#myotome weakness
Text
youtube
Does the pain originate from the extremity or the spine? with Dr., Nick Rainey
Determining whether pain originates from the extremity (such as an arm or leg) or the spine can be challenging and often requires a thorough assessment by a healthcare professional. Pain can be referred, meaning that it is felt in a different location than its actual source.
#upper spine pain#advanced spine and pain#severe leg pain#severe spinal stenosis#failed back syndrome#decompress spine#nevro spinal cord stimulator#neck decompression#spine problems#spine and pain center#lumbar facet syndrome#spine and pain management#l4 l5 stenosis treatment#spinal stenosis therapies#spinal muscles#myotome testing#myotome weakness#the spine?#Does the pain originate from the extremity or the spine? with Dr.#Nick Rainey#Youtube
0 notes
Text
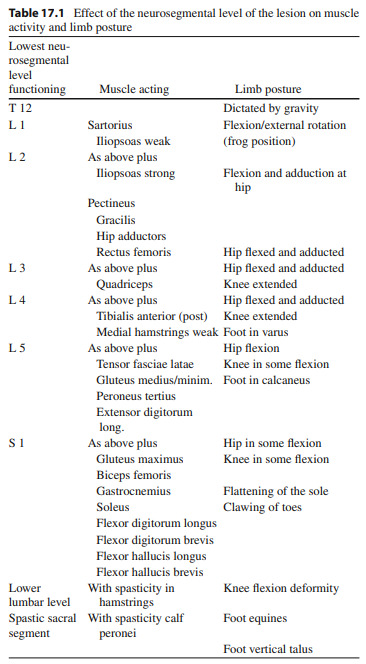
Findings in various levels of myelomeningocele
what is interesting is that myelomeningocele helped a lot in the study of the nerve root muscle supply by two means: first it gives a unique opportunity for stimulation of motor nerve roots and second to study of motor root lesions.
at least 50% of nerve supply to an individual muscle must be lost before clinical paralysis can be detected
infants born with myelomeningocele and treated conservatively are liable to remain paralyzed or become increasingly paralyzed. among the factors responsible for this deterioration may be traction exerted on the nerve roots passing from the plaque of spinal cord to the intervertebral foramina when the MM sac fools up with cerebrospinal fluid during the first week of life and the caudal roots tend to be more severely affected.
so lets go back to the title of this article, findings in various levels of myelomeningocele.
paralysis below T12: complete paralysis of lower limbs
paralysis below L1: weak to moderate hip flexion + weak sartorius = hip flexion and external rotation

paralysis below L2: strong hip flexion + moderate hip adduction = hip flexion and adduction

paralysis below L3: normal hip flexion + normal hip adduction + normal knee extension = hip flexion and adduction and knee extension
paralysis below L4: normal hip flexion + normal hip adduction + some hip abduction in flexion + normal knee extension + strong dorsiflexion and inversion = flexion and adduction and external rotation of hip + recurvatum of knee + calcaneo-varus foot


paralysis below L5: normal hip flexion + normal hip adduction + moderate abduction + no hip extension + normal knee extension + moderate knee flexion + normal inversion + moderate eversion + strong dorsiflexion + no planterflexion = hip flexion without adduction or abduction + semi-flexed knee + foot calcaneus

paralysis below S1: normal hip flexion + normal hip adduction + normal hip abduction + moderate hip extension + normal hip internal and external rotation + strong knee flexion + normal dorsiflexion + normal inversion + normal eversion+ moderate planterflexion + normal toes extension + strong great toe flexion + no foot intrinsic muscles (except abductor hallucis + flexor hallucis brevis) + weak flexor digitorum longus = clawing of toes and flattening of the skin of the sole of the foot

paralysis below S2: weak intrinsic muscles of foot = at clinical examination it is difficult to detect any abnormality but, with growth development of clawing of the toes.
