#also will being a dr at a mortal hospital and it being like a medical drama where the only way to save
Text
considering the state of camp it's likely half of will's medical equipment is failing or from a previous century and therefore so out of date there's no longer parts made for it, so not only are you being prepped for surgery where your surgeon is like 15 but he also walks in with the most out of date unrecognizable equipment you've ever seen and then knocks you out with the anesthetic....
#i just dont believe they have updated equipment routinely because i mean how are they even getting the stuff in the first place#lots of medical equipment purchases require proof of your practice and they cant really do that#also will being a dr at a mortal hospital and it being like a medical drama where the only way to save#a patient is some obscure piece of medical equipment from 1830 but nobody can figure out what the manual says (if there even is one)#and will walks in and says “ahh!” and just uses the machine without reading a single piece of paper like its another routine day#pjo#will solace#chb
28 notes
·
View notes
Text
Trans research and scientific consensus
(2020) - Study of 139,829 students finds that in comparison to other students, transgender identity, especially non-binary identity, is associated more with perpetrating bullying than being bullied. Non-binary identity was most strongly associated with involvement in bullying, followed by [transgender] opposite sex identity and cisgender identity.
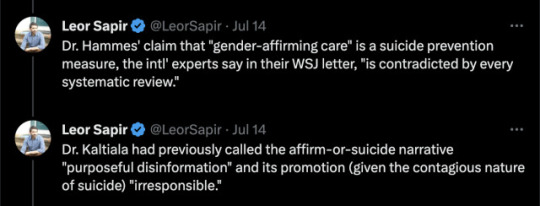
(2023) 21 leading experts on pediatric gender medicine from 8 countries wrote a letter to Wall Street Journal expressing disagreement over how gender dysphoria in youth is treated, voicing concerns against things such as the affirmative model and research conducted outside of the US has found hormonal interventions for gender dysphoria to be without reliable evidence. Among these international experts is Dr. Rita Kaltiala, chief psychiatrist at Tampere university gender clinic and author of several peer-reviewed studies on trans medicine and Finland's top authority on pediatric gender care.
(2023) Landmark study from Denmark on 3,800 transgender patients pulled data from hospital records and applications from legal gender changes and discovered 43% of this group had a psychiatric illness compared with 7% of non-trans group, and despite "gender affirming care" and legal gender changes, still had 7.7 the rate of suicide attempts and 3.5 times the rate of suicide deaths. Researchers state this rate is likely even higher due to missing data.
(2016) Study finds association with increased risk of multiple sclerosis for trans women taking estrogen/reducing testosterone levels.
(2023) Metadata study shows, at best, no improvement for patients in gender-affirming care. "The conclusions of the systematic reviews of evidence for adolescents are consistent with long-term adult studies, which failed to show credible improvements in mental health and suggested a pattern of treatment-associated harms. Three recent papers examined the studies that underpin the practice of youth gender transition and found the research to be deeply flawed. Evidence does not support the notion that “affirmative care” of today’s adolescents is net beneficial."
(2011) Long term follow up of 324 transgender people having undergone sex reassignment surgery in Sweden, found that trans women retained male patterned incidents and rates of violence and had a greater significance and rate of rape and sexual violence than cisgender men. The study also found, "Persons with transsexualism, after sex reassignment, have considerably higher risks for mortality, suicidal behaviour, and psychiatric morbidity than the general population. Our findings suggest that sex reassignment, although alleviating gender dysphoria, may not suffice as treatment for transsexualism, and should inspire improved psychiatric and somatic care after sex reassignment for this patient group."
(2020) Largest study to date on 641,860 people finds association with autism and "gender diversity", "Gender-diverse people also report, on average, more traits associated with autism, such as sensory difficulties, pattern-recognition skills and lower rates of empathy — or accurately understanding and responding to another person’s emotional state".
(2022) US study examining 10 years of data on 952 people finds large percentages of young adults prescribed hormones for trans identity no longer getting the drugs 4 years later. Discontinuation rate for both sexes combined = 30%. Female discontinuation rate as high as 44%. The standard disinformation pushed is that only 1-2% of people who begin medical transition end up desisting. But these figures show that in this cohort of young adults, the overall rate of discontinuing hormone treatment ranged from a low of 10% to a high of 44% within a space of just 4 years.
Abruzzese et al. 2023 'The Myth of “Reliable Research” in Pediatric Gender Medicine: A critical evaluation of the Dutch Studies—and research that has followed'
More to come.
#trans#transgender research#transgender health#trans health care#gender critical#detrans#desistance#detransition#FTM#MTF#non binary#gender studies#gender identity#LGBTQ#trans identity#gender diverse#autism#gender dysphoria#gender affirming care#gender affirmation#transitioning#protect trans kids#protect trans youth
495 notes
·
View notes
Note
I'd love to see Carlisle mated to a patient he saved when she was just a child. Determined as she is she manages to track him down and has a picture of them when she was a child. Please and thank you!!
❝a blast from the past❞
✭ pairing :Carlisle Cullen x reader
✭ fandom : twilight
✭ summary : (y/n) has been treated by Carlisle as a child and all these years later she still wanted to know who that man was, so like any other normal person she tracks him down with the help of the internet
✭ authors note : in my unpopular opinion I don’t really find this man all that attractive no more and I feel y’all hype him up for no reason :)
✭ twilight masterlist



The soft hum of the hospital's fluorescent lights filled the sterile hallway as Dr. Carlisle Hale moved briskly between patient rooms. A respected physician in the quaint town of Thornwood, he was known not only for his exceptional medical skills but also for his quiet, enigmatic demeanor. People whispered that he was too good to be true, an ethereal being walking among mortals.
It was a particularly busy afternoon, and Carlisle was engrossed in studying a patient's chart when a knock on his office door interrupted his thoughts. He looked up to find the head nurse, Evelyn, standing there with a concerned expression.
"Dr. Hale, we have a new patient. She insists on seeing you. Her name is (Y/N)," Evelyn explained, her tone indicating that this patient was unlike any other they'd encountered.
"(Y/N)? I'm not familiar with that name," Carlisle replied, his brow furrowing. The name stirred no memories in him, and he prided himself on knowing every patient's history.
Evelyn handed him a folder containing the patient's information. As Carlisle read through the pages, his eyes widened in recognition. "(Y/N)… I can't believe it," he whispered to himself.
Flashbacks of a rainy night years ago flooded his mind. A car crash had left a young girl on the brink of death, her parents unable to survive the collision. Carlisle had been the doctor on call that night, and he had fought relentlessly to save the child's life. He could never forget the gratitude in her eyes as she regained consciousness.
With newfound determination, (Y/N) had tackled her recovery head-on, defying all odds. But as time passed, her memories of that night faded, leaving only fragments of a faceless savior.
Carlisle took a deep breath, still processing the fact that the very same patient he had saved was now standing at the threshold of his life once more.
"Send her in, Evelyn," he instructed, his voice betraying a mixture of emotions.
The door creaked open, revealing a grown woman with determination in her eyes. Her gaze met Carlisle's, and time seemed to stand still. Recognition sparked in her eyes, and a small gasp escaped her lips.
"Dr. Cullen ," she breathed, her voice barely audible.
"(Y/N)," Carlisle replied, his voice tinged with both surprise and joy. He rose from his seat and approached her, a mixture of feelings swirling within him.
Tears glistened in her eyes as she held out a photograph, worn at the edges from years of handling. Carlisle took the photo, his heart skipping a beat as he recognized the little girl he had saved all those years ago, her smile wide and innocent.
"I never forgot," (Y/N) whispered, her voice breaking. "You saved my life, and I've been searching for you ever since."
Carlisle's eyes met hers, a connection forming between them that transcended time. The unspoken bond they had forged on that fateful night had endured, and now destiny had brought them back together.
As the weight of their shared history settled upon them, Carlisle realized that his world was about to change in ways he couldn't imagine. The girl he had saved had grown into a woman of strength and determination, and their paths were destined to intertwine once more.
"(Y/N)," Carlisle repeated, his voice soft but filled with emotion. He gazed at the photograph, feeling the weight of the years that had passed since that rainy night.
Her eyes never left his face, searching for recognition and finding it in the depths of his gaze. "(Y/N)," he continued, his voice taking on a warm, nostalgic tone. "I remember you. You were so brave."
Tears welled in her eyes, and a relieved smile curved her lips. "I knew I had to find you, Dr. Cullen. I had to thank you properly."
He shook his head gently, a touch of humility in his eyes. "It was my duty, and I'm glad I could help."
As they stood there, a sense of connection formed between them that defied explanation. It was as if the threads of fate had woven their lives together, only to reunite them at this very moment.
"(Y/N)," he said her name once more, savoring the sound of it on his lips. "You've grown into a remarkable woman."
Her cheeks flushed with a mixture of gratitude and shyness. "It's thanks to you, Dr. Cullen. You gave me a chance at life."
Carlisle's heart swelled with a mixture of emotions as he looked at the woman before him. The photograph in his hand captured the essence of the girl he had saved, and now he was face to face with the embodiment of her strength and resilience.
"(Y/N)," he said softly, the weight of what he was about to say settling upon him. "There's something you should know. What happened that night… It was more than just chance. It was fate."
Her eyes widened with curiosity and a touch of uncertainty. "Fate? What do you mean?"
Carlisle hesitated, searching for the right words. "I… I'm not just a doctor. I'm different, (Y/N). I have abilities that go beyond what you might expect."
She regarded him with a mixture of surprise and intrigue. "Abilities? What kind of abilities?"
Taking a deep breath, Carlisle chose his words carefully. "I'm not like ordinary humans. I have gifts that allow me to do things that others can't. And that night, when I saved you, something extraordinary happened."
"(Y/N)" leaned in closer, captivated by his words. "What happened?"
"I… I don't fully understand it myself," Carlisle admitted. "But our connection, the bond that formed between us that night, it's not something that happens every day. It's a rare and profound occurrence."
Her eyes searched his, a mix of wonder and disbelief in her gaze. "Are you saying that we're connected in some special way?"
He nodded, his expression serious yet sincere. "Yes, (Y/N). I believe that our lives are intertwined by something greater than ourselves. And now that you're here, I can't ignore the significance of this moment."
A mixture of emotions played across her features—astonishment, curiosity, and a spark of something more. "(Y/N)" stepped closer, her hand reaching out to touch his arm. "Dr. Cullen, if there's more to our connection, then I want to understand it. I want to know the truth."
Carlisle's heart swelled with a mixture of admiration and tenderness. Here was the young girl he had saved, now a woman standing before him, ready to embrace the mysteries of their shared history.
"As we navigate this journey together, (Y/N)," he said gently, "I promise to reveal all that I can. But know that there's more to discover, more to our story than what meets the eye."
She nodded, determination in her eyes. "Then I'm ready to uncover the truth, Dr. Cullen."
And so, as the bonds of fate drew them closer, Carlisle and (Y/N) embarked on a journey that would unravel the mysteries of their connection, and lead them down a path neither could have foreseen.
#x reader#x reader one shot#x reader oneshot#twilight imagines#twilight imagine#twilight scenario#twilight masterlist#twilight carlisle#carlisle cullen x reader#carlisle cullen#carlisle imagine#carlisle cullen imagine#carlisle imagines#carlilsle cullen imagines#x reader requests#twilight x you#twilight x y/n#twilight x reader
176 notes
·
View notes
Text
STORY AT-A-GLANCE
If you’re sedentary and begin to exercise, you get a dose-dependent decrease in mortality, diabetes, depression, high blood pressure, coronary disease, osteoporosis, sarcopenia, falls and more
People who are doing the highest volume of vigorous exercise start losing longevity benefits. If you’re doing full distance triathlons when you're in your 40s and 50s, your risk of atrial fibrillation increases by 500% to 800%
In the case of moderate exercise — loosely defined as exercising to the point where you're slightly winded but can still carry on a conversation — there’s clear evidence that more IS better and cannot be overdone
Every 1,000 steps you get on average per day reduces your mortality by 10% to 15%. Benefits plateau around 12,000 steps (6 miles) a day
Strength training adds another 19% reduction in all-cause mortality on top of the 45% reduction that you get from one hour of moderate exercise per day. However, benefits cease once you go beyond one hour per week. The sweet spot is 20 to 40 minutes of strength training, two to three times a week. Above 60 minutes per week, the benefits of strength training are nullified, and you’re worse off than if you did no resistance training at all
In the video above, I interview Dr. James O'Keefe, a cardiologist with the Mid-America Heart Institute at St. Luke's Hospital in Kansas City, about exercise dosing. He completed his cardiology training at Mayo Clinic.
He and three other coauthors published a meta-analysis in the March-April 2023 issue of Missouri Medicine,1 the journal of the Missouri State Medical Association, which has profound implications. I view this study as a landmark that radically changed my views on exercise.
