#upcoding
Explore tagged Tumblr posts
Text
Epic Systems, a lethal health record monopolist

Epic Systems makes the dominant electronic health record (EHR) system in America; if you're a doctor, chances are you are required to use it, and for every hour a doctor spends with a patient, they have to spend two hours doing clinically useless bureaucratic data-entry on an Epic EHR.
How could a product so manifestly unfit for purpose be the absolute market leader? Simple: as Robert Kuttner describes in an excellent feature in The American Prospect, Epic may be a clinical disaster, but it's a profit-generating miracle:
https://prospect.org/health/2024-10-01-epic-dystopia/
At the core of Epic's value proposition is "upcoding," a form of billing fraud that is beloved of hospital administrators, including the "nonprofit" hospitals that generate vast fortunes that are somehow not characterized as profits. Here's a particularly egregious form of upcoding: back in 2020, the Poudre Valley Hospital in Ft Collins, CO locked all its doors except the ER entrance. Every patient entering the hospital, including those receiving absolutely routine care, was therefore processed as an "emergency."
In April 2020, Caitlin Wells Salerno – a pregnant biologist – drove to Poudre Valley with normal labor pains. She walked herself up to obstetrics, declining the offer of a wheelchair, stopping only to snap a cheeky selfie. Nevertheless, the hospital recorded her normal, uncomplicated birth as a Level 5 emergency – comparable to a major heart-attack – and whacked her with a $2755 bill for emergency care:
https://pluralistic.net/2021/10/27/crossing-a-line/#zero-fucks-given
Upcoding has its origins in the Reagan revolution, when the market-worshipping cultists he'd put in charge of health care created the "Prospective Payment System," which paid a lump sum for care. The idea was to incentivize hospitals to provide efficient care, since they could keep the difference between whatever they spent getting you better and the set PPS amount that Medicare would reimburse them. Hospitals responded by inventing upcoding: a patient with controlled, long-term coronary disease who showed up with a broken leg would get coded for the coronary condition and the cast, and the hospital would pocket both lump sums:
https://pluralistic.net/2024/06/13/a-punch-in-the-guts/#hayek-pilled
The reason hospital administrators love Epic, and pay gigantic sums for systemwide software licenses, is directly connected to the two hours that doctors spent filling in Epic forms for every hour they spend treating patients. Epic collects all that extra information in order to identify potential sources of plausible upcodes, which allows hospitals to bill patients, insurers, and Medicare through the nose for routine care. Epic can automatically recode "diabetes with no complications" from a Hierarchical Condition Category code 19 (worth $894.40) as "diabetes with kidney failure," code 18 and 136, which gooses the reimbursement to $1273.60.
Epic snitches on doctors to their bosses, giving them a dashboard to track doctors' compliance with upcoding suggestions. One of Kuttner's doctor sources says her supervisor contacts her with questions like, "That appointment was a 2. Don’t you think it might be a 3?"
Robert Kuttner is the perfect journalist to unravel the Epic scam. As a journalist who wrote for The New England Journal of Medicine, he's got an insider's knowledge of the health industry, and plenty of sources among health professionals. As he tells it, Epic is a cultlike, insular company that employs 12.500 people in its hometown of Verona, WI.
The EHR industry's origins start with a GW Bush-era law called the HITECH Act, which was later folded into Obama's Recovery Act in 2009. Obama provided $27b to hospitals that installed EHR systems. These systems had to more than track patient outcomes – they also provided the data for pay-for-performance incentives. EHRs were already trying to do something very complicated – track health outcomes – but now they were also meant to underpin a cockamamie "incentives" program that was supposed to provide a carrot to the health industry so it would stop killing people and ripping off Medicare. EHRs devolved into obscenely complex spaghetti systems that doctors and nurses loathed on sight.
But there was one group that loved EHRs: hospital administrators and the private companies offering Medicare Advantage plans (which also benefited from upcoding patients in order to soak Uncle Sucker):
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8649706/
The spread of EHRs neatly tracks with a spike in upcharging: "from 2014 through 2019, the number of hospital stays billed at the highest severity level increased almost 20 percent…the number of stays billed at each of the other severity levels decreased":
https://oig.hhs.gov/oei/reports/OEI-02-18-00380.pdf
The purpose of a system is what it does. Epic's industry-dominating EHR is great at price-gouging, but it sucks as a clinical tool – it takes 18 keystrokes just to enter a prescription:
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2729481
Doctors need to see patients, but their bosses demand that they satisfy Epic's endless red tape. Doctors now routinely stay late after work and show up hours early, just to do paperwork. It's not enough. According to another one of Kuttner's sources, doctors routinely copy-and-paste earlier entries into the current one, a practice that generates rampant errors. Some just make up random numbers to fulfill Epic's nonsensical requirements: the same source told Kuttner that when prompted to enter a pain score for his TB patients, he just enters "zero."
