#hypo and hyperthyroidism
Explore tagged Tumblr posts
Text
sometimes i tell people ive had the same family doctor my whole life and theyre like "wow thats so nice i bet they know u so well!" and like. youd think! you really would think. However
#good morning#sometimes u find out at 7am that ur doc has been so hyperfixated on watching for signs of inherited hyperthyroidism#that she perhaps completely missed the fact and signs that my thyroidism was not hyper but hypo#even tho the top 3 symptoms are things i sought help from her for 🙃#im not my MOTHER!!!!!!!!!
5 notes
·
View notes
Text
They raised my thyroid pill dose and I've been feeling anxious and no appetite lately and I'm wondering if it's just making me hyperthyroid. But honestly I would prefer it over being hypo and it seems like the dose is never correct and when it works, it's only a matter of time before it doesn't anymore.
7 notes
·
View notes
Text
So.
I think my immune system might be doing the same thing to my parathyroid glands as it does my thyroid gland...
Attack it just long enough to cause it to relentlessly spill hormone, but not enough that it can't heal [the downside of healing well] so basically my body is periodically flooding itself with hormone in a way that completely ignores anything that's meant to trigger hormone release.
That's why I have Hashimoto's but am hyperthyroid instead of hypo thyroid...
And similarly I think this might be primary hyperparathyroidism caused by autoimmune attack.
Which of course is dangerous and near impossible to treat because all the usual culprits that would trigger the release of hormone -or stop it- don't matter or have any impact, because the gland isn't *releasing* the hormone, my immune system is making it leak out, but my body also won't stop trying to produce the stupid hormone.
I think this is driving up my blood phosphorus and thus calcium levels, causing all my symptoms this time and last time[s], hence the bone pain, struggle for my kidneys -which outside of attacks work fine enough- to keep up with all the blood minerals and etc...
The problem is that the usual ways of calming down pth production won't help.
I normally control my thyroid hormone levels by restricting iodine and b vitamins...
I cannot get a full list of what your body uses to make pth out of the internet. It's only mentioned -in an unrelated search- that your body needs magnesium to make it... Magnesium, the one thing that can stop me from having heart attacks from high blood calcium. The one thing I will be forced to take if I start getting any chest pain again.
This leaves the solution at restricting all vitamins it might use to release or make hormone and also restrict calcium and phosphorus, because the excess levels of those are obviously not getting the gland to stop releasing hormone...
The problem with that is that the full list covers almost all macro nutrient minerals your whole body needs for everything all the time... Which is why hyperparathyroidism is usually managed by surgically removing whatever ones of 4 glands are acting up...
But for that to be done I would have to have a doctor catch the hormone levels being high during an attack and get them to also check my blood mineral levels, and concede it is in fact autoimmune and that I can't solve it by just eating more or less of the usual suspects.
I went through this same song and dance with my thyroid for over 10 years and still haven't gotten any help or answers because my body is behaving atypically even for having a rarer condition.
I might have luck with an h4 antihistamine but you can't get those without a prescription, so if I don't figure out how to manage this with diet, the problem isn't likely to go away and is liable to turn dangerous again at any time.
The first attack I ever had lasted a year and a half and the worst of it included daily cardiac spasms [heart attacks with no clot that still risk stopping your heart].
I have already been in for this problem countless times since it started and it's the only reason I am not going in for it now. They already willfully missed the problem more than 20 times even when I was having heart attacks and going into hypertensive crisis.
I need to drag out of the internet what I can do to intentionally nerf my pth production that isn't too essential to other body systems, or find a way to calm my immune system the fuck down about my own glands without taking anything that's heard on my kidneys, which are being taxed by obscene levels of minerals in my blood.
This mc fucking explains the swelling in my throat too that didn't seem to be my thyroid gland [big gland, very visible] but is right in the same area.
Usually this shit is caused by a tumour, but I mcfucking guarantee you it's just autoimmune bullshit I can't do much about and that doctors will ignore unless I completely corner them with it.
This probably also means vitamin c needs to be off the table even though in studies people with higher vitamin c tend to reabsorb less phosphorus from their kidneys...
And no fucking wonder a multivitamin, organ stress and potential rexposure to corona triggered this, on top of a bunch of extra phosphorus from coca cola... And no wonder calcium is making it worse, and no wonder the loratadine seems to help long term but fuck up my kidney function short term.
The annoying thing? Even taking advil/ibuprofen to keep down the selling makes you retain more water.
I need to keep the swelling down some so I can stand up and move. I'm thinking of re-incorporating small doses of loratadine and anything else that will calm down any part of my immune system.
My kidneys aren't having volume processing issues AT ALL. In fact, they are processing MORE fluids daily than google says they aught to be able to, so long as I keep having enough salt and potassium.
Currently my plan is still to try to give myself DODNE on purpose to stop the attack.
And I can slowly re-introduce minerals and vitamins up to whatever level doesn't trigger symptoms.
But if I need surgery to fix this, with corona virus still being a thing, I might be thoroughly fucked. I cannot be under anesthesia while maintaining my proper breathing mask so they don't infect me in the hospital, so getting surgery is a pretty near 100% guarantee of being fully re-infected with corona, which is what almost killed me the first time and set all this off.
I am so fucking tired.
Maybe that's why all those heavy regimes of antihistamines only temporarily nerfed my kidney function and didn't seem to do any permanent damage to their function? Maybe I can still fix this if I know the exact problem I am targeting.
I'm going to try to find more information on exactly how the body produces pth...
4 notes
·
View notes
Text
This is not a "this kind of disabled person should kill themselves or their experiences with their disability warrants killing themselves" post. People with these illnesses and disabilities can and do live full beautiful lives and deserve to be able to enjoy themselves and live long lives.
This is an "if I gained these illnesses or disabilities because I have family history of them on top of my multiple illnesses and disabilities I likely would die very young without extremely extensive support that I do not and will never have access to and I'm complaining about that" post. That said.
If I get any of the following diseases or disabilities I will just fucking die, actually.
Diabetes
Cancer
Progressive endometriosis or pcos
Rheumatoid arthritis
Alzheimers disease or some other form of dementia
Chronns disease
Any type of non-fatal organ failure
Parkinsons disease
Muscular dystrophy of any kind (I experience atrophy but not dystrophy and I am able to regain muscle mass with a lot of time and work, something not possible for people suffering with most kinds of dystrophy)
Any form of substance abuse or addiction
High cholesterol
High blood pressure
Low blood pressure
Hypo or hyperthyroidism
Any type of seizure disorder
That is all thank you.
