#thoracic myelopathy treatment
Text
Thoracic Myelopathy Treatment in India
IndoSpine Hospital is the best hospital for thoracic myelopathy treatment in India. Our spine specialists thoroughly analyse the patient’s condition and provide effective treatment including medication, physical therapy, decompression surgery or laminoplasty. Our labs are equipped with state of the art machines that help to give precise results with utmost care. Book an appointment with the thoracic myelopathy specialist today.

#thoracic myelopathy treatment#back pain treatment#spine specialist india#lower back pain surgery#spine hospital in india#spine surgeon#indospine hospital#spine doctor in india
0 notes
Text
Top Doctors You Should Know About
Choosing a top doctors greenslopes can be one of the most difficult tasks a person may ever have to face. And it is even harder if you are relying on awards and reviews to find a reputable doctor.
A recent ABC News report explains how some of these awards are meaningless and can be rigged by doctors who have financial relationships with the award companies.
1. Dr William A. Abbas
Dr Abbas is a doctor who focuses on treating patients of all ages. He provides preventive care, including routine checkups and tests, as well as coaching them on how to live healthier lives.
He is experienced in many medical conditions, including heart disease and cancer. He is also skilled in helping patients manage their diabetes, asthma and other chronic health issues.
His patient-centered approach makes him one of the best doctors in his field, and he values the time he has with his patients. He believes that a doctor-patient relationship should last long enough for him to thoroughly evaluate each patient’s health and answer their questions and concerns.
He has a wide range of experience in thoracic surgery, including robotic thoracic surgery and advanced thoracic endoscopy. He is also known for his expertise in foregut diseases, such as esophageal motility disorders and complex antireflux procedures. He is a member of the American College of Thoracic Surgeons and the Society for Robotic Thoracic Surgery.
2. Dr Khalid Abbed
Dr Khalid Abbed is a neurosurgeon who specializes in the treatment of conditions that affect the nervous system. He provides invasive and minimally invasive surgical procedures for disorders such as traumatic brain injuries, tumors, and Parkinson’s disease.
He has 24 years of experience and works at Hartford HealthCare Medical Group in Bridgeport, CT. He treats patients in New Haven and Stamford.
In his practice, Dr Abbed frequently treats Low Back Pain, Radiculopathy (Not Due to Disc Displacement), and Cervical Spine Myelopathy. He accepts most insurance plans and is accepting new patients.
He joined Hartford HealthCare on March 16 from Yale School of Medicine where he was a professor, clinical vice chair, and chief of spine surgery. He will also serve as co-physician-in-leader of the Ayer Neuroscience Institute. He will oversee neurosurgical services and lead the institute’s expansion into Fairfield County and throughout Connecticut. He is skilled in the minimally-invasive treatment of spine ailments and will work with healthcare leaders to improve patient care and develop less invasive, more intelligent medical technologies.
3. Dr John Burris
Dr John Burris is a preventative medicine specialist practicing in Vail, CO. He participates in the planning and evaluation of health services, researches diseases in specific populations, and helps manage health care organizations.
He is also a neonatologist, and his clinical and research interests include care of complex newborns, nutrition in breastfed infants, improvement in respiratory outcomes of premature neonates, and graduate medical education. He is also an associate director of the Complex Delivery Service at GCH, and spearheaded the initiation of less invasive surfactant administration in the GCH NICU which now is the standard of care for infants meeting criteria for surfactant deficiency.
He has been in practice for over 28 years, and receives good ratings from patients. They say he explained their conditions well and didn’t rush them through their appointment.
4. Dr Akhtar
Dr Akhtar is a hematologist and medical oncologist with extensive experience in treating patients with blood disorders. He provides chemotherapy, pain management, access to clinical trials and follow-up care.
His passion for the field of medicine was sparked by his parents, respected physicians. He strives to live up to the same standards, and he is committed to providing compassionate and exemplary medical care for all patients.
He is board-certified in hematology, internal medicine and oncology. His special interests include treatment of cancer, blood disorders and bone marrow transplants.
In addition to his private practice, he is also Director of the Orangi Pilot Project (OPP) in Karachi, Pakistan. The OPP focuses on assisting disadvantaged people in low-income settlements to lift themselves out of poverty. The program is based on participatory development, poverty alleviation, microfinance, endogenous rural development, and grassroots approaches to development. It has been replicated in various parts of the world and continues to be implemented today.
0 notes
Text
Pilates: Do You Really Need It? This Will Provide Help To Decide!
Pilates does not provide cardiovascular activity. Pilates workouts promote power and balanced muscle growth as well as flexibility and increased vary of movement for the joints. They vary from computerized, table-based mostly units that cost 1000's of dollars and are normally discovered within the places of work of chiropractors or physical therapists to over-the-door items that value not more than $20. In distributed native course of for healing, the important thing methods are the extension of candidates of linked nodes and enhancing loops by making use of a message-passing algorithm impressed from statistical physics. The next part in the process occurred as wind and frost brushed away on the gentle interior space of some of these fins, finally perforating them with a window. 2006 National Park Services The unusual rock formations in Arches National Park have been formed by wind and water over tens of millions of years. High above the Colorado River, Arches National Park is a geological maelstrom that has been formed by eon after eon of weathering by rain, snow, ice, and wind. Arches National Park is greater than a concentration of spectacular rock arches.
The research indicates that if in case you have had the pain for lower than 60 days, and it has been confirmed with an MRI, the issue might be traced to a disk and also you may benefit extra from intermittent traction. Optimizing the Jastrow factor is essential to restrict the exponential value of the CI growth as a result of, while the Jastrow issue cannot affect the nodes, it will probably cut back the burden of correcting the likelihood density from any worth given by a Slater determinant (see Eq. While a working multi-determinant algorithm will be constructed on the basis of the multi-determinant growth of the earlier section, a significant step ahead could be taken using the idea developed in Ref. It often takes several sessions to get used to utilizing this apparatus. Keep in thoughts it takes a minimum of 20 pounds of pull, which equals about 2-1/2 gallons of water. These treatments can keep your pores and skin trying vibrant and youthful. The entire idea of traction is that you retain your body relaxed while the appropriate quantity of pressure is applied. But cervical and higher extremity signs seem to show the most promise in being positively affected by intermittent traction.
This is probably because it's totally tough to get sufficient drive on the lumbar spine to drag it due to the problem in holding onto the upper body and lower body whereas making use of the pressure. What we do know is how a lot pressure of pull is required to get certain areas of the spine to separate between segments. When executed along side stabilization workout routines, joint manipulations, postural corrections and movement corrections, your chances of seeing enchancment are much greater., Erhard, RE., Piva, SR. (2004). Intermittent cervical traction and thoracic manipulation for management of mild cervical compressive myelopathy attributed to cervical herniated disc: a case series. The unproven principle is that if the disks are pulled, they are going to regain hydration or have an inflow of water. If you're stinking up the joint and ceaselessly gasping to catch your breath, your daily exercise sessions will probably be most unwelcome no matter how tolerant your employer is otherwise. Some folks find it useful to get an train prescription from their docs. By honing their abilities for this new stage of networking, tech professionals will discover new challenges and alternatives for years to come back.
A digital node will be simulated by an actual node (we name the prevailing non virtual nodes as real nodes). We'll first discuss the distinction between sustained and intermittent traction. Ok, let's first look at the baseline. First tighten them, then loosen up them. This would then make them more shock absorbent. Sights like these are what make the journey to Arches National Park worthwhile for travelers from all over the world. All programs depend on the flexibility to get an excellent hold on the physique segments so as to tug with enough pressure (not less than half the body weight) to make a distinction. So, with 건마 to go the other method, it’ll take a long-term dedication of lots of smaller goals. Without the data on the present state of parts, a mitigator cannot decide what (if any) action to take to continue operation of the system. It's possible you'll not have time to let Calgon take you away, however a fast, hot shower can nonetheless do you a world of good at the tip of your busy day. Don’t let the price resolve for you, although.
1 note
·
View note
Text
NEUROLOGICAL MANIFESTATIONS AND PORPHYRIA: ON THE PURPOSE OF A CASE in Open Access Journal of Medical and Clinical Surgery by Diego Julián Alvis-Peña

Abstract
Acute Intermittent Porphyria (AIP) is a pathology caused by a defect in the porphobilinogen deaminase enzyme that catalyzes the third stage of synthesis of the heme group; It has been associated with an extensive list of symptom manifestations, which can include skin changes, neuropsychiatric symptoms, peripheral neuropathy, and acute neuro visceral attacks.
The objective of this case report is to present the basic aspects of this disease, to focus on diagnostic tests and the improvement of functionality with the management of intravenous fluids, physical therapy, and diet.
We present the case of a 29-year-old adult woman with acute intermittent porphyria with a history of urinary infection, intestinal obstruction due to cecum volvulus, and motor and sensory involvement. During her hospital stay, the treatment was multidisciplinary. The patient was discharged in good general condition with outpatient follow-up.
Keywords: Porphyria, Acute Intermittent Porphyria, Neurologic Manifestations, Porphyrins (source: MeSH NLM).
Introduction
Porphyria is a group of metabolic disorders of the heme biosynthesis pathway, characterized by excessive accumulation and excretion of porphyrins and their precursors [1]. Porphyria is not a single disease, it is a group consisting of 9 disorders: acute intermittent porphyria (AIP), hereditary porphyria, variegate porphyria, δ-aminolevulinic acid dehydratase deficiency porphyria, cutaneous porphyria, hepatoerythropoietic porphyria, congenital erythropoietic porphyria, erythropoietic protoporphyria, and X-linked protoporphyria [2,3].
The heme pathway consists of 7 steps that occur in the mitochondria and cytoplasm [4]. The first step starts with succinyl CoA and Glycine substrates these are used by δ- aminolevulinic acid synthase to synthesize δ-aminolevulinic acid (ALA) [4,5]. After this ALA dehydratase uses ALA to create porphobilinogen, which porphobilinogen deaminase then uses as a substrate to produce hydroxymethylbilane. Uroporphyrinogen III synthase uses hydroxymethylbilane to synthesize uroporphyrinogen III. Decarboxylation of uroporphyrinogen III then produces coprophyrinogen III [4,6], which undergoes 3 additional steps in the mitochondria to finally synthesize heme [4,5,7]. Estimates of the combined prevalence of acute Porphyrias are 5 cases per 10000 persons [8]. Of the types of acute porphyrias, that due to delta aminolevulinic acid dehydratase deficiency is extremely rare, whereas acute intermittent porphyria is the most common with an overall European prevalence of approximately 1 in 2000 [9], with a higher incidence of 1 in 1000 in Sweden and with a high incidence in ethnic groups in Argentina and Spain [10].
