#postnatal depression and covid
Text
"Three years into the pandemic, with the removal of almost all mitigation measures in most countries, it's clear the virus has hit the world very hard. So far, almost 681 million infections and more than 6.8 million deaths have been reported.
This is perhaps best visualised by its impact on life expectancy. There were sharp declines seen across the world in 2020 and 2021, reversing 70 years of largely uninterrupted progress.
The excess mortality driving this drop in life expectancy has continued. This includes in Australia, where over 20,000 more lives than the historical average are estimated to have been lost in 2022."...
"The indirect impacts on the health systems in rich and poor countries alike continue to be substantial. Disruptions to health services have led to increases in stillbirths, maternal mortality and postnatal depression.
Routine child immunisation coverage has decreased. Crucial malaria, tuberculosis and HIV programs have been disrupted.
A paper out this week highlights the severe impact of the pandemic on mental health globally.
Meanwhile, more evidence of long COVID has emerged around the world. At least 65 million people were estimated to be experiencing this debilitating syndrome by the end of 2022.
The Australian Institute of Health and Welfare estimates 5-10 per cent of people who are infected with SARS-CoV-2 will develop long COVID, with symptoms persisting for more than three months.
That's between 550,000 and 1.1 million Australians, based on the more than 11 million cases reported so far."...
"We cannot assume there will be a natural exit to the pandemic, where the virus reaches some benign endemicity, a harmless presence in the background.
In fact, there is little indication anything like that is imminent.
In Australia, since the beginning of January, more than 235,000 COVID cases have been reported, almost as many as in 2020 and 2021 combined. Since the start of January, there have been 2,351 COVID-related deaths, more than twice as many as in the whole of 2020 and around the same as in the whole of 2021."...
"As we enter the fourth year of the pandemic, we must not leave it up to the virus to fix itself.
The biggest lesson of the past three years is there's little chance that is going to work, at least without an intolerably high cost.
Rather, we can end the pandemic by choice. We know what to do. But we are simply not doing it."
91 notes
·
View notes
Text
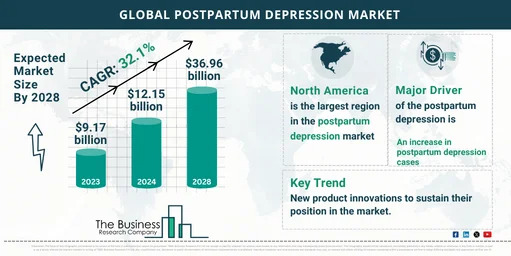
Understanding Market Size, Share, and Forecast for Postpartum Depression Treatment
Overview and Scope
Postpartum depression (PPD) refers to a condition, which is a type of mood disorder that affects some women after giving birth and can remain undiagnosed for long periods of time. It is characterized by feelings of sadness, hopelessness and a lack of interest or pleasure in once-enjoyable activities.
Sizing and Forecast
The postpartum depression market size has grown exponentially in recent years. It will grow from $9.17 billion in 2023 to $12.15 billion in 2024 at a compound annual growth rate (CAGR) of 32.5%. The postpartum depression market size is expected to see exponential growth in the next few years. It will grow to $36.96 billion in 2028 at a compound annual growth rate (CAGR) of 32.1%.
To access more details regarding this report, visit the link:
https://www.thebusinessresearchcompany.com/report/postpartum-depression-global-market-report
Segmentation & Regional Insights
The postpartum depression market covered in this report is segmented –
1) By Types: Postpartum Blues; Postpartum Anxiety; Postpartum Obsessive Compulsive Disorder; Postpartum Panic Disorder; Postpartum Post-Traumatic Stress Disorder; Postpartum Psychosis; Other Types
2) By Treatment: Psychotherapy; Medication; Supplements; Other Treatments
3) By Route of Administration: Oral; Parenteral; Other Route Of Administration
4) By Distribution Channel: Hospital Pharmacy; Retail Pharmacy; Online Pharmacy; Other Distribution Channels
5) End-Users: Hospitals; Specialty Clinics; Homecare; Other End-Users
North America was the largest region in the postpartum depression market in 2023. The regions covered in postpartum depression market report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East and Africa.
Intrigued to explore the contents? Secure your hands-on sample copy of the report:
https://www.thebusinessresearchcompany.com/sample.aspx?id=13024&type=smp
Major Driver Impacting Market Growth
An increase in postpartum depression cases is expected to propel the growth of the postpartum depression market going forward. Postpartum depression is an exaggerated worry that develops after giving birth. There may be physical symptoms in addition to it. Postnatal depression and postpartum anxiety frequently coexist and in the first year after giving birth, symptoms might start at any time. Postpartum depression is frequently treated with psychotherapy, commonly known as talk therapy or mental health counseling, medication, or a combination of the two, which results in the growth of the market.
Key Industry Players
Major players in the postpartum depression market are Pfizer Inc., Johnson & Johnson, Roche Holding AG, Merck & Co., AbbVie Inc., Novartis AG, Sanofi SA, Bristol Myers Squibb Co., Sage Therapeutics Inc.
The postpartum depression market report table of contents includes:
1. Executive Summary
2. Market Characteristics
3. Market Trends And Strategies
4. Impact Of COVID-19
5. Market Size And Growth
6. Segmentation
7. Regional And Country Analysis
.
.
.
