#ehr interoperability software
Explore tagged Tumblr posts
Text
Healthcare Interoperability Standards: What Providers Must Know

Healthcare interoperability aims to provide a secure way for numerous systems to access, exchange, and cooperatively use patient information. Thus, interoperability in healthcare allows public health administrators, providers, payers, and patients to quickly and easily view information.
Crucial interoperability elements include open data schemes and standards. Therefore, using healthcare interoperability systems, providers can share data. In addition, patients can use a variety of channels to access their information, including kiosks and mobile devices.
Understanding Interoperability Standards
Health Information Exchange (HIE) refers to the capacity of systems on a network to communicate with one another. With HIE healthcare communication, clinicians should be able to consolidate, share, and use data.
In addition, HIE systems must be able to exchange data in a way that makes it easily accessible, but secure, and accurate. Furthermore, throughout this process, there should be very little need for human interaction.
Using interoperability, clinicians can access patient information despite their location or which type of Electronic Health Records (EHR) software they’re using.
With healthcare interoperability, clinicians and patients enjoy a seamless exchange of information. In addition, patient care and health outcomes will improve, and healthcare will become more cost-effective.
Read More: https://prognocis.com/healthcare-interoperability-standards-what-you-should-know/
#interoperability standards#ehr software#ehr interoperability software#electronic health record software#progocis ehr
0 notes
Text

A Updated Guide to Healthcare Informatics Software
The current state of healthcare is characterized by an ongoing data flood and an increasing focus on digital effectiveness. A key component of this revolution is healthcare informatics software, which gives clinicians the means to improve patient care, streamline processes, and glean insightful information from enormous medical databases. For healthcare workers at every stage of their employment, this thorough reference is a useful resource.
#mHealth app#Healthcare information technology#healthcare software development#Healthcare’s EHR Interoperability#healthcare interoperability#electronic health records#Healthcare Informatics Software
0 notes
Text
Breaking Down Barriers: The Importance of Interoperability in Healthcare
In today's digital age, the adoption of Electronic Health Record (EHR) software has transformed the way healthcare providers manage patient information and deliver care. EHR solutions streamline processes, enhance communication, and improve patient outcomes. However, one critical factor that can significantly impact the effectiveness of EHR systems is interoperability. Let's explore why interoperability matters in healthcare and how it can benefit patients, providers, and the healthcare ecosystem as a whole.

What is Interoperability in Healthcare?
Interoperability refers to the ability of different healthcare systems, software, and devices to securely exchange and use patient information seamlessly. In other words, interoperability enables EHR solutions��from different vendors to communicate with each other and share data efficiently, regardless of the platform or technology used.
Why Does Interoperability Matter?
Enhanced Care Coordination: Interoperability enables healthcare providers to access comprehensive patient information from various sources in real-time, facilitating seamless care coordination across different specialties, settings, and organizations. This ensures that providers have a complete picture of a patient's medical history, medications, allergies, and treatment plans, leading to more informed decision-making and better outcomes.
Improved Patient Safety: By promoting the exchange of accurate and up-to-date patient information, interoperability helps reduce the risk of errors, duplicate tests, and adverse drug events. This enhances patient safety and reduces the likelihood of medical errors that can result from incomplete or fragmented health records.
Efficient Workflow: Interoperable EHR software solutions streamline workflows by eliminating the need for manual data entry, faxing, and paper-based processes. This saves time, reduces administrative burden, and allows healthcare providers to focus more on patient care, ultimately improving efficiency and productivity.
Empowered Patients: Interoperability gives patients greater control over their health information, allowing them to access and share their medical records securely with other healthcare providers as needed. This promotes patient engagement, empowers individuals to take an active role in their healthcare decisions, and fosters collaboration between patients and providers.
Interoperability Standards: To achieve seamless data exchange, interoperability standards such as HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) play a crucial role. These standards establish common formats, protocols, and vocabularies for exchanging health information, ensuring compatibility and consistency across different systems.
Interoperability and Population Health Management: Interoperable EHR solutions facilitate population health management initiatives by aggregating and analyzing data from diverse sources. This enables healthcare organizations to identify trends, track outcomes, and implement targeted interventions to improve the health of entire patient populations.
Conclusion
In an increasingly interconnected healthcare landscape, interoperability is essential for optimizing patient care, improving clinical outcomes, and driving innovation. By breaking down data silos and enabling seamless information exchange, interoperable EHR software solutions empower healthcare providers to deliver more coordinated, efficient, and patient-centered care.
At Meditab, we recognize the critical role that interoperability plays in advancing healthcare delivery. Our comprehensive EHR solution is designed to promote interoperability, enabling seamless data exchange and collaboration across the healthcare continuum. To learn more about our interoperable EHR software solution and how it can benefit your practice, visit our website here or contact us today.
Together, let's embrace interoperability and harness the power of connected health to transform the future of healthcare delivery.
#ehr software#ehr solutions#ehr software companies#ehr integration#interoperability#interoperability healthcare
0 notes
Text
Healthcare IT Integration Market Size Expected to Reach USD 11.16 Billion by 2030
The global Healthcare IT Integration market size, which was valued at USD 4.38 billion in 2022, is anticipated to witness remarkable growth, reaching USD 11.16 billion by 2030. This projection reflects a robust Compound Annual Growth Rate (CAGR) of 12.4% over the forecast period spanning from 2023 to 2030.
The increasing demand for efficient healthcare delivery systems, coupled with the rising adoption of electronic health records (EHRs) and other digital solutions, is driving the growth of the Healthcare IT Integration market. Healthcare organizations worldwide are realizing the significance of integrating disparate systems and applications to streamline workflows, improve patient care, and enhance operational efficiency.
Key Market Segments:
The Healthcare IT Integration market is segmented by Products & Services type, End User, and Regions:
Products & Services Type:
Products: Interface Engines, Media Integration Software, Medical Device Integration Software, Other Integration Tools
Services: Support and Maintenance Services, Implementation and Integration Services (Training and Education Services, Consulting Services)
End User:
Hospitals
Clinics
Diagnostic Imaging Centers
Laboratories
Other End Users
Regions: The global market forecast covers various regions across the globe.