Without doubt, we need exercise. The question is, how much? Many of us who are committed to being optimally healthy tend to overdo it, which is certainly true in my case. Had I had the information in O’Keefe’s study earlier, I could have saved myself a lot of time and effort.
Too Much Exercise Can Backfire
As it turns out, O’Keefe also has a history, just like me, of overdoing it when it comes to exercise, which is ultimately what led him to pursue this research, trying to find out where the sweet spot is — the amount of exercise that delivers the greatest benefits.
"I've always used exercise, whether I'm nervous or happy or sad. Exercise has been my coping mechanism. I played varsity basketball and ran track. When I quit playing basketball in college and focused on medicine, I made a personal note that I have to exercise every day because this is super important for me.
A lot of people have this notion that if some is good, more is better. So I got into triathlons and I was running 5K, 10K races and occasional marathons. I was really, really fit and I was pushing my body. But when I got to be about 45, I started to get palpitations and sometimes I'd get this aching after a really high intensity bike ride or things like that.
I realized, ‘Wait a minute, where did I get this notion that if exercise is good, this extreme exercise in middle age is better?’ It's just not. And so I started doing research. I have a lot of connections around the world in the clinical research community. We started looking at this question, and sure enough, it's quite obvious that you can overdo exercise.
I did a TED Talk on it. It has millions of views. And I've just focused on this. Exercise is good for you — 70% of U.S. adults don't get enough exercise, and they would be healthier getting more exercise, any exercise.
In fact, the first 20 minutes of exercise will get you most of the benefits. Even getting out for a walk is dramatically better than sitting on the couch, sitting in front of a screen or sitting behind a windshield.
We have a sedentary lifestyle, and if you don't actively incorporate movement into your day, you're going to be in trouble, no question about it, just like following the standard American diet will absolutely get you in trouble.
But about 2% of people are overdoing it. It might be 5%. Highly active people, competitive people. And it's probably because the world you and I live in — I know a lot of people like this. I see patients like this all the time.
They come with AFib, or accelerated atherosclerosis with a lot of calcium in the coronary, or ventricular problems. It can even shorten your lifespan if you get really extreme about it."
Do We Have Programmed Life Expectancy?
O’Keefe recounts the story of how his mentor at the Mayo Clinic, decades ago, would admonish him when he’d go for a run at lunchtime saying "You know James, you're just wasting your heartbeats. Your heart has only so many heartbeats."
His mentor made the case that everything appears to have a sort of programmed life expectancy that correlates with your heart rate. A hummingbird, for example, has a heart rate of 500 beats a minute and lives a year or two. The mouse has a similarly high heart rate and lives about two years. Animals with really slow heart rates, on the other hand, like the whale, can live 200 years.
This is not to make a case for being a couch potato though. "It’s a complex math problem," O’Keefe says. What you want is to do enough exercise so that your pulse remains nice and low while you’re not exercising.
"That's the way to maximize your heart rate," he says. "But you don't want to be exercising intensely for five, seven hours a day, let alone do a full-distance triathlon. You're just asking way too much of your heart. There’s an intuitive logic about this as well. Like everything in nature, you're better off not [being] in the extremes.
And that's true with exercise. When you drill down on what types of exercise really correlate best with longevity, it's not the maximum amount of high intensity interval training. Some of that's important, but more is not necessarily better for vigorous intense exercise."

Download this Article Before it Disappears
Download PDF
Take-Home No. 1: Too Much Vigorous Exercise Backfires Big Time
O’Keefe’s systematic review revealed that if you’re sedentary and begin to exercise, you get a dose-dependent decrease in mortality, diabetes, depression, high blood pressure, coronary disease, osteoporosis, sarcopenia, falls and more. So, most definitely, you can dramatically slow aging and improve life expectancy with exercise.
However, at the very high end, the people who are doing the highest volume of vigorous exercise start losing those benefits.
"They're not as bad off as sedentary people, but virtually every study you can find, they will lose some of those benefits for longevity, and certainly for things like atrial fibrillation.
If you go from sedentary to exercise moderately, you have less atrial fibrillation. But if you're doing full distance triathlons when you're over age 40 or 45, you start seeing a 500% to 800% increase in atrial fibrillation."
O’Keefe cites a recent large-scale study that followed about 1 million individuals for more than 10 years. While vigorous exercise up to 75 minutes per week reduced the risk of all-cause mortality and other diseases in a dose-dependent manner, benefits plateaued after that.
So, people who were doing four to seven hours of vigorous exercise per week didn't get any additional benefit, "and probably, from a cardiovascular standpoint, lost a little bit," O’Keefe says.
Take-Home No. 2: You Cannot Overdo Moderate Exercise
In the case of moderate exercise, however — loosely defined as exercising to the point where you're slightly winded but can still carry on a conversation — it’s very clear that more IS better and cannot be overdone.
"We're talking gardening, housework, walking, recreational bike riding, yoga, nonintense swimming, pickleball. [When doing] these things, more is better," O’Keefe says.
Perhaps even more surprising, moderate exercise also improves all-cause survival better than vigorous exercise — about two times better. "If you look at the people who are doing the most vigorous exercise compared to the people doing the most moderate exercise, the moderate exercisers have twice as good a reduction in long-term mortality as the high volume vigorous exerciser," he says. What this means in practical terms is that:
a)There’s no need to engage in high-intensity strenuous exercise beyond 75 minutes per week. Doing so can be highly counterproductive. If you’re an overachiever, stick to moderate exercise instead and your benefits will continue to accrue and your efforts won’t eventually backfire.
b)Once you get into your mid-40s and 50s, exercise should be fun and stress-reducing, not competitive. In his analysis, O’Keefe also stresses the importance of "social exercise" over solo exercise: playing a game of pickleball with friends, for example.
Several years ago, he conducted a study with colleagues in Copenhagen, Denmark, in which they looked at long-term granular data on physical activity and longevity.
Playing tennis conferred 9.5 years of extra life expectancy; playing badminton got seven years; running, swimming and cycling were associated with just 3.5 years of extra life expectancy. Health club activities such as weightlifting and running on a treadmill only conferred 1.5 years of additional life expectancy compared to sedentary life.
At first, O’Keefe thought the analysis had somehow gone wrong. But then he realized it was the social aspects of the sports that conferred the added benefits.
"Exercising and making social connections at the same time, that is an absolute goldmine of a longevity activity," he says. "That means that even walking with your dog or your friend or [playing] pickleball is huge ... The whole thing is to move your body in a fun, playful manner and make it social."
What Big Data Tell Us About the Benefits of Walking
Walking should not be underestimated either. The average American walks about 3,800 steps a day, which is just short of 2 miles. It’s about 2,000 steps per mile, and every 1,000 steps you get on average per day reduces your mortality by 10% to 15%, O’Keefe notes.
"There's been more and more studies on this all the time, using activity trackers. We’re getting big data, like the UK biobank, which is a half a million people, and there's a sizable subgroup of them who have been wearing activity trackers and been followed for 10 years now.
Clearly, more is better. You get the big gains going from sedentary lifestyles — 2,000 to 3,000 steps a day — up to 7,000 or 8,000. [Here] you have this very steep reduction in mortality, improvement in survival. It continues to about 12,000 steps a day. Most of the studies show that it plateaus at 12,000."
Track Your Steps, but Beware of EMFs
If you’re strapped for cash, you don’t need to invest in a special fitness tracker. Most cellphones have free activity trackers, so all you need to do is carry your phone with you. It’s not ideal due to the electromagnetic fields (EMFs) emitted, but you could put it in airplane mode.
I recently gave a lecture at an autism event called Documenting Hope in Orlando. They’re committed to research and have invested hundreds of thousands of dollars to do detailed analyses of autistic children to identify the causes of autism.
I almost fell off my chair when I heard the results. EMF was the No. 2 cause of autism. No. 1 was antibiotics, No. 3 was toxins, and No. 4 was vaccines. So, please, do take EMF exposures seriously. While adults aren’t going to develop autism from EMF exposure, it can still cause neurological damage. So, keep your cellphone in airplane mode when not in use, or better yet, in a Faraday bag.
Take-Home No. 3: Overdoing Strength Training Is Worse Than Doing Nothing at All
O’Keefe’s meta-analysis also detailed the sweet spot for strength training, and the results truly shocked me. I radically changed my exercise program after reviewing these data.
Without question, strength training will improve muscle mass, muscle and bone strength. It can also boost your testosterone level if not overdone. It helps to improve mood and prevent falls. As you get into your 30s, you start to lose muscle mass and if you don't train to maintain muscle mass, you’ll eventually end up with sarcopenia (low muscle mass) or osteoporosis (low bone density). O’Keefe comments:
"I've always been a fan of strength training ... But again, the devil is in the details about the dosing. When you look at people who do strength training, it adds another 19% reduction in all-cause mortality on top of the 45% reduction that you get from one hour of moderate exercise per day.
When I strength train, I go to the gym and spend anywhere from 20 to 40 minutes, and ... I try to use weights that I can do 10 reps with ... After that, you're feeling sort of like spent and ... it takes a couple of days to recover. If you do that two, at the most three, times a week, that looks like the sweet spot for conferring longevity."

The graph above, from the meta-analysis, shows the J-shaped dose-response for strength training activates and all-cause mortality. As you can see, the benefit maxes out right round 40 to 60 minutes a week. Beyond that, you’re losing benefit.
Once you get to 130 to 140 minutes of strength training per week, your longevity benefit becomes the same as if you weren't doing anything, which is nothing short of shocking. If you train for three to four hours a week, you actually end up with WORSE long-term survival than people who don't strength train!
Recall, when you’re doing intense vigorous exercise in excess, you’re still better off than people who are sedentary. But for some (yet undetermined) reason, excessive strength training leaves you worse off than being sedentary.
So, the take-home message here is that 20 minutes twice a week on non-consecutive days, or 40 minutes once a week is the sweet spot. You also don’t want your exercise regimen to center around strength training. It should be an add-on, as you get far greater benefits simply from walking, or any other moderate exercise.
What About When You Do KAATSU?
Now, there may be a caveat to this. Conventional strength training involves lifting weights that are anywhere from 70% to 90% of your one-rep max, and that’s the style of weight training most studies are based on. Another form of strength training is blood flow restriction (BFR) training or to use the Japanese term, KAATSU.
In KAATSU, you’re using very light weights — 70% lower than conventional weightlifting. Considering you’re not pushing your body to the max with heavy weights, you can likely train longer than one hour a week without nullifying benefits. It’s closer to moderate movement exercise than conventional resistance training.
O’Keefe is not familiar with KAATSU and has not studied its effects, but he agrees that it makes rational sense that you should be able to work out longer when doing KAATSU — maybe two to three hours a week.
Get Your Nature Fix
O’Keefe’s paper also discusses the benefits of spending time in nature. A British study cited found you need at least 1.5 to two hours outdoors each week for good health, even if it’s only a local park or tree-lined street.
"And then forest bathing is really interesting," he notes. "Japanese people who live in Tokyo, one of the biggest cities in the world, will get on a bullet train and an hour or two later be at the mountains and in the forest. They go hike around or even just sit in nature and smell the pine and the fresh air. Then they get on the bullet train and go back home.
They show reductions in blood pressure and improvement in mood. And there's really, really strong benefits ... It’s been shown to ... reduce anxiety and improve sleep and all those kinds of things that are important for well-being."
4 notes
·
View notes
Text
Women at Higher Risk of Mortality Following a Heart Attack, Study Finds

Introduction:
A recent study comparing outcomes among men and women following a heart attack has revealed that women are more likely to die after experiencing a heart attack compared to men. The findings emphasize the need for improved monitoring and care for women in the aftermath of a heart attack, calling for greater attention to be given to their specific needs. Cardiovascular disease remains the leading cause of death globally, with heart attacks and strokes accounting for the majority of related fatalities.
Study Highlights Disparity in Outcomes:
While men are more prone to cardiovascular conditions, research indicates that women tend to experience worse outcomes during hospital stays following a heart attack. Factors such as advanced age, increased prevalence of other health conditions, and lower usage of stents to address blocked arteries contribute to this discrepancy. Stents are small mesh tubes that help restore blood flow in narrowed or weakened arteries.
Study Methodology and Findings:
The study examined data from 884 patients, with women comprising slightly over a quarter of the participants. Women in the study were, on average, older than men and exhibited a higher prevalence of high blood pressure, diabetes, and prior stroke. However, men were more likely to smoke and have coronary artery disease. The researchers found that women faced a significantly higher risk of adverse outcomes, including death, both in the short and long term, compared to men who received the same treatment.