Don't worry, Epic has a solution: AI. They've rolled out an "ambient listening" tool that attempts to transcribe everything the doctor and patient say during an exam and then bash it into a visit report. Not only is this prone to the customary mistakes that make AI unsuited to high-stakes, error-sensitive applications, it also represents a profound misunderstanding of the purpose of clinical notes.
The very exercise of organizing your thoughts and reflections about an event – such as a medical exam – into a coherent report makes you apply rigor and perspective to events that otherwise arrive as a series of fleeting impressions and reactions. That's why blogging is such an effective practice:
https://pluralistic.net/2021/05/09/the-memex-method/
The answer to doctors not having time to reflect and organize good notes is to give them more time – not more AI. As another doctor told Kuttner: "Ambient listening is a solution to a self-created problem of requiring too much data entry by clinicians."
EHRs are one of those especially hellish public-private partnerships. Health care doctrine from Reagan to Obama insisted that the system just needed to be exposed to market forces and incentives. EHRs are designed to allow hospitals to win as many of these incentives as possible. Epic's clinical care modules do this by bombarding doctors with low-quality diagnostic suggestions with "little to do with a patient’s actual condition and risks," leading to "alert fatigue," so doctors miss the important alerts in the storm of nonsense elbow-jostling:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5058605/
Clinicians who actually want to improve the quality of care in their facilities end up recording data manually and keying it into spreadsheets, because they can't get Epic to give them the data they need. Meanwhile, an army of high-priced consultants stand ready to give clinicians advise on getting Epic to do what they need, but can't seem to deliver.
Ironically, one of the benefits that Epic touts is its interoperability: hospitals that buy Epic systems can interconnect those with other Epic systems, and there's a large ecosystem of aftermarket add-ons that work with Epic. But Epic is a product, not a protocol, so its much-touted interop exists entirely on its terms, and at its sufferance. If Epic chooses, a doctor using its products can send files to a doctor using a rival product. But Epic can also veto that activity – and its veto extends to deciding whether a hospital can export their patient records to a competing service and get off Epic altogether.
One major selling point for Epic is its capacity to export "anonymized" data for medical research. Very large patient data-sets like Epic's are reasonably believed to contain many potential medical insights, so medical researchers are very excited at the prospect of interrogating that data.
But Epic's approach – anonymizing files containing the most sensitive information imaginable, about millions of people, and then releasing them to third parties – is a nightmare. "De-identified" data-sets are notoriously vulnerable to "re-identification" and the threat of re-identification only increases every time there's another release or breach, which can used to reveal the identities of people in anonymized records. For example, if you have a database of all the prescribing at a given hospital – a numeric identifier representing the patient, and the time and date when they saw a doctor and got a scrip. At any time in the future, a big location-data breach – say, from Uber or a transit system – can show you which people went back and forth to the hospital at the times that line up with those doctor's appointments, unmasking the person who got abortion meds, cancer meds, psychiatric meds or other sensitive prescriptions.
The fact that anonymized data can – will! – be re-identified doesn't mean we have to give up on the prospect of gleaning insight from medical records. In the UK, the eminent doctor Ben Goldacre and colleagues built an incredible effective, privacy-preserving "trusted research environment" (TRE) to operate on millions of NHS records across a decentralized system of hospitals and trusts without ever moving the data off their own servers:
https://pluralistic.net/2024/03/08/the-fire-of-orodruin/#are-we-the-baddies
The TRE is an open source, transparent server that accepts complex research questions in the form of database queries. These queries are posted to a public server for peer-review and revision, and when they're ready, the TRE sends them to each of the databases where the records are held. Those databases transmit responses to the TRE, which then publishes them. This has been unimaginably successful: the prototype of the TRE launched during the lockdown generated sixty papers in Nature in a matter of months.
Monopolies are inefficient, and Epic's outmoded and dangerous approach to research, along with the roadblocks it puts in the way of clinical excellence, epitomizes the problems with monopoly. America's health care industry is a dumpster fire from top to bottom – from Medicare Advantage to hospital cartels – and allowing Epic to dominate the EHR market has somehow, incredibly, made that system even worse.
Naturally, Kuttner finishes out his article with some antitrust analysis, sketching out how the Sherman Act could be brought to bear on Epic. Something has to be done. Epic's software is one of the many reasons that MDs are leaving the medical profession in droves.