Market Outlook:
The increasing adoption of electronic health records (EHRs) and healthcare information exchange (HIE) solutions is propelling the demand for Healthcare IT Integration products and services. Interface engines and integration software play a pivotal role in connecting disparate systems within healthcare organizations, enabling seamless data exchange and interoperability.
Moreover, the emergence of advanced technologies such as artificial intelligence (AI), machine learning (ML), and blockchain in healthcare is further driving the need for robust IT integration solutions. These technologies require seamless integration with existing healthcare IT infrastructure to harness their full potential in improving patient outcomes and optimizing healthcare processes.
As healthcare providers continue to prioritize interoperability and data exchange to support value-based care initiatives and enhance patient engagement, the demand for Healthcare IT Integration solutions is expected to witness significant growth in the coming years.
2 notes
·
View notes
Text
An API developer in DigitalAPICraft Company thinks API will revolutionize the healthcare ecosystem
The rise of digital health solutions has transformed how we approach healthcare. APIs play a major role in this transformation, enabling seamless integration with existing systems and data sources. For instance, wearable devices and mobile health applications can utilize APIs to seamlessly transmit health data to EHRs, enabling healthcare providers to monitor patients remotely and gain valuable insights into their health status. API also enables the integration of telemedicine platforms, which allows patients to easily schedule medical appointments, securely share their medical information, and receive virtual care. APIs are sets of rules and protocols that allow different software applications to communicate and interact with each other. Here's how APIs could potentially revolutionize the healthcare ecosystem:
Innovation and Development: APIs can encourage innovation by allowing developers to create new applications and services that leverage healthcare data. For instance, wearable devices and health monitoring apps can connect to APIs to provide patients and healthcare providers with real-time health data.
Data Exchange and Integration: APIs can facilitate the secure exchange of patient data between healthcare providers, hospitals, clinics, and even patients themselves. This can lead to more coordinated and efficient care, as healthcare professionals can access the information they need in real-time.
Patient Empowerment: APIs can empower patients by giving them access to their own health data. Patients can use this data to make informed decisions about their health and share it with different healthcare providers as needed.
Research and Analytics: APIs can make it easier for researchers to access and analyze large sets of anonymized healthcare data for epidemiological studies, clinical trials, and medical research.
Security and Compliance: While APIs offer many benefits, data security and patient privacy are critical concerns in healthcare. Implementing robust security measures and complying with relevant regulations like HIPAA (Health Insurance Portability and Accountability Act) is essential when developing healthcare APIs.
Personalized Healthcare: APIs can enable the integration of patient data from various sources, which can then be used to provide personalized treatment plans and recommendations. This can lead to more effective treatments tailored to individual patients.
Telemedicine and Remote Monitoring: APIs can play a crucial role in telemedicine by enabling video consultations, remote patient monitoring, and virtual healthcare services. This is especially important in situations where in-person visits are challenging or not feasible.
Data Exchange and Integration: APIs can facilitate the secure exchange of patient data between healthcare providers, hospitals, clinics, and even patients themselves. This can lead to more coordinated and efficient care, as healthcare professionals can access the information they need in real-time.
Interoperability: APIs can enable different healthcare systems, such as electronic health records (EHR) platforms, medical devices, and mobile applications, to seamlessly exchange data and share information. This can lead to improved patient care by providing healthcare providers with a comprehensive view of a patient's medical history and data.
The API developer's belief in the revolutionary potential of APIs in the healthcare ecosystem is well-founded. However, it's important to recognize that while APIs offer tremendous opportunities, they also come with challenges that need to be carefully addressed to ensure the safe and effective use of healthcare data. One APIMarketplace comes with a package of features and benefits, which can totally change the way you run your organization and provide you with a much more efficient and hassle-free system, leading you to better results. So don’t wait visit DigitalAPICraft.com and get a free demo of One APIMarketplace today.
For more information: https://digitalapicraft.com/

2 notes
·
View notes
Text
Leading Benefits of Online Medical Billing Software for Healthcare Providers in 2024
Top Benefits of Online Medical Billing Software for Healthcare Providers in 2024
In teh rapidly evolving healthcare industry of 2024, technology continues to reshape how providers deliver services, manage administrative tasks, and enhance patient care. Among these technological innovations, online medical billing software stands out as a game-changer. It streamlines billing processes, reduces errors, and boosts revenue cycle management, helping healthcare providers operate more efficiently and focus more on patient health. This comprehensive guide explores the top benefits of online medical billing software for healthcare providers in 2024.
Introduction
Medical billing is a complex, time-consuming process that involves coding, claims submission, payment processing, and follow-up. Traditionally performed manually or with outdated software, it often led to billing errors, delayed reimbursements, and increased administrative overhead. Thankfully, online medical billing software offers a modern, cloud-based solution designed to address these challenges. As we step into 2024, embracing this technology is not just beneficial but essential for healthcare practices seeking growth, compliance, and efficiency.
What is Online Medical Billing Software?
Online medical billing software is a cloud-based platform that automates and simplifies the billing and coding process for healthcare providers. it integrates seamlessly with electronic health records (EHR) systems, facilitates electronic claims submission, manages patient data, and provides real-time analytics. Unlike traditional desktop software, online billing solutions offer accessibility from any device with an internet connection, ensuring flexible and efficient management of billing operations.
Top Benefits of Online Medical Billing Software in 2024
1. enhanced Billing Accuracy and Reduced Errors
Manual data entry and complex coding processes are prone to errors which can delay payments or cause claim denials. Online medical billing software automates coding, validation, and claim submission processes, drastically reducing human error. Accurate billing ensures faster reimbursements and improves cash flow.
2. Accelerated Claims Processing and Faster Payments
With integrated electronic claim submission and automatic validation checks, online billing software speeds up the entire billing cycle.real-time claim tracking and instant rejection alerts enable speedy corrections, minimizing delays and increasing the likelihood of timely reimbursements.
3. Improved Revenue Cycle Management (RCM)
Effective revenue cycle management is vital for practice sustainability.Online billing solutions provide comprehensive dashboards and analytics that help monitor claims, denials, and collections. Some platforms even suggest revenue optimization strategies based on payment patterns, enabling healthcare providers to maximize profitability.
