#multisystem inflammatory syndrome
Text
The Weather
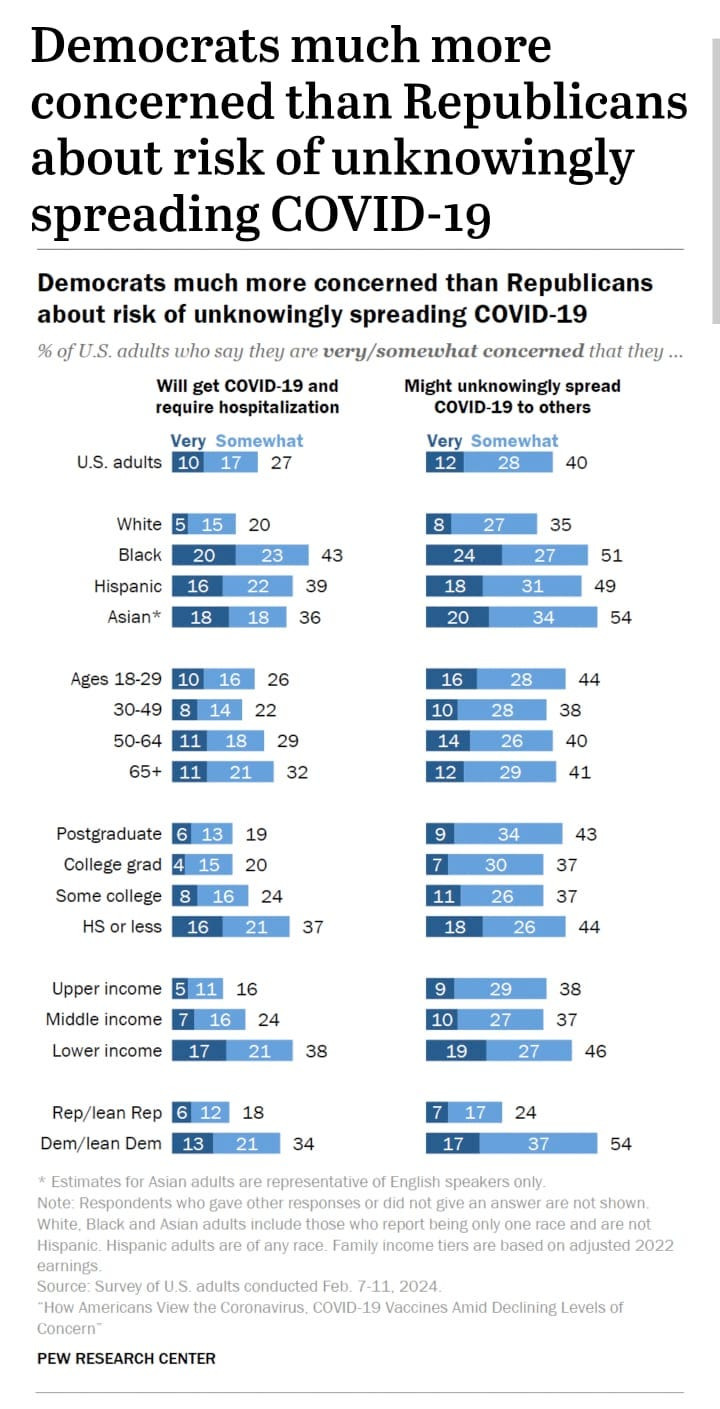
Amid the CDC’s COVID-minimizing and dangerous rollback to isolation guidance, a new Pew Research poll shows that 27% of Americans are very or somewhat concerned that they will get COVID and require hospitalization, and 40% (nearly half) of Americans are very or somewhat concerned that they will unwittingly spread COVID to others. This number rises substantially for low income brackets, and Black, Hispanic, and Asian adults. Concern about hospitalization was highest in adults with a high school education or less. Despite efforts by the CDC, the Biden Administration, and corporate media to downplay the public’s concern about COVID, these numbers show that a substantial proportion of Americans care about protecting one another.
A popular program providing free rapid antigen tests through the USPS ended on March 9, 2024. Despite the limitations of rapid antigen tests, these home tests continue to be a vital way to quickly identify COVID cases, both to prevent further onward spread as well as to identify the need for treatment with Paxlovid. You can use our letter campaign to let your elected officials know we still need free rapid home tests.
COVID wastewater levels are decreasing, with no states registering “Very High” levels as of 3/15/2024. Eight states are currently at “High” and 15 are at “Moderate” levels of SARS-CoV-2 detected in wastewater.

Wastewater levels show a downward trend in the provisional data (gray shaded area) in all regions. The national wastewater levels are overall indicated as “Low.” Lower wastewater activity is an indication of lower overall viral spread, which is certainly a good thing. However, the “Low” designation is not a representation of low risk in our day-to-day lives, and continued masking and multilayered precautions continue to be necessary to protect ourselves and our communities. State and local trends can also provide additional information, where available.

A recent Axios article highlights the expanding broad utility of wastewater testing for COVID and other infectious diseases, as well as the uncertain footing of the funding and infrastructure for this essential surveillance tool. We encourage you to write your elected officials to let them know you want to keep and expand wastewater testing in your area and nationally.
Wins
On March 13, the People’s CDC hosted a press conference to push back on the CDC’s elimination of COVID isolation guidance and demand accountability to the public (watch the video or read the press release). The online publication (pre-proof) of the People’s CDC External Review in the peer-reviewed scientific journal American Journal of Preventive Medicine Focus was also announced, which is an important authoritative resource highlighting both shortcomings of the CDC’s approach and recommendations for a more transparent, effective, and equitable pandemic response going forward. The full External Review report can be found on the People’s CDC website.
March 15 was Long COVID Awareness Day, and Senator Bernie Sanders along with six cosponsors (Tim Kaine, Edward Markey, John Hickenlooper, Tina Smith, Robert Casey, and Tammy Baldwin) introduced Resolution 590 to formally recognize March 15 as Long COVID Awareness Day. You can ask your senators to support this resolution using this letter campaign. Senator Sanders released a video promising legislation to increase funding for Long COVID research and clinical care, as well as emphasizing the importance of prevention, including vaccination and masking. For more info on Long COVID Awareness Day, see the “Long COVID” section below.