so this study came with a conclusion regarding the innervation of muscles of the lower limbs

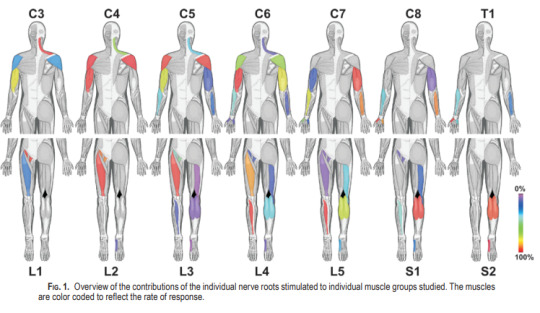
but newer studies using direct intraoperative nerve root stimulations during decompressive surgery concluded that a significant number of roots innervate a broader range of muscles than expected.
this table summarizes the neurological findings in MM
References:
(1) SHARRARD WJ. THE SEGMENTAL INNERVATION OF THE LOWER LIMB MUSCLES IN MAN. Ann R Coll Surg Engl. 1964 Aug;35(2):106-22. PMID: 14180405; PMCID: PMC2311748.
(2) Schirmer CM, Shils JL, Arle JE, Cosgrove GR, Dempsey PK, Tarlov E, Kim S, Martin CJ, Feltz C, Moul M, Magge S. Heuristic map of myotomal innervation in humans using direct intraoperative nerve root stimulation. J Neurosurg Spine. 2011 Jul;15(1):64-70. doi: 10.3171/2011.2.SPINE1068. Epub 2011 Apr 8. PMID: 21476796.
(3) Graham, H. K., & Parsch, K. (2009). Neural Tube Defects, Spina Bifida, and Spinal Dysraphism. Children’s Orthopaedics and Fractures, 265–286. doi:10.1007/978-1-84882-611-3_17
0 notes
Text
Is There A Neck-Shoulder Syndrome?| Lupine Publishers

Lupine Publishers| Anesthesia and pain medicine Journal
Abstract
Concomitant presentation of neck and shoulder pain is a common clinical scenario which can present a significant diagnostic and therapeutic dilemma. Neck and shoulder pain presentations can be separated into four different categories: Primary neck pathology with referred pain to the shoulder, primary shoulder pathology with referred pain to the neck, primary neck and primary shoulder pathology, and primary neck pathology resulting in secondary shoulder pathology. Primary neck pathology resulting in secondary shoulder pathology is mechanically plausible but not proven. Authors are proposing this scenario to be described as “neck-shoulder syndrome.” For instance, C5 and/or C6 cervical radiculopathy can result in rotator cuff, deltoid, biceps and scapular muscle weakness as these nerve roots innervate the shoulder girdle musculature which in turn could produce shoulder/scapular muscle imbalance resulting in shoulder impingement signs. A patient may present with features of both cervical radiculopathy and shoulder impingement syndrome in this scenario. At this time there are no agreed clinical criteria for a diagnosis of “neck-shoulder syndrome.” As with any other syndrome, management differences can only be well studied once the entity has been properly defined. In this article, authors set out to summarize how to best approach patients presenting with both neck and shoulder pain while describing features of proposed “neck-shoulder syndrome.” It is paramount to take a comprehensive and holistic approach towards patients presenting with concomitant neck and shoulder pain as the symptoms may not always represent isolated entities.
Keywords: Neck and shoulder pain; Neck-shoulder syndrome; Pain treatment; Differential diagnosis of neck and shoulder pain
Introduction
Co-existent neck and shoulder pain has been described in limited fashion in the literature as a unique diagnosis, but the concomitant presentation of neck and shoulder pain is a common scenario in primary care and orthopedic offices [1,2]. Gorski et al described “shoulder impingement syndrome” where patients presented with neck pain secondary to rotator cuff tendinopathy [1]. Compere et al described a “neck, shoulder, and arm syndrome” which primarily referred to neuropathic pain in the neck, shoulder and arm resulting from a brachial plexus lesion [2]. When patients present with both neck and shoulder pain, it can present a significant diagnostic dilemma[3]. “Hip spine syndrome” has recently been described, and “neck-shoulder syndrome” likely represents an analogous entity involving the cervical spine and upper limb [4]. It is estimated that among primary care office visits, neck pain accounts for approximately 20-30% and shoulder pain for 10-20% of musculoskeletal complaints. From this population, combined neck and shoulder problems account for approximately 6-10% [3,5,6,7].