27. Competitive Landscape And Company Profiles
28. Key Mergers And Acquisitions
29. Future Outlook and Potential Analysis
Explore the trending research reports from TBRC:
Mental Health Apps Global Market Report 2024
Behavioral and Mental Health Software Global Market Report 2024
Residential Substance Abuse And Mental Health Facilities Global Market Report 2024
Contact Us:
The Business Research Company
Europe: +44 207 1930 708
Asia: +91 88972 63534
Americas: +1 315 623 0293
Email: [email protected]
Follow Us On:
LinkedIn: https://in.linkedin.com/company/the-business-research-company
Twitter: https://twitter.com/tbrc_info
Facebook: https://www.facebook.com/TheBusinessResearchCompany
YouTube: https://www.youtube.com/channel/UC24_fI0rV8cR5DxlCpgmyFQ
Blog: https://blog.tbrc.info/
Healthcare Blog: https://healthcareresearchreports.com/
Global Market Model: https://www.thebusinessresearchcompany.com/global-market-model
0 notes
Text
توصلت دراسة عن الاغلاق إلى وجود أزمة صحية عقلية غير مشخصة بين الأمهات الجدد
توصلت دراسة عن الاغلاق إلى وجود أزمة صحية عقلية غير مشخصة بين الأمهات الجدد
Shutterstock
فيكي فالون، جامعة ليفربول؛ سيرجيو أ. سيلفيريو, كينجز كوليدج لندن, وسيان ماكلويد ديفيز, جامعة جون مورز ليفربول
لقد أظهر بحثنا الجديد أن الأمهات الجدد عانين من معدلات عالية وبشكل مثير للقلق من الاكتئاب والقلق خلال الإغلاق الأول. وكان أحد العوامل الرئيسية التي ساهمت في شعورهم بهذه الطريقة هو التأثير النفسي لتدابير التباعد الاجتماعي.
فقد فحصت دراستناالتجارب النفسية والاجتماعية لأكثر من…

View On WordPress
#corepaedianews#Postnatal depression#New mothers#lockdown#depression#social distancing#Mental health#Anxiety#Postnatal#Coronavirus insights#كوربيديا#كوربيديا للاخبار#Coronavirus UK#Corepaedia#Covid-19
0 notes
Text
Post-natal depression has increased during the ongoing pandemic, says study
Post-natal depression has increased during the ongoing pandemic, says study
[ad_1]
By: Lifestyle Desk | New Delhi |
Published: July 1, 2020 9:40:19 pm


The ongoing pandemic has had an adverse effect on mental health. (Source: Getty Images)
Mental health has been a serious concern during the ongoing pandemicand new research suggests that postnatal depression has increased by three times. The study,…
View On WordPress
#indian express#indian express news#postnatal depression#postnatal depression during covid#pregnant women#pregnant women depression
0 notes
Text
Thousands of pregnant women in England were denied vital help for their mental health because of the pandemic, analysis from leading psychiatrists shows.
In 2020-21, 47,000 were expected to access perinatal mental health services to help with conditions such as anxiety and depression during or after giving birth, but only 31,261 managed to get help in the most recent data for the 2020 calendar year only, according to analysis from the Royal College of Psychiatrists.
Up to one in five women have perinatal mental health problems, such as depression, anxiety and other conditions occurring during pregnancy or in the first year after the birth of a child.
The Royal College of Psychiatrists found that the pandemic was not the sole reason the mental health of thousands of women was overlooked. Variation in care across the country due to lack of local investment in perinatal mental health services meant that in many areas in England pregnant women and new others cannot get support.
Trudi Seneviratne, a registrar of the Royal College of Psychiatrists, said: “Staff in perinatal mental healthcare have made every effort to support women in these extremely challenging times but services have been under unprecedented strain. Funding for mental health facilities is long overdue but is more urgent in the face of the Covid-19 pandemic.”
Vicki Nash, head of policy, campaigns and public affairs at Mind, said the findings were “deeply concerning”.
“More broadly, women are among several groups that have borne the brunt of the Covid crisis with many juggling caring roles with working and home schooling, leading to a deterioration in women’s mental wellbeing,” she said.
The Royal College of Psychiatrists is calling for funding in the next spending review. Psychiatrists are also calling on local health bosses in certain areas to address longstanding funding issues.
Perinatal mental health support was broadly on track before the pandemic. In 2019-20, 30,625 women accessed perinatal mental health services, against the expectation of 32,000 outlined in the NHS long term plan.
In all local areas in England, at least 7.1% of pregnant women and new mothers are expected to need support from mental health services. North central London is the worst performing area in the country with just 150 out of 1,521 pregnant women or new mothers expected to access specialist support, managing to get it.
Leanne Howlett, 34, experienced postnatal depression after her first child was born five years ago and had similar problems when her baby daughter was born in 2019. However, this time as she was struggling with her mental health and her daughter turned five-months-old, the pandemic also struck.
“Before coronavirus I had a nurse coming to see me weekly at home and a psychiatrist appointment, and then overnight all these face-to-face meetings switched to phone calls,” Howelett said, adding that it was harder to talk about big issues such as having suicidal thoughts remotely.
She also lost the support of friends and family, and her son could no longer go into nursery, leaving her feeling alone. “Suddenly l felt really on my own with it all, even though support was there, it was not the same.”
Howlett said she worried that services would now permanently move to being provided via telephone calls, saying more funding was needed. She also worries about cuts to health visitors, noting that it is often during these appointments that mothers “reach out” and “ask for help”.