Acute porphyrias present with acute attacks of neurovisceral symptoms (severe abdominal pain, nausea, constipation, confusion and seizures) and can be life-threatening [11]. Therefore, acute porphyria should be considered within the diagnostic possibilities in a patient consulted for acute abdominal pain, neuropsychiatric alterations and dysautonomic crises [11,12]. This diagnosis can be made quickly by demonstrating abnormally elevated levels of porphobilinogen as well as delta aminolevulinic acid (LAA) of 1.5 to 7 mg/dl in 24-hour urine [11,13]. A timely diagnosis and adequate treatment improve the prognosis of patients diagnosed with this pathology and prevents the development of neurological complications. We report a case of Porphyria in a 29-year-old female patient admitted to the emergency department of a tertiary hospital with acute abdominal pain and neurological disorders.
Case Description
A 29-year-old female patient with no relevant pathological history, was admitted for clinical picture of abdominal pain in upper abdomen associated with emesis of food content to the point of not tolerating the oral route, laboratories were ordered (blood count, urinalysis, CRP, liver function, amylase, The only finding was a slight elevation of amylase with a decreasing control at 6 hours, pathological uranalysis, normal ultrasound of the abdomen, interpreted as a urinary tract infection, it was decided to manage with antibiotic therapy with first generation cephalosporin and analgesia. The following day the patient consulted the emergency room again due to persistent abdominal pain, this time diffuse with absence of stools, abolished hydro-aerial sounds and abdominal distention; Given the above, general surgery was requested, who ordered a CAT scan of the abdomen and in view of the imaging findings of colon dilatation without distal gas, with evidence of hydro- aerial levels, they commented that it looked like a possible sigmoid volvulus, the patient was taken to an exploratory laparotomy where a right hemicolectomy was performed due to cecal volvulus with the need for a latero-lateral anastomosis.
In his initial recovery process his evolution was stable but on postoperative day 2 he presented tachycardia, diaphoresis, generalized abdominal pain and absence of stool, an abdominal x-ray was requested with the presence of gas and fecal matter; The studies were expanded with a new CT scan of the abdomen with dilatation of the left colon with the presence of gas, therefore, it was considered possible postoperative ileus, it was decided to manage with electrolyte replacement and passage of nasogastric tube with partial clinical improvement of the picture, however, she remained symptomatic and an infectious profile was considered, However, she remained symptomatic and an infectious profile was taken, urine culture and blood culture were compactible with acute infectious symptoms and antibiotic therapy with ampicillin sulbactam was ordered for 5 days with clinical improvement, negative acute phase reactants and as a final outcome she was discharged at the end of the antibiotic therapy cycle, completing 18 days of hospitalization since readmission.
One month after discharge, the patient consulted again for clinical symptoms consisting of muscle weakness predominantly in the lower limbs and inability to walk, with a feeling of hypoesthesia, this had manifested in postoperative control consultation with general surgeon who considered possible deconditioning vs. polyneuropathy and therefore referred to the emergency department for evaluation by neurology and physiatry. Once in the emergency department the patient was evaluated by a neurologist who considered the initial diagnostic impression as myopathy vs. polyneuropathy. Paraclinical tests were ordered with preserved renal function, no complement consumption, normal blood count, non- pathological urinalysis, with slightly increased ESR, normal CPK, electromyography with a final report of asymmetric neuropathic pattern suggestive of a motor neuron disease in progression, possibly ALS vs. progressive spinal atrophy. Given the paraclinical reports, an evaluation by the physiatrist was requested, who ruled out myopathy or polyneuropathy, since the CPK report was negative and there was evidence of alteration in the neurological examination with muscle strength in the right triceps 3/5, psoas and quadriceps 2/5, other muscle groups 4+/5, bilateral patellar arreflexia, left achilles clonus and right achilles hyperreflexia, left babinski, good head control and regular trunk control due to abdominal weakness, adopts sitting with help. The patient's sensory and motor level T6, hypoesthesia up to L1, dysesthesia in L2 and L3; paraclinical and semiological findings not compatible with these diseases; so, the diagnostic impression was given that the patient had a thoracic myelopathy vs. spinal cord injury and on the third day of her admission a brain and spine MRI was requested with no evidence of alterations (Figure 1).
Due to the aforementioned findings, a new concept was requested by the neurology service, who decided to rule out causes of infectious, autoimmune and inflammatory origin on the 5th day of hospital stay, also during the same period it was considered to begin to rule out heavy metal diseases plus CSF studies with lumbar puncture with meningeal panel which is reported on the 7th day and no alteration was evidenced, only abnormal report of cyanocobalamin deficit (Table 1) during this time the patient remained stable, with no changes in muscle strength or tendon muscle reflexes; On the 6th day of hospitalization a battery of studies for acute intermittent porphyria (AIP) is indicated, including levels of porphobilinogen in urine in 24 h, report that was positive with 2.80 mg/24 hours (Figure 2), also presented a positive urine color change test (light urine to dark urine). With these reports, the diagnosis of PAI was made, medical management was initiated according to the recommendations of the guidelines for PAI with support management, restriction of risk medications, ideal diet for patients with PAI according to the recommendations of the nutritionist, fluid therapy with 10% dextrose and physical therapy with subsequent improvement of the neuro-visceral pattern of the patient and she was discharged with comprehensive outpatient physical therapy after completing 20 days of hospital stay. It should be noted that during the two hospitalizations the patient required a psychiatrist's concept since she presented sleep disorder and emotional lability, managed with tricyclic antidepressants, finally during the control consultation with neurology one month after discharge, the patient was evaluated with recovery of muscle strength and sensitivity, without presenting any clinical deterioration.
Discussion
The neurological and visceral manifestations of porphyria have been recognized for over a century, with cases reported as early as 1890, and many detailed descriptions of individual cases have been reported since then, such as the case of British King George III. Porphyria is a group of metabolic disorders of the heme biosynthesis pathway, characterized by an excessive accumulation and excretion of porphyrins and their precursors; within this group we have PAI, which is an autosomal dominant genetic disease, described to have a genetic penetrance as high as 10%. The prevalence of genetic carrier is estimated at 1/10000 inhabitants, but the prevalence of cases is only 1-5/100000 inhabitants [14,15]. The pathophysiology of acute intermittent porphyria results from a partial defect of porphobilinogen deaminase, which is the third enzyme in the heme group biosynthetic pathway, caused by a mutation in the hydroxymethylbilane synthase gene; this is an autosomal dominant disorder; it usually does not manifest before puberty and the development of symptomatology is more prevalent in females than males; typically patients have abdominal pain, which is intermittent with colicky features and may extend to the dorsum and extremities, this can often be accompanied by constipation, nausea, vomiting, ileus symptoms and paresthesia; and on many occasions psychiatric symptoms [15]. Attacks of PAI usually produce severe acute abdominal pain in association with neuropsychiatric symptoms, there is also a degree of motor neuropathy with proximal and distal involvement as seen in acute inflammatory demyelinating polyneuropathy or chronic inflammatory demyelinating polyneuropathy [14,15]. In the case of our patient, her initial clinical picture showed bizarre visceral symptoms that progressed to the point of generating an intestinal obstruction, with time she developed motor and sensory neurological symptoms and psychiatric disorders; symptomatology compactible with the classic clinical presentation of acute intermittent porphyria attack as documented in the literature (Table 2). Porphyria is a difficult disease to diagnose because of its low prevalence, and given the frequency of asymptomatic cases it is difficult [15,16].
The treatment is ideally supportive, and is based on the detailed review of drugs that may be a risk in patients with porphyria and that can generate an acute attack as in the case of barbiturates, anticomiciales, ergotamine, antibiotics such as sulfonamides, progestogens, among others [16]; Likewise, the prevention of caloric restriction and prolonged fasting is a common cause of IAP attacks, for which a good carbohydrate intake and the administration of fluid therapy (preferably 10% dextrose in 0.45% saline solution), antiemetic agents, analgesics, and anticonvulsant drugs are indicated in patients with seizures [17,18]; the only specific treatment for acute attacks of IAP is intravenous Pan hematin [17,19]. In the case of our patient, only supportive management was performed, performing irrigation drug restriction, diet for patients with PAI high in carbohydrates, fluid therapy with 10% dextrose and comprehensive physical therapy ordered by the physiatry service.
To conclude, the diagnosis of PAI is difficult to make without adequate clinical suspicion on the part of the treating physician and should be considered in patients who after the second decade of life consult repeatedly for abdominal pain without reasonable cause associated with neuropsychiatric symptoms. The diagnosis can be quickly confirmed with the demonstration of porphyrins in urine, the treatment is ideally supportive and with hemin in acute attacks and should be given early to avoid fatal evolution or irreversible neurological lesions.
Regarding our Journal: https://oajclinicalsurgery.com/
Know more about this article
https://oajclinicalsurgery.com/oajcs.ms.id.10025/
https://oajclinicalsurgery.com/pdf/OAJCS.MS.ID.10025.pdf
#Porphyria#Acute Intermittent Porphyria#Neurologic Manifestations#Porphyrins#oajcs#clinical surgery#Diego Julián Alvis-Peña
1 note
·
View note
Text
Cervical pain symptoms and treatment
WHAT IS CERVICAL SPONDYLOSIS?
Cervical pain symptoms and treatment
Cervical Spondylosis
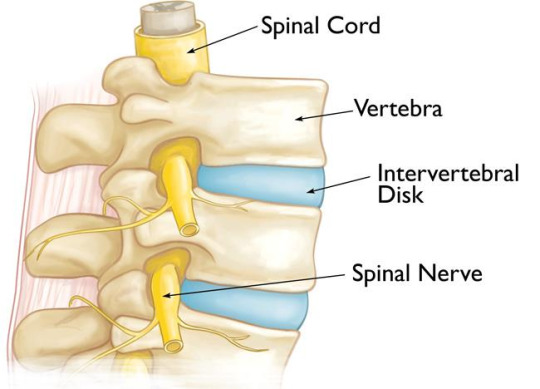
Cervical spondylosis is a typical, age-related problem of the cervical spine that is situated in the neck area. This condition is otherwise called neck joint inflammation or cervical osteoarthritis. With age, the cervical plates bit by bit face mileage bringing about the breakdown of the construction. The liquid present between the cervical plates is lost which makes the spine stiffer, prompting cervical torment. This outcomes in changes during the bones, plates, and joints at the spine of the neck.