Discussion
Concomitant neck and shoulder pain presentations can be separated into four different categories: Primary neck pathology with referred pain to the shoulder, primary shoulder pathology with referred pain to the neck, primary neck and primary shoulder pathology, and primary neck pathology resulting in secondary shoulder pathology
Primary neck pathology with referred pain to the shoulder
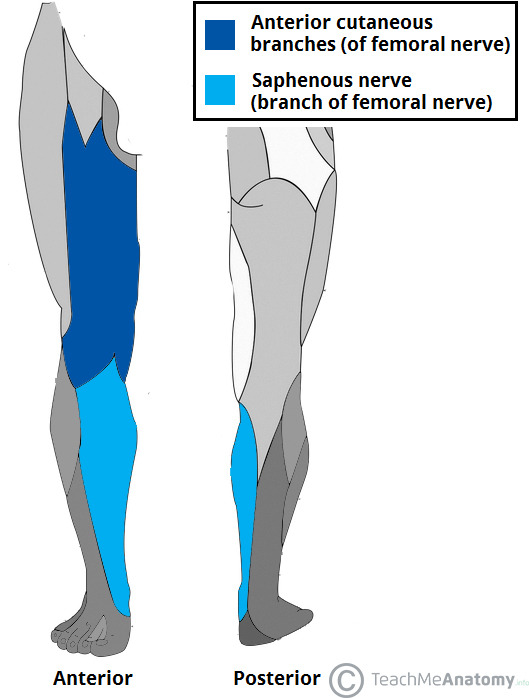
An isolated C5 and/or C6 radiculopathy without shoulder pathology could certainly present with neck and shoulder pain due to C5 and C6 dermatomal symptoms corresponding to the shoulder region. C5 or C6 myotomal pain can cause pain in the deltoid, scapula and biceps, and can mimic shoulder pathology [8,9]. This scenario is typically straightforward as the physical examination will be absent of shoulder impingement signs. Classically, cervical radiculopathy examination can demonstrate positive cervical root impingement signs (Spurling’s maneuver), myotomal weakness, dermatomal sensory abnormalities and blunted reflexes in a specific root distribution. Several neuropathies involving brachial plexus and its proximal branches will also refer pain to neck and shoulder simultaneously.
Primary shoulder pathology with referred pain to the neck
Primary shoulder pathology should not directly lead to neck pathology, and such cases are not well described in the literature. Nevertheless, patients with shoulder pathology may develop pain and tightness in the trapezius muscle on the ipsilateral side and referred pain in the cervical area. Restricted motion at the glenohumeral joint may also lead to overuse and pain in the scapulothoracic musculature. A general concern in musculoskeletal medicine is that symptomatic pathology in a joint may refer pain to a joint below and/or above.
Primary neck and primary shoulder pathology
Degenerative arthritis can affect multiple joints. Thus, many patients may have both glenohumeral arthritis and cervical spondylosis. The radiographic incidence of glenohumeral arthritis is reported as 32.8% in people over 60 years of age [10]. Radiographic evidence of cervical spondylosis is present in 50% of people over 50 years of age and 75% of individuals over 65 years of age [11]. As both conditions are common, both can present as “pain generators.”
Primary neck pathology resulting in secondary shoulder pathology
Primary neck pathology resulting in secondary shoulder pathology is mechanically plausible although not proven. For instance, C5 and/or C6 cervical radiculopathy can result in rotator cuff, deltoid, biceps and scapular muscle weakness as these nerve roots innervate the shoulder girdle musculature. This could produce muscle imbalance and poor shoulder/scapular mechanics. A patient may present with features of both cervical radiculopathy and shoulder impingement syndrome in this scenario. In clinical practice, it is not uncommon to see a patient with chronic neck pain presenting with insidious onset of shoulder pain later in the course. Authors are proposing this unique presentation be referred to as “neck-shoulder syndrome.” Although most clinicians would treat this as separate neck and shoulder pain, they may be related diagnoses.