When we make our voices heard, whether with the press, with scientific publications, or with elected officials, we win.
Variants
In the CDC’s most recent Nowcast predictions, JN.1 continues to be the most prevalent variant in the United States (86.5%), with a predicted decrease in JN.1 and sublineage JN.1.13 increasing (9.5%).

Vaccines
The CDC has recommended spring boosters for people age 65 and older, at least 4 months after the previous updated dose. As of 3/2/2024, only about 42.4% of adults age 65 and older had gotten an updated vaccine, and many who were vaccinated in the fall may not realize they are eligible for another dose.
In addition to the spring boosters recommended for people aged 65 and older, immunocompromised people are eligible for more frequent vaccination. The CDC states, “You can self-attest to your moderately or severely immunocompromised status, which means you do not need any documentation of your status to receive COVID-19 vaccines you might be eligible to receive.”
As a reminder, the currently available COVID vaccine formulations (2023-2024, first available in fall 2023) are effective against the JN.1 variant, with about 54% protection against symptomatic disease. For people of all ages, immunity wanes after 6 months, and, although current eligibility is more limited, we continue to support access to vaccination at least every 6 months for all ages.
If you have not received one of the updated COVID vaccines released last Fall, you can use this tool to find local vaccine providers that are Bridge Access Participants. The Bridge program is currently available through December 31, 2024.
COVID in Kids
In a recent report in the CDC’s MMWR publication, cases of Multisystem Inflammatory Syndrome in Children (MIS-C) in 2023 were highlighted. MIS-C is an inflammatory response to a COVID infection that usually occurs 2-6 weeks following an infection. MIS-C may be serious and can affect the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal tract. Although rates of MIS-C have slowed since 2020-2021, 112 cases were reported in 2023, with 82.1% of those occurring in unvaccinated children. Among cases in vaccinated children, 60% occurred in children who had not received a booster within the last year. As of 3/2/2024, only about 13.5% of eligible children aged 6 months to 17 years have received a 2023-2024 COVID vaccine. More info on Long COVID in kids is presented below under “Long COVID.”
It is clear that kids need protection from COVID, and current efforts are inadequate. We demand that public health authorities take action to protect our children. You can find more information to support protecting kids in our Urgency of Equity toolkit.
Long COVID
March 15 marked the second annual International Long Covid Awareness Day. Across the globe, Long Covid survivors, their allies, and the community fight for increased research, treatment, and visibility for people living with Long Covid.
Searching #LongCovidAwarenessDay on most social media platforms will connect you to posts from people all over the world describing their experience navigating their ongoing symptoms while trying to educate others about the barriers they face in seeking accessible and effective treatments.
Up to 5.8 million children in the US may be affected by Long COVID. A recent study published in the journal Pediatrics from the American Academy of Pediatrics shows that vaccination reduces the risk of Long COVID in children by about 40%.
Take Action
Super Tuesday has come and gone with nominees in most parties now established for races at the local, state, and national level later this year on November 5th.
People’s CDC wants to remind you that regardless of the outcomes of these elections, we must always continue to organize and fight back against the state’s abandonment of science in favor of corporate interests.
We urge you to use and share our letter campaign demanding that elected officials renew and expand programs to provide free Rapid Antigen Tests (RATs). You can also continue to urge elected officials to support maintaining and extending COVID isolation guidance via our letter campaign. Over 13,000 letters have already been sent, and you can use the same template to send follow up letters.
Whether it’s joining a local mutual aid organization or fighting for increased accessibility measures (required masking, improved air quality, and multilayered precautions) in groups you are already part of, your actions can make your communities safer for all people.
#op#covid#pcdc#covid19#covid-19#sars-cov-2#people's cdc#covid 19#coronavirus#covid pandemic#pandemic#coronavirus pandemic#covid isn't over#long covid#long covid awareness day#long covid awareness#mis-c#multisystem inflammatory syndrome#covid news#covid conscious#covid vaccine#medical news#medical#uspol#img#described in alt text
7 notes
·
View notes
Note
Hey sorry to bug you but I saw your post in the tag and you’re the only other person I’ve seen on this site with multisystem inflammatory syndrome. I’m having a hard time accessing medical treatment and was wondering if you know of any groups for people dealing with this ?
Hey, you're not a bother at all, questions relating to health are always welcome.
Unfortunately, I'm not entirely sure, mainly because I wouldn't know where to look for that kind of thing (I don't really seek out group support, sorry), but what might help is looking for people who are dealing with long covid and/or seeing doctors who are keeping up to date with long covid research. You'd be surprised of what kind of symptoms can pop up from long covid outside of MIS.
A lot of support also initially depends on where you live. I live in a developing country and there's still not very much research being done about the effects of covid because of other health crises happening in the country. So it all depends on where you live if there's local support for your symptoms. Aside from that, MIS can only really be mitigated (never cured) through diet, rest, and exercise, just like most other chronic conditions.
Anyways, thanks for reaching out. Stay safe and have a good one.
#exe gets an ask#MIS#Multisystem Inflammatory Syndrome#covid#long covid#covid is not over#Sorry I couldn't be of much help
1 note
·
View note
Text
VIDEO: 12 year old Maddie De Garay (Cincinnati, OH) was vaccine injured and permanently disabled less than 24hr after her 2nd Pfizer dose on Jan.20, 2021 (click here)
============================================================================
Fishers, IN - 10 year old girl Arianna developed CRPS (Complex Regional Pain Syndrome) within 24 hours of COVID-19 booster shot in Jan.2023 (click here)
Hong Kong - 11 year old girl Siu Yik-Tung developed myocarditis 3 weeks after 2nd Pfizer mRNA jab, spent a month in Children’s Hospital Intensive Care Unit, July 2022 (click here)(click here)
Her aunt said that Siu's organs have recovered and are functioning again, but the nerves for her legs will take more time to recover and she will be wheelchair-bound until her muscles gain strength again.
