#eosinophil x nk cell
Text

NK Cell x Eosinophil
Cells at Work
8 notes
·
View notes
Text

now that i have motivation to draw i can finally make fanart of these girls ^_^
#i thought about them in 2018 too i hope past me is happy now#nk cell x eosinophil#my art#hataraku saibou#caw#cells at work#nk cell#eosinophil#it looks wonky but i'm not gonna fix it xD
176 notes
·
View notes
Text
Cells at Work as Among Us Imposters [headcanons]:
U-1146:
-will definitely not kill anyone
-Stays by AE3803 the whole time
-only sabotage
AE3803:
-Won't hesitate to kill anyone but U-1146
-won't be able to bring herself to kill U-1146 making everyone know its her.
NK Cell:
-Will kill Killer T Cell first
-will kill anyone in sight
-will kill even though there are other players around
-higher chance of being killed by her if you have a pet
- "I want to see them shiver in sadness."
-has a killing spree
Killer T Cell
- will kill NK Cell first
- "You really think I could fit inside the vent"
- "It's AE3803"
-probably doesn't know what he's doing
-self reports but ends up giving a dumb excuse
Dendritic Cell
- Very very very manipulative
- WILL use personal information to against you; making him innocent.
-won't kill anyone
-only sabotage
-goes with the flow. No strategy needed
Macrophage
-Will kill you but chose not to
-Sabotage 24/7
-never uses vents
-blames Killer T Cell
Platelets:
-physically CANNOT kill nor sabotage
-ends up making the game get restarted when they become imposter.
Commander T Cell
-sticks with Regulatory T Cell
- Killer T Cell will be his first target
-calculates every move
-sounds like he's giving a speech in the meeting.
Regulatory T Cell
-Can't kill anyone since Commander T Cell is following her
-Sabotages 24/7
- stays silent during the meeting
B Cell
- "A knife??? Where's the gun??"
-will kill Mast Cell first
-if not able to, will blame her instead it
-"Mast Cell. I saw her kill AE3803"
Mast Cell
-doesn't like killing anyone
-if she has to, she'll kill B Cell and B Cell only.
-Hides in vents
-keeps fighting with B Cell
Memory Cell
-doesn't remember where he last was
-gets really nervous he ends up confessing
-a horrible imposter
- "I was at the thing with the thing"
Eosinophil
-Too shy to kill anyone
-hesitates a lot
-somehow still wins the match
Basophil
- Nothing.
- absolutely N o t h i n g.
#nk cell#cells at work#cancer cells#cells#u 1146#ae3803#wbc x rbc#white blood cell x red blood cell#U 1146 x AE3803#killer t cell#hataraku saibou#hataraku saibō#hataraku saibo#basophil#eosinophil#Nk Cell c killer t cell#ship#among us#among us headcanons
81 notes
·
View notes
Photo








first (accidental) date pt. 2
pt. 1: https://pfeldspart.tumblr.com/post/177816181740/first-accidental-date-pt-1-did-you-notice-the
#hataraku saibou#cells at work#Red Blood Cell#white blood cell#rbc x wbc#wbc x rbc#pink blood cell#hataraku saibo#killer t#Dendritic cell#eosinophil#nk cell
1K notes
·
View notes
Text
Ok so, Mio Izumi, artist for friends, posted a tweet (x) sharing new years drawing for the cells and I'm,,,


Looks like the eye colors aren't super reliable because they change from one to another, but what i can tell is that Dendritic has neon greenish eyes/brown eyes, M cell has kinda cyan (more green) eyes/brown as well, Nk has like, yellow green colored eyes. Eosinophil in this also has pink for her uniform, Cross has god damn brown hair?? (I imagined him blonde oh my god) Also Reg T has purple eyes. Highlight for me is little M cell just, there tho, i love him, he is just a tiny bartender man..
#cells at work#hataraku saibou#hataraku saibō#cells at work friends#caw friends#hataraku saibo friends#pls i love this so much..#also headcanoned cross has blue eyes nooo
20 notes
·
View notes
Note
what about eosinophil x nk cell? 👀
i just think they'd be really cute and from what i remember (haven't watched season one in a while) eosinophil was very timid. i think nk could help her develop more confidence
HI EO/NK IS MY BREAD AND BUTTER
i love this pairing sm sm and i wish... i wish there was more of it... its a very good opposites attract. the way i see it is eo would develop into being little a confident, as a treat, really someone who starts to value herself a little more because nk is hellbent on getting her Cute Ass Soft Girlfriend To See She Is Perfect Damnit! eo's like wwell i dont know i dont really do much and some people tell me i suck and nks like already whipping out the lesbian death note idk. and shes like No babygirl. ily. perfect as you are. and then they kiss
i should go back to writing eo/nk honestly the ideal set up is eo seeing Buff Woman from across the battlefield and going "oh my god im gay". and i think u1146 and eo are mlm/wlw solidarity so i think shed be like Bruh!!!!!! there was this really cute girl ?!?! i think shes out of my league tho?!? and hes like oh! nk? and shes like YOU KNOW HER??? like the gay jumps out. full force. so hes like yea ill introduce you guys and nk is clueless. bt nk sees eo just, a complete blushing mess, and very cute and soft, Friendshaped... so shes like GUHHH MY HEAAAAART and then thye fall in love! which is really girlboss of them i think.
also i just want an excuse to have nk benchpress eo and princess carry eo everywhere... eos embarrassed by it but she loves it and nks like dw babygirl i gotchu!! i will protect you!!!!! and eos like >//////< oki
tldr I LOVE EO/NK AND THIS IS THEM VVVV

#HI I JUST I JUST LOVE THIS DYNAMIC#IM SORRY THIS ASK GOT SO FUCKING LONG BUT I#I LOVE . I LOVE THESE LESBIANS SM#cells at work#they have a big place in my tiny heart#THANK YOU ANON...THANK YOU
10 notes
·
View notes
Text
Cells at work Masterlist
The Cells at work fandom found me and I couldn't be happier :D So here is the masterlist, more works will be out soon!
General:
-Neutrophil squad headcanons
-Killer T hobbies/habits headcanons
-NK x Killer T headcanons
-U2048 Headcanons
-U1146/AE3803 Headcanons
-RBC squad headcanons
-Jealous/Protective WBC
-Human sick AU
-Eosinophil hcs
-Nk cell headcanons
-AE3803 being angry to U1146
-AE3803 being sick
-U2626 being sick
-Neutrophils sleepwalking
-Social Media AU (ft.@quinn-marie1213)
-Neutrophil squad that didn't know RBC&WBC where dating
-Human!Krav MagaAU
-Sick!NK cell with Caretaker Killer T headcanons
-U1196 reacting to the squad sleepwalking
-U2048 & squad as kids headcanons
Commenting abt ppl ideas (Flan comments):
Just me commenting ideas and comments with ppl in my inbox, sometimes they are related to the hcs-
-4986 Chaotic/Gentlemen friend
-RBC confessing
-Squad being protective of 3803
-3808 handling herself in bad situations
-Talking about the Krav Maga AU
13 notes
·
View notes
Text
Reviewing questions:
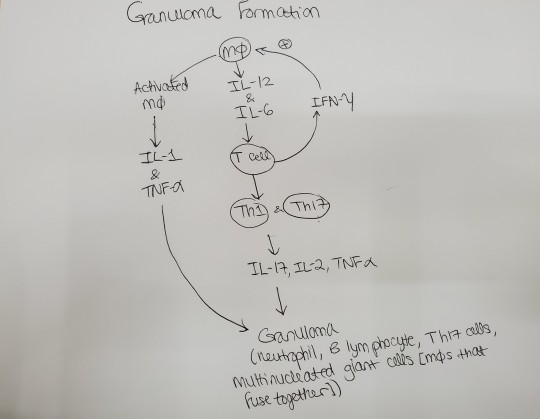
Non-caseating granulomas with multinucleated giant cells (macrophages that fuse together and therefore the multinucleated giant cells have multiple nuclei) and increased serum calcium are seen in pts with sarcoidosis. You see bilateral hilar lymphadenopathy. Activated macrophages make 1,25-dihydroxyvitamin D-> increased Ca2+. I remember posting about why sarcoidosis causes increased calcium before. Here's what I said:
I wasn’t understanding how/why sarcoidosis causes hypercalcemia. It’s because the epithelioid histiocytes [macrophages in the epithelial tissue] of the granulomas have alpha 1 hydroxylase, which converts vitamin D to the active form, which makes you absorb more calcium. I know alpha 1 hydroxylase is in the kidney. Apparently, it’s also in the noncaseating granulomas you see in sarcoidosis.
