#myotome testing
Explore tagged Tumblr posts
Text
youtube
Does the pain originate from the extremity or the spine? with Dr., Nick Rainey
Determining whether pain originates from the extremity (such as an arm or leg) or the spine can be challenging and often requires a thorough assessment by a healthcare professional. Pain can be referred, meaning that it is felt in a different location than its actual source.
#upper spine pain#advanced spine and pain#severe leg pain#severe spinal stenosis#failed back syndrome#decompress spine#nevro spinal cord stimulator#neck decompression#spine problems#spine and pain center#lumbar facet syndrome#spine and pain management#l4 l5 stenosis treatment#spinal stenosis therapies#spinal muscles#myotome testing#myotome weakness#the spine?#Does the pain originate from the extremity or the spine? with Dr.#Nick Rainey#Youtube
0 notes
Text





Master Myotome Testing for Precise Neurological Assessments!
Understanding myotomes is crucial for identifying nerve root injuries, spinal disorders, and muscle weaknesses. Effective testing allows medical professionals to pinpoint dysfunctions and create targeted rehabilitation plans.
At ANF Academy, we go beyond textbook knowledge—learn advanced clinical assessment techniques that enhance diagnostic accuracy and improve patient outcomes.
#inflammation#anf therapy#physical therapy#chronic pain#pain therapy#injury#doctors#physiotherapy#anf academy#medical course#medical education#wellness
1 note
·
View note
Text
Reflect on collaborative practice within the multidisciplinary team
There’s something different about walking into a clinic compared to an acute hospital. In hospitals, things feel more controlled. Patients are booked, files are reviewed, and there’s usually some time to mentally prepare. In the clinic? Not so much. On some days, like Thursday the 17th of April 2025, you don’t know who’s going to walk through the OT doors. And that’s exactly what happened. A woman came in with shoulder pain and hand numbness, and I was thrown into a whirlwind of learning that I’ll never forget.
She was 40 years old, living alone in Mayville, Durban, and came with a referral letter… but it was meant for physiotherapy. As soon as my supervisor saw her file, she suggested we do a joint session, physio and OT together. I felt my stomach drop. I wasn’t ready. At least, that’s what I told myself. I had no time to plan. No time to research the diagnosis. Just me, a file, and a patient in pain. But that’s the reality of being a health care professional, you don’t always get a heads-up. Sometimes, you need to adapt instantly and trust the knowledge and instincts you’ve been building for the past few weeks.
I joined the physio students in their session. They were being assessed, so the pressure was already high. I remember how nervous the student looked when their supervisor walked in. She stumbled through her initial screening, and then the supervisor quickly stepped in to guide the session. I stood quietly, absorbing everything. They started with posture checks, shoulder protraction, neck position, scapula placement and moved on to range of motion: shoulder abduction, flexion, all which increased her pain levels. Then came the neurological testing: dermatomes from C4–T1 using light touch, reflex testing (biceps reflex was absent), and myotomes. Each detail painted a clearer picture. I was fascinated. I could see the theory I learned in class come alive. She had been diagnosed with shoulder osteoarthritis, but as the physio supervisor worked through each test, the puzzle started coming together. The pain, the numbness, the weakness, it wasn’t just OA. It was cervical radiculopathy, a condition caused by nerve compression in the neck (Wainner et al., 2003).
I was witnessing a real-time differential diagnosis, and suddenly, the connection between textbook theory and real-world practice became so clear. It gave me a deep appreciation for the depth of physiotherapy assessments and made me reflect on the unique value we bring as heath care workers to the MDT team. This woman had been ironing clothes for a living since she was 14 years old. Every day, from 7 a.m. to 4:30 p.m., seven days a week. Repetitive motion, poor ergonomics, prolonged standing and barely any rest breaks had taken their toll. The physical strain made sense. While physios focused on identifying the anatomical source of the pain, I started thinking: What does this pain mean for her daily life? Her independence? Her income? This is where OT steps in. We go beyond the diagnosis. We focus on the function, the occupation. Our role is to bridge the gap between impairment and participation. Her occupation wasn’t just a job. It was her independence, her identity, and her income.
Using my understanding of ergonomics and kinesiology, I started planning how I’d approach her intervention. Scapular protraction (shoulders rolled forward) and neck flexion (head leaning down) are common postures when ironing for long periods, especially without proper setup. Her poor scapular positioning and cervical posture likely contributed to her nerve compression (Falla et al., 2017). She needed education on joint protection and energy conservation — small changes that could protect her body while keeping her occupation sustainable (AOTA, 2020). I also thought about how to make these changes realistic for her lifestyle. What if she doesn’t have space for an adjustable ironing board? What if she can’t afford ergonomic tools? This forced me to think creatively: how do we deliver low-cost, accessible solutions that still respect the person’s lived reality? I had to consider her reality: she lives alone. As a therapist, I used my knowledge of joint protection principles (JPP) and energy conservation principles (ECP) to address these concerns. For instance, to distribute pressure and reduce strain, I encouraged her to use both hands and employ leverage when ironing. This approach would allow her to share the load and avoid overloading one side of her body. Introducing a small, portable cart or stool could help reduce repetitive bending and provide more mobility, especially in the absence of an adjustable board. For balancing rest and activity, I suggested incorporating short breaks every 15-20 minutes of ironing. This would prevent prolonged muscle tension and give her body a chance to recover before fatigue sets in. I also recommended planning her tasks ahead of time, ensuring she avoids rushing and is more mindful of alternating between heavy and light activities. I emphasized resting before exhaustion to prevent overuse injuries. The key was finding low-cost solutions, such as using a basic stool or a cart from a local store while integrating practical rest strategies into her routine. By allowing extra time for activities and taking breaks when needed, these modifications would promote a sustainable ironing habit without compromising her comfort or well-being. Ergonomics, joint protection and energy conservation principles would be essential to help her maintain her occupation without worsening her symptoms (AOTA,2020).