“It is at the weighing clinic [when the baby is weighed after birth] that women reach out. I would not have picked up a phone to get help and if there is no weighing clinics then new mothers are not seeing professionals face to face after having baby,” she added.
An NHS spokesperson said: “We have already ensured that there is a specialist perinatal mental health service everywhere in the country, and as part of our Long Term Plan will continue to expand, so that at least 66,000 women will be able to access specialist care every year by 2023-24.
“This expansion includes the recently-announced hubs bringing together maternity services, reproductive health, and psychological therapy under one roof for women who have mental health needs as a result of their maternity experience.”
6 notes
·
View notes
Note
Hello, Wishing you a glorious Sunday.
I have finished your nanny affair fanfiction. I adored it. I have began your Bridesmaids fiction I am captured by it.
Please I ask questions from NSFW ABC, fanfiction writers and a couple of my own questions and NSFW ABC for The Bridesmaids.
NSFW= F. M. T. U. Fanfiction writers= 4. 13. 26. 28. My ques= How do you picture Harry. Layla. Nicki. Remy. Alec? Do you think Laila is scared to love or to be loved? I see elements where it looks like they love each other but they seem to scared to say the word. Are Layla and Harry going to tell everyone soon? I would love it if Layla asked Harry to be her boyfriend.
Kind regards
Shy fan
Hi morning Shy fan,
Aww thanks hope you are having a fab day! 😊 Wow! This has to be the biggest ask I've had 🤣🤣 I'm glad you liked my TNA series and ATB has you hooked.
NSFW answers
F - Favourite position.
This is possibly the most boring answer ever, so I'm sorry! 🤦♀️ In the first scene where they DTD Laila admits she hasn't EVER climax in the missionary position until she meet Harry so I'm just guessing maybe this is her new favourite position.
M - Motivation.
I think just each other's touch turns them on especially Laila she hadn't have anyone touch her in that way for 8 years! 🤣🤣 but if I really had to think about it I suppose Harry kissing her neck gets her all hot and bothered.
T - Toys.
I don't think toys are off limits I think that would be something they would both be interested in but they have only just started getting intimate with each other. It will probably be something their explore soon.
U - Unfair.
In previous chapter we have seen they like to tease each other quite a bit. The gym shower scene comes to mind 😈😈😈 sorry if you haven't gotten that far yet.
Fanfic writers answers
4. Are there any writers that inspire you?
Yes, there are I'm just going to list a few of them! Because their work is amazing if you haven't already check it out.
@secretaryunpaid @khoicesbyk @aussieez @txemrn @lem-20 @shewillreadyou @irisofpurple @lifeaskim @thefrenchiemama
13. First fandom I wrote for?
This question depends if you mean published or unpublished? Unpublished was my first Adam and Ellie series it was sat in my drafts for 10 months it wasn't until after I wrote and published my TNA FF that I finally published A&E.
26. Is there anything you've wanted to write, but you've been to scared to try?
There is a couple actually I would love to do an Open Heart One Shot but I read the OH FF on here I could never do it justice it deserves or get Ethan down to a T like the talented writers on here.
The second was something I WAS scared to write about but now I have done it now and received such amazing comments about it, so now I'm no longer scared. This is my Alone A&E series with touches the subject of postnatal depression which I went through with my smallest baby.
28. How well do you handle criticism when it comes to your writing?
I didn't handle it well a few weeks ago when I was sent Anon hate. But I have recently realised to only listen to criticism from people who don't hide behind Anon HATE. As it take a lot more courage to criticise with them knowing who you are! 😘
Your Questions
How do I picture Laila, Harry, Nikki, Remy and Alec?
Laila and Harry I'd like to keep it to myself how I picture them because I think the readers have their own Harry and Laila in their minds. Nikki? Well, she is base on a friend I have. We don't always talk and with covid we haven't been able to meet up but before when we got together our hubby's would shake their heads knowing we were going to get into some kinda trouble. I will say she's blonde 👱♀️but that's it. As for Remy and Alec I picture them like this from Shadow Hunters like Jace in my TNA FF -------->

Do you think Laila is scared to love or be loved?
I think it a little of both if you remember in the Meet the characters chapter her first BF cheated on her....then Josh her fiancé well he died but you find out a lot more about that in the next chapter and it will reveal reasons why she is so scared to love again.....! But I am glad you can see a hint that they do love each other this is what I was aiming for 🥰
Are Laila and Harry going tell everyone soon?
I'm guessing you mean their families as their best friends know already. I think they will but maybe once they make it official as it is a big thing especially to Laila who hasn't had a BF in 8 years.
As for Laila asking Harry to be her boyfriend?
I think that's a genius idea I think it would show him that she's ready for this to be serious and we are in 2021 right! Why not!! 😉
This has been so much fun so thanks Shy Fan hopefully soon you'll reveal who you are 😘
11 notes
·
View notes
Text
*TRIGGER WARNING*
Update.
Hello lovely followers. Thank you for all of your kind messages, I have now responded to them individually and privately. I’ve written a little update for those of you who are interested.
Since last time I posted, things have got worse- much worse.
I continued to engage with the CRHTT but it was felt that I needed more support than they could offer in the community, so I was asked if I wanted to go to an inpatient mother and baby unit (MBU). I declined, until they threatened to section me, so I went in voluntarily.
I was placed in an isolation room and tested for COVID-19, then moved to the main ward once that came back negative. I was on Level 3 (one-to-one) observations.