Expert Insights:
Dr. Steven Gundry, a cardiothoracic surgeon and renowned expert, expressed concern over the historical disregard of women's heart complaints and stressed that pre-menopausal women are equally vulnerable to heart disease. Dr. Gundry refuted the long-held belief that estrogen protects women against heart disease, emphasizing the urgent need to address the issue.
Potential Factors Influencing Higher Mortality Rates:
Although the study did not delve into the specific reasons for the gender-based differences in outcomes, experts suggest several factors. Women often exhibit atypical symptoms during a heart attack, such as indigestion or shoulder pain, which can delay prompt diagnosis and treatment. Additionally, women's smaller arterial diameter makes stent placement more challenging, further contributing to poorer outcomes. Gender bias and a lack of awareness among healthcare providers may also lead to women's complaints being dismissed, even in emergency settings.
Importance of Timely Diagnosis and Treatment:
Undiagnosed heart failure is another critical issue highlighted by recent research. Many patients treated with loop diuretics, drugs used to alleviate congestion caused by heart failure, may not have received an accurate heart failure diagnosis. This is particularly true for women, who constitute a significant proportion of those with undiagnosed heart failure. The combination of undiagnosed heart failure and inappropriate loop diuretic usage can have detrimental consequences.
Implications and Takeaways:
The study's findings underscore the necessity of earlier detection and treatment of heart conditions in women. Medical professionals should maintain a high index of suspicion for heart failure in patients requiring loop diuretics. Preventive measures such as lifestyle modifications, including diet and exercise, assume added significance in reducing the risk of heart failure, particularly for women. Addressing gender disparities in heart disease care remains a critical challenge that demands attention and intervention.
Conclusion:
The study's findings reveal a concerning disparity in outcomes between men and women following a heart attack. Greater awareness, improved diagnostic methods, and tailored treatment approaches are essential to address the specific needs and risks faced by women in cardiovascular care. The medical community must prioritize a gender-sensitive approach to ensure better outcomes and reduced mortality rates for women affected by heart disease.
1 note
·
View note
Text
Learn about “Nurses-led AMR practice change: a design and humanities participatory approach to healthcare innovation in policymaking” by Dr. Fernando Carvalho at the CME/CPD/CE accredited 11th World Nursing, Healthcare Management, and Patient Safety Conference on November 15-18, 2022 in San Francisco, USA

About of Dr. Fernando Carvalho
With more than fifteen years of experience working in a variety of professional and academic contexts around the world, he is an award-winning designer, researcher, and educator. Since 2005, my artwork has been displayed in museums and galleries throughout the USA, Brazil, Spain, England, and Spain.
Dr. Fernando Carvalho has a private practise and works for companies like the NHS, Memorial Hospital of South Bend, Unicef, Heineken Brewers, Kiefer, Sony Music, and the Federation of Industries of Rio de Janeiro on healthcare services, medical devices and hospital interiors, Paralympic sports accessories, civil construction equipment, signage, wayfinding, and digital solutions.
He has worked on projects as varied as after-school programmes for kids in Rio de Janeiro's "favelas," training programmes for craftsmen, and undergraduate and graduate courses in design and architecture in the UK, the USA, Brazil, Chile, and Portugal. He has also conducted research and developed curriculum for these programmes.
We are pleased to inform you that Dr. Fernando Carvalho is going to present his research work on "Nurses-led AMR practice change: a design and humanities participatory approach to healthcare innovation in policymaking" at the CME/CPD/CE accredited 11th World Nursing, Healthcare Management, and Patient Safety Conference on November 15-18, 2022 in San Francisco, USA & enhance your knowledge on Nursing, Healthcare and patient safety.
Avail Certifications by registering here: https://nursing.universeconferences.com/registration/
AMR's Effect on Nursing
Drug-resistant antimicrobial infections are linked to adverse health outcomes, such as lengthened hospital stays, complications, and mortality, which have a significant impact on both human health and the health-care system.
Microbiological Resistance
Microorganisms (such as bacteria, fungi, viruses, and parasites) evolve and develop resistance to the drugs typically used to treat their diseases, which is known as antimicrobial resistance (AMR). This is a critical issue since several kinds of illnesses that were once treatable with normal care, like gonorrhoea, tuberculosis, and pneumonia, are now showing signs of being resistant to one or more antimicrobials (e.g., antibiotics, antifungal agents).
Microorganisms (such as bacteria, fungi, viruses, and parasites) evolve and develop resistance to the drugs typically used to treat their diseases, which is known as antimicrobial resistance (AMR). This is a critical issue since several kinds of illnesses that were once treatable with normal care, like gonorrhoea, tuberculosis, and pneumonia, are now showing signs of being resistant to one or more antimicrobials (e.g., antibiotics, antifungal agents).
Function of the Nurse
In the fight against AMR, nurses are crucial players and may help with the wise use of antibiotics in a variety of ways, such as:
· Examine and keep an eye out for infection symptoms and adverse consequences of antibiotic use.
· Use caution when prescribing and stopping.
· Serve as stewards for laboratory tests and microbiological.
· Patient and public education
· Put infection control and prevention strategies into action.
· Make sure the right allergies are recorded.
AMR in the medical field
Antimicrobial resistance: what is it? Antimicrobial Resistance (AMR) is a condition in which bacteria, viruses, fungi, and parasites evolve over time and cease to respond to antibiotics, making infections more difficult to cure and raising the risk of disease transmission, life-threatening sickness, and death.
Register here: https://nursing.universeconferences.com/registration/
Healthcare Innovations
Healthcare innovation can be as straightforward as altering a form to speed up a patient's check-out by five minutes or as sophisticated as an immunotherapy that targets particular cancer cell types. Healthcare innovations are any advancements, no matter how simple or advanced, that enhance patient experiences and health outcomes.
Several medical innovations
· Artificial intelligence.
· Things in the Internet of Medicine.
· Telemedicine.
· Analytics and Big Data.
· Integrated technology
· Health on the go.
· 3D printer.
· Utilizing the cloud.
Policy Innovations for Health
The direction of health policy is changing right now. It is becoming more and more obvious that the current health care system needs to be changed if we are to preserve and improve our health at this point in time. We need to change direction and adopt a fundamentally different mindset when it comes to health and health policy, as evidenced by our enormous understanding of what promotes health as well as the exponentially rising prevalence of chronic diseases, obesity, and mental health issues. What we mean by "policy innovations for health" is exactly this. The definition of what we refer to as the "health system" is eroding, and how we conduct our daily lives now depends heavily on our state of health. The state of one's health has grown to be a significant economic and social force in society. This changes the pressure for policy innovation from a focus on the current healthcare system to a restructuring of how we view health in 21st-century cultures. The dynamics of the health society put to the test how we think about and situate health in the context of policy, as well as how we carry out health policy. They also alter who should be a part of the policy-making process. This issue is starting to receive attention from both the government and outside of it, thanks to new partnerships for health and ideas like "Health in All Policies." The most significant of the policy improvements for health in the 21st century will likely result from the redefining of the roles of citizen and patient.
Register here: https://nursing.universeconferences.com/registration/
Experience and Education of Dr. Fernando Carvalho
Experience
· Assistant Professor of Design
· Senior Lecturer in Product Design
· Associate Lecturer
· Postdoctoral Research Fellow – Criminal Justice Policy Development (DACRC / SDI)
· Doctor of Philosophy (PhD), Human Factors in Complex Systems Lab
Education
· Loughborough University
· University of Notre Dame
MFA, Industrial Design / Healthcare Design
· Pontifícia Universidade Católica do Rio de Janeiro
BFA, Visual Communication and Product Design
Objectives of the 11NHPSUCG Conference:
The nursing, healthcare management, and patient safety conference's goal is to promote and undertake collaborative multidisciplinary research in cutting-edge methodology and technologies in nursing education and nursing practice. It gives vital chances for the Nursing and Healthcare Management Community, as well as our collective body of knowledge, to grow and improve.
Contact us:
Email us at [email protected]
WhatsApp: https://wa.me/442033222718
You can access all the conference sessions here: https://nursing.universeconferences.com/
Submit the abstract here: https://nursing.universeconferences.com/submit-abstract/
Register here: https://nursing.universeconferences.com/registration/
0 notes
Text
Is Technology Helping or Hindering Medical Negligence Mortality Rates?
Is healthcare technology really as positive as it seems? We explore this question through discussing some of the positive and negative impacts tech is having on medical negligence mortality rates.
Technological advancements are increasingly changing the face of the healthcare industry, from basic monitoring and admin, all the way to surgical interventions that can improve accuracy in the operating theatre.
The aim of these advances is ultimately to streamline processes and reduce cases of fatal medical negligence claims across the board. That said, is this the case in reality, and are there any negative impacts of technologies being relied upon in the medical field?
In this article, we’ll be exploring the answers to this question by discussing some of the positive and negative impacts of technology on mortality rates. Take a look
How Technology is Helping to Reduce Medical Negligence Mortality Rates
Starting with the positive ways in which technologies can help to reduce the chances of medical negligence, and therefore reducing mortality rates, some pointers include:
Simplified Procedures
Technological advances can help to simplify administration procedures throughout hospitals, which can avoid errors across the board. The most obvious example of this being used in practice is the centralisation of systems across countries. This can make processes easier, quicker and more accurate for both hospital staff and patients.
A more specific example of a technology that could help with this is iris scanning, which could help to accurately and quickly identify patients within facilities to avoid any mishaps.
Less Human Error
Human error is a big cause of negligence within the medical field, not just by doctors and nurses in the field, but even at the administration level. Medical filing and record keeping can lead to negligence errors, and the use of technology can help to avoid these sorts of mistakes.
Another human error issue which could be avoided is the loss of surgical equipment, like sponges, within bodily cavities during surgeries. There are manual methods of avoiding these mishaps, but technologies like electronic assistance could help to streamline this process, making things more efficient and reducing the chance of post-operative complications.
Reducing Medication Errors
According to research, “medication errors are frequent and… adverse drug events, or injuries due to drugs, occur more often than necessary”. The frequency of injuries related to medical examination or treatment far outweighs those from aeroplane and automobile crashes, which gain far more public attention. Overall, it’s said that between 28% and 56% of adverse drug events are preventable.
With the advent of advancements in medicinal technology, interventions involving information systems are proven to reduce errors when administering medication. Examples of technologies that are helping with this include:
Computerised physician order entry
Physician decision support from computers
Robots filling prescriptions
Bar codes
Automated dispensers
Medical administration of drugs via computers
Improving Accuracy
Surgical technologies are constantly improving to increase accuracy during surgeries. For example, augmented reality can offer more complete data within a surgeon’s field of vision. This can improve the safety of the patient, as well as their outcomes due to reducing the risk of postoperative complications.
Some ways these sorts of technology can do so, include increasing the accuracy of placing instruments during surgeries. Also, the surgeon’s eyes and hands can remain where they are, without such as risk of detrimental movement.
Dr Shin from Becker’s hospital said, “With conventional navigation and robotic platforms, a consistent limitation for the surgeon is having to take our eyes away from the field. This can have drawbacks, especially when passing instruments around neural and vascular structures where millimetres can make a difference. It is exciting to see how continued development will account for such limitations.”
Ongoing Record Keeping
Patient monitoring to understand the body both before and after any medical intervention may help to reduce misdiagnosis and malpractice, as well as improve post-operative care. Advances in technology available to the general public, like smart watches, which continually monitor a person’s health, may be instrumental in making this accessible to the masses.
Identify Malpractice
Cameras and CCTV footage throughout hospitals can help to identify medical malpractice. Some systems are advanced enough to keep an eye on the surgical team’s checklist, ensure the right patient is in the operating room, and the correct procedure is being carried out. Therefore, any issues can be spotted and rectified before further damage.
This can help to streamline the process, and ensure preventative measures can be put in place. It can also help to identify risk factors for medical negligence to avoid them happening before they are carried out.
How Technology is Increasing Medical Negligence Mortality Rates
As you can see, there are plenty of potential benefits of using technology to reduce the advent of medical negligence. But, what are some of the negative impacts? We’ll be exploring these next…
Over Reliance
Over reliance on technology has the risk of making hospital staff complacent. Once they’ve been through the rigorous education required to become a doctor or nurse, the reliance on technology once in the field may reduce skill and ability.
Of course, this is purely speculation, and we cannot know how each individual staff member may react to the technological help. However, this is a potential impact that should be considered.
Medical Negligence in Practice Will Always Continue
Medical technologies can limit the number of cases of negligence in terms of medication administration, hospital admin and more, but it can’t always help to avoid negligence in the field. For example, in emergency situations where the doctor’s judgement and education comes into play, human error may be more likely.
Common examples of this could emerge during childbirth, when emergency situations may arise, and decisions must be made quickly. Excessive force may be utilised in these situations, causing injuries to the mother and baby. These situations cannot easily be avoided through the use of technology.