From self-doubt to self-belief. At the start of the session, I was overwhelmed. I didn’t feel ready. But by the end of it, something had shifted. I asked questions, made observations, and applied theory to practice in a meaningful way. I had faced a challenge, and I had grown from it, not because I had all the answers, but because I had the courage to keep asking. I realized that being part of a multidisciplinary team is not just a checklist item, it’s a lifeline. Through this one joint session, I saw how combining perspectives creates a clearer, fuller picture for the patient. I also saw that I don’t have to know everything, I just have to be willing to learn, ask, and adapt.
This experience taught me that interdisciplinary teamwork is more than collaboration, it’s a safety net for both the client and each professional still learning. I saw how physiotherapy and OT roles differ, overlap, and complement each other. While physiotherapy provided clarity around diagnosis in this session, OT looked forward towards long-term participation and meaningful engagement. I want to get better at engaging with other professionals during sessions, even when it makes me nervous. I plan to practice by starting small: I will try to grow more confident in communicating with other professionals, talking to strangers in the clinic waiting room, initiating conversations with other students, and asking for feedback from supervisors more often. This session also taught me to value every member of the healthcare team and to see myself as one of them. Moving forward, I want to advocate more boldly for occupational roles in MDTs, and never let fear stop me from speaking up. I also want to deepen my clinical reasoning by reviewing assessments like dermatomes and reflex tests and seeing how they relate to function, not just diagnosis. Because OT isn’t just about understanding what’s wrong, it’s about empowering someone to live well despite it. This experience reminded me why I chose OT: it’s not just about treating dysfunction, it’s about protecting occupation, identity, and dignity.
In this case, OT isn’t just about the shoulder, or the nerve. It’s about the person behind the injury like the woman who irons for a living and making sure she can keep doing what matters, in a way that doesn’t hurt her.
References
American Occupational Therapy Association. (2020). Occupational therapy practice framework: Domain and process (4th ed.). American Journal of Occupational Therapy, 74(Suppl. 2), 7412410010p1–7412410010p87.
Falla, D., Jull, G., Russell, T., Vicenzino, B., & Hodges, P. (2017). Effect of neck exercise on sitting posture in patients with chronic neck pain. Physical Therapy, 87(4), 408–417.
Wainner, R. S., Fritz, J. M., Irrgang, J. J., Boninger, M. L., Delitto, A., & Allison, S. (2003). Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine, 28(1), 52–62.
0 notes
Text
Pathophysiology of Pain Pain is a physical manifestation of something being wrong within the body. Pain is an indicator of an injury or of a physical illness. Often, it is one of the first indicators that there is something wrong with the health of the patient and anyone experiencing pain should seek medical attention. Acute, chronic, and referred pain are three very different things but are often confused, even by medical experts. Pathophysiology: Acute pain tends to begin suddenly and is usually a sharp pain. It is considered a symptom of a disease or physical injury (Acute 2008). Examples of acute pain can include, but are no means limited to: surgery and recovery, broken bones, burns, cuts, contusions, and muscle injury. There is always a cause for acute pain, although the cause may or may not be serious and therefore it always requires investigation. Within the body, the polymodal peripheral receptors create sensations which are unpleasant for the person. These are modulated in the dorsal horn as well as in the anterior columns of the spinal cord and then moves up to the cerebral cortex (Fink 2005,-page 277). It is within the cerebral cortex that the pain is registered and the patient then experiences the sensation. Chronic pain is more long-term pain which tends to last beyond a period associated with temporary conditions. Long-term medical conditions like fibromyalgia can cause chronic pain (Understanding 2013). It is a more complicated type of pain than acute because the underlying cause of the pain is more important than treating the symptom itself, a process which can take a great deal of time and can frustrate the patient leading to depression and an exacerbation of symptoms. Patients dealing with chronic pain issues are abnormally sensitive to painful stimuli and this is attributed to a response to the activation of low-threshold mechanoreceptive A beta fibres. Three processes within the spinal cord are believed to be responsible for the different sensory processing in chronic pain patients: increased excitability, decreased inhibition, and structural reorganization (Woolf 1994,-page 525). Referred pain is a more mysterious form of pain than the other two. Pain is felt in one part of the body but that is not the location of the medical problem or physical injury (Vecchiet 1999,-page 489). This can make the cause of the pain difficult for medical staff to locate and diagnose because they will often test in the region of pain and only look at referred pain as a possibility when all avenues here are examined. Besides the origination point of the symptom, there