Although the majority of the staff are wonderful, and it’s a very nice ward, I no longer wanted to stay here and was put on a temporary section when I insisted on leaving. I was then assessed and placed on a section 2.
The suicidal thoughts persisted and when I was downgraded to less intrusive observations I attempted to end my life. Clearly I failed. The staff who found me were absolutely lovely to me, bless them, which somehow made me feel worse. I was taken to the closest A&E and had both internal stitches and surface stitches on my neck. The doctor who treated me said I was extremely lucky that I didn’t hit my carotid artery. Since that was my plan, I certainly didn’t feel lucky.
I was placed on Level 3 observations again.
Today I had a review with the doctor and my core team here on the ward, which I hadn’t been looking forward to but it wasn’t as bad as I had expected.
The consultant thinks I have developed postnatal depression and is taking me off the antidepressant (sertraline) the community psychiatrist prescribed and I’m going to try mirtazapine instead. He thinks this may help with my sleep also.
As for Ezra, the staff are brilliant with him, he’s loving all the groups and activities, he’s learnt to crawl, is trying new foods, has another tooth coming, and has been pulling himself into standing position. I continue to be amazed every single day.
So that’s where things are at the moment.
Would love to receive some post or something, if anyone could be so kind as to send me something please inbox me for the address.
Hope all my fab followers are well and are doing better than I am at the moment.
Stay golden x
@finding-mollies-marbles
#mental health#recovery#mental illness#schizophrenia#paranoid schizophrenia#inpatient#mbu#postnatal depression#depression#medication#clozapine#aripiprazole#sertraline#mirtazapine#psych ward#mental hospital#trigger warning#trigger#warning
9 notes
·
View notes
Text
COVID-19 Hikes Depression Among New Moms
COVID-19 Hikes Depression Among New Moms
collected survey data between February and July 2020 from 670 U.S. postpartum patients who completed the Edinburgh Postnatal Depression Scale online and provided demographic information.
This study found that moms who fed infants formula had 92% greater odds of screening positive for postpartum depression and were 73% more likely to screen positive for major depressive symptoms, compared to…

View On WordPress
0 notes
Text
Study examines relationship between prenatal and postnatal stress, depression, and infant motor development during COVID
Study examines relationship between prenatal and postnatal stress, depression, and infant motor development during COVID
In a recent study posted to the Research Square* preprint server, researchers estimated the impact of antenatal and postnatal maternal mental health on the motor developments of the newborn during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic.
Ever since SARS-CoV-2 emerged in 2019, the rate of prenatal and postnatal depression and stress in pregnant women has…
View On WordPress
0 notes
Text
Lockdown study finds undiagnosed mental health crisis among new mothers
Lockdown study finds undiagnosed mental health crisis among new mothers
Shutterstock
Vicky Fallon, University of Liverpool; Sergio A. Silverio, King’s College London, and Siân Macleod Davies, Liverpool John Moores University
New mothers experienced worryingly high rates of depression and anxiety during the first lockdown, our new research has revealed. One of the major contributing factors to them feeling this way was the psychological impact of social distancing…

View On WordPress
#Anxiety#Corepaedia#corepaedianews#Coronavirus insights#Coronavirus UK#Covid-19#depression#lockdown#Mental health#New mothers#Postnatal#Postnatal depression#social distancing#كوربيديا#كوربيديا للاخبار
0 notes
Text
Students’ Mental Health During COVID-19 Pandemic


Sonny K . Gaid Jr. is a transgender woman and currently, a third year student taking up Bachelor of Science in Technology Communication Management at University of Science and Technology of Southern Philippines - CDO campus. She is an LGBTQIA+ and Trans Rights Advocate . In her free time, she enjoys watching documentaries Mental health has been a central theme during the pandemic. This blog offers insights and promotes awareness about the importance of mental health in students. Whenever you think about mental health, what would be the first thing that comes to your mind? Anxiety? Depression? Emotional Stress ? . Mental health is an essential aspect of health and wellbeing. Our psychological, emotional, and social well-being are all aspects of our mental health. It has the power to greatly change our relationship with ones self and those around us through stimulating our everyday perceptions, emotions, and habits. Taking care of our mental health is pivotal if we are to try to live a good balanced existence. “Over 60 per cent reported disruptions to mental health services for vulnerable people, including children and adolescents (72 per cent), older adults (70 per cent), and women requiring antenatal or postnatal services (61 per cent)” – World Health Organization survey. Academic institutions have faced unusual barriers and challenges as they sought to suddenly transition classes to a virtual setting, ensure fair participation for every learners, facilitate instructors’ and students’ academic requirements, and develop strategies in the midst of enormous turbulence in the context of the severe COVID-19 pandemic. The pandemic has generated a lot of anxiety, pressure, and sadness. These stimuli can lead to mental health problems for everyone, and they can aggravate adverse responses in persons who already have mental health problems.

