#at least in recent memory for my brain back to 2010/2012
Text
just saw US champs has 42!!!!! senior gymnasts qualified
Genuinely how are they going to manage that with tv / timing / etc. Like even last year was ~30ish and that was a lot
#and they never really split up champs like they do classics#at least in recent memory for my brain back to 2010/2012#the tv broadcast is going to be a nightmare#although if usag is smart they will stagger the top 10-15 gymnasts between flights so we can see all the routines
3 notes
·
View notes
Note
Hey, I just read your post on ADHD/EFDD and was just wondering if you have read any research articles on this and if you have, could you tell me which ones because it all sounds super interesting and I need to choose a topic for my psych lit review and I’m thinking about doing something to do with all the stigma around and misconceptions about different mental health disorders.. it’s totally okay if not tho, I know it’s a big ask, but thanks anyway
That sounds like such a great topic!!! I would be HONORED to help :D
The first person I think of when discussing the term EFDD is Dr. Russell Barkley. He’s one of the leading ADHD experts, and has been a spearhead for studying executive dysfunction in people with ADHD for decades. Very much ahead of his time compared to the DSM. I’ve had his book “Taking Charge of Adult ADHD” recommended to me so many times, but have yet to read it.
Here’s some free stuff, though!
[reblogs appreciated because Tumblr hates posts with links and I wanna make sure this anon sees it!]
I tried to include some short stuff and longer stuff, some articles, images, videos, and comic recs, so you can choose based on your current energy and focus level :) I’ve also bolded links and key points of each source if you like skimming. Let’s go!
...................................
Here’s an interesting article/study on EFDD! They found that “ADHD [is] associated with deficits in inhibition, managing one’s attention, self-directed speech and rule-following, self-motivation, and even self-awareness [...] ADHD therefore involves deficits in self-restraint, [...] selfsensing and imagery, self-control of emotion, and self-directed play for problem-solving.”
Thank you for motivating me to look up some articles, because I learned some new things, too! For instance, they assert that ADHD could also be called SRDD (Self-Regulation Deficit Disorder), but conclude the article by saying either SRDD or EFDD fits better than ADHD, and that the terms could be used interchangeably, because SR (self-regulation) and EF (executive function) are effectively talking about the same things. So his assertion is that even if the name ADHD never changes, it can still be scientifically classified as either of the other terms. I believe in recent years he’s preferred EFDD more and more.
[note that the above article/study is from 2011, back when we were on the DSM-IV, so a lot of research has been done since then]
...................................
If that article’s a bit wordy or you want something more visual and up-to-date, here’s a really detailed PowerPoint presentation used during the 2018 ADHD Symposium! It’s long but well-organized so you can just read the big headers or you can read all the bullet points explaining it. Keep in mind this was a lecture, so some of it probably made more sense in person. I’m glad I read this, because I realize the terminology I’ve used is slightly off: according to the Symposium, there aren’t “subtypes” of ADHD, but the different names (ADHD-PI, ADHD-PH, and ADHD-C) are really just used to show the prevalence of certain symptoms in that individual. So they’re all terms for ADHD, but “subtype” was poor word choice on my part.
Oh! I just found a video of him giving a lecture in 2012 using many of the same PowerPoint slides! Here ya go! It’s a bit longer than the other videos I’ve linked below (13min), but it might make the slides easier to interpret :)
...................................
If you want a really short and basic overview, here’s a video explaining 5 main ways executive functions affect the brain and how they work differently in people with ADHD. [I put the video below as well if you wanna stay on tumblr] It’s from 2010, but it holds up. It only covers 5 big ones, so remember (if you can) that executive function affects EVERYTHING and the symptoms will affect everyone differently and at different levels.
This is just the most basic overview and a good place to start:
youtube
...................................
Here’s one where he talks about our Time-Blindness! (below) I was going to pick a couple favorite quotes to give you an idea, but that’d wind up being a transcript of the whole video because HE GETS IT. This is from 2014, but I CANNOT recommend it enough!!! He mentions that ADHD doesn’t have a deficit of attention, but rather a deficit of intention. He describes us as having a near-sighted sense of time, and talks about deadlines, “laziness,” etc.
ALSO he talks about how our brains DON’T CONNECT our knowledge to our performance (back of brain to front) like everyone else’s, so we have the same level of knowledge and intelligence, but can’t access and use it the way others can. This is why teaching skills and organization/memory/time-management tips isn’t helpful -- we can learn them, but our knowledge and action centers are separated, so actually doing them/sticking with them is just as hard as before.
If you don’t watch the whole thing, at least skip to 3:29 cause that part’s really funny and relatable (ok the whole thing is relatable):
youtube
...................................
And of course, I highly recommend the YouTube channel How to ADHD! I have a couple friends who work on it, and they REALLY know their stuff! (They’re the ones who taught me during a game night that RSD isn’t a real term and it should be called “rejection-sensitivity” as part of the emotional dysregulation umbrella)
I went looking and found this video (below) has the BEST explanation of it that I’ve seen in such a concise, entertaining way. I hadn’t seen this one before, but it even covers some of the things I mentioned in that post your ask is about! Especially the Internal Restlessness that I mentioned as the true “hyperactivity” we all share; even though some of us also express outward hyperactivity, both presentations come from the same restlessness in our brains.
youtube
^^^This has some great examples, visuals, animations, and different ways of explaining and thinking about our symptoms! If you want more about this, the description has a bunch of links to their sources! Jessica and everyone else who works on this channel is great at making the videos watchable for people with ADHD (even if we have to rewind sometimes)
Here's Jessica's official Twitter @HowtoADHD! (I was today years old when I found out that she follows me)
...................................
And if you want something REALLY short and simple, here’s a 2 minute animation comparing living with ADHD to trying to film a movie with a director who keeps falling asleep [below]
youtube
....................................
If you like comics:
My favorite ADHD comic artists are: ADHD Alien [@ADHD_Alien on Twitter and @adhd-alien on Tumblr]; Dani Donovan [@danidonovan on Twitter and @danidonovan on Tumblr -- we’re somehow twitter mutuals and she is such a sweetheart. She has some really good infographics, too!!]; ADHD Bri [@AdhdBri on Twitter and @adhdbri on Tumblr]; and dreamadept [@yume_dango on Twitter and @yume-dango on Tumblr]
They’re all well-researched, funny, genuine, intelligent, insightful, talented artists who depict ADHD in a very accurate and relatable way. Go check ‘em out and support them! :D
....................................
I’m gonna stop there for now, but PLEASE feel free to add on to this with other sources, questions, videos, thoughts, comic artists, etc.!!! Hope this helps someone out there!
#adhd#actuallyadhd#efdd#executive function deficit disorder#how to adhd#dr. russell barkley#I hope you see this in time for your essay!!!#tried to give you a variety of sources and places to start#quinpost#quinanswer#oof I'm sure I forgot some adhd comic artists I love but maybe I'll remember later lol#Anonymous
107 notes
·
View notes
Link
Released with little fanfare this move to more muted songwriting is proof Swift’s music can thrive without the celebrity drama
Taylor Swift announced the existence of her eighth album an uncharacteristic 17 hours prior to its release: “Most of the things I had planned this summer didn’t end up happening,” she said – among them, a headline slot at Glastonbury – “But there is something I hadn’t planned on that DID happen.” Swift only released her last album, Lover, last August. If she was surprised to have emerged from lockdown with Folklore – a 16-track album largely produced (remotely) by the National’s Aaron Dessner – her fans were even more stunned by the fact that Swift would release a record with zero fanfare.
Swift pioneered the art of the all-consuming album rollout. It usually starts with her sharing coded hints that her well trained fans understand immediately. Then there are teasers for lyric videos that beget actual blockbuster videos, strewn with self-mythologising references for Swifties and journalists to unpick. It’s a smart promotional strategy-by-proxy for an artist who has done little press in the past five years, and a good way of making your actions seem as if they were written in the stars. There are sometimes baffling brand endorsements. The often unpopular lead single seldom sounds like the rest of the album. By the time that arrives, a weariness has descended: the sense that one of pop’s all-time greatest songwriters is overcompensating despite her clear talent.
Recent albums, too, have been consumed with the various dramas that have plagued her since the country ingenue became a pop superstar with 2012’s Red. Despite the last 12 months bringing a new, high-profile disagreement with her former label and enduring disputes with Kanye West, thankfully Folklore features none of that, beyond inadvertently arriving the same day as West said he was releasing a new album. Moreover, Swift conveys the sense that her tendency to desire the last word, in public and private, has been her undoing: “I was so ahead of the curve, the curve became a sphere / Fell behind all my classmates and I ended up here,” she sings on This Is Me Trying.
Folklore proves that she can thrive away from the noise: if you interpret “classmates” as pop peers, Swift is no longer competing. Bombastic pop makes way for more muted songwriting, and a singular vision compared to the joyful but spread-betting Lover. With concerts off the table for the foreseeable future, no longer needing to reach four sides of a stadium may have proven liberating.
Elements of her fanbase have long wanted her to revisit the Nashville songcraft of her youth through an adult lens, but this isn’t that album. Folklore is largely built around the soft cascades of piano, burbling guitar and fractured, glitchy electronica that will be familiar to fans of the National’s post-2010 output – at least part of the album came about from Swift writing to Dessner’s musical sketches. Swift’s most coherent record since her staunchly country days, it’s nonetheless her most experimental, developing on Lover’s stranger, more minimalist end. More than one song evokes the intimate celestial tenderness of Sufjan Stevens circa Carrie and Lowell. At the opposite end of the scale, This Is Me Trying subtly grows into its wracked orchestral grandeur, sounding more unsettling still for how Swift’s voice, processed at a ghostly, vast remove, seems to encompass the whole song with her desperation.
Swift is known for her vocal directness – there is no pop star as adroit at searing a chorus into your brain, or as winking in her tartness – if not her range. But the demands of pop processing mean her voice has never been heard as it is here: the acceptance that colours it on The 1, a bouncy reminiscence of a lost lover from her “roaring twenties”; how weatherworn yet at peace she sounds as she remembers the good parts of a treacherous relationship on Cardigan, a song as cavernous and shimmering as a rock pool in a cave. Her vocal trademarks remain in the yo-yoing vocal yelps on August, and the climactic, processed cri de coeur of My Tears Ricochet, and she holds her own against the wounded bark of Bon Iver’s Justin Vernon on Exile, which paints a split first in scenes of overt betrayal, and then gorgeous, subtle harmonies at crossed purposes indicating a problem deeper than one infidelity.
Given the more earthy production, some will characterise Folklore as showing a more authentic side of Swift. Not only would that be facile, asserting some authentic self is also explicitly not her aim. In a brief essay included in the liner notes, she says of the album’s concept: “The lines between fantasy and reality blur and the boundaries between truth and fiction become almost indiscernible.” She writes that some songs are about her and others are about invented characters. More interesting than parsing which is which (many are obviously both) is the sense that Swift is interrogating her own self-conception and challenging that personal mythology: how helpful and true those ideas are to herself as a woman of 30.
Swift’s longest lyrical obsession is the loss of innocence, a theme she makes fairly devastating here. Set to high piano flurries, Seven switches between hopscotch-rhyme verses about childhood rituals, and pleading, choral depictions of herself at seven, “in the weeds, before I learned civility,” she sings. “I used to scream ferociously / Any time I wanted.” What conditioning beat out of her as a girl, it beat back in decades later: the tense, slippery Mad Woman traces the self-perpetuating cycle of women being angered by being labelled angry – both massively improve on Lover’s slightly facile gender inequality treatise, The Man, because they’re personal, not projections. Later she recalls naive young love, “back when we were still changing for the better”, then, on Illicit Affairs, willingly entering into a deceitful relationship with someone who “showed me colours you know I can’t see with anyone else”.
The self-awareness that Swift displayed on Lover deepens in Folklore, where she subtly considers the murky line between corruption and complicity, between being a victim and a catalyst. The recriminations are fewer, the fights fairer, and her sense of responsibility in them greater. The seismic shocks of her Reputation-era rude awakening about her public image are still felt: “I can change everything about me to fit in,” she sings on Mirrorball, a gorgeous pedal steel wooze made with Jack Antonoff. Yet she tentatively asserts what’s at her core: the deep dedication she sings about on the resonant, minimalist Peace, and the abiding romanticism of Invisible String.
Lockdown has been a fruitful time for this sort of soul-searching, the absence of much in the way of new memory-formation triggering nostalgic reveries and regrets. This strange summer of arrested development is steadily ending. Folklore will endure long beyond it: as fragmented as Swift is across her eighth album – and much as you hope it doesn’t mark the end of her pop ambitions – her emotional acuity has never been more assured.
26 notes
·
View notes
Text
2019 & 2020
Hello everyone! So yeah, this yearly blog post is about three... four months late... it covers two years now.
I did have a lot of things written last year, last time, but the more things have changed, the more I’ve realized that a lot of things I talked about on here... were because I lacked enough of a social life to want to open up on here.
In a less awkwardly-phrased way, what I’m saying is, I was coping.
Not an easy thing to admit to in public by any means, but I reckon it’s the truth. Over the past two years, I’ve made more of an effort to build better & healthier friendships, dial back my social media usage a bit (number 1 coping strategy), not tie all my friendships to games I play, especially Dota (number 2 coping strategy), so that I could be more emotionally healthy overall.