will be secondary hyperalgesia within the referred zone. Although science has not yet proved the exact reason for referred pain, it is largely believed that it is not central convergence mechanism, wherein the dorsal horn neurons diverge within the deep tissue. It is hypothesized that nociceptive input from the skeletal muscles refer to myotomes outside the areas of origin and are spread by central sensitization to spinal segments near the origin point. Diagnosis: In terms of diagnosis, the most important thing is to locate the underlying cause for the pain, whether it is acute, chronic, or referred (Woessner 2013). First, muscles, nerves, and tissues near the area of pain will be examined to determine if there is a direct cause of pain which can be linked to the patient. If this is not possible, then further examination and testing must be undertaken. Acute pain is rarely, if ever, diagnosed as the sole problem of a patient because of the understanding that there must be a correlation between pain and causation. Referred pain also requires a cause for the discomfort and diagnosis of pain in and of itself is not acceptable in this context. Rather, the source for the pain must be ascertained for treatment. This is less true with chronic disease and chronic pain because in certain cases the pain itself is a disease, such as fibromyalgia. Prescription of Treatment: Acute pain is usually treated with medications such as anti-inflammatory medication, narcotics like morphine or codeine, and acetaminophen (Acute 2008). In addition, acute pain can be treated by holistic methods such as acupuncture or relaxation techniques. It can also be treated with more invasive treatments like surgery. In referred pain, a similar course is usually undertaken. The priority is upon finding the cause for the pain and in treating that cause moreso than treating the pain for itself. Works Cited Acute vs. chronic pain. (2008). Cleveland Clinic: Cleveland, OH. Fink, W.A. (2005, May). The pathophysiology of acute pain. Emergency Medicine Clinics of North America. 23(2). 277-84. Understanding pain. (2013). Pain Care Clinic: London, England. https://www.paperdue.com/customer/paper/pathophysiology-of-pain-98464#:~:text=Logout-,PathophysiologyofPain,-Length2pages Vecchiet, L., Vecchiet, J., & Giamberardino, M.A. (1999). Referred muscle pain: clinical and pathophysiologic aspects. Current Review of Pain. 3(6). 489-98. Woessner, J. (2013). Referred pain vs. origin of pain pathology: understanding the organic and physiological patterns of referred pain helps to identify the true origin of pathology and inform proper treatment. Practical Pain Management. Vertical Health Media. Woolf, C.J. & Doubell, T.P. (1999, Aug.). The pathophysiology of chronic pain -- increased sensitivity to low threshold A beta-fibre inputs. Current Opinion in Neurobiology. Dept. Of Anatomy and Developmental Biology: University College, London, UK. 4(4). 525-34. Read the full article
0 notes
Text
All the General Character lists
zoloje yay
Urochordata
Exclusively marine and cosmopolitan, found in all seas at all depths.
Mostly sedentary, some free-swimming.
Simple (solitary), aggregated in groups or composite (colonial)
Size (0.25-250mm), shape, and color variable.
Adult body degenerate, sac-like, unsegmented, without paired appendages and usually without tail.
Notochord present only in larval tail, hence "urochordata".
Respiration through test and gill-slits
Mostly hermaphrodite. Fertilization cross and external.
Development indirect including a free-swimming tailed larva with basic chordate characters. Metamorphosis retrogressive.
Asexual reproduction by budding common.
Cephalochordata
Marine, widely distributed in shallow waters
Mostly sedentary and buried with only anterior body end, projecting above bottom sand.
Body small, 5 to 8 cm long, slender, fish-like, metameric and transparent.
Head lacking. Body has trunk and tail.
Paired appendages lacking. Median fins present.
Exoskeleton absent. Epidermis single-layered.
Notochord rod-like, persistent, extending from rostrum to tail, hence the name Cephalochordata.
Sexes separate. Gonads numerous and metamerically repeated. Gonoducts lacking. No asexual reproduction.
Fertilization external in sea water.
Development indirect, including a free-swimming larva.
Cyclostomata
Body elongated, eel-like.
Median fins with cartilaginous fin rays, but no paired appendages. Tail diphycercal.
Skin soft, smooth containing unicellular mucous glands but no scales.
Trunk and tail muscles segmented into myotomes separated by myocommata.
Endoskeleton fibrous and cartilaginous. Notochord persists throughout life. Imperfect neural arches over notochord represent rudimentary vertebrae.
Jaws absent in group Agnatha
Mouth ventral, suctorial and circular, hence "cyclostomata".
Dorsal nerve cord with differentiated brain. 8-10 pairs of cranial nerves.
Sexes separate or united. Gonad single, large, without gonoduct.
Fertilization external. Development direct or with a prolonged larval stage.
Chordata
Aquatic, aerial or terrestrial. All free-living with no fully parasitic forms.
Body small to large, bilaterally symmetrical and metamerically segmented.
A postanal tail usually projects beyond the anus at some stage and may or may not persist in the adult.
Exoskeleton often present; well developed in most vertebrates.
Bodywall triploblastic with 3 germinal layers: ectoderm, mesoderm, and endoderm.
A skeleton rod, the notochord, present at some stage in life.