“The challenge with mental health is that it is often hidden and you may not know who is struggling. Please take the opportunity to reach out to family, friends, colleagues and even strangers and see how they are. Together, we can strengthen our community safety net and ensure no one is left behind.”–Marc Liberati, Chairperson, UNV Staff Association Committee A research of Journal of Medical Internet, as of the 195 students, 138 (71%) indicated increased stress and anxiety due to the COVID-19 outbreak. Multiple stressors were identified that contributed to the increased levels of stress, anxiety, and depressive thoughts among students. These included fear and worry about their own health and of their loved ones (177/195, 91% reported negative impacts of the pandemic), difficulty in concentrating (173/195, 89%), disruptions to sleeping patterns (168/195, 86%), decreased social interactions due to physical distancing (167/195, 86%), and increased concerns on academic performance (159/195, 82%). To cope with stress and anxiety, participants have sought support from others and helped themselves by adopting either negative or positive coping mechanisms. (Son, C., Hegde, S., Smith, A., Wang, X. and Sasangohar, F., 2020)

The significance of mental health ought to be reiterated, specifically as humanity remains to deal with a pandemic that has caused the country to stoop down in a devastating manner. Many students all over the world are dealing with the challenges of online learning amidst of pandemic. By assisting in the implementation of comprehensive assessments, school-based mental health experts can give immediate assistance to students that might be at risk for psychological problems. Although the main objective of each education assistance is to assist all student’s developmental needs. Provided the wide range of mental health problems that students may encounter during the pandemic, academic institutions and teachers must facilitate in distinguishing at-risk students through comprehensive assessment and endorse for unified assessment of the academic institution population during virtual learning period. In addition, they must raise awareness of the significance of mental health assessment with their students.
“First and most importantly, we need to advocate against mental health stigma as people with mental health conditions still often experience severe human rights violation and discrimination. Don’t be afraid to speak up and seek assistance whenever you feel unwell or mentally distressed.” –Shalina Miah, Manager, UNV Regional Office for Asia and the Pacific
0 notes
Text
Can you run while pregnant?


If you like to keep fit, you might be wondering, can you run while pregnant? Pregnancy can be an amazing and confusing time. Your body is starting to change and you know that you have to make some other changes too. Can you still roll out your yoga mat at the local gym, use weights or sign up for a run? You know that going for a personal best might not be a good idea when you are expecting a baby, but can you still hit the treadmill in the gym or should you skip it and head for the showers?
Is it safe to run while pregnant?
While you’re not going to be hitting any personal bests, you can still pull on your training shoes. Prenatal personal trainer Tami Smith of Fit Healthy Momma told Live Science: “Unless your doctor recommends you avoid running, there is nothing wrong with keeping up with your runs during pregnancy, but you might have to modify quite a bit, especially near the end.” Although, Smith added, “If you weren’t a runner before pregnancy, chances are you should wait until after you’ve given birth to begin.”
Obstetrician-gynecologist and fitness professional Carla DiGirolamo of Boston IVF told Live Science that what you’ll be able to do is linked to your baseline level of fitness. “My recommendations for an accomplished triathlete will be different from a sedentary individual. But my general recommendation — assuming an uncomplicated pregnancy — is to stick with her current fitness level at her discretion with an awareness of any pregnancy symptoms she is having,” DiGirolamo said. She cautioned that during the second trimester when the body’s center of gravity changes, falling is a potential risk. “Another risk is pain in the pelvis as the bones begin to separate and the cartilage between the pelvic bones is more stressed,” said DiGirolamo.
Finding the right gear to support your changing body is key, said run coach and pre- and postnatal fitness specialist Christine Nichols. “I recommend that my pregnant runners get fitted for shoes mid-pregnancy as your feet can grow and your gait can change and therefore you may feel more comfortable in a different shoe or shoe size,” Nichols said. “Investing in a belly band can also be very helpful with round ligament pain, back pain and for more added support during exercise.” For more advice on running shoes, take a look at this feature on what is gait analysis?
(Image credit: Getty)
What are the benefits of running through pregnancy?
A runner’s high may be rare, but it’s clear that exercise gives pregnant women a mental boost. Researchers from the University of Alberta found that mothers-to-be who were physically active in the early days of the COVID-19 pandemic had a 30% lower chance of suffering from depression.
While a workout will help with cardiovascular health and weight management, it also comes with an added perk for moms-to-be as it helps to control blood sugar levels. “Insulin resistance worsens in pregnancy due to the production of [the hormone] human placental lactogen,” said DiGirolamo. “Movement increases the uptake of blood glucose by the muscles, thereby helping to maintain healthy blood glucose levels.”
(Image credit: Getty)
Which exercises should you avoid while pregnant?
Prenatal trainer Tami Smith said that safe and effective exercises for the first trimester include walking, jogging, cycling, resistance training (squats, lunges, bicep curls), yoga and Pilates. Morning sickness may curb some plans, so the key is to listen to your body. “I highly recommend lots of walking and at least three days per week of strength training as you’re going to need a strong, capable lower body to deliver your baby and support your pregnancy weight,” said Smith. “Avoid intense jarring movements or engaging in activities that put you at risk for falling or getting injured.”
The second trimester should be similar in terms of exercise, but with the main precaution being that it’s recommended that you not lie flat on your back after about 20 weeks of pregnancy. “During this trimester, your belly will likely start to ‘pop’ so it’s important to be aware of things like where you’re resting weights (avoid the pelvic area and belly for things like hip thrusts),” said Smith. “Many pregnant women, especially as they near the end of their second trimester, find that they need to scale their exercise back a bit. This can look like lowering weight selection or scaling back the intensity of running.”
For the third trimester, if you’re experiencing a normal, healthy pregnancy, you can stick with your regular workouts with modifications. “You should never ‘push through’ any kind of pain or discomfort,” said Smith. “If you wake up feeling sore and overly tired, it might not be the best day to hit the gym for a lifting session. Instead, a long, leisurely walk can be just what your body needs. Your physical fitness before and during pregnancy will determine how much you can do in your third trimester.”