Pictured: me looking a whole lot like @dril on the outside, although not so much on the inside. (Photo by my lovely partner.)
To some degree, I believe it’s important to be able to talk about yourself a bit more openly in a way that is generally not encouraged nor made easy on other social networks (looking at you, Twitter). I know that 2010-me would be scared to approach 2020-me; and it’s my hope that what I am writing here would not help him with that, but also help him become less of an insecure dweeb faster. 😉
Not that recent accomplishments have stopped me from being any less professionally anxious. Sometimes the impostor syndrome just morphs into... something else.
Anyway, what I’m getting at is, the first reason it took me until this year to finish last year’s post is because, with my shift in perspective, and these realizations about myself, I do want to keep a lot more things private... or rather, it’s that I don’t feel the need to share them anymore? And that made figuring out what to write a fair bit harder.
The other reason I didn’t write sooner is because, in 2018, I wrote my "year in review” post right before I became able to talk about my then-latest cool thing (my work on Valve’s 2018 True Sight documentary). So I then knew I’d have to bring it up in the 2019 post. But then, I was asked to work on the 2019 True Sight documentary, and I know it was going to air in late January 2020, so I was like, “okay, well, whatever, it, I’ll just write this yearly recap after that, so I don’t miss the coach this time”. So I just ended up delaying it again until I was like... “okay, whatever, I’ll just do both 2019 and 2020 in a single post.”
I think I can say I’ve had the privilege of a pretty good 2019, all things considered. And also of a decent 2020, given the circumstances. Overall, 2019 was a year of professional fulfillment; here’s a photo taken of me while I was managing the augmented reality system at The International 2019! (The $35 million dollar Dota 2 tournament that was held, this that year, in Shanghai.)

If I’d shown this to myself 10 years ago it would’ve blown my mind, so I guess things aren’t all that bad...!
I’ve brought up two health topics in these posts before: weight & sleep.
As for the first, the situation is still stable. If it is improving, it is doing so at a snail’s pace. But quite frankly, I haven’t put in enough effort into it overall. Even though I know my diet is way better than it was five or six years ago, I’ve only just really caught up with the “how it should have been the entire time” stage. It is a milestone... but not necessarily an impressive one. Learning to cook better things for myself has been very rewarding and fulfilling, though. It’s definitely what I’d recommend if you need to find a place to start.
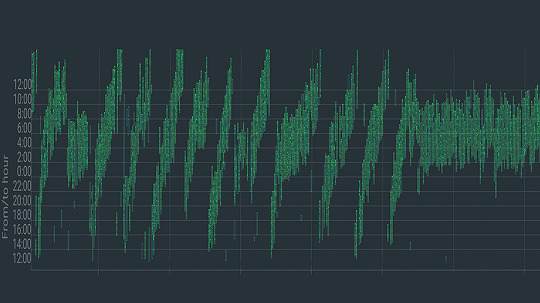
As for sleep, throughout 2019, I continued living 25-hour days for the most part. There were a few weeks during which I slowed down the process, but it continued on going. Then, in late December of 2019, motivated by the knowledge that sleep is such a foundational pillar of your health, I figured I really needed to take things seriously, and I managed to go on a three month streak of mostly-stable sleep! (See the data above.)
Part of what helped was willingly stopping to use my desktop computer once it got too late in the day, avoiding Dota at the end of the day as much as possible, and anything exciting for that matter... and, as much as that sounds like the worst possible stereotype, trying to “listen to my body” and recognizing when I was letting stress and anxiety build up inside me, and taking a break or trying to relax.
Also, a pill of melatonin before going to bed; but even though it’s allegedly not a problem to take melatonin, I figured I should try to rely on it as little as possible.
Unfortunately, that “good sleep” streak was abruptly stopped by a flu-like illness... it might have been Covid-19. The symptoms somewhat matched up, but I was lucky: they were very mild. I fully recovered in just over a week. I coughed a bit, but not that much. If it really was that disease, then I got very lucky.

(Pictured: another photo by my lovely SO, somewhere in Auvergne.)
My sleep continued to drift back to its 25-hour rhythm, and I only started resuming these efforts towards the fall... mostly because living during the night felt like a better option with the summer heat (no AC here). I thought about doing that the other way (getting up at 3am instead of going to bed at 7am), and while it’d make more sense temperature-wise, that would have kept me awake when there were practically no people online, and I was trying to have a better social life then, even if had to be purely online due to the coronavirus, so... yeah.

I’ve been working from home since 2012! I also lived alone for a number of years since then. For the most part, it hasn’t been a great thing for my mental health. Having had a taste of what being in an office was like thanks to a couple weeks in the Valve offices, I had the goal of beginning to apply at a few places here and there in March/April. Then the pandemic hit, so those plans are dead in the water. I wanted 2020 to be the year in which I’d finally stop being fully remote, but those plans are now dead in the water.
Now, at the end of the year, I don’t really know if I want to apply at any places. There’s a small handful of studios whose work really resonates with me, creatively speaking, and whose working conditions seem to be alright, at least from what I hear... but, and I swear I’m saying this in the least braggy way possible... there’s very little that beats having been able to work on what I want, when I want, and how much I want.
This kind of freelance status can be pretty terrifying sometimes, but I’ve managed (with some luck, of course) to reach a safe balance, a point at which I’ve effectively got this luxury of being able to only really work on what I want, and never truly overwork myself (at least by the standards of most of the gaming industry). It’s a big privilege and I feel like it’d take a lot to give it up.
Besides the things I mentioned before, one thing I did that drastically improved my mental health was being introduced to a new lovely group of friends by my partner! I started playing Dungeons & Dragons with them, every weekend or so! And in the spirit of a rising tide lifting all boats, I managed to also give back to our lovely DM, by being a sort of “AM” (audio manager)... It’s been great having something to look forward to every week.

Something to look forward to... I’ve heard about the concept of “temporal anchors”. I had heard about how the reason our adult years suddenly pass by in a blur is because we now have more “time” that’s already in our brains, but now I’m more convinced that it’s because we’re going from a very school routine such as the one schools impose upon us, to, well... practically nothing.
I thought most of my years since 2011 have been a blur, but none have whooshed by like 2020 has, and I reckon part of that is because I’ve (obviously) gone out far far less, and most importantly there wasn’t The Big Summer Event That The International Is, the biggest yearly “temporal anchor” at my disposal. The anticipation and release of those energies made summer feel a fair bit longer... and this year, summer was very much a blur for me. In and out like the wind.
I guess besides that, I haven’t really had that much trouble with being locked down. I had years of training for that, after all. Doesn’t feel like I can complain. 😛

(Pictured: trip to Chicago in January of 2019... right when the polar vortex hit!)
Work was good in 2019, and sparser in 2020. Working with Valve again after the 2018 True Sight was a very exciting opportunity. At the time, in February of 2019, I was out with my partner on little holiday trips around my region, and, after night fell, on the way back, we decided to stop in a wide open field, on a tiny countryside path, away from the cities, to try and do some star-gazing, without light pollution getting in the way.