A cartilaginous or bony, living and jointed endoskeleton present in the majority of members.
Pharyngeal gill slits present at some stage; may or may not be functional.
Digestive system complete with digestive glands.
Sexes separate with rare exceptions.
Pisces
Aquatic, marine, or freshwater, herbivorous or carnivorous, cold-blooded, oviparous or ovoviviparous vertebrates.
Body usually spindle-shaped, streamlines and differentiated into head, trunk and tail. A neck is absent.
Locomotion by paired pectoral and pelvic fins along with median dorsal and caudal, supported by true dermal fin rays. Muscular tail used in propulsion.
Exoskeleton of dermal scales, denticles, or bony plates covering body surface.
Endoskeleton cartilaginous or bony. Jaws are hinged. Notochord more or less replaced by true vertebrae.
Respiration by gills. Gill-slits 5-7 pairs, naked or covered by operculum.
Heart 2 chambered, 1 auricle and 1 ventricle. Venous or single circuit. Sinus venosus and renal and portal systems present.
Kidneys mesonephric. Excretion ureotelic.
Brain with usual 5 parts. 10 pairs of cranial nerves.
Sexes separate. Gonads typically paired. Gonoducts open into cloaca or independently.
Amphibia
Aquatic or semiaquatic (freshwater), air and water breathing, carnivorous, cold-blooded, oviparous, tetrapod vertebrates.
Head distinct, trunk elongated. Neck and tail maybe present or absent.
Limbs usually 2 pairs (tetrapod), some limbless. Toes 4-5 (pentadactyl) or less. Paired fins absent. Median fins, if present, without fin rays.
Skin soft, moist, glandular. Pigment cells (chromatophores) present.
Exoskeleton absent. Digits clawless. Some with concealed dermal scales.
Endoskeleton mostly bony. Notochord does not persist. Skull with 2 occipital condyles.
Respiration by lungs, skin and mouth lining. Larvae with external gills which may persist in some aquatic adults.
Heart 3-chambered, 2 auricles and 1 ventricle. Sinus venosus present. Aortic arches 1-3 pairs. Renal and hepatic portal systems well developed.
Brain poorly developed. Cranial nerves 10 pairs.
Sexes separate. Male without copulatory organ. Gonoducts open into cloaca. Fertilization mostly external. Females mostly oviparous.
Development indirect.
Reptilia
Predominantly terrestrial, creeping or burrowing, mostly carnivorous, air-breathing, cold-blooded, oviparous, and tetrapodal vertebrates.
Body bilaterally symmetrical and divisible into 4 regions: head, neck, trunk, and tail.
Limbs 2 pairs, pentadactyl. Digits provided with horny claws. However, limbs absent in a few lizards and all snakes.
Exoskeleton of horny epidermal scales, shields, plates, and scutes.
Skin dry, cornified and devoid of glands.
Endoskeleton bony. Skull with one occipital condyle (monocondylar). A characteristic t-shaped interclavicle present.
Heart usually 3 chambered/partially 4 chambered, 4 chambered in crocodiles. Sinus venosus reduced. 2 systematic arches present. RBC oval and nucleated. Cold-blooded.
Respiration by lungs throughout life.
Brain with better development of cerebrum than in Amphibia. Cranial nerves 12 pairs.
Sexes separate. male usually with muscular copulatory organ.
Parental care usually absent.
Aves
Feather-clad, air-breathing, warm-blooded, oviparous, bipedal, flying vertebrates.
Limbs are two paired. Forelimbs are modified as wings for flying. Hindlimbs are large and variously adapted for walking, running, scratching, perching, food capture, swimming, or wading.
Pectoral muscles of flight are well developed.
Endoskeleton fully ossified, light but strong and without epiphyes. Long bones pneumatic or hollow and have no marrow. Usually, there is a fusion of bones.
Heart completely 4 chambered. There is neither sinus venosus nor truncus arteriosus. Only right aortic arch persists in adult. Renal portal system vestigial. RBCs nucleated.
Birds are the first vertebrates to have warm blood. Body temp. is regulated.
Respiration by compact, spongy, non-distensible lungs continuous with thin-walled air-sacs.
Brain large but smooth. Cerebrum, cerebellum, and optic loves greatly developed. Cranial nerves 12 pairs.
Sexes separate. Sexual dimorphism often well marked.
Parental care well marked.
Mammalia
Hair-clad, terrestrial, air-breathing, mostly warm-blooded, viviparous, tetrapod vertebrates.
Body distinctly divisible into head, neck, trunk, and tail.
Respiration always by lungs (pulmonary). Glottis protected by a fleshy and cartilaginous epiglottis. Larynx contains vocal cords.
Heart 4 chambered with double circulation. Only the left aortic arch present. Renal portal system absent. RBCs small, circular, and non-nucleated. Body temperature regulated.
Brain highly evolved. Both cerebrum and cerebellum large and convoluted. Optic lobes small and 4 in number. Corpus callosum present connecting both cerebral hemispheres. Cranial nerves 12 pairs.
Sexes separate. Sexual dimorphism generally well marked. Male has an erectile copulatory organ or penis. Testes commonly found in a bag or scrotum outside the abdomen. Eggs are small, with little yolk and no shell.