Literature Search
We conducted a comprehensive search in the PubMed database in order to identify relevant studies on “neck-shoulder syndrome.” Based on the review of the available literature, there are no agreed upon clinical criteria for a diagnosis of “neck-shoulder syndrome” despite its common clinical presentation nor is there a well described “neck-shoulder syndrome.” As with any other syndrome, management differences cannot actually be studied until the entity has been appropriately defined. This article will concentrate on how to best approach patients presenting with both neck and shoulder pain while describing features of proposed “neckshoulder syndrome.”
Presentation
In patients presenting with neck and shoulder pain, a thorough history is paramount in identifying the etiology of the patient’s pain.
Location: Patients with primary neck pathology can experience pain extending beyond the neck based on the etiology. Disorders that affect the lower cervical nerve roots will often result in pain distal to the shoulder which can be characterized by radiation into the arm in a clear dermatomal or myotomal distribution [12]. In addition, Dwyer et al described reproducible pain patterns that can refer into the shoulder, trapezius and occiput from cervical zygapophyseal joint pathology [13-15]. Pain from a primary shoulder problem can also refer pain to the neck, periscapular region and distally into the arm although not typically extending below the elbow [16]. Associated paresthesias are not classically associated with a primary shoulder problem.
Onset: Onset of symptoms is also a key component of the history. Degenerative cervical pathology can have insidious onset although acute disc herniations can have a sudden onset that may be precipitated by trauma. Whiplash injuries are known to precipitate neck pain which can be of myofascial and/or cervical facet in origin. Shoulder disorders can also be of insidious (overuse injuries) or acute onset (trauma). Sudden onset of shoulder pain with restricted motion can be associated with acute calcific tendinitis or adhesive capsulitis. Neuralgic amyotrophy (Parsonage Turner syndrome/ brachial neuritis) has a unique presentation where patients usually experience severe, acute pain following exercise, recent illness, immunization, surgery or trauma [17]. As the initial severe pain starts to resolve, neurological deficits will become apparent, which is in contrast to most presentations of cervical radiculopathy where pain will continue with associated neurological symptoms. Onset of symptoms plays a key role in proper identification of proposed “neck-shoulder syndrome.” Development of shoulder pain (especially in the absence of injury) after onset of neck/radicular pain can be considered primary neck pathology with secondary shoulder pathology and can be referred to as “neck-shoulder syndrome.” Shoulder pain in this scenario is likely secondary to rotator cuff and periscapular muscle weakness/imbalance caused by C5 and/or C6 cervical radiculopathy. This clinical scenario is not well studied in the literature, hence prevalence and incidence is not known. Among patients with cervical radiculopathy, studies report a frequency of C5 nerve root involvement at 5-10%, C6 at 20-25%, and C7 at 45-60% [12,18].
Exacerbating factors: Pain with overhead arm movements generally suggests primary shoulder pathology. However same pattern can also be present in peripheral neuropathies like thoracic outlet syndrome and spinal accessory, suprascapular, or axillary neuropathy. Shoulder pain with side lying on the affected upper limb tends to be associated with shoulder impingement and acromioclavicular joint arthropathy.
Features of systemic diseases: In patients who present with neck and shoulder pain in the absence of trauma, the history will need to include an assessment for widespread involvement that may suggest systemic disease processes like fibromyalgia, polymyalgia rheumatica, myofascial pain syndrome and myopathy.
Red flags: The history should also include an evaluation for findings to suggest a disease process that requires more urgent evaluation. Red-flag symptoms to assess for include gait imbalance, hand clumsiness, bowel/bladder dysfunction (cervical myelopathy), pain after high impact trauma (fractures), unintentional weight loss (Pancoast tumor), chest pain (cardiac ischemia), blurry vision, nausea/vomiting and vertigo (vertebral artery dissection/ insufficiency).