#I already have disabilities and illnesses that would massively complicate any of these if I got them#What would be a perfectly manageable condition for anyone else would be fatal to me#Not because I would be upset about it and give up#Though I would be upset#But because if I developed like arthritis or something performing basic functions will become impossible#And I will be fully immobile#So without care that I can not afford and do not have access to I will likely die very fast#disability#chronic illness#chronic health#mental health#mental illness#cripple#cripple punk#disabled
8 notes
·
View notes
Text
The Endocrine System
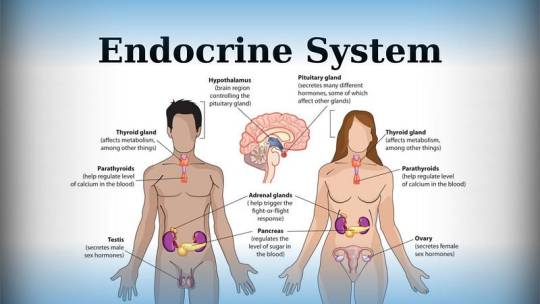
Introduction
The endocrine system is a complex network containing a symphony of hormonal interactions crucial for maintaining physiological equilibrium. Comprising glands, organs, and tissues dispersed throughout the body, its influence allows various bodily functions, spanning from metabolism to reproduction and beyond. This topic endeavors to provide an in-depth exploration of the endocrine system, encompassing its anatomy, physiological functions, associated conditions, and strategies for proactive care. By indulging into this indispensable regulatory system, we aim to equip readers with a comprehensive understanding to prioritize their hormonal health effectively.
Anatomy of the Endocrine System
The anatomy of the endocrine system is contained by an array of specialized glands, organs, and tissues, each endowed with the capacity to synthesize and dispatch hormones into the bloodstream. Principal among these are:
Endocrine Glands: These specialized tissues, including the pituitary gland, thyroid gland, and adrenal glands, secrete hormones directly into circulation, exerting systemic effects.
Endocrine Organs: Organs such as the hypothalamus, pancreas, and reproductive glands contribute to hormonal regulation, interfacing closely with the nervous system to modulate physiological responses.
Endocrine-Related Tissues: Adjunct to traditional endocrine structures, adipose tissue, kidneys, and even the heart harbor the capability to produce hormones, further augmenting the system’s complexity and regulatory capacity.
Functions of the Endocrine System
The cardinal function of the endocrine system is hormone secretion, holding up varied network of intercellular communication. Hormones, acting as molecular messengers, traverse the bloodstream to target cells, eliciting diverse physiological responses.
Key functions include:
Metabolism Regulation: Hormonal content govern metabolic processes, dictating energy expenditure, glucose homeostasis, and lipid metabolism.
Homeostatic Control: Endocrine signaling regulates internal threshold, modulating blood pressure, fluid balance, and body temperature.
Development and Growth: Hormonal interplay underpins growth trajectories and developmental milestones, steering embryonic stages and pubertal maturation.
Sexual Function and Reproduction: Hormonal modulation governs reproductive physiology, controlling fertility, libido, and secondary sexual characteristics.
Neuroendocrine Integration: The endocrine system reveals intimately with the nervous system, harmonizing behavioral and physiological responses, including mood regulation and sleep-wake cycles.
Conditions and Disorders
A spectrum of endocrine-related ailments afflicts individuals, stemming from hormonal imbalances, glandular dysfunctions, or neoplastic proliferations. Noteworthy conditions encompass:
Diabetes and Metabolic Disorders: Spanning type 1 and type 2 diabetes, metabolic syndrome, and obesity, these conditions disrupt glucose homeostasis and metabolic equilibrium.
Endocrine Cancers and Tumors: Malignancies affecting endocrine tissues, including adrenal tumors, pituitary adenomas, and thyroid malignancies, necessitate specialized oncological management.
Thyroid Dysfunction: Hypo- and hyperthyroidism, thyroid nodules, and autoimmune thyroiditis typify prevalent thyroid disorders, precipitating diverse clinical manifestations.
Reproductive and Sexual Health Disorders: From polycystic ovary syndrome (PCOS) to erectile dysfunction, disruptions in reproductive hormone signaling manifest as infertility, menstrual irregularities, and sexual dysfunction.
Proactive Care and Health Maintenance
In fostering endocrine wellness, a holistic approach integrating lifestyle modifications and environmental awareness is imperative. Strategies for promoting endocrine health encompass:
Lifestyle Optimization: Embracing a balanced diet, regular exercise regimen, and adequate sleep hygiene fosters metabolic resilience and hormonal equilibrium.
Environmental Vigilance: Mitigating exposure to endocrine-disrupting chemicals pervasive in everyday products, such as plastics, pesticides, and personal care items, reduces the risk of hormonal perturbations.
Health Surveillance: Individuals with familial predispositions to endocrine disorders benefit from proactive screening and vigilant symptom monitoring, facilitating early intervention and optimal disease management.
Conclusion
The endocrine entails physiological regulation, producing hormonal interactions essential for vitality and well-being. By looking at anatomy, physiological functions, associated conditions, and avenues for proactive care, this discourse endeavors to foster a comprehensive understanding of the endocrine system Empowered with knowledge, individuals can prioritize their hormonal health, embracing proactive measures to optimize their overall well-being and quality of life.
For medical students navigating the study of endocrinology and seeking guidance and academic support during their study period, Expert Academic Assignment Help offers invaluable assistance. With our expertise and resources, we provide tailored solutions to aid in comprehension, research, and academic success. Don’t hesitate to reach out to us for personalized assistance and elevate your understanding of this vital field. Your academic journey awaits, and we’re here to help you excel.
Contact us at [email protected] for professional assistance,
#assignment help#medical students#healthcare#nursing school#nursing student#medical school#medical student#pharmacy student#pharmacology#endocrine system#endocrinologist#pharmacy technician
2 notes
·
View notes
Text
... I don't think anybody is suggesting that? Just a possible way to sidestep current bigotry. There are a lot of endocrine disorders that have nothing to do with being trans or intersex or have multiple other causes or origins - Hashimoto's, primary hyperparathyroidism, genitourinary syndrome of menopause, hypo/hyperthyroidism, and metabolic syndrome, just to name a couple off the top of my head. In fact, all of the ones I just listed can also be caused in perisex cis, intersex or perisex trans people who have/had a uterus due to peri/menopause.
Nobody is asking intersex people to act as meat shields. I get the reaction, but in this case, I think it's wildly, wildly misplaced, and could cause vulnerable trans people to not use tools to protect themselves. Please don't shame people who are trying to protect themselves in a way that genuinely has nothing to do with you. I get why you have such a strong reaction, but...
There are so, so many hormone disorders treated with HRT. Making this change to their medical records is a choice every person has to make on their own with their doctor based on what's best for them, and like... I don't see anybody saying "pretend to be intersex," friend.

I know people aren't here for the news, but trans folks, I'm thinking of you tonight and how you deserve better.