Fertilization internal, preceded by copulation.
After birth, young nourished by milk secreted from mammary glands of mother.
Parental care well-developed reaching its climax in humans.
Mammals show greatest intelligence among all animals.
1 note
·
View note
Text
Neurology
I had a preceptorship with a neurologist, and it was awesome! We saw four patients in three hours, and it didn't feel rushed at all. The neurologist also did a lot of procedures on these patients, from outpatient nerve blocks to the EMG setup he had right in his office.
One patient in particular had a strange numbness in one of his feet, and through a complete history and a full hour of EMG testing, we figured out that it was a very strange presentation of sciatic nerve compression, which was so interesting.
The one big takeaway for me was that when you he did the myotome portion of his neuro exam, he pushed with all his might until he actually overcame the patient's strength (impressive especially when your patient is a lot bigger than you are). He said that because many doctors shy away from doing this, slight weaknesses and asymmetry can go unnoticed, meaning a worse prognosis when they finally present to a neurologist.
I really like neuro because a lot of it is like a puzzle. All the symptoms are coming from one place and you have to figure out where. Now especially with all the procedures I saw available to outpatient neurologists, it's definitely on my list.
25 notes
·
View notes
Photo

A myotome is a group of muscles which are innervated by a single spinal nerve which has derived from the same embryological segment. In this way, it is described as the motor equivalent of a dermatome, which is an area of skin innervated by a single spinal nerve. Individual muscles can be innervated by more than one nerve or by a nerve which originates from multiple spinal nerves. Therefore, muscles can be made up of more than one myotome. For example, the quadriceps femoris muscle is innervated by the femoral nerve. The femoral nerve arises from the lumbar plexus and has its origins from L2-L4. Therefore the quadriceps femoris muscle is a part of the L2, L3, and L4 myotomes. The main function of the quadriceps femoris muscle is to extend the leg at the knee joint so this movement can be used to test L2-L4 myotomes. The femoral nerve also innervates the iliacus, pectineus, and sartorius muscles. Therefore all of these muscles, including the quadriceps femoris muscle, are part of the L2-L4 myotomes Credit @physiotherapyscape ⚠️ Disclaimer: this is for informational purpose only; not medical advice; if you have pain or functional limitations, seek a medical professional Make yourself a priority, invest in your health, book online at Brisbane Massage Therapy www.brisbanemassagetherapy.com.au #brisbanemassagetherapy #brisbaneremedialmassage #brisbanemassage #remedialmassage #physiotherapy #physicaltherapy #fitness #physio #rehab #health #exercise #chiropractic #mobility #workout #athlete #strength #physicaltherapist #movement #yoga #crossfit #massagetherapy #chiropractor #pt #physiotherapist (at Brisbane Massage Therapy) https://www.instagram.com/p/CiL6wI6J0pJ/?igshid=NGJjMDIxMWI=
#brisbanemassagetherapy#brisbaneremedialmassage#brisbanemassage#remedialmassage#physiotherapy#physicaltherapy#fitness#physio#rehab#health#exercise#chiropractic#mobility#workout#athlete#strength#physicaltherapist#movement#yoga#crossfit#massagetherapy#chiropractor#pt#physiotherapist
0 notes
Photo

Finally I got round to making this post! I thought this might be helpful to all those who are studying physiotherapy, these are by no means the best books for PT out there I just found them really useful in both first and second year. I would recommend maybe checking these books out in the library first before buying them to see if you like them. I’ll sorta give an overview of each book and why I found it useful so you guys can sort of get a feel on what’s good about it. Also I’ll link where you can buy it on amazon, but you can get it on second hand book websites or eBay for possibly cheaper.
Everything will be under the cut so this post isn't hella long on people’s dash
1. The physiotherapist’s pocketbook
Good: SO MUCH INFORMATION! It has info on dermatomes/myotomes, the origin/insertion of all the main muscles, normal levels of obs, common drugs used and so much more.Small which means it can fit inside the pocket of your tunic quite easily so you can carry it wherever you go on placement.
Bad:
Only ‘bad’ thing I can really say about this book is that it is a little on the pricey side considering how small it is, but in my opinion it is worth the money because for placement it literally has everything you can possibly need.