Because of the liquid drying out and degeneration of the plates and ligament in the encompassing region, unusual development or spray of bones called osteophytes can happen prompting the narrowing of the section from where spinal nerves leave, causing a connected condition called cervical spinal stenosis.
What is Spondylosis?
Spondylosis is an umbrella term that is utilized to portray any degeneration of the spinal line. Spondylosis manifestations include intense pain and back in advanced age. Cervical spondylosis is pervasive among moderately aged and old individuals with over 85% of individuals more seasoned than 60 years being a casualty of this problem that causes cervical neck torment. Early cervical spondylosis can likewise happen yet it is uncommon.
Spondylitis versus Spondylosis
Spondylitis and spondylosis both influence the spinal rope however there is an essential contrast between the two. The significance of spondylitis is that it is the aggravation of at least one regular cervical vertebrae prompting torment in the spine. Cervical spondylosis generally alludes to any sort of degeneration of the spine. Along these lines, despite the fact that the impacts of both the illnesses may be comparable, their starting point and cause are totally extraordinary. Understanding the distinction among spondylosis and spondylitis is significant on the grounds that it assists the specialists with deciding the course of treatment and the right drugs for the patient.
What is cervical lordosis?
Each individual has an ordinary bend of the spine which is known as lordosis. The deficiency of cervical lordosis alludes to the circumstance where an individual's spinal bend curves strangely and in an expanded manner internal. This can prompt exorbitant tension on the spinal rope that causes torment, distress, and outrageous deadness. The deficiency of cervical lordosis is regularly one of the contributing reasons for serious instances of cervical spondylosis.
What is Cervical Vertebrae?
Cervical vertebrae of the spine are the most slender and most sensitive bundle of seven hard rings present between the foundation of the skull and the thoracic vertebrae at the storage compartment.
2.
Bolt
Manifestations OF CERVICAL SPONDYLOSIS
Cervical Spondylosis
Cervical spondylosis manifestations can fluctuate from one individual to another and the degree of cervical spine torment relies upon the age of the influenced individual. A portion of the normal spondylosis side effects are:
Extreme solidness at the neck prompts manifestations of cervical torment in neck
Hefty cervical spondylosis migraine that may begin at the fundamental cervical spondylosis torment spaces of the neck
Torment in the shoulder and arms that outcomes in the powerlessness to move the hands
Inability to appropriately turn the head around because of outrageous torment
Spondylosis indications show granulating clamor or sensation when endeavors are made to turn the neck around
With enough rest and appropriate rest, cervical agony indications will in general improve. The manifestations of cervical torment are greatest toward the beginning of the day and afterward again around evening time before bed.
On the off chance that osteophytes cause cervical stenosis in the cervical bone, it squeezes the spinal line prompting a condition called cervical spondylotic myelopathy. The myelopathy significance is only it alludes to any illness of the spinal line. The beginning of this auxiliary condition can bring about the accompanying manifestations of spondylosis:
A sensation of unusual shivering, deadness, and shortcoming in the fringe areas like the arms, hands, feet, and legs
Absence of equilibrium and coordination which prompts strolling and development hardships
The spondylosis neck bone prompts strange reflexes and causes irregular muscle fits
The event of incontinence or the deficiency of power over one's urinary bladder and defecations
3.
img
Reason for CERVICAL SPONDYLOSIS
The typical mileage of the bones in the spinal string are the primary cervical spondylosis causes that outcome in degenerative spondylosis. Other potential reasons for cervical agony can be the accompanying:
Bone Prods or Unusual Outgrowths of Bones called Osteophytes:
As the spine declines and gets more vulnerable because of advanced age, the body reacts by developing new and additional issues that remains to be worked out the spine more grounded. This strange arrangement of bones or cervical osteophytes is called bone prods. These additional bones can squeeze the spine, for example, the nerve and the spinal string in the cervical area prompting a terrible instance of cervical circle illness.
Dried out Spinal Plates:
The spinal string is comprised of little bones called vertebrae which comprises of little liquid filled circles. The liquid in the middle of the bones is thick and behaves like cushion like pads that ingest the shock of substantial exercises like lifting, curving and different developments. With age, the liquid can get dried out driving because of a condition called plate parching. This makes the bones rub against one another during exercises that cause neck spondylosis and brings about intense agony in the risky space of the neck.
Herniated Circles:
In this condition, spinal circles foster breaks in them that outcome in spillage of the liquid present between them. This interior padding material that breaks out can press against the spinal nerves and bones bringing about deadness of the arms and serious agony.
Injury:
Any kind of neck injury because of a mishap can prompt the beginning of gentle cervical spondylosis which speeds up the maturing interaction of the cervical spine.
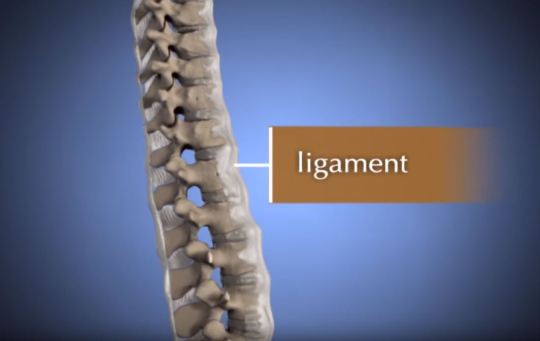
Firmness of the Tendon:
Tendons are groups of stringy connective tissue that interfaces bones and ligaments together. With age, these tendons can become stiffer that influences the general neck development prompting a cervical issue at the neck.
Unnecessary Pressure and Abuse:
Individuals who are utilized in areas that require hefty liftings like development work and more inclined to foster neck spondylitis and spondylosis. Since the beginning, this sort of occupation squeezes the neck and spinal rope prompting early lumbar spondylosis and side effects of cervical spondylosis.
4.
img
Hazard Elements OF CERVICAL SPONDYLOSIS
The most serious danger factor of cervical spondylosis is maturing and subsequently, it can't be totally kept from occurring. Yet, there are positively different variables that can speed up the beginning of this condition. Such factors include:
Neck injury because of a mishap
Business related distressing exercises that require substantial actual activities like truly difficult work
Helpless stance which means going through a similar neck developments or standing firm on your head in an awkward footing for a delayed timeframe, particularly for individuals who maintain work area sources of income. This is called dull pressure.
Hereditary components and family ancestry
Smoking
Being overweight and inert for a significant stretch of time
5.
Bolt
STEPS TO Forestall CERVICAL SPONDYLOSIS
There are sure cervical spondylosis home treatment estimates that can be applied to forestall this condition. These home solutions for cervical agony include:
Keep great consideration of the neck and shoulder locale. Try not to stack weighty articles on the head or neck. Try not to rest on a high-pad.
For individuals with work area occupations, focus on the stance you by and large will in general follow during work. Try to extend enough in the middle of your work hours. The fixing of your cervical spine is significant for the duration of the day. Recline your head every so often.
Swimming is viewed as a casual exercise for cervical agony. Try to swim regularly and perform general proactive tasks. Try not to be dormant for an extensive stretch of time. Exercise for cervical spondylitis is educated for individuals experiencing indications regarding spondylitis in the neck
6.
img
Analysis OF CERVICAL SPONDYLOSISCervical Spondylosis Analysis
How to fix cervical torment? This relies upon how well the illness is analyzed in any case. Making a precise analysis of the condition includes precluding other potential factors that can cause neck torment overall. Based on the consequences of tests, the specialist may allude the patient to a muscular subject matter expert or a nervous system specialist for additional cervical spondylosis treatment. Determination tests include:
1. Actual Assessments:
The previously set of material science tests to decide the legitimate course of spondylosis treatment incorporates testing the reflexes of the patient and check for the presence of muscle shortcoming and shortages in the tangible nerve work. For cervical spondylitis treatment, specialists additionally run tests to decide the scope of neck development and the overall condition of the general strolling development to comprehend cervical treatment important. This load of tests assist the specialist with comprehension if the spinal nerves and lines are under any kind of additional pressing factor. To affirm the finding of cervical spondylosis, specialists will arrange imaging tests and nerve work tests.
2. Imaging Tests:
X-Beam Imaging - To check for the presence of bone spikes and other strange development of spinal bones
Registered Tomography (CT) Sweep - To get nitty gritty pictures of the cervical district
X-ray Output - This strategy includes the utilization of radiowaves that assist the specialist with deciding the presence of squeezed nerves
Myelogram - For this situation, an infused stacked with a tracer color is utilized to feature the spaces of the c spine, Combined with CT Sweep or X-Beams, specialists can discover better pictures of the influenced regions.
3. Nerve Capacity Tests:
Electromyogram (EMG) - This test is utilized to decide whether the nerves of the body are working in an ordinary manner. EMG records the entry of nerve signals in the body by estimating the electrical movement of the nerves.
Nerve C
Comments
0 notes
Text
How to Find Best Brain Tumor Treatment Hospital in India ?
Treatment for a brain tumor differs depending on several factors such as a person's age, general health, and the size, location, and type of tumor. Treatment of brain cancer is usually complex. Most treatment plans involve several consulting doctors. Surgery to remove the tumor is typically the first option once a brain tumor has been diagnosed. The purpose of surgery is to confirm that the abnormality seen during testing is indeed a tumor and to remove the tumor. If the tumor cannot be removed, a sample of the tumor will be taken to identify its type. Radiation and chemotherapy are other modalities may also be used. Spine and Brain India directed by Dr. Arun Saroha offers one of the best brain tumor treatment in India.
Delhi is a hub for medical tourists flocking in from all corners of the world to receive superlative treatment from the best in the field. Dr. Arun Saroha is a noted neurosurgeon available in Delhi and Gurgaon with over 20 years of experience treating a wide variety of neurological conditions varying from acute pain to the most complex spinal deformity in both adult and pediatric patients. He has successfully performed over 7000 procedures with patients from different parts of the world. He is one of the best brain tumor doctor in Delhi who has the highest expertise in treating different types of brain tumor in adults as well as pediatric patients. He is well known for recommending the most effective and safest treatment options, delivering expert care tailored to the needs of the individual patients.
Dr. Arun Saroha is the Director of Neurosurgery at Max Hospital, Saket New Delhi and Gurgaon. Max Hospital is one of the top hospital in India offering the best brain and spine treatment using the latest technologies that increases the precision of the surgeon’s work and thereby improving the outcome of the treatment. In addition to the advanced technologies being utilized, correct diagnosis is the key to effective treatment. Doctors in India are known for their accurate diagnosis and best treatment at affordable rates as compared to Western countries.