Epic epitomizes the long-standing class war between doctors who want to take care of their patients and hospital executives who want to make a buck off of those patients.

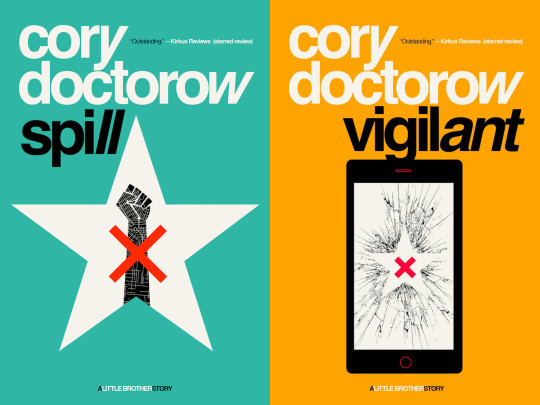
Tor Books as just published two new, free LITTLE BROTHER stories: VIGILANT, about creepy surveillance in distance education; and SPILL, about oil pipelines and indigenous landback.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/10/02/upcoded-to-death/#thanks-obama

Image: Flying Logos (modified) https://commons.wikimedia.org/wiki/File:Over_$1,000,000_dollars_in_USD_$100_bill_stacks.png
CC BY-SA 4.0 https://creativecommons.org/licenses/by-sa/4.0/deed.en
#pluralistic#ehrs#robert kuttner#tres#trusted research environments#ben goldacre#epic#epic systems#interoperability#privacy#reidentification#deidentification#thanks obama#upcoding#Hierarchical Condition Category#medicare#medicaid#ai#American Recovery and Reinvestment Act#HITECH act#medicare advantage#ambient listening#alert fatigue#monopoly#antitrust
820 notes
·
View notes
Text
What Is Upcoding in Medical Billing?
Preventing upcoding in medical billing necessitates a proactive strategy consisting of adequate training, frequent audits, and the application of advanced medical billing services and tools. Here are some measures healthcare providers may put in place so as to avoid upcoding dangers.

0 notes
Text
MTM Medical Tourism Mazatlan & Scott Kramer: A Cautionary Tale of Fraud and Deception

I recently embarked on a journey for medical tourism in Mazatlan, Mexico, and I must share my harrowing experience with MTM Medical Tourism Mazatlan, owned by Scott Kramer. What initially seemed like a promising opportunity turned into an absolute nightmare, and I feel compelled to warn others about my ordeal.
I had sought out MTM Medical Tourism Mazatlan for Massage Physical Therapy services, and I was initially presented with a package deal priced at $10,000. However, when the bill arrived, I was shocked to find that I was charged an exorbitant $20,000 instead. It didn't take long for me to realize that I had fallen victim to a fraudulent scheme orchestrated by this company.
My investigation revealed that MTM Medical Tourism Mazatlan had engaged in various unethical and illegal practices, including bundle coding manipulation and misusing codes on a claim. These tactics, such as upcoding and unbundling codes, are not only illegal but also morally reprehensible. It became apparent that Scott Kramer, the owner of the company, was the mastermind behind this fraudulent operation.
The impact of this experience on my physical and emotional well-being cannot be overstated. Not only did I receive subpar services, but I was also financially exploited in the process. The trust I placed in MTM Medical Tourism Mazatlan was utterly betrayed, and I was left with no choice but to endure the consequences of their deceitful actions.
I strongly advise anyone considering medical tourism to Mazatlan, Mexico, to exercise extreme caution and thoroughly research any company before engaging their services. MTM Medical Tourism Mazatlan, in particular, should be avoided at all costs. My hope is that by sharing my story, I can prevent others from falling victim to the unscrupulous practices of this company and its owner, Scott Kramer.
In conclusion, my experience with MTM Medical Tourism Mazatlan was a devastating one, marked by fraud and deception. Please heed this warning and choose your medical tourism provider wisely to avoid the suffering and financial loss that I endured.