Thailand - 7 year old girl Pimpakarn Khotphakdi developed dark purple spots on her skin and began oozing blood from her eyes and skin 2 weeks after Pfizer COVID-19 mRNA vaccine, April 2022 (click here)
Bongara, Peru - 8 year old boy Richard Jeferson Bustamante Bautista got Stevens-Johnson Syndrome after 2nd Pfizer mRNA dose on Feb.21, 2022 (click here)
Sao Paolo, Brazil - 10 year old Luisa Petenuci suffered cardiac arrest 12 hours after her 1st Pfizer COVID-19 mRNA vaccine on Jan.18, 2022 (click here)
Minnesota - 6 year old boy Milo Edberg developed myocarditis after Pfizer COVID-19 vaccine on Dec.10, 2021. He remained intubated for a month and a half (click here)
Pennsylvania - 8 year old Harper Gewin had a stroke and brain hemorrhaging 7 days following Pfizer mRNA jab (Nov.2021) (click here)
Publications
Thailand - 12 year old girl developed “Toxic epidermal necrolysis” after 1st dose of Pfizer COVID-19 mRNA jab, published November 2021 (click here)
San Diego, CA - 12 year old boy developed “Eosinophilic cellulitis” one day after 2nd dose of Pfizer COVID-19 mRNA jab, Jan.2022 (click here)
Florida - 10 year old girl developed Acute disseminated encephalomyelitis with autoimmune brain lesions after 2nd Pfizer COVID-19 mRNA jab, July 2022 (click here)
China - 11 year old girl developed MIS-C after inactivated COVID-19 vaccine, Feb.2023 (click here)
Saudi Arabia - 12 year old boy developed multisystem inflammatory syndrome (MIS-C) following 2 doses of Moderna mRNA vaccine, March 2022 (click here)
South Korea - 12 year old boy developed acute kidney injury after 2nd dose of Pfizer COVID-19 mRNA vaccine, Jan.2022 (click here)
VAERS ID: 2187799 - 10 yo boy (New Jersey) (March 2022)
44 days after 1st dose of Pfizer, he starts having what has become an almost daily “episode” that would be described as a panic attack with hallucinations. He becomes very disoriented, stating that images appear and words sound very fast to him. After episode is over, he is able to articulate what he experienced. This is completely out of character for him, he is very social, good student and athlete.
VAERS ID: 2163473 - 8 yo girl (Virginia) (Feb 2022)
40 days after 1st Pfizer dose, girl changed mentally. Appears to have seizure but it’s not a seizure. She cannot respond during these episodes and began to see and hear things that aren’t there. Happens over and over, has 5 emergency visits.
A month later she is still undiagnosed and having memory loss, regression, delirium in waves. Unaware of age, year of birth, season, counting 1 to 10. Before 1st Pfizer dose, she had no neurological troubles, she was a straight A student who was bright and happy. She has lost memory and regressed. Woke up a different person who became unable to be touched or consoled. Permanently disabled.
VAERS ID: 2018697 - 9 yo boy (New Jersey) (Dec 2021)
One day after 1st Pfizer dose, he had a severe headache for 2 days. Could barely speak, not really talking and not really responding. Had hallucinations and Alice in Wonderland Syndrome. Everything looked small. Has not recovered.
VAERS ID: 2014388 - 8 year old girl (Illinois) developed vaginal bleeding 9 days after Pfizer on Dec.12, 2021
VAERS ID: 2002198 - 11 year old boy (California) - developed persistent tremors in arms and legs after 1st Pfizer mRNA jab (Dec.2021)
VAERS ID: 1976737 - 5 year old girl (Tennessee) 24 hr after 1st Pfizer mRNA jab developed seizures, behavior changes, motor tics (Dec.2021)
Australia TGA 698578 - 8 year old girl had pericarditis after Pfizer mRNA jab (Jan.21, 2022)
Australia TGA 697752 - 10 year old boy had myocarditis and pericarditis after Pfizer mRNA jab (Jan.20, 2022)
Australia TGA 697518 - 8 year old boy suffered swelling to: scrotum, face, lips, eyes, rash, chest pain (Jan. 20, 2022)
Australia TGA 755787 - 6 year old girl developed Pericarditis after Moderna vaccine (Oct.21, 2022)
Australia TGA 767774 - 5 year old girl developed vaginal hemorrhage after Pfizer vaccine (Feb.28, 2023)
My Take…
I hit the substack limit on how much I can fit into one article.
Every parent should have this information in their legal files.
These are COVID-19 vaccine side effects in children that should never have been given these toxic pharmaceutical products.
Not safe or effective.
69 notes
·
View notes
Text
BroadlyEpi Newsletter
Hello! This newsletter will have both last weeks content and some less recent articles as well (excluding archived MMWR Boosters as otherwise that’d be way too many links). I hope you’re all doing great!
MMWR Boosters (Current Edition):
MMWR Booster for: Outbreak Linked to Morel Mushroom Exposure — Montana, 2023, Weekly / March 14, 2024 / 73(10);219–224
MMWR Booster for: Notes from the Field: Surveillance for Multisystem Inflammatory Syndrome in Children — United States, 2023 , Weekly / March 14, 2024 / 73(10);225–228
MMWR Booster for: Surveillance of Waterborne Disease Outbreaks Associated with Drinking Water — United States, 2015–2020 , Surveillance Summaries / March 14, 2024 / 73(1);1–23
MMWR Booster for: Notes from the Field: Measles Outbreak — Cook County, Illinois, October–November 2023, Weekly / March 14, 2024 / 73(10);229–230
MMWR Booster for: Surveillance for Coccidioidomycosis, Histoplasmosis, and Blastomycosis During the COVID-19 Pandemic — United States, 2019–2021 / Weekly / March 21, 2024 / 73(11);239–244
MMWR Booster for: Tuberculosis Preventive Treatment Update — U.S. President’s Emergency Plan for AIDS Relief, 36 Countries, 2016–2023 / Weekly / March 21, 2024 / 73(11);233–238
MMWR Booster for: Notes from the Field: Expanded Laboratory Testing for Varicella — Minnesota, 2016–2023 / Weekly / March 21, 2024 / 73(11);245–246
Epi Explained, ThuRsday and PyFriday Tutorials:
Epi Explained: Understanding T-Tests, Relative Risk and SIR Models
ThuRsday Tutorial: How to Calculate T-Tests, Relative Risk and SIR Models in R
PyFriday Tutorial: How to Calculate T-Tests, Relative Risk, and SIR Models in Python
As a final general announcement, we’re happy to report that BroadlyEpi is now a major sponsor of the Twin Strangers Production network of Audio Drama Podcasts. If you haven’t checked out any of their great work, you absolutely should.
