treated by a hospital. A better CMI generally leads to higher reimbursements. However, achieving an accurate CMI depends entirely on precise and thorough clinical documentation. If not, the hospitals might end up being underpaid for the care they offer.
Regulatory compliance is also a significant concern. Hospitals have strict Medicare and insurance regulations to follow when assigning DRG codes. Non-compliance can lead to audits, fines, or repayment requests. Also, hospitals have to deal with the issue of resource allocation during the provision of high-quality care within the budget constraint of fixed DRG payments. This calls for meticulous planning, optimal workflows, and continuous monitoring of patient outcomes.
The Role of ICS in Supporting Physicians
Outsourcing medical billing and coding services providers in India such as Info Hub Consultancy Services (ICS) play a vital role in supporting hospitals and physicians. These experts transform physicians’ documentation into accurate DRG codes that reflect the delivered care. Apart from ensuring appropriate reimbursement, this also reduces errors that may result in delays or denials.
Additionally, coders ensure that all the details, including complications and secondary diagnoses, are accurately documented by thoroughly examining medical records, thus preventing underpayment. They also update themselves with changing Medicare policies and insurance rules to enable healthcare providers to remain compliant and avoid fines.
Moreover, ICS serve as guardians of financial health within the hospital system. With assistance from professional offshore medical billing and coding services in India, physicians can be confident that the billing side of their practice is handled with precision and expertise.
#Medical Billing Services Agency#Best Medical Billing Agency#Offshore Medical Billing and coding#Offshore Medical Billing Services India#Offshore Medical Billing Agency India#Best Offshore Medical Billing Company India#Offshore Medical Billing Company In India#Outsource Medical Billing Services Agency India#Best Outsource Medical Billing Agency India#1 Outsource Medical Billing Services Company India#Professional Medical Billing Services Agency India#Outsourcing Medical Billing Services India#Medical Billing and Coding Company#Outsourcing Medical Billing and Coding
0 notes
Text
Explore the World of Medical Billing: A Rewarding Career
Embarking on a career in medical billing and coding can be a rewarding choice, offering stability, competitive compensation, and flexible work arrangements. As a critical bridge between healthcare providers and insurance companies, this field ensures proper reimbursement for medical services. According to the U.S. Bureau of Labor Statistics, coding jobs are expected to increase by 9% by 2033,…
#Billing software#Certification in medical billing#Coding and billing#Healthcare administration#Healthcare industry trends#Insurance claims processing#Medical billing career#Professional development#Revenue cycle management
0 notes
Text
youtube
What is CPC? | Certified Professional Coder Explained
Discover what CPC (Certified Professional Coder) is and how it plays a vital role in the healthcare industry. Learn about CPC certification, medical coding requirements, job opportunities, and how to become a certified coder. Get insights into CPC exam preparation and career growth in medical coding. Hashtags: #CPC #CertifiedProfessionalCoder #MedicalCoding #CPCExam #MedicalCodingCareer #HealthcareJobs #CPCCertification
#certified professional coder#certified coder#certified medical coder#medical coder#certified professional coder training#certified professional coder salary#certified professional medical coder#guide to certified professional coder#how to become a certified professional medical coder#what is medical coding#certified professional coder exam#how to become a medical coder#tip certified medical coder#the american academy of professional coders#certified coder exam#Youtube
0 notes
Text
The funny psychological horror circus show has a fucking death grip on me, so it’S OC TIME BOIIIIII!!!
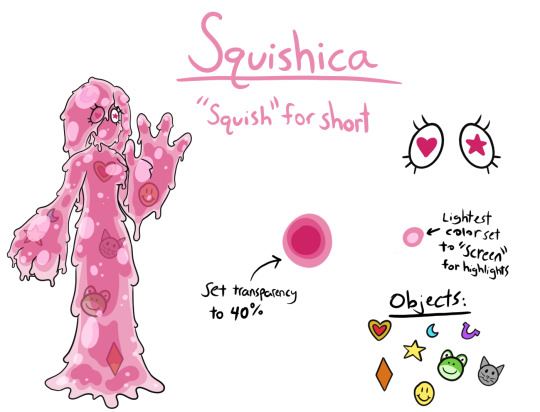
I made a whole ramble/shitpost about her earlier, but basically she’s a sweet slime girl with an inferiority complex and imposter syndrome.