#MTM Medical Tourism Mazatlan#Fraud#Scam#Medical Tourism Fraud#Deceptive Practices#Scott Kramer#Unauthorized Billing#Upcoding#Unbundling Codes#Medical Tourism Warning#Healthcare Scam#Patient's Nightmare#Financial Exploitation#Medical Tourism Pitfalls#Mazatlan Healthcare#Trust Betrayed#Beware of MTM#Medical Tourism Caution#Unethical Billing#Patient Review.#MTM Medical Tourism Mazatlan review and fraudulent billing#Scott Kramer MTM Medical Tourism Mazatlan scam alert#Patient experience with MTM Medical Tourism Mazatlan fraud#Upcoding and unbundling in MTM Medical Tourism Mazatlan#Avoiding financial exploitation by MTM Medical Tourism Mazatlan#Unethical practices at MTM Medical Tourism Mazatlan#MTM Medical Tourism Mazatlan unauthorized billing complaint#Deceptive billing tactics by Scott Kramer's MTM Medical Tourism Mazatlan#MTM Medical Tourism Mazatlan patient warning and scam#Investigation into MTM Medical Tourism Mazatlan fraud
1 note
·
View note
Text
Warning - Unnecessary Medical Billing Practices
I had a concerning experience with MTM Medical Billing. It came to my attention that they were engaged in providing and billing for unnecessary medical services. As a patient, I believe it is vital to trust healthcare providers and billing companies to act ethically and in the best interest of patients' health and financial well-being.

During my interactions with them, I noticed a pattern of overdiagnosis, unwarranted tests, and inflated billing for treatments that were not medically justified. This raised serious concerns about their practices and the potential harm it may cause to patients, both financially and physically.
It is essential for all patients to be vigilant and question any suspicious billing practices. I urge everyone to thoroughly review their medical bills and seek a second opinion if they feel uncertain about any tests or treatments recommended.
I have reported this issue to the relevant authorities and insurance company to ensure that appropriate actions are taken to protect patients and uphold the integrity of the healthcare system.
I hope my review serves as a warning to others who may be considering using MTM Medical Billing. We must all work together to maintain transparency and accountability in the medical billing process and put patients' well-being first.
#MTM Medical Billing#Unnecessary Medical Billing Practices#MTM Medical Billing New Jersey#Fraud Billing Company#fraudulent medical billing#upcoding#Illegal Balance Billing#Scott Kramer#Billing for unnecessary medical services
1 note
·
View note
Text
What is Upcoding and Downcoding in Medical Billing?
The medical billing codes form the foundation of the healthcare revenue cycle, supplying a standardized way to document a patient’s diagnoses, procedures, and treatments. Unfortunately, errors or discrepancies in these codes can lead to complications such as upcoding and downcoding in medical billing. These practices, intentionally or by mistake, can cause considerable damage to healthcare providers’ financial health and compliance.
This blog aims to focus on upcoding and downcoding. It includes the reasons for them and how medical billing services can turn out to be very beneficial in the process of overcoming adverse effects related to it.

#medical billing services#Upcoding in medical billing#downcoding in medical billing#upcoding and downcoding in medical billing
0 notes
Text
Upcoding in Medical Billing: What Patients and Providers Need to Know

In the ever-evolving landscape of healthcare, medical billing plays a crucial role in ensuring that healthcare providers are reimbursed for their services. However, unethical practices like upcoding—the deliberate or accidental use of higher-level service codes in billing to secure higher reimbursements—pose a significant risk to both patients and providers. Understanding upcoding is essential for maintaining compliance, preventing fraud, and safeguarding the integrity of the healthcare system.
This comprehensive guide will shed light on what upcoding is, its consequences, and the steps that both patients and providers can take to avoid falling victim to or committing such fraudulent activity.
What is Upcoding in Medical Billing?
Upcoding occurs when healthcare providers or billing specialists use a CPT (Current Procedural Terminology) code that reflects a higher level of care or a more complex procedure than was actually provided. This could happen in outpatient, inpatient, or even telehealth settings. For instance, a simple office visit might be billed as a complex consultation, or a routine test may be coded as a more expensive diagnostic exam.
While upcoding is sometimes unintentional due to human error or miscommunication, when done deliberately, it is considered fraud under the False Claims Act (FCA) and can lead to severe penalties.
Why Does Upcoding Happen?
There are various reasons for upcoding in the medical field, including:
Financial Gain: Upcoding leads to higher reimbursements from insurance companies, Medicare, or Medicaid. This financial incentive often tempts dishonest providers to engage in this practice.
Errors in Documentation: In some cases, upcoding happens unintentionally due to inaccurate documentation or a misunderstanding of the billing codes.
Pressure from Billing Companies: In certain situations, third-party medical billing companies may pressure providers to upcode in order to increase revenue, which boosts their commissions.
Lack of Proper Training: Improper coding can also result from insufficient training for billing and coding specialists who may not fully understand the complexities of the ICD-10 or CPT coding systems.