2. Principles of neuromusculoskeletal examination and assessment
Good: This book is very detailed when it comes to the assessment of the different joints of the body. It has the general subjective and objective assessment but then it also has separate chapters going into more detail on each joint so highly useful for specific special tests on the joint and how you perform them
Bad: I found it was very repetitive in each section and when I read it I have to sort of just skim read the pages because I get bored reading the same thing again and again. So I have to flick through a lot of pages and read a lot of the things I read in the first section before I get to what I really am looking for I guess
3. Principles of anatomy and physiology
Good: I actually only mainly used this in first year because thats when our anatomy and physiology exams were. Out of all the books this to me was the easiest to follow and understand, has your standard anatomy and physiology no different to other textbooks it was just the layout I preferred
Bad: It has the same info as other books as expected, sometimes it wasn't as detailed in certain sections so I had to look for other books which was kinda a hassle but no single book is perfect so I did use this with other anatomy and physiology textbooks too but this was the main one I found myself using
4. Joint structure and function
*side note that I actually used the 3rd edition and preferred that edition
Good: I used this book when the principles of anatomy and physiology didn't have enough information on the biomechanics of a joint e.g. scapulohumeral rhythm. I found that this book really explained concepts clearly enough for me to understand, the 3rd edition had black and white drawings which I found super useful
Bad: As any other book, some sections I found way tooo long to read and sometimes I just wanted them to get to the point haha but also it is kinda just filled with words not too many diagrams so if you don't learn like that then I'm not sure if this book is for you
So those were the main 4 books that I mainly used last year, obviously I did use other textbooks depending on the topic I was studying but for general information I used the books above, I’ll link other books below that I didn't necessarily use a lot but I used sometimes and they were good/books my course mates used
Honourable mentions:
Tidy’s physiotherapy - I didn't use this a lot but it is a good alternative to book 2 and my friends have preferred this over that book because it is easier to follow they said. But I haven't used it enough to give a thorough opinion on it
Concise book of muscles - I really only used this in first year when I needed to learn origin and insertion of the muscles but it is very accurate and has very good images of the muscles
Gray’s anatomy flashcards - Now I never actually bought these because I personally felt I didn't need them but one of my friends did buy these and loved them as they are very detailed and are a good way to learn your anatomy. I have heard there are other cheaper alternative to these flashcards so I’d recommend looking around first
The anatomy colouring book - Again I don't actually own this book (I own an alternative book) but this is the colouring book most people find the best out of all of them, so if you learn like this then I’d recommend having a look at this as I do know it is detailed and a good learning resource
So those are the books! Sorry for the hella long post, I thought I would at least make it a little detailed so you guys have an idea on what they were good for/not so good for. Hopefully this was helpful to some of you since when I started my course I was stuck on the kind of books that were good, check if your course has a reading list as that is always a good place to start. If you have any other questions on particular books or other books I used then feel free to hit me a message!
#studying#studyspo#study#student#studyblr#studyspiration#university#notes#textbooks#anatomy#physiology#physiotherapy student#physiotherapy#my own post#study notes#studysthetics#anatomy notes#my own
4 notes
·
View notes
Text
Stuff I Learned: Ortho Seminar
October 31, 2017: You Can’t Afford to Wait
Treatment of open fractures
Antibiotics + anti-tetanus toxoid
Soft tissue debridement (second look on Day 2-3)
Bony compartment: external fixation
Life-saving > limb-saving > function-saving
Limb threatening injures: open fractures, compartment syndrome, vascular injury, dislocation of major joints
FAST has largely been replaced by rapid CT
Compartment pressure measurement: digital manometer or syringe + manometer
November 2, 2017: Foot and Ankle Disorders
Arch of foot is maintained by plantar fascia
In plantar fasciitis, the tender spot is the medial aspect of the calcaneal bone
The navicular tubercle is the attachment of the tibialis posterior tendone, the dynamic control factor of the arch
Tibialis posterior dysfunction leads to adult flat foot
Unlike calcaneal fracture, medial/lateral malleolar fractures are low energy
Ankle sprains are most commonly inward, affecting the anterior talofibular ligament (ATFL) and calcaneo-fibular ligament (CFL); usually the posterior talofibular ligament (PTFL) is not affected
November 4, 2017: Peripheral Neuropaties
Cubitus valgus deformity stretches the ulnar nerve
Osteoarthritis causes compressive neuropathy by osteophyte formation or deformity
Surgical management is by anterior transposition; post-operative mortality is worse if symptomatic for > 1.5 years
November 11, 2017: Lower Back Pain
Myotome with exclusive L5 innervation: big toe dorsiflexion and hip abduction
Deformities due to back pain: loss of lumbar lordosis, listing
Prolapsed intervertebral disk causes pain during forward flexion of the spine (unlike spinal stenosis)
Consider for surgery in disk prolapse if there is still pain after conservative treatment for 6 weeks
MRI: TR few hundred = T1, few thousand = T2
Straight leg raising test positive on contralateral side = cross sciatica
November 11, 2017: Arthritis
Ficat classification of AVN
Stage I: normal
Stage II: subchondral sclerosis
Stage III: subchondral collapse, crescent sign
Stage IV: secondary OA
DDx finger drop in RA
Radial nerve palsy (posterior interosseous nerve)
Extensor tendon rupture
Volar subluxation of MCPJ
Ulnar dislocation of extensor at MCPJ