And it’s there and then that I received their message, while looking at the stars with my SO! The timing and location turned that into a very vivid memory...
I then got to spend a couple weeks in their offices in late April / early May. I was able to bring my partner along with me to Washington State, and we did some sightseeing on the weekends.

(Pictured: part of a weekend trip in Washington. This was a dried up lakebed.)
After that, I worked on the Void Spirit trailer in the lead to The International. In August, those couple weeks in Shanghai were intense. Having peeked behind the curtain and seen everything that goes into production really does give me a much deeper appreciation for all the work that goes unseen.
Then after that, in late 2019, there was my work on the yearly True Sight documentary, for the second time. In 2018, I’d been tasked with making just two animated sequences, and I was very nervous since that was my first time working directly with Valve; my work then was fairly “sober”, for lack of a better term.

(Pictured: view from my hotel room in Shanghai.)
For the 2019 edition, I had double the amount of sequences on my plate, and they were very trusting of me, which was very reassuring. I got to be more technically ambitious, I let my style shine through (you know... if it’s got all these gratuitous light beams, etc.), and it was real fun to work on.
At the premiere in Berlin, I was sitting in the middle of the room (in fact, you could spot me in the pre-show broadcast behind SirActionSlacks; unfortunately I had forgotten to bring textures for my shirt). Being in that spot when my shots started playing, and hearing people laughing and cheering at them... that’s an unforgettable memory. The last time I had experienced something like that was having my first Dota short film played at KeyArena in 2015, the laughter of the crowd echoing all around me... I was shaking in my seat. Just remembering it gets my heart pumping, man. It’s a really unique feeling.

So I’m pretty happy with how that work came out. I came out of it having learned quite a few new tricks too, born out of necessity from my technical ambitions. Stuff I intend to put to use again. I’m really glad that the team I worked with at Valve was so kind and great to work with. After the premiere, I received a few more compliments from them... and I did reply, “careful! You might give me enough confidence to apply!”, to which one of them replied, “you totally should, man.” But I still haven’t because I’m a massive idiot, haha. Well, I still haven’t because I don’t think I’m well-rounded enough yet. And also because, like I alluded to before, I think I’m in a pretty good situation as it is.
It’s not the first encouragements I had received from them, too; there had been a couple people from the Dota team who, at the end of my two week stay in the offices, while I was on my way out, told me I should try applying. But again, I didn’t apply because I’m a massive idiot.

(Pictured: view from the Valve offices.)
To be 200% frank, even though there’s been quite a few people who’ve followed my work throughout the years, comments on Reddit and YouTube, etc. who’ve all said things along the lines of “why aren’t you working for them ?”, well... it’s not something I ever really pursued. I know it’s a lot of people’s dream job, but I never saw it that way. I feel like, if it ever happened to me... sure, that could be cool! But I don’t know if it’s something I really want, or even that I should want?
And if you add “being unsure” to what I consider to be a lack of experience in certain things, well... I really don’t think I’d be a good candidate (yet?), and having seen how busy these people are on the inside, the last thing I want to do is waste their time with a bad application. That would be the most basic form of courtesy I can show to them.
Besides, Covid-19 makes applying to just about any job very hard, if not outright impossible right now. And for a while longer, I suspect.