2 notes
·
View notes
Text
Reviewing questions:
Blindness is a potentially devastating complication of sarcoidosis. Ocular sarcoid can develop in up to half of all cases and most commonly presents as anterior uveitis or keratoconjunctivitis. The most serious complication is optic neuritis.
A complete ophthalmologic examination at the time of diagnosis is recommended, as asymptomatic disease can result in permanent visual impairment. All patients with sarcoidosis should have a careful history and physical examination to identify other organ involvement before having further testing, including ECG, pulmonary-function testing, and baseline laboratory studies (calcium level, alkaline-phosphatase level, renal-function, and hepatic-function tests) to evaluate the extent of disease.
McConnell's sign is defined as right ventricular free wall akinesis with sparing of the apex. Typically this looks as if the apex of the RV is a trampoline. Echocardiogram shows right ventricular strain and a positive McConnell sign, which is indicative of pulmonary embolism (PE).
All patients who have known or suspected bronchiectasis and who are acutely ill with suspected lower respiratory tract infection should be empirically treated with an antipseudomonal antibiotic, such as cefepime until culture results are available to guide treatment decisions.
Heerfordt’s syndrome (uveoparotid fever) is another collection of clinical findings specific enough to diagnose sarcoidosis without a biopsy. These signs and symptoms include uveitis, parotid gland enlargement, and facial nerve palsy.
Lofgren’s syndrome is a form of acute sarcoidosis. Sarcoidosis is a multisystem disease characterized by the presence of noncaseating granulomas and although classically described in African Americans, it has one of its highest prevalences in the northern European population. Clinical variants exist with certain forms having diagnostic and prognostic value. Lofgren’s syndrome is the combination of erythema nodosum, bilateral hilar adenopathy, migratory polyarthralgias, and fever. This pattern is so consistent that it has 95% diagnostic specificity and allows diagnosis of sarcoidosis without a biopsy. Among European patients, the presence of Lofgren’s syndrome portends to a good prognosis. For mild disease symptomatic treatment with non-steroidal anti-inflammatory agents is reasonable or low dose prednisone may be added.
The optimal management of laryngotracheitis (croup) is determined by the severity of disease. There are numerous scoring systems for croup severity, with the Westley croup score being the most validated and most often used. The Westley croup severity scale includes evaluation for the presence of stridor at rest, retractions, and cyanosis as well as assessment of mental status and air entrance. Regardless of any official scoring system, most physicians would consider the presence of retractions and stridor at rest to be indications of moderate to severe disease that requires evaluation in the emergency department. The presence of cyanosis, confusion, depressed mentation, agitation, severe retractions, or absent breath sounds would indicate severe disease and/or the possibility of impending respiratory failure.
Mild cases of croup are treated on an outpatient basis with cool mist therapy and fluid replacement. Moderate cases may require supplemental oxygen, oral or intramuscular corticosteroids, or racemic epinephrine. Severe cases are best treated with hospitalization and racemic epinephrine.
Bottom Line: The most important step in initial management of laryngotracheitis includes nebulized epinephrine (racemic or L-epinephrine) and dexamethasone along with humidified oxygen, fever reduction, and hydration. Epinephrine acts almost immediately, while steroids have a delayed onset of action.
Pneumothorax is defined as a collection of air in the pleural space. The result is pleural separation of the visceral and parietal pleura. Spontaneous pneumothorax lacks an antecedent event (e.g. trauma). There are two types: primary and secondary. Primary spontaneous pneumothorax (PSP) occurs in patients without recognizable underlying lung disease. Secondary spontaneous pneumothorax (SSP) occurs in patients with visible underlying lung disease (e.g. COPD). The most common etiology of PSP is rupture of a subpleural bleb (which are usually not seen on imaging and are undiagnosed). Many cases initially diagnosed as PSP may eventually be diagnosed as SSP after further workup.
Management depends on the size of the pneumothorax. The spectrum of management includes watchful waiting, aspiration, chest tube insertion, and thoracoscopy with pleurodesis or lung resection.
Rhinosinusitis can be defined as either viral/bacterial and if bacterial, as complicated/uncomplicated. Complicated rhinosinusitis implies the extension of disease outside the nasal cavity/sinuses into adjacent structures, such as soft tissues, ophthalmologic tissues, and nervous system.
Current criteria for the presumptive (many of these cases may still be viral) diagnosis of acute bacterial rhinosinusitis (ABRS) include persistent symptoms lasting more than 10 days without any evidence of clinical improvement or a biphasic illness pattern which is also called double worsening, meaning the patient was sick, improved, and then became sicker a second time within a short time frame, usually within a 10 day period. The IDSA guidelines from 2012 also recommend the use of a high fever greater than 39C associated with severe symptoms for 3-4 days as being more consistent with bacterial rhinosinusitis. According to the guidelines by the American Academy of Otolaryngology-Head and Neck Surgery published in 2015, fever itself early in the course of illness is not sensitive or specific enough to warrant treatment based on this vital sign alone, and they do not recommend using this as criteria for the diagnosis of ABRS. They agree with the other criteria used by the IDSA and acknowledge that a "severe" presentation may warrant the use of antibiotics as recommended by the IDSA and the American Academy of Pediatrics which considers more than 3 days of high fever and purulent nasal discharge as a severe presentation of ABRS in children.
Summary Criteria for the Diagnosis of ABRS
Signs or symptoms of acute rhinosinusitis present for 10 days or more after symptom onset with no improvement
Acute worsening of improving rhinosinusitis within 4-6 days of symptom onset or "double-sickening."
Severe rhinosinusitis: onset of high fever greater than 39C and severe symptoms within 3-4 days of onset
Tx of ABRS: amoxicillin, amoxicillin-clavulanate, doxycycline if PCN allergic, or respiratory fluoroquinolone in kids who can't take doxycycline. I just had a pt in clinic who had bacterial rhinosinusitis and I gave him amoxicillin-clavulanate.