Prior to entering the digital circus, Squishica was a 32 year old Intensivist at an ICU. She was confident and could be intimidating, but she treated each of her patients with kindness and warmth. She was very close with her staff members, they were like family to her as far as she was concerned, and she was fiercely protective of them all.
Despite always appearing strong and confident though, deep down Squishica struggled with feelings of inadequacy. Despite the praise and admiration she received, Squishica never felt like she deserved any of it. To her, there was ALWAYS something she could’ve done better, something that she could’ve done differently. She felt like a fraud because everyone treated her like she was perfect, but she wasn’t and it made her feel like she was deceiving everyone. She tried to combat this by always going above and beyond in her work, believing that she would only be worthy of praise if she could truly be perfect. Squish never allowed these insecurities and feelings to show, and successfully maintained the facade of a strong and confident doctor.
Upon entering the Digital Circus however, she no longer remembers her past life. Finally allowing for her “real” self, the goopy and anxious mess she always hid from everyone, to be on full display. Hence why I specifically made her slime lol
Squishica is kind and sweet to everyone, and she goes out of her way to help wherever she can but it’s often accompanied by self depreciating comments about how she’s “sorry for being a bother” or she “knows that she could’ve done better”. Poor thing just no self esteem whatsoever, but still wants to be helpful.
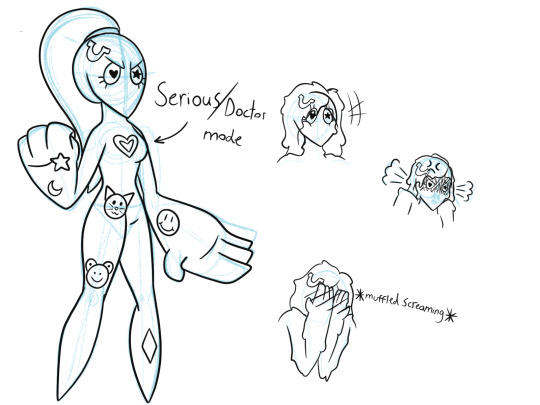
However when some kind of medical emergency happens, IE someone starts abstracting, she does a full 180 personality wise. All these thoughts, terminology, and feelings from her time as an ICU doctor come crashing over her. She doesn’t understand what any of it is, but suddenly she feels so calm and sure of herself, like she’s done this before and knows with certainty what needs to be done. She quite LITERALLY hardens up, and suddenly she’s the strong and commanding ICU doctor she was as a human. She quickly takes control of the situation, and immediately gets to work talking her “patient” down from the edge. She’s cool and composed, but kind and gentle as she slowly helps her “patient” stabilize. As she’s doing this, she’s COMPLETELY oblivious to the stunned awe of the rest of the crew as they watch her save someone from something they had only ever known to be impossible to come back from, all she’s focused on is her “patient” in front of her.
It’s only when her “patient” is somewhat stabilized that Squish notices everyone staring at her. Instead of commenting however, she starts barking orders at everyone like “Ragatha and Gangle, go make sure we have a hospital bed prepared for (blank); I want them admitted to the hospital for continued surveillance until further notice. Jax and Kinger, assist (blank) back to their room and help get them situated in bed prior to admission; but go slowly, we can’t risk exacerbating their condition by moving too quickly! Zooble, while (blank) is getting settled I want bloodwork done for their thyroid, liver, and kidney function. I’m most concerned about their thyroid function right now, so if the hormone levels are off, ping Dr. Drayden in endocrinology STAT! Pomni, I need a full set of vitals on (blank); please send those to me as soon as you’ve obtained them and start work on documentation a full recount of everything that happened. I will need that recount of the event to fill out necessary paperwork for the hospital. Caine, (blank) is in fragile condition right now and they could easily nosedive again; I need you to accompany (blank) back to their bed and keep watch over them as they’re being admitted. If the patient shows ANY signs of possible relapse, call a code blue IMMEDIATELY!”
She speaks with such authority and confidence, no one even stops to question her; instead everyone starts scurrying around and following her orders. It’s only when Zooble pauses for a moment while trying to locate needles and is like “Wait…We don’t even HAVE blood, do we??” That everyone recognizes what they’re doing and stops. Except for Kinger,Jax, and Caine because (blank) really did need to be taken back to their room and couldn’t be left alone.