(Pictured: the Tuilière & Sanadoire rocks.)
I’m still unhappy about the amount of “actual animation” I get to do overall since I like to work on just about every step of the process in my videos, but well. It’s getting better. One thing I am happy with though, is “solving problems”. And new challenges. Seeking the answers to them, and making myself be able to see those problems, alongside entire projects, from a more “holistic” way, that is to say, not missing the forest for the trees.
It’s hard to explain, and even just the use of the term “holistic” sounds like some kind of pompous cop-out... but looking back on how I handled projects 5 years ago vs. now, I see the differences in how I think about problems a lot. And to some extent I do have my time on Valve contracts to thank a LOT in helping me progress there.
Anyway, I’m currently working on a project that I’m very interested & creativefuly fulfilled by. But it has nothing to do with animation nor Dota, for a change! There are definitely at least two other Dota short films I want to make, though. We’ll see how that goes.
Happy new year & take care y’all.
4 notes
·
View notes
Text
How I Talk About Trauma
Inspired by early 2010 essay “why me and why now”
I recently mentioned to friend that I have nearly 30 years worth of memoir essays stashed mostly in expertly hidden journals and spiral bound notebooks throughout my home. I hadn’t ever really mentioned to anyone, really, ever. I have/had no intention of ever doing anything with my often rambling stories mixed with poetry and observation. This friend gave me just enough encouragement and expressed just enough curiosity that I decided to go back and see if I had enough to cobble together a cohesive creative memoir piece.
I’m not the sort of gal who thinks people are all that interested in reading about my life. I’m afraid of their judgment and wonder how easily my style of oversharing and conversational prose will sit with them. I do know that people are interested in hearing my stories. I’ll often make some self-deprecating comment in passing, only to find myself explaining my comment through some story about a personal traumatic event. In these moments, I’m at my most vulnerable, letting people in to see behind the curtain, hoping for their empathy and secretly desiring that they find inspiration in the “Meghan then versus Meghan now” of it all. There’s an additional must mention element to sharing our stories that didn’t exist to the same extent when I wrote the essay that inspired this one and definitely was an issue for the vast majority of my other still-buried writings, social media. The proliferation of social media and the encompassing issues around what we share, how we share, who sees it and any potential impacts can’t be ignored. The fear of the judgment and ugliness of the keyboard armies can’t be understated. There are people who will define you by what you share and their are people who will use your vulnerability to their advantage for whatever perverse enjoyment they get out of destroying the lives of other for attention. This is a very real fear to me as I write this now, trusting the reader with my feelings and saying always with an asterisk, this is my life as I was/am living it. This is my perspective, interpretation/reinterpretation of events that in some cases happened 30 years ago. Anyone who says they remember something exactly how it happened even 5 years ago, especially a traumatic event, well- I wouldn’t call them a liar, it’s an important piece of my thinking I’m sharing here- but I would say it’s likely someone else from their life remembers it slightly differently and recalls a drastically different set of outcomes and experiences. It’s important I mention that because so often when people publish personal essays or memoirs the colloquial “that didn’t happen that way” or “that’s not what I remember” comments almost always occur. So I say with an asterisk that this essay discusses events and feelings as I remember them, colored by my perspective then versus now and altered by my overall ability to be subjective or objective about what was going on. You may remember me differently. You may have seen me a different way than I actually felt. I may have lied to you (more on that later). I may be lying to myself (lots more on that later). I may be remembering different timeframes and my reactions and confusing them, so let’s talk about that now.
When we talk about trauma, communally, socially or even in mass media, we often hear it, see it, experience it, as a story arch. The beginning is the traumatic event/s, the middle is either the present or the immediate outcome, and the ending is either the present or the big reveal of why present person is who present person is. In the sneakiest depictions, we may not know what the real trauma story is until the very end and you find yourself pointing at the screen ( I did this last week myself) and saying, “I knew it! I knew all along that’s what really happened!” This is called the unreliable narrator. The story is told first person subjective so you are experiencing the events as the narrator remembers and experiences them and possibly not the way they happened. This leads us to feel mislead but there’s an important aspect of how our brains operate at work here. Our brains are designed to help us survive. It’s a hard wired evolutionary instinct. What that means from a trauma aspect is that the brain often finds a way to cope with trauma, whether it sudden or long-lasting trauma. That coping mechanism, often defined in the most simple terms is flight or fight. I’m not a fan of either term because experience tells me it’s not simple to know if your brain is “flighting or fighting”. You may not physically run away and you may not physically fight back. Trauma response just isn’t that simple, it’s hard for me to understand, even years later what my brain was doing and somethings I don’t recall at all or come to me in the most obscure or totally in-opportune times. I will say that what I’m about to share and most of what I share is a form of flight and this flight always makes me an unreliable narrator. Those closest to me have heard me say, likely way too many times, I do not trust myself as the narrator of my own story. That’s a sad and scary place to be. I do think my brain remembers thing in ways that make them easier for me to deal with. Repression has a way of creating a false sense of yourself and the way things were. That’s why we feel tricked as an audience. We feel we weren’t showed what really happened. The truth is we are shown almost always what some observer think happened from their perspective. We can often collect similar observations and determine a set of common descriptions and then say, we now have the factual actual occurrence but it’s still really not what happened. If we had some omnipotent recording system that was unfiltered and unedited by any human then we could potentially see what actually happened all the time but I guarantee at least one person would still pipe up and say, “that’s not what happened at all”. Anyway, as you’re reading and if you see anything that you do think happened some other way, I want to hear from you. Not so we can argue because as I just explained, I’m more likely to believe YOU than my own memories, but so we can share how we both experienced that same event.
Ok. So recently I’ve been doing some pretty deep work on managing my response to trauma. After 20+ years of therapy, I feel like an expert patient who’s finally having an “aha” moment. That moment isn’t refreshing or relieving, it can take weeks of introspection on a tiny realization for me to get anywhere with it but I guess, unluckily, I have lots of time for isolated introspection. This is another important point for my long term friends who know I have a deep fear of alone time. Not the few hours at the end of a work day alone time, but weeks or months of mostly alone time. These kinds of alone time usually send me on the dark and anxious paths of my mind and I start doing whatever I can to avoid the paths and avoid the dark, mainly because when I allow myself to live in the dark and anxiety- very bad things happen. I know that sounds ominous, but it will make much more sense later. For now, just know that being alone means putting my sanity at risk. This year made being alone unavoidable and finding a peace with that, a way to introspect, to accept my darkness and then force myself to sit with it has been my challenge.
Fairly recently, friends have been sending me podcasts, books, meditations, TedTalks, and even virtual webinar recordings focused on mental health issues. I love all of it to be frank. Not the material itself, sometimes it doesn’t really speak to me, but I love that I have that community, one that I know I fostered just by being vulnerable and shining a light on my own struggles with mental health. I wasn’t always receptive to these suggestions- I felt criticized and judged- like am I that crazy people think I need more help? Eventually I realized it’s love. Someone is sharing something that helped them and frankly that’s what inspires this essay on an essay too. This helped me. You may not write but maybe just reading it will help you.
The first line of my early 2010 essay which isn’t dated until page 3 (this tells me I wrote an entire section much earlier based on content, then came back and finished it) was “why me”. This is a common thought pattern well established by a seeming luck to be unlucky. There’s years that I’ve said, maybe next year so much bad shit won’t happen, most of the time maybe slightly less shit happens but I’m likely to remember it all as constant shit anyway. I’ll remember a slightly more nostalgic time frame, only to remember, oh but XYZ happened too, so that wasn’t a good time. The difference in 2020 is everyone had a “shit what else could happen” year so it was the first time I didn’t feel so alone in that. There’s an exhaustion in one crazy whatever happening after another that I felt less alone in. That’s doesn’t mean I’m happy we are all sharing in a long term trauma event but it is less isolating to know we are in this together, even if our individual situations are different.
Any hoo, back to why me. The why me of 2009 to 2012 was cervical and ovarian cancer. The why me was quitting my MBA program. The why me was my marriage falling apart. The why me was finally, my career falling apart too. It’s still hard to talk about how I felt during that time. Most of the time, I felt nothing. In fact, I say that over and over in my 2010 essay. I felt nothing for no one, not even myself. However I know some of my friends from that time, just read that line and thought, no you were all over the place, all the time, emotionally. I felt nothing. It was like I was a walking emotion that didn’t actually exist inside. Let’s call it dissociation or flight from trauma. Things were happening, I was a walking talking person but my soul, my sense of self, were somewhere else. Without even knowing it, I glassed myself off from what was happening and didn’t feel genuine pain or sadness. I did, but really I didn’t, I really wasn’t there for it. I couldn’t today tell you what my body experienced as I just remember the raw emotional expressions but again I didn’t actually feel them. I know if you were there, you remember them too.
I spend several paragraphs talking about how much I’m hiding from everyone and how afraid I am I’ll be found out ( yup! That happened). What’s odd is I’m not sad that I’m clearly isolating myself. I see that so clearly now. My fear of rejection and abandonment created a situation where I was extremely isolated and feeling- rejected and abandoned. I read all the things I thought were good ideas in order to keep up appearances but also know all that was a total failure pretty much the entire time. I had many epic public breakdowns. There was no charade at all. I didn’t pull the wool over anyone’s eyes . Absolutely zero people thought I had my shit together. So why? Why did I hide so much that could’ve helped me get through this?!? Why did I lie to my friends and family? Why did I not ask for help, and in lots of cases, refuse help only to drop my ignored broken life shit on someone else to manage? Because I was lying to myself too.
I’ve always believed there’s a “most people” and excluded myself from this category. Not because I think I’m some extraordinary soul, just the opposite. I often think “most people” have this shit figured out and wouldn’t act this way. Well, maybe but probably not. How someone reacts to any given set of circumstances is related to how many and how bad the circumstances they’ve managed have been. What if nothing else bad had happened in my life and I had just gotten cancer in my early thirties? Hard to say how I would have managed if that had been my only big bad thing ever. Maybe I still wouldn’t have coped because I had no learned coping skills. It wasn’t my first rodeo with a big bad thing though and the coping skills I had “learned” were super effective for short term, violent trauma, but completely ineffective for long term can’t check out from life trauma. No one tells you that, by the way, no one tells you that your coping skills suck. When we hear about trauma we are so focused on outcome we rarely talk about the way there.
Page 3 of my essay is pretty bad. I’ll likely edit it out of memoir existence but a few things are clear. In January 2010 I wrote, I can’t do this anymore. Until I read this I recalled my last suicidal expression as being in 2003. This makes me doubt my narration that I only expressed suicidal depression during isolated timeframes. I want to say it’s because I didn’t want to remember I was there in 2010. The other thing very clear on page 3 is desperation. Knowing that I spent another two years in that state isn’t comforting. I wrote, “I feel desperate for love. Desperate for understanding. Desperate for stability.” Just the other day,I said that again, I just want to be and feel normal. But normal is subjective to your perspective and what I’m living could be a good and acceptable life for a good number of people. I haven’t yet learned flipping that mindset. That sense that, god damn it, this isn’t normal. If anything, social media has only made that comparison syndrome worse. The glossy beings we all present on FB and Instagram all have little bearing to our inner selves. I can never win in a comparison to a manufactured brand of someone else. That doesn’t mean I think you’re fake. It means I know I sanitize my life for public consumption so I’m fairly certain others do too. This comparison takes you out of what you’re living and into what you could or should be, so it’s also an escape, a flight from what is happening.
By page four, I’m planning, I’m planning on burning every bridge, breaking every perceived enemy, and leaving my life in ruins. I’m fantasizing about how everyone will regret how they treated me. I remember this feeling. It’s probably the only one I connect with from that time-rage. I was grieving so many things in that space but not working through it. I clearly am mad because I wrote, “fuck this life. I’m sick of all of it.” At this date, I knew I needed a plan to try to get out of everything. It felt like an emergency. I spent the next two years making every bad decision I possibly could. It’s like when there’s a fire but there’s nothing but lighter fluid, so you desperately use lighter fluid. There’s lots of things I know are in another essay for another time about 2010-2012. We have time to talk about self-hatred taking the form of destructive behavior. It’s clear my self hate was already at play here,
And this is the part I wanted to share, I forgot about this until it came up in therapy the other day. Late 2009 I had an abortion. I didn’t forget that I had it, but I told myself, and likely you a different story. A story that felt safe and relatable but I so convinced myself of that story that I knew I was lying when I talked about it to my counselor. The story is there though written on page 5 and it’s most likely the truest one. When I got pregnant, I wasn’t thinking about my diagnosis. If I told you at all that I was pregnant and lost it, I likely said it just like that. I was pregnant and miscarried. However, none of that was the truth. The truth is, I knew my marriage was over. I knew I hated my husband and our fake shared life. I knew I didn’t want to deal with him for the next 18 plus years of my life. I was also plagued by the knowledge I was too fucked up to be a good mom to anyone, likely ever. I was 100% convinced I should never have kids. In a fit of rage, I scheduled to get the pill and then purposefully planned it when my husband was out of town, I went through that by myself as some sort of sick means of punishment for all the bad things I felt I was. So here I am writing this 2010 essay and I write, “I’m a horrible human being that has no soul”. It’s important that you know, reader, I didn’t tell my husband. There’s a part of me that believes I saved that information to tell him at the moment it would most hurt (yes, I did that). That kind of rage, I don’t wish on anyone, ever.
So let’s talk about rage and trauma before I wrap this up and you all walk away disappointed at the resilient image you may have had of me until today. I don’t know if rage is fight or flight. Rage feels like an escape to me, but I was also fighting for my life. Everything felt so out of control and “happening to me”. I felt desperate to escape that and BE IN CONTROL. The lies we tell ourselves are to survive. We tell ourselves this isn’t so bad, it justified, or it will pass. What if I hadn’t lied? I will live with that regret for a long time, along with questioning my basic human decency. I am choosing to not excuse my behavior beyond saying, if you’ve ever felt that scared, desperate and full of rage you may see the desire to lash out or the desire to run away as explainable.
This last little bit may redeem me, so hold tight. You may wonder why talk about all this now. Because then is now. Not on that level of crazy messed up shit, but that girl/woman is still inside me. We are all living through a trauma, a shared one. Many of us read that sentence and think, that’s so melodramatic. It’s really not. If any of the following things happened to you in 2020 raise your hand:
Job loss/furlough/early retirement
Relationship status change
Relocation
Financial hit from work/ revenue loss
Loss of social circle
Loss of a friend/family/significant other
Severe illness/surgery/ injury/medical issues
Isolation
Not being able to go to restaurants/gyms/ or other spaces that give you joy
Anxiety over job/finances
Fear of a pandemic
Difficulty in relationships due to politics, religion or pandemic
Anxiety about the future
Cancelled/rescheduled/reimagined vacations, celebrations, holidays, life events
We really are in this together. We’ve all experienced some level of change and trauma this year. What if we chose compassion? What if I told you we can learn from our trauma? That resilience isn’t just about where I am now and everything I’ve accomplished. What if the trauma story arch finished with me, saying to you, it may take a long time to get better? What if I shared my stories with more people and told them that there’s a more successful way then just getting through and overachieving to compensate for trauma? Do you have to have some major come back to be the hero of your own story? Trauma healing is a journey. Some things take longer than others, some things you cope and have to deal with the outcome later, but it’s not punishment. It didn’t take me 10 years to rebuild my life because I deserve punishment. It took me ten years to rebuild my life because I had and still have other traumas that have come along and forced me to confront my coping mechanism. There’s no hiding and running away from me, I’m always there, getting in my own way. It’s not enough to live, I want to thrive. Thriving is about accepting and forgiving all those younger selves who did the best they could with the tool set I allowed them to have. If you give a young child a new tool, do they know how to use it or do they poke at it and bang it on things trying to figure out it’s purpose? You parents know the answer. Children are innately curious but depending on age, also short of patience. They will move on to something else if they see no use to a tool. What’s required is instruction. We learn to cope by watching those around us and I’m gonna be frank and say American culture sucks at coping. Again, it’s not about the outcome! The journey. The journey. Everyday I get up and I continue the journey. I get pissed off, saddened by setbacks, I fall into old familiar brain paths, I vent, I introspect,I forgive myself and keep trying. Stick with me, we’ll get stronger.
0 notes
Text
Urban Hospitals of Last Resort Cling to Life in Time of COVID
Victor Coronado felt lightheaded one morning last month when he stood up to grab an iced tea. The right side of his body suddenly felt heavy. He heard himself slur his words. “That’s when I knew I was going to have a stroke,” he said.