The best brain surgeon in Delhi and Gurgaon, Dr. Arun Saroha, is also one of the very few in the country who treats pediatric neurosurgical conditions, including hydrocephalus, chiari I malformations, a rachnoid cysts, spine disorders including tethered cord, spinal tumors, vascular malformations, head and spine trauma. The particular types of brain conditions that arise in children differ in important ways from those found in adults. For children, particular risks and benefits correspond to particular treatments in ways that may be different than for adults.
Most of the hospitals in India are internationally accredited, thus enhancing customer’s access to better healthcare services and meeting their expectations. The accredited healthcare organization practices and delivers continuous quality services and functions in the best interests of all patients giving importance to access, affordability, efficiency and quality healthcare services.
Spine and Brain India headed by Dr. Arun Saroha, one of the best brain surgeon in Delhi and Gurgaon is dedicated in providing comprehensive diagnosis and treatment for all types of brain and spine conditions including Cervical, Thoracic and Lumbar Disorders, Disk Herniation, Spinal Stenosis, Spondylolisthesis, Spondylotic Myelopathy, Brain and Spine Trauma, Brain Tumors for both adult and pediatric patients.
youtube
#brain tumor surgery#SPINE AND BRAIN INDIA#best brain surgeon in Delhi and Gurgaon#best brain and spine treatment#Dr. Arun Saroha#best brain tumor doctor in Delhi#Brain Surgery in Gurgaon#Brain tumor doctor in Delhi NCR
0 notes
Link
Comprehensive Myelopathy Spinal Cord Surgery in India. Myelopathy describes any neurologic deficit related to the spinal cord. It can be cervical, thoracic or lumbar, the most common of which is cervical spondylotic myelopathy and is caused by arthritic changes the cervical spine. If your symptoms are mild, you may find relief with non-surgical treatments. These include pain medication, activity modification or physical therapy. Any treatment program should be under the guidance of a medical professional because with myelopathy the spinal cord is being overly compressed.
#Comprehensive Myelopathy Spinal Cord Surgery in India#Comprehensive Myelopathy Spinal Cord Surgery in Delhi#Best Hospital for Comprehensive Myelopathy Spinal Cord Surgery#Best Doctors for Comprehensive Myelopathy Spinal Cord Surgery
0 notes
Photo




My best friend and her step mom have opened an etsy store in order to cover their pug’s treatment. Their pug, Friday, was diagnosed with herniated discs in his lumbar and thoracic regions. He had a diagnostic CT scan and they are now waiting to find out if the neurologist recommends surgery. They’re also waiting to find out the results of a blood test, which will tell if he has degenerative myelopathy, which is basically a canine version of ALS, or Lou Gehrig’s disease. His surgery and treatment will be very costly and they need any help they can get in order to cover the costs. All of the money made from the etsy store will go toward Friday’s treatment. Any additional money after his treatment is covered will go toward the organization Pug Rescue of Florida (PROOF, http://pugrescueofflorida.org/ ) Friday means the world to my best friend and her family. Anyone who has owned a dog knows how important they are. Please purchase a bracelet if you’re able to (theyre aromatherapy bracelets !!) or simply share this post. Thanks! Etsy store - http://etsy.me/2oiLRzr
89 notes
·
View notes
Text
Revision surgery in thoracic disc herniation
http://monchiropracteur.com/ monchiropracteur.com Abstract
Purpose
Surgical treatment failures or strategies for the reoperation of residual thoracic disc herniations are sparsely discussed. We investigated factors that led to incomplete disc removal and recommend reoperation strategies.
Methods
As a referral centre for thoracic disc disease, we reviewed retrospectively the clinical records and imaging studies before and after the treatment of patients who were sent to us for revision surgery for thoracic disc herniation from 2013 to 2018.
Results
A total of 456 patients were treated from 2013 to 2018 at our institution. Twenty-one patients had undergone previously thoracic discectomy at an outside facility and harboured residual, incompletely excised and symptomatic herniated thoracic discs. In 12 patients (57%), the initial symptoms that led to their primary operation were improved after the first surgery, but recurred after a mean of 2.8 years. In seven patients (33%) they remained stable, and in two cases they were worse. All patients were treated via all dorsal approaches. In all 21 cases, the initial excision was incomplete regarding medullar decompression. All of the discs were removed completely in a single revision procedure. After mean follow-up of 24 months (range 12–57 months), clinical neurological improvement was demonstrated in seven patients, while three patients suffered a worsening and 11 patients remained stable.
Conclusion
Our data suggest that pure dorsal decompression provides a short relief of the symptoms caused by spinal cord compression. Progressive myelopathy (probably due to mechanical and vascular deficits) and scar formation may cause worsening of symptoms.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material. http://link.springer.com/10.1007/s00586-019-06212-w?utm_source=dlvr.it&utm_medium=tumblr http://monchiropracteur.com/
0 notes
Text
Affordable Thoracic Myelopathy Treatment in Ahmedabad
IndoSpine Hospital is the best hospital for affordable thoracic myelopathy treatment in Ahmedabad. Our spine experts carefully analyze the root cause of the conditions and draft an effective treatment plan based on it. Our spine hospital is equipped with all the machines and devices required for various examinations and diagnoses. Book your appointment today.
#thoracic myelopathy treatment#best thoracic myelopathy treatment#affordable thoracic myelopathy treatment#Thoracic Myelopathy Treatment in Ahmedabad#best hospital thoracic myelopathy#IndoSpine Hospital
1 note
·
View note
Text
Spinal Fractures: Common Cause of Teen Back Pain

This generation is characterized by its extremely active lifestyle and breakneck pace. The forerunners in this race are teenagers. Armed with their gargantuan passion, zeal, and motivation, teenagers don’t want to stop at all. They want it all, and they want it fast. This leads to adopting an unhealthy lifestyle. One that boosts productivity but takes a toll on the body and its well-being. People between the ages group of 18-25 are most susceptible to this. Their extremely busy schedule leaves them with almost no time to rest. Their machine-like functioning body thus starts giving signals that it needs oiling and maintenance. These signals are in the form of various physical ailments. The most common grievance being back pain. Teenagers and young adults are often found complaining about having the back of a 90-year old. They believe it is just them, but research shows otherwise. The chances of experiencing LBP (low back pain) are almost as high as 80% by the time one gets to the age of 20.
Causes of Back Pain in Teenagers: –
Back pain in teenagers can be of different types and have different sources of origin. The nature of back pain depends on the lifestyle and also sometimes on genetics. Here are some of the major causes and forms of back pain.
Muscle-Related Pain

This an external affliction of the muscles surrounding the spinal cord region. It does not involve the spinal cord itself. It is primarily focused near the thoracic and lumbar regions. This pain is characterized by continuous resonating pain. It usually disappears after proper resting and when the strained muscles are relaxed. Improper posture, carrying a heavy load, faulty sports equipment, psychosocial distress, anxiety and in some cases, even a past injury can cause such pain.
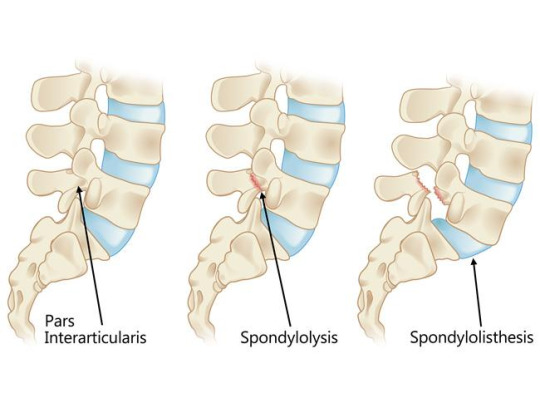
Spondylolysis
Spondylolysis is caused when a gap formation or separation takes place between vertebral bones. It is a common occurrence in young athletes and teenagers who tend to hyperextend their backs.
Spondylolisthesis
This is an acute condition in which one vertebra slips on top of the other. It can lead to chronic pain, and if not treated, immediately made lead to permanent deformity. It might need spinal infusion and surgery at a later point.
Disc Injuries and vertebral fractures
A fracture in the vertebra can be a result of some sudden shock or impact. This could occur while engaging in some extreme sports, gymnastics, or being involved in an accident. Damage to the vertebra or the intervertebral discs needs to attended immediately. Surgical procedures to prevent further damage to the area of fracture becomes a necessity.
Other Causes
Some other causes of chronic back pain could the presence of a spinal tumor, an infection, or inflammatory arthritis.
Spinal Fractures
In this article, we shall take a closer look at the bone-related injuries in the spinal cord. To be more specific fractures, cracks, and deformities in the spine. The spine is one of the most essential parts of our body. It protects the spinal cord, which relays the information from the brain to the different parts of our body. Damage to the spine can even lead to partial and complete paralysis. Thus, it is imperative to ensure that the spine stays protected from serious injuries. Immediate medical attention must be provided to prevent grievous harm to our bodies.
Symptoms
A fracture in the spine is detected using an X-ray. However, certain early signs and symptoms can help identify a fracture. These symptoms include back pain, muscle cramps, severe neck pain, weakness, partial or complete paralysis.
Causes
A fracture in the spine most commonly occurs when the person is involved in some accident. In fact, car accidents make up 45% of spinal cord related injuries. Extreme sports, falling, and improper posture are some other causes of a spinal fracture.
Diagnosis

Once the symptoms are experienced, the patient needs to visit a hospital or a nursing home. There the spinal fracture can be detected with the help of an X-ray, CT scan, or MRI scan. These are medical imaging techniques that help the doctors to take a look at the bone structure.
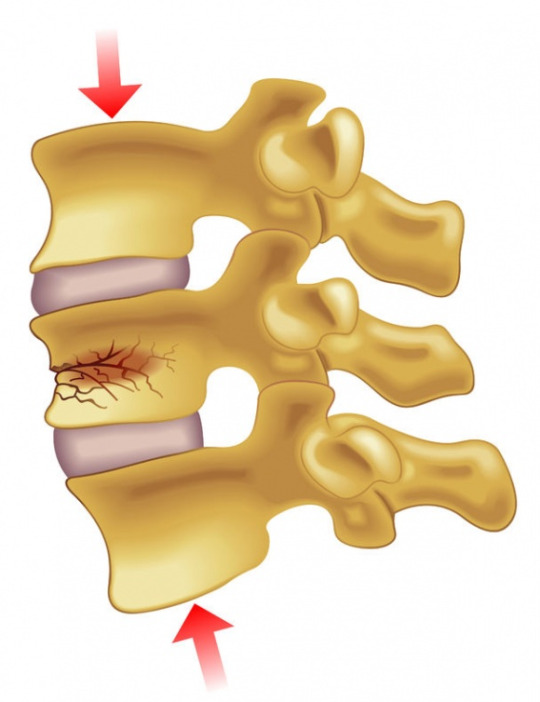
Types of Spinal Fracture
Compression Fracture – This kind of fracture is prevalent among people suffering from osteoporosis. Owing to weak bone structure, a sudden shock or impact results in a fracture in the vertebra. A special case in which the front part bends under pressure is called wedge fracture, due to the wedge-shaped deformity.