November 21, 2017: Basic Science
T scores are used for post menopausal women and for men more than 50 years old; Z scores for pre menopausal women and for men less than 50 years old + children
DEXA looks at hip and spine
Surgical treatment of axial compression fracture: posterior instrumentation and correction of kyphosis, anterior decompression and fusion
3 column theory: flexion compression affects 1 column, axial compression affects 2
November 21, 2017: Cervical Spine Disorders
Hoffmann: disinhibition of C8
Lhermitte’s sign: a sign of C1/C2 subluxation, paresthesia upon neck flexion
Cervical myelopathy: 75% episodic progression, 20% steady progression, 5% rapid deterioration
Oblique XR to look at neural foramina
Cervical radiculopathy: 80% recover completely with conservative treatment
Causes of cervical myelopathy: spondylosis, PID, instability
OPLL = ossified posterior longitudinal ligament (more common in Asian, obesity)
November 25, 2017: Common Shoulder Problems
Most common bone involved in osteoporosis of shoulder: neck of humerus (surgical)
Ligament will not lead to chronic pain of shoulder but labrum will (anterior, posterior, superior, inferior): apprehension for anterior, superior lead to chronic pain
Frozen shoulder stages: freezing (inflammatory), frozen, thawing
Combing hair (shoulder movement): flexion, abduction (front only), external rotation (back)
Wearing coat: external rotation
November 25, 2017: Common Knee Problems
ACL is intra articular and MCL is extra articular; ACL will swell immediately after trauma; MCL delayed
Immediate swelling of knee DDx
ACL tear (72%)
Osteochondral fracture (14%)
Patellar dislocation (6%)
The meniscus is avascular, aneural, and alymphatic
To prevent DVT, must exercise gastrosoleus
Majority of knee location is after a high energy trauma and majority will reduce, leaving no trace on XR
Knee dislocation = Grade 3 laxity in collateral ligament + cruciate ligament
November 27, 2017: Common Orthopedic Problems
Injection of steroid into tendon sheath = high risk of tendon rupture
Trigger finger is due to inflammation of the flexor tendon leading to narrowing of tendon sheath, therefore stuck at A1 pulley region at the MCPJ of 3rd or 4th digit
Mallet finger: caused by acute forced flexion of extended digit
Wall test: ask patient to lean against wall on back and touch wall on other points of the body to check for ankylosing spondylitis
Why spine fracture in AS patient won’t heal: abnormal curvature, stiff joint
November 27, 2017: Hand Injuries
Principles of fracture management
Reduce if necessary
Immobilize if necessary
Always rehabilitate
Nerve entrapment: if there is muscle atrophy, it is advanced; do not manage conservatively
Tinel sign: tap from distal to proximal
Froment’s sign: adductor pollicis paralysis due to ulnar nerve palsy; patient uses flexion via median nerve to compensate when asked addut thumb
November 30, 2017: Common Hip Disorders
Shenton’s line is broken in any disruption of the normal intracapsular anatomy (e.g. hip location, DDH)
Blood supply to the femoral head is retrograde = distal to proximal
AVN treatment
Ficat I-II: core decompression
Ficat II-III: vascular bone graft
Ficat IV: total hip replacement
Joint aspirate cell count
Normal: < 200
Septic arthritis: 80,000 to 200,000
Joint aspiration: anterior approach to avoid femoral blood supply, causing iatrogenic AVN
XR of AVN vs simple hip OA: unilateral, joint space initially preserved, collapsed femoral head
November 30, 2017: Childhood Injuries
Children’s bones are less dense, more porotic, more vascular with a thicker periosteum: form callus quicker
Capitulum always articulates with the radius
Children: physis not ossified, so a fracture on XR may look like a dislocation
Elbow dislocation is RARE! Consider physeal fracture
Physeal fracture: if germinal zone is damaged there is growth retardation/arrest
Supracondylar fractures occur around 6-7 years old
Type I: undisplaced
Type II: displaced, posterior cortex contact
Type III: displaced, no cortical contact (extension type)
November 30, 2017: They are too important to miss
Fracture stages: hematoma, inflammation, callus formation, lamellar consolidation, bone remodeling
Callus formation happens at around 3-6 weeks
Osteosarcoma: metaphysis most commonly affected
Osteosarcoma radiographic features
Codman’s triangle (due to periosteal elevation, early, not specific)
Sunburst appearnace (specific, late)
In children, hematogenous osteomyelitis occurs in the metaphysis since the blood vessel loops back the avascular cartilage, resulting in slower flow; in adults , who do not have metaphysis, it is septic arthritis
Codman’s triangle DDx: tumor, trauma, infection, hematoma
Acetabular fractures are high energy
December 12, 2017: Common Pediatric Problems
Breech presentation in the 3rd trimester is the single most important risk factor for DDH: increase risk by 10-15x
Ossificaiton of bone occurs at around 5-6 months for boys and 4-5 months for girls
Ultrasound is oversensitive, leading to many false positives
Acetabular index angle > 30 degrees is abnormal
Pavlik harness carries at 1% risk of AVN
Perthes is a self-limiting condition with onset between 4 and 8, but the outcome is variable depending on the extent of the collapse
Gold standard treatment for talipes equinovarus is non-operative
2 notes
·
View notes
Text
My patient: Radicular L. Back Pain
My patient “Rad” has been coming to the clinic for about 4 weeks now with complaints of low back pain and radicular symptoms into the right thigh, right medial foot, and slightly into the right calf.
My patient has lordosis of the lumbar spine and significant kyphosis of the thoracic spine. The patient is active and wants to return to activities like swimming, walking long distances, and simply standing for long periods of time without having symptoms in the right leg.
The primary complaint is numbness and tingling in the medial right calf and foot. The patient also has some numbness and tingling into the lateral thigh which occurs less frequently, but can cause the patient discomfort from time to time. All of his symptoms are aggrivated with long periods of standing, walking, and swimming. He does not feel pain, but simply notes a discomfort disscribed as a constant part of his thigh or foot “falling asleep”.