4. Increased Compliance with Regulations
Staying compliant with evolving healthcare regulations like HIPAA, CMS guidelines, and ICD-10 coding standards is crucial. Online medical billing software is regularly updated to adhere to current regulations,reducing the risk of penalties and audits.
5. Enhanced Data Security and Privacy
security is paramount in healthcare. Cloud-based billing solutions employ robust encryption, user access controls, and audit trails to safeguard sensitive patient data. This ensures compliance with data protection laws and peace of mind for providers and patients alike.
6. Seamless integration with EHR and Practice Management Systems
Integration with Electronic Health Records (EHR) and other practice management tools allows for automatic data synchronization, eliminating redundancy and minimizing discrepancies. This interoperability streamlines workflows and enhances overall operational efficiency.
7. Cost Savings and Operational Efficiency
Transitioning to online billing software reduces reliance on paper, minimizes billing staff workload, and decreases administrative overhead. These cost savings enable healthcare providers to allocate resources elsewhere, such as patient care or practice expansion.
8. Accessibility and Flexibility
Being cloud-based, online medical billing software offers access from multiple devices and locations.This flexibility supports remote work and allows billing staff to operate efficiently outside the traditional office setting, especially important amidst remote work trends in 2024.
Practical tips for Choosing the Right Online Medical Billing Software
Evaluate integration capabilities with your existing EHR and practice management systems.
Prioritize data security features to ensure compliance and protect sensitive data.
Consider automation features such as automatic claim rejection alerts or payment posting.
Check for real-time reporting and analytics tools to monitor financial performance.
Assess customer support and training options to maximize software benefits.
Case Study: Success Story of a Mid-Sized Healthcare Practice in 2024
Practice Type
Challenge
Solution Implemented
Results Achieved
Multi-specialty clinic
High claim rejection rates and slow payment turnaround
Adopted cloud-based medical billing software with automated claim verification
Reduced rejection rate by 35%, sped up payment cycle by 20 days
First-Hand Experience: Why We Switched to Online Medical Billing Software
As a healthcare provider, we found manual billing processes time-consuming and error-prone. After switching to a reputable online medical billing platform in 2024, our practice experienced a meaningful boost in revenue, compliance, and staff productivity. With real-time dashboards and automated claim handling, we could focus more on patient care while the billing remained accurate and clear. This firsthand experience highlights how online solutions are essential for modern practices aiming for growth and efficiency.
Conclusion
In 2024, online medical billing software is transforming healthcare practices by making billing processes more efficient, accurate, and secure. From speeding up claims and payments to ensuring regulatory compliance and reducing operational costs,the top benefits of this technology are undeniable. Healthcare providers who embrace these digital solutions gain a competitive edge, improve cash flow, and enhance patient satisfaction. As the industry continues to evolve, investing in reliable online medical billing software is a strategic move towards a more streamlined and profitable practice.
Whether you’re a small practice or a large hospital system, leveraging the power of cloud-based billing solutions can unlock new levels of operational excellence. stay ahead of the curve in 2024 by choosing the right software tailored to your needs-your practice’s financial health depends on it.
https://medicalcodingandbillingclasses.net/leading-benefits-of-online-medical-billing-software-for-healthcare-providers-in-2024/
0 notes
Text
What Is eClinicalWorks EMR and Why Does It Matter?
eClinicalWorks EMR is a widely used electronic medical record system designed to improve clinical workflows and patient care. Many providers rely on eCW EMR to manage patient data securely and efficiently.
How is eCW EHR Different from EMRs?
While EMRs focus mainly on internal record-keeping, eCW EHR (Electronic Health Record) provides a broader view, sharing data across practices. eClinicalWorks EHR supports full patient histories and interoperability across healthcare networks.

What Makes eClinicalWorks Software Stand Out?
Known for its flexibility and innovation, eClinicalWorks software includes features like telehealth, patient portals, and mobile apps. It’s more than a medical record system—eClinicalWorks EMR software enhances engagement and decision-making.
How Can You Connect eClinicalWorks with Other Systems?
Seamless eClinicalWorks integration is vital for facilities that rely on multiple platforms. With robust eClinicalWorks integration solutions, healthcare providers can connect lab systems, billing software, and external APIs.
What Is the Role of APIs in eClinicalWorks?
The eClinicalWorks API allows developers to build apps and tools that communicate directly with the system. This is crucial for customization and deep eClinicalWorks integration with third-party platforms.
Why Use eClinicalWorks Integration Software?
For advanced workflows, eClinicalWorks integration software offers real-time syncing and automation. It ensures consistent data flow between systems and improves how eClinicalWorks software interacts with external tools.
What Are eClinicalWorks Integration Services?
eClinicalWorks integration services provide expert-led support to connect, configure, and maintain integrations. These services are often paired with the eClinicalWorks API to build custom solutions for unique healthcare needs.
How Do eClinicalWorks Tools Help Providers?
From scheduling to billing, eClinicalWorks software simplifies administrative tasks. With the right eClinicalWorks integration solutions, practices can eliminate redundancies and speed up their operations.
Why Is Choosing the Right EMR Important?
Using a powerful system like eClinicalWorks EMR software can improve clinical accuracy and patient satisfaction. The right eCW EHR setup ensures compliance, security, and smooth collaboration.
Conclusion:
Whether you're optimizing workflows or building custom connections, eClinicalWorks integration services and eClinicalWorks integration software are key to unlocking its full potential. The right configuration turns good tools into great care.
0 notes
Text
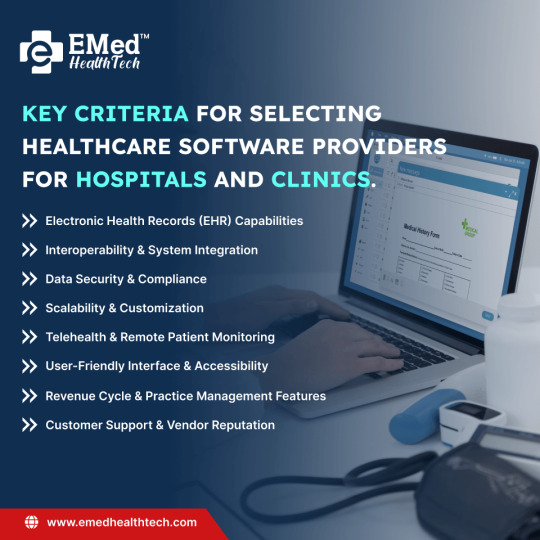
Planning to invest in healthcare software for your hospital or clinic? Before you choose a provider, here are the 8 key criteria you shouldn't ignore — from EHR and interoperability to security, telehealth, and support.