Bottom Line: In patients with ABRS who require antibiotic therapy, the initial therapy of choice is with amoxicillin with or without clavulanate.
One of the feared complications of acute bacterial rhinosinusitis (ABRS) is orbital cellulitis. This infection commonly develops in the setting of ABRS due to the direct extension of bacteria from the sinus cavity into the orbit. Commonly it can project through the roof of the maxillary sinus. Additionally, there can be extension through the adjacent soft tissues. The diagnosis of this condition is clinical and is confirmed with radiographic imaging (CT scan of the sinuses). The presence of pain/difficulty with eye movement, double vision, eye swelling, and erythema should be concerning for orbital infection. The initial imaging test of choice would be with a contrasted CT study of the face and orbits. An MRI could also be performed and has similar accuracy, but is generally slower and more expensive to obtain. Additionally, patients with suspected orbital cellulitis should be evaluated by ophthalmology in the emergency department and started on IV antibiotics with coverage for MRSA (vancomycin generally).
If the sinuses are the suspected source, ampicillin-sulbactam or piperacillin-tazobactam can be added to vancomycin as long as there is no concern for CNS involvement. If the CNS is involved, it should be noted that both ampicillin-sulbactam and piperacillin-tazobactam have relatively poor CNS penetration, and a 3rd generation cephalosporin (ceftriaxone) should be used with the addition of metronidazole for coverage of anaerobic organisms. General guidelines for sepsis and infection should be followed with the physician obtaining the regular laboratories including a complete blood count, metabolic profile, blood cultures, and lactate.
Symptoms of Complicated ABRS:
Proptosis or impaired extraocular movements
Painful eye movements
Diplopia or impaired vision
Periorbital edema or erythema
Cranial nerve palsies
Altered mental status
Neck stiffness/meningeal signs
Papilledema
Complications of ABRS:
Meningitis
Orbital cellulitis
Cavernous sinus thrombosis/thrombophlebitis
Preseptal cellulitis
Ruptured eardrum:
Tympanic membrane perforations are commonly caused by trauma or acute otitis media and are usually noted on otoscopic examination. Perforations with marked hearing loss or other concerning neurologic signs such as nystagmus, ataxia, or vomiting should receive a prompt evaluation by an otolaryngologist. Supportive care only is a perfectly reasonable treatment plan for patients with simple perforations with minimal hearing loss and no neurologic signs. Many perforations will heal spontaneously within 4 weeks and require no intervention.
#sarcoidosis#McConnell#Heerfordts syndrome#Lofgrens syndrome#Lofgren#croup#PTX#sinusitis#rhinosinusitis#ruptured ear drum
3 notes
·
View notes
Video
youtube
EP.11 ติดโควิด โอไมครอนดีกว่าฉีดวัคซีน จริงหรือเปล่า?
EP.11 โควิดสายพันธุ์โอไมครอน มีอาการไม่รุนแรง น่าจะเป็นจุดจบของการระบาดโควิดสักที
มีการแนะนำให้ประชาชนทั่วไป สามารถติดโควิดสายพันธุ์โอไมครอน เพื่อให้เกิดภูมิคุ้มกันแบบหมู่ เพื่อให้การระบาดของโควิดสิ้นสุด ทุกคนมีภูมิคุ้มกัน ข้อมูลเหล่านี้ต้องระวัง ถึงแม้ว่า โควิดสายพันธุ์โอไมครอนจะมีอาการไม่รุนแรง แต่การติดโควิด อาจเกิดภาวะแทรกซ้อนจากการติดได้ เช่น อาการรุนแรง การติดเชื้อซ้ำซ้อน การหายใจล้มเหลว ไตวาย ต้องฟอกเลือดล้างไต หรือเอาสานอักเสบออก และเกิดภาวะลิ่มเลือดอุดตันได้ ทำให้การรักษายากมากขึ้น
นอกจากนั้น ยังสามารถเกิดอาการตามหลังโควิดได้ เช่น Long COVID syndrome หรือ Multisystem inflammatory syndrome in adult (MIS-A) or MIS-C ส่งผลให้ผู้ป่วยมีคุณภาพชีวิตที่แย่ลง
การติดโควิด เราไม่สามารถพยากรณ์ได้เลยว่า ภาวะแทรกซ้อนจะเกิดขึ้นเมื่อไหร่ และสามารถเกิดได้กับทุกกลุ่มอาการ ตั้งแต่ อาการน้อย ปานกลาง และรุนแรง ซึ่งข้อมูลปัจจุบัน การฉีดวัคซีน มีข้อดี และได้ประโยชน์กว่าการได้รับการติดโควิดสายพันธ์โอไมครอน
KS clinic หมอกิตติศักดิ์ - หมอสีชมพู หมอรักษาปอด หมอรักษาตา อุดรธานี
นพ.กิตติศักดิ์ อาจารย์แพทย์ประจำโรงพยาบาลศูนย์อุดรธานี
คลินิกแพทย์เฉพาะทาง อายุรศาสตร์ระบบทางเดินหายใจ และภาวะวิกฤตระบบหายใจ ประจำโรงพยาบาลศูนย์อุดรธานี
รักษาโรคทางอายุรกรรมระบบทางเดินหายใจ เช่น หอบหืด ถุงลมโป่งพอง ไข้หวัด ไอ หอบเหนื่อย เอกซเรย์ปอดผิดปกติ ก้อนในปอด ส่องกล้องปอด นอยกรน ฉีดวัคซีน ภูมิแพ้ และ โรคทั่วไป (เบาหวาน ความดันโลหิตสูง ปวดข้อ ฯลฯ)
โดยเเพทย์ผู้มีประสบการณ์
ปลอดภัยได้มาตราฐาน
สอบถาม • นัดคิว • ปรึกษา•
KS clinic หมอกิตติศักดิ์ - หมอสีชมพู หมอรักษาปอด หมอรักษาตา อุดรธานี
โทรสอบถาม 0926-361-362
LineID: @ksclinic.udon (มี @ ด้วยนะคะ)
ติดตามเราได้ที่
เฟชบุ๊ค: https://www.facebook.com/ksclinic.udon/
https://www.tumblr.com/blog/ksclinicudon/
https://ksclinicudon.blogspot.com/
https://www.instagram.com/ksclinicudon/
ที่อยู่ https://goo.gl/maps/8yjDMnAbPRUdiYXs6
ที่อยู่ 140/19-20 ไพร์มสแควร์ ถนนหน้าสถานีรถไฟ ต.หมากแข็ง อ.เมือง จ.อุดรธานี
เทศบาลนครอุดรธานี 41000
ทางคลินิกเปิดบริการทุกวัน เวลา 17.00น - 20.00น
วันเสาร์ อาทิตย์ และวันหยุดนักขัตกฤษ์ เวลา 10.00น - 20.00น.