Coronado was rushed to Mercy Hospital & Medical Center, the hospital nearest his home on Chicago’s South Side. Doctors there pumped medicine into his veins to break up the clot that had traveled to his brain.
Coronado may outlive the hospital that saved him. Founded 168 years ago as the city’s first hospital, Mercy survived the Great Chicago Fire of 1871 but is succumbing to modern economics, which have underfinanced the hospitals serving the poor. In July, the 412-bed hospital informed state regulators it planned to shutter all inpatient services as soon as February.
“If something else happens, who is to say if the responders can get my husband to the nearest hospital?” said Coronado’s wife, Sallie.
While rural hospitals have been closing at a quickening pace over the past two decades, a number of inner-city hospitals now face a similar fate. And experts fear that the economic damage inflicted by the COVID-19 pandemic on safety-net hospitals and the ailing finances of the cities and states that subsidize them are helping push some urban hospitals over the edge.
By the nature of their mission, safety-net hospitals, wherever they are, struggle because they treat a large share of patients who are uninsured — and can’t pay bills — or are covered by Medicaid, whose payments don’t cover costs. But metropolitan hospitals confront additional threats beyond what rural hospitals do. State-of-the-art hospitals in affluent city neighborhoods are luring more of the safety-net hospitals’ best-insured patients.
These combined financial pressures have been exacerbated by the pandemic at a time their role has become more important: Their core patients — the poor and people of color — have been disproportionately stricken by COVID-19 in metropolitan regions like Chicago.
“We’ve had three hospital closures in the last year or so, all of them Black neighborhoods,” said Dr. David Ansell, senior vice president for community health equity at Rush University Medical Center, a teaching hospital on Chicago’s West Side. He said the decision to close Mercy “is really criminal in my mind, because people will die as a result.”
Mercy is following the same lethal path as did two other hospitals with largely lower-income patient bases that shuttered last year: Hahnemann University Hospital in Philadelphia, and Providence Hospital in Washington, D.C., which ended its inpatient services. Washington’s only public hospital, United Medical Center — in the city’s poorest ward — is slated to close in 2023 as well, and some services are already curtailed.
Slow Death of Urban Safety Nets
So far, urban hospital closures have remained infrequent compared with the cascading disappearance of their rural counterparts. But the closing of a few could portend problems at others. Even some of those that remain open may cut back crucial specialties like labor and delivery services or trauma care, forcing patients to travel farther for help when minutes can matter.
Nancy Kane, an adjunct professor at Harvard T.H. Chan School of Public Health who has studied urban safety-net hospital changes since 2010, said that “some close, but most of them have tried to get into a bigger system and hang on for a few more years until management closes them.”
For much of the 20th century, most cities ran their own hospitals to care for the indigent. But after the creation of Medicare and Medicaid, and as the rising cost of health care became a burden for local budgets, many jurisdictions turned away from that model. Today only 498 of 5,230 general hospitals in the country are owned by governments or a public hospital district.
Instead, many hospitals in low-income urban neighborhoods are run by nonprofits — often faith-based — and in some cases, for-profit corporations. In recent years owners have unloaded safety-net hospitals to entities with limited patience for keeping them alive.
In 2018, the for-profit hospital chain Tenet Healthcare Corp. sold Hahnemann to Joel Freedman, a California private equity investor, for $170 million. A year later, Freedman filed for bankruptcy on the hospital, saying its losses were insurmountable, while separating its real estate, including the physical building, into another corporation, which could ease its sale to developers.
In 2018, Tenet sold another safety-net hospital, Westlake Hospital in Melrose Park, Illinois, a suburb west of Chicago, to a private investment company. Two weeks after the sale, the firm announced it would close the hospital, which ultimately led the owners to pay Melrose Park $1.5 million to settle a lawsuit alleging they had misled local officials by claiming before the sale they would keep it open.
Some government-run hospitals are also struggling to stay open. Hoping to stem losses, the District of Columbia outsourced management of United Medical Center to private consulting firms. But far from turning the hospital around, one firm was accused of misusing taxpayer funds, and it oversaw a string of serious patient safety incidents, including violations in its obstetrics ward so egregious that the district was forced to shut the ward down in 2017.
Earlier this year, the district struck a deal with Universal Health Services, a Fortune 500 company with 400 hospitals and $11 billion in revenues, to run a new hospital that would replace United, albeit with a third fewer beds. Universal also operates George Washington University Hospital in the city in partnership with George Washington University. That relationship has been contentious: Last year the university accused the company of diverting $100 million that should have stayed in the medical system. In June, a judge dismissed most of the university’s complaint.
No Saviors for Mercy
Chicago has three publicly owned hospitals, but much of the care for low-income patients falls on private safety-net hospitals like Mercy that are near their homes and have strong reputations. These hospitals have been sources of civic pride as well as major providers of jobs in neighborhoods that have few.
Fifty-five percent of Chicagoans living in poverty and 62% of its African American residents live within Mercy’s service area, according to Mercy’s 2019 community needs assessment, a federally mandated report. The neighborhoods served by Mercy are distinguished by higher rates of death from diabetes, cancer and stroke. Babies are more likely to be born early and at low weight or die in infancy. The nearest hospitals from Mercy can be 15 minutes or more away by car, and many residents don’t have cars.
“You’re going to have this big gap of about 7 miles where there’s no hospital,” Ansell said. “It creates a health care desert on the South Side.”
Dr. Maya Rolfe, who was a resident at Mercy until July, said the loss of the hospital’s labor and delivery department would cause substantial harm, especially since African American women suffer from a higher rate of maternal mortality than do white women. “Mercy serves a lot of high-risk women,” she said.
Mercy, a nonprofit, has been in financial trouble for a while. In 2012, it joined Trinity Health, a giant nonprofit Roman Catholic health system headquartered in Michigan with operations in 22 states. In the next seven years, Trinity invested $124 million in infrastructure improvements and $112 million in financial support.
During that time, the hospital continued to be battered by headwinds facing hospitals everywhere, including the migration of well-reimbursed surgeries and procedures to outpatient settings. Likewise, patients with private insurance, which provides higher reimbursements than government programs do, departed to Chicago’s better-capitalized university hospitals, including Rush, the University of Chicago Medical Center and Northwestern Memorial Hospital. Seventy-five percent of Mercy’s revenues come from government insurance programs Medicare and Medicaid.
Only 42% of its beds were occupied on average, according to the most recent state data, from 2018. Mercy told state regulators it is losing $4 million a month and required at least $100 million in additional building upgrades to operate safely.
Trinity said it spent more than a year shopping for a buyer. After that yielded no success, Mercy joined forces with three other struggling South Side hospitals to consolidate into a single health system planning to build one hospital and a handful of outpatient facilities to replace their antiquated buildings. They sought state financial help.
The plan would have cost $1.1 billion over a decade. At the close of the legislative session, Illinois lawmakers — already strapped for funding because of the economic effects of the pandemic — balked at the hospitals’ request for the state to cover half the cost. Lamont Robinson, a Democratic state representative whose district includes Mercy Hospital, said that was because the group did not declare where the new hospital would be built.
“We were all supportive of the merger but not with the lack of information,” Robinson said.
Mercy said in an email that the location would have been chosen after the hospital organizations combined and chose new leaders. Trinity said in a statement: “We are committed to continuing to serve the Mercy Chicago community through investment in additional ambulatory and community-based services that are driven by high-priority community needs.”
Blame for Mercy’s closure has been spread widely to include the city and state governments as well as Mercy’s owner. Trinity Health had $8.8 billion in cash and liquid investments at the end of March and until the pandemic hit had been running a slight profit. Earlier this year in Philadelphia, Trinity Health announced it would phase out inpatient services at another of its safety-net hospitals, Mercy Catholic Medical Center-Mercy Philadelphia Campus, a 157-bed hospital that has been around since 1918.
“People put their money where they want to,” said Rolfe, the former medical resident at Mercy in Chicago. Noting that the city has no qualms about spending large sums to beautify its downtown while other neighborhoods are in danger of losing a major institution, she said: “It shows to me that those patients are not that important as patients that exist in other communities.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
USE OUR CONTENT
This story can be republished for free (details).
Urban Hospitals of Last Resort Cling to Life in Time of COVID published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text
Urban Hospitals of Last Resort Cling to Life in Time of COVID
Victor Coronado felt lightheaded one morning last month when he stood up to grab an iced tea. The right side of his body suddenly felt heavy. He heard himself slur his words. “That’s when I knew I was going to have a stroke,” he said.
Coronado was rushed to Mercy Hospital & Medical Center, the hospital nearest his home on Chicago’s South Side. Doctors there pumped medicine into his veins to break up the clot that had traveled to his brain.
Coronado may outlive the hospital that saved him. Founded 168 years ago as the city’s first hospital, Mercy survived the Great Chicago Fire of 1871 but is succumbing to modern economics, which have underfinanced the hospitals serving the poor. In July, the 412-bed hospital informed state regulators it planned to shutter all inpatient services as soon as February.
“If something else happens, who is to say if the responders can get my husband to the nearest hospital?” said Coronado’s wife, Sallie.
While rural hospitals have been closing at a quickening pace over the past two decades, a number of inner-city hospitals now face a similar fate. And experts fear that the economic damage inflicted by the COVID-19 pandemic on safety-net hospitals and the ailing finances of the cities and states that subsidize them are helping push some urban hospitals over the edge.
By the nature of their mission, safety-net hospitals, wherever they are, struggle because they treat a large share of patients who are uninsured — and can’t pay bills — or are covered by Medicaid, whose payments don’t cover costs. But metropolitan hospitals confront additional threats beyond what rural hospitals do. State-of-the-art hospitals in affluent city neighborhoods are luring more of the safety-net hospitals’ best-insured patients.
These combined financial pressures have been exacerbated by the pandemic at a time their role has become more important: Their core patients — the poor and people of color — have been disproportionately stricken by COVID-19 in metropolitan regions like Chicago.
“We’ve had three hospital closures in the last year or so, all of them Black neighborhoods,” said Dr. David Ansell, senior vice president for community health equity at Rush University Medical Center, a teaching hospital on Chicago’s West Side. He said the decision to close Mercy “is really criminal in my mind, because people will die as a result.”
Mercy is following the same lethal path as did two other hospitals with largely lower-income patient bases that shuttered last year: Hahnemann University Hospital in Philadelphia, and Providence Hospital in Washington, D.C., which ended its inpatient services. Washington’s only public hospital, United Medical Center — in the city’s poorest ward — is slated to close in 2023 as well, and some services are already curtailed.
Slow Death of Urban Safety Nets
So far, urban hospital closures have remained infrequent compared with the cascading disappearance of their rural counterparts. But the closing of a few could portend problems at others. Even some of those that remain open may cut back crucial specialties like labor and delivery services or trauma care, forcing patients to travel farther for help when minutes can matter.
Nancy Kane, an adjunct professor at Harvard T.H. Chan School of Public Health who has studied urban safety-net hospital changes since 2010, said that “some close, but most of them have tried to get into a bigger system and hang on for a few more years until management closes them.”
For much of the 20th century, most cities ran their own hospitals to care for the indigent. But after the creation of Medicare and Medicaid, and as the rising cost of health care became a burden for local budgets, many jurisdictions turned away from that model. Today only 498 of 5,230 general hospitals in the country are owned by governments or a public hospital district.
Instead, many hospitals in low-income urban neighborhoods are run by nonprofits — often faith-based — and in some cases, for-profit corporations. In recent years owners have unloaded safety-net hospitals to entities with limited patience for keeping them alive.
In 2018, the for-profit hospital chain Tenet Healthcare Corp. sold Hahnemann to Joel Freedman, a California private equity investor, for $170 million. A year later, Freedman filed for bankruptcy on the hospital, saying its losses were insurmountable, while separating its real estate, including the physical building, into another corporation, which could ease its sale to developers.
In 2018, Tenet sold another safety-net hospital, Westlake Hospital in Melrose Park, Illinois, a suburb west of Chicago, to a private investment company. Two weeks after the sale, the firm announced it would close the hospital, which ultimately led the owners to pay Melrose Park $1.5 million to settle a lawsuit alleging they had misled local officials by claiming before the sale they would keep it open.
Some government-run hospitals are also struggling to stay open. Hoping to stem losses, the District of Columbia outsourced management of United Medical Center to private consulting firms. But far from turning the hospital around, one firm was accused of misusing taxpayer funds, and it oversaw a string of serious patient safety incidents, including violations in its obstetrics ward so egregious that the district was forced to shut the ward down in 2017.
Earlier this year, the district struck a deal with Universal Health Services, a Fortune 500 company with 400 hospitals and $11 billion in revenues, to run a new hospital that would replace United, albeit with a third fewer beds. Universal also operates George Washington University Hospital in the city in partnership with George Washington University. That relationship has been contentious: Last year the university accused the company of diverting $100 million that should have stayed in the medical system. In June, a judge dismissed most of the university’s complaint.
No Saviors for Mercy
Chicago has three publicly owned hospitals, but much of the care for low-income patients falls on private safety-net hospitals like Mercy that are near their homes and have strong reputations. These hospitals have been sources of civic pride as well as major providers of jobs in neighborhoods that have few.
Fifty-five percent of Chicagoans living in poverty and 62% of its African American residents live within Mercy’s service area, according to Mercy’s 2019 community needs assessment, a federally mandated report. The neighborhoods served by Mercy are distinguished by higher rates of death from diabetes, cancer and stroke. Babies are more likely to be born early and at low weight or die in infancy. The nearest hospitals from Mercy can be 15 minutes or more away by car, and many residents don’t have cars.
“You’re going to have this big gap of about 7 miles where there’s no hospital,” Ansell said. “It creates a health care desert on the South Side.”
Dr. Maya Rolfe, who was a resident at Mercy until July, said the loss of the hospital’s labor and delivery department would cause substantial harm, especially since African American women suffer from a higher rate of maternal mortality than do white women. “Mercy serves a lot of high-risk women,” she said.
Mercy, a nonprofit, has been in financial trouble for a while. In 2012, it joined Trinity Health, a giant nonprofit Roman Catholic health system headquartered in Michigan with operations in 22 states. In the next seven years, Trinity invested $124 million in infrastructure improvements and $112 million in financial support.
During that time, the hospital continued to be battered by headwinds facing hospitals everywhere, including the migration of well-reimbursed surgeries and procedures to outpatient settings. Likewise, patients with private insurance, which provides higher reimbursements than government programs do, departed to Chicago’s better-capitalized university hospitals, including Rush, the University of Chicago Medical Center and Northwestern Memorial Hospital. Seventy-five percent of Mercy’s revenues come from government insurance programs Medicare and Medicaid.
Only 42% of its beds were occupied on average, according to the most recent state data, from 2018. Mercy told state regulators it is losing $4 million a month and required at least $100 million in additional building upgrades to operate safely.
Trinity said it spent more than a year shopping for a buyer. After that yielded no success, Mercy joined forces with three other struggling South Side hospitals to consolidate into a single health system planning to build one hospital and a handful of outpatient facilities to replace their antiquated buildings. They sought state financial help.
The plan would have cost $1.1 billion over a decade. At the close of the legislative session, Illinois lawmakers — already strapped for funding because of the economic effects of the pandemic — balked at the hospitals’ request for the state to cover half the cost. Lamont Robinson, a Democratic state representative whose district includes Mercy Hospital, said that was because the group did not declare where the new hospital would be built.
“We were all supportive of the merger but not with the lack of information,” Robinson said.
Mercy said in an email that the location would have been chosen after the hospital organizations combined and chose new leaders. Trinity said in a statement: “We are committed to continuing to serve the Mercy Chicago community through investment in additional ambulatory and community-based services that are driven by high-priority community needs.”
Blame for Mercy’s closure has been spread widely to include the city and state governments as well as Mercy’s owner. Trinity Health had $8.8 billion in cash and liquid investments at the end of March and until the pandemic hit had been running a slight profit. Earlier this year in Philadelphia, Trinity Health announced it would phase out inpatient services at another of its safety-net hospitals, Mercy Catholic Medical Center-Mercy Philadelphia Campus, a 157-bed hospital that has been around since 1918.
“People put their money where they want to,” said Rolfe, the former medical resident at Mercy in Chicago. Noting that the city has no qualms about spending large sums to beautify its downtown while other neighborhoods are in danger of losing a major institution, she said: “It shows to me that those patients are not that important as patients that exist in other communities.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
USE OUR CONTENT
This story can be republished for free (details).
from Updates By Dina https://khn.org/news/urban-hospitals-of-last-resort-cling-to-life-in-time-of-covid/
0 notes
Text
America's opioid crisis has become an “epidemic of epidemics”
America's opioid crisis has become an “epidemic of epidemics”