Other Implications of Medical Technology
There are also a number of other negative implications of technology use in hospitals, which don’t necessarily affect mortality rates, but may impact hospital staff and patients. These may include:
Financial implications
Staff training
Limited scalability
Risks of contamination
Who’s the Blame if Medical Malpractice Occurs?
As you can see, there are plenty of positives to introducing more tech into the world of healthcare. However, there are some issues.
With the advancement of technology to intervene in potential cases of malpractice, when negligence does occur, it may become tricky to isolate the key problem within each individual situation. This can mean that patients have no clear pathway for blame, which may complicate matters of law.
It’s key that with these advancements comes strict record keeping which can help to isolate the causes of any incidences that do occur.
What do you think of the increasing use of technology in the healthcare industry? Do you think it’ll help or hinder mortality rates?
Technical Doctor's insight:
Contact Details :
[email protected] or 877-910-0004
www.technicaldr.com
0 notes
Text
Ladies, ask for a doctor that is a woman. It could save your life.
Women are at a potentially fatal disadvantage on the operating room table, according to a “troubling” new study of more than 1.3 million patients treated by 2,937 doctors.
Gender presents a life-or-death risk for women, the study finds, with females 15% more likely to die or incur serious complications if operated on by a male surgeon, medical researchers at Vanderbilt University in Nashville, Tennessee and University of Toronto in Ontario, Canada reported.
They based their joint analysis — conducted from November 2020 to March 2021 and published this month in JAMA Surgery — on data from 1,320,108 patients who received both elective and medically necessary surgeries between 2007 and 2019.
Of that group, 717,548 were “sex discordant” — meaning the surgeon and patient were of different genders (more than 180,000 of those being women with male surgeons — and adverse outcomes). However, average rates of patient mortality and related complications improved about equally among all other scenarios, whether women operated on women, women on men or men on men.
“What is surprising and troubling is that negative outcomes, including complications and death, were linked to sex discordance,” said Florida surgeon Dr. Amalia Cochran in a published research letter tied to the study. “Unfortunately, this association disproportionately affected female patients. The association between surgeon-patient sex discordance and outcomes sounds the alarm for urgent action.”
The research team co-led by Dr. Cochran and Dr. Andrea N. Riner also accounted for age, health and other conditions that could give way to surgical complications.
Study authors said more research is needed to determine the root of the results, but Cochran suggested a greater need to promote more women going into medicine, as men by far dominate the field, with male doctors still outnumbering female doctors, 64% to 36%, according to 2019 data from the Kaiser Family Foundation.
“In 2019, only 22% of general surgeons in the US were women, and orthopedic surgery had the lowest representation of female surgeons at 5.8%,” Dr. Cochran said, citing statistics from the Association of American Medical Colleges.
“However, self-reflection is warranted on the way in which we provide care,” she added. “Surgeons likely believe they provide the same quality of care to patients irrespective of identity. However, these data underscore an under-appreciated phenomenon and highlight a measurable repercussion of implicit bias.”
Meanwhile, past studies suggest that women may actually make more ideal doctors. Similar research published in 2018 found that death rates among 580,000 heart patients in Florida emergency rooms were overall lower if treated by female doctors compared to when men wore the white coats.
The difference was marginal in another 2016 study — a margin of 32,000 lives, that is. More than 1.5 million hospitalized Medicare patients were found less likely to die at the hospital or be readmitted after seeing a female doctor. The difference was only a half percentage point overall, but made tens of thousands of lives of difference.
713 notes
·
View notes
Note
Your AU seems really cool!!! Can you explain a little bit to me?
for sure! i know my first post about it was a LOT of words so ive been meaning to write a summary - that being said, this feels just as long if not longer LJFDKSLFJDSLKFDJS WHOOPS
SHORTEST SUMMARY: matt, for reasons of his own, digs out his old necronomicon from zombeh attack and begins a considerably faster-spreading zombie apocalypse with his new undead minions. included in his undead minions is jon, who he revived, eduardo, who is matt's necronomicon-powered enforcer, and mark, who is basically just a glorified manservant.
the situation is serious enough that the red army becomes involved, and tord decides to take matters into his own hands.
since the incident in 'the end', it seems as though matt, tom, and edd have been having some very complicated feelings. the dark power of the necronomicon seems to be affecting them each in very different ways that im exploring in the au. :3
edd's powers amplify his emotions and his emotions amplify his powers. despite this, he seems to be having a suspiciously good time despite the fact that it's the end of the world. tom's…. gestures at the tom puddle. toms "coping" (ill explore his character more thoroughly i pwomise >:U) and matt's…… coping by doing crimes against humanity u__u
longer details:
general idea is that the main four are very emotionally unavailable to each other, and that combined with the ew worlds zaniness means that theyre ~traumatized~ and dealing with it kind of badly.
zombeh attack is all pretty much canon, except theres specific medication treatments that can be used to unzombify people - so instead of being sucked into the necronomicon, released from the mortal coil, and generally zombified, matt, tord, tom and edd basically just had to keep on living with minor zombification symptoms. (the ambulance ride was very stressful LMAOOOO)
zombification has its benefits, including somewhat-easy replacement of limbs and heavily increased tenacity - but the detriments, including nerve damage, physical and mental trauma, etc, are considerably worse. matt managed to replace his arm early enough that he still has his old arm, but it's definitely not working perfectly. this, combined with the memory gun incident and vampirism have made his physical and mental situation a little bit… stressful for him! the incident in 'the end'
tords leg was already long-rotted by the point of hospitalization, and he ended up eventually creating his own robotic prosthesis, similar to his eventual super awesome robot arm. needless to say the guy definitely has issues from being dead for a while, eventually culminating in his betrayal in 'the end' :3 he's got a heavy hero complex and seems to take every responsibility very seriously, but also struggles with his own mortality and weakness
tom and edd………….. have got their own issues that i am just taking oddly seriously (zany emoji)
TL;DR trauma boys powered up by necronomicon, tord comes home and goes 'wtf is wrong with you' and everyones like 'what the fuck is wrong with YOU' and the answer is ~society~
poweredd, necromancer matt, monster tom, and tords here too! 8-)
19 notes
·
View notes
Note
Last place I lived, there were a ton of proverbs/sayings to the tune of "trip to the doctor will damage you more than the disease": it seemed a given, the abuse & lack of power. The chronic pain community on tumblr's also really good about not taking shit from drs after being mistreated too many times. I think older ppl are treated with less abuse in medical setting, partly b/c Doctors Be Like That & partially b/c older people Take No Shit & are very assertive about what can/can't be done to 'em
I’ve talked a lot (sort of?) on here about the pervasive problems with how doctors treat people, and how harmful that is to autistic people specifically. Mostly because I, specifically, have a horribly debilitating fear of going to the doctor that I feel like I can’t/shouldn’t refer to as “trauma” but that “phobia” doesn’t really describe at all. Like…I’m incredibly good at ignoring/managing anxiety, but medical things are a whole other tier. I straight up can’t go in a doctor’s office without shaking like a chihuahua. I went just to get tested for covid last year and crashed so hard from the adrenaline that I was too exhausted to do anything but lie in bed for like two days.
I especially hate needles, and for a couple years a while back the smell of rubbing alcohol would trigger shooting pain in my arms. It was fucking weird.
The thing thats fucked up is that the fear wasn’t really linked to being actually exposed to the thing, like with a phobia. I have a lot of nightmares about medical stuff when I’m anxious, kind of always have? I developed a lot of super debilitating fears of different when I was a preteen having panic attacks for the first time (fun) and most of them linked in some way to medical things. For a solid year or two of my life I was 100% convinced I had any of a number of serious illnesses, and it only hit me this past year how most of them were things that were 100% treatable. It was never like…cancer or something that could realistically threaten my life. The fear always centered on like…being hospitalized. Because that was The Worst Thing Imaginable, like my ability to imagine bad things just stopped there (and I was a kid who was like. Very, very, very much aware of my own mortality). My brain never got to the concept that “okay but if that happened they would be able to help you and you would be okay” because I couldn’t conceptualize anything coming “after” Medical Treatment.
I feel like it’s linked to a few bad experiences I had as a very young kid, but it wouldn’t have gotten this bad if my experiences with doctors weren’t so generally pervasively bad. I’m autistic. I don’t like unpredictability. I don’t like to be touched by strangers. It gets harder for me to communicate when I’m stressed. For most of my life my experience with doctors was “person in position of authority that feels entitled to access to your body and will do things to your body without explaining them,” and now I’m on levels of neurosis you mortals can’t even imagine.
But there’s the initial damage, right? And then there’s the damage that comes of everyone around you insisting your fears are irrational and there’s something wrong with you. I always hated the label of “phobia” because I was supposed to accept that it was irrational to be afraid of being forced to give unlimited access to my body to a stranger that wouldn’t communicate with me or treat me decently.
Everything I read about how to free myself from the horrible nightmare-scape I was in assumed there was something wrong with me. It took so, so long for me to encounter anything that even considered the idea that maybe there was something wrong with how I was treated, instead of something being wrong with my feelings.
And this is the thing that’s really…traumatic about being autistic. Your boundaries are wrong; people aren’t wrong for violating them. Your behavior is wrong; people aren’t wrong for bullying you. If something traumatizes you that most people can “get over,” it’s not traumatic, it’s something wrong with you.
Long story short, this is how I learned how our understanding of psychological harm is prescriptive, not descriptive.
People who otherwise understand bodily autonomy get really weird about this subject. Because in our culture, doctors are Authority Figures, and they’re trying to help you, so you shouldn’t be assertive in setting the terms for your care, you shouldn’t refuse examinations you’re uncomfortable with, you shouldn’t kick medical professionals to the curb when they can’t or won’t communicate with you in the way you need. You can’t even express frustration without people siding with the doctor, because they have a degree, and that means people can’t be abusive bastards, or something.
It’s not consent if there isn’t a real, informed choice, even if you technically did agree. We understand this about sex. It’s not “Yes” if “No” is not an option. And yet, medical professionals regularly will try to coerce and pressure you into letting them do things to your body, and often completely obscure the fact that a choice is available. “You have to do X,” they will tell me, conveniently leaving out the fact that no the fuck I do not.
“We recommend that you do X, here are the benefits and risks” is acceptable. “Our policy is not to do Y unless you’ve had X” is acceptable. But “you have to do X” is not, because it’s not true, because I can get up and leave at any second, watch me, I’ll do it right now. If you have a problem with that, well, your move. I spent 1.5 years in Krav Maga, I’m faster than you, and I bite.
If you bring this up to people they will be horrified, because there might be risks to refusing something recommended! People that otherwise perfectly understand consent often cannot understand this, and regress into the mindset of a Republican politician when you have this conversation with them. Suddenly, bodily autonomy does not matter, and actually other people should make the choices about your body because you might make the risky choice, and obviously you shouldn’t have the right to do that, even though it’s your body.
Let’s think about this. Let’s be thoughtful. Who will be healthiest in the long run, the person who learns that their feelings and choices matter in a doctor’s office and is able to build up a good relationship with medical professionals, or the person who experiences coercion and disrespect and ends up so psychologically fucked up that they avoid medical professionals even when they’re sick, in pain, and suffering?
My body is for me, you have access to it because you are PROVIDING A SERVICE TO ME. The moment you disregard my choices, you are no longer doing your job.
As far as I am concerned, it’s the same mistake people make with dogs. “No” is viewed as disrespect, just as a growl is viewed as disrespect. But “No” is polite. It’s “Here are my boundaries. You’re free to back off.” Instead of just, you know, biting.
89 notes
·
View notes
Text
the worst case scenario 2
i did decide to make this a little parter thing, but really want to be as sensitive as poss (honestly using this as a sort of therapy for what I see myself ah). So please do not read if anything in the warnings may trigger. I very much am not trying to ‘romanticise’ these sorts of situations in any way but also be aware medically this is NOT accurate.This part is short but I think there will be more.
warnings: hospital - ICU, respirators / mention of death , maternal mortality / talk of family dynamics and abandonment of a child
[previous part]
The sight Nikki walked into is something that as a parent you never want to see. Walking into this cold and otherwise empty ‘relatives room’ to see her son collapsed in a world of pain onto his best mates chest. Tom was too busy sobbing to even notice her entrance but her and Harrison instantly locked eyes . Not even able to muster up a greeting smile, Harrison just nodded her in, admitting her entrance to the most horrific situation.
It was about half an hour since she had been texting Haz, arranging when they’d be able to come and visit the newborn in hospital or whether it would be better to just wait till the new family got settled back at home, when Nikki had got a call from Tom’s number. With an excited grin she had instantly whipped her phone off the kitchen counter within one ring- a facial expression that didn’t last long at all.