Physical Examination
In addition to a detailed history, a thorough physical examination is key for proper diagnosis and identification of the pain generator(s). A thorough neurological exam plays an essential role in distinguishing neck from shoulder pathology. Sensory, motor and reflex changes in a specific nerve root distribution are characteristic of cervical radiculopathy. C5 and C6 cervical radiculopathies may result in periscapular and shoulder/rotator cuff muscle weakness while C7 radiculopathy is unlikely to cause shoulder weakness. Rotator cuff pathology may result in shoulder weakness with preserved elbow flexion while a C5 radiculopathy can result in weakness of both. Testing deltoid strength with the arms at the sides instead of in shoulder abduction can aid in differentiating pain inhibition versus true weakness.
Provocative Testing
Provocative testing can assist in the diagnosis of cervical and shoulder disorders [9, 19]. Among them, provocative tests for shoulder impingement may help distinguish primary versus secondary shoulder pathology in proposed “neck-shoulder syndrome”(Table 1) [18-30].
In patients with neck and shoulder pain, one test by itself may not have enough sensitivity and specificity to make a diagnosis and most physical exam maneuvers are not pathognomonic. A combination of multiple exam components and a thorough history are necessary to accurately identify the etiology of symptoms.
Table 1: Provocative tests for common cervical and shoulder problems and reported validity.

Diagnostic Testing
When presented with both neck and shoulder pain, history and physical exam should dictate appropriate use of diagnostic tests. Although imaging studies such as radiography, CT and MRI can reveal many pathologies, further testing should be done to identify the true pain generator. When suspecting pain mediated by a cervical zygapophyseal joint, cervical diagnostic medial branch blocks can be considered. A shoulder injection of lidocaine with or without corticosteroid can be done for diagnostic and perhaps therapeutic reasons. In cases of secondary shoulder pathology, this may give the patient partial benefit, but a primary cervical pathology should still be investigated [9]. Electrodiagnostic testing with electromyography (EMG) and nerve conduction studies (NCS) can be employed when suspecting myopathy, brachial plexopathy, peripheral neuropathy or radiculopathy. When evaluating neck and shoulder pain, scientific evidence suggests using a combination of history, physical examination, imaging modalities, diagnostic injections and electrodiagnostic study to make the appropriate diagnosis.
Treatment
Success of any proposed treatment algorithms will depend on an accurate diagnosis. There is scant evidence on how to approach the concomitant presentation of neck and shoulder pain. Treatment should be geared toward the primary site of pathology whether it be the cervical spine or the shoulder [3]. Lack of current literature evidence underscores the importance of describing a “neckshoulder syndrome,” as it can lead to studies looking at management differences. It can be hypothesized that in patients with cervical radiculopathy with secondary rotator cuff impingement, treatment of the primary lesion will likely yield eventual improvement at the secondary site although no studies have been done on this topic.
Conclusion
The concomitant presentation of shoulder and neck pain is a common scenario in primary care and orthopedic offices and can present a diagnostic and therapeutic dilemma. A careful history and thorough physical examination along with ancillary studies can often yield the correct diagnosis and successful treatment. Primary neck pathology resulting in secondary shoulder pathology is mechanically plausible but not proven. Authors are proposing this scenario to be described as “neck-shoulder syndrome.” Appropriately describing a “neck-shoulder syndrome” can lead to further studies looking at management differences. A prospective study looking at incidence of shoulder impingement signs in chronic C5 and/or C6 radiculopathy patients could be helpful in delineating diagnostic criteria for “neck-shoulder syndrome.” Above all, it is paramount to take a comprehensive and holistic approach towards patients presenting with concomitant neck and shoulder pain as the symptoms may not always represent isolated entities.
Acknowledgements
The authors would like to thank Dr. David Janerich for his help with the development of the article.