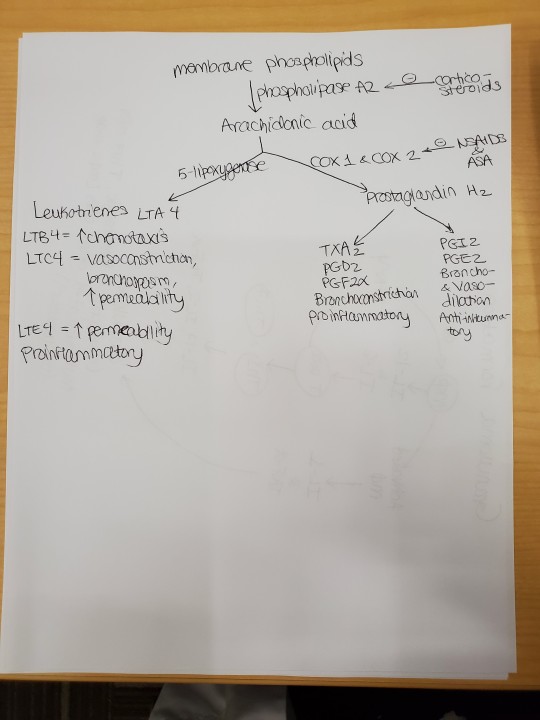
Glucocorticoids can be given to treat sarcoidosis in the short term. Glucocorticoids reduce inflammation by decreasing transcription of proinflammatory genes-> decreased macrophage and lymphocyte activation, so no inflammatory mediators (IL-1, IFN-gamma). Glucocorticoids also prevent endothelial cells from expressing selectins, which are necessary for neutrophils to leave the blood and go to sites of cytokine release. Glucocorticoids basically prevent margination and emigration of neutrophils-> increased neutrophil count in the blood. IL-8 = inflammatory cytokine that summons neutrophils; reduced by steroids. IL-10 = anti-inflammatory cytokine; increased by steroids. Steroids also cause apoptosis of eosinophils, monocytes, and lymphs-> susceptibility to infection. Steroids inhibit phospholipase A2-> decreased PGEs and leukotriene. Adverse effects of steroids include weight gain and glucose intolerance.
DiGeorge syndrome-> no thymus, so no T cells-> recurrent sinopulmonary infections. The structures that derive from the 3rd and 4th pharyngeal pouches (i.e., thymus) don't develop. Specifically, the ventral wings of the third pharyngeal pouch give rise to the thymus gland. In DiGeorge syndrome, this fails. Without a thymus, T cells can't mature and pts are susceptible to bacterial, viral, fungal, and protozoal pathogens. T cells are in the paracortex of lymph nodes (the cortex contains the naive B cells and the medulla contains the memory B cells). The paracortex of lymph node is undedeveloped in pts with DiGeorge syndrome (because there are no T cells to inhabit the paracortex).
Eosinophils respond to IgG and IgA on parasites by releasing their granules (e.g., major basic protein) and reactive oxygen species, which kill the parasites. This is antibody-dependent cell-mediated cytotoxicity. Th2 and mast cells make IL-5, which stimulates eosinophil activation and proliferation.
The Membrane Attack Complex (MAC) is made with complement factors C5b, C6, C7, C8, and C9. The MAC kills bacteria such as N. meningitidis. If you lack complement factors C5b through 9 (terminal complement deficiency), you can't make MAC and thus are susceptible to N. meningitidis meningitis. The petechial rash (on palms and soles, among other places) that you may see in N. meningitidis meningitis is due to vasculitis of small blood vessels due to N. meningitidis.
SCID = Sever Combined Immunodeficiency; can be X-linked recessive or AR; T cells don't develop; B cells also don't function normally; pts present with failure to thrive, recurrent viral, fungal, and opportunistic infections, and diarrhea. Pts will have hypogammaglobulinemia (not enough immunoglobulins) and lymphopenia (not enough B cells and T cells). When you do candidal antigen skin testing, these pts don't respond (no induration at site). In the candidal antigen skin test, you are trying to elicit the cell-mediated immune response of the type IV HSR, which involves not only CD8+ cytotoxic T cells, but also CD4+ helper T cells and macrophages. Macrophages are APCs, which present candida Ag to helper T cells, who then release cytokine to activate cytotoxic T cells, which destroy infected cells. IFN-gamma from both helper and cytotoxic T cells enhances macrophage phagocytosis of candida. Tx of SCID = stem cell transplant. Must r/o congenital HIV.
CD14 is the cell marker for macrophages. I didn't know that and that's what a question was asking. -_-
I answered a question where an old man got the flu even though he was vaccinated. The reason he got the flu was because of impaired naive B cell production. Vaccines expose you to antigens and your B cells should respond by making antibodies to the antigen. Vaccine failure will occur if the pt has atopy, uses steroids, or has impaired naive B cell production due to aging (called immunosenescence). So immunosenescence makes an older pt less likely to respond to a vaccine. Apparently, chronic inflammation with aging causes the B cells and T cells to respond to antigens the pt has already encountered and makes the pt less likely to respond to new Ags (e.g., those presented to the immune system in a flu vaccine).
From Wikipedia:
Immunosenescence refers to the gradual deterioration of the immune system brought on by natural age advancement. The adaptive immune system is affected more than the innate immune system.
Immunosenescence involves both the host's capacity to respond to infections and the development of long-term immune memory, especially by vaccination.[2] This age-associated immune deficiency is ubiquitous and found in both long- and short-living species as a function of their age relative to life expectancy rather than chronological time.[3] It is considered a major contributory factor to the increased frequency of morbidity and mortality among the elderly.
T cells are made in the bone marrow and mature in the thymus, hence T cells are also called "thymocytes." He explained T cell maturation with positive and negative selection really well in OnlineMedEd, so I won't go over it again here. I get it. Hopefully I will remember it.
Macrophages infected with intracellular pathogens (like mycobacterium tuberculosis) release IL-12-> T cells and NK cells release IFN-gamma-> macrophages become activated and increase phagocytosis; macrophages also release TNF-alpha, which leads to granuloma formation. IFN-gamma binds the IFN-gamma receoptor on macrophages-> receptor dimerization-> activation of Janus kinase 1 and 2-> STAT1 translocated to nucleus-> increased macrophage phagocytosis and killing of bacteria. Problems with the IFN-gamma pathway-> inability to kill M. tuberculosis-> disseminated infection.
From Wikipedia:
The JAK-STAT signalling pathway is a chain of interactions between proteins in a cell, and is involved in processes such as immunity, cell division, cell death and tumour formation. The pathway communicates information from chemical signals outside of a cell to the cell nucleus, resulting in the activation of genes through a process called transcription. There are three key parts of JAK-STAT signalling: Janus kinases (JAKs), signal transducer and activator of transcription proteins (STATs), and receptors (which bind the chemical signals).[1] Disrupted JAK-STAT signalling may lead to a variety of diseases, such as skin conditions, cancers, and disorders affecting the immune system.[1]
The JAK-STAT pathway in cytokine receptor signalling can activate STATs, which can bind to DNA and allow the transcription of genes involved in immune cell division, survival, activation and recruitment. For example, STAT1 can enable the transcription of genes which inhibit cell division and stimulate inflammation.
IFN-apha and beta are made by cells infected by viruses; the interferons prevent protein synthesis in virally infected cells. Specifically, IFN-alpha and beta cause cells to make enzymes that degrade viral proteins (e.g., RNAse L).
Neutrophils respond to IL-8, a pro-inflammatory cytokine. Pus = liquor puris + leukocytes (mostly neutrophils). So pus is basically dead neutrophils and a proteinaceous fluid called liquor puris. Chemotaxis = IL-8 released by macrophages at site of infection summons neutrophils. Other chemokines = leukotriene C4, C5a, 5-HETE.