Burst Fracture – Burst fracture is a result of a severe accident like a car crash. The spine gets completely crushed, and a lot of vertebrae are fractured. The bone breaks into pieces in several regions. These fragments pose a threat of causing damage to the spinal cord.
Fracture Dislocation – A fracture in the spine can lead to certain vertebrae from getting dislocated. When the body is involved in an accident, the vertebra can shift from its original position and lead to a fracture-dislocation.
Treatments Available
Treatments can be broadly categorized into surgical and non-surgical procedures.

Surgical Procedures
ANTERIOR CERVICAL DISCECTOMY AND FUSION (ACDF)
This form of treatment is offered to the patients suffering from a cervical slip disc. The procedure requires an incision to reach the affected area and remove the disk to decompress the spine and relief the tension from the nerves. An artificial replacement is provided in place of the removed cervical disc to offer stability to the structure of the spine.
CERVICAL LAMINOPLASTY
This procedure is an ideal treatment for those who suffer from myelopathy or compression of the spinal cord. The spinal cord of the patient undergoes an ‘extension’ or ‘stretch’ from one side of the spine to another, as well as from top to bottom, to release the pressure from the spinal cord. It also gradually reduces strain from the nerves and prevents any complication.
CERVICAL POSTERIOR FORAMINOTOMY
When your back suffers through pain for a prolonged period, especially after a pinched nerve, Cervical Posterior Foraminotomy is applicable. Usually, the reason is due to the compression of nerves, or a herniated disk. Hence, it becomes important to perform incision and make space for the nerves to move freely and release the tension. Thus, relieving the pain.
LAMINECTOMY
Sometimes the spinal cord builds intense pressure. The pressure can result in intense pain, and there are several reasons for it; a herniated disk is usually the common culprit. However, the surgical procedure receives its name as it is a process of removal of lamia from the spinal canal. It releases pressure and offers relief.
CORPECTOMY
This method is only employed when all others fail. It is performed when a person suffers through a spinal fracture, infection, or other medical condition. When all else fails, this method will remove the damaged parts like disk or vertebra, from the spine to offer relief and prevent nerves from getting compressed.
LUMBAR DISC MICROSURGERY
The main purpose of this procedure is to relieve the patient off the excruciating leg pain, also known as Sciatica. It is a minimalistic surgical procedure in which the ‘herniated’ disk gets removed, and nerves under pressure are released.
VERTEBROPLASTY
It is a process in which medical experts take non-surgical measures and offer opportunities to strengthen the vertebra of the spine.
SCOLIOSIS CORRECTION SURGERY
Scoliosis is the bending of the spine to the sideways, almost like a curve, a physical deformity. To fix the issue, the surgeon utilizes tools like screws in the defective bones and uses rods to assist in correcting the posture over time.
KYPHOSIS CORRECTION SURGERY
Kyphosis is similar to Scoliosis. However, it is the forward bending of the spine instead of the sideways. It requires similar treatment measurements for proper recovery.
MIS SPINAL FUSION
It is a new medical surgery where specialists use microscopic equipment to carry out the procedure. The method is least painful of all, as there are minute incisions and cuts, barely felt, after the surgery. It is a perfect option for patients that are obese or overweight in general.
Non-Surgical Procedures
FACET JOINT INJECTIONS
It delivers small amounts of anesthetic and steroid medication to relieve pain in the neck and back. It also helps in diagnosing and locating the source of pain to provide immediate relief.
LUMBAR EPIDURAL STEROID INJECTION
It is a pain management procedures prevalent in spinal surgeries and medical conditions. From severe leg pain due to spine compression and herniated disk to other deformity-based pain, it is a very efficient method. A pain management specialist will introduce anti-inflammatory and anesthetic agents to the root of the cause and offer relief.
LUMBAR TRANSFORAMINAL EPIDURAL STEROID INJECTION
This is a pain-monitoring treatment, or known as ‘pain-treatment.’ It is usually employed when a patient is suffering through excruciating pain due to some form of spinal injury. Usually, it is due to the lumbar spine problems and requires attention to numb the pain in the legs and possibly lower back. The doctor who is in charge of the treatment will use a combination of anti-inflammatory and anesthetic injection and insert it into the main affected region (The spine) to offer relief to the patient.

0 notes
Text
What is Conservative Treatment for a Herniated Disc?
The term “conservative treatment” means that the treatment used to address an issue, such as a herniated disc in the lower back, is non surgical in nature and consists of other alternatives such as injections, medications, and physical therapy.
Herniated Discs Conservative Treatment New York NY – Better Health Chiropractic
Chiropractic treatments focus on providing conservative, alternative care for neck, back, and other spinal discomfort and conditions. The majority of conservative herniated disc treatment options are used in conjunction with others in order to achieve the best possible results. The ultimate goal of non-surgical lumbar decompression and other similar treatments is to help patients alleviate their pain and experience a healthier back and spine.
In cases where non-surgical treatment for herniated discs are not advised due to immediate danger and need for emergency care, surgery may still be the necessary choice. However, in most cases, surgical intervention is only used when conservative treatments do not provide the necessary relief.
Herniated Discs Conservative Treatment NYC – Better Health Chiropractic
What is a Cervical Herniated Disc?
A cervical herniated disc occurs when the inner part of the disc herniates, or starts to leak outwards. This puts pressure on the surrounding nerves and occurs primarily in those between 30 and 50 years of age. While they can be caused due to injury, most occur for seemingly no reason at all.
Arm pain is a common symptom of cervical herniated discs, a symptom that is caused by pressure on the cervical nerve. Along with pain, tingling and numbness are also common as is muscle weakness.
Since the discs are in relative close contact with the nerves and not a lot of “free space” is present in the area, even the smallest herniation can cause intense pain.
What is a Thoracic Disc Herniation?
A herniated disc in the thoracic spine occurs when the inner material of a disc leaks. The result is often moderate to severe pain in the upper back as well as numbness and radiating discomfort. The type of pain experienced can vary depending upon the location of the herniation. The following are the most common symptoms experienced for:
Central disc protrusion: upper back pain (myelopathy)
Lateral disc herniation: radiating abdominal and chest wall pain
Centro-lateral disc herniation: upper back pain, radiating pain, myelopathy
Thoracic back pain can be present in a number of forms, and can be easily exacerbated when either sneezing or coughing. Pain can radiate throughout the body, especially in the chest and gut, which can make diagnosis challenging. Oftentimes, what ends up being a herniated disc in the thoracic spine is originally mistook for a heart, kidney, gastrointestinal, or lung problem.
There are many issues and disorders of the spine that can sometimes present with similar symptoms, which can make diagnosis tricky as well. These include infection, metabolic disorders, spinal fractures, and the like. This is why visiting a chiropractor can be so beneficial and can help you to determine whether the issues you’re experiencing are chiropractic in nature.
youtube
What is a Lumbar Disc Herniation?
A herniated disc in the lower back, or a lumbar disc herniation, can be yet another cause for seeking out the assistance of a disc herniation specialist. These discs are integral in helping to absorb vertebral shock, supporting the upper body, and allowing for multi-directional movement.
When a herniated disc in the neck or lower back starts to leak, the disc can quickly begin to aggravate nearby nerves and cause moderate to significant pain throughout the body. Pain due to lumbar disc herniation often occurs out of the blue for no reason at all. It often becomes apparent after participating in a grueling activity such as lifting heavy objects or even simple, everyday motions like twisting the lower back. These kinds of movements can exacerbate a slipped disc, bulging disc, or other spinal injuries.
Lumbar disc issues, similar to a herniated disc in the neck, are most common in individuals who are between the ages of 35 and 50. As people age, it’s more likely for individuals to develop a bulging disc, slipped disc, or herniation. Since discs typically lose fluid over time, they become less pliable, harder, and more prone to damage. Disc degeneration, which causes these types of changes, begins relatively early in life.
Like in the case of a herniated disc in the thoracic spine, lumbar herniations can cause a number of side effects. Since the herniation often places pressure on the spinal nerve root, the result can be intense, shooting sciatic pain in the legs and buttocks.
Fortunately, non-surgical treatment for herniated discs can often treat lumbar herniations and the symptoms rarely last longer than a month. There are three primary reasons why these types of spinal injuries and issues aren’t long-lasting: (1) The body fights against the herniation which makes it shrink in size. (2) Water from within the disc is resorbed which causes the disc to shrink and the nerves to be affected far less. (3)Specific exercises have been shown to move the herniation away from the discs themselves.
Herniated Discs Conservative Treatment – Chiropractic Consultation
Schedule a Consultation with Dr. Eingorn about Herniated Discs Conservative Treatment
Dr. Eingorn is a chiropractor who has over 25 years of experience treating patients who are dealing with neck or back injuries through the use of spinal decompression. His focus is on helping individuals who are living with herniations that require the assistance of a disc herniation specialist.
If you’ve been living in pain, it’s time to reach out for professional assistance. Herniations do not heal themselves without decompression or other similar treatments, so seeking help is a must. Dr. Eingorn takes a very thorough approach to chiropractic care and offers a number of non-surgical lumbar decompression treatments. Decompression is a proven technique that Dr. Eingorn has used to help patients who are living with a herniated disc and other similar spinal injuries and issues.
To schedule an appointment to learn more about spinal decompression and the other herniated disc treatment options available to you, give the office of Dr. Eingorn a call today at 646-553-1884.