Met with the distant sound of crying first, Harrison’s deeper voice then emitted itself from her phones speaker, alerting her to the fact everything was very not right. He’d asked her to come to the hospital, said it was Y/n, that the baby was fine and then hung up. Dom immediately agreed to come with her but right now he was still parking the car, having dropped Nikki off right at the front. It had sounded that bad.
Now, she knelt down infront of Haz and Tom, the latter who still was leaning over the arm rest and currently silently crying into his friends chest. Haz didn’t miss Nikki’s hands shaking as she reached out and rubbed up and down her sons back, the action prompting him to suddenly lean up to face her. He was broken. Totally and completely broken. Wordlessly, Nikki looked up for a second, communicating with Harrison so as if rehearsed he stood up and Nikki took his place in the chair - giving him a break from being Tom’s support. Beyond appreciative of how well Nikki could read a situation, Haz quietly but still in a hurried fashion made his way to the door.
Because he was about to crack too - Tom couldn’t see him like that, not right now at least. And so his legs, completely of their own volition, carried him down the hallways. He had absolutely no idea what time it was, all sense of time passing had completely been thrown off earlier in the morning. He was oblivious to a lot, very much in his own thoughts and only realised where he had ended up when a nurse he vaguely recognised managed to garner his attention.
“You’re here for baby Holland? She’s just round here.”
“I-“ He couldn’t respond but the nurse just nodded and then started off down the hallway, practically forcing the blonde to follow a couple of meters till they got to a perspex viewing window.
“She’s the little cutie in the far corner over there.” The brunette middle aged lady softly spoke as she pointed through the glass to the incubator in the corner. “ Don’t worry about all the equipment, the doctors already come round and cleared her. She’s good to go home when you guys are…are ready.” Her words had trailed off, Harrison guessed she didn’t know how to phrase the current ‘situation’ Tom and Y/n were in either. After a couple of moments, the nurse placed a gentle hand on Harrison’s shoulder, giving it a squeeze. “You want to have a cuddle? I know your not dad but…”
“Yeh-yeh…please.”
Harrison just felt awful. The little girl was barely hours into life and yet she wasn’t receiving nearly as much as love as she should be. Instead unnamed and alone in a cold and clinical setting. So he silently nodded away, taking in all the instructions the nurse gave as she sat him down in the arm chair next to the incubator.
Once she placed the little blanket wrapped bundle in his arms the nurse smiled gently up at Haz “You want to feed her? I’m sure she’d prefer it from you than me love?” Ah. Now Haz really was stuck between a rock and a hard place. She’d never been given a feed before - except presumably the midwifes.
“I-uh Y/n hasn’t even so I probably shouldn’t…”
“I can promise you Miss Y/l/n would probably want her baby to be cared for by someone that loves her and that Miss Y/l/n trusts herself.” Ooof. How were nurses so intuitive? She literally read his mind and broken down all the ill-founded ideas Harrison had built up.
“I’m not her Dad.”
“But you care.” Looking down once and briefly at the squished little face that wormed herself into Harrisons broad chest a little more, he then immediately nodded in agreement. Looking almost relieved, the nurse handed him a bottle and directed him as to how to hold it. After mere moments she gasped happily, leaning back whilst the blonde boy waited for her input.
“She’s latched on easy peasy. You’re doing great, I can leave you to it if you want - I’ll only be round the corner.”
“Can you check if there’s any news on Y/n?” The kind lady nodded, before promptly exiting the room - leaving the two actually alone for the first time ever.
He didn’t even think about it, whilst Haz cradled her in one arm and held the bottle up at the angle shown by the nurse, he quietly spoke to the little bundle.
“I’m sorry you were lonely… your mum and dad love you lots and lots… we all do.” Not realising he was crying, Harrison almost scared himself when a single strangled and repressed sob escaped from his chest. “ You’re mum…. She’s a pain in the arse right?” Haz laughed a little wetly “ She’s sarky as hell and she always has an answer… you’d probably think she’s a badass… she is. And-and…. Your dad is just scared… He loves you I promise, he just… he’s worried about you mum.” Now there was actual tears welling up and overflowing his lower lash line, not matter how much he tried to blink them away. “But whatever… whatever happens. You got all of us kiddo… you got me.”
Jolted out of his thoughts by the ladies knuckles rapping twice on the door, Harrison immediately shook himself out of it, wiping his face on his arm to hopefully remove all the evidence of the slight emotional breakdown.
“Mr Osterfield… the doctor wanted me to let you know he’s on his way to talk to Mr Holland.”
||||||||||||||||||||||||||||||
Harrison managed to get back to Tom, Nikki and now Dom before Dr Webber returned, so with a greeting nod to Dom he too took a seat opposite Nikki and Tom. His best mate wasn’t crying anymore, which could be considered a positive were it not for the sinisterly empty look in his eye. He looked almost robotic, staring almost straight ahead at the light grey wall, sat straight and rigidly except for his one hand clasped in Nikki’s.
“You went to see the baby?” Nikki broke the silence, making Harrison smile sadly over at her with a nod. It didn’t even look as though Tpm heard his mum speak, even if he was sat right next to her. “She’s okay?”
“Yeh…I gave her a bottle. She-she’s very cute.” Harrison could see Nikki’s face morph into one of kindness before she looked left toward her son. Nikki was still yet to see to unnamed girl but just thinking about her made her heart flutter. And then stop when she thought about what that little girl was already going through, barely hours into existence.
“You hear that Tom? Maybe you could go down and see her soon? After we’ve spoken to the doctor?” Nikki was only trying to do the best thing, Harrison knew it and deep down Tom did know it too. But now really really wasn’t the time for some gently encouragement from his mother, it wasn’t just Tom being a little stubborn. This was his whole entire world falling apart around him. He didnt have the energy or focus to even shoot down his mother, instead Tom chose to stay completely still - engrossed in his own thoughts.
From the outset, when you take that leap and say to a person ‘I think we should try for kids now’ you are completely putting yourself at the mercy of the other. But when they agree? Then it’s a commitment. Not it the same way marriage is - because that’s a completely selfish gesture, you get married because YOU want to be married to each other. Rather, agreeing to have a kid is a promise, a promise of something more. Promising that you are bringing this life into the world - and half of that life is yours. You create it together and it becomes a joint responsibility. You can never, no matter what people think, ever stop being a parent. At the end of it all there will be another person that knows, scientifically, it is half you. Even if they never met you - they still ‘knew’ you. They would know you had to exist, they would see things in themselves that cannot be explained rather than the influence of their creator.
And sure, it didn’t always work out that way. A parent would up and leave, a child always with questions and a sense of betrayal. But that child… they know you. Because there is half of you in them.
So it was Y/n and Tom together that was slumbering blissfully on a ward downstairs. That was the scary thing. Tom was so sure he didn’t have it in him. He wouldn’t do this without her. He couldn’t be a dad to a baby without a mum. He couldn’t be a parent without Y/n.
Almost thankfully for the atmosphere in the room, a soft know had them all snatching their heads up the very same grey slightly potato like doctor waddled in, this time followed by 2 others; a tall, dark haired woman with a soft and empathetic smile; then another man but this one tall and slender, unlike the other two who were wearing professional clothes, he was donned in scrubs (with the scrub hate too).
“Mr Holland and uh… family” Dr Webber awkwardly greeted the new arrivals of Nikki and Dom, somehow apparently sensing they were Tom’s and not Y/n’s parents who were hours away. Oh fuck, Tom hadn’t even phoned them yet.
“This is Dr Alison Goodwell and then Dr Rohan Avinash, he is Y/n’s surgeon.” They filed in and took seats surrounding them, Dom and Harrison standing up to stand off to the side, not wanting to get in the way of the doctors. All Tom could do though was overanalyse everything. Why was the surgeon here? What was this other lady doing here? A pathologist? — no, he wasn’t going to think like that. Then the taller and most scary looking of the three inched forward, commanding the attention of the whole room.
“Mr Holland, I just wanted to go over what happened. Ms Y/l/n developed plactental accreta, which was the cause of the what we call here a post partum haemorrhage. When you raised the alarm she had already lost, at best guess, 3 pints of blood which is a lot, there’s no denying. Dr Webber and his team quickly brought her up to my team in surgery. We transfused her with blood but we couldn’t stabilise her and the bleeding didn’t show any signs of stopping so we had to perform emergency surgery….” Dr Avinash slowed down as he took in how close Tom looked to bursting out in tears once again, offering him the chance to have a moment to collect himself. Vehemently shaking his head in refusal, Tom crung his hands together furiously. He just needed to know. “Okay… Now the nature of the surgery, because we had to be so quick…it is quite invasive and is a lot of stress to put on anyones body. That and the amount of blood she had already lost makes the situation very dangerous. Sometimes when this happens a persons heart-“ Tom’s breath halted in his throat at the mention of her heart, Harrison sharing the bleak trigger which made him shift uncomfortable between his two feet. “-notices this, it goes into what we call hypovoloemic shock, this just basically means its not getting enough volume of blood to pump properly. So we have had to stimulate Ms Y/l/n’s heart with electricity to keep it pumping-“
“You shocked her?” He felt so numb and now adrenalin was coursing through his own veins, images like you see on TV shows of her body arching up not he table from the volts of electricity.
“I’m afraid we did have to but it meant we could keep her stable enough to fix the bleed. I am sorry to say this but we’ve had to remove her whole womb because it was so damaged.”
“But Y/n?” Again Harrison lost all willpower of control, though to be fair he wasn’t sure if he was being impatient or not - this doctor appeared to be delivering this news painfully slowly, as if to torture everyone as much as possible.
“Your fiancé lost a lot of blood and her body went through a lot” The towering doctor kept his focus on Tom the whole time, Harrison’s interjection seemingly falling on selectively deaf ears. “We’ve had to use a machine to control her breathing and for the moment she is still in a very dangerous place. Right now she is stable but I don’t want to make any promises to you. We are nowhere close to out of the woods yet.” Seemingly, feeling compelled to add in, the brunette doctor spoke for the first time since entering.
“But it’s still one hurdle she has got through… Now that the surgeons are finished with Ms Y/l/n me and the other intensive care doctors will be keeping a very close eye on her okay? We are all going to be working with you and your family 24/7, to keep Y/n as comfortable as possible.” Her soft smile managed to somehow break through to Tom, who jerkily nodded while Nikki squeezed his hand tight. There had been a lot of that going on today and even if Tom would say he wished nothing more that it was Y/n rather than his mums grip - he still appreciated it. The doctor continued, leaning forward so her elbows were resting on the tops of her thighs. “Right now she’s asleep and probably will be for quite a while. We first want to be sure she’s not in any pain, so she is sedated. Now assuming everything goes okay tonight and she stays stable we might want to think about possibly reducing that sedation, however for right now I hope you are all in agreement that we just want to make sure she’s comfortable?” The whole room nodded steadily in response which the doctor acknowledged with a satisfied smile.
“And we are all aware this is a lot to take in so if you have any questions or think of any please just let us know - it’s important that you guys are all fully in the know… How is your daughter?” Dr Webber started off so well, Tom was almost going to smile thankfully at him, until he mentioned it. Instantly, the cold and empty look reappeared behind Tom’s eyes as the room was held in silence for long enough to be uncomfortable. To be fair, the doctor wasn’t to know that recently Tom had taken to refusing to acknowledge he even had a child.
“I-she’s really good… the nurse there said she’s ready to leave whenever” Harrison had to show that at least someone was looking out for her, he couldn’t not.
“Okay” sharing a knowing look with Harrison, Dr Webber pitifully clasped his hands together, before looking back to Tom. “Would you like Dr Alison take you up to see her, sir?”
again pls let me know if anyone is very not okay with this, i can take it down and not write any more!
157 notes
·
View notes
Photo

Regular Exercise May Help Protect Against Severe Covid
More exercise means less risk of developing severe Covid, according to a compelling new study of physical activity and coronavirus hospitalizations. The study, which involved almost 50,000 Californians who developed Covid, found that those who had been the most active before falling ill were the least likely to be hospitalized or die as a result of their illness.
So, for the new study, which was published Tuesday in the British Journal of Sports Medicine, researchers and physicians at Kaiser Permanente Southern California, the University of California, San Diego, and other institutions decided to compare information about how often people exercised with whether they wound up hospitalized this past year because of Covid.
Now, the researchers drew anonymized records for 48,440 adult men and women who used the Kaiser health care system, had their exercise habits checked at least three times in recent years and, in 2020, had been diagnosed with Covid-19. The researchers grouped the men and women by workout routines, with the least active group exercising for 10 minutes or less most weeks; the most active for at least 150 minutes a week; and the somewhat-active group occupying the territory in between.