TNF-alpha, IL-1, and IL-6 induce inflammation during sepsis. TNF-alpha from macrophages summons neutrophils and more macrophages.
In chronic lung transplant rejection, small airways become inflamed due to lymphocytes-> scar tissue blocks small airways (bronchiolitis obliterans).
Wiskott Aldrich syndrome = X-linked recessive mutation of genes coding for cell cytoskeleton proteins; pts present with thrombocytopenia (low platelets) + eczema + B cell and T cell deficiency (presents as recurrent infections). Platelets will be abnormal-> petechiae, epistaxis. No B cells-> pyogenic infections; no T cells-> opportunistic infections. Tx = bone marrow transplant.
HLA-DP, HLA-DQ, and HLA-DR are the genes that encode MHC Class II. In bare lymphocyte syndrome type II, you lack MHC Class II, so you can't activate B cells and T cells (normally, APCs present foreign antigens to naive B cells on their MHC-II receptors; this then causes B cells to activate T cells, which give the costimulatory signal to B cells, allowing the B cells to proliferate and class switch).
#sarcoidosis#hypercalcemia#interleukins#multinucleated giant cell#DiGeorge syndrome#steroids#major basic protein#meningitis#MAC#immunology#SCID#vaccines#immunosenescence#opsonization#Fab#antibody#cell markers#interferon gamma#IFN gamma#Janus kinase#JAK STAT#JAKSTAT#interferons#pus#transplant rejection#Wiskott Aldrich syndrome#MHC#HLA#IL12#chemotaxis
15 notes
·
View notes
Text
300+ TOP MEDICINE Objective Questions and Answers
MEDICINE Multiple Choice Questions :-
1. Which of the following investigation is useful for Myocardial metabolism and blood flow ?
a) CT scan
b) MRI scan
c) Positron Emission Tomography scan
d) Chest X-ray
Ans: c
2.Barr body is seen in
a) Buccal mucosa smear
b) RBC
c)WBC
d) Saliva
Ans: a
3. Which is not a acute phase reactant
a) C-Reactive protein
b) Haptoglobulin
c) Complement
d) alpha feto protein
Ans:d
4.Which of the following disorders have been shown to be genetically transmitted by singleautosomal dominant enes?
a) Catatonic schizophrenia"
b) Phenyl ketonuria
c) Creutzfeldt - Jacob diseased
D) Huntington's disease
Ans:d
5.False statement about fragile - X syndrome is '
a) Breakage in long arm of X chromosome
b) Common genetic disorder
c) Micro - orchidism
d) Long face
Ans:c
6.C3 and C4 levels are raised in
a) Autoimmune disease
b) SLE
c)RA
d) All of the above
Ans:a
7.Which one of the following statements about Natural Killer (NK) cells is not correct?
a)NK cells can lyse tumour cells and virus infected cells in vitro, without previous sensitization
b)NK cells are found in peripheral blood and lymphoid tissue
c)NK cells are CD 3 positive
d)NK cells lyse the target cells by antibody degendent cellular cytotoxicity
Ans:c
8.The chromosomal anomaly in Klinefelter syndrome is
a)47XXY
d)45XO
c)47XXX
d)47XXXX
Ans:a
9.Down syndrome is due to
a) Trisomy 21
b) Translocation 13-15/21
c) Translocation 22/21
d) All of the above
Ans:d
10.Interferons secreted by all except
a) Monocytes
b) Macrophages
c) Fibroblast
d) Lymphocytes
Ans:a

MEDICINE MCQs
11.The translocation in Burkitt's lymphoma is between chromosome
a) 8 and 14
b) 9 and 22
c) 11 and 13
d) 8 and 12
Ans:a
12.Non immune hydrops is not a feature of which of the following
a) Chromosomal abnormalities
b) Alpha thalassemia
c) Renal malformations in foetus
d) Foetal cardiac abnormalities
Ans:c
13.Carcinoembryonic antigen is seen in
a) Colorectal carcinoma
b) alcoholic cirrhosis
c) Emphysema
d) Diabetes mellitus
Ans:a
14.DNA analysis can be done from all except
a) Monocyte
b) Lymphocyte
c) Fibroblast
d) Amnion cell
Ans:c
15.A stable heritable alteration of DNA is known as
a) Translocation
b) Mutation
c) Syngamy
d) Gene fixation
Ans:b
16.Commonest blood group
a) A
b) B
c) AB
d)0
Ans:d
17.One of the following is not a_ chromosomal breakage syndrome?
a) Bloom's syndrome
b) Fredrichs Ataxia
c) Xeroderma pigmentosa
d) Fanconi's Anemia
Ans:b
18.Commonest chromosomal syndrome is: *
a) Trisomy 13
b) Trisomy 17
c) Trisomy 21
d) Fragile X syndrome
Ans:c
19.Which is true of Type II hypersensitivity?
a) Antigen against tissue
b) IgE mediated
c) Antibody directed to tissue antigen
d) Immune complex mediated
Ans:c
20.Analysis of protein antigen is done by
a) PCR
b) Western Blot
c) Southern blot
d) Northern blot
Ans:d
21.Vitamin D resistant rickets is inherited as
a) autosomal dominant
b) autosomal recessive
c) x-linked recessive
d) x-linked dominant
Ans:d
22.In Philadelphia chromosome there is translocation between chromosomes
a) 11 and 22
b) 9 and 22
c) 5 and 13
d) 8 and 14
Ans:b
23.Hintingtons chorea is
a) Autosomal dominant
b) Autosomal recessive
c) X linked dominant
d) X linked recessive
Ans:a
24.The part of RNA which does not code for protein is
a) Exon
b) Introns
c) Codon
d) Meson
Ans:b
25.All of the following are X-linked recessive disorder except
a) Myotonic Dystrophy "
b) Christmas disease
c) Hemophilia
d) Duchenne's Muscular Dystrophy
Ans:a
26.The passive transfer of delayed hypersensitivity in man is mediated by
a) Interferon
b) Skin reactor factor
c) Lymphotoxin
d) Transfer factor
Ans:d
27.Which of the following is true concerning Ig M?
a)It is the reaginic antibody
b)It is important in the first few days of the primary immune response
c)It peaks after Ig G has reached its peak
d)It is the smallest of the immunoglobulin molecules
Ans:b
28.Which HLA antigens are recognized by cells
a)T-helper
b)T-effector
c)T-suppressor
d)Bcell
Ans:a
29. Pataus syndrome due to
a) Trisomy 21
b) Trisomy 18
c) 18 P
d) Trisomy 13
Ans:d
30. Treatment of serum sickness may include all except:
a) Epinephrine
b) Steroids
c) Gammaglobulin
d) Antihistamines
Ans:c
31.Opsonizing toxins are
a)C3a
b)C3b
c)C5a
d)C5-C9
Ans:b
32. HLA-B27 associated with all except
a) Psoriasis
b) Behcets syndrome
c) Reiters syndrome
d) Ankylosing spondylitis
Ans:b
33.Recombinant DNA technique was first done on genome of
a)E.coli
b)Bacteroids
c) Pseudomonas
d) Proteus
Ans:a
34.The following disease are transmitted by autosomal recessive genes
a) Idiopathic hemochromatosis
b)Von Reckling Hausen's disease
c) Von Willebrand disease
d) Cystic fibrosi
Ans:d
35.Otospongiosis is
a) autosomal dominant
b) autosomal recessive
c) X-linked dominant
d) X-linked recessive
Ans:a
36.Not a X-linked Recessive disease
a) Laurence Moon Beidel syndrome
b) Nephrogenic diabetes
c) Muscular dystrophy
d) Colour blindness
Ans:a
38.Bone marrow transplantation as a treatment modality can be advisedin all of the following cases which are newly diagnosed except
a) Combined immunodeficiency
b) CML
c) Aplastic anemia
d) All
Ans:d
39.Interferon is not used in which of the following:
a) Hairy cell leukemia
b) Chronic myeloid leukemia
c) Chronic hepatitis B infection
d) Myelomonocytic leukemia
Ans:d
40.Which among the following does not secrete interleukin I alpha
a) Lymphocyte
b) Fibroblast
c) Macrophage
d) Neutrophils
Ans:d
41.Which of the following immunocompetent cells is concerned with cell mediated immunity and humoral immunity
a) Monocytes
b) Neutrophils
c) Eosinophils
d) Lymphocytes
Ans:d
42. Barrbody is seen in
a) turners syndrome
b) Klinefelters syndrome
c) testicular feminization
d) light chain IgG
Ans:b
43. Bence Jones proteins are
a) heavy chain IgG
b) present in bone marrow
c) seen in lymphoma
d) 46 XY
Ans:d
44. DNA analysis is useful for all except
a) Thalassemia
b) Hemophilia
c) Ectodermal dysplasia
d) Duchenne's dystrophy
Ans:c
45. Disease where gene therapy has been attempted or considered include:
a) Adenosine deaminase deficiency
b) Hemophilia A
c) Cystic fibrosis
d) Hypercholesterolemia
e) All of the above
Ans:e
46.Passive transfer of delayed hypersensitivity in man is mediated by
a) Interferon
b) Skin reactor factor
c) Lymphotoxin
d) Transfer factor
Ans:d
47. True about transmission of an x-linked recessive disease are
a)All daughters will have disease
b)All sons will be carriers
c)50% of sons & 50% of daughters will have disease
d)50% of sons of an affected mother will contract disease
Ans:b
48. Single gene disorder is
a) glycogen storage disease
b) retinoblastoma
c)DM
d)HT
Ans:b
49.Edwards syndrome is
a) Trisomy 21
b) Trisomy 18
c) Trisomy 13
d)5P
e) 18Q
Ans:b
50.The commonest cause of primary immuno deficiency is
a) Ig A deficiency
b) Agamma globulinemia
c) Congenital immunodeficiency
d) Acquired immuno deficiency
Ans:a
MEDICINE Objective type Questions with Answers
51.Cyclosporin mainly affects
a) CD4+cells
b) CD 8 cells
c) B-cells
d) CD 3 +cells
Ans:a
52) AH of the following statements regarding mast cells are true except
a) they contain heparin proteoglycan
b) their number is increased in patients with bronchial asthma
c) disodium cromoglycate brings about their degranulation
d) they have receptors for Fc portion of IE.