Herniated Discs Conservative Treatment
Areas of Service
Dr. Eingorn and Better Health Chiropractic (https://betterhealthchiropracticpc.com) provide conservative treatment for disc herniations of the lower back, upper back, and neck for patients from these areas of NYC:
Manhattan, NYC, Midtown NY, Battery Park City NY, Financial District NY, TriBeCa NY, Chinatown NY, Greenwich Village NY, Little Italy NY, Lower East Side NY, NoHo NY, SoHo NY, West Village NY, Alphabet City NY, Chinatown NY, East Village NY, Lower East Side NY, Two Bridges NY, Chelsea NY, Clinton NY, Gramercy Park NY, Kips Bay NY, Murray Hill NY, Peter Cooper Village NY, Stuyvesant Town NY, Sutton Place NY, Tudor City NY, Turtle Bay NY, Waterside Plaza NY, Lincoln Square NY, Manhattan Valley NY, Upper West Side NY, Lenox Hill NY, Roosevelt Island NY, Upper East Side NY, Yorkville NY, Hamilton Heights NY, Manhattanville, Morningside Heights NY, Harlem NY, Polo Grounds NY, East Harlem NY, Randall’s Island NY, Spanish Harlem NY, Wards Island NY, Inwood NY, Washington Heights NY
The post <span lang ="en">What is Conservative Treatment for a Herniated Disc?</span> appeared first on NYC Chiropractor – Better Health Chiropractic New York – Call 646-553-1884.
This blog post originally appeared here: http://bit.ly/2WQ3Nlt
0 notes
Text
What is Conservative Treatment for a Herniated Disc?
The term “conservative treatment” means that the treatment used to address an issue, such as a herniated disc in the lower back, is non surgical in nature and consists of other alternatives such as injections, medications, and physical therapy.
Herniated Discs Conservative Treatment New York NY – Better Health Chiropractic
Chiropractic treatments focus on providing conservative, alternative care for neck, back, and other spinal discomfort and conditions. The majority of conservative herniated disc treatment options are used in conjunction with others in order to achieve the best possible results. The ultimate goal of non-surgical lumbar decompression and other similar treatments is to help patients alleviate their pain and experience a healthier back and spine.
In cases where non-surgical treatment for herniated discs are not advised due to immediate danger and need for emergency care, surgery may still be the necessary choice. However, in most cases, surgical intervention is only used when conservative treatments do not provide the necessary relief.
Herniated Discs Conservative Treatment NYC – Better Health Chiropractic
What is a Cervical Herniated Disc?
A cervical herniated disc occurs when the inner part of the disc herniates, or starts to leak outwards. This puts pressure on the surrounding nerves and occurs primarily in those between 30 and 50 years of age. While they can be caused due to injury, most occur for seemingly no reason at all.
Arm pain is a common symptom of cervical herniated discs, a symptom that is caused by pressure on the cervical nerve. Along with pain, tingling and numbness are also common as is muscle weakness.
Since the discs are in relative close contact with the nerves and not a lot of “free space” is present in the area, even the smallest herniation can cause intense pain.
What is a Thoracic Disc Herniation?
A herniated disc in the thoracic spine occurs when the inner material of a disc leaks. The result is often moderate to severe pain in the upper back as well as numbness and radiating discomfort. The type of pain experienced can vary depending upon the location of the herniation. The following are the most common symptoms experienced for:
Central disc protrusion: upper back pain (myelopathy)
Lateral disc herniation: radiating abdominal and chest wall pain
Centro-lateral disc herniation: upper back pain, radiating pain, myelopathy
Thoracic back pain can be present in a number of forms, and can be easily exacerbated when either sneezing or coughing. Pain can radiate throughout the body, especially in the chest and gut, which can make diagnosis challenging. Oftentimes, what ends up being a herniated disc in the thoracic spine is originally mistook for a heart, kidney, gastrointestinal, or lung problem.
There are many issues and disorders of the spine that can sometimes present with similar symptoms, which can make diagnosis tricky as well. These include infection, metabolic disorders, spinal fractures, and the like. This is why visiting a chiropractor can be so beneficial and can help you to determine whether the issues you’re experiencing are chiropractic in nature.
youtube
What is a Lumbar Disc Herniation?
A herniated disc in the lower back, or a lumbar disc herniation, can be yet another cause for seeking out the assistance of a disc herniation specialist. These discs are integral in helping to absorb vertebral shock, supporting the upper body, and allowing for multi-directional movement.
When a herniated disc in the neck or lower back starts to leak, the disc can quickly begin to aggravate nearby nerves and cause moderate to significant pain throughout the body. Pain due to lumbar disc herniation often occurs out of the blue for no reason at all. It often becomes apparent after participating in a grueling activity such as lifting heavy objects or even simple, everyday motions like twisting the lower back. These kinds of movements can exacerbate a slipped disc, bulging disc, or other spinal injuries.
Lumbar disc issues, similar to a herniated disc in the neck, are most common in individuals who are between the ages of 35 and 50. As people age, it’s more likely for individuals to develop a bulging disc, slipped disc, or herniation. Since discs typically lose fluid over time, they become less pliable, harder, and more prone to damage. Disc degeneration, which causes these types of changes, begins relatively early in life.
Like in the case of a herniated disc in the thoracic spine, lumbar herniations can cause a number of side effects. Since the herniation often places pressure on the spinal nerve root, the result can be intense, shooting sciatic pain in the legs and buttocks.
Fortunately, non-surgical treatment for herniated discs can often treat lumbar herniations and the symptoms rarely last longer than a month. There are three primary reasons why these types of spinal injuries and issues aren’t long-lasting: (1) The body fights against the herniation which makes it shrink in size. (2) Water from within the disc is resorbed which causes the disc to shrink and the nerves to be affected far less. (3)Specific exercises have been shown to move the herniation away from the discs themselves.
Herniated Discs Conservative Treatment – Chiropractic Consultation
Schedule a Consultation with Dr. Eingorn about Herniated Discs Conservative Treatment
Dr. Eingorn is a chiropractor who has over 25 years of experience treating patients who are dealing with neck or back injuries through the use of spinal decompression. His focus is on helping individuals who are living with herniations that require the assistance of a disc herniation specialist.
If you’ve been living in pain, it’s time to reach out for professional assistance. Herniations do not heal themselves without decompression or other similar treatments, so seeking help is a must. Dr. Eingorn takes a very thorough approach to chiropractic care and offers a number of non-surgical lumbar decompression treatments. Decompression is a proven technique that Dr. Eingorn has used to help patients who are living with a herniated disc and other similar spinal injuries and issues.
To schedule an appointment to learn more about spinal decompression and the other herniated disc treatment options available to you, give the office of Dr. Eingorn a call today at 646-553-1884.
Herniated Discs Conservative Treatment
Areas of Service
Dr. Eingorn and Better Health Chiropractic (https://betterhealthchiropracticpc.com) provide conservative treatment for disc herniations of the lower back, upper back, and neck for patients from these areas of NYC:
Manhattan, NYC, Midtown NY, Battery Park City NY, Financial District NY, TriBeCa NY, Chinatown NY, Greenwich Village NY, Little Italy NY, Lower East Side NY, NoHo NY, SoHo NY, West Village NY, Alphabet City NY, Chinatown NY, East Village NY, Lower East Side NY, Two Bridges NY, Chelsea NY, Clinton NY, Gramercy Park NY, Kips Bay NY, Murray Hill NY, Peter Cooper Village NY, Stuyvesant Town NY, Sutton Place NY, Tudor City NY, Turtle Bay NY, Waterside Plaza NY, Lincoln Square NY, Manhattan Valley NY, Upper West Side NY, Lenox Hill NY, Roosevelt Island NY, Upper East Side NY, Yorkville NY, Hamilton Heights NY, Manhattanville, Morningside Heights NY, Harlem NY, Polo Grounds NY, East Harlem NY, Randall’s Island NY, Spanish Harlem NY, Wards Island NY, Inwood NY, Washington Heights NY
The post <span lang ="en">What is Conservative Treatment for a Herniated Disc?</span> appeared first on NYC Chiropractor – Better Health Chiropractic New York – Call 646-553-1884.
This blog post originally appeared here: http://bit.ly/2WQ3Nlt
What is Conservative Treatment for a Herniated Disc? published first on https://betterhealthchiropracticnyc.wordpress.com
0 notes
Text
Cervical pain symptoms and treatment
Cervical pain symptoms and treatment is a typical, age-related problem of the cervical spine that is situated in the neck district. This condition is otherwise called neck joint pain or cervical osteoarthritis. With age, the cervical plates steadily face mileage bringing about the breakdown of the design. The liquid present between the cervical circles is lost which makes the spine stiffer, prompting cervical torment. This outcomes in changes during the bones, plates, and joints at the spine of the neck.
Because of the liquid lack of hydration and degeneration of the plates and ligament in the encompassing region, strange development or spray of bones called osteophytes can happen prompting the narrowing of the entry from where spinal nerves leave, causing a connected condition called cervical spinal stenosis.
What is Spondylosis?
Spondylosis is an umbrella term that is utilized to depict any degeneration of the spinal string. Spondylosis manifestations include intense undeniable irritation and back in advanced age. Cervical spondylosis is common among moderately aged and old individuals with over 85% of individuals more seasoned than 60 years being a survivor of this problem that causes cervical neck torment. Early cervical spondylosis can likewise happen yet it is uncommon.
Spondylitis versus Spondylosis
Spondylitis and spondylosis both influence the spinal rope however there is a fundamental distinction between the two. The importance of spondylitis is that it is the irritation of at least one run of the mill cervical vertebrae prompting torment in the spine. Cervical spondylosis for the most part alludes to any sort of degeneration of the spine. Along these lines, despite the fact that the impacts of both the illnesses may be comparable, their starting point and cause are totally extraordinary. Understanding the contrast among spondylosis and spondylitis is significant in light of the fact that it assists the specialists with deciding the course of treatment and the right prescriptions for the patient.
What is cervical lordosis?
Each individual has an ordinary bend of the spine which is known as lordosis. The deficiency of cervical lordosis alludes to the circumstance wherein an individual’s spinal bend curves unusually and in an expanded manner internal. This can prompt inordinate tension on the spinal line that causes agony, distress, and outrageous deadness. The deficiency of cervical lordosis is frequently one of the contributing reasons for extreme instances of cervical spondylosis.
What is Cervical Vertebrae?
Cervical vertebrae of the spine are the most slender and most fragile bundle of seven hard rings present between the foundation of the skull and the thoracic vertebrae at the storage compartment.
Bolt
Side effects OF CERVICAL SPONDYLOSIS
Cervical Spondylosis
Cervical spondylosis side effects can differ from one individual to another and the degree of cervical spine torment relies upon the age of the influenced individual. A portion of the normal spondylosis indications are:
Extreme firmness at the neck prompts indications of cervical agony in neck
Hefty cervical spondylosis migraine that may start at the principle cervical spondylosis torment spaces of the neck
Agony in the shoulder and arms that outcomes in the powerlessness to move the hands
Inability to appropriately turn the head around because of outrageous torment
Spondylosis indications show granulating clamor or sensation when endeavors are made to turn the neck around
With enough rest and appropriate rest, cervical agony side effects will in general improve. The side effects of cervical torment are most extreme in the first part of the day and afterward again around evening time before bed.