53K notes
·
View notes
Text
Kayakalpa Clinic by Dr. Shruthi — Your Trusted Endocrine & General Health Center in Vadodara

Led by Dr. Shruthi, a renowned MD physician in Vadodara and an expert in metabolic health, the clinic provides a personalized, holistic approach to treating a wide range of conditions — from chronic diseases to hormone-related issues.
Whether you’re looking for a female general physician near me or a trusted endocrinologist in Vadodara, we focus on early diagnosis, lifestyle guidance, and long-term management for optimal health outcomes.
Our Expertise Includes:
Best general physician in Vadodara for routine care, chronic illness management & diagnostics
Best endocrinologist in Vadodara for hormone imbalance, thyroid disorders & diabetes
PCOS treatment clinic in Vadodara offering customized care for hormonal and menstrual health
Diabetes specialist in Vadodara for expert management and reversal guidance
Thyroid doctor in Vadodara with a focus on hypo/hyperthyroidism and auto-immune conditions
Obesity treatment in Vadodara with metabolic correction and weight loss support
High blood sugar treatment Vadodara with lifestyle and insulin resistance interventions
Insulin resistance treatment in Vadodara for pre-diabetes and metabolic syndrome
Diabetes reversal program in Vadodara based on evidence-backed protocols
Endocrine clinic in Vadodara for all hormonal disorders in men and women
Hormone specialist near Vadodara addressing imbalances affecting mood, metabolism, and energy
Visit Us At:
Kayakalpa Clinic by Dr. Shruthi Meraki Latitude, 211/212, Old Padra Rd, Dev Deep Nagar, Tandalja, Vadodara, Gujarat 390020 Phone: 09023268462
Clinic Timings:Monday — Saturday 10:30 AM — 1:00 PM 5:00 PM — 7:30 PM Sunday: Closed
Location:- https://maps.app.goo.gl/cfWCqhTCgS96JuPKA
If you’re looking for a diabetes management clinic near me or a compassionate PCOS treatment doctor in Vadodara, Kayakalpa Clinic is here to guide your journey toward better health — with personalized care that puts your well-being first.
0 notes
Text
Best Endocrinology Hospital in Kerala: Where Expertise Meets Compassionate Care
The endocrine system, often called the body’s hormonal powerhouse, plays a critical role in regulating essential functions such as metabolism, growth, reproduction, and mood. When things go wrong—be it due to thyroid imbalances, diabetes, PCOS, or rare glandular disorders—seeing an expert endocrinologist is crucial. If you're in search of the Best Endocrinology Hospital in Kerala, this guide will help you make an informed decision.
Why Endocrinology Care Requires a Specialist Approach
Endocrine disorders are complex and often interconnected. A simple hormonal imbalance can affect multiple organs, so diagnosis and treatment require a multidisciplinary and highly personalized approach. Kerala, known for its advanced healthcare infrastructure and skilled specialists, is home to several hospitals that offer world-class endocrinology care.
Here’s what sets a leading endocrinology hospital apart:
✅ Board-certified endocrinologists and diabetologists
✅ Advanced hormone testing and diagnostic labs
✅ Multi-specialty collaboration (e.g., cardiology, nephrology, gynecology)
✅ Long-term care and lifestyle management programs
✅ Patient education and digital follow-up systems
Top 5 Features of the Best Endocrinology Hospital in Kerala
1. Specialized Endocrinology Department
Look for a hospital with a dedicated endocrinology wing that covers all major hormonal disorders, including:
Thyroid diseases (hypo/hyperthyroidism, goiter, nodules)
Diabetes and insulin resistance
PCOS and infertility
Pituitary and adrenal gland disorders
Growth and puberty disorders in children
2. Comprehensive Diagnostic Support
The best hospitals offer in-house lab facilities for:
Hormonal assays
Thyroid function tests
Blood glucose monitoring
Imaging (ultrasound, CT, MRI for glandular imaging)
3. Multidisciplinary Teams
Because hormonal issues often affect multiple systems, effective treatment involves endocrinologists working closely with dietitians, nephrologists, gynecologists, and other specialists.
4. Patient-Centered Care
Top hospitals don’t just treat symptoms—they educate patients about long-term disease management, lifestyle changes, and follow-up care.
5. Reputation and Reviews
Patient testimonials, accreditation (e.g., NABH), and national rankings can help identify a hospital's reputation and consistency in care.
Top Hospitals Often Ranked Among the Best in Kerala for Endocrinology
Here are a few healthcare institutions frequently recommended by patients and professionals alike:
🏥 Amrita Institute of Medical Sciences, Kochi
Renowned for its world-class endocrinology department and research-driven approach, Amrita offers comprehensive care for all endocrine disorders.
🏥 Aster Medcity, Kochi
A state-of-the-art multispecialty hospital with a strong team of endocrinologists. Offers diabetes care, thyroid clinics, and hormone therapy under one roof.
🏥 KIMSHEALTH, Trivandrum
Recognized for its patient-focused care model and advanced diagnostic tools in managing both common and rare hormonal conditions.
🏥 Lakeshore Hospital, Kochi
Offers robust support for endocrine emergencies and chronic conditions. Its integrated care approach is ideal for complex hormonal disorders.
🏥 Baby Memorial Hospital, Kozhikode
Known for combining modern endocrine treatment with patient education and long-term follow-up, especially in northern Kerala.
Why Kerala?
Kerala is not only a popular health tourism destination but also a leader in healthcare outcomes in India. With its mix of qualified doctors, advanced medical infrastructure, and holistic treatment philosophies, Kerala is an ideal choice for anyone seeking specialized endocrine care.
Final Thoughts
Choosing the Best Endocrinology Hospital in Kerala means choosing long-term health, expert guidance, and compassionate care. Whether you're facing a common thyroid issue or a rare pituitary condition, the right hospital can provide the accurate diagnosis, treatment, and support you need to lead a healthy life.
Don’t wait for symptoms to worsen—consult an experienced endocrinologist and take control of your hormonal health today.
0 notes
Text
Homeopathic Remedies For Hypo And Hyperthyroidism

Homeopathy is a gentle, side-effect-free treatment for thyroid disorders. Naturally control hypothyroidism and hyperthyroidism with personalized treatment. Both hypothyroidism and hyperthyroidism can significantly impact one’s quality of life, but with proper diagnosis and treatment, these conditions are manageable. If you experience symptoms of thyroid dysfunction, consult a healthcare professional for evaluation and personalized care.
#Best homeopathy medicine treatment#Hyperthyroidism treatment in homeopathy#Thyroid Management Homeopathy Clinic in Abu Dhabi#Homeopathy Remedies for Thyroid Abu Dhabi#Homeopathic Remedies For Hypothyroidism In Abu Dhabi#Best Homeopathy Medicine For hyperthyroidism Abu Dhabi
0 notes
Text
Fun fact about ADHD with this I found out due to an incident that landed me in the hospital: we are naturally very low on B12 vitamins and it can actually make our memories worse. It can also lead to neurological problems. We have a genetic lack of the stuff. I had a severe deficiency of it that left me loosing an entire 8 days. Started taking it and WOO BOY I can remember what I had for dinner yesterday. Had a conversation recently where I only forgot one word.