Trusted healthcare software companies in the US like EMed HealthTech offer scalable, compliant solutions tailored to your needs.
0 notes
Text
Global Nursing Resource Allocation Market is driven by Patient Care Demand

The Global Nursing Resource Allocation Market encompasses solutions designed to streamline the distribution and scheduling of nursing staff across healthcare facilities, including hospitals, clinics, and long-term care centers. These platforms integrate real-time data analytics, shift-management modules, and workload forecasting tools to ensure optimal nurse-to-patient ratios, reduce overtime costs, and enhance patient outcomes. By leveraging cloud-based software and artificial intelligence algorithms, healthcare administrators gain market insights into staffing patterns and can dynamically adjust resources to meet seasonal fluctuations and emergency needs.
Advantages of these resource allocation systems include improved operational efficiency, reduced burnout among nursing staff, and significant cost savings by minimizing unnecessary labor expenses. As patient acuity levels and care complexity rise globally, the need for advanced Global Nursing Resource Allocation Market solutions becomes paramount. Hospitals seek robust market research-backed tools to maintain compliance with regulatory staffing mandates and to support business growth through higher patient satisfaction scores. Enhanced interoperability with electronic health record (EHR) systems further bolsters data-driven decision-making and promotes seamless workforce collaboration.
The nursing resource allocation market size is expected to reach US$ 4.71 Bn by 2032, from US$ 2.40 billion in 2025, at a CAGR of 10.1% during the forecast period. Key Takeaways Key players operating in the Global Nursing Resource Allocation Market are:
-Cerner Corporation
-Allscripts
-McKesson Corporation
-Optum, Inc.
-IBM
These market players continually invest in research and development to expand their service portfolios, leveraging advanced analytics and AI-driven modules to enhance market share and market growth. Cerner Corporation’s solutions emphasize real-time workload balancing, whereas Allscripts focuses on predictive scheduling to address peak demand periods. McKesson Corporation has integrated resource allocation with its supply chain services, creating a holistic ecosystem for healthcare providers. Optum, Inc. leverages big-data capabilities to offer comprehensive workforce optimization strategies, while IBM incorporates cognitive computing to forecast staffing needs based on historical patient volume and acuity. Collectively, these companies maintain a strong market position by pursuing strategic partnerships, mergers, and acquisitions, facilitating global expansion and solidifying their presence in key regions. Growing demand for automated nursing resource allocation solutions is fueled by increasing labor costs, nurse shortages, and stringent regulatory requirements. Healthcare facilities face market challenges related to managing complex shift rotations, minimizing overtime, and preventing clinician burnout. The adoption of cloud-enabled platforms offers scalable market opportunities, allowing institutions of all sizes to implement sophisticated scheduling and staffing models. As industry trends shift toward value-based care, providers are under pressure to optimize resource utilization while maintaining high-quality patient outcomes. This drives demand for end-to-end solutions that seamlessly integrate with existing EHR systems and payroll infrastructure. Moreover, evolving market dynamics, such as rising chronic disease prevalence and an aging population, underscore the critical need for flexible workforce management tools to support fluctuating patient loads and seasonal care demands.
‣ Get More Insights On: Global Nursing Resource Allocation Market
‣ Get this Report in Japanese Language: 世界の看護資源配分市場
‣ Get this Report in Korean Language: 글로벌간호자원할당시장
‣ Resources- Global Nursing Resource Allocation: An Analysis
0 notes
Text
Cerner Healthcare Software: Revolutionizing Patient Care with Technology

In the rapidly evolving world of healthcare, the integration of technology into patient care has become essential. One of the pioneers in this transformation is Cerner Corporation, a global healthcare technology company known for its cutting-edge electronic health record (EHR) solutions. With a mission to improve the health of communities through innovative software and services, Cerner plays a significant role in shaping the future of healthcare delivery.
What is Cerner?
Founded in 1979 and headquartered in North Kansas City, Missouri, Cerner is a leading provider of health information technology (HIT) solutions, services, devices, and hardware. Cerner’s software solutions are widely used by hospitals, clinics, and healthcare systems around the world to manage clinical, financial, and operational tasks.
At its core, Cerner integration software is an Electronic Health Record (EHR) system that enables healthcare providers to store, access, and manage patient information digitally. In 2022, Cerner was acquired by Oracle Corporation, combining the strengths of two tech giants to enhance healthcare innovation.
Benefits of Using Cerner in Healthcare
Improved Patient Care
With easy access to complete patient records, providers can make more informed decisions, leading to better diagnosis and treatment.
Efficiency and Time Savings
Automating routine tasks and digitizing paperwork reduces administrative burdens and lets healthcare professionals focus more on patient care.
Enhanced Communication
Cerner supports secure messaging between providers and patients, improving engagement and satisfaction.
Data-Driven Insights
Analytics tools help healthcare organizations track performance, monitor public health trends, and make strategic decisions.
Challenges and Criticism
While Cerner is a robust and widely-used system, it’s not without its challenges:
Complexity: Some users find Cerner’s interface complex and not user-friendly.
Cost: Implementation and maintenance can be expensive for smaller institutions.
Training Requirements: Staff need time and resources to learn how to use the system effectively.
The Future of Cerner and Oracle Health
With Oracle’s acquisition, Cerner is expected to benefit from advanced cloud infrastructure, artificial intelligence, and analytics capabilities. The goal is to create a unified national health record database, enhance interoperability, and reduce healthcare disparities by leveraging big data and AI.
Oracle has also announced plans to make Cerner’s system more accessible via a mobile-friendly interface and to accelerate the software’s transition to the cloud.
Conclusion
Cerner healthcare software represents a significant step forward in the digital transformation of healthcare. By centralizing patient data, supporting clinical decisions, and improving administrative efficiency, Cerner empowers healthcare providers to deliver safer, more personalized care. As it continues to evolve under Oracle’s leadership, Cerner is poised to play a pivotal role in the future of global healthcare.