In the event that osteophytes cause cervical stenosis in the cervical bone, it squeezes the spinal rope prompting a condition called cervical spondylotic myelopathy. The myelopathy significance is only it alludes to any infection of the spinal rope. The beginning of this auxiliary condition can bring about the accompanying manifestations of spondylosis:
A sensation of unusual shivering, deadness, and shortcoming in the fringe areas like the arms, hands, feet, and legs
Absence of equilibrium and coordination which prompts strolling and development challenges
The spondylosis neck bone prompts strange reflexes and causes arbitrary muscle fits
The event of incontinence or the deficiency of authority over one’s urinary bladder and solid discharges
img
Reason for Cervical pain symptoms and treatment
The typical mileage of the bones in the spinal line are the fundamental cervical spondylosis causes that outcome in degenerative spondylosis. Other potential reasons for cervical torment can be the accompanying:
Bone Spurs or Abnormal Outgrowths of Bones called Osteophytes:
As the spine deteriorates and gets more fragile because of advanced age, the body reacts by developing new and additional unresolved issues the spine more grounded. This strange development of bones or cervical osteophytes is called bone spikes. These additional bones can squeeze the spine, for example, the nerve and the spinal rope in the cervical district prompting an awful instance of cervical circle infection.
Got dried out Spinal Disks:
The spinal string is comprised of little bones called vertebrae which comprises of little liquid filled circles. The liquid in the middle of the bones is thick and behaves like cushion like pads that retain the stun of hefty exercises like lifting, winding and different developments. With age, the liquid can get got dried out driving because of a condition called circle drying up. This makes the bones rub against one another during exercises that cause neck spondylosis and brings about intense agony in the risky space of the neck.
Herniated Disks:
In this condition, spinal plates foster breaks in them that outcome in spillage of the liquid present between them. This inward padding material that breaks out can press against the spinal nerves and bones bringing about deadness of the arms and serious agony.
Injury:
Any kind of neck injury because of a mishap can prompt the beginning of gentle cervical spondylosis which speeds up the maturing interaction of the cervical spine.
Solidness of the Ligament:
Tendons are groups of stringy connective tissue that associates bones and ligaments together. With age, these tendons can become stiffer that influences the general neck development prompting a cervical issue at the neck.
Inordinate Stress and Overuse:
Individuals who are utilized in areas that require substantial liftings like development work and more inclined to foster neck spondylitis and spondylosis. Since the beginning, this sort of occupation squeezes the neck and spinal line prompting early lumbar spondylosis and manifestations of cervical spondylosis.
img
Hazard FACTORS OF CERVICAL SPONDYLOSIS
The most serious danger factor of cervical spondylosis is maturing and thus, it can’t be totally kept from occurring. However, there are surely different elements that can speed up the beginning of this condition. Such factors include:
Neck injury because of a mishap
Business related distressing exercises that require weighty actual activities like hard work
Helpless stance which means going through a similar neck developments or standing firm on your head in an awkward foothold for a delayed timeframe, particularly for individuals who maintain work area sources of income. This is called dreary pressure.
Hereditary variables and family ancestry
Smoking
Being overweight and dormant for an extensive stretch of time
Bolt
STEPS TO PREVENT CERVICAL SPONDYLOSIS
There are sure cervical spondylosis home treatment estimates that can be applied to forestall this condition. These home solutions for cervical agony include:
Keep great consideration of the neck and shoulder district. Try not to stack weighty articles on the head or neck. Try not to rest on a high-pad.
For individuals with work area occupations, focus on the stance you by and large will in general follow during work. Try to extend enough in the middle of your work hours. The fixing of your cervical spine is significant for the duration of the day. Recline your head sometimes.
Swimming is viewed as a casual exercise for cervical torment. Make a point to swim regularly and perform general proactive tasks. Try not to be inert for a significant stretch of time. Exercise for cervical spondylitis is instructed for individuals experiencing manifestations with respect to spondylitis in the neck.
img
Determination OF CERVICAL SPONDYLOSIS
Cervical Spondylosis Diagnosis
How to fix cervical torment? This relies upon how well the illness is analyzed in any case. Making a precise analysis of the condition includes precluding other potential factors that can cause neck torment by and large. Based on the aftereffects of tests, the specialist may allude the patient to a muscular subject matter expert or a nervous system specialist for additional cervical spondylosis treatment. Determination tests include:
Actual Examinations:
The originally set of physical science tests to decide the appropriate course of spondylosis treatment incorporates testing the reflexes of the patient and check for the presence of muscle shortcoming and shortfalls in the tactile nerve work. For cervical spondylitis treatment, specialists additionally run tests to decide the scope of neck development and the overall condition of the general strolling development to comprehend cervical treatment fundamental. This load of tests assist the specialist with comprehension if the spinal nerves and strings are under any kind of additional pressing factor. To affirm the finding of cervical spondylosis, specialists will arrange imaging tests and nerve work tests.
Imaging Tests:
X-Ray Imaging – To check for the presence of bone spikes and other unusual development of spinal bones
Processed Tomography (CT) Scan – To get point by point pictures of the cervical district
X-ray Scan – This technique includes the utilization of radiowaves that assist the specialist with deciding the presence of squeezed nerves
Myelogram – For this situation, an infused stacked with a tracer color is utilized to feature the spaces of the c spine, Coupled with CT Scan or X-Rays, specialists can discover better pictures of the influenced regions.
Nerve Function Tests:
Electromyogram (EMG) – This test is utilized to decide whether the nerves of the body are working in an ordinary manner. EMG records the section of nerve signals in the body by estimating the electrical action of the nerves.
Nerve Conduction Study – Cervical pain symptoms and treatment al pain symptoms and treatment,
0 notes
Text
Spontaneous Regression of a Large Symptomatic Calcified Central Thoracic Disc Herniation: A Case Report with a Review of the Literature-Juniper publishers
Abstract
Disc herniations in the thoracic spine are rare and the incidence of symptomatic thoracic disc herniation (TDH) is 1 in a million. The incidence of asymptomatic TDH varies from 11-13%. They are classified as small (≤10%), medium (11-20%), large (21-40%), or giant (≥41%) based on the extent of canal compromise on advanced imaging. The large symptomatic calcified central TDHs are best treated operatively, as the disc fragment could be adherent to the dura or remain intra-dural [1]. We hereby report a case of one such large central calcified TDH at the T7-T8 level in a 46 year old gentleman who presented with axial mid-thoracic back pain and right-sided radicular symptoms along the intercostal nerve distribution, in addition to tingling and numbness in his lower extremities. The calcified extruded intra-dural disc fragment regressed spontaneously over two and half months, while the patient was waiting for a scheduled elective decompression surgery. The relevant MRI and CT scan images with a review of the salient literature are discussed. We believe this to be the first such case of a spontaneous regression of a large symptomatic central calcified TDH to be reported in English literature that is documented with CT and MRI scans.
Keywords: Disc herniation; Calcification; Thoracic spine; Spontaneous regression; Radiculopathy; Myelopathy
Introduction
The thoracic spine is the least common region to present with a disc herniation in comparison to cervical and lumbar regions. Majority of thoracic disc herniations (THDs) are asymptomatic and detected incidentally on magnetic resonance imaging (MRI). The incidence of asymptomatic TDH varies from 11-13% [2]. They are classified as small (≤10%), medium (11-20%), large (21-40%), or giant (≥41%) based on the extent of canal compromise on advanced imaging studies (i.e. CT and MRI) [1,3]. Thoracic disc herniations (TDHs) are rare and most commonly affect the thoraco-lumbar junction, with the T11-T12 disc being the most frequently herniated due to the greater spinal mobility and weakness of the posterior longitudinal ligament [4]. Up to 75% of thoracic disc herniations occur below the T8 vertebra, and herniation of the upper thoracic spine is very rare. A large proportion of TDHs are asymptomatic and little is known regarding the natural history of symptomatic TDHs. They affect older individuals most commonly, and a history of a precipitating event or trauma is often absent in at least half to two-thirds of the affected individuals [5]. The symptoms are secondary to chronic spinal cord compression with the calcification of an extruded fragment suggestive of co-existent degenerative changes. Younger individuals may present with a soft disc herniation and a history of acute trauma or a precipitating event that is responsive to non-operative management. Patients with a TDH may present with axial back pain, radiculopathy, and/or myelopathy with a neuro deficit. Males are more commonly affected than females, and surgery is the treatment of choice for large symptomatic calcified central TDHs [6]. The discectomy of TDHs constitutes 0.15-4% of all disc surgical procedures and the intra-operative localization of the correct surgical level is challenging [7]. A spontaneous regression of a large symptomatic calcified central TDH is rare and no case report exists to this day to the best of our knowledge in English literature. We hereby report one such case of a spontaneous resorption of a large symptomatic calcified central T7-T8 TDH in a 46 year old gentleman with relevant MRI and CT image illustrations. A review of the relevant literature with some of the proposed theories explaining such a spontaneous regressive phenomenon is also discussed.
Case Report
A 46 year old, right hand dominant academician presented with a seven month history of axial mid-thoracic back pain with discomfort and occasional radicular pain around the right hemi-thorax to the senior author’s office (MRP). The pain was associated muscle spasms on the right side of midline that warranted the intake of non-steroidal anti-inflammatory drugs (i.e. NSAIDs). He had tried a structured physical therapy program and chiropractic treatment for few months, which was marginally helpful in alleviating his symptoms. The pain was aggravated during activities that involved vibration and jarring (especially travelling), and his symptoms were partially relieved with rest and NSAIDs. Increasingly, over the recent three months, he began getting tingling and numbness in his lower extremities that initiated this consultation in our office. His Oswestry disability index (ODI) at the first clinic visit was 32%. The back pain: radicular hemi-thoracic pain ratio was 70:30 at the time of his first consultation. He denied co-existent red flag signs (i.e. bladder or bowel involvement and foot drop). His past medical history was significant for arthritis, hypertension, and type II diabetes mellitus. His past surgical history included a herniorraphy in his early twenties for an inguinal hernia. He was otherwise in good health and denied any recent history of weight loss, night pains, loss of appetite, fever with night sweats, or chills and rigors. At his most recent annual physical check-up, the assessment by his primary care physician was negative for any concerns of malignancy, hemochromatosis, hyperparathyroidism, gout, pseudogout, and hypercalcemic states. His personal history was negative for the use of tobacco products and his alcohol consumption was minimal (<3 drinks per week).