Prenatal fitness specialist Christine Nichols confirms that there is no hard and fast rule and what you can do throughout pregnancy depends on the individual. “Some women will be able to continue running, others will not, some women will be able to continue squatting, others may struggle with it,” said Nichols. “A good rule of thumb to follow is to do what feels comfortable — if side squats hurt, then don’t do them, stick to regular squats and other movements that feel okay and don’t cause any pain.”
Consult with your doctor or obstetrician-gynecologist about which exercises are suitable for you.
New post published on: https://livescience.tech/2021/10/06/can-you-run-while-pregnant/
0 notes
Text
Impacts on Prenatal and Postnatal Mental Health in COVID-19
Impacts on Prenatal and Postnatal Mental Health in COVID-19
In this study, the Canadian researchers analyzed the prenatal and postnatal stress and depression in mothers and infant motor outcomes in two months of birth.
Source link

View On WordPress
0 notes
Text
MY BIRTH STORY
Trigger warning/s: Birth trauma and postnatal mood disorders
Less than a quarter of healthy, low risk, first time parents will have a normal birth in an Australian hospital. With the recent release of Birth Time: the documentary in Australia and New Zealand, I felt that revisiting my birth story was timely.
It’s a clichéd adage but it’s true: for me, the birth plan went well and truly out the window. In fact, it was never let into the building.
EST. READING TIME: 5 minutes
In my early twenties, I used to avoid making eye contact with the family planning section at the chemist. These days I have an emergency stash of tests in my bedside drawer. I’m not even late - my period tracker says it’s due today - but I have a nagging feeling that won’t go away.
I pee on the stick, and there’s only one line. Oh well. I shrug, insouciant, throw out the test and go about my day.
Until four in the afternoon, when I sit bolt upright on the couch and realise that I, generally a rule follower, hadn’t waited for that result. In fact, the box tells you to wait five minutes. So much for sitting on the couch with an egg timer.
I dig through the bin and in my shaking hands is a positive pregnancy test (note: those trying to conceive affectionately refer to this as a BFP). I test again, and again. I can’t wait, I race in my car to Victoria Park where my boyfriend of two years is working, with three BFPs sitting in the cup holder.
And so begins the uncontrollable for the Type A control freak.
In a pandemic, there are already things I can’t control. I’m redeployed to a different unit at my work and can no longer take potential COVID patients.
I’m anxious, exhausted and most of all - experiencing morning sickness that will turn into hyperemesis. Then, I have to take extended time off work.
As I do with most things, I jump straight into the deep end of pregnancy world and obsessively research. I avoid the foods you’re meant to avoid, and I buy all of the pre-baby accoutrements. Birthing ball, new yoga mat (and maternity yoga pants to boot), and the books. Oh my god, the books.
I do the hypnobirthing classes and listen to birthing stories while hiking with my dogs.
Being pregnant is simultaneously my new persona and hobby. I honestly still wouldn’t change a thing now, in spite of what I know, because even through vomiting for 7, nearly 8, months; I love being pregnant with all my heart.
I neatly type up a birth plan, beautifully formatted and fonted. Natural, natural, natural. No episiotomy. No pain relief. Don’t even offer it to me - I’ll ask. No interventions unless necessary. Delayed cord clamping. Immediate skin to skin. Quiet, low lighting, music. To me, this was a covenant between myself and the computer. Absolute, resolute and set in stone.
By the third trimester my partner and I have the hospital bag meticulously packed, nursery ready, and the big waiting game to do. Eager for our little family to be complete.
At my 38 week appointment, our obstetrician informs us that baby isn’t showing any signs of coming any time soon. I take that as a challenge and research a litany of labour-inducing old wives’ tales.
PSA: none of these actually work. If you are healthy with no complications, your baby will come when ready. Don’t rush. Even when you feel as if you can’t possibly be pregnant for single millisecond more. Your baby isn’t term until 40 weeks.
But here’s the kicker; the impending threat of an induction and/or caesarean looms overhead. I’m told I am a small girl. He appears to be a big baby. His head isn’t engaged at all. And that the clock is ticking.
Now I wonder what might have happened had that idea never been put into my head. If I had been given the space to accept my birth as it would come. Real birth. Normalised.
The pitfalls don’t just lie with mainstream media. You are being sold something. The expensive classes will tell you that having a natural birth without medication is possible, if you buy our book. The private obstetrician will tell you that you need an induction, an epidural, a caesarean; pay us.
At 39 weeks, the Friday before Christmas, my baby is showing signs of coming. What follows is 9 days of latent, or prodromal, or pre, or (my least favourite term) false labour.
On the Monday we go into hospital. With contractions 3 minutes apart, we are told my cervix and uterus aren’t agreeing. Simply put: head isn’t engaging, cervix isn’t dilating. And that I’ll know it when I’m in real labour.
During the week that follows I try exercises from Spinning Babies to get some relief from the round the clock contractions, Jack gives me massages and on one night I even give a glass of red wine and a bubble bath a go.
Websites that want to sell me something tell me that it’s because I’m too stressed for the labour to progress. Try our tea.
Why are we capitalising on something so sacred as birth?
I walk with one foot on the curb and one foot on the path - and I do this for kilometres. Through King’s Park in 30-degree heat. Along the coast. Around the neighbourhood.