If you’re ADHD and craving chicken constantly and can’t handle other meats or feel sick after red meat/IBS symptoms: get B12. Chicken has it. You need it. Vegan alternatives are bananas, blueberries, oranges, some mushrooms, and beetroot. Several water flavorings you can find that have B12 on it and are usually organically sourced. The water is easier for me as I don’t have to remember to take a pill every morning. You need a lot of B12 on the daily so it’s hard to overdose on the vitamin.
B12 is important for breaking down proteins. If you don’t have it, those proteins bind to your nerves and can cause nerve damage and brain damage in later stages. I do not have constant access to a psychiatrist for my ADHD management so I did not find this out until it landed me in the hospital. I lost 8 days total of memory (of which ADHD drink hoard in my bed turned out to save my life as I couldn’t move. All I know is that I was found and we have no idea what happened during those 8 days outside of me not being able to move much for a while and that I kept myself barely hydrated enough not to die from dehydration) and developed numbness in one foot. All because I lacked B12. (I’m better now dw, but recovering from it has been far longer than it took for it to ravage my brain once I hit the point of no return. Recovery process for any vitamin deficiency that causes injury and illness averages at 6 months.)
B12 deficiency has also been linked to worsening mental states and can actually cause neurotypical people to act like Karens and develop narcissistic tendencies. Especially if it’s sudden and out of nowhere.
Short version to say: keep yourself safe and healthy. Figure out if your memory issues are from a vitamin deficiency that affects neurodivergents the most or if it’s from your own brand of brain spiciness. B12 isn’t the only vitamin that can do all this. I’m just stating from my own personal experience and being told B12 is most likely for neurodivergents.
I’ll add links and resources a little later in the replies/edit/reblog this when it’s not 2am in the morning. I am not a doctor just spreading my knowledge due to what happened to me and stating what to keep an eye out for as it appeared in me.
There are four stages. I made it to Stage 3. It can take years or months to reach this point.
Symptoms can include:
-Memory loss
-Brain fog/ forgetfulness
-Confusion
-New audio processing issues (like being able to hear something fine but you can’t understand what is being said. A friend described it as “dyslexia but for hearing” and I feel it fits.)
-Inability to continue thought or topic
-IBS-like symptoms when eating protein rich foods
-Migraines and headaches (mine were behind my eyes)
-Trouble walking (chronic clumsiness)
-Nausea
-Increased heart rate
-Depression
-Sudden change in mental state
-Mental impairment
-Permanent neurological damage
-Nerve damage
-Fibromyalgia-like symptoms (especially if your doc says “it’s like fibromyalgia but you’re not testing positive for it.” This was a direct quote for me.)
-Numbness in toes and fingers
-Tinnitus
-Joint pain
-Insomnia
-“Visible” heartbeat between your thumb and forefinger, may move your thumb in time to your heartbeat (left hand)
-Hypo/hyperthyroid-like symptoms (especially if you have the symptoms but do not test positive for it.)
-Overheat easily (mine included little to no sweat but no blocked pores or dehydration)
-Worsening vision
-AFAB: Ovarian cysts/worsening cramps/new fainting spells/loss of libido
-AFAB: Endometriosis is not confirmed to be linked officially but I’m mentioning here because it developed for me during the stages I had
-AMAB: Loss of libido/erectyle dysfunction/testicular discomfort/one doc mentioned taint cramps when they were discussing how B12 can affect people with me and I want to let you know that one sent me for a loop
This isn’t all of them, and you may not have all of them, but they’re major tells for it /more can develop over time and ones that are common for neurodivergent people. Especially if they’re in tandem with each other. The noticeable symptoms started out as the similarities to hypothyroidism for me then went into fibromyalgia-like. I thought the memory loss stuff was normal for ADHD but not the level it actually was. Hope this helps!
the curse of adhd:
i will remember with absolute clarity, when the thought strikes me that i have a text to send someone, that this is the fourth time in three days i've attempted to send this specific text
i will forget, in the time it takes me to pick up my phone, that i picked it up intending to send a text
#adhd#adhd problems#adhd things#adhd hacks#adult adhd#adhd memory issues#vitamin b12#executive dysfunction
52K notes
·
View notes
Text
Irregular Periods: Causes, Symptoms, and When to Seek Medical Help

A healthy menstrual cycle is typically a sign that your reproductive system is functioning well. While minor fluctuations are normal, consistently irregular periods can signal a deeper hormonal or health-related issue that shouldn’t be ignored.
What Is an Irregular Period?
A regular menstrual cycle typically occurs every 21 to 35 days and lasts 3 to 7 days. If your cycle is unpredictable, varies in length each month, or skips altogether, it may be considered irregular.
Signs of an Irregular Period Include:
Periods occurring less than 21 or more than 35 days apart
Missed periods for 2–3 months (without pregnancy)
Excessively heavy or light bleeding
Spotting between periods
Periods that last longer than 7 days
Painful cramps with no apparent cause
Common Causes of Irregular Periods
1. Hormonal Imbalances
Fluctuations in estrogen and progesterone levels can impact your cycle.
Conditions that cause this include:
Polycystic Ovary Syndrome (PCOS)
Thyroid disorders (hypo- or hyperthyroidism)
Perimenopause
2. Stress and Emotional Health
High stress levels can disrupt the hypothalamus — the brain center that regulates hormones, affecting ovulation and cycle timing.
3. Sudden Weight Changes
Extreme weight loss or gain can interfere with hormone production. Low body fat or obesity may delay or stop ovulation.
4. Over-Exercising
Athletes or those doing intense physical training may stop menstruating due to hormonal shifts and low energy availability.
5. Birth Control
Hormonal contraceptives may temporarily change your cycle. Some IUDs and injections can also stop periods altogether.
6. Chronic Conditions
Diabetes, celiac disease, and eating disorders like anorexia or bulimia can interfere with hormone balance.
7. Medications
Certain medications (like antipsychotics, chemotherapy, or antidepressants) may disrupt your menstrual cycle.
When to Worry About Irregular Periods
Occasional changes aren’t usually a cause for concern, but seek medical attention if you notice:
No periods for 3 or more months (not due to pregnancy)
Bleeding between periods or after intercourse
Very heavy bleeding (changing pads every 1–2 hours)
Severe cramping or pelvic pain
Facial hair growth or acne (signs of PCOS)
Unexplained weight gain or fatigue
A consultation at a private hospital in New Delhi can help identify the root cause early.