Upon being confronted about what the heck just happened, Squish finally snaps out of it and softens back into her soft goopy self. She timidly explains that she has no clue what came over her or how she even knew any of what she was saying or doing, but it was like she somehow instinctively knew what to do.
Ragatha points out that Squish looked and sounded like a real doctor and Pomni chimes in that Squish might’ve been a doctor before coming here, to which everyone agrees is the likely scenario given how easily she handled everything. Squish on the other hand nearly melts into a puddle insisting there’s no way that could possibly be true, she’s so passive and weak! How could SHE have all people have been a doctor?? It’s just not possible!
Nevertheless she’s now the unofficial “doctor” of the circus, despite her protests that wouldn’t be able to do it, her old instincts have kicked in several times since then and each time it happens she’s just a LITTLE more convinced that maybe, JUST maybe, she really WAS a doctor and that she CAN do this.
She often gets called “Doc” or “Dr. Squish” lol.
Here are some bonus doodles for your amusement.
#tadc#the amazing digital circus#tadc oc#my art#digital art#tadc squishica#jax primarily calls her doc after that whole event#the best part is after everything was over pomni looks at caine like ‘why did you do what she said?? you’re in charge here??’#and caine deadass like ‘well she sounded so certain in her orders that it didn’t occur to me that saying no was an option’#his coding basically made him go ‘oh there’s a doctor here. we must listen to them because they are the medical professional here.’#but also if the normally shy and meek lady now looks like a military officer and is handing out order you do what she says#because she honestly might kill you if you don’t lmao
10 notes
·
View notes
Text
Best Medical Coding Training Institutes in Andhra Pradesh, Karnataka, and Hyderabad
Introduction:
Medical coding is a critical field in healthcare that helps ensure accurate billing and compliance with regulations. As the healthcare industry continues to grow, there is an increasing demand for skilled professionals who can navigate the complexities of medical coding. Choosing the right training institute is essential for gaining the necessary knowledge and certification. In this article, we will explore the best medical coding training institutes in Andhra Pradesh, online medical coding training in Karnataka, and the certified professional coder course in Hyderabad to help you make an informed decision about your career in medical coding.
Best Medical Coding Training Institutes in Andhra Pradesh:
When it comes to medical coding training in Andhra Pradesh, several institutes stand out due to their comprehensive curriculum, experienced trainers, and successful placement records. The best medical coding training institute in Andhra Pradesh offers a structured program that covers various coding systems such as ICD-10, CPT, and HCPCS. These institutes focus on practical knowledge, ensuring that students are well-prepared for the challenges of the medical coding profession.
Additionally, top institutes provide certification preparation for coding exams, which are crucial for gaining professional recognition. The training programs are designed to meet the needs of both beginners and experienced professionals looking to enhance their skills.
Online Medical Coding Training in Karnataka:
For those in Karnataka or those seeking flexible learning options, online medical coding training in Karnataka is an excellent choice. Online courses provide the convenience of studying at your own pace while receiving high-quality instruction. Many institutes offer live sessions, recorded lectures, and interactive assignments to ensure a comprehensive understanding of medical coding.
Online training programs often cater to students across various states, offering opportunities to pursue certification as a Certified Professional Coder (CPC) without the need to attend in-person classes. This flexibility makes it ideal for those balancing work and study commitments.
Certified Professional Coder Course in Hyderabad:
For individuals seeking certification, the certified professional coder course in Hyderabad is a popular option. These courses prepare students for the Certified Professional Coder (CPC) exam, which is recognized globally and opens doors to career opportunities in medical coding. The training in Hyderabad is highly regarded for its practical approach and expert instructors who guide students through the essential aspects of medical coding.
Whether you're a recent graduate or someone looking to switch careers, enrolling in a certified professional coder course in Hyderabad provides you with the knowledge and credentials needed to excel in the industry.
Conclusion:
Medical coding offers a rewarding career with a high demand for skilled professionals. Choosing the right training program is crucial to ensuring success in this field. By enrolling in the best medical coding training institute in Andhra Pradesh, opting for online medical coding training in Karnataka, or pursuing a certified professional coder course in Hyderabad, you are investing in your future. With the right training and certification, you can embark on a fulfilling career in the rapidly growing healthcare industry.