The researchers gathered data, too, about each person’s known risk factors for severe Covid, including their age, smoking habits, weight, and any history of cancer, diabetes, organ transplants, kidney problems and other serious, underlying conditions.
Then the researchers cross checked numbers, with arresting results. People in the least-active group, who almost never exercised, wound up hospitalized because of Covid at twice the rate of people in the most-active group, and were subsequently about two-and-a-half times more likely to die. Even compared to people in the somewhat-active group, they were hospitalized about 20 percent more often and were about 30 percent more likely to die.
Of the other common risk factors for severe disease, only advanced age and organ transplants increased the likelihood of hospitalization and mortality from Covid more than being inactive, the scientists found. “Being sedentary was the greatest risk factor” for severe illness, “unless someone was elderly or an organ recipient,” says Dr. Robert Sallis, a family and sports medicine doctor at the Kaiser Permanente Fontana Medical Center, who led the new study. And while “you can’t do anything about those other risks,” he says, “you can exercise.”
Of course, this study, because it was observational, does not prove that exercise causes severe Covid risks to drop, but only that people who often exercise also are people with low risks of falling gravely ill. The study also did not delve into whether exercise reduces the risk of becoming infected with coronavirus in the first place.
But Dr. Sallis points out that the associations in the study were strong. “I think, based on this data,” he says, “we can tell people that walking briskly for half an hour five times a week should help protect them against severe Covid-19.” A walk — or five — might be especially beneficial for people awaiting their first vaccine, he adds. “I would never suggest that someone who does regular exercise should consider not getting the vaccine. But until they can get it, I think regular exercise is the most important thing they can do to lessen their risk. And doing regular exercise will likely be protective against any new variants, or the next new virus out there.”
By Gretchen Reynolds (The New York Times).
77 notes
·
View notes
Text
shinrin-yoku (Ethan x MC)
Book: Open Heart
Pairing: Dr Ethan Ramsey x F!MC (Dr Noelle Valentine)
Word Count/Rating: ~1.7k, PG
Summary: When life's difficulties hit, Noelle navigates her way through them by turning to the nature.
Category: Hurt & Comfort
Warnings: mentions of trauma
A/N: May is a Mental Health Awareness month and here in the UK the theme is nature. My MC, just like me, runs to the woods when things get tough. It helps her clear her head and reconnect with inner strength.
I struggle with mental health myself and it’s important for me to speak up and address the subject. There is nothing worse than shaming or discrediting someone’s difficult feelings. It’s fine not to be fine.
If you struggle alone, please don’t. My inbox will welcome you with open arms. Two heads are better than one, even if we just complain, at least we can complain together 💜
For @choicesmaychallenge2021 Day 13 - Mental Health

SHINRIN-YOKU - A Japanese term for ‘forest bathing’ or the sense of well-being you experience while in nature.
~~
It all starts with a seed.
This tiny element which, without aid, is sentenced to certain death.
But give it the right soil.
Give it water, sun.
And it can grow.
Into something big.
Powerful.
Scary.
~~
She is five years old.
They live in a townhouse, a classy Victorian era building. Undistinguished, one of many merging into the background of a typical London street. The colors are also very standard, dirty white married to ivory beige, bar for the deep green door - their rebel child.
For the random passerby, it’s nothing special.
But for her, the walls of a storey house encapsulate the whole world.
The garden behind the house is neat and clean, visibly well taken care of.
She doesn’t remember exact details anymore, but she remembers begging her parents to go camping in the garden with her brother.
The ticklish feeling of long and slim blades of grass on her tiny feet.
Looking at the stars with pure awe and delight, that only the unspoiled mind of a child is capable of.
The plot of land that the house has been built on borders a beautiful forest. A wooden fence separates the two.
To her, it’s a passage to a magical world.
A world without any particular order, living its own life, unconstricted by rules.
Not in the slightest does it resemble the garden on her side of the fence, where things grow according to the rules laid out by the adults.
There is a feeling inside her that she’s too young to name, to throw it in lingual context.
It’s not until years later that she realized what it had been.
Freedom.
To grow however you please.
To be what you want to be.
Robust, effuse trees tower over her, making her feel so small.
As if she hasn’t already been feeling small enough, living in a world full of giants.
But they mean something else too.
They bring a secret and a promise.
Promise of a bigger world out there, far from the confines of the place she calls home.
The forest draws her, singing a melody that only her heart can understand.
One day, she will be a part of it.
~~
She lives the teenage dream life.
That’s what everyone says.
She doesn’t have any real problems.
She’s lucky not having to worry about money.
She’s got friends.
Her family is great.
She just needs to stop whining.
Her life is perfect.
Their words, not hers.
None of them know what happens behind closed doors.
The childhood forest is a cloudy memory.
Her home is now thousands of miles away, in a city with a giant red bridge, which for some bizarre reason has ‘golden’ in its name.
But the call from nature doesn’t care about distance.
It can find you about anywhere.
It’s different and yet the same.
Because nature beats in one rhythm and speaks in the same language, everywhere.
The morning is chilly and humid.
She’s wearing a wooly coat, carelessly threw on a pair of PJs hiding underneath.
Her steps are brisk, breathing short and heartbeat elevated.
Something’s bothering her blanched face.
The voice, again.
When it first appeared, she thought it had her best interest at heart. Used to give her advice and like a good friend, ream her out when she did something bad.
Over time, things took a turn for the worse.
Snarky comments. Casually mentioned wrongdoings. Feedback on what she could have done better, differently.
Noelle hoped the voice would go away on its own.
It hasn’t.
Not only did the voice not go away, but it was actually growing stronger with each passing day. Became more vocal. Judgmental. Openly hostile.
It fed on her fears.
It’s your fault - it told her - that your parents are getting divorced.
You are not good enough.
Even a lie, repeated enough times, will finally become the truth. And so it did for her, to the point where she couldn’t distinguish her own voice from the voice of the tormentor. Sounds faded into one.
Whoever said words can cut like a knife was right.
But those who knew thoughts could leave scars that are much deeper, were truly wise.
The young, beautiful girl who never hurt a soul, became a hostage.
A prisoner locked in the jail of her own head.
A giant tear rolled down her face.
Made of all the words her heart couldn’t say.
She hugged the tree tightly and inhaled the woodsy aroma, the scent filling her lungs fully.
It’s sensuous.
Just like that, she is small again.
~
She’s got all that she ever wanted.
Degree from one of the best medical schools.
Graduating with honors and glowing recommendations from even the strictest professors, who kept assuring her that her future in medicine is so bright it’s actually blinding.
Then, a dreamy residency in one of the most prestigious hospitals in the country.
Pretty impressive, right?
Even a fool could see that.
But the only fool whose opinion she cared about, couldn’t.
All these things were clearly not good enough for Ethan Ramsey to stay.
She wasn’t good enough for him to stay.
Not longer than a year ago he was just a concept, an ideal without a face, body and voice. To her, he was a celebrity, a hero, someone whom mortals don’t have access to.
It was preposterous to consider for even a second Dr Ramsey could actually see something in an intern.
Standing among the moss-covered trees, every fiber of her being was filled with the thought of him.
Did the Amazonian forest remind him of her, just like every forest around reminded her of him?
Just when she won the battle for her career, she lost another.
Because life had to be a zero-sum game.
As painful as that would have been, she wished she had something to hold onto.
A scene she could replay in her mind.
An image of him walking away.
Or saying goodbye.
But he left without a word.
That was the pattern. That was history repeating itself.
She took her shoes off and stepped on the soil frosted with morning dew. It’s cold and wet.
It’s refreshing.
She is grounding.
Reconnecting with Earth.
Tunes in with the rivers of grass, towers of trees, fences of bushes.
If the trees could speak, they’d tell stories not many people would believe in.
Tales of heartbreaks.
Parables of spirits.
They are all nature’s poems.
Hauntingly beautiful.
Riveting.
Written without a single word.
Because nature speaks its very own language that only the soul, not the mind, can understand.
Pain is ripping her apart.
But it reminds her that she’s alive.
And this, in itself, is a miracle.
~~
She doesn’t know who she is anymore.
Some people call her a survivor.
But it doesn’t feel like the right word.
So many things in her died.
So much was lost.
The attack took a lot from her.
Danny. Bobby.
Sense of security.
Identity.
Direction.
Right and wrong, good and bad, righteous and vicious.
These are all just words.
Someone needs to come and teach her the meaning of them anew.
Draw lines, mark out frontiers.
Save her from herself.
The ground is soaked. Torrential rain turned the soil into soft mud, warm and easily slipping through her fingers. She falls on her knees, praying for the ground to consume her.
Fill every part of her.
Silence the internal cacophony.
To sink into oblivion.
Not many people knew about the panic attacks and recurring nightmares. They’re always the same.
She’s standing in the middle of a swamp.
Danny and Bobby are drowning, their arms reaching out for her.
She knows she can only save one of them.
She runs out of time trying to figure out how to save both.
As a result, they both die.
Time stands still and yet everything is spinning, moving, racing.
The reality is a riot of overbright colours.
Suddenly, a ring breaks the silence. A polyphonic intruder. She looks at the screen through hooded eyes and notices the caller’s name. It’s him. He’s petrified. Worried to death. Asks her to stay where she is.
Some time later, maybe 10 minutes, maybe an hour - who knows? - he emerges from the gathering of stocky oaks.
The moment he catches the sight of her, he starts running. She notices a lab coat underneath the jacket.
He’s soaking wet.
Even though he is so close, he doesn’t slow down.
Crashing into her, he scoops her in his arms.
Catches her in the tightest of embraces.
Asks her if she’s fine.
No. Not that question again.
She’s tired of people fussing over her and gets angry.
Had it not been for the attack, would he even be here? The voice asks mockingly.
It doesn’t matter to her.
He’s there now.
Deep baritone is gentle and full of concern.
It’s not like that. It’s not his intention to fuss.
He’s simply worried.
Because she is the most important thing to him in the whole world.
Yes, he wasted so much time.
That’s why he refuses to lose even one more second.
A dam breaks within her.
Eliciting a quiet sob.
She clutches his shirt, holds onto him for dear life.
Moments later, she’s screaming at the top of her lungs.
Singing her poignant birdsong.
How is she supposed to cope?
Will things ever go back to normal?
What is normal anyway?
In the confines of the infamous patient room she never felt more scared in her life.
But here, out in the open, she feels so safe.
As if she’s had a silent agreement with nature, which vouched to protect her at all costs.
And this time, nature had an ally.
Because Ethan will protect her, even if it’s the last thing he does.
Holding onto each other, they stand in the nothingness.
It keeps them grounded.
Connected to their roots.
Turning over new leaves.
Bending before they break.
Growing.
They get lost.
Mother Nature has a reward for those who do.
They have a chance to find themselves.
Over and over again.
~~~
If you made it this far - thank you & you're awesome 🥰
Tag list: @genevievemd @gryffindordaughterofathena @terrm9@starrystarrytrouble @the-pale-goddess @jamespotterthefirst @lisha1valecha @writer-ish @maurine07 @drakewalkerfantasy@iemcpbchoices @liaromancewriter @lem-20 @lucy-268 @oldminniemcg @queencarb @qrkowna @mercury84choices @lsvdw-blog @utterlyinevitable @stygianflood @udishaman @romewritingshop @romereadingshop @alina-yol-ramsey @stateofgracious @xxsugarplumfluffsxx @binny1985 @tsrookie @fayeswiftie @archxxronrookie @tinkertailorsoldierspy @schnitzelbutterfingers @wingedhairstylemusicweasel @theinvisibledreamergirl @custaroonie @irisofpurple @chasingrobbie @ethandaddyramseyx @quixoticdreamer16 @coffeeheartaddict @takemyopenheart @aworldoffandoms @potionsprefect @choicesficwriterscreations @openheartfanfics
#open heart#Ethan Ramsey x mc#choices fic writers creations#fics of the week#mental health awareness
56 notes
·
View notes
Text
distance
Yuukoku no Moriarty | SherLiam | Pandemic (AO3)
MTP Angst Week 2021 - Day 7: Free
-
The past few days had truly been harrowing, even for Sherlock.
As if the hospital filling to over-capacity hadn’t been enough, the sudden lockdown had also pretty much driven everyone mad, what with all the panic-buying and incidents of looting all around. John hadn’t taken kindly to the impatient jerk in the waiting area who likened the current events to a warzone, but hadn’t really disagreed, either. Patients were still patients, after all, no matter how badly a doctor felt about them.
Liam only chuckled in amusement when Sherlock ranted about the incident over the phone later that evening. “Dr. Watson was a former army medic, after all,” he reminded gently, before being consumed once more by a fit of coughing. He was definitely getting worse, but still insisted that he could take care of himself alone in their flat somehow. As much as Sherlock would have liked to get him admitted to the hospital, he couldn’t go home at the moment, either, having taken over Liam’s shifts instead.