Diagnosing the Cause of Irregular Periods
Your gynecologist will begin with:
Medical history and symptom discussion
Pelvic exam
Blood tests (to check thyroid, estrogen, prolactin, insulin, and androgen levels)
Ultrasound (to detect ovarian cysts, uterine fibroids, or endometrial thickness)
Endometrial biopsy (if needed in rare cases)
Accurate diagnosis is essential for a personalized treatment plan.
Treatment Options for Irregular Menstruation
1. Lifestyle Modifications
If stress, weight, or diet is contributing:
Manage stress through yoga, meditation, or therapy
Adopt a balanced diet rich in iron, vitamins, and healthy fats
Exercise moderately — avoid extremes
Maintain a healthy BMI
2. Hormonal Treatments
Birth control pills regulate cycles and reduce heavy bleeding
Progestin therapy can trigger a regular period in women with hormonal imbalance
Hormone replacement (in perimenopausal women) balances estrogen and progesterone levels
3. PCOS Management
Metformin (for insulin resistance)
Anti-androgens (to reduce acne and excess hair growth)
Ovulation-inducing medications (if pregnancy is desired)
4. Thyroid Disorder Treatment
Thyroid medications can stabilize hormone levels and restore a normal cycle.
5. Surgical Options
In cases of fibroids or structural abnormalities, minor surgical procedures like laparoscopy or hysteroscopy may be recommended.
Discuss these options with your doctor at the best gynecologist hospital in Delhi for a safe and effective care plan.
Can Irregular Periods Affect Fertility?
Yes — irregular ovulation can make it difficult to predict fertile days or even ovulate at all. However, with proper treatment, many women go on to conceive successfully.
Your doctor may suggest:
Ovulation tracking
Lifestyle adjustments
Fertility medications (like Clomiphene or Letrozole)
IUI or IVF, if necessary
Natural Remedies That May Help
While not a substitute for medical treatment, these may support cycle regulation:
Spearmint tea: Helps reduce testosterone in women with PCOS
Cinnamon: Supports insulin sensitivity and hormonal balance
Vitamin D and magnesium: May help regulate menstruation
Chasteberry (Vitex): Promotes progesterone balance
Always consult a doctor before starting supplements.
Final Thoughts
Irregular periods are your body’s way of signaling that something is off. Whether it’s due to stress, a hormonal imbalance, or a medical condition, timely care can help you restore a regular cycle and avoid long-term complications.
0 notes
Text
Just realized that I stayed on the pill for 8 years
So everyone that I befriended during my university years didn't met the "true" me at all
Started using it to "control" my endometriosis Stopped using it because I thought that this much time on only one type of pill wouldn't be good on the long term and I was right! I don't have diarrhea as frequently as when I was on the pill
Now I will try to control the symptoms with diet and exercise, since birth control doesn't do shit to treat the sickness just delays the inevitable while potentially fucking other parts of my body
And goddamnit I forgot how much blood it usually goes out
Also, I also have to take thyroid hormones bc I don't have mine anymore, and I found an article saying that some birth controls may interact negatively with the thyroid hormone. But there are not many articles talking about that? Why? Many people have Hypo or Hyperthyroidism and also have to take birth control. Why we don't have more research about that?
This is my rambling for tonight
0 notes
Text
Is Your Pet’s Energy a Sign of Thyroid Trouble? Recognizing Symptoms of Hypo and Hyperthyroidism
Many pet owners don’t realize their cat’s sudden weight loss or their dog’s constant fatigue could point to thyroid issues. If you’ve visited a Virginia Beach veterinary hospital recently, you may have heard about the rising cases of hypothyroidism and hyperthyroidism in pets.
These two conditions affect the thyroid gland but have opposite impacts.
Hypothyroidism, common in dogs, means the thyroid isn’t producing enough hormones. Symptoms can include dull coat, weight gain, cold intolerance, or general lethargy. It’s a sneaky condition that progresses slowly, which is why regular veterinary checkups are key to early detection.
Hyperthyroidism, on the other hand, is almost exclusively seen in cats, especially those over 10 years old. It occurs when the thyroid gland produces too much hormone, leading to hyperactivity, ravenous appetite, weight loss, and a scruffy coat. Left untreated, it can result in heart problems or high blood pressure.
A skilled veterinarian can identify these disorders through blood work and clinical evaluation. The team at a Virginia Beach veterinary hospital will likely recommend hormone replacement pills for hypothyroidism and options like methimazole or radioactive iodine for hyperthyroid cats.
In either case, consistency in treatment and routine monitoring are essential. Your pet may need lifelong medication or follow-up labs every few months to maintain balance.
Being aware of the signs helps you act quickly. Whether it’s a sluggish pup or a high-strung senior cat, don’t brush off those changes—thyroid disorders are manageable with the right care plan and professional guidance.
1 note
·
View note
Text
I’d like to offer up as an 11th:
Rosalyn Yalow (1921 - 2011 CE, America)
A medical physicist, National Medal of Science holder, and first American woman to win a Nobel prize for Physiology and Medicine (sixth woman ever to win a Nobel prize) for her co-creation of radioimmunoassay (RIA), which allows for detection of things like hormone levels in the blood, which were previously too hard to measure. This technique now allows us to diagnose hormone and endocrine disorders like diabetes, PCOS and hypo/hyperthyroidism. And thanks to RIA, her and her research partner/co-creator (Solomon Berson) were also able to prove that type 2 diabetes was caused by insulin resistance instead of a total lack of insulin. Thanks to her work, she’s sometimes referred to as the Mother of Endocrinology.
10 Jewish Women from History
Karima bat-Ammar, AKA al-Wuhsha the Broker (11th - 12th CE, Cairo)
One of the few people mentioned in the Cairo Geniza with enough information to form a clear picture about her life. She was briefly married, but soon divorced and formed her own successful business in investments and loaning money. Known as eccentric and untamed, she became important enough that, despite the male-dominated society of Cairo, both her daughter and her granddaughter cited their connection to her in their own legal documents.
Anna Hebrea (~ 1500s CE, Rome)
A beautician and cosmetician established in Rome, and one of the earliest businesswomen of her profession to be documented. She was successful and well known even outside of Rome, and had noble customers, such as countess Caterina Sforza.
Seble Wongel (? - 1567 CE, Ethiopia)
Born into a noble Jewish family from Beta Israel kingdom of Simien and a descendant of King Solomon, she was married to the emperor of Ethiopia in what was likely a major political alliance. An influential figure in the Ethiopian-Adal War, she conducted a prison exchange and brought home her son Menas, who would later become emperor in 1559.