( ปิดทำการทุกวันพุธ )
0 notes
Text
Kineret for Rheumatoid Arthritis
What is KINERET used for?
Kineret is a prescription medication named an interleukin-1 receptor antagonist (IL-1ra) used for reducing the signs/symptoms and slowing the damage of moderate/severe active RA in patients aged 18 years and older when one or more other medications for RA have failed. It is also used for the treatment of patients with a form of Cryopyrin-Associated Periodic Syndromes (CAPS) named Neonatal-Onset Multisystem Inflammatory Disease (NOMID). Treatment of kineret 100 mg is not prescribed for children with Juvenile Rheumatoid Arthritis.
How should I use Kineret: Kineret should be used exactly as your healthcare professional tells you to. You may not have to use all of the liquid medication in the prefilled syringe. The kineret injection is administered under your skin. Inject this medication at about the same time every day. In case you have complications with kidney, your healthcare professional may need to change how often you administer your kineret dosage. In case you miss/forget a dose of Kineret injection, discuss with your doctor in order to determine when you can use your next injection.

What are the possible side effects of Kineret?
Treatment with Kineret may be responsible for causing serious side effects, including:
serious infections: Kineret therapy may lower your ability in order to fight infections. While on therapy with Kineret, call your doctor right away in case you:
get an infection
have any sign of an infection including a fever/chills
have any open sores on your body
You may get an infection in case you receive a live vaccine while on kineret dose. You should avoid receiving live vaccines while on therapy with Kineret.
allergic reactions: Stop treatment with Kineret and call your doctor or seek emergency help promptly in case you have any of these signs or symptoms of an allergic reaction:
swelling of face/lips/mouth/tongue
trouble breathing
wheezing
severe itching
skin rash/redness/swelling outside of the injection site area
dizziness or fainting
fast heartbeat or pounding in your chest (tachycardia)
sweating
Reduced ability of the body to fight infections (immunosuppression): It is unspecified if the treatment with drugs that are responsible for causing immunosuppression, like kineret 100 mg, affects your risk of getting cancer.
Reduced white blood cell count (neutropenia): Kineret treatment may cause you to have a reduced number of white blood cells (neutrophils). Neutrophils are necessary in order to fight infections. You must have the blood tests prior to starting anakinra 100 mg therapy, then monthly for three months. After the initial three months you must have your blood tested every three months for up to one year.
Apart from serious, certain most common side effects of Kineret (anakinra injection) also reported, which may include:
injection site skin reactions.
rheumatoid arthritis (RA) gets worse even with therapy, in case you already have RA
headache
nausea and vomiting
diarrhea
joint pain
fever
feeling like you have the flu
sore throat or runny nose
sinus infection
Report your healthcare professional in case you have any persistent side effects. These are not the entire possible side effects of Kineret.
Who should not use a Kineret?
Avoid using inj kineret 100 mg in case you are allergic to proteins made from bacteria named E.Coli or any of the other existing ingredients in Kineret.
What should I tell my healthcare professional prior to using Kineret?
Prior to using Kineret therapy, inform your healthcare professional if:
you have an infection or a known history of infections that keep coming back or other complications that may increase your risk of getting infections.
you have kidney problems.
you want to receive any vaccines. Individuals using
kineret injection 100 mg should not receive live vaccines.
you are pregnant or want to become pregnant. Kineret therapy may harm your unborn baby.
you are breastfeeding or want to breastfeed. The drug kineret may pass into your breast milk. You and your doctor should decide in case you will use Kineret or breastfeed.
How should I store Kineret?
Store Kineret in the refrigerator between 36°F to 46°F (2°C to 8°C). Avoid freezing or shaking Kineret. Keep the vials of Kineret in its original carton and away from the light. Keep it out of the reach of children.
Price: As with all medications, the kineret injection price can vary. To buy this medication at the best price, kindly contact us at - 9310090915.
NOTE: The piece of information provided in this article is intended to be helpful and educational, but it does not constitute an endorsement by us and is not meant to be a substitute for professional medical advice
1 note
·
View note
Photo

It is Autoinflammatory Disease awareness month! Did you know that an Autoinflammatory Disease is similar to an Autoimmune Disease but is not the same thing? An Autoinflammatory Disease (AIF) is when the innate immune cells are activated without the presence of an infection or injury. This can result in inflammation or fever occurring. An Autoimmune Disease (AD) is when adaptive immune cells lose their ability to tolerate other cells in the body. This results in the immune system attacking healthy tissues. Unlike AIFs, ADs have very unique symptoms such as temperature sensitivity, hair loss, etc. There are many types of Autoinflammatory Diseases including but not limited to ...Behçet’s disease, Familial Mediterranean Fever (FMF), Neonatal Onset Multisystem Inflammatory Disease (NOMID), Tumor Necrosis Factor Receptor-Associated Periodic Syndrome (TRAPS), Deficiency of the Interleukin-1 Receptor Antagonist (DIRA), Chronic Atypical Neutrophilic Dermatosis With Lipodystrophy and Elevated Temperature (CANDLE), and more. Sources: https://www.niams.nih.gov/health-topics/autoinflammatory-diseases and https://www.autoimmuneinstitute.org/articles/about-autoimmune/autoimmune-vs-autoinflammatory/ [Image Description: Red background with white text that is titled "Did You Know?" below reads " Autoinflammatory diseases (AIF) refer to problems with the innate immune system’s reactions. The innate immune system includes which uses white blood cells instead of antibodies to destroy invaders. AIFs occur when innate immune cells are activated without an infection or injury being present. This can cause intense inflammation episodes that result in symptoms such as fever, rash, or joint swelling." "@Invisible_Illness_Network"]recLWqMKjnvshsQFL, recKpWVY36R4uDyX9
0 notes
Text
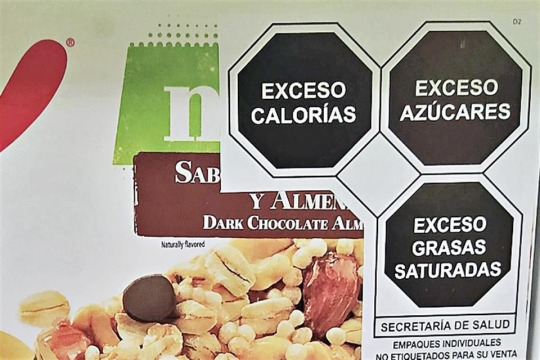
So I've been eating more health conscious lately since I recently got diagnosed with Multisystem Inflammatory Syndrome (MIS) and have a high risk for prediabetes because of it and you can tell I have no idea what the fuck I'm doing because when I try to count calories I'm only having 500-700 a day max when I so desperately need 1500 minimum. (Which I'm easily achieving today on my cheat day, go figure)
I'm sure I'll ease into this diet better over time but good gods. No sugar? No carbs? In this economy? Do you know how much shit has hidden sugar in it? I'm just thankful Mexico has these handy stickers telling me it has an excess.