0 notes
Text
Population Health Management Market Driven by Rising Chronic Diseases and Value-Based Care Adoption
The Population Health Management (PHM) Market is gaining momentum as healthcare systems worldwide transition toward data-driven, patient-centered, and cost-efficient care models. According to market research insights, the increasing prevalence of chronic diseases, rising healthcare costs, and regulatory reforms are prompting providers, payers, and public health agencies to adopt PHM solutions at an accelerating pace.
What is Driving the Population Health Management Market?
Population Health Management focuses on improving health outcomes across groups of individuals by analyzing patient data, coordinating care, and optimizing resource allocation. The key drivers behind the market’s expansion include:
Rising Chronic Disease Burden: Conditions like diabetes, hypertension, and heart disease demand long-term monitoring and coordinated interventions, which PHM platforms support through real-time insights and risk stratification.
Value-Based Care Incentives: Governments and private payers are rewarding providers for quality and outcomes, pushing organizations to adopt PHM models that emphasize preventive and cost-effective care.
Healthcare IT Growth: The proliferation of electronic health records (EHRs), telemedicine, wearable devices, and patient engagement tools has created a data-rich environment ideal for PHM deployment.
Cost Containment Pressures: Escalating healthcare expenditures, particularly in the U.S. and other high-income regions, are forcing systems to adopt smarter, more efficient care delivery mechanisms.
Government Policies and Incentives: Regulatory programs such as the Affordable Care Act (ACA), CMS value-based programs, and similar global initiatives continue to promote population health strategies through funding and policy reforms.
Emerging Market Trends
The PHM market is evolving through several technological and strategic trends:
AI and Predictive Analytics: Artificial intelligence is being increasingly used to identify high-risk patients, predict hospital readmissions, and tailor interventions based on behavioral and clinical data.
Cloud Adoption: Cloud-based PHM solutions offer scalability, cost savings, and seamless data sharing, especially for small to mid-sized healthcare organizations.
Interoperability Standards: There is growing emphasis on data exchange standards to connect disparate healthcare systems and ensure seamless coordination across care teams.
Focus on Social Determinants of Health (SDOH): Providers are incorporating non-clinical data—such as housing, income, and education—into population health tools to understand and address broader health influencers.
Market Segmentation Insights
The Population Health Management Market is segmented by component, delivery mode, and end user:
By Component:
Software
Services (including consulting, implementation, and training)
By Delivery Mode:
On-Premise
Cloud-Based
By End User:
Healthcare Providers
Payers (Insurance Companies)
Employer Groups
Government Bodies
Services dominate the component segment due to the ongoing demand for implementation support and platform optimization. Cloud-based delivery is witnessing rapid adoption due to reduced infrastructure costs and remote access capabilities.
Regional Market Overview
North America remains the largest market, driven by regulatory mandates, the presence of major vendors, and widespread adoption of healthcare IT.
Europe is expanding steadily, supported by national digital health strategies and interoperability initiatives across countries.
Asia-Pacific is emerging as a high-growth region due to rising investments in digital healthcare, increased chronic disease prevalence, and growing awareness of PHM’s benefits.
Competitive Landscape
The global PHM market is competitive and marked by technological innovation and strategic partnerships. Leading players include:
Optum, Inc. (UnitedHealth Group)
Cerner Corporation (now part of Oracle)
Epic Systems Corporation
IBM Corporation
Allscripts Healthcare Solutions
Koninklijke Philips N.V.
These companies are focused on expanding analytics capabilities, enhancing user interfaces, and integrating PHM tools with broader digital health ecosystems.
Challenges to Address
Despite promising growth, several challenges remain:
Data Privacy and Security: Protecting sensitive health data across systems remains a top concern, particularly with increasing cyber threats.
Interoperability Barriers: Integration with legacy systems and diverse data sources can be complex and resource-intensive.
Cost and ROI Concerns: Smaller healthcare providers may struggle with initial investments and uncertain returns from PHM adoption.
Workforce Readiness: The successful implementation of PHM strategies requires training and upskilling clinical and IT staff.
Conclusion: A Transformative Shift in Healthcare Delivery
The Population Health Management Market is at the forefront of transforming global healthcare by enabling data-driven decision-making, proactive care management, and improved patient outcomes. As healthcare systems continue to embrace value-based models and digital transformation, PHM solutions will play a pivotal role in achieving efficiency, equity, and long-term sustainability.
Read more about PHM Market
About Mordor Intelligence:
Mordor Intelligence is a trusted partner for businesses seeking comprehensive and actionable market intelligence. Our global reach, expert team, and tailored solutions empower organizations and individuals to make informed decisions, navigate complex markets, and achieve their strategic goals.
With a team of over 550 domain experts and on-ground specialists spanning 150+ countries, Mordor Intelligence possesses a unique understanding of the global business landscape. This expertise translates into comprehensive syndicated and custom research reports covering a wide spectrum of industries, including aerospace & defense, agriculture, animal nutrition and wellness, automation, automotive, chemicals & materials, consumer goods & services, electronics, energy & power, financial services, food & beverages, healthcare, hospitality & tourism, information & communications technology, investment opportunities, and logistics.
For any inquiries or to access the full report, please contact:
[email protected] https://www.mordorintelligence.com/
0 notes
Text
Mercado de Sistemas de Información de Laboratorio: Proyecciones y Avances hasta 2034

El mercado de sistemas de información de laboratorio ha cobrado una relevancia significativa en el ámbito sanitario global, gracias a su papel fundamental en la mejora de la eficiencia, precisión y manejo de datos dentro de los laboratorios clínicos. En 2024, este mercado alcanzó un valor aproximado de USD 2,10 mil millones y se proyecta que crecerá a una tasa de crecimiento anual compuesta (CAGR) del 9,00% entre 2025 y 2034, lo que podría elevar su valor a unos USD 4,97 mil millones para finales del período previsto.
Impulsores del Crecimiento del Mercado
El crecimiento sostenido del mercado está respaldado por varios factores, siendo uno de los más destacados la digitalización acelerada en el sector salud. Los laboratorios clínicos y las instalaciones médicas están adoptando soluciones informáticas cada vez más sofisticadas que automatizan procesos clave como la gestión de muestras, generación de informes, control de calidad y administración de resultados, reduciendo los errores humanos y optimizando el flujo de trabajo.