Gracia Mendes Nasi (1510 - 1569 CE, All Across Europe)
Born in Lisbon, Portugal, to a family of Conversos from Spain, who fled to Portugal for religious freedom but ended up forcibly converted a few years later. When he husband died, he left part of his fortune to her. Over the years, she lived in many places, including Antwerp, Venice and Ferrara, and finally Istanbul, making a name for herself as a businesswoman and provider for Jewish communities. In 1579, she established her own printing business, and became the first woman printer and publisher in the Ottoman Empire. She ended up having influence over kings, dukes, and popes, which often allowed her to create escape networks for Jews fleeing persecution. She donated towards the building of synagogues and yeshivas, and ended up getting a lease from the sultan on the region of Tiberias, which she built into a new center for refugees and others who wished to settle there in what is considered one of the earliest attempts at a modern Zionist movement.
Asenath Barzani (1590 - 1670 CE, Kurdistan)
From the Barzani family, who were well known Kabbalists and rabbis in northern Kurdistan. Her father, a rabbi and leader of the Jewish community, taught her Torah to prepare her as his successor, since he had no sons. Her marriage was only allowed to go through once it was promised that she could spend her time as a Torah scholar. After her husband’s death, the leadership of his yeshiva passed to her. She became a well known Torah scholar and successfully ran the yeshiva for many years. She was well versed in Hebrew, Torah, Talmud, Midrash, and Kabbalah, and was also known as a poet. She became the focus of several Kurdish stories, including a story where she is able to summon angels and saves a synagogue form being burned down.
Shinah Solomon Etting (1744 - 1822, Baltimore)
Born to a merchant in New York City, she married at the age of fourteen and soon thereafter moved to York, Pennsylvania, where she had eight children. Together with her husband, she ran a small store in York. After her husband died in 1778, she moved to Baltimore and, using her inheritance, purchased a small boarding house. The boarding house would later become successful enough that she was able to assist two of her sons in busines ventures, and become a stockholder in Union Bank. She had her portrait painted three times: twice by Charles Peale Polk, and once by John Wesley Jarvis.
Eliza Davis (1817 - 1903 CE, London)
A Jewish woman born in Jamaica, she and her husband later moved to London after her husband bought Charles Dickens’ home. In 1863, she wrote to Dickens in protest over the portrayal of Fagin in Oliver Twist, and absurd number of times that he is referred to as “the Jew.” Although initially defensive, Dickens soon stopped the printing of Oliver Twist and changed parts of the text. In addition to Dickens, she was said to have had correspondence with several other notable individuals, including the Private Secretary to Queen Victoria.
Sabat Islambouli (1867 - 1941 CE, Syria)
Born into a Kurdish Jewish family, she studied at the Women’s Medical College of Pennsylvania in the United States, and, after graduating with a medical degree in 1890, became one of the first Kurdish women physicians from Syria. After she graduated, she returned to Damascus, and later moved to Cairo in 1919.
Jerusha Jhirad (1891 - 1984 CE, India)
An Indian physician from the Bene Israel Jewish community of India. After graduating from Grant Medical College in Bombay in 1912, she became the first women to be given a scholarship by the Indian government to study abroad. She attended school and later worked in London, specializing in obstetrics and gynaecology. From 1920 to 1924, she was a leading medical officer at a maternity hospital in Bangalore, and from 1929 to 1947 was a leading officer at a hospital for women and children in Mumbai. She was a founding member of the Bombay Obstetric and Gynaecological Society and president of the Federation of Obstetric and Gynaecological Societies of India, and for ten years was the president of the Association of Medical Women in India. She was a supporter of sex education. In 1950, she presided at the sixth All India Obstetric and Gynaecological Congress in Madras. In addition to her medical accomplishments, she also founded a congregation among the Bene Israel community with her sister in 1925.
Polina Gelman (1919 - 2005 CE, Soviet Union)
A flight navigator in the women’s 46th Guards Night Bomber Aviation Regiment in World War II, she was awarded the title Hero of the Soviet Union in 1946. After the war, she continued her career as a military officer, and graduated from the Military Institute of Foreign Languages in 1951. At some point in her career, she served as an advisor and translator to Cuba. She finally settled in Moscow in 1957, where she taught political economy in college until 1990.
#jewish women#judaism#women's history#reblog comment#fun fact I’m actually related to her.#and not like distantly related either.
231 notes
·
View notes
Text
The Essential Preconception Guide: What to Do Before You Get Pregnant
Preconception care is a vital yet often overlooked component of reproductive health. Evidence shows that addressing health and lifestyle factors before conception can significantly improve pregnancy outcomes for both mother and baby.
This data-driven guide outlines key preconception strategies, supported by research and clinical recommendations from global health organizations.
1. Schedule a Preconception Health Visit
According to the CDC, only 14% of women receive preconception counseling despite its proven benefits in reducing adverse pregnancy outcomes.
At your preconception appointment, your provider may:
Review personal and family history for genetic risks
Screen for infectious diseases (e.g., rubella, varicella, STIs)
Assess immunization status
Manage chronic conditions such as diabetes or hypertension
Source: CDC, Preconception Health and Health Care, 2022
2. Folic Acid Supplementation: A Proven Preventive
Folic acid supplementation reduces the risk of neural tube defects (NTDs) by up to 70% when taken before conception and during early pregnancy.
Recommended dosage: 400–800 mcg/day
Start at least 1 month before conception
Higher doses (e.g., 4 mg/day) may be required for women with a previous NTD-affected pregnancy
Source: U.S. Preventive Services Task Force (USPSTF), 2017
3. Nutritional Status and Micronutrient Support
Micronutrient deficiencies are linked to complications such as low birth weight, preeclampsia, and preterm birth.
Key nutrients and deficiency rates:
Iron: ~38% of reproductive-aged women globally are iron-deficient
Vitamin D: Up to 41.6% of U.S. adults are deficient
Iodine: Essential for fetal brain development—moderate deficiency affects ~2 billion people worldwide
Folic Acid: As above, critical for early neural development
Testing and individualized supplementation are recommended based on dietary intake and lab markers.
Sources: WHO, NHANES, Lancet Global Health
4. Lifestyle Modifications and Risk Reduction
Modifiable behaviors have a strong impact on fertility and fetal health.
Smoking: Increases risk of infertility by 60% and miscarriage by up to 23%
Alcohol: Even low to moderate intake can affect fetal brain development; zero alcohol is safest
Caffeine: Doses above 200 mg/day linked to increased miscarriage risk
Physical Activity: At least 150 minutes/week of moderate activity recommended for most women
Sources: ACOG, British Medical Journal (BMJ), March of Dimes
5. Chronic Condition Management
Poorly controlled chronic diseases are associated with higher risks of stillbirth, congenital anomalies, and maternal complications.
Examples:
Diabetes: Increases congenital malformation risk by 4–10 times if uncontrolled during early pregnancy
Hypertension: Linked to preeclampsia and intrauterine growth restriction
Thyroid disorders: Both hypo- and hyperthyroidism can impair fertility and fetal development
Source: American Diabetes Association, Endocrine Society, WHO
6. Healthy Weight and Fertility Outcomes
BMI is directly associated with fertility and pregnancy outcomes.