“Fine, I get it,” Sherlock conceded as soon as Liam finally quieted down, his ragged breathing over the speaker filling the dead air in the darkened call room. It would certainly have driven anyone else mad with worry, but not them— not now, not yet. “I’ll keep calm and carry on. You take care of yourself, okay?”
Sherlock was lying about being calm, of course, and Liam knew it. “I will.”
.
Zoom wasn’t exactly to blame, but Sherlock hated not being able to read Louis like a book.
The Moriartys’ video glitched once more, and Louis turned the camera off with a grumble. Albert’s warm baritone still carried over despite the spotty audio quality, however, and Liam brightened considerably at the mention of a care package on its way from London. “There’s also a pack of toiletries in there for Mr. Holmes, should he need them.”
“Only the bare minimum, of course,” Louis added with contempt. He still hated the idea of his brother getting together with Sherlock for the longest time, but it wasn’t as if he could chase them all the way up to Durham right now. In hindsight, maybe he should have taken the time to know the younger Moriarty better then before all this happened. “That’s okay,” Sherlock answered, overlapping with Liam’s “It’s all right, I’ll just add more from our supplies here at home.”
Sherlock couldn’t tell from the awkward gasp that followed if Louis was still being hostile. He evidently wanted to say more in protest, but just then the free plan’s forty minutes were up, and the call cut off by itself. Technology, for all its advancements, still had many frustrating limitations, and the steadily increasing mortality census on the ER boards were proof of that.
.
Miss Hudson, on the other hand, was a lot easier to calm down, though still evidently frustrated at being the only one in their friend group left behind in London. “You guys should seriously take care of yourselves! I’ve seen it on the news; more and more people are getting sick!”
John only laughed nervously from his FaceTime screen, exchanging a worried glance with Mary beside him. Despite the sharp drop in elective surgeries the past few days, the couple still remained busy as ever, answering the call for redeployment to the overburdened and understaffed hospital frontlines. To their credit, both were adequately experienced and competent as general practitioners, making Sherlock’s work easier by leaps and bounds.
They were both literally in the adjacent call room right now, making Sherlock wonder if Miss Hudson was actually jealous of that, too. He, for one, was petulantly so, having not gone home to Liam for a week and a half now— not that he would admit to that, though.
He was starting to hate all of this, to be honest. Consecutive shifts, lockdown, quarantine, Liam getting sick—
“Hey. Are you even listening, Sherlock?” Miss Hudson was frowning at him through her screen, while three sharp knocks were made on his door. John’s eyebrows were likewise furrowed even through the safety goggles he had hastily put on, and Sherlock did not want to figure out what expression he must have beneath that N95 mask. “You really should go home, Sherlock. Mary went to HR to get your forms.”
The very insinuation of rest sapped away at the little remaining energy Sherlock so desperately tried to hold on to, and he staggered forward into John’s waiting arms. “It’s complicated,” he muttered weakly before passing out.
.
Sherlock barely registered the short drive home, his mind preoccupied with worry over Liam’s condition. The worst of it was fortunately already over, but he still wasn’t well enough to return to work.
He had been working the ICU shift when Liam had called in sick over a fever and moderately productive cough that had developed overnight. Sherlock had immediately feared the worst, recalling the patient with critical pneumonia who had expired a few days earlier; it was Liam who had intubated her at the ER.
The test came out positive; of course it would. “A necessary hazard, really.” It did not reassure Sherlock one bit.
In hindsight, the arrangement they had decided on was reckless and irresponsible, with Liam isolating himself in their flat and Sherlock living in the hospital, taking on Liam’s shifts as well to make himself useful. He had never cursed the lack of mobile phone signal there as much as he had the past few days, only being able to call Liam by the window at the call room for a few minutes every night.
John called Sherlock out on it when he found out. It was a good thing Albert and Louis didn’t find out even after all those Zoom calls. God forbid Mycroft even hears a word of it.
Liam met them at the front door when they arrived, a little more color now returned to his face compared to last week. “He’s just exhausted,” John assured, helping tuck Sherlock into the newly-made bed. The rest of their room had been cleaned up, too; Liam had been taking care of himself better than he’d feared, after all.
As soon as John saw himself out, Sherlock felt a weak slap to his forehead, followed by long, thin fingers brushing his bangs out of his face. “Still a handful, as always, Sherly.” Liam was nothing but affectionate beneath his admonishing tone, and he was definitely smirking behind the mask he wore.
“Go back to bed,” Sherlock mumbled, unwilling to move any part of his body at the moment. As much as they both wanted to take care of each other right now, neither of them were well enough for it yet. Between them both, at least Liam could now carry on with the house chores and outside affairs, so that’s one less worry off his mind.
He felt Liam’s damp face mask softly touch his forehead in a kiss, which was immediately wiped away and replaced with a cooling pad. “I will, dear. Text If you need anything; I’ll be outside.”
Sherlock lifted his blanket over his face to hide a rising blush, despite the mask he was already wearing. Awfully sneaky of Liam; he really is doing better.
.
“Remind me how we got together again,” Sherlock murmured over the phone, looking out the bedroom window. There was a nice, cool breeze, and the stars were especially beautiful. The street below was eerily empty, with the sidewalk lamps turned on to the lowest setting. It made for an overall quiet night unusual in this day and age, and he found that he liked the silence more than he thought.
To his left, Liam sat on the kitchen balcony, phone also in hand, a thin shawl draped over his nightshirt and pyjamas. “I don’t believe there was an exact moment, if you ask me,” he answered fondly, warm red eyes flitting over to meet Sherlock’s gaze. “It simply just happened.”
It wasn’t really much of an answer, but Sherlock did not disagree at all. Theirs had always been a subtle friendship, so it came as no surprise to them the moment everything clicked and fell into place. But none of that mattered to them, in the end. They both just knew, and it was enough.
Sherlock settled for a satisfied hum, cradling his phone between his neck and shoulder as he watched Liam do the same. “I was scared to death,” he confessed, eyebrows furrowing mournfully once more. “It was hard, always fearing the worst everyday. Overworking myself helped take my mind off things. Kind of.” He laughed to himself, stretching a hand out the window to touch the balcony ledge. “And now I’m relieved. A little ill, but relieved nonetheless.”
Liam moved closer, as well, taking Sherlock’s outstretched hand and threading their fingers together. “It was the same for me, Sherly. It may just have been a week in isolation, but everyone’s calls kept me from falling into utter despair. I was most worried that you’d also catch it while working, and that you would…”
Oh, how he wished he could kiss Liam right there and then. The current state of world affairs didn’t allow for it, however. Not in the next few weeks, it seemed.
So they quietly stayed that way for a few more moments, not letting go despite the growing soreness in both their arms. They will have to rethink their work schedule by tomorrow morning. There will be more compromises, more risks, more looming crises. More grief and pain and loss all around. “It will be difficult.”
A rueful smile, the first of many to come. “Such is the life we chose.”
For now, though, they have this night to cherish, and to look back on in the coming days. It will have to be enough.
-
Cardiorenal Syndrome and Other Stories
#yuukoku no moriarty#yuumori#moriarty the patriot#mtp angst week 2021#sherliam#sherlock holmes#william james moriarty#hospital AU#Medical AU#pandemic#isolation#phone/video calls#overworking#light angst#hopeful ending#crs etc
15 notes
·
View notes
Text
STORY AT-A-GLANCE
Within weeks of the pandemic outbreak, it had become apparent that the standard practice of putting COVID-19 patients on mechanical ventilation was a death sentence; 76.4% of COVID-19 patients (aged 18 to 65) in New York City who were placed on ventilators died. Among patients over age 65 who were vented, the mortality rate was 97.2%
The recommendation to place COVID patients on mechanical ventilation as a first-line response came from the World Health Organization, which allegedly based its guidance on experiences and recommendations from doctors in China. But venting COVID patients wasn’t recommended because it increased survival. It was to protect health care workers by isolating the virus inside the vent machine
Data suggest around 10,000 patients died with COVID in NYC hospitals after being put on ventilators in spring 2020. Other metropolitan areas also saw massive spikes in deaths among younger individuals who were at low risk of dying from COVID. It’s possible many of these deaths were the result of being placed on mechanical ventilation
The WHO must be held accountable for its unethical recommendation to sacrifice suspected COVID patients by using ventilation as an infection mitigation strategy — especially considering they’re now trying to get unilateral power and authority to make pandemic decisions without local input
Showing how the WHO’s recommendation to put patients on mechanical ventilation resulted in needless death among people who weren’t at great risk of dying from COVID is perhaps one of the most powerful talking points a country can use to argue for independence and rejection of the WHO’s pandemic treaty
Within weeks of the pandemic outbreak, it had become apparent that the standard practice of putting COVID-19 patients on mechanical ventilation was a death sentence.1
By early April 2020, many doctors were already questioning their use, as data2 showed 76.4% of COVID-19 patients (aged 18 to 65) in New York City who were placed on ventilators died. Among patients over age 65 who were vented, the mortality rate was a whopping 97.2%.
If you were older than 65, you were 26 times more likely to survive if you were NOT placed on a vent.3 A small study from Wuhan, China, put the ratio of deaths at 86%,4 and in Texas, 84.9% of patients died after more than 96 hours on a ventilator.5
In a widely-shared YouTube video6 (above) posted March 31, 2020, Dr. Cameron Kyle-Sidell, a critical care specialist at the Mount Sinai Health System in New York, warned that “we must change what we are doing if we want to save as many lives as possible.” Sidell was adamant that doctors were “treating the wrong disease” and that putting COVID patients on mechanical ventilation was all wrong.
“We are operating under a medical paradigm that is untrue,” Sidell said. “I fear that this misguided treatment will lead to a tremendous amount of harm to a great number of people in a very short time … This method being widely adopted at this very moment at every hospital in the country … is actually doing more harm than good.”
Why Were COVID Patients Put on Vents?
The recommendation to place COVID patients on mechanical ventilation as a first-line response came from the World Health Organization,7 which in early March 2020 published a COVID-19 provider guidance8 document to health care workers, based on experiences and recommendations from doctors in China.
According to the WHO, treatment needed to be rapidly escalated to mechanical ventilation. Ideally, patients should be placed on it immediately.9 What escaped the public was the primary reason why. Venting COVID patients wasn’t recommended because it increased survival; rather, it was to protect health care workers by isolating the virus inside the mechanical vent machine.
Using less invasive positive air pressure machines could result in the spread of infectious aerosols, the WHO warned. In other words, they put patients to death to “save” staff and other, presumably non-COVID, patients. That ventilation and sedation were used to protect hospital staff was highlighted by The Wall Street Journal in a December 20, 2020, article,10 which noted:
“Last spring, doctors put patients on ventilators partly to limit contagion at a time when it was less clear how the virus spread, when protective masks and gowns were in short supply.
Doctors could have employed other kinds of breathing support devices that don’t require risky sedation, but early reports suggested patients using them could spray dangerous amounts of virus into the air, said Theodore Iwashyna, a critical-care physician at University of Michigan and Department of Veterans Affairs hospitals in Ann Arbor, Mich.
At the time, he said, doctors and nurses feared the virus would spread through hospitals. ‘We were intubating sick patients very early. Not for the patients’ benefit, but in order to control the epidemic and to save other patients,’ Dr. Iwashyna said. ‘That felt awful.’”
As dryly noted by James Lyons-Weiler in a January 23, 2023, Substack article,11 “euthanizing humans is illegal. Especially for the benefit of other patients. It should feel awful.”
Fauci Knew Vents Did More Harm Than Good
youtube
Even Dr. Anthony Fauci, in a mid-June 2022 lecture (above), admitted that placing patients on mechanical ventilation did more harm than good.
“We very, very readily would put people on mechanical ventilation, when we found out, through clinical experience, it might have been better just to make sure we positioned them properly in the prone or supine position, and not necessarily to intubate someone so readily, which might have actually caused more harm than good. We learned that as we got more experience.”
Yet government treatment guidelines, to this day, include invasive mechanical ventilation.12 If the White House Coronavirus Task Force knew in the summer of 2022 that venting patients caused more harm than good, why didn’t they instruct hospitals to stop using it? Or at bare minimum, strongly advise against it?
And why did the government continue to financially incentivize the use of mechanical ventilation after they’d realized how bad it was? While many hospitals did cut down on their use of mechanical ventilation toward the end of 2020 and beyond, it still hasn’t been entirely replaced with noninvasive strategies shown to be far more effective.13

Download this Article Before it Disappears
Download PDF
Many ‘COVID Patients’ Didn’t Have COVID
The matter becomes even more perverse when you consider that many “COVID cases” were patients who merely tested positive using faulty PCR testing. They didn’t have COVID but were vented anyway, thanks to the baseless theory that you could have COVID-19 and be infectious without symptoms.