A memorial calling into question God's existence in Huntington, West Virginia, on April 20, 2017. Brendan Smialowski/AFP/Getty Images
Rising intravenous drug use has created new public health epidemics of hepatitis C and deadly bacterial infections.
On the one hand, the young mother who came into the Kanawha-Charleston Health Department clinic in Charleston, West Virginia, last fall had good news for the doctors there: She'd been off heroin for four days.
Yet she was far from well. She had a painful dental abscess in her jaw that was causing yellow pus to drain out of her ear. She had hepatitis C. She'd recently missed her period and was worried she might be pregnant with her third child.
The staff at the clinic, which is also a needle exchange, told me they estimate that at least 70 percent of their patients who use intravenous drugs are seeking not just fresh needles but treatment for hepatitis C, which they developed during drug use and can cost $20,000 to $90,000 to treat per person. Others have another kind of dangerous infection called bacterial endocarditis, or a combination of the two.
The United States often measures the severity of its opioid crisis in drug overdose deaths. Driven by prescription opioids, heroin, and the deadly synthetic opioid fentanyl, drug overdoses claimed 64,000 lives in 2016 alone, more than the entire death toll during the Vietnam War.

Brendan Smialowski/AFP/Getty Images
Paraphernalia for smoking and injecting drugs after it was found during a police search in Huntington, West Virginia, on April 19, 2017.
But on top of the skyrocketing overdoses, there is a related public health crisis that's largely overlooked and gravely underfunded. Opioid and heroin use is causing a dramatic spike in new hepatitis C infections, as well as dangerous bacterial infections that, if left untreated, can cause strokes and require multiple open-heart surgeries. Doctors and public health officials also fear America is on the brink of more HIV outbreaks, driven by intravenous drug use.
With the federal government slow to act, small needle exchange clinics like the one run by Charleston's city health department are on the front lines, desperately trying to stop or slow the spread of these infections by treating them and encouraging patients to seek addiction treatment.
“This really is an epidemic of epidemics,” said Dr. Michael Brumage, the Charleston health department's executive director. “The number of overdoses does not convey the full scope of the tragedy that's playing out in front of us.”
Lawmakers and federal officials often cite $45 billion as the amount of money needed to treat the drug crisis, but experts say the real number to treat addiction and disease brought on by drugs is likely four times that. It would account for costs like curing hepatitis C ($20,000 to $90,000 per person) and open-heart surgery for bacterial endocarditis ($100,000 to $200,000). A bipartisan spending bill Congress passed last month contains $6 billion in funding for opioid abuse and mental health treatment, which local officials say is nowhere close to what's needed.
With little help from the federal government, clinics like Kanawha-Charleston are badly underresourced in their fight against drugs and the diseases they cause.
“I feel like I probably just see the tip of the iceberg on this because I'm typically seeing the sickest folks in the hospital”
America's opioid epidemic started in the 1990s and early 2000s when doctors began prescribing opioids for pain. Due to a combination of factors, including pharmaceutical companies pushing pills, doctors believing the drugs were safe, and incentives for a fast, efficient health care system that prioritized quick fixes, opioid prescriptions proliferated. The US is by far the leading prescriber of opioids in the world.
As prescriptions for addictive opioids like OxyContin became harder to come by, some people turned to heroin.