Ans:c
53. Wilms tumor is characterized by which chromosomal aberration
a) lip-
b) llq-^
c) 13p-
d) 13q-
Ans:a
54. Percentage of Rh positivity is
a) 80%
c)92%
d)93%
b) 85%
Ans:d
55. All are X linked diseases except
a) Myotonic dystrophy
b)G6PD
c) Fabrys disease
d) Hemophilia A
Ans: a
56. Father has Autosomal dominant disease. Mother is normal with no family history of the disease. What are the chances of son getting the disease
a) 100%
b)50%
c)25%
d)0%
Ans:b
57. Dominant trait expresses in
a) homozygous state
b) heterozygous state
c) both homo and heterozygous state
d) males
Ans: c
58.Most important HLA for organ transplantation and tissue typing
a) HLA-A
b)HLA-B
c)HLA-C
d)HLA-D
Ans:d
59.All of the following are autosomal dominant disorders except
a) tuberous sclerosis
b) polyposis coli
c) cystic fibrosis
d) myotonic dystonia
Ans:c
60.X linked recessive disease is characterized by
a) Vertical transmission
b) 50% female carriers if male is affected
c) 50% male affected if female is diseased
d) 50% male carriers if female is diseased
Ans:d
61.Achondroplasia is inherited as
a) autosomal dominant
b) autosomal recessive
c) x-linkeddonlinant
d) x-linked recessive
Ans:a
62.All are Autosomal recessive except
a)-Cystic fibrosis
b) Hypercholesterolemia
c) Wilsons disease
d) Sickle cell anemia
Ans:b
63. Short stature with widely spread nipples and webbing of neck is seen in
a) Down's syndrome
b) Turner's syndrome
c) klinefelter's syndrome
d) Edward's syndrome
Ans:b
64.Pick out product manufactured at present by genetic engineering
a) Interferons
b) Rabies vaccine
c) Gammaglobulin
d) Tuberous sclerosis
Ans:b
65.All of the following are autosomal recessive except
a) Albinism
b) Alkaptonuria
c) Cystic fibrosis
d) Tuberous sclerosis
Ans:d
66.Which one of the following immunoglobulins is^characteristically elevajtedm filariasis?
a)IgA
b)IgE
c)IgG
d)TgSr
Ans:b
67.Which is not X-recessive?
a) beta thalassemia
b) G6PD deficiency
c) hemophilia A
d) colour blindness
Ans:a
68.Commonest chromosomal anomaly
a) fragile
b) trisomy 21
c) trisomy 13
d) trisomy 18
Ans:b
69.Interferon is not used in
a) CML
b) Polymyositis
c) Hairy cell leukaemia
d) Chronic hepatitis C infection
Ans:b
70. Mode of action of actinomycin - D is to prevent:
a) RNA elongation
b) DNA synthesis
c) DNA elongation
d) None of the above
Ans:a
71. A 15-year old girl presents with history of 7 days high fever, toxic appearance, anaemia, petechiae over skin, ulcers in the mouth and mild hepatosplenomegaly with total count of 30,000/cu mm.The most important investigation for diagnosis would be:
a) Blood culture
b) Splenic puncture
c) Liver biopsy
d) Bone marrow aspiration
Ans:a
72. Chemoprophylaxis is used in all except
a) Malaria
b) Typhoid
c) Meningococcal meningitis
b) gram negative enterobacteriae
Ans:b
73. Endotoxic shock is due to
a) gram positive bacteria
b) gram negitive entrobacteriae
c) viruses
d) gas gangrene
Ans:b
74. The endotoxin which leads to endotoxic shocks is actually
a) Lipoprotein
b) Lipopolysaccharide
c) Polysaccharide
d) Polyamide
Ans:b
75.Probenecid excretion is increased by
a) penicillin
b) cephalosporin
c)NaHC03-
d) tetracycline
Ans:a
77. Immunoglobulin administration is life saving in one of the following conditions:
a) Rabies
b) Clostridium
c) Poliomyelitis
d) Typhoid
Ans:b
78. Pick out the vaccine that gives lifelong protection after the initial course of vaccination
a) TAB vaccine
b)HDCV
c) Measles vaccine
d)BCG vaccine
Ans:c
79. Tetracyclines are useful in infections of
a) Rickettsia
b)Chlamydiae
c)LGV
d)All
Ans:d
80.True statement regarding Ciprofloxacin is
a) Excreted mainly through bile
b) Antacid when given with, facilitates absorption
c) It can be given only orally
d) Belongs to Fluroquinolones group
Ans:d
81.The antibiotic which is acid labile is
a)Ampicillin
b) Cloxacillin
c)Gentamicin
d) Methicillin
Ans:d
82.Cinchonism is due to
a) Quinine
b)Chloramine
c)Digoxin
d)Digitoxin
Ans:a
84. The half life of chloroquine is :
a) 6 hours
b) 7 days
c) 12 hours
d) 24 hours
Ans:b
85.Which of the following combination is not synergistic
a)Penicillin and streptomycin in endocarditis
b)Amphotericin B and flucytosine in cryptococcal meningitis
c)Penicillin and chlortetracycline in pneumococcal meningitis
d)Sulphamethoxazole and trimethoprim in UT1
Ans:c
86.Nosocomial pneumonia is caused most commonly by
a) streptococcal
b) mycoplasma
c) gram negative bacteria
d) viruses
Ans:c
87. The persistence of one of the following clinical feature indicates very poor prognosis in a case of endotoxin shock:
a) Generalized weakness
b) Low volume pulse
c) Tachycardia
d) Oliguria
e) Restlessness
Ans:d
88.Treatment of travellers diarrhoea is
a) sulfaguanidine
b) Diphenoxylate and atropine
c) metronidazole
d) Chloromycetin and Streptomycin
Ans:b
89. The following are characteristic of central fever except
a) No diurnal variation
b) No sweating
c) decreased response to External cooling
d) Resistant to antipyretics
Ans:c
90. Ampicillin is used in all except
a) Pseudomonas
b) Proteus
c) Streptococci
d) Staphylococci
Ans:d
91.First generation cephalosporins are not effective in... infection
a) Pseudomonas
b) Proteus
c) Streptococci
d) Staphylococci
Ans:a
92.Which of the following is a useful bedside test in septicemia assessment?