As student physical therapist, it is my challenge to remedy this patients condition to the best of my abilities. This has lead me to find the best evidence for how I can help. You can follow along!
Up until now, I have focused on manual therapy techniques to relieve pain and improve the biomechanics around the joint segments of his L4-5 lumbar segments on the right which show significant muscle guarding and stiffness. At this current clinic, gaining mobility in the spine is encouraged with extension press ups. The patient has seen improvements with the combination of press up extensions and manual therapy.
Breifly looking at some pictures of dermatomal and peripheral nerve patterns, we can take a look at my clinical reasoning to determine that the patients symptoms are not distal to the spinal nerves of the lumbar spine. Or at least, the majority of the symptoms origin from a more proximal location along the nerves exiting the lumbar spine.
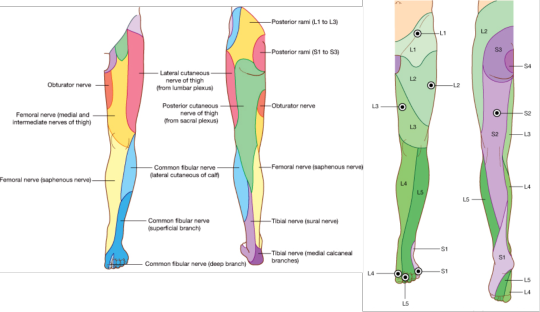
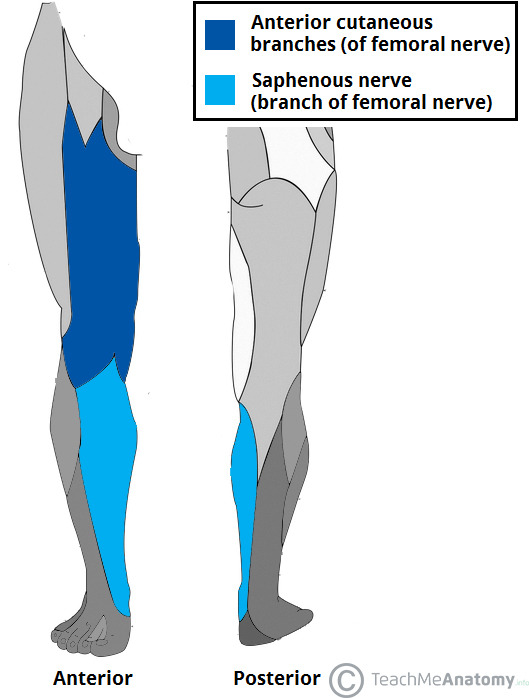
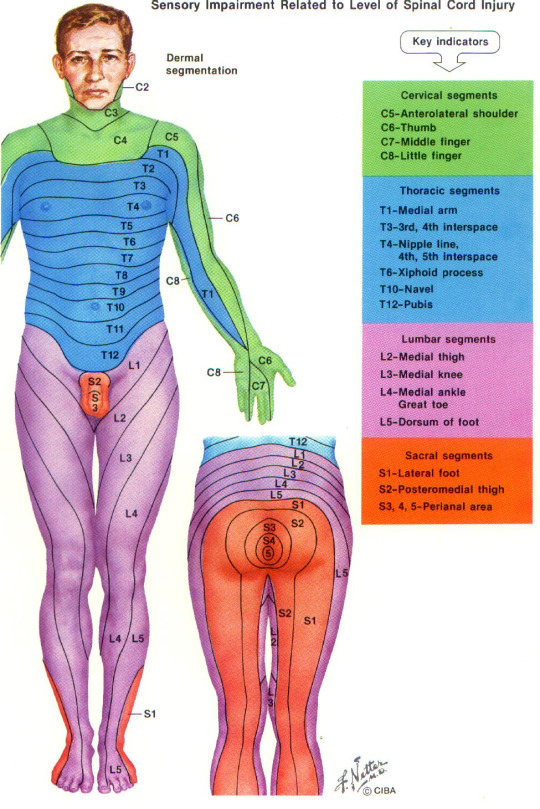
Looking at these diagrams, you can observe my reasoning for proximal nerve compression involving spinal nerve roots instead of more distally located compression. Distal compression of the nerve may indeed be present, however, the primary symptoms follow a sensory pattern that indicates possibility of L3, L4 involvement on the right side.
So is there muscular involvement? Myotome testing is negative. However, there is noted weakness of the right gluteus maximus and medius muscles compared to the left side. The innervation for these muscles involves the superior gluteal nerve with spinal innervation involvement of L4,5,S1.
When performing slump tests, streight leg raise with tibial nerve bias, and femoral nerve tension tests, the patient has noted positive symptom aggrivation. The symptoms were especially aggravated in the medial foot with a tibial nerve bias straight leg raise.
So this gives you some idea of the presentation of my patient. I am on a quest to determine if nerve mobilization to nerves containing (L2, L3 due to some discrepancy on the pattern of these nerves in the thigh), L4, L5 nerve roots will improve patient symptoms in the foot and lateral thigh.
I am researching an article: Effectiveness of neural mobilization in patients with spinal radiculopathy: A critical review
3 notes
·
View notes