But the proliferation of intravenous drug use has led to a syndemic, or “multiple diseases feeding off of one another,” according to Tufts University public health professor Thomas Stopka.
One risk is infections from dirty needles, injection tools, and water to mix drugs. People often think of shared needles as the culprit for infection, but simply using the same needle or spoon to cook drugs multiple times is also a risk factor, as is not sanitizing skin or needles with rubbing alcohol.
Then there's the matter of what's actually being injected. Some drug users in Charleston use toilet water to mix their drugs, according to clinic staff. Sometimes, they'll draw water out of the brown, silty Kanawha River, said Abdul Muhammad, 56, a local Charleston resident and drug user who attended a Narcan training session at the clinic this fall.
“A lot of people are careless,” Muhammad said, speaking of the young drug users he sees. “They don't get the capacity of the dangers.”
When bacteria builds up in needles or in the cookers used to mix drugs, it gets shot into a person's bloodstream along with the drug, where it can travel anywhere throughout the body. Bacterial infections like this are called endocarditis; they are most dangerous when they reach the heart valve, causing nodules of bacteria to build up.
“If the infection is left unchecked and undiagnosed, it can become several inches in length and width and look like a sail billowing throughout the heart chamber,” said Dr. Jonathan Eddinger, a cardiologist at Catholic Medical Center in Manchester, New Hampshire.
There are 40,000 to 50,000 new cases of bacterial endocarditis in the US each year, but it's not known exactly how many come from injecting drug use. One study found the prevalence of drug-induced endocarditis and other serious infections nearly doubled between 2002 and 2012, from about 3,421 cases nationwide to 6,535.
What's particularly worrying about the potential rise of these infections among drug users it that on average, they cost more than $120,000 per patient to treat. Out of the $15 billion hospitals billed to treat opioid patients in 2012, more than $700 million went to treating patients with infections.
Catholic Medical Center is one of the two main hospitals in New Hampshire's largest city, and it has seen a sharp rise in bacterial endocarditis. In 2008, doctors saw one or two cases of infected heart valves per month. By 2016, that had risen to about eight to nine cases per month, Eddinger said.
“The number is probably enormous,” he said. “I feel like I probably just see the tip of the iceberg on this because I'm typically seeing the sickest folks in the hospital.”
Sometimes patients require multiple complicated surgeries, including open-heart surgery, with no guarantee that one will be enough if the patient can't stay clean.
Endocarditis patient James Pernal found that out the hard way, after about six or seven years of IV drug use. Vox contacted Pernal on the online forum Reddit after he wrote about his experience on a page for people who had experienced bacterial endocarditis. When Pernal messaged back, he was in still the hospital, recovering from his latest bout of the infection. Earlier in the year, endocarditis had given him his first stroke and nearly killed him, he said.
“When I got to the hospital I was rushed to ICU,” Pernal wrote. “Had no idea I had a vegetation growing in my mitral valve. It ended up going into my brain causing the stroke.”
“You don't really feel anything from endocarditis,” he added. “It's not painful, but after being on antibiotics in hospital for a month, the corrosion and plaque on the exterior of my heart traveled to my foot, causing it to turn purple and look like Freddy Krueger's face. They said it could have gone to my internal organs and killed me overnight so I was lucky it just went to my foot.”
If caught early enough, an infection can be cleared up with an intensive regimen of antibiotics. But if it gets worse, patients as young as 20 or 30 are at risk of stroke. Doctors have to perform open-heart surgery to replace the infected heart valve, which can cost between $100,000 and $200,000. Patients often don't see a doctor until they realize something is seriously wrong with them, which is complicated by stigma or fear that the police could get involved, Eddinger said.
“We don't get them regularly until they're very ill,” he said. “They're embarrassed, quite honestly.”
After his stroke and the infection in his foot, Pernal couldn't walk for a few weeks, and he eventually had to have open-heart surgery so that doctors could repair his damaged valves. Pernal estimated he spent a third of 2017 in hospitals from an infection he got from dirty needles.
“Mostly, people get it from dirty needles,” he wrote. “I can't stress using a clean needle each time you dose. Honestly though I'd stress not even to go IV route. It's not worth the damage it can do. It's a way bigger issue than addicts think. Everyone thinks it won't happen to them, but it can and will.”
Cases of hepatitis C associated with intravenous drug use are rising too
Another serious unintended consequence of the opioid crisis is the fast-rising rate of hepatitis C, a virus that spreads quickly through dirty needles. The United States has seen a threefold increase in hepatitis C cases over the past five years; the number of new cases rose from 853 in 2010 to 2,436 in 2015, according to the Centers for Disease Control and Prevention.
The opioid crisis has spurreda dramatic risein hepatitis C infections, especially among younger users. Between 2004 and 2014, there was a 400 percent increase in hepatitis C infections in Americans ages 18 to 29, according to the CDC. There's a similarly bleak picture for people ages 30 to 39, with a 325 percent increase in infections.
New research by the CDC suggests that this spike in hepatitis C infection rates is associated with a rise in intravenous drug use. As government researchers analyzed national and state data, they found infection rates rising at a similar trajectory to hospital admissions for opioid injection.
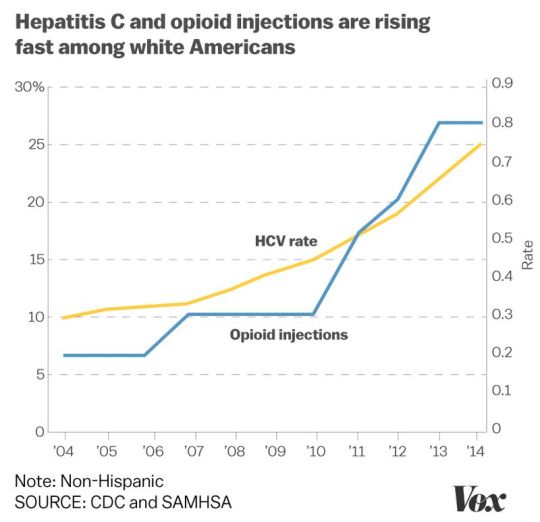
Christina Animashaun/Vox
Part of the reason hepatitis C rates are spiking so much is the virus is much more resilient than other viruses like HIV. Whereas the HIV virus dies quickly outside the body, the HCV virus (which causes hepatitis C) can survive longer and therefore is easier to transmit. If left untreated, hepatitis C can cause liver cancer or cirrhosis.
In West Virginia, the state arguably hardest hit by opioid addiction, hepatitis C cases have tripled in just the past three years, according to Dr. Rahul Gupta, West Virginia's health commissioner. Rural areas had more than double the rate of cases as in urban areas, according to a 2015 report from the CDC.

Brendan Smialowski/AFP/Getty Images
A woman suspected of acting under the influence of heroin shows her arms to local police in Huntington, West Virginia, on April 19, 2017.
The good news is that there is a cure for hepatitis C; the bad news is that the cheapest course of treatment costs more than $20,000 and ranges all the way up to $90,000. Therefore, many state Medicaid programs have strict rules around paying for treatment.
One of the first patients at the Kanawha-Charleston clinic on a rainy fall day had recently discovered he was positive for the disease. (Clinic staff estimate 70 percent of the patients who come in have contracted hepatitis C through IV drug use.)
The man was soft-spoken and polite, with shaved silver hair, weathered skin, and holes in the knees of his jeans. He was carrying a black messenger bag full of used needles, which tumbled out into a plastic collection box when he turned it upside down. He asked clinic volunteer Sarah Embrey whether his insurance would pay for the hepatitis C cure. Embrey, a local pharmacist, looked at his state Medicaid card.
“You've got to be clean,” she told him.
West Virginia's Medicaid program only pays for it once in a person's lifetime, and if the patient is addicted to opioids, he needs to demonstrate he's been sober before insurance pays for the cure.
The man nodded. He said he had recently kicked heroin but was still shooting crystal meth.
“I feel like that was a big step,” he said.
“Syndemic” diseases feeding off each other cost our health system billions of dollars
It costs tens of thousands to perform open-heart surgery on a patient who has bacterial endocarditis. And there's no guarantee one surgery will be enough if patients continue to inject drugs. Eddinger has seen the same person in for a heart valve replacement multiple times; in fact, 25 percent of endocarditis patients in his hospital are repeat patients, about 250 over the past five years.
Not only is surgery costly, but the risk of complications goes up each time one is performed. The risk “goes up exponentially as they go in, and these folks aren't coming in healthy to begin with; they're coming in sick,” Eddinger said.
For all these reasons, University of Kentucky researcher Dr. Laura Fanucchi is adamant that evidence-based treatment like Suboxone, therapy, and counseling need to be offered to bacterial endocarditis patients, so that there's less of a chance they'll land back in the hospital in need of a second surgery.

Spencer Platt/Getty Images
A second bout of endocarditis “is often worse than the first, and these are young people,” Fanucchi said. “It's devastating.”
With little help coming from the federal government, needle exchanges are racing against time
Public health officials across the country are fearful that the drug crisis could precipitate an HIV outbreak. This happened in Indiana in 2015, when about 190 people were diagnosed with HIV from shared needles. The outbreak convinced the state's then-governor, Mike Pence, to allow needle exchanges to open up access to clean needles. It helped get the state's crisis under control, but even so, the cost to the state was vast.
Officials estimated each patient diagnosed with HIV would take $1 million of state money when health care and public assistance was factored into the total cost. That meant taxpayers were looking at paying at least $190 million to take care of 190 people. And that's just in one state.
Needle exchanges serve a dual purpose: making sure drug users are injecting with clean equipment to prevent infection, and getting dirty needles off the streets and disposed of properly. There is a collection box outside the health department that can hold 38 gallons of needles; it was full in the first five days. Once Charleston city officials collect the needles, they have a machine that sanitizes and crushes them up, turning them into small pieces of plastic that can be disposed of.