For more Lupine Publishers Open Access Journals Please visit our website:
https://lupinepublishers.us/
For more Global Journal of Anesthesia & Pain Medicine articles Please Click Here:
https://lupinepublishers.com/anesthesia-pain-medicine-journal/index.php
To Know More About Open Access Publishers Click on Lupine Publishers: https://lupinepublishers.com/
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
#Lupine Publishers#Lupine Publishers Group#Open Access Journals#Anesthesia Jounal#Pain medicine#pain management#general anesthesia#local anesthesia#surgery#post operative#critical care
3 notes
·
View notes
Text
Neurology
I had a preceptorship with a neurologist, and it was awesome! We saw four patients in three hours, and it didn't feel rushed at all. The neurologist also did a lot of procedures on these patients, from outpatient nerve blocks to the EMG setup he had right in his office.
One patient in particular had a strange numbness in one of his feet, and through a complete history and a full hour of EMG testing, we figured out that it was a very strange presentation of sciatic nerve compression, which was so interesting.
The one big takeaway for me was that when you he did the myotome portion of his neuro exam, he pushed with all his might until he actually overcame the patient's strength (impressive especially when your patient is a lot bigger than you are). He said that because many doctors shy away from doing this, slight weaknesses and asymmetry can go unnoticed, meaning a worse prognosis when they finally present to a neurologist.
I really like neuro because a lot of it is like a puzzle. All the symptoms are coming from one place and you have to figure out where. Now especially with all the procedures I saw available to outpatient neurologists, it's definitely on my list.
25 notes
·
View notes
Text
My patient: Radicular L. Back Pain
My patient “Rad” has been coming to the clinic for about 4 weeks now with complaints of low back pain and radicular symptoms into the right thigh, right medial foot, and slightly into the right calf.
My patient has lordosis of the lumbar spine and significant kyphosis of the thoracic spine. The patient is active and wants to return to activities like swimming, walking long distances, and simply standing for long periods of time without having symptoms in the right leg.
The primary complaint is numbness and tingling in the medial right calf and foot. The patient also has some numbness and tingling into the lateral thigh which occurs less frequently, but can cause the patient discomfort from time to time. All of his symptoms are aggrivated with long periods of standing, walking, and swimming. He does not feel pain, but simply notes a discomfort disscribed as a constant part of his thigh or foot “falling asleep”.
As student physical therapist, it is my challenge to remedy this patients condition to the best of my abilities. This has lead me to find the best evidence for how I can help. You can follow along!
Up until now, I have focused on manual therapy techniques to relieve pain and improve the biomechanics around the joint segments of his L4-5 lumbar segments on the right which show significant muscle guarding and stiffness. At this current clinic, gaining mobility in the spine is encouraged with extension press ups. The patient has seen improvements with the combination of press up extensions and manual therapy.
Breifly looking at some pictures of dermatomal and peripheral nerve patterns, we can take a look at my clinical reasoning to determine that the patients symptoms are not distal to the spinal nerves of the lumbar spine. Or at least, the majority of the symptoms origin from a more proximal location along the nerves exiting the lumbar spine.