a) Peripheral smear
b) Micro ESR assay
c)CRP levels
d) Urine microscopy
Ans:a
93.PTJO in a farmer dealing with goats milk is usually due to
a) Anthrax
b) Brucella
c) Mycobacterium
d) Histoplasma
Ans:b
95.Prognosis is related to incubation period in
a) Cholera
b) Rabies
c) Tetanus
d) Diphtheria
Ans:c
96.The following statement about arboviruses is FALSE
a)Complications include encephalitis and Hemorrhage
b)Transmission is typically by the ingestion of infected water
c)They occur predominantly in temperate climates
d)Incubation period is usually more than one month
Ans:b
97.The most common cause of seizures in a patient
a) Toxoplasmosis
b)Cryptococcal meningitis
c) Progressive multifocal leukoencephalopathyof AIDS is
Ans:a
98. HIV is a
a) Retrovirus
b) Flavivirus
c) Oncovirus
d) Arbovirus
Ans:a
99. Bronchopneumonia due to measles occurs because of
a) Running nose
b) Sinusitis
c) Immuno modulation
d) Bronchial obstruction
Ans:c
100. The most common ophthalmic lesion in AIDS is
a) Hard exudates
b) Cotton wool spots
c) Angioid Streaks
d) Microaneurysms
Ans:b
MEDICINE Questions and Answers pdf Download
Read the full article
0 notes
Text
ABIM: Allergy and Immunology
ABIM syllabus can be found here
Let me know if you find any errors
Sources: UWorld, MKSAP 16/17, Rizk Review Course, Louisville Lectures, Knowmedge (free version)
Anaphylaxis:
- cutaneous + shock symptoms OR allergen exposure + 2 organ damage
- increased histamine, increased tryptase
- Tx: IM or SC 0.3-0.5mg of 1:1000 Epi Q5-15 minutes into lateral thigh (give IV Epi 1:10000 if in shock)
Aspirin idiosyncrasy - Samter syndrome: asthma + nasal polyp + ASA sensitivity
Stinging insect hypersensitivity - undergo venom skin testing and immunotherapy
Asthma:
- normal spirometry doesn’t rule out asthma
Exercise and cold-induced asthma:
- PRN SABA
- pre-treat 15-30 minutes before exposure with Albuterol/Cromolyn/Nedocromil
Allergic bronchopulmonary aspergillosis:
- brown sputum, IgE>1000
- Dx skin test, IgG, IgE
- Tx: Itraconazole, steroids
Nasal polyps and Aspirin sensitivity:
- Samter Syndrome (asthma, nasal polyp, ASA sensitivity)
- Tx: ASA desnsitization or LAMA (Montelukast/Zafirlukast)
Occupational asthma: avoid trigger; symptoms may not resolve for months
Asthma and pregnancy: continue Rx
Asthma mimics (vocal cord dysfunction): flat loop, restrictive pattern (decreased TLC) but normal DLCO
Undifferentiated asthma:
- metacholine challenge; bronchodilator improves FEV1/FVC >22%
- r/o GERD and vocal cord dysfunction
Rhinitis, sinusitis, conjunctivitis:
Allergic rhinitis:
- Dx with empiric Tx (intranasal corticosteroids > antihistamines)
- confirm Dx with allergy skin test > RAST (ELISA IgE assay)
- add ipratropium bromide for severe symptoms
Rhinitis medicamentosa:
- i.e., Pseudoephedrine/Afrin/Oxymetolazone, also beta blockers, OCP
- Tx: stop topical decongestant
- start short court of prednisone or intranasal corticosteroids
Food allergy: occurs within 2 hours, Dx with food challenge > RAST
Urticaria and angioedema
- AVOID ASA/NSAIDs!!
- Tx: non-sedating antihistamine (Cetirizine, Ranitidine) --> + H2 blocker (Cimetidine, Ranitidine)
- chronic treatment: MTX, AZT, Cyclosporine
Hereditary angioedema: NO HIVES/URTICARIA! DO NOT GIVE EPI!
- complement activation --> bradykinin: slow progressive symptoms over days with light serpiginous non-pruritic rash, and abdominal pain
- check C4, C1 inhibitor
- Tx: C1 inhibitor, Kallekrein I, bradykinin receptor antagonist, Danazol; if emergency: FFP
Urticarial vasculitis: lesion/hives that persists > 24 hours with purpura/ecchymosis on resolution --> Dx: skin bx
Allergic angioedema: mast cell --> RAPID HIVES, PRURITUS
- Tx: antihistamine, corticosteroid, Epi
Chronic urticaria: >6 weeks
Skin disorders:
Fixed drug eruption: ovoid skin lesions recurs at same location with repeat drug administration
Jarisch-Herxheimer: fever, HA, rash, hypotension for 2-48hrs; Tx continue Abx and supportive Tx
DRESS (Hypersensitivity Syndrome): acute papules, facial edema, fevers, arthralgia, gen LN
- Dx: Eosinophilia, increased AST/ALT, lymphocytosis
- Tx: IVIg
Drug allergy other than drug-induced urticaria and angioedema:
- examples: Allopurinol, beta lactam, NSAIDs, Sulfa
- type I: anaphylaxis
type 2: days-months: cytopenias
type 3: vasculitis/serum sickness
type 4: rash, fever, multiorgan
Autoimmune systemic disorders:
Mastocytosis: myalgias, abdominal pain, diarrhea, pruritus, marked hypotension/shock
Allergic interstitial nephritis:
- fever, eosinophils, hematuria, rash, edema;
- common culprits: Allopurinol, PCN, Cephalosporin, PPI, Quinolones, Sulfas, Phenytoin, Rifampin
Eosinophilic esophagitis: solid food dysphagia (food gets stuck in throat), Dx: endoscopic esophagus biopsy with eosinophils, Tx: PPIs and steroids
Eosinophilic pneumonia: smoker with “photographic negative pulmonary edema”; Tx: oral corticosteroids
Eosinophilic granulomatosis with polyangitis (Churg-Strauss): flares with LAMA and steroid taper; Tx: STOP LAMA and resume steroids
Hypersensitivity pneumonitis: CD4:CD8 <1, avoid trigger; Tx flares with steroids
Allergic complications of transfusions:
Febrile transfusion reaction: 1 degree rise in temp, don’t stop transfusion, Tx: acetaminophen
Hemolytic transfusion reactions: STOP TRANSFUSION, Tx: IVF +/- diuretics
Transfusion-related acute lung injury (hypotension, stop transfusion, vent management and supportive treatment) vs Transfusion-associated circulatory overload (hypertension, give blood slowly and with diuretics)
Transfusion-related urticaria: DON’T STOP TRANSFUSION; Tx: antihistamines
Transfusion-related anaphylaxis: Tx: stop blood, Epinephrine
Primary immunodeficiency disorders:
Antibody deficiency (common variable immunodeficiency): associated autoimmune diseases
- decreased IgG and IgM/IgA --> recurrent sinopulm infection + chronic diarrhea, meninigitis, skin/joint, eye infection
- may develop granulomatous lung nodules/lung fibrosis/ILD, splenomegaly, lymphadenopathy
- associated gastric adenocarcinoma, intestinal lymphoma, non-Hodgkins lymphoma
- send protein (tetanus and dipth toxoid) and polysaccharide PNA IgG titers while off IgG x 5 months; vaccinate if low and then check again in 4 weeks
Complement deficiency: associated with SLE
- Dx: CH50 assay --> if normal: alternative and leptin pathway components
IgA deficiency: most common
- respiratory infection, Giardia infection, transfusion reaction with IgA so transfuse with WASHED pRBC
- associated with autoimmune diseases (RA, SLE)
Immunodeficiency clues:
1. within 1 year: 2+ ear infections or non-allergic sinus infections or >1 pneumonia
2. recurrent viral infections (herpes, cold, wart)
3. recurrent deep abscesses
4. persistent thrush/fungus
5. infection with normally harmless TB
- B cell (Ig): sinopulmonary, gastroenteric, septic arthritis
- T cell (~HIV): associated with autoimmune disorders (ITP, RA, SLE), chronic diarrhea, opportunistic infections (PCP, fungi, mycobacerium); check PPD, mumps
- Phagocytic: skin abscesses/periodontal; test: Nitrblue tetrazolium respiratory burst
- Complement: associated with autoimmune diseases (Hereditary angioedema), Neisseria (meningitis), pyogenic bacterial infections
- NK: severe recurrent Herpes; Hemophagocytic lymphohistiocytosis/macrophage activation syndrome
5 notes
·
View notes
Text
Haematology
Haematology is a discipline concerned with the production, function, and disorders of blood cells and blood proteins. We are familiar with blood from the time of our first skinned knee, but what is it really made of? Blood is a liquid consisting of plasma (water, electrolytes, nutrients, waste products, and many soluble proteins) in which red cells, platelets and a variety of white cells are suspended. Its volume is about 70 mL/kg or about 5L total in an average size adult. 40-50% of blood volume is occupied by red cells.