Además, el aumento de la demanda de diagnósticos precisos y rápidos ha fomentado la adopción de estos sistemas avanzados. Esto se ve especialmente en laboratorios hospitalarios, centros de diagnóstico independiente y laboratorios de investigación, donde la capacidad para procesar grandes volúmenes de datos con rapidez y seguridad es crítica.
Innovaciones Tecnológicas y Automatización
La integración de tecnologías emergentes, como la inteligencia artificial (IA), machine learning, y la computación en la nube ha revolucionado el funcionamiento de los sistemas de información de laboratorio. Estas tecnologías permiten un análisis predictivo, una mejor gestión de datos y una personalización del tratamiento, lo cual contribuye a mejorar los resultados clínicos.
También se ha observado una fuerte inclinación hacia soluciones interoperables, capaces de integrarse sin problemas con otros sistemas como los registros médicos electrónicos (EHR) y las plataformas de gestión hospitalaria. Esta conectividad mejora la visibilidad de los datos y permite un enfoque más holístico de la atención al paciente.
Segmentación del Mercado
El mercado puede dividirse en varios segmentos clave:
Por tipo de componente: software y servicios
Por tipo de entrega: local (on-premise), basado en la nube y modelos híbridos
Por uso final: hospitales, laboratorios clínicos independientes, centros de diagnóstico, laboratorios farmacéuticos y de investigación
Entre estos, el modelo basado en la nube está ganando terreno rápidamente debido a sus ventajas en términos de flexibilidad, accesibilidad remota y menor coste de implementación.
Tendencias Regionales
Geográficamente, América del Norte lidera el mercado global debido a su infraestructura médica avanzada, mayor gasto en salud y rápida adopción tecnológica. Sin embargo, se espera que la región de Asia-Pacífico experimente un crecimiento acelerado gracias al aumento de las inversiones en digitalización del sector salud, expansión de la red hospitalaria y mejoras en la conectividad.
Europa también muestra un desarrollo sólido impulsado por políticas sanitarias favorables y la presencia de una base tecnológica consolidada.
Desafíos del Mercado
A pesar del crecimiento proyectado, existen ciertos desafíos que podrían limitar el avance del mercado. Entre ellos se incluyen:
Altos costos iniciales de implementación
Falta de personal capacitado en tecnología digital en entornos de laboratorio
Problemas relacionados con la interoperabilidad entre sistemas heredados y nuevos
Preocupaciones sobre la seguridad de los datos y la privacidad del paciente
Superar estos obstáculos requerirá estrategias gubernamentales claras, formación continua de los profesionales sanitarios y una evolución continua de las soluciones tecnológicas ofrecidas por los proveedores.
VISITA TAMBIÉN: Mercado de Procedimientos Quirúrgicos Robóticos en América Latina
Perspectivas y Oportunidades
El futuro del mercado de sistemas de información de laboratorio es prometedor. A medida que los avances tecnológicos continúan evolucionando y los laboratorios adoptan nuevas formas de trabajo digitalizado, se abren oportunidades significativas para empresas que desarrollan soluciones innovadoras. Además, las asociaciones entre hospitales, proveedores de software y entidades de investigación están dando lugar a productos cada vez más especializados y eficientes.
El periodo 2025-2034 se perfila como una década de expansión para este sector, especialmente con el impulso de políticas de salud electrónica, el crecimiento de la medicina personalizada y el enfoque global en mejorar los tiempos de diagnóstico.
¿Quieres conocer más sobre este sector en expansión?
Para un análisis más detallado con datos segmentados, tendencias clave, perfiles de los principales actores del mercado y proyecciones hasta 2034, consulta el Informes de Expertos (IDE). Este recurso es esencial para empresas tecnológicas, laboratorios, inversores y profesionales del sector salud que buscan tomar decisiones informadas y estratégicas en un entorno digital en constante cambio.
0 notes
Text
Surgical Information System Market Growth Trends and Future Opportunities in Global Healthcare Industry

The global healthcare industry continues to evolve rapidly, driven by advances in technology, patient-centered care models, and increased demands for efficiency and quality. Among the many technological innovations reshaping the sector, the surgical information system market has emerged as a key component in improving the safety, coordination, and outcomes of surgical procedures. These systems are becoming indispensable in modern operating rooms by streamlining workflow, enhancing data accuracy, and enabling real-time communication among care teams.
What Is a Surgical Information System?
A surgical information system is a specialized subset of healthcare information technology that focuses on managing, documenting, and coordinating activities related to surgical care. These systems typically support preoperative, intraoperative, and postoperative stages of surgery. They are used in hospitals, ambulatory surgical centers, and specialty clinics to assist in scheduling, patient documentation, anesthesia records, surgical planning, inventory management, and compliance with regulatory standards.
SIS platforms integrate with other hospital information systems, including electronic health records (EHR), radiology information systems (RIS), and laboratory information systems (LIS). This interoperability allows for more comprehensive and efficient patient care. In addition, surgical information systems can provide analytics that help improve clinical decision-making, reduce errors, and optimize resource utilization.
Market Drivers
The growth of the surgical information system market is fueled by several key factors. One of the most significant is the rising volume of surgical procedures worldwide. As populations age and chronic diseases like cardiovascular disorders, cancer, and diabetes become more prevalent, the demand for surgeries continues to increase. This rising demand necessitates improved surgical coordination and workflow efficiency, which SIS platforms are designed to deliver.
Another major driver is the growing adoption of healthcare IT solutions to reduce medical errors and ensure better patient outcomes. Governments and regulatory bodies across the globe have implemented initiatives aimed at digitizing healthcare systems, which in turn has accelerated the implementation of surgical information systems in healthcare facilities.
Market Challenges
Despite its promising outlook, the surgical information system market faces several challenges. One of the primary barriers to adoption is the high initial cost of implementation and the ongoing expenses related to software maintenance, staff training, and system upgrades. Smaller hospitals and rural healthcare providers may find it difficult to justify these costs without sufficient government support or a clear return on investment.