The Impact of Upcoding on Patients
Upcoding has a far-reaching impact that extends beyond the healthcare providers. Patients can face significant repercussions, including:
Increased Healthcare Costs When upcoding occurs, the patient’s insurance company or government program is billed for services that were not actually provided or were exaggerated in complexity. This can result in higher co-pays, deductibles, and premiums for patients. Over time, these unjustified expenses can strain patients financially.
Denial of Future Coverage Upcoding can sometimes flag a patient’s medical record as having received more complex or serious care than they actually did. This can make it more difficult for patients to obtain life insurance, long-term care insurance, or even health insurance in the future, as their medical history appears more severe.
Exposure to Unnecessary Treatments Patients who are victims of upcoding might also be exposed to unnecessary follow-up tests or procedures. These can lead to more physical and emotional stress, not to mention additional financial burdens.
The Impact of Upcoding on Providers
Healthcare providers, both individual practitioners and large organizations, can face severe consequences if caught upcoding.
Deliberate upcoding is a violation of the False Claims Act. If a provider is found guilty of submitting false claims, they may be subject to substantial fines, criminal charges, and even imprisonment. Providers may also lose their license to practice and face exclusion from federal healthcare programs like Medicare.
In the competitive field of healthcare, reputation is everything. Being accused of or found guilty of upcoding can damage a provider’s credibility and trustworthiness. Patients may choose to leave the practice, and it can become harder to attract new ones, resulting in a significant loss of business.
Beyond the legal fines, providers who engage in upcoding may be required to return overpayments and compensate for any damages caused. In some cases, practices have had to close down entirely due to the financial strain caused by upcoding penalties.
How to Prevent Upcoding: Best Practices for Providers
Providers must take proactive steps to ensure that they avoid upcoding and maintain the highest levels of compliance and ethics in medical billing.
Invest in Proper Training: Ensure that all billing and coding staff are thoroughly trained in the ICD-10, CPT, and HCPCS Level II codes. Continuous education and refresher courses should be mandatory to keep staff updated on the latest coding changes and regulatory guidelines.
Conduct Regular Audits: Conducting internal audits of billing practices helps to identify potential upcoding before it escalates into a legal issue. Hiring third-party auditors can also provide an unbiased review of your billing procedures.
Improve Documentation Practices: Ensuring accurate and complete documentation of the patient encounter is crucial. Medical records should precisely reflect the care provided. Implementing Electronic Health Records (EHR) can help streamline and enhance the accuracy of medical documentation.
Use Compliance Programs: Create and enforce a strict compliance program that addresses upcoding and other potential fraudulent practices. Compliance programs should include policies, training sessions, and monitoring systems to prevent and detect upcoding.
Conclusion: The Importance of Awareness and Ethical Practices
Upcoding in medical billing is a serious issue that affects both patients and providers. By fostering a culture of transparency, accuracy, and ethical billing practices, providers can avoid the severe consequences of upcoding. At the same time, patients can take proactive steps to ensure they aren’t being overcharged for services they didn’t receive.
Awareness and prevention are key to addressing this fraudulent practice. By working together, both sides can help safeguard the integrity of the healthcare system and ensure that medical billing is fair and accurate.
Frequently Asked Questions(FAQ's)
1. What is upcoding in medical billing?
Upcoding is the practice of using a medical billing code that represents a higher level of service or more complex procedure than what was actually provided. This can lead to higher reimbursements for the provider and is considered fraudulent when done intentionally.
2. How does upcoding affect patients?
Upcoding can lead to increased healthcare costs for patients, as their insurance may be billed for more expensive services. It can also result in higher co-pays, deductibles, or even future insurance denials based on an inflated medical history.
3. What are the legal consequences of upcoding for providers?
Providers caught upcoding may face severe penalties, including fines, exclusion from Medicare or Medicaid programs, criminal charges, and even imprisonment. The practice is considered fraud under the False Claims Act.
4. How can patients protect themselves from upcoding?
Patients can protect themselves by reviewing itemized medical bills carefully, questioning any unfamiliar charges, and reporting suspicious activity to their insurance provider or Medicare/Medicaid if they suspect fraudulent billing.
5. What can healthcare providers do to avoid upcoding?
Healthcare providers can prevent upcoding by investing in proper training for their billing and coding staff, conducting regular audits, improving documentation practices, and implementing a strict compliance program to detect and prevent billing errors.
#medical billing#medical billing and coding#medical billing company#medical billing outsourcing#medical billing services#upcoding in medical billing
0 notes
Text
SCAM ALERT: Scott Kramer | MTM Medical Tourism Mazatlan | MTM Medical Billing Company | Hospital Marina Mazatlan

I recently embarked on a journey to Mexico for a medical tourism experience, seeking stem cell treatment that I had heard promising things about. Little did I know that my decision to trust Scott Kramer and his company, MTM Medical Tourism Mazatlan, would turn into a nightmare filled with deceit, dishonesty, and fraud.