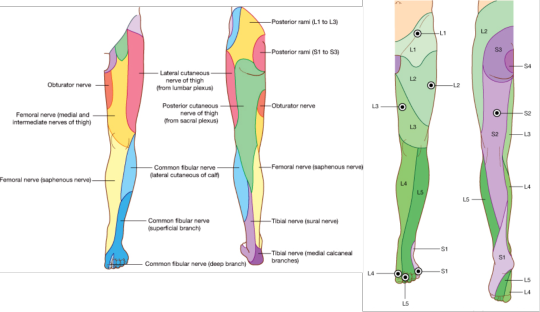
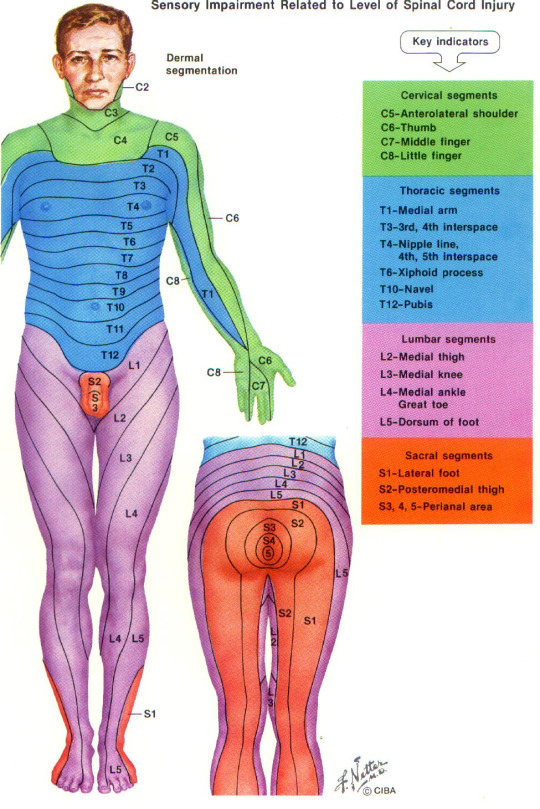
Looking at these diagrams, you can observe my reasoning for proximal nerve compression involving spinal nerve roots instead of more distally located compression. Distal compression of the nerve may indeed be present, however, the primary symptoms follow a sensory pattern that indicates possibility of L3, L4 involvement on the right side.
So is there muscular involvement? Myotome testing is negative. However, there is noted weakness of the right gluteus maximus and medius muscles compared to the left side. The innervation for these muscles involves the superior gluteal nerve with spinal innervation involvement of L4,5,S1.
When performing slump tests, streight leg raise with tibial nerve bias, and femoral nerve tension tests, the patient has noted positive symptom aggrivation. The symptoms were especially aggravated in the medial foot with a tibial nerve bias straight leg raise.
So this gives you some idea of the presentation of my patient. I am on a quest to determine if nerve mobilization to nerves containing (L2, L3 due to some discrepancy on the pattern of these nerves in the thigh), L4, L5 nerve roots will improve patient symptoms in the foot and lateral thigh.
I am researching an article: Effectiveness of neural mobilization in patients with spinal radiculopathy: A critical review
3 notes
·
View notes
Text
A double determination of central motor conduction time in the assessment of Hirayama disease
Hirayama disease (HD) is a benign neurological disease associated with unilateral or asymmetric weakness and/or amyotrophy in the muscles supplied by the C7-T1 myotomes, without significant sensory involvement and myelopathy (Hirayama, 2000; Zhou et al., 2010; Wang et al., 2012).
from # All Medicine by Alexandros G. Sfakianakis via alkiviadis.1961 on Inoreader http://ift.tt/2wgnbKO
from OtoRhinoLaryngology - Alexandros G. Sfakianakis via Alexandros G.Sfakianakis on Inoreader http://ift.tt/2tTmGpD
0 notes
Text
A double determination of central motor conduction time in the assessment of Hirayama disease
Hirayama disease (HD) is a benign neurological disease associated with unilateral or asymmetric weakness and/or amyotrophy in the muscles supplied by the C7-T1 myotomes, without significant sensory involvement and myelopathy (Hirayama, 2000; Zhou et al., 2010; Wang et al., 2012).
from #ORL-Sfakianakis via xlomafota13 on Inoreader http://ift.tt/2wgnbKO
from OtoRhinoLaryngology - Alexandros G. Sfakianakis via Alexandros G.Sfakianakis on Inoreader http://ift.tt/2vnPkDB
0 notes
Text
A double determination of central motor conduction time in the assessment of Hirayama disease
Hirayama disease (HD) is a benign neurological disease associated with unilateral or asymmetric weakness and/or amyotrophy in the muscles supplied by the C7-T1 myotomes, without significant sensory involvement and myelopathy (Hirayama, 2000; Zhou et al., 2010; Wang et al., 2012).
from #ORL via xlomafota13 on Inoreader http://ift.tt/2wgnbKO
from OtoRhinoLaryngology - Alexandros G. Sfakianakis via Alexandros G.Sfakianakis on Inoreader http://ift.tt/2wgvO8o
0 notes