On clinical examination by the senior author (MRP), he had some midline tenderness in the mid-thoracic region over the spinous processes with a good range of motion (ROM) of both the cervical and lumbar spine. Motor strength testing revealed normal strength, tone and power (i.e., Medical Research Council [MRC] grade 5/5 motor strength) in his lower extremities. He had right-sided radiculopathy/anterior-chest band like discomfort with hemi-thoracic tenderness along the course of the T7- T9 dermatomal distribution. His right shoulder and scapular function were normal and negative for intrinsic shoulder pathology. The deep tendon reflexes in his knees and ankles were normal. The Romberg’s sign was negative, his gait was normal, and he effortlessly performed tandem-walking.
A working diagnosis of a potential space occupying lesion (SOL) in the thoracic region, causing mechanical compression of the spinal cord and/or nerve root(s), was suspected. An immediate MRI scan was arranged, which revealed a large mass causing the ventral effacement of CSF flow / signal at the T7- T8 level. His T2 weighted MRI images are illustrated in (Figure 1a & 1b). The differential diagnosis included disc herniation and other benign intra-axial neoplasms (i.e. meningioma and schwannoma). A CT scan was requested to further understand the lesion, study the extent of calcification / bony, and the intradural involvement (if any). The key CT sagittal and axial images are depicted in (Figure 2a & 2b). From these, the diagnosis narrowed down to a large central calcified TDH, following a discussion at the multi-disciplinary team (MDT) meeting.
The patient was seen at the office a week later to discuss the results of his CT and MRI scans. The natural history of disc herniation, available treatment options, risks, complications, prognosis, including watchful waiting, were extensively discussed. Surgical management, using an anterior trans-thoracic approach with a vascular co-surgeon for access, was discussed at length. A surgical discectomy with decompression was recommended and offered, given that he was persistently symptomatic with lower extremity tingling and numbness for at least three months, and because non-operative treatment failed. He chose to electively schedule the surgery in two months (seeking time off work for his post-operative recovery and making alternative arrangements for his academic/professional commitments) with an understanding that it would be undertaken immediately should there be a change in neurology and/or any bladder and bowel involvement.
He was seen in the pre-assessment clinic two weeks prior to the scheduled surgical date, reporting spontaneous improvement in his back pain and anterior-chest band like tightness, and with a resolution of his lower extremity tingling/numbness. His ODI was 4%. The proposed surgery was withheld and an interval MRI scan of his thoracic spine was requested. The T2 weighted images at two months from his initial MRI revealed the regression of the large central calcified TDH and this is illustrated in (Figure 3a & 3b). He had a complete resolution of his symptoms while waiting for surgery and he had normal neurology.He signed a written consent form and permitted us to submit and publish his clinical course of events as a case report provided he remained anonymous.
Discussion
We have reported a case of a large central calcified TDH that has spontaneously regressed over four and half months while the patient was waiting for surgical decompressive surgery. The treatment of choice for a symptomatic large central calcified TDH is operative excision by the anterior trans-throacic approach [8]. Spontaneous regressions of such central calcified discs are very rare and we believe this to be the first such reported case in English literature. The only other case report we could identify in English was a calcified right-sided foraminal T7-T8 TDH with a nucleus pulposus calcification in a 36 year old woman that regressed spontaneously over three months, as reported by Piccirilli et al. [9]. Though interestingly, our case also had the disc herniation occur at the same level (i.e. T7-T8), but it was strikingly different and unique in several aspects, in that our case had
A large central calcified TDH,
The absence of nucleous pulposus calcification, and
A decade older male patient (46 year old gentleman vs. 36 year old woman).
The pathogenesis of this rare phenomenon of spontaneous resorption is poorly understood. Proposed theories postulated to explain it include [10-12]:
Dehydration of the herniated fragment and its subsequent resorption,
Activation of the inflammatory process leading to degradation and resorption,
Re-accommodation of the nucleus pulposus in the inter vertebral disc space, or
The bathing of extruded disc material in epidural space by blood vessels, which facilitate neovascularisation and eventual macrophage infiltration with phagocytosis.
The clinical course of a TDH is variable, and a patient can present with non-spinal symptoms and an atypical pain pattern mimicking other organ system involvement to frank myelopathy. Though the spinal cord is smallest in diameter in the thoracic region, the cord: canal ratio is at least 40% compared to 25% in the cervical region, which make sit sensitive to compressive effects [4]. Varying degrees of myelo-radiculopathy, Brownsequard syndrome to paraplegia are reported with symptomatic TDHs [13]. The incidence of bladder and/or bowel involvement in TDHs varies from 15-20%. A high degree of clinical suspicion, supplemented by a thorough history, physical examination, and confirmation by the appropriate diagnostic imaging, is essential for accurate diagnosis.
Calcification of inter vertebral discs could potentially occur at three places:
The annulus fibrosus,
The fibro cartilaginous plate, and
Centrally in the nucleus pulposus.
Von Lushka was the first to describe this phenomenon in adults and observed such calcifications, especially in the annulus fibrosus, to be almost always asymptomatic [14]. The calcification of the nucleus pulposus is secondary to the deposition of amorphous calcium salts in degenerated tissue and might regress spontaneously, especially in children. Disc calcification also correlated significantly with the morphologic degree of degeneration. CT myelography is considered to be the investigation of choice for the evaluation of calcified TDHs, as it demonstrates the degree of canal encroachment / intra-dural extension better than other imaging modalities [15].
Giant TDHs occupy at least 40% of the canal dimensions and were first defined by Hott et al. [3]. They produced severe neurological deficit and were associated with poor functional outcome compared to small and medium TDHs. The authors recommended open thoracotomy, rather than thoracoscopy, in treating such giant calcified TDHs. Barbanera et al. [16] reported a series of 7 patients who had symptomatic giant calcified TDHs and none of them regressed spontaneously. Brown et al. [17] evaluated 55 patients with symptomatic TDHs and observed only 15 patients needed surgery (27%). Encouraged by those findings, they recommended a less aggressive surgical approach, as TDHs did not necessarily cause severe neurological compromise. Wood et al. [2] studied the natural history of asymptomatic TDHs and recommended mere observation to be justifiable, even in symptomatic individuals whose chief complaint was axial spinal pain. Outside of English literature, we identified only four cases (three publications) of a spontaneous resorption of a TDH in the French and Italian languages.
Coevoet et al. [18] reported a case of a T9-T10 protrusion that regressed spontaneously over 13 months. Martinez-Quinone et al. [19] reported a case of a T6-T7 TDH in a 47 year old male that regressed spontaneously. Neither of the two reports specified if those discs were calcified. Eap et al. [20] reported two cases of a spontaneous resorption of a calcified TDH. They included a left T8-T9 foraminal herniation in a 48 year old and a large central T12-L1 herniation (similar to our case) in a 45 year oldpatient.
Komori et al. [21] observed extensive rim enhancement on follow-up MRI imaging to be predictive of spontaneous resorption. A gadolinium enhanced diethylenetriaminepentaacetic acid (Gd- DTPA) MRI could be used to evaluate the neovascularisation zone and might give an insight into the dynamics of disc resorption. Auito et al. [22] studied the determinants of spontaneous resorption in lumbar disc herniation by longitudinal Gd-DTPA enhanced MRI scans, focusing on the rim enhancement zone, and they observed that a higher rim enhancement thickness, a higher degree of HNP displacement, and the age group of 41-50 years to be associated with better resorption rate. The clinical symptom alleviation correlated well with the rate of disc resorption, and dramatic clinical improvement was seen at the end of two months. Unfortunately no such studies have been reported until now for TDHs.
Conclusion
In summary, a large symptomatic calcified central TDH can be treated with careful observation, as long as the patients are capable of coping with the pain and do not have any lower extremity motor weakness or other red flag signs. A better understanding of pathomechanisms that attempt to further elucidate the complex interplay between disc calcification, disc angiogenesis, and disc degeneration is desired, so that strategies are developed to predict disc herniations that regress spontaneously. Studies focusing on investigating such link mechanisms are desired and constitute grounds for further research. Such studies might also explain which TDHs would most likely regress on their own and define the role of surgery vs. non-operative treatment in the management of symptomatic large central calcified TDHs.
To know more about Open Access Journal of Head Neck & Spine Surgery please click on:
https://juniperpublishers.com/jhnss/index.php
To know more about Open access Journals Publishers please click on : Juniper Publishers
#Head and Neck Surgery Journal#Journal of Head Neck & Spine Surgery#Journal of Spine Surgery#Juniper Publishers#Open Access Journals
0 notes
Text
Looking for the best spine doctor in Delhi? Here’s our safe choice!
India is the most prominent destination due to highest quality of treatment provided at an affordable cost. Delhi is a hub for medical tourists to receive the best spine treatment in the country. Dr. Arun Saroha is one of the best spine doctor in Delhi. He is the Director of Neurosurgery at Max Hospital Saket, New Delhi and Gurgaon. He has successfully performed over 7000 spine and brain surgeries in over 20 years of experience and continues to offer life changing treatments to both pediatric and adult patients. He hones surgery of brain and spine including gliomas, meningiomas, pituitary tumors, skull base tumors, craniopharyngiomas, pineal tumors, epilepsy, back spinal cord tumors, pediatric neuro surgery, cervical, thoracic and lumbar disorders, disc herniation, spinal stenosis, spondylolisthesis, spondylotic myelopathy, traumatic and degenerative spinal instability and deformity. He is best known for his exceptionally low complications and high success rate for the most complex patients. There isn’t a condition that cannot be treated in India where the patient needs to go to the West for spine treatment.

Dr. Arun Saroha, one of the best spine doctor in Delhi is also one of the very few in the country who treats pediatric neuro and spine patients. The particular types of brain conditions that arise in children differ in important ways from those found in adults. For children, particular risks and benefits correspond to particular treatments in ways that may be different than for adults. Hence, it is of great importance to consult the right doctor. His surgical expertise also includes extensive experience with minimally invasive techniques as well. Minimally invasive spine surgeries involves smaller incisions, less muscle destruction and lesser blood loss. Dr. Arun Saroha’s reliable and high quality customized treatment makes him one of the top neurosurgeon in India prolonging lives and improving quality of life.
youtube
#best spine doctor in Delhi#Dr. Arun Saroha#Best spine surgeon in India#spine specialist in gurgaon#spine surgeon in gurgaon#Best spine hospital in india#Best spine surgery hospital in india
0 notes