Underweight (BMI <18.5): May lead to anovulation and low birth weight
Overweight (BMI 25–29.9): Higher risk of gestational diabetes, cesarean delivery
Obesity (BMI ≥30): Linked to miscarriage, congenital anomalies, and stillbirth
Even a 5–10% weight reduction in overweight individuals can restore ovulation and improve fertility.
Source: American Society for Reproductive Medicine (ASRM)
7. Fertility Awareness and Timing
Accurate cycle tracking can improve time-to-pregnancy outcomes.
Ovulation typically occurs 14 days before the start of the next period
Fertile window: ~5 days before ovulation + day of ovulation
Use of ovulation predictor kits (OPKs) or basal body temperature tracking can enhance precision
Couples are encouraged to seek fertility evaluation if conception does not occur within:
12 months of trying (if <35 years old)
6 months (if ≥35 years)
Sources: NIH, Fertility and Sterility Journal
8. Mental Health and Pregnancy Readiness
Mental health conditions such as depression and anxiety affect up to 15–20% of women of reproductive age.
Untreated perinatal depression increases the risk of poor birth outcomes
Certain psychiatric medications may need adjustment prior to conception
Cognitive-behavioral therapy (CBT) and mindfulness-based therapies show strong efficacy for mood support during the periconceptional period
Source: Journal of Affective Disorders, APA
9. Social Support and Partner Involvement
Social support during the preconception and pregnancy phases is linked to:
Lower maternal stress and anxiety
Increased prenatal care compliance
Improved birth satisfaction and postpartum wellbeing
Couples who engage in preconception care together report higher levels of relationship satisfaction and shared decision-making.
Source: Journal of Obstetric, Gynecologic & Neonatal Nursing (JOGNN)
10. Financial and Healthcare Planning
Lack of access to care is a major barrier to healthy pregnancy outcomes.
In the U.S., average out-of-pocket costs for prenatal care and delivery: $2,000–$4,500 with insurance
Uninsured individuals face significantly higher costs and limited access to early prenatal care
Preconception care can be an opportunity to:
Enroll in insurance or Medicaid programs
Identify preferred hospitals and birth centers
Understand maternity leave and parental benefits
Source: Health Affairs, Kaiser Family Foundation (KFF)
Conclusion
The data is clear: intentional, evidence-based preconception care significantly enhances pregnancy outcomes. By addressing health risks and optimizing well-being before conception, individuals and couples can create the foundation for a safer pregnancy and a healthier baby.
Disclaimer: This content is intended for informational purposes only and does not constitute medical advice. Please consult your healthcare provider for individualized recommendations.
0 notes
Text
have been inspired by this so i want to add on to this: Hyperthyroidism and T1D often go hand in hand (read this link!). If you have a character with Hyperthyroidism, consider giving a close relative T1D! Disabilities, especially ones that are autoimmune, do not happen randomly. Almost always, there is some hereditary factor involved, and often, when a person has one autoimmune disease, it puts them at risk for others developing.
Another thing I want to mention: if you intend putting characters through huge amounts of stress, and they have a relative with an autoimmune disease or have a preexisting condition, consider making them begin to present common symptoms of autoimmune disorders (Common symptoms include: fruity breath, muscle cramps, rapid weight loss, rapid weight gain, extreme hunger, loss of appetite, hair loss, muscle weakness, aggravation of other preexisting conditions, etc.). Huge amounts of stress can cause the onset or acceleration of autoimmune conditions. For example, I am T1D! After a close family member passed, I was put through immense levels of distress, which accelerated the onset of my Hidradenitis Suppurativa. Both of these conditions are autoimmune and consist of the immune system attacking itself, so be sure to keep that in mind when giving characters autoimmune disorders. Sometimes the body attacks itself and other times it doesn't work properly in other ways. Giving a character two kinds of autoimmune conditions with different causes can sometimes be dicey. It's not impossible, but dicey.
Also, just a general pet peeve: when you're writing a T1D character, please note the differences between T1D and T2D. Yes, they are similar, but some extra tips:
T1D patients often use different materials (CGM's, insulin pumps, pens) than T2D patients. T1D's typically use CGM's known as Dexcom, while T2D's use Freestyle Libre or Medtronic. This isn't to say that T1D's don't use other types or that T2D's don't use Dexcom, it is simply that the two groups are geared towards materials better suited for their needs. Similar case for insulin pumps, except Omnipod is geared towards children while t:Slim is geared towards teenagers and adults.
Lows and highs can happen for both. However, some are more prone to hypoglycemia (low), while others are prone to hyperglycemia (high). Generally, T2D's are more prone to hyperglycemia (as hypo would usually happen by taking too much medication), while it varies more for T1D's.
Regardless of T1 or T2, all diabetics that take insulin have a certain sugar to insulin ratio. Some people need more insulin than others. For me, my ratio is much higher than others, so I require more insulin. However, there are people who hardly require much at all! Ex: a 3:1 carb-insulin ratio means for every 3 carbs, you need one unit of insulin. (One unit of insulin = 1/100 mL of insulin; 1mL insulin = 100 units insulin)
T2D has a different cause than T1D. T1D can have it's onset accelerated, but it's typically predetermined from the moment you're conceived (basically, you're doomed). T2D is a little different in the sense that it can be caused by being overweight, low exercise, and high fat intake PAIRED with other factors. It's not always caused like this, but it's severity can almost always be significantly reduced via exercise, weight loss, and proper dieting. The same cannot be said for T1D's. For T1D's, it's typically lifelong.
forgot to add this but WE CAN EAT WHATEVER WE WANT!!!! Candy is not off limits, and neither are sugary foods or drinks so long as we take the correct amount of insulin for it. (Another reason why it's imperative that you do NOT give a T1D sugar or insulin they didn't ask for. Both risk bad outcomes.)
If I think of anything else I'll add on later probably!!!
Disabilities that You Should Consider Representing in Your Writing More… part 1
[large text: Disabilities that You Should Consider Representing in Your Writing More… part 1]
While all disabilities are underrepresented in basically all sorts of media, it’s hard to not notice the trend in what disabilities make up the majority of representation. It’s especially visible when having a blog like this, where we can see what disabilities writers even consider including in their writing, and which ones never come up.
One in four people are disabled. With eight billion people alive it means there’s a lot of disabled people, and a lot of reasons why they are disabled in the first place - but this diversity is rarely represented, even on this blog, and anyone who has been following for a while has probably noticed that fact.
To be blunt: there are disabilities other than “amputee” and “(otherwise invisibly disabled) mobility aid user”. Does that mean that it’s wrong to write either of those? Of course not, and we don’t want to imply that it is. Does it mean that when you are deciding on what to give your character, you should think beyond just those two? Absolutely. Disability is a spectrum with thousands of things in it - don’t limit yourself for no reason and embrace the diversity that’s built into it instead.