Another significant hurdle is data security and privacy. With the increasing use of cloud-based platforms and the growing volume of sensitive patient data being stored and transmitted electronically, concerns about cybersecurity breaches are becoming more pronounced. Ensuring compliance with regulatory frameworks such as HIPAA (Health Insurance Portability and Accountability Act) in the U.S. and GDPR (General Data Protection Regulation) in Europe is critical for vendors and healthcare organizations alike.
Regional Insights
North America currently leads the global surgical information system market, thanks to its well-established healthcare infrastructure, high adoption rate of advanced IT systems, and supportive government policies. The United States, in particular, has been a front-runner in embracing healthcare IT innovations, driven by initiatives such as the HITECH Act and Meaningful Use program.
Europe is another prominent region in the market, with countries like Germany, the UK, and France investing heavily in digitizing their healthcare systems. Meanwhile, the Asia-Pacific region is expected to witness the fastest growth during the forecast period. Increasing healthcare expenditure, a growing middle-class population, and rising awareness about the benefits of surgical IT solutions are contributing to the market’s expansion in countries like China, India, and Japan.
Competitive Landscape
The surgical information system market is moderately fragmented, with several global and regional players competing for market share. Major companies in the sector include Cerner Corporation, Meditech, Allscripts Healthcare Solutions, McKesson Corporation, and GE Healthcare. These companies are investing in R&D and strategic partnerships to expand their product offerings and enhance system capabilities.
In addition to large players, there is also a growing number of specialized vendors that offer tailored SIS solutions for specific surgical specialties or smaller healthcare settings. This trend is increasing market diversity and encouraging innovation.
Future Outlook
Looking ahead, the surgical information system market is poised for sustained growth. The integration of artificial intelligence (AI) and machine learning (ML) into SIS platforms could revolutionize surgical planning and risk assessment by enabling predictive analytics and personalized treatment protocols. Similarly, the use of augmented reality (AR) and virtual reality (VR) in surgical training and simulation is likely to become more prominent, offering a new dimension to surgical education and preparation.
As healthcare systems around the world continue to prioritize quality, efficiency, and patient safety, the demand for comprehensive, interoperable, and intelligent surgical information systems will only grow. Stakeholders that invest in scalable and secure SIS solutions today will be better positioned to meet the surgical care demands of tomorrow.
0 notes
Text
Why Software Testing is Critical in Healthcare Applications

In an era where digital transformation is redefining every industry, the healthcare industry stands at the forefront of technological innovation. From electronic health records (EHRs) and telemedicine to advanced medical devices and healthcare data analytics, software plays a pivotal role in delivering safe, effective, and timely medical care. However, the complexity and sensitivity of healthcare systems make them highly vulnerable to software glitches, which can result in life-threatening consequences. That’s why software testing is not just important—it’s absolutely critical in the development and deployment of healthcare applications.
The High Stakes of Healthcare Software
Unlike other industries, mistakes in healthcare software aren’t just inconvenient—they can be catastrophic. An undetected bug in a medical device or healthcare analytics platform could lead to incorrect diagnoses, delayed treatments, or even patient fatalities. This is especially crucial for medical device testing, where devices such as infusion pumps, pacemakers, and diagnostic imaging systems rely heavily on embedded software.
Every software release in healthcare must meet stringent regulatory standards, such as those from the FDA (U.S.), EMA (Europe), or ISO 13485. Testing isn’t just about functionality; it also ensures compliance, performance, security, and most importantly, patient safety.
Ensuring Accuracy with Software Testing
Accuracy is the cornerstone of any healthcare application. Whether it's processing patient data, generating diagnostic reports, or delivering remote consultations, even the smallest miscalculation or error can cascade into larger issues.
Through rigorous software testing, developers can identify and rectify issues at every stage of the software development lifecycle (SDLC). Functional testing ensures that features work as intended; integration testing verifies that systems interact seamlessly; and regression testing ensures that updates or patches don’t introduce new issues. These practices are essential for safeguarding the reliability and accuracy of healthcare systems.
Medical Device Testing: A Specialized Discipline
Medical device testing goes beyond traditional software validation. It involves a comprehensive examination of how hardware and software work together under various real-world conditions. Regulatory authorities often require validation protocols to demonstrate that a device performs reliably across all intended uses.
Key aspects of medical device testing include:
Verification and validation (V&V) of embedded software
Simulations and stress tests to evaluate performance under peak usage
Risk analysis and usability testing, to identify and mitigate potential failures
Interoperability testing with other devices and hospital systems
In short, medical device software must go through exhaustive testing before hitting the market, ensuring safety and efficacy for patients.
The Role of Testing in Healthcare Data Analytics
The advent of healthcare data analytics and healthcare analytics tools has revolutionized how medical decisions are made. These tools analyze vast amounts of structured and unstructured data to uncover insights that aid diagnosis, treatment, and operational efficiency. However such powerful tools are only as good as the accuracy and integrity of the software behind them.
Without rigorous software testing, healthcare analytics platforms could produce skewed results, leading to poor clinical decisions. Testing ensures:
Data integrity and accuracy: Verifying that data is correctly imported, processed, and reported
Security and privacy: Especially critical in protecting sensitive patient data (e.g., under HIPAA regulations)
Performance and scalability: Ensuring that platforms can handle large volumes of data without degradation
Predictive accuracy: Validating that machine learning algorithms or AI models function as intended
Addressing Security and Compliance Challenges
With cyberattacks on the rise, especially targeting the healthcare industry, robust security testing has become indispensable. A single breach can compromise thousands of patient records, leading to financial losses and irreparable reputational damage.
Software testing helps address these concerns by:
Identifying and fixing vulnerabilities through penetration testing and code reviews
Ensuring encryption and access controls are properly implemented
Confirming compliance with healthcare regulations such as HIPAA, GDPR, and HITECH
Agile and Automated Testing for Faster Delivery
The healthcare industry is under pressure to innovate rapidly, especially in times of global health crises. To balance speed with safety, many organizations are adopting agile methodologies and test automation.
Automated testing enables continuous integration and delivery (CI/CD), allowing healthcare providers to roll out updates quickly without compromising quality. It also frees up manual testers to focus on exploratory and high-risk testing areas, such as user interfaces or clinical workflows.