#best medical coding training institute in andhra pradesh#online medical coding training in karnataka#certified professional coder course in hyderabad
0 notes
Text
Medical Billing Services in Chandler, Arizona (AZ) - 24/7 Medical Billing Services
Leading Medical Billing Services provider in Chandler, Arizona (AZ). 12+ years of expert Medical Billing Services. Call 888-502-0537 now!
#Medical Billing Chandler#Medical Billing and Coding Chandler#Medical Billing Company Chandler#Medical Billing Services Chandler#top Medical Billing Services Chandler#Leading Medical Billing Services Chandler#Medical Billing Agency Chandler#Top Medical Billing Agency Chandler#Top Medical Billing Specialist Company Chandler#Medical Billing Management company Chandler#Best Medical Billing service Company Chandler#Professional Medical Billing Company Chandler#Cheap Medical Billing Company Chandler#Cheap Medical Billing services provider Chandler#Cheap Medical Billing services Specialists#Outsourcing Medical Billing Chandler#Top Outsourcing Medical Billing Chandler#Best Outsourcing Medical Billing Chandler#Outsourcing Medical Billing Services Chandler#Medical Billing Services provider Chandler#Best Medical Billing Service Experts Chandler#Medical Billing Company Experts Chandler#Best Medical Billing Company Experts Chandler#Professional Medical Billing Company#Outsourcing Medical Billing#Top Medical Billing Company Chandler#remote Medical billing Chandler#Medical Billing#Medical Coding#Medical Coding Chandler
0 notes
Text
Why a Medical Coding Certificate Program is Your Gateway to a Rewarding Healthcare Career
In today's evolving healthcare landscape, one career path that has steadily gained momentum in Kerala is medical coding. With the increasing demand for skilled professionals who can bridge the gap between healthcare providers and insurance companies, pursuing a Medical Coding Certificate Program in Kerala can open doors to a secure and rewarding career. This blog explores what medical coding entails, why certification matters, and how a certificate program in Kerala can help you build a future-proof profession in the healthcare industry.
Understanding Medical Coding: The Backbone of Healthcare Administration
Medical coding involves converting healthcare diagnoses, procedures, and medical services into standardised codes. These codes play a crucial role in billing, insurance claims, and ensuring the accuracy of health records. Each time a patient visits a doctor, receives treatment, or undergoes a test, a medical coder ensures that every detail is documented in code form using international coding systems like ICD-10, CPT, and HCPCS.
Medical coders play a crucial role in the healthcare system by ensuring that services are accurately coded, helping hospitals and clinics receive proper reimbursement, and maintaining compliance with regulations. Errors in medical coding can result in claim denials, revenue loss, or even legal complications, making this profession both essential and in high demand.
Why Choose a Medical Coding Certificate Program in Kerala?
Kerala is known for its robust educational infrastructure and strong presence in the healthcare sector. The state’s increasing number of hospitals, diagnostic centres, and medical institutions has created a high demand for certified medical coders. Here’s why enrolling in a Medical Coding Certificate Program in Kerala is a wise career move:
1. Rising Job Opportunities
The healthcare industry in Kerala is expanding rapidly, driven by a combination of public health initiatives and private sector investments. With digital transformation and the growth of medical tourism, the need for medical coders who can ensure efficient documentation and billing has significantly increased.
2. Affordable Education with High ROI
Compared to many other regions, certificate programs in Kerala offer quality education at a relatively low cost. This makes medical coding an accessible career option for students and professionals looking for a quick return on investment.
3. Short-Term, Skill-Oriented Courses
Most Medical Coding Certificate Programs in Kerala are designed to be completed within 4 to 6 months, making them ideal for individuals looking to enter the workforce quickly. These programs focus on practical knowledge and real-world coding applications.
4. Global Career Opportunities
Certification from a reputable program prepares you to meet international coding standards. This opens the door to remote job opportunities and positions with international healthcare organisations, medical billing companies, and insurance firms.
What to Anticipate in a Medical Coding Certificate Program
A well-structured certificate program in Kerala typically covers the following areas:
Introduction to Anatomy and Physiology: Understanding the human body is essential for accurately interpreting medical documentation.