#exe talkz#normal mode#IBS#MIS#tw disordered eating#calorie deficit diet#husband and I are trying to figure out what I can and can't eat and it's a doozy - these stickers save a lot of time and money ngl#I have a great relationship with food but having to be health conscious to prevent worse disease stresses me tf out#I'm like not hungry 70% of the time and when I am - I'm craving everything I'm not supposed to have#Which for the record is sugars - carbs - and my bad FODMAP foods (lactose - onion - garlic - and mushrooms)#Yes I know - I can't have onions/garlic - that ruins like 90% of recipes I find online since everyone and their mother needs it#But if I eat those bitches I could land myself in the hospital so lol lmao even
2 notes
·
View notes
Text
COVID-19 in 2023 has been full of revelations and controversy.
Most health leaders involved in the U.S. pandemic response have resigned or been replaced, with one leaving his agency with a study that received much fanfare for a somewhat controversial take on vaccines.
Compared to 2022, the science on the effectiveness and risks of masking and vaccinations has become increasingly clear with the release of highly authoritative studies this year.
Let us review the top 10 major events that took place in relation to COVID in 2023.
1. FDA and CDC Find More COVID Vaccine Adverse Events, Including Stroke
Beginning in January, documents released under the Freedom of Information Act (FOIA) found that the U.S. Centers for Disease Control and Prevention (CDC) detected hundreds of safety signals for Pfizer and Moderna COVID-19 vaccines. This included adverse reactions of myocarditis, multisystem inflammatory syndrome in children (MIS-C), ventricle dysfunctions in the heart, and many more.

The FDA and the CDC released a joint statement declaring they detected stroke as a new safety signal in older people who took the Pfizer bivalent boosters. They later said the current evidence is insufficient. (Madalina Vasiliu/The Epoch Times, Daniel Chetroni/Shutterstock)
Days later, researchers affiliated with the FDA published a preprint finding that older people who received the Pfizer booster shot had a higher rate of Bell’s palsy, a type of facial paralysis.
In a statement released in May, the FDA determined that “the current evidence does not support the existence of a safety issue,” as findings of stroke among the elderly decreased. They added that agencies will continue to evaluate new data as they become available.
19 notes
·
View notes
Photo

COVID-19 Brief - Government Oversight: Vaccine Risks FDA researchers in a federally funded cohort study of 3+ million children (aged 5-17 years) who received BNT162b2 COVID-19 vaccination found those aged 12 to 17 face a heightened risk of myocarditis and pericarditis (heart inflammation and heart condition) as compared to those who did not receive she vaccine. The research published in the Journal of the American Medical Association on May 22, 2023; reported that a threshold of risk was reached, requiring the warning be published. The vaccine was also attributed to increased risks of encephalitis or encephalomyelitis; anaphylaxis; common thromboses with thrombocytopenia; seizures or convulsions; Bells palsy; deep vein thrombosis; pulmonary embolism; disseminated intravascular coagulation; immune thrombocytopenia; narcolepsy; appendicitis; nonhemorrhagic stroke; Guillain-Barré syndrome; multisystem inflammatory syndrome in children; transverse myelitis; cerebral and abdominal (unusual site) thrombosis with thrombocytopenia; Kawasaki disease; hem...(CLASSIFIED, see full brief at www.graymanbriefing.com)
0 notes
Text
Abstract
Background: COVID-19 vaccines have been linked to myocarditis which in some circumstances can be fatal. This systematic review aims to investigate potential causal links between COVID-19 vaccines and death from myocarditis using post-mortem analysis. Methods: We performed a systematic review of all published autopsy reports involving COVID-19 vaccination-related myocarditis through July 3rd, 2023. All autopsy studies that include COVID-19 vaccine-induced myocarditis as a possible cause of death were included, without imposing any additional restrictions. Causality in each case was determined by three independent reviewers with cardiac pathology experience and expertise. Results: We initially identified 1,691 studies and, after screening for our inclusion criteria, included 14 papers that contained 28 autopsy cases. The cardiovascular system was the only organ system affected in 26 cases. In 2 cases, myocarditis was characterized as a consequence from multisystem inflammatory syndrome (MIS). The mean and median number of days from last COVID-19 vaccination until death was 6.2 and 3 days, respectively. Most of the deaths occurred within a week from the last injection. We established that all 28 deaths were causally linked to COVID-19 vaccination by independent adjudication. Conclusions: The temporal relationship, internal and external consistency seen among cases in this review with known COVID-19 vaccine-induced myocarditis, its pathobiological mechanisms and related excess death, complemented with autopsy confirmation, independent adjudication, and application of the Bradford Hill criteria to the overall epidemiology of vaccine myocarditis, suggests there is a high likelihood of a causal link between COVID-19 vaccines and death from suspected myocarditis in cases where sudden, unexpected death has occurred in a vaccinated person. Urgent investigation is required for the purpose of risk stratification and mitigation in order to reduce the population occurrence of fatal COVID-19 vaccine-induced myocarditis.