On Christmas Eve, I can’t sleep, speak or move through the contractions and we wait as long as possible. We camp on the fold out bed in the living room (those without air conditioning throughout improvise), the birthing playlist quietly crooning and candles burning. I do my breathing and mantras; relax, relax, relaaaaax. And the contractions stop as abruptly as they started, 20 hours later.
I cry. Low keening, animalistic sobbing. I don’t understand what is happening to me. I don’t feel confident in making the choice whether or not to go to the hospital anymore.
They tell you the hospital is the safest place to birth and in the same breath tell you to avoid the hospital unless you’re damn near crowning.
I’m new to this. It’s my first time. I feel scared, unsupported and alone. I’m in so much pain.
I just want to meet my baby.
Barely two days later, I shake Jack awake. I’ve got a Miss Clavel feeling. Something is not right. Instinctively I know that after nine days of exhausting labour that doesn’t seem to be going anywhere, I will be too tired to push.
I call the hospital and ask if I can come in.
Have you just had enough? A voice asks on the other end.
So I don’t take the Panadol or the shower or the bath. We roll into the birthing unit and I’m put on the monitor. Like the High Striker at a fairground, I get the sense that the rolling peaks on the screen need to reach acceptable heights before I’m taken seriously.
The midwife is watching for decelerations, which don’t happen, but also doesn’t see any accelerations. My baby is tired, and I don’t blame him.
And then I am asked the question.
What do you want to get out of being in hospital today? Do you want to have your baby?
I nod, because yes. So comes the new plan. Break my waters and start the syntocin drip tomorrow. Temazepam and Panadeine Forte tonight. So quickly everything I imagined for my birth is going out the window, but I’m desperate.
The next morning we waddle into the birthing suites to start my induction bright and early. I feel robbed of the moment my waters break as it is cracked with something that looks like a crochet hook on a glove. With a gush and then a steady trickle, all the amniotic fluid keeping my baby safe and sound floods out. My obstetrician tells me it’s meconium stained, the paediatric RN in me fleetingly panics. But it is all systems go. I race from active labour to transition. I can only focus on the contractions.
I want my mum.
I’m offered the epidural I’d refused the day prior again but I shake my head. Not in the birth plan. Gas and air only, please. I end up screaming into the Entonox mouthpiece every 2 minutes and throw up all over myself before I allow myself the grace of an epidural. Which only works for about fifteen minutes before I’m once again writhing and screaming, one leg ice numb but the rest of me on fire. Intense pressure between my legs, the urge to push. But it’s only been a couple hours.
My mum arrives in the hospital. On the birth plan, she was meant to be waiting outside. She stands near me now, in the birthing suite.
I’m making noises I am not proud of and inform my midwife of my need to push. Oh, it’s too soon? Pardon me. Before the midwife’s assessment I steel myself to be told I am nowhere near, after a week of disappointment and being nowhere near.
Oh. You’re having a baby.
I ask if we need to wait for the doctor when she tells me she’s calling my obstetrician.
No, she laughs. You don’t have to wait.
With my knees to my chest, I’m told to stop pushing and so I stop. Afterwards, my partner tells me that our son was getting distressed despite my best efforts to get him out and the obstetrician was pulling back on the cord that was tight around his neck. And my poor tired baby’s heart rate drops dangerously. I’m given a deadline to push him out, but I can’t and I’m given the episiotomy I had expressly verboten on my birth plan. He is vacuum assisted out. He is safe.
I’m handed a small, beanlike baby covered in blood and vernix. I kiss him and end up with blood on my face. He doesn’t cry.
He’s taken off my chest and it feels like the longest pause before he lets out the best scream I’ve ever heard.
My mum looks at me. He’s beautiful, she mouths. Is he okay? He’s okay.
My partner cuts the cord. No delayed cord clamping, breathing is more important. Oliver is soon enough placed back onto my chest.
And he is beautiful.
What starts days later as the baby blues progresses into postnatal depression and anxiety. It took me a long time to accept what happened was birth trauma. That my birth story is ridiculously common, even amongst my group of friends, and that’s not due to our failure as the birthing parent. I can’t tell you how long I felt I only had myself to blame for having false expectations. And how much value I put into my ability to birth the “right” way as a direct translation of my ability to mother. How I felt that my son’s birth complications were my fault (it wasn’t). Too many Australian birthing parents are made to feel this way.
So I write this birth story once more, and I let go of what happened for my own sake. I didn’t fail. My son is beautiful, and worth every second of the agony it took to get him here.

A previous version of this post was published on my friend’s blog Mummy Neutral as ‘Type A and the Uncontrollable Pre-Labour’ in January 2021.
Please check her blog out as she posts some really raw and beautiful insights into pregnancy, birth and motherhood.
If you’re feeling distressed about anything discussed or about your own birth experience, please click the life ring symbol at the top of my blog for some helpful links. Call Lifeline on 13 11 14 if you need immediate assistance.
Birth Time: the documentary is showing in select cinemas now. You can visit the website to find out more and if you have birthed in Australia in the last 5 years, you can complete a survey about your experience.
1 note
·
View note
Text
New Release: Expect the Unexpected by Ann-Marie Gilbert
New Release: Expect the Unexpected by Ann-Marie Gilbert
AUTHOR SHARES HEARTFELT BIRTH TRAUMA JOURNEY AS POSTNATAL DEPRESSION TRIPLES IN COVID PANDEMIC
Two in every five mothers suffer with postnatal depression
Postnatal depression has almost tripled in the coronavirus pandemic, with two in every five new and expectant mothers reporting symptoms.