Robert Nickelsberg/Getty ImagesUsed syringes in the bottom of a trash bin at Howard Center in Burlington, Vermont, on May 24, 2016. The center provides a needle exchange program, supplies, counseling, and other services.
The Charleston health department only runs the clinic for five hours per day, one day per week, typically seeing about 400 people in that time. Most people come in for the clean needles, cookers, and cotton swabs, while others are seeking medical attention.
Needle exchanges are controversial because some people believe they enable drug use, but multiple studies have found them to be effective at reducing infection rates among drug users. In Charleston, the city's needle exchange has partnered with local doctors and behavioral health specialists to provide even more services to the local population - treating flesh wounds and infections in the clinic and trying to get drug users into treatment.
The price tag often cited by the White House and Congress to treat America's opioid crisis is $45 billion - though there's little sign that amount will ever be allocated. And experts say that's just a quarter of what's needed. If you take into account the costs of treating the diseases associated with addiction like hepatitis C and bacterial endocarditis, the number is closer to $186 billion over a decade, according to Dr. Richard Frank, a health economist at Harvard.
This gets to another problem public health providers are seeing: It's much easier to get addicted in America than it is to get clean. A 2016 report by the surgeon general found that just 10 percent of Americans with a drug use disorder obtain specialty treatment.
Clinic staff in West Virginia can hand out clean needles, treat wounds, and encourage people to seek treatment, but in many states, there are not enough available beds at treatment facilities and not enough drug maintenance programs offering Suboxone or methadone to meet the needs of Americans with drug addiction.
Preventive and harm reduction programs like the Kanawha-Charleston clinic in West Virginia cost money upfront, but if they are able to prevent the spread of bacterial endocarditis, hepatitis C, and HIV in their area, they could ultimately save the taxpayers a lot of money in the long run, the Charleston health department's Brumage said.
“If we prevent one to two cases of endocarditis, this program pays for itself,” he said.
Join the conversation
Are you interested in more discussions around health care policy? Join our Facebook community for conversation and updates.
via America's opioid crisis has become an “epidemic of epidemics”
0 notes
Text
It Feels A Lot Like 2007 Again: Reflecting On The Previous Peak
Reflection helps us appreciate how far we’ve come. Reflection also helps us learn from our mistakes. In this post, I’d like everybody to reflect on several key items: Career, Finances, Health, Family, and Happiness. See if you can tie the five together and weave a story about who you are today.
The one thing I know for sure is that 2017 feels a lot like it did 10 years ago. But this time, every asset class is expensive. I’ve got folks asking me about investing in cryptocurrencies when they haven’t even invested in stocks. Other folks are asking whether they should use their HELOC to buy another property with an 80% loan-to-value ratio. Everybody has maximum investing FOMO right now!
It’s an exhilarating time, but it’s also a perilous time for those who don’t have perspective.
Life In 2007
Career: I was finishing up my third year as a VP at a large investment bank in San Francisco. 2007 was also the year I turned 30. Given my boss recently departed to become a client, I was left to take over the west coast business. Knowing my worth, I asked for a raise and a promotion and got them. If they lost me to a competitor, they would have been screwed for at least six months as they scrambled to find and train my replacement.
30 years old was a significant age because I finally felt like I could be taken seriously. Getting my MBA in 2006 also gave me a confidence boost. I was loving my career because I was finally my own boss in San Francisco. Sure, I had to work with the head of the office and a more senior colleague in a different department, but for the most part, I was free to control my own schedule. So long as the business was coming in, nobody could complain.
In 2007, I thought I could easily work for 10 more years and then call it quits for good. Little did I know the financial crisis would crush my industry and cause me to pursue a different path just four years later.
Related: A List Of Career Limiting Moves To Blow Up Your Future
Finances: I received the biggest bonus of my life in 2007 due to a negotiation I had with my big boss in Hong Kong. It was a handshake agreement, so you never know until the end of the year when bonuses are paid. But he delivered as promised. From that day on, I decided to be loyal until the very end.
Although the stock market was booming, I was still hesitant to go all-in due to the dotcom bubble that began to collapse in 2000. Instead of investing everything I had in the stock market, I decided to invest most of my savings in real estate. At least with real estate, if all went to hell, I’d still have something to sleep in.
I bought my first SF property in 2003, lived in it for two years, and was renting it out to a couple in 2007. In 2005, I decided to take out a $1,200,000 mortgage and buy a single family house in the Marina district for $1,523,000. It was the cheapest house for its size in the neighborhood because it was on a busy block next to the busiest street.
Because my real estate investing experience was positive, and I had just received a big bonus, I decided to buy a $718,000, 2/2 vacation condo at The Resort At Squaw Creek, Lake Tahoe in 2007. I loved the place because that’s where I took my girlfriend on our first getaway date back in 2001.
I was delirious about my financial luck and felt I just couldn’t lose. I was imagining that my compensation would continue to grow by 10-20% a year for the next five years. There were some warning signs about the stock market and real estate market getting ahead of themselves, but I didn’t listen carefully. Instead, I myopically focused on my fortunate career situation. I wish someone with decades of experience sat down with me to run through the pros and cons of buying more property then.
Notice the frequency. Nobody know when the next downturn will begin.
Health: Work was stressful given the 60-70 hour work weeks. But at least my chronic back pain from 2000-2003 was gone. But what replaced my chronic back pain was teeth grinding and TMJ. It hurt to speak for more than an hour. I remember paying $700 to a specialist dentist who ground down parts of my molars so I could get some relief when I closed my jaw.
I was in OK shape because I started aggressively playing tennis again. But of course, I suffered from occassional tennis elbow pain that kept me from swinging freely. I weighed between 162-165 lbs, which was a normal weight for someone 5’10” tall.
Now when I look back on my diet, I realize I ate extremely unhealthy due to frequent client entertainment. I’d often take clients to fancy steak restaurants and nice lounges. The wagyu beef and Moscow Mules tasted especially good thanks to a corporate card with a $200/head budget.
I remember telling myself that no matter what, living in San Francisco was healthier than living in Manhattan.
Family: My girlfriend graduated college in 3.5 years and came out to live with me in December 2001. She was 27 in 2007, and I was unsure whether starting a family was a good idea yet. Work was extremely busy and I had all this pressure to keep the ship afloat given my boss left.
But I knew she was the one, so I proposed during the heart of the financial crisis in 2008. We got married in Hawaii in December 2008.
If the financial crisis didn’t hit, I would have been more confident to start a family by 2010. It would have been nice to get parental leave and company benefits. Further, since our son is the best thing that has ever happened to us, he would have been in our lives for seven years longer.
It’s so difficult to figure out when is the best time to have children. Even if you decide now is the time, it might take several years to conceive.
What I do know is that having a life partner through my entire post college journey has been priceless.
Related: When Is the Best Time To Have Children? A Physical And Financial Decision
Happiness: I was ecstatic about getting a raise and a promotion. Part of my happiness stemmed from having gone to public high school and public university. Never in my wildest dreams had I thought I’d have a job at a respectable investment bank and earn a healthy income. If I had gone to an elite private school, I’m not sure I’d be as happy because I would have expected all these things and more.
It’s funny, but the memories that stands out most from this time period were figuring out what ring to buy and the cozy little wedding on our favorite beach in Hawaii the next year.
My happiness level has never really fluctuated much since graduating from college in 1999. It’s always been about a 7-8 out of 10. The happiness of getting recognized at work only lasted for maybe three months. The pressure to deliver took over.
Life in 2017 And Beyond
The most important thing I learned from 10 years ago is thinking that I couldn’t lose, and then losing big when the financial crisis hit in 2008. I remember swearing to myself in 2010 that if my investments ever came back to pre-crisis levels I would take some money off the table. I tried to do so in 2012 by selling my primary residence in order to pay off a ~$1,000,000 mortgage and live in a small two bedroom, one bathroom apartment. But nobody wanted to buy my four bedroom house.
The difference with 30 year olds in 2017 versus my 30 year old self in 2007 is that I went through the dotcom collapse in 2000. I saw paper millionaires end up with nothing within a couple years. They had to start all over, like the guy who made my breakfast croissant each morning. As a result, I tried to diversify as much as possible.
It’s hard to really know how scary recessions can be if you’ve never been in one with significant money at stake. Everybody likes to say they’ll hold on to their investments and buy more during a downturn. But when your investments are down 30%+ and many of your colleagues are getting fired, the first thing you do is think about survival, not dumping every last cent you have in the stock market.
I’m praying that I’ll finally be satisfied with what I have today and no longer grind as hard. My health depends on it. Staying in San Francisco and being surrounded by so many success stories has finally taken its toll. My recent bout of chronic back pain reminded me not to forget the point of financial independence and owning a lifestyle business: a better life.
Some Final Thoughts
* It’s easy to extrapolate explosive growth in your career and net worth in a bull market. The problem is, nobody wants to work forever and things always change. Be more conservative with your expectations. Don’t confuse brains with a bull market.
* No matter how much money you make or have, your steady state of happiness won’t really change. Stop thinking that if you get to X amount you will be happy. Retire by a certain age, not a financial figure. There will always be something that will give make you feel bad. But the good thing is, you’ll likely revert back to your steady state.
* If you’re relatively young (under 40), it’s worth swinging for the fences during the good times. It’s worth allocating some funny money to chase unicorns. Money is abundant and cheap. Once the spigot shuts off, dumb ideas no longer get funded and silly job offers are no longer given.
* Learn when to cash in your chips by setting goals. You made these goals because you decided how much was enough. If you’ve somehow found yourself way beyond your goals, then absolutely focus on using your profits for a better life. The saddest thing is losing a massive lead.
* Even if you buy at an inopportune time, if you wait long enough, you’ll likely eventually get back to even. Just look at us now.
* The next 10 years will go by faster than the previous 10 years. Make the most of it.
Related: Recommended Net Worth Allocation By Age Or Work Experience
I’d love to hear about where you were 10 years ago, and what you learned about yourself then that you will apply to your life now? Time truly accelerates the older we get. Let us not waste a single minute.
The post It Feels A Lot Like 2007 Again: Reflecting On The Previous Peak appeared first on Financial Samurai.
from https://www.financialsamurai.com/feels-lot-like-2007-again/
0 notes