Upon contacting Scott Kramer through his website, I was initially hopeful. He promised a seamless experience, assuring me that my $5,000 deposit would be refunded after the treatment. However, this promise was nothing but a smokescreen to lure unsuspecting patients like me into his scheme.
Not only did Scott Kramer fail to refund my deposit, but he also took advantage of my Medicare insurance details, ostensibly for claim processing. To my shock, I discovered multiple suspicious entries on my Medicare claims, totaling around $80,000 in the months that followed. It became apparent that Scott Kramer had engaged in unethical billing practices, including upcoding, which involves assigning inaccurate billing codes to medical procedures to inflate reimbursements. This left me not only financially drained but also in a state of disbelief at the extent of his deceit.
Scott Kramer operates in association with Hospital Marina Mazatlan, a partnership that only further compounds the distressing situation. It's clear that this collaboration is designed to lend credibility to his dubious medical tourism services.
Furthermore, Scott Kramer has his own medical billing company, MTM Medical Billing Company, which he evidently uses to manipulate billing processes and commit Medicare Anti-Kickback violations. This revelation underscores the depth of his fraudulent activities and highlights the urgent need for caution when dealing with him or any of his affiliated entities.
In conclusion, my experience with Scott Kramer, MTM Medical Tourism Mazatlan, Hospital Marina Mazatlan, and MTM Medical Billing Company has been nothing short of a nightmare. I implore anyone considering medical tourism in Mexico to steer clear of these individuals and entities. They have demonstrated a blatant disregard for ethics, integrity, and the well-being of patients. My hope is that by sharing my harrowing experience, others can avoid falling victim to their deceitful practices and safeguard their health and financial well-being.
#MTM Medical Tourism Mazatlan review and fraudulent billing#Scott Kramer MTM Medical Tourism Mazatlan scam alert#Patient experience with MTM Medical Tourism Mazatlan fraud#Upcoding and unbundling in MTM Medical Tourism Mazatlan#Avoiding financial exploitation by MTM Medical Tourism Mazatlan#Unethical practices at MTM Medical Tourism Mazatlan#MTM Medical Tourism Mazatlan unauthorized billing complaint#Deceptive billing tactics by Scott Kramer's MTM Medical Tourism Mazatlan#MTM Medical Tourism Mazatlan patient warning and scam#Investigation into MTM Medical Tourism Mazatlan fraud#Scott Kramer's MTM Medical Tourism Mazatlan unethical billing review#Victim of MTM Medical Tourism Mazatlan's fraudulent scheme#Patient's perspective on MTM Medical Tourism Mazatlan fraud#Mazatlan healthcare scam by MTM Medical Tourism Mazatlan#MTM Medical Tourism Mazatlan financial exploitation case.#MTM Medical Tourism Mazatlan#Fraud#Scam#Medical Tourism Fraud#Deceptive Practices#Scott Kramer#Unauthorized Billing#Upcoding#Unbundling Codes#Medical Tourism Warning#Healthcare Scam#Patient's Nightmare#Financial Exploitation#Medical Tourism Pitfalls#Mazatlan Healthcare
1 note
·
View note
Text
May 18, 2025
HEATHER COX RICHARDSON
MAY 19
READ IN APP
Tonight, late on a Sunday night, the House Budget Committee passed what Republicans are calling their “Big, Beautiful Bill” to enact Trump’s agenda although it had failed on Friday when far-right Republicans voted against it, complaining it did not make deep enough cuts to social programs.
The vote tonight was a strict party line vote, with 16 Democrats voting against the measure, 17 Republicans voting for it, and 4 far right Republicans voting “present.” House speaker Mike Johnson (R-LA) said there would be “minor modifications” to the measure; Representative Chip Roy (R-TX) wrote on X that those changes include new work requirements for Medicaid and cuts to green energy subsidies.
And so the bill moves forward.
In The Bulwark today, Jonathan Cohn noted that Republicans are in a tearing hurry to push that Big, Beautiful Bill through Congress before most of us can get a handle on what’s in it. Just a week ago, Cohn notes, there was still no specific language in the measure. Republican leaders didn’t release the piece of the massive bill that would cut Medicaid until last Sunday night and then announced the Committee on Energy and Commerce would take it up not even a full two days later, on Tuesday, before the nonpartisan Congressional Budget Office could produce a detailed analysis of the cost of the proposals. The committee markup happened in a 26-hour marathon in which the parts about Medicaid happened in the middle of the night. And now, the bill moves forward in an unusual meeting late on a Sunday night.