1 Some of the important proteins in the blood are:
· Albumin, which contributes a large portion of the oncotic pressure of plasma.
· Immunoglobulin (antibodies), which combat infection
· A number of proteins involved in the clotting cascade.
2 The cellular components of blood include:
· Red blood cells (RBC, about 5 x 106 / µL), which carry oxygen to tissues
· Platelets (about 250,000 / µL), which facilitate clotting.
· White blood cells (WBC, about 5,000 / µL), which fight infection. WBC can be further subdivided into neutrophils, lymphocytes (T, B, and natural killer [NK] cells), monocytes, eosinophils, and basophils (listed in order of typical frequency).
One of the most common blood test in wakad ordered by all medical specialties is the complete blood count, or CBC. The pathology labs in wakad uses an analyzer that functions both as a spectrophotomer and a flow cytomer. This instrument can determine the concentration (count) of RBC, platelets and WBC, the hemoglobin (Hgb) concentration, and the mean size of the red cells (MCV). The flow cytometer can accurately distinguish and count the various types of WBC, which it reports as a “differential”. The hematocrit (Hct), which represents the percentage of blood volume occupied by red cells, is calculated from the RBC count and the MCV. As the CBC results can tell you a great deal about potential disease processes affecting a patient.
Note the higher values in the newborn. This is due to the predominance of HgbF (fetal), which is more efficient at extracting oxygen from the placenta but less efficient in delivering oxygen to the tissues (left shifted O2 dissociation curve, see below). The differences between adult males and females are due to testosterone(hormonal test in wakad), which increases erythropoietin production. In aged men, testosterone(hormonal test in wakad) levels fall and the disparity between men and women decreases. The mean cell volume (MCV) can be a helpful clue as to the cause of low Hgb levels.
#diagnosticscentersinwakad pathologylabsinwakad bloodtestinwakad#feverprofiletestinwakad fertilitytestinwakad hormonaltestinwakad
0 notes
Text
so
eosinophil x nk cell. anyone?
19 notes
·
View notes
Text
TIẾP CẬN BỆNH LÝ SUY GIẢM MIỄN DỊCH TIÊN PHÁT Ở TRẺ EM Ở TRẺ EM
PHÁC ĐỒ ĐIỀU TRỊ TIẾP CẬN BỆNH LÝ SUY GIẢM MIỄN DỊCH TIÊN PHÁT Ở TRẺ EM Ở TRẺ EM
I. ĐỊNH NGHĨA
Bệnh lý suy giảm miễn dịch tiên phát (SGMD tiên phát) là bệnh lý di truyền gây rối loạn phát triển hệ thống miễn dịch của cơ thể, làm giảm chức năng hoạt động của các miễn dịch tế bào và miễn dịch dịch thể.
Bệnh có thể xuất hiện ở bất cứ lứa tuổi nào, tuy nhiên trẻ dưới 2 tuổi có tỉ lệ cao.
II. CHẨN ĐOÁN
1. Công việc chẩn đoán
a. Hỏi: tìm các dấu hiệu cảnh báo của bệnh.
• Dấu hiệu mệt mỏi, lừ đừ, bỏ ăn, chậm lên cân hay sụt ký, ho thường xuyên, tiêu chảy kéo dài, sốt kéo dài, nấm miệng.
• Tiền sử cá nhân:
- Tiền sử sơ sinh có chậm rụng rốn trên 30 ngày.
- Tiền sử biến chứng sau tiêm chủng các vaccin sống.
- Tiền sử tiêu chảy kéo dài.
- Vết thương không làm sẹo.
- Tiền sử nhiễm trùng nặng, kéo dài hoặc tái phát nhiều lần, cụ thể sau 10 dấu hiệu theo Feffrey Modell Foundation (FMF):
1. Bị nhiễm trùng ở tai từ bốn lần hoặc nhiều lần hơn trong vòng 1 năm.
2. Bị viêm xoang nặng từ hai lần hoặc nhiều lần hơn trong vòng một năm.
3. Có hai tháng hoặc nhiều tháng hơn dùng kháng sinh mà hiệu quả kém.
4. Bị viêm phổi hai lần hoặc nhiều lần hơn trong vòng một năm.
5. Không lên cân và tăng trưởng theo bình thường.
6. Bị áp xe cơ quan hoặc mô dưới da tái phát nhiều lần.
7. Nấm miệng hoặc nấm da kéo dài.
8. Cần đến truyền kháng sinh để điều trị triệt để nhiễm trùng.
9. Bị nhiễm trùng nặng, nhiễm trùng huyết hai hoặc nhiều hơn trong năm.
10. Tiền sử gia đình bị suy giảm miễn dịch tiên phát: có người bị bệnh
nhiễm trùng tái phát, bệnh tự miễn, tử vong không rõ nguyên nhân
(dưới 30 tuổi).
- Mắc bệnh dị ứng, tự miễn, đau khớp.
b. Khám lâm sàng:
khám toàn diện, cần lưu ý các dấu hiệu sau.
• Tổng trạng có lừ đừ, suy kiệt, sụt cân, suy dinh dưỡng nặng.
• Đánh giá mức độ và vị trí nhiễm trùng.
• Tuổi lúc phát bệnh, vị trí bệnh để chẩn đoán thể bệnh.
• Vị trí nhiễm trùng thường gặp.
• Một số bệnh SGMD tiên phát lúc mới phát là bệnh lý miễn dịch như: Thiếu máu huyết tán tự miễn, xuất huyết giảm tiểu cầu miễn dịch, viêm tuyến giáp tự miễn, viêm mạch máu, Lupus đỏ hệ thống, viêm khớp dạng thấp.
• Một số bệnh SGMD tiên phát lúc mới phát bệnh là bệnh lymphoma, tim bẩm sinh (thể thân động mạch chung), hoặc hạ Calci máu, hoặc X-quang không có tuyến ức.
c. Đề nghị xét nghiệm
• Xét nghiệm sàng lọc ban đầu:
- Huyết đồ đầy đủ.
- Điện di protein.
- Xét nghiệm khảo sát nhiễm trùng.
• Xét nghiệm chuyên sâu:
- Định lượng IgG, IgM, IgA,IgE.
- Khảo sát dấu ấn miễn dịch tế bào lympho.
- Chẩn đoán di truyền (khi có hypogammaglobulin, tìm đột biến gen Btk).
2. Chẩn đoán xác định (theo WHO 2007, khi bệnh nhân hội đủ các tiêu chuẩn sau)
• Có nhiễm trùng tái phát nhiều lần: khi có trên 2 dấu hiệu cảnh báo trong 1 năm (10 dấu hiệu cảnh báo theo JMF 40).
• Bất thường tế bào bạch cầu về số lượng hay chức năng trong máu ngoại biên.
• Bất thường nồng độ kháng thể miễn dịch trong huyết tương.
• Có tính di truyền trong gia đình.
• Xác định có gen đột biến.
3. Chẩn đoán có thể
Khi bệnh nhân hội đủ các tiêu chuẩn sau:
a. Có nhiễm trùng tái phát nhiều lần: khi có trên 2 dấu hiệu cảnh báo (10 dấu hiệu cảnh báo theo JMF *).
b. Giảm tế bào bạch cầu có 1 trong các tiêu chuẩn sau
• Lympho bào < 2,2 x 109/L (sơ sinh), < 2,5 x 109/L (trẻ < 5 tuổi) hoặc < 1,5 x109/L (trẻ > 5 tuổi). VÀ
• Giảm nồng độ kháng thể khi có 1 trong các tiêu chuẩn sau:
- Agammaglobulin: IgG < 100mg/dL.