Medical Terminology: Learners acquire the vocabulary utilised by medical practitioners.
ICD-10, CPT, and HCPCS Coding Systems: These are the most commonly used coding standards.
Regulatory Compliance: Training includes understanding HIPAA, healthcare fraud prevention, and data privacy.
Hands-On Training: Most programs offer practical experience through case studies, assignments, and mock coding scenarios.
These programs are often delivered through a combination of classroom teaching and online modules, allowing flexibility for working professionals and students.
Who Should Enrol?
A Medical Coding Certificate Program in Kerala is ideal for:
Fresh Graduates: Particularly those from life science, nursing, or pharmacy backgrounds.
Healthcare Professionals: Nurses, lab technicians, or hospital administration staff looking to shift into a more data-driven role.
Career Changers: Individuals from other fields seeking a stable and in-demand career in healthcare.
Career Prospects After Certification
Upon completing a medical coding certificate program, professionals can work in various settings such as:
Hospitals and Clinics
Medical Billing Companies
Health Insurance Providers
Diagnostic Laboratories
Remote Healthcare Coding Agencies
Job roles may include Medical Coder, Medical Billing Executive, Claims Analyst, and Health Information Technician. With experience and further specialisation, coders can progress into roles like Coding Auditor, Compliance Officer, or Team Lead.
Salary Expectations
The average starting salary for certified medical coders in Kerala ranges from ₹15,000 to ₹25,000 per month. With experience and international certification, professionals can command significantly higher salaries, including remote jobs for global companies that pay in foreign currencies.
Final Thoughts
The healthcare industry shows no signs of slowing down, and the demand for skilled professionals will only continue to grow. By enrolling in a Medical Coding Certificate Program in Kerala, you’re not just acquiring a skill—you’re stepping into a career that offers stability, growth, and the potential to work globally.
Whether you’re a recent graduate, a healthcare worker looking to upskill, or someone seeking a fresh start in a meaningful industry, medical coding offers a clear, achievable path forward. Kerala’s strong healthcare infrastructure, affordable education, and growing opportunities make it one of the best places to begin your journey in this vital and rewarding field.
#Medical Coding Certificate Program in Kerala#Cigma Medical Coding Academy#Transcription Courses in Kochi#Medical Coding Courses in Kochi#Medical Billing Courses in Kochi#Billing Certificate Program in Kochi#Transcription Certificate Program in Kochi#Medical Coding Academy#Australian Clinical Coding Training#Certificate Program in Medical Billing Kerala#Certificate Program in Medical Transcription Kochi#Medical Transcription Course Kochi#Medical Coding Institute#Best Medical Coding Institute in Kerala#Medical Coding Course in Kerala#Best medical coding academy in Kerala#Medical Coding Auditing training in Kochi#AM coding training in Kochi#Clinical Coding training Kerala#Dental Coding training India#Health information Management courses in Kerala#Saudi Coding training in Kerala#Post graduate program in Health information management in Kochi#CPMA Training in Kerala#Medical coding Training Kerala#Professional Medical Coding Courses in Kerala#medical coding programs in Kochi#medical coding certification courses Kerala#AAPC institute of Medical Coding Kochi#Mangalore
0 notes
Text
Optimizing Financial Management with Chiropractic Billing Services

In the healthcare sector, chiropractic care plays a vital role in managing musculoskeletal conditions, improving mobility, and enhancing patients' overall quality of life. However, managing the financial aspects of a chiropractic practice can be challenging due to the unique nature of treatments, frequent patient visits, and varying insurance policies. This is where medical billing services come into play, ensuring that chiropractic practices can focus on providing care while their financial operations run smoothly. These services streamline the billing process, minimize errors, and enhance reimbursement rates, which ultimately leads to better revenue management for chiropractic practices.
What Are Chiropractic Billing Services?
Chiropractic billing services are specialized financial solutions designed to meet the unique needs of chiropractic practices. These services are a critical component of Revenue Cycle Management (RCM) services, which oversee the entire process of patient billing, from claim submission to final payment. Chiropractic billing services handle everything from insurance verification and coding of chiropractic adjustments to following up on claims and managing denials. Since chiropractic care often involves ongoing treatments and multiple patient visits, these billing services ensure that claims are submitted accurately and promptly, reducing delays and maximizing revenue.