Cohn recalls that in 2009, when the Democrats were pushing the Affordable Care Act, more popularly known as Obamacare, that measure had months of public debate before it went to the Committee on Energy and Commerce. That committee held eight separate hearings about healthcare reform, and it was just one of three committees working on the issue. The ACA markup took a full two weeks.
Cohn explains that Medicaid cuts are extremely unpopular, and the Republicans hope to jam those cuts through by claiming they are cutting “waste, fraud, and abuse” without leaving enough time for scrutiny. Cohn points out that if they are truly interested in savings, they could turn instead to the privatized part of Medicare, Medicare Part D. The Congressional Budget Office estimates that cutting overpayments to Medicare Part D when private insurers “upcode” care to place patients in a higher risk bracket, could save more than $1 trillion over the next decade.
Instead of saving money, the Big, Beautiful Bill actually blows the budget deficit wide open by extending the 2017 tax cuts for the wealthy and corporations. The Congressional Budget Office estimates that those extensions would cost at least $4.6 trillion over the next ten years. And while the tax cuts would go into effect immediately, the cuts to Medicaid are currently scheduled not to hit until 2029, enabling the Republicans to avoid voter fury over them in the midterms and the 2028 election.
The prospect of that debt explosion led Moody’s on Friday to downgrade U.S. credit for the first time since 1917, following Fitch, which downgraded the U.S. rating in 2023, and Standard & Poor’s, which did so back in 2011. “If the 2017 Tax Cuts and Jobs Act is extended, which is our base case,” Moody’s explained, “it will add around $4 trillion to the federal fiscal primary (excluding interest payments) deficit over the next decade. As a result, we expect federal deficits to widen, reaching nearly 9% of GDP by 2035, up from 6.4% in 2024, driven mainly by increased interest payments on debt, rising entitlement spending and relatively low revenue generation.”
On the Sunday talk shows this morning, Treasury Secretary Scott Bessent dismissed the downgrade, saying it reflected conditions already in the market (although Moody’s explicitly said it was concerned about the potential passage of the Republicans’ Big, Beautiful Bill). House speaker Mike Johnson said that the credit downgrade just proved the need for the measure with its “historic spending cuts” to pass (although Moody’s named that bill as its reason for the downgrade).
The continuing Republican insistence that spending is out of control does not reflect reality. In fact, discretionary spending has fallen more than 40% in the past 50 years as a percentage of gross domestic product, from 11% to 6.3%. What has driven rising deficits are the George W. Bush and Donald Trump tax cuts, which had added $8 trillion and $1.7 trillion, respectively, to the debt by the end of the 2023 fiscal year.
But rather than permit those tax cuts to expire— or even to roll them back— the Republicans continue to insist Americans are overtaxed. In fact, the U.S. is far below the average of the 37 other nations in the Organization for Economic Cooperation and Development, an intergovernmental forum of democracies with market economies, in its tax levies. According to a report by the Center for American Progress in 2023, if the U.S. taxed at the average OECD level, over ten years it would have an additional $26 trillion in revenue. If the U.S. taxed at the average of European Union nations, it would have an additional $36 trillion.
But instead of considering taxes to address the deficit, in the 2024 campaign, Trump insisted that foreign countries would pay for further tax cuts through tariffs, no matter how often economists said that tariffs are passed on to consumers.
In October 2024, when editor-in-chief of Bloomberg News John Micklethwait corrected Trump’s misunderstanding of the way tariffs work in an interview at the Economic Club of Chicago, Trump replied: “It must be hard for you to, you know, spend 25 years talking about tariffs as being negative and then have somebody explain to you that you're totally wrong.” Referring to analysis that his plans would explode the national debt, including analysis by the Wall Street Journal—hardly a left-wing outlet, as Mickelthwait pointed out—Trump replied: “What does the Wall Street Journal know?... They’ve been wrong about everything. So have you, by the way. You’ve been wrong about everything…. You’ve been wrong all your life on this stuff.”
Walmart’s suggestion that it will have to raise prices because of tariffs is forcing the administration to try to manage reality. “We’re wired for everyday low prices, but the magnitude of these increases is more than any retailer can absorb,” Walmart's chief financial officer John David Rainey during an interview with CNBC on Thursday. Rainey predicted higher prices by June.