- Hypogammaglobulin IgG < 400mg/dL.
- Panhypogammaglobulin: IgG < 400 mg và IgAị, IgMị.
- Severve selective IgA deficiency: IgA < 7mg/dL (>4 tuổi).
- Partial selective IgA deficiency: IgA > 7 và thấp so với bình thường ± độ lệch chuẩn.
- Hyperimmunoglobulin E syndrome: IgE >2000 IU/ml.
c. Bất thường tế bào T, B hay NK khi có 1 trong các tiêu chuẩn sau
• Tế bào CD4 < 1000 tb/ụl (trẻ < 5 tuổi); < 500tb/ụl (trẻ > 5 tuổi).
• Tế bào CD19 < 100 tb/ụl (hay dưới 2% lympho bào).
• CD16/56 < 2%.
d. HOẶC có bất thường bạch cầu hạt (neutrophil)
• Neutrophil > 25, x 109/L và có dấu ân tế bào CD18 (-), CD11 giảm
• Neutrophil < 1,0 x109/L.
• HOĂC: phết máu ngoại biên:
- Hạt azurophilic hiện diện trong neutrophil, eosinophil hoặc
- Neutrophil chỉ có 2 thùy và không có hạt.
e. Và hoặc có tiền sử gia đình
4. Chẩn đoán phân biệt các thể bệnh SGMD tiên phát có giảm kháng thể
Bảng 1. Đặc điểm miễn dịch và chẩn đoán phân tử của các thể bệnh SGMD tiên phát có giảm kháng thể miễn dịch. Theo Bonilla F.A. uptodate (2011).
Bệnh
Tên bệnh viết tắt
Flow
cytometry Serum
Immunoglobulin
(mg/dL) Chẩn
đoán di
truyền Tuổi
phát
bệnh Miễn
dịch
liệu
pháp
X-linked
Agammaglobulinemia
XLA
B < 2% IgG< 400
IgM<20
IgA< 20 B cell
tyrosine
kinase > 6
tháng
tuổi Cần
Hyper IgM syndrome: Activation-induced adenosine deaminase deíiciency Uracil nucleoside glycosylate deíiciency
AID
UNG
T ↔
B ↔ IgG < 200
IgA < 20
IgM: 100-3700 CD40
ligand > 6
tháng
tuổi Cần
Common variable immunodeíiciency
CVID
T ↓ và
hoặc
B ↓ IgG < 400
IgM < BT
IgA < BT Chưa
xác
định Mọi
tuổi Cần Severe combine
immunodeficiency SCID T < 20% IgG↓
IgM↓ ┴
IgA↓ Tùy đột
biến < 6
tháng Cần Selective IgA deficiency IGAD ↔ IgA< 7
IgG↔ IgM ↔ TACI > 4
tuổi Không IgG subclass deficiency IGGSD ↔ IgG subclass ↓ Mọi
tuổi Tùy Wiskott Aldrich
syndrome WAS CD8 ↓
B ↔ IgG ↔, IgM↓
IgA↑, IgE ↑ WAP Sơ
sinh Cần Transient
hypogammaglobulinemia
of infancy THE T ↔
B ↔ IgG ↓
IgM ↔
IgA ↔ Không 3-24
tháng Không
• Ký hiệu viết tắt:
↔: không thay đổi
↓: giảm
↑: tăng
>: cao hơn
<: thấp hơn
• Tên viết tắt
- XLA: X-linked agammaglobulinemia.
- AID: activation-induced adenosine deaminase deficiency.
- CVID: common variable immunodeficiency.
- IGAD: IgA deficiency.
- IGGSD: IgG subclass deficiency.
- SAD: specific antibody deficiency (with normal immunoglobulins).
- THI: transient hypogammaglobulinemia of infancy.
- TACI: Transmembrance activator and calcium-modulator and cyclophilin ligand interactor”.
- WAP: Wiskott Aldrich Protein.
- WAS: Wiskott Aldrich syndrome.
III. ĐIỀU TRỊ & PHÒNG BỆNH
1. Nguyên tắc
Đây là bệnh lý di truyền do đó phát hiện sớm, chẩn đoán sớm và can thiệp sớm sẽ cải thiện tiên lượng sống của bệnh nhi.
• Điều trị phòng ngừa nhiễm trùng.
• Điều trị nhiễm trùng cơ hội.
• Miễn dịch liệu pháp.
• Lưu ý về chủng ngừa.
2. Miễn dịch liệu pháp
• Chỉ định Immunoglobulin: nhiễm trùng nặng: nhiễm trùng huyết, viêm phổi nặng, nhiễm trùng thần kinhh trung ương.
• Liều: Immunoglobulin trung bình 0,4 g/kg/lần truyền tĩnh mạch chậm tùy theo chế phẩm.
• Phản ứng khi dùng IVIG trong bệnh SGMD tiên phát
- Phản ứng liên quan tới tốc độ truyền.
- Sốc phản vệ.
3. Kháng sinh phòng bệnh
• Chỉ định: kháng sinh phòng bệnh khi bệnh nhân SGMD tiên phát có 1 trong các tiêu chuẩn sau:
- Bệnh nhân bị giảm kháng thể gammaglobulin; giảm IgA; hay giảm chọn lọc các thể phụ của IgG và bệnh SGMD không có chỉ định truyền Immunoglobulin định kỳ. Đối với nhóm này có chỉ định dùng kháng sinh trong giai đoạn cụ thể: mùa dễ mắc bệnh như mùa lạnh hay mùa mưa, hoặc trong giai đoạn trẻ nhỏ.
- Bệnh nhân giảm nặng kháng thể và có dùng IVIG định kỳ nhưng vẫn có nguy cơ nhiễm trùng.
• Kháng sinh: chọn một trong các thuốc sau, 3 ngày/tuần.
- Amoxicillin: 20 mg/kg/ngày uống 1 lần.
- Trimethoprim-Sulfamethoxazol (Bactrim): 5 mg/kg/ngày.
4. Chủng ngừa
Bệnh nhân được chỉ định chủng ngừa theo lịch. Không chủng ngừa các vaccin sống giảm độc lực như sởi, quai bị, rubella, polio, cúm, rotavirus và BCG.
5. Giáo dục về phòng bệnh cho gia đình
• Tăng cường biện pháp vệ sinh: Rửa tay, vệ sinh răng miệng, nước sinh hoạt
• Hạn chế tiếp xúc gần gũi, ngủ chung với người các thành viên trong gia đình. Khuyến cáo các thành viên gia đình, người tiếp xúc lân cận nên chủng ngừa đầy đủ nhất là cúm.
• Tái khám và theo dõi qúa trình phát triển, phòng tránh nhiễm trùng
LƯU ĐỒ CHẨN ĐOÁN SUY GIẢM MIỄN DỊCH TIÊN PHÁT
(Lấy từ Hauk. PJ et al (2011) Immunodeficiency. Current Diagnosis & Treatment in Pediatrics.31:921)
.Bài viếtTIẾP CẬN BỆNH LÝ SUY GIẢM MIỄN DỊCH TIÊN PHÁT Ở TRẺ EM Ở TRẺ EM xuất hiện lần đầu tại website http://khamgiodau.com
0 notes
Photo







first (accidental) date pt. 1
did you notice the eosinophiil/nkcell/shannon/kannon that i snuck in the background?