Hospitals also received massive financial incentives to diagnose patients with COVID — whether they had it or not — and to put them on a vent. They also received bonuses for using toxic remdesivir, and they were paid for each COVID death as well. The entire system was set up to reward hospitals for misdiagnosing, mistreating and ultimately killing patients.
China also benefited from the WHO’s misguided advice. While the U.S. clamored for more ventilators, Chinese hospitals started relying on them less and instead they were being exported in huge quantities.14
How Many COVID Patients Were Killed by WHO’s Bad Advice?
Just how many COVID-19 patients were killed by being placed on mechanical ventilation in the spring of 2020? That’s a question attorney and author Michael P. Senger tries to answer in his May 25, 2023, article “The Great COVID Ventilator Death Coverup.”15 He writes, in part:
“... the establishment is trying to argue that while ventilators were overused in spring 2020, doing more harm than good ... the ventilators themselves did not kill anyone.16 An astonishing argument, even by the abysmal standards of the COVID era.
But, since everyone supporting this narrative is arguing that there were no ventilator deaths in spring 2020, all we have to do is prove there were a significant number of ventilator deaths and what’s left of the establishment’s credibility on the initial months of COVID falls apart.
In addition to the anecdotal evidence ... several unsettling data points have long strongly suggested that there weren’t just some ventilator deaths in spring 2020, but rather a pretty frightening number of them ...
The CDC reports17 that 18,679 patients died with COVID in New York City hospitals throughout spring 2020. And, according to the sample in JAMA,18 just over half of those who died with COVID in NYC hospitals were put on ventilators. Accordingly, around 10,000 patients died with COVID in NYC hospitals after being put on ventilators in spring 2020 ...
Additionally, as Jessica Hockett has documented19 in meticulous detail through multiple methods, New York City experienced a sharp, breathtaking mortality event just after its lockdown and response to COVID began, which was unlike that experienced anywhere else or at any other time.
Given its singularity, this horrifying mortality event, quite simply, cannot be attributed to natural causes. Jumping off Hockett’s work, below is a chart of weekly all-cause hospital inpatient mortality from January 2018 through April 2023, split between patients ages 65+ (blue line) and patients under 65 (red line).
This spike in inpatient hospital mortality in New York City in spring 2020, especially among young people, is unparalleled in any other time period, even as COVID deaths supposedly began to climb again in 2021.”
Inpatient Mortality Around the US, 2020 Through Present
Senger goes on to show the same all-cause mortality graphs for hospital inpatients for each of the largest cities in the U.S.: Chicago, Dallas, Houston, Los Angeles and Washington, D.C. All show massive spikes in hospital deaths, especially among the elderly (65 and older), around the same time periods as NYC. He also produced charts for deaths on the state level, as follow:20
A Strawman Argument
Senger continues:21
“A couple of points on these charts. First, while the spike in mortality in the NYC area in spring 2020, especially among young people, is without parallel, it’s not the only one we see.
These spikes in mortality among young people are conspicuous because it’s long been known that COVID’s infection fatality rate (IFR) is extremely skewed toward the elderly. This, for example, is the most widely-cited data on COVID’s IFR by age:22

Thus, these spikes in mortality among young people cannot be attributed to COVID. Most notably, a significant spike in mortality appears among all age groups in California at the end of 2020 ...
One possibility is that, while the use of ventilators was generally scaled back, hospitals in California may have still been engaging in broad intubation or other iatrogenic practices by the end of 2020 ...
Even more strangely, Texas experienced a surge in deaths among young people in summer 2021 that was not accompanied by a corresponding increase in mortality among the elderly; this, frankly, may have had nothing to do with COVID.
That said, the fact remains that the New York area experienced a uniquely sharp, awful mortality event in spring 2020 which is not adequately explained by any of these other factors.
And doctors were under significant pressure to put patients on ventilators in spring 2020, even if it was merely unconscious; politicians had purchased tens of thousands of ventilators at exorbitant prices, and hospitals did receive more funding if patients were placed on ventilators.
Coupled with the above anecdotes about patients being placed on ventilators for extended periods to protect staff — and the fact that over 10,000 patients in New York City died after being intubated — it’s clear that a horrifying number of patients were likely killed by mechanical ventilators.
Yet astonishingly, despite all these facts, the establishment is arguing that no patients were killed by ventilators in spring 2020. This, to me, is the kind of implausible, overly-defensive argument one makes when they’re panicked.
Across America, tens of thousands of patients were placed on ventilators in spring 2020; given the vast majority of those patients died, it simply begs credulity that none of them were killed by ventilators.
When a deadly procedure is applied to tens of thousands of patients, even a baseline level of human error would imply that the procedure was applied to at least some fraction of those patients by mistake.
The establishment has responded with subsequent studies23 claiming to show that ‘early intubation’ actually reduced the time patients spent on ventilators, and thus didn’t kill any of them. But this is a straw-man argument ...
[T]he issue isn’t whether patients were intubated ‘early’ or ‘late’ relative to any symptoms they might have shown — the issue is whether patients were placed on ventilators who should have never been on them to begin with, or otherwise kept on them too long.”
A Morally Indefensible Coverup
Senger points out that, in speaking with other attorneys, most agree that hospitals face virtually no risk of litigation over ventilator deaths, for the simple reason that everyone perceived COVID to be a global emergency, and during emergencies, you just do the best you can with what you have and what you know.
“Regardless of how much harm was done, it’s simply too difficult to prove that the procedure violated the emergency standard of care given the information coming from China at the time,” he writes.
Even so, “the situation is morally inexcusable,” Senger says, adding that we do need to get to the bottom of how and why these patients died. I agree. While Senger wants the truth to understand what happened and to honor the diseased, I would add that we need the truth in order to avoid making the same mistake again, because there will be a next time.
The WHO Must Be Held to Account
The WHO must be held accountable for its unethical recommendation to sacrifice suspected COVID patients by using ventilation as an infection mitigation strategy — especially considering they’re now trying to get unilateral power and authority to make pandemic decisions without local input.
Showing how the WHO’s recommendation to put patients on mechanical ventilation resulted in needless death among people who weren’t at great risk of dying from COVID is perhaps one of the most powerful talking points a country can use to argue for independence and rejection of the WHO’s pandemic treaty.
They simply cannot be trusted to make sound medical decisions for the whole world. No one is. We need to allow local medical experts to make the calls in situations like this, and to collaborate and share information between themselves. The top-down one-size-fits-all medical paradigm that the WHO wants to implement is nothing short of disastrous, and the COVID pandemic response proves it.
Also, let’s not forget that the misuse of mechanical ventilation created the appearance that COVID was exceptionally deadly, regardless of your age, which in turn helped promote acceptance of the experimental COVID shots that are now a leading cause of frequent sickness, chronic disability and excess deaths. Of course, that’s also being covered up.
In the final analysis, the WHO’s handling of the COVID pandemic will undoubtedly go down as the worst in medical history. Can we really trust them to make better decisions in the future?
I think not, which is why we must do everything in our power to prevent the U.S. from signing the pandemic treaty. Better yet, we need to exit the WHO entirely. To that end, I urge you to contact your local House representatives and Senators and urge them to:
Support the No WHO Pandemic Preparedness Treaty Without Senate Approval Act24,25,26,27,28
Withhold funding for the WHO
Support U.S. withdrawal from the WHO
7 notes
·
View notes
Text
More than 600 babies have been born prematurely and needing critical care to mothers hospitalised by Covid-19, The Independent can reveal — as women are warned they are up to three times more likely to have an early birth with the virus.
The figures, which cover 17 months of the pandemic, prompted calls for the government to make pregnant women of all ages eligible for Covid-19 booster jabs.
Concern about pregnant women avoiding the vaccine has pushed chief medical officer Chris Whitty to urge mothers-to-be to get fully jabbed, with take-up rates in this group as low as 15 per cent last month.
Data uncovered by The Independent from a national maternity conference shows that, out of 3,306 babies born to mothers admitted to hospital with Covid-19 between the start of the pandemic in March 2020 and July 2021, 694 were born prematurely and of those 604 were so ill they had to be admitted to a critical care unit.
Dr Patrick O’Brien, from the Royal College of Obstetricians and Gynaecologists (RCOG), said there have been preventable admissions of women to intensive care, and even deaths.
“This is a universal view among doctors and among the midwife advisory groups and among the scientific advisory groups,” he said. “So can I please encourage all women who are pregnant or wishing to become pregnant to get their vaccination.”
Professor Marian Knight, a top maternal mortality expert, shared data from the UK Obstetric Surveillance System showing that, between February and September this year, more than 1,000 pregnant women were admitted to hospital with Covid-19, around 98 per cent of whom were unvaccinated.
She said the risk of premature births was the most important impact of Covid-19 on pregnant women “that isn’t really talked about or recognised.”
“We know that if you are admitted with symptoms of Covid, in pregnancy, you as a woman have about a one in 10 chance being admitted to intensive care,” she said. “But you’ve got a one in five chance of having a preterm baby.
“And that’s between two and three times higher than your risk of having a preterm baby without Covid.”
Professor Knight said it had been “really difficult” for pregnant women as messaging around vaccination has changed over the past year.
However, she and Dr O’Brien both called for all pregnant women to be made eligible for booster vaccines — following a similar move last week by counterparts in the US.
Current guidance from the UK Joint Committee for Immunisations and Vaccinations (JCVI) is that only pregnant women who are over 40 or within a clinically vulnerable group are eligible.
Professor Knight’s figures show that 13 pregnant women died during the February 2021 Covid wave after being admitted to hospital with the disease, compared to 11 and nine in the previous two waves.
Dr O’Brien said: “Pregnant women are at increased risk of severe Covid-19 and serious infection can also put their babies at risk due to being born prematurely. We would urge the government to ensure there is a plan in place for pregnant women to receive the booster vaccine as we enter winter.
“Many pregnant women will be coming to the point where they had their second Covid-19 vaccine six months ago and it is crucial they and their baby remain protected.”
He explained: “It’s not so much that the virus directly affects the babies, it’s that the virus is causing us to deliver the baby early.”
Births earlier than 28 weeks increase the risk of severe long-term harm, while after 34 weeks babies are usually fine.
Professor Asma Khalil, of the RCOG, added: “We know that prematurity is associated with the risk of disability and also higher chance of needing admission to a neonatal care unit.
“I think if you put everything together, Covid can harm the mother and the baby, and we know that the best way to protect the mother and baby is to get their vaccination.”
‘They moved him without letting us see him’
Asya, from southeast London, spoke to The Independent about the “awful” experience of having her son Daniel born at 28 weeks after she contracted Covid-19 last December, before vaccines were available.
Leading up to his birth, 35-year-old Asya, who was seven months pregnant, contracted Covid-19 along with her husband.
“Suddenly, after about five days, I thought I felt less movements from the baby,” she said. “They took me to A&E, then moved me into the labour ward. The next day they said the baby is in respiratory distress, we need to get him out and I was going to have to have an emergency C-section.”
Although her husband was out of isolation, infection control rules meant he was not allowed at the birth, nor was he able to see his wife initially.
“They showed me my baby for a second and then they showed him to my husband and then sent him to the neonatal unit,” said Asya.
“Daniel was born very small and actually tested positive for Covid-19. He had to be intubated, he had bleeds in his brain, and due to a bleed in his lung they moved him to a different hospital to a higher level neonatal unit. They moved him without letting us see him and we were not allowed to visit him initially.”
Eventually Asya and her husband were able to see their son, but only separately and once a day through “many layers of PPE”.
Daniel was on the neonatal unit for eight weeks. Describing her experience during this time, Asya said: “It was really, really hard. One of the hardest things was the issue with pumping breast milk… I didn’t have that much milk, probably because of the trauma and being separated from him, but it was really important for me to maintain my supply so I can try to breastfeed him eventually.”
She told how scary it was for herself and her husband coming home from hospital and having to leave Daniel behind.
Doctors don’t yet know conclusively whether Covid or a urinary tract infection (UTI) contributed to Daniel’s premature birth.
However, Asya said: “If I’d had a possibility to get a vaccine, I would have done. I have had both the vaccines now and I’m going to get the booster. And I very much recommend that pregnant women get it. It’s really sad just to wonder what would have happened if I’d been able to be vaccinated then.”
Daniel is now well and healthy at 10 months old.
Throughout the experience Asya and her husband were supported by Camp Simcha, a national charity that supports seriously ill children in the Jewish community.
Daniel Gillis, its deputy chief executive and head of service, said the organisation had seen a 150 per cent increase in the number of premature and sick babies who needed support compared to 2020.
7 notes
·
View notes