Author Ann-Marie Gilbert is all too familiar with these issues. Her new book, ‘Expect the Unexpected’,…

View On WordPress
0 notes
Text
‘My experience of postnatal depression’
Leeds Mum, Farzana, talks to us about her experience of postnatal depression...
Tell us a bit about yourself
I am Farzana Khatun, a twenty eight year old British Bangladeshi woman. At the young age of twenty one, I became a wife. Despite all the joys that come with marriage, moving away from my family to a different city affected my mental health. The stark contrast in family life from a busy household to an empty one brought many negative emotions such as loneliness. I was no longer alone when I got pregnant in 2015 but as is the case with many other mothers, I was diagnosed with both postnatal and postpartum depression. Mental health is very much not recognised in the Asian community as it’s a taboo topic. Many even go as far as to be in denial as they excuse it as physical illness. It is discussed as a weakness and therefore Asian children fear for the reaction if they express their feelings. Especially amongst men, the ‘breadwinners’ of the family lock up their emotions as they believe this weakness may affect their masculinity and status in the family. Mental health is a stigma that is gossiped and laughed about within families as everybody denies the feelings of anxiety and depression they feel towards events.
What were your initial thoughts of the country going into lockdown?
For every woman, bringing a life into this world is a daunting concept. These natural nerves and fears are doubled when you are to give birth during such a vulnerable time with doctors who are overwhelmed and the possible risk of illness. My second experience with labour was the most traumatising. Only when I was in active labour was my husband given permission to stay during labour, leaving me to be completely alone with my thoughts at the beginning. Things took a turn when my baby’s heartbeat slowed down and I was sent to have an emergency c-section. All the chaos in the delivery room was so different from my first time with childbirth as it lacked the confidence and assurance my family gave me. Just the knowledge of having a family to go home to comfort me and the baby, helping me with mysterious rashes and first baths were all things I longed for. My new family of four was difficult to handle at the beginning as having to recover from the c-section and taking care of a newborn overwhelmed me.
How have you spent your time during a lockdown?
Having a baby during lockdown was a completely abnormal experience. The atmosphere at the hospital was very unwelcoming as everyone was unsure of how to deal with this new pandemic. The midwives seemed absent and I could sense the silent hesitance as I was forced to be completely independent despite struggling to move. The whole situation was out of my control as many of my requests were unanswered. One request included a female doctor but due to the pressure that the NHS was under this could not happen. Having a female doctor was an essential factor for me because throughout my whole life I have been familiarised most with women through my traditional parents and this unfamiliarity made my labour an awkward process. My baby’s first Eid was celebrated at home, with her dad at work and only the three of us at home. A time that is normally a very joyous and busy time was quiet and regular. On the other hand, this experience allowed me to grow and understand myself better as a mother. I underestimated my ability to be independent with my children to attend to their every need and the bright side of this situation is that I grew even closer to my children.
What support networks have you built up during the lockdown?
A support network that I discovered during lockdown was the Perinatal Mental Health Service, a network I am very grateful for. During the lockdown, help is difficult to find as everyone is going through their own problems with the significant number of deaths occurring every day. The Perinatal Mental Health Service is a service which allows mothers to share their worries with other people who are in the same situation. It gave me an opportunity to cope with all of the overwhelming problems which were heightened by the fact that my family were unable to visit. I kept in contact with my family through frequent FaceTime calls however they were simply an imitation of the real thing and they were unable to experience the newborn baby feelings with me. The only adult connection I had was with my husband and something that was particularly hard was feeling completely useless as my husband worked, cooked, cleaned and cared for the children.
Have you still felt well connected to the Muslim community during the lockdown?
During the lockdown, I was able to witness the strength of the Muslim community. Due to the fact that Eid was celebrated alone and Friday prayers were not taken place the Muslim community was more attentive to other families. The advice was shared around and everybody comforted each other on the unusualness of this year’s celebration. On many different platforms, the Muslim community expressed their availability to help as during lockdown especially people questioned the purpose of life as they came to a realisation that the next day is not guaranteed with many losing multiple relatives weekly. Eid is the celebration of the end of a month of fasting and this month was also very different due to Covid-19. Ramadan is normally the month that Muslims are the closest as they break their fast together and sympathise with the needy. It was particularly hard this year for many Muslims as without the constant activities, we were more aware of our hunger and it was especially hard since, for example, my mother had to break her fast alone for the first time in her life. It affected us all in little ways.
Are you aware of how Covid-19 is disproportionately affecting Black, Asian and Minority Ethnic (BAME) communities and how does this make you feel?
Covid-19 is affecting BAME communities to a much higher extent and I personally know of many relatives who have been affected by it. There is nothing that can be done of that fact, but if this is acknowledged by the NHS why are BAME communities not being prioritised since we are evidently more at risk? This is very frustrating as despite the progress we have made towards discrimination, there is so much still to be done.
What are your hopes for the future?
Unfortunately, there are so many problems in society today and the first step to erasing these problems is by educating people from childhood. The older generation tends to be more stubborn about their beliefs on the sincerity of mental health but if the new generation is taught that mental health should not be a taboo and is a natural part of life society would change as we know it. I hope for a future where I felt that society genuinely cared for my physical and mental being and not the economic gain they would receive from it. In the future, I would like to have perinatal meetings in person to have the full experience of relating with other mothers in my situation.
#bamecommunity mumsgroups mumsupport newmum mentalhealthambassadors mentalhealthmatters endthestigma
0 notes