Pt. 2 here: https://pfeldspart.tumblr.com/post/177816215025/first-accidental-date-pt-2-pt
#hataraku saibou#cells at work#Red Blood Cell#white blood cell#rbc x wbc#wbc x rbc#pink blood cell#hataraku saibo#comic#eosinophil#nk cell
715 notes
·
View notes
Text
Going through questions:
Nitroblue tetrazolium testing is used for diagnosis of Chronic Granulomatous Disease (CGD). Normally, neutrophils will turn blue on nitroblue tetrazolium testing because of the respiratory burst in phagolysosomes, but there is no blue color change in CGD because there is no production of oxidative species. CGD is due to an X-linked Recessive NADPH oxidase mutation. NADPH oxidase catalyzes production of reactive oxygen species, which kill bacteria. NADPH also catalyzes activation of granule proteases, like elastase, in phagosomes. Mutation of NADPH oxidase gene-> deficient NADPH oxidase-> neutrophils and macrophages can't kill bacteria that they phagocytose. This leaves pts susceptible to recurrent fungal and bacterial infections, especially catalase + bugs (staph aureus, serratia marcenscens, aspergillus, burkholderia cepacia, and nocardia). The skin, lungs, liver, and lymph nodes are often infected in these pts. For diagnosis of CGD, you want to measure neutrophil superoxide production with either the Nitroblue Tetrazolium (NBT) test or with flow cytometry using dihydrorhodamine (DHR). The DHR test is better.
IL-12 presented to naive helper T cells by macrophages causes naive helper T cells to differentiate into Th1 cells, which release IFN-gamma; IFN-gamma activates cytotoxic CD8+ T cells and macrophages to kill intracellular pathogens. Mycobacterium is an intracellular pathogen that is killed this way. People with IL-12 deficiency can't mount a cell-mediated immune response and are susceptible to mycobacterium infection. Interferon gamma is given to treat these pts.
In OnlineMedEd, Dustyn said that in graft vs host disease, the lymphocytes in the donor tissue trigger the recipient to make antibodies against the recipient. In this question I just answered, it says that T lymphs in the donated organ are sensitized to the recipient's MHC Ag and then they attack the host's tissues. Donor T cells from the donated organ go into the host's tissues, become sensitized to the host's MHC antigens, and then the donor CD4+ and CD8+ T cells destroy host cells. The GI tract, the skin, and the liver are usually affected. The pt can get a rash that includes the palms and soles.
IL-2 is made by CD4+ helper T cells and activates more CD4+ helper T cells, cytotoxic CD8+ T cells, Natural Killer cells, monocytes, and B cells. T cells and natural killer cells activated by IL-2 kill renal cancer and metastatic melanoma. I posted a picture showing how immumosuppressants work. So IL-2 causes activation of macrophages and NK cells, proliferation and differentiation of helper T cells, growth and secretion of IFN-gamma from T cells, and proliferation of B cells.
Macrophages, B cells, dentritic cells = Antigen-Presenting Cells (APCs); they have MHC Class II, which they use to present angtigens to CD4+ helper T cells.
Type IV (T cell-mediated/delayed type) HSR = T lymphs release cytokines that cause induration 24-48 hours after exposure to the Ag. So cytokines, CD8+ T cells, and macrophages cause the type IV HSR. Poison ivy is a type IV HSR.
Poison ivy, poison oak, and poison sumac make urushiol, which attaches to proteins (haptenization)-> T-cell mediated immune response. CD8+ T cells destroy keratinocytes with the haptenated proteins.
Accumulation of ADA-> destruction of lymphocytes. Adenosine is converted to inosine by adenosine deaminase (ADA). ADA also catalyzes the conversion of deoxyadenosine to deoxyinosine. If ADA is absent, then deoxyadenosine is converted to dATP and that causes lymphocyte apoptosis. Hairy cell leukemia is a lymphocyte cancer, which can be treated with ADA inhibitor (cladribine). ADA deficiency also causes SCID, which is lack of B and T cells.
Hib vaccine is made with the polysaccharide capsule of Hib conjugated to tetanus toxoid carrier protein (or N. meningitidis outer membrane protein). The protein conjugation elicits T cell mediated immune response-> B cell activation-> memory B cells, which causes long term immunity. The capsule isn't effective at eliciting the T cell response in pts younger than 2 years old because their humoral immunity is underdeveloped. So conjugating the capsule polysaccharide to a protein increases the humoral response against the capsule via T cell activation. T cells-> B cell stimulation-> memory B cells.
Steroids cause neutrophil count to increase because it prevents them from marginating (lining up against the walls of blood vessels). Steroids can cause hypomania and psychosis. Steroids decrease basophils, eosinophils, lymphs, and monocytes.
Mycophenolate inhibits IMPDH, which prevents conversion of inosine monophosphate to guanosine monophosphate. This prevents DNA and RNA synthesis in lymphs. Mycophenolate is used to prevent transplant rejection.
Eosinophils release major basic protein, which causes the induration that occurs 2 to 10 hours after exposure to an allergen. It's responsible for the late phase of a dermatologic type I HSR and is IgE-mediated. Major basic protein damages tissue. Wheal and flare is the early phase of a type I HSR in the skin. The late phase induration of the skin is due to release of major basic protein from eosinophils. Contrast this with type IV HSR, which is T cell-mediated and takes days, rather than hours, to develop.
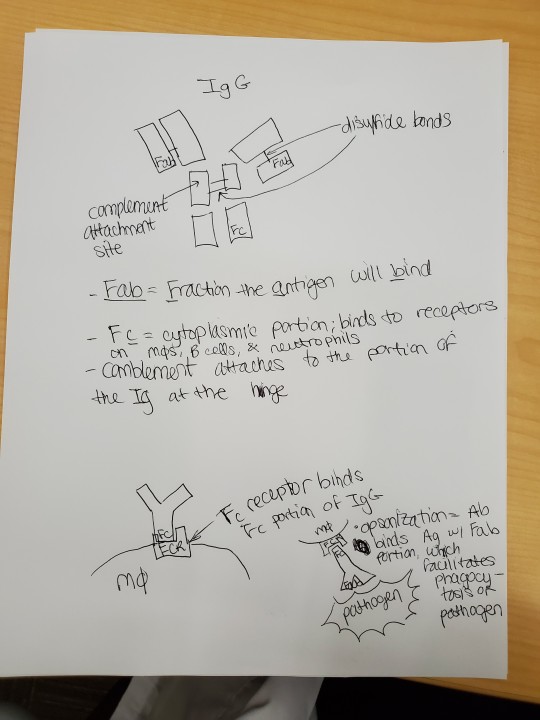
Classical complement pathway starts with C1 binding to 2 IgGs or 2 IgMs. C1 binds Fc region of heavy chain near the hinge point. After IgM binds to an antigen, the C1 binding site is revealed and C1 can bind to it, activating complement.
There are more steps in WBCs leaving the vessels to get to the cytokines than what he mentioned in OnlineMedEd. The steps of inflammation are: margination, rolling, activation, tight adhesion and crawling, and transmigration. He grouped it differently in the video. Rolling is when the neutrophil slows down via interaction of its sialylated carbohydrate groups with selectins on endothelial cells. For example, sialyl Lewis X or PSGL-1 on neutrophils with selectins on endothelial cells. Then integrins on the endothelial surface (ICAM-1) stop the WBCs. In the tight adhesion and crawling phase of inflammation, CD18 beta 3 integrins on neutrophils bind to ICAM on endothelial cells. Then PECAM lets neutrophils slide through the spaces between the blood vessel wall cells during transmigration. Leukocyte adhesion deficiencies (LADs) prevent leukocytes from migrating from the blood to the site of cytokine release. LAD type 1 = no CD18-> no beta 2 intergins-> skin infections with no pus and delayed separation of umbilical cord.
C1 inhibitor deficiency leads to cleavage of C2 and C4-> excessive activation of complement system; also causes angioedema and GI symptoms.
Hemolytic Disease of the Fetus and Newborn (HDFN) occurs when the mom has type O blood and thus makes IgG against type A and B blood. If this mom's baby has type A, B, or AB blood, her IgG can diffuse across the placenta and cause hemolysis in the baby. But moms with type A or B blood make IgM antibodies (anti-B if the mom has type A blood; anti-A if the mom has type B blood), which can't cross the placenta, and thus don't cause hemolysis in the newborn. In contrast to Rh disease, HDFN can occur during the first pregnancy because the mom makes anti-B and anti-A IgGs in response to similar antigens that are encountered early in life.
Leukotriene B4 causes neutrophil chemotaxis.
#immunology#nitroblue tetrazolium#CGD#chronic granulomatous disease#dihydrorhodamine#NBT#GVHD#interleukins#IL2#IL12#HSR#ADA#adenosine deaminase#SCID#hairy cell leukemia#poison ivy#urushiol#contact dermatitis#major basic protein#complement
3 notes
·
View notes