2 notes
·
View notes
Text
Lupine Publishers | The Use of Sodium-Glucose Cotransporter 2 Inhibitors in Non-Alcoholic Fatty Liver Disease
:

Opinion
Non-alcoholic fatty liver disease (NAFLD) encompasses a spectrum of progressive liver abnormalities from simple hepatic steatosis to non-alcoholic steatohepatitis (NASH) to advanced fibrosis, cirrhosis, and/or hepatocellular carcinoma [1]. Parallel to the rising burden of obesity and metabolic syndrome, NAFLD has emerged as the leading cause of chronic liver disease at an estimated global prevalence of 24% [2]. Besides its known clinical burden for liver-related morbidity and mortality, NAFLD is potentially linked with other extra-hepatic chronic diseases and may be considered a multisystem condition. Particularly, NAFLD increases the risk of type 2 diabetes, cardiovascular diseases, chronic kidney disease, and all-cause mortality [1]. Potential pathophysiologic mechanisms underlying the detrimental effects of NAFLD include hyperglycemia, systemic inflammation, and increased oxidative stress [3]. Sodiumglucose cotransporter 2 (SGLT2) inhibitors are a new class of antidiabetic agents that inhibit the reabsorption of sodium and glucose in the proximal tubules of the kidney [4]. Commonly used SGLT2 inhibitors include canagliflozin, dapagliflozin, and empagliflozin. Large-scale randomized placebo-controlled trials have demonstrated the benefits of SGLT2 inhibitors in reducing adverse cardiovascular/renal events in patients with cardiometabolic conditions, including diabetes, obesity, and chronic kidney disease [5]. In regard to liver function, numerous studies have revealed that SGLT2 inhibition reduced the levels of partate aminotransferase (AST) as well as alanine aminotransferase (ALT) in patients with type 2 diabetes and established cardiovascular disease [6], highlighting the potential role of SGLT2 inhibitors in patients with NAFLD.
The use of SGLT2 inhibitors is associated with reductions in liver fat content in NAFLD. In a meta-analysis of patients with type 2 diabetes and NAFLD, SGLT2 inhibitors improved hepatic steatosis and reduced levels of ALT [7]. In the E-LIFT trial which included 52 patients with type 2 diabetes and NAFLD, empagliflozin treatment reduced liver fat, as measured by MRI-derived proton density fat fraction [8]. While these results seem to support the role of SLGT2 inhibitors in NAFLD, it is important to note that prior investigations are carried out in patients with diabetes. Although the reductions in ALT and AST were independent of levels of glycated hemoglobin in the EMPA-REG OUTCOME trial [6], the effects of SGLT2 inhibitors on NAFLD and hard cardiovascular endpoints in the absence of diabetes remain unknown. Further to this is the uncertain mechanisms underlying the improvement of NAFLD with SGLT2 inhibitors. While the glucose-lowering effects of SGLT2 inhibitors have been postulated as a major mechanism through which SGLT2 inhibitors alleviate hepatic dysfunction, the absence of protection against hepatic dysfunction with other potent hypoglycemic agents, including DPP4 inhibitors and metformin, speak against this hypothesis and highlight that there might be other potential mechanisms responsible for the observed benefits of SGLT2 inhibitors. As our understanding of SGLT2 inhibitors progresses, their pleiotropic effects are becoming increasingly apparent. Recent studies have shown that treatment with SGLT2 inhibitors significantly reduced the levels of pro-inflammatory cytokines that are associated with NAFLD, including interleukin-6 (IL-6) and C-reactive protein (CRP) [9,10]. SGLT2 inhibitors also exhibit antioxidant properties, protecting tissue damage/fibrosis due to oxidative stress, and might also ameliorate atherosclerotic changes which are well-known to be associated with NAFLD [11]. Taken together, SGLT2 inhibitors are a promising therapeutic strategy for NAFLD. Further clinical trials are warranted to establish the benefits of SGLT2 inhibitors in patients with NAFLD regardless of the presence of diabetes to halt the rapidly growing pandemic of NAFLD and its assorted comorbidities/complications.
For More Lupine Publishers Open Access Journals Please visit our Website:
https://lupinepublishers.com/index.php
For more Current Trends in Gastroenterology and Hepatology articles please click here: https://lupinepublishers.com/gastroenterology-hepatology-journal/index.php
#lupine publishers#lupine journals#articles#submission#gastroenterology#hepatology#lupine open access journals
0 notes
Text
Exaggerated responses to a virus long gone | Science#Exaggerated #responses #virus #long #Science
Multisystem inflammatory syndrome in children is caused by abnormal cell activation
#Exaggerated #responses #virus #long #Science

View On WordPress
0 notes
Text
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a disabling multisystem illness in which individuals are plagued with fatigue, inflammatory symptoms, cognitive dysfunction, and the hallmark symptom, post-exertional malaise. While the cause of this disease remains unknown, there is evidence of a potential infectious component that, along with patient symptoms and common onsets of the disease, implicates immune system dysfunction. To further our understanding of the state of ME/CFS lymphocytes, we characterized the role of fatty acids in isolated Natural Killer cells, CD4+ T cells, and CD8+ T cells in circulation and after overnight stimulation, through implicit perturbations to fatty acid oxidation. We examined samples obtained from at least 8 and as many as 20 subjects for immune cell fatty acid characterization in a variety of experiments and found that all three isolated cell types increased their utilization of lipids and levels of pertinent proteins involved in this metabolic pathway in ME/CFS samples, particularly during higher energy demands and activation. In T cells, we characterized the cell populations contributing to these metabolic shifts, which included CD4+ memory cells, CD4+ effector cells, CD8+ naïve cells, and CD8+ memory cells. We also discovered that patients with ME/CFS and healthy control samples had significant correlations between measurements of CD4+ T cell fatty acid metabolism and demographic data. These findings provide support for metabolic dysfunction in ME/CFS immune cells. We further hypothesize about the consequences that these altered fuel dependencies may have on T and NK cell effector function, which may shed light on the illness’s mechanism of action.
0 notes