Conclusion
In the healthcare industry, where software reliability can mean the difference between life and death, software testing is not optional—it is essential. Whether it’s medical device testing, EHR systems, or healthcare data analytics, comprehensive testing safeguards patient safety, ensures compliance, and builds trust in digital health technologies. As the landscape of healthcare continues to evolve, driven by data and digital platforms, organizations must prioritize robust testing strategies to deliver effective, secure, and high-quality solutions. The cost of overlooking testing is far greater than the investment required to do it right.
#medical device testing#healthcare data analytics#test automation#healthcare analytics#Verification and validation
0 notes
Text
Choosing the Right Epic Integration Partner for Scalable Solutions
Epic, one of the leading electronic health record (EHR) platforms in the healthcare industry, provides seamless integration options for various systems, applications, and workflows. With the right Epic integration services, healthcare providers can streamline operations and enhance patient care. This guide explores how Epic integration solutions help build more connected and efficient healthcare ecosystems.

What Is Epic Integration?
Epic integration refers to the process of connecting the Epic EHR system with external healthcare tools, software, or data platforms. This ensures that clinical workflows, billing systems, and patient engagement platforms work together in harmony. Effective Epic systems integration enables organizations to reduce manual tasks and ensure real-time data availability.
Why Epic Systems Integration Matters?
Epic systems integration improves communication between departments, reduces data entry errors, and allows care teams to access the information they need. Whether it’s labs, pharmacies, or imaging centers, integrated systems ensure data flows accurately. Many hospitals invest in Epic API integration to further automate these connections and enable third-party apps.
Epic API Integration: Flexibility and Customization
Epic API integration allows developers to access key data endpoints within the Epic environment. This is essential for creating custom mobile apps, analytics dashboards, or patient portals. By leveraging Epic integration services, organizations can build tailored solutions without compromising data security or regulatory compliance.
How Epic EHR Integration Enhances Workflow?
Smooth Epic EHR integration ensures that clinical staff can document, retrieve, and share patient information effortlessly. This reduces clinician burnout and improves decision-making. Effective Epic integration solutions help ensure all health records are accessible from a single platform, boosting both productivity and care quality.
Epic EMR Integration for Seamless Data Exchange
Epic EMR integration enables the synchronization of medical records across various platforms. It ensures that vital health data—such as diagnoses, lab results, and medications—can be shared securely and quickly. Organizations that adopt Epic integration often experience fewer data silos and improved care coordination.
Choosing the Right Epic Integration Partner for Scalable Solutions
Selecting the right Epic integration partner is key to long-term success. Look for providers with proven experience in Epic EMR integration and a deep understanding of healthcare compliance. The right partner will offer flexible Epic integration solutions that scale with your organization's growth while ensuring data security and system performance.
Conclusion:
As the demand for interoperability grows, Epic EHR integration and related services will become even more critical. Organizations that invest in quality Epic integration services can future-proof their systems, deliver better care, and remain competitive in an evolving healthcare landscape.
0 notes
Text
Customizable Hospital Management System Software: Tailoring MediBest
Why Every Hospital Needs a Flexible Healthcare Management System
No two healthcare facilities share the same size, specialty mix, or regulatory landscape. Off-the-shelf platforms often force hospitals to bend workflows to the software, adding friction and cost. Studies on HMS adoption highlight customizability and scalability as top success criteria for modern deployments.

Modular Design from a Trusted Hospital Software Company
MediBest—a leading hospital software company—builds its solution as Lego-style modules that you can switch on or off as your organisation evolves. Popular options include:
Patient registration & EHR
OPD / IPD management
Laboratory & radiology interfaces
Pharmacy, inventory, and supply chain
Billing, claims, and revenue-cycle analytics
HR, payroll, and duty rosters
This plug-and-play architecture lets you launch core functions first and add new service lines later without rewriting code. Google My Business :-
Workflow Personalisation Without the Headaches
MediBest’s low-code configuration engine adapts screens, fields, and alerts to match local SOPs—no developers required. Common custom layers include:
Role-based dashboards showing KPIs that matter to finance, nursing, or housekeeping.
Form builders that capture specialty-specific data (e.g., oncology staging, maternal histories).
Rule engines that trigger tasks or notifications when clinical or financial thresholds are crossed.
Customisation happens in the admin console, so your IT team controls changes and stays vendor-independent.
Interoperability & Security Baked In
Tailoring should never compromise compliance. MediBest’s healthcare management system software delivers:
HL7 / FHIR APIs for lab devices, PACS, and national registries
End-to-end encryption and role-based access that meet HIPAA/GDPR guidelines
Audit logs that track every field change for effortless accreditation reporting
OSPlabs notes that aligning HMS modules with existing workflows improves efficiency while protecting data integrity. Osplabs
Business Benefits of a Customisable Healthcare Management System
Faster user adoption: Staff see familiar forms and processes, cutting training time.
Higher ROI: You pay only for the modules you deploy and can expand as revenue grows.
Continuous improvement: Drag-and-drop edits mean you refine workflows in days, not months.
Competitive edge: Rapidly spin up new clinics or service lines with consistent, branded experiences.
Implementation Roadmap for Tailored Success
Assess current workflows and define pain points.
Prioritise modules that deliver quick wins (often registration and billing).
Configure prototypes with department champions for feedback.
Run phased go-lives, measuring KPIs such as patient wait time and claim denial rates.
Iterate quarterly using MediBest’s analytics to fine-tune forms, alerts, and reports. Click Here :
Frequently Asked Questions
1. How does customisable hospital management system software improve patient care? Personalised workflows reduce data entry errors, speed up clinical decision-making, and let clinicians spend more time with patients instead of navigating rigid screens.
2. Will tailoring MediBest increase implementation time or cost? No. Most configurations use a drag-and-drop interface, so hospitals avoid custom code, lengthy testing cycles, and hefty change-order fees.
3. Can MediBest integrate with my existing lab, pharmacy, or radiology systems? Yes. MediBest supports HL7, FHIR, and REST APIs, allowing seamless data exchange with legacy devices and third-party software.
MEDIBEST :- CONTANT NOW :- Corporate Office 303, IT Park Center, IT Park Sinhasa Indore, Madhya Pradesh, 452013 Call Now +91 79098 11515 +91 97139 01529 +91 91713 41515 Email [email protected] [email protected]
0 notes