The Importance of Medical Billing and Coding in Chiropractic Care
Accurate medical billing and coding is essential for chiropractic practices to ensure that they are compensated for the services they provide. Chiropractic care involves various treatments, such as spinal adjustments, physical therapy, and other therapeutic services, each of which requires precise coding to avoid errors. Incorrect or incomplete coding can lead to claim denials or underpayments, which can negatively affect a practice’s cash flow. By partnering with experienced billing professionals who specialize in medical billing and coding, chiropractic practices can ensure that their claims are submitted correctly and in compliance with industry standards, leading to improved financial outcomes.
Benefits of Healthcare IT in Chiropractic Billing
In the digital age, Healthcare IT has transformed the way billing services are managed, offering numerous benefits for chiropractic practices. Advanced billing software and electronic health record (EHR) systems streamline the billing process by automating tasks such as claim submission, coding, and patient record management. Healthcare IT reduces human error, speeds up payment cycles, and allows for better communication between chiropractic providers and insurance companies. Additionally, real-time tracking and reporting features enable chiropractic practices to monitor the status of claims and payments, ensuring that revenue is managed efficiently. Healthcare IT enhances both the accuracy and efficiency of chiropractic billing, leading to improved practice operations.
Chiropractic Billing Services at Mediclaim Management
Mediclaim Management offers specialized Chiropractic Billing Services designed to meet the needs of chiropractic practices. With a deep understanding of the unique challenges that chiropractors face, their team of billing experts ensures that all aspects of the billing process are handled with precision and care. Mediclaim Management’s Chiropractic Billing Services help providers reduce billing errors, increase claim approval rates, and expedite reimbursements. By partnering with Mediclaim Management, chiropractic practices can focus on delivering high-quality care to their patients while ensuring that their financial operations run smoothly in the background.
With Mediclaim Management’s Chiropractic Billing Services, chiropractic providers can optimize their revenue cycle, reduce financial stress, and ensure that their practice remains financially healthy. This allows chiropractors to focus on what truly matters—improving the health and well-being of their patients.
#medical billing#Optimizing Financial Management with Chiropractic Billing Services#In the healthcare sector#chiropractic care plays a vital role in managing musculoskeletal conditions#improving mobility#and enhancing patients' overall quality of life. However#managing the financial aspects of a chiropractic practice can be challenging due to the unique nature of treatments#frequent patient visits#and varying insurance policies. This is where medical billing services come into play#ensuring that chiropractic practices can focus on providing care while their financial operations run smoothly. These services streamline t#minimize errors#and enhance reimbursement rates#which ultimately leads to better revenue management for chiropractic practices.#What Are Chiropractic Billing Services?#Chiropractic billing services are specialized financial solutions designed to meet the unique needs of chiropractic practices. These servic#which oversee the entire process of patient billing#from claim submission to final payment. Chiropractic billing services handle everything from insurance verification and coding of chiroprac#these billing services ensure that claims are submitted accurately and promptly#reducing delays and maximizing revenue.#The Importance of Medical Billing and Coding in Chiropractic Care#Accurate medical billing and coding is essential for chiropractic practices to ensure that they are compensated for the services they provi#such as spinal adjustments#physical therapy#and other therapeutic services#each of which requires precise coding to avoid errors. Incorrect or incomplete coding can lead to claim denials or underpayments#which can negatively affect a practice’s cash flow. By partnering with experienced billing professionals who specialize in medical billing#chiropractic practices can ensure that their claims are submitted correctly and in compliance with industry standards#leading to improved financial outcomes.#Benefits of Healthcare IT in Chiropractic Billing#In the digital age
0 notes
Text
What are Audio Transcription Services
Audio Transcription Services Audio transcription services are invaluable for keeping accurate records and references to dialogue. They convert spoken language into written text, making information accessible and easy to reference. These services support various sectors, enhancing productivity, inclusivity, and efficiency. By understanding how they work and their benefits, one can appreciate their…

View On WordPress
#academic transcription#accurate transcription services#audio transcription services#business transcription#confidential transcription services#corporate transcription#court transcription#focus group transcription#intelligent transcription#legal transcription#media transcription#medical transcription#pharmaceutical transcription#professional transcription services#transcription with time codes#verbatim transcription
0 notes