This is, simply, a list of common disabilities. This is just a few of them, as this is part one of presumably many (or, at least three as of right now). By “common” we rather arbitrarily decided on “~1% or more” - so at least 1 in 100 people has the disabilities below, which is a lot. Featuring!: links that you should click, sources of the % that are mostly just medical reports and might be hard to read, and quick, very non-exhaustive explanations to give you a basic idea of what these are.
Intellectual disability (about 1.5%) Intellectual disability is a condition we have written about at length before. It’s a developmental disability that affects things such as conceptualization, language, problem-solving, or social and self-care skills. ID can exist on its own or be a part of another condition, like Down Syndrome, Congenital Iodine Deficiency, or Fetal Alcohol Spectrum Disorders. This post covers a lot of basic information that you might need. We have an intellectual disability tag that you can look through!
Cancer survivors (5.4% in the US, about 0.55% worldwide) A cancer survivor is a pretty self-explanatory term. There is a lot of types of cancer and some of them are very common while others are very rare, which makes this a very diverse category. Cancers also have different survival rates. While not every survivor will have disabling symptoms, they definitely happen. Most of the long-term side effects are related to chemotherapy, radiation, and other medication, especially if they happened in children. They can include all sorts of organ damage, osteoporosis, cognitive problems, sensory disabilities, infertility, and increased rate of other cancers. Other effects include removal of the affected area, such as an eye, a spleen, breasts, or the thyroid gland, each of which will have different outcomes. Cancer, and cancer treatments, can also result in PTSD.
Diabetes (about 8.5%, ~95% of that are type 2) Diabetes is a group of endocrine conditions that cause hyperglycemia (high blood sugar) for various reasons depending on the type. The vast majority of people have type 2 diabetes, which can cause fatigue, poor healing, or feeling thirsty or hungry. A diabetic person will use insulin when needed to help manage their blood sugar levels. There are many complications related to diabetes, from neuropathy, to retinopathy, and chronic kidney disease, and there's a lot of disabilities that coexist with diabetes in general! You might want to check out the #how to write type 1 diabetes tag by @type1diabetesinfandom!
Disabling vision loss (about 7.5%) Blindness and low vision are a spectrum, ranging from total blindness (around 10% of legally blind people) to mild visual impairment. Blindness can be caused by countless things, but cataracts, refractive errors, and glaucoma are the most common. While cataracts cause the person to have a clouded pupil (not the whole eye!) blind eyes usually look average, with strabismus or nystagmus being exceptions to that fairly often (but not always). Trauma isn't a common cause of blindness, and accidents are overrepresented in fiction. A blind person can use a white cane, a guide dog or horse, or both. Assistive solutions are important here, such as Braille, screenreaders, or magnifying glasses. We have a blindness tag that you can look through, and you might want to check out @blindbeta and @mimzy-writing-online.
Psoriasis (about 2-4%) Psoriasis is a chronic skin condition with multiple subtypes; it can cause intense itching, pain, and general discomfort, and often carries social stigma. It’s an autoimmune and non-contagious disability that affects the skin cells, resulting in raised patches of flaky skin covered with scales. It often (30%) leads to a related condition, psoriatic arthritis, which causes joint pain, tenderness, and fatigue, among other things.
Stroke survivors (0.5-1%) A stroke survivor is a person who has survived any kind of stroke (ischemic, hemorrhagic, etc.). While the specific symptoms often depend on the exact location on where the stroke happened, signs such as hemiplegia, slurred speech, vision problems, and cognitive changes are common in most survivors to some degree. When someone has a stroke as a baby, or before they are born, it can result in cerebral palsy, epilepsy, and other disabilities. We have a brain injury tag that you can look through!
Noonan Syndrome (about 0.1-1% - mild is 1%, severe 0.1%) Noonan Syndrome is a disability that is almost never mentioned in any context, but certainly not around the topic of writing disabled characters. It’s a congenital condition that can cause cardiomyopathy, chronic joint pain, hypermobility, short stature, facial differences such as ptosis, autism, and various lymphatic problems among other things. Some people with Noonan Syndrome might use mobility aids to help with their joint pain.
Hyperthyroidism (about 1.2%) Hyperthyroidism is a condition of the endocrine system caused by hormone overproduction that affects metabolism. It often results in irritability, weight loss, heat intolerance, tremors, mood swings, or insomnia. Undertreated hyperthyroidism has a rare, but extremely dangerous side effect associated with it called a thyroid storm, which can be fatal if untreated.
Hypothyroidism (>5%) Hypothyroidism is an endocrine condition just as hyperthyroidism is, and it causes somewhat opposite symptoms. Due to not producing enough thyroid hormones, it often causes fatigue, depression, hair loss, weight gain, and a frequent feeling of being cold. It’s often comorbid with other autoimmune disabilities, e.g. vitiligo, chronic autoimmune gastritis, and rheumatoid arthritis. Extreme hypothyroidism can also be potentially fatal because of a condition known as Myxedema coma (or “crisis”), which is also rare.
Deafblindness (about 0.2-2%) Being DeafBlind is often considered to be an extremely rare disability, but that’s not really the case. DeafBlindness on its own isn’t a diagnosis - it can be caused by a wide range of things, with CHARGE syndrome (congenital), Usher syndrome (born deaf, becomes blind later in life), congenital rubella, and age-related deafness and blindness being some of the most common reasons. DeafBlindness is a wide spectrum, the vast majority of DeafBlind people aren’t fully blind and deaf, and they can use various ways of communication. Some of these could be sign language (tactile or not), protactile, the deafblind manual, oral speech (aided by hearing aids or not), the Lorm alphabet, and more. You can learn more about assistive devices here! Despite what various media like to tell you, being DeafBlind isn’t a death sentence, and the DeafBlind community and culture are alive and thriving - especially since the start of the protactile movement. We have a DeafBlindness tag that you can look through!
It’s probably worth mentioning that we have received little to no asks in general for almost all the disabilities above, and it’s certainly not due to what mods answer for - majority of our inbox is amputee-related, and we haven’t had mods that answer those for somewhere around four years now. Our best guess is that writers don’t realize how many options they have and just end up going for the same things over and over.
Only representing “cool” disabilities that are “not too much while having a particular look/aura/drama associated” isn’t what you should aim for. Disabled people just exist, and all of us deserve to be represented, including those whose disabilities aren’t your typical “cool design” or “character inspo”. Sometimes we are just regular people, with disabilities that are “boring” or “too much”, and don’t make for useful plot points.
mod Sasza (with huge thank yous to mod Sparrow, Rot, and Virus for their contributions with research and data!)
2K notes
·
View notes