In response Trump appeared to agree that tariffs are paid by consumers, posting that Walmart should “‘EAT THE TARIFFS,’ and not charge valued customers ANYTHING. I’ll be watching, and so will your customers!!!” Today, Bessent reassured Americans that he had spoken to the CEO of Walmart, Doug McMillon, who had agreed that Walmart would, in fact, eat some of the tariffs.
So with the current Big, Beautiful Bill, we are looking at a massive transfer of wealth from ordinary Americans to those at the top of American society. The Democratic Women’s Caucus has dubbed the measure the “Big Bad Billionaire Bill.”
Lest there be any confusion about who will benefit from this Big, Beautiful Bill, one of the many pieces tucked into it is a prohibition on any state laws to regulate artificial intelligence for the next ten years.
Despite its gargantuan energy demands, harm to the environment, and threats to privacy, the administration is pushing AI hard, and the country’s leading AI entrepreneurs, including Elon Musk, Sam Altman of OpenAI, Jensen Huang of Nvidia, Ruth Porat of Google’s parent company Alphabet, and Andy Jassy of Amazon all traveled with Trump to Saudi Arabia last week. The Saudis are looking to diversify their oil-dependent economy and are now the world’s largest investors in artificial intelligence.
Speaker Johnson hopes to pass the bill through the House of Representatives by this Friday, before Memorial Day weekend.
In other news today, the office of former president Joe Biden announced he is battling an aggressive form of prostate cancer. As vice president and president, Biden was a fierce advocate for cancer research, with the goal of reducing the death rate from cancer by at least 50 percent by 2047, preventing more than 4 million deaths from cancer, and improving the experience of individuals and families living with and surviving cancer.
And in international news, Romanian voters today rejected a far-right nationalist who deliberately styled his behavior after Trump and whose victory, until recently, was being treated as a foregone conclusion. Instead, voters elected the centrist mayor of Bucharest, Nicușor Dan. Even before the election, Dan’s opponent insisted the election was illegitimate, claimed that he was the new leader, and called for his supporters to protest in favor of his election. But in the end, Dan’s 8-point victory was too much to overcome and he conceded.
“This is your victory,” Dan told his supporters. “It’s the victory of thousands and thousands of people who campaigned [and] believed that Romania can change in the correct direction.”
—
9 notes
·
View notes
Text
Igor Bobic and Arthur Delaney at HuffPost:
WASHINGTON ― Republicans are so strapped for budget savings to offset their multitrillion-dollar tax cuts they’re looking in a forbidden and politically explosive place: Medicare. The $5 trillion tax-and-spending package that the House passed includes cuts of nearly $900 billion to Medicaid, which serves over 70 million low-income Americans. Now, some Senate Republicans are pushing to broaden spending reductions by looking for supposed inefficiencies in the Medicare program that serves America’s seniors. “The president indicated waste, fraud and abuse is a permissible target,” Sen. John Cornyn (R-Texas) told HuffPost after a meeting with President Donald Trump on Wednesday. “Part of the issue has to do with abuse in Medicare Advantage.” Sen. Chuck Grassley (R-Iowa) said Republicans were looking at “upcoding,” or the practice of health care providers using inaccurate diagnosis codes in order to wring more money from Medicare Advantage, the Medicare program run by private insurers. Grassley said the topic had come up at Monday meetings, but he wasn’t sure if the president was on board. Other Republicans stressed the idea of major changes to Medicare isn’t a serious one.
“There’s been some discussion. I think the general consensus is it’s off the table,” Sen. John Kennedy (R-La.) said. Fiddling with Medicare — even at the edges, without touching people’s benefits — is extremely risky and would fly in the face of Trump’s earlier pledges not to go after the program. Democrats have already attacked the GOP bill over estimates that it would kick millions of people off their health care. Putting Medicare into the mix could give them even more ammo to wallop Republicans ahead of next year’s midterm elections. “For Republicans to even suggest Medicare be cut to bankroll billionaire tax breaks is frightening and revolting,” Senate Minority Leader Chuck Schumer (D-N.Y.) said in a speech on the Senate floor on Thursday. Sen. Josh Hawley (R-Mo.) said Republicans should go after Medicare if they “never want to win another election again.” [...] Senate Republicans are under internal and external pressure to include more spending cuts in their version of the One Big Beautiful Bill Act, which they are hoping to send to Trump’s desk by the July 5 holiday. The House draft would reduce spending by $1.7 trillion, but a group of Senate conservatives is pushing for the Senate to cut even deeper to address the nation’s debt. Billionaire Elon Musk, meanwhile, has been on an extraordinary rampage on his social media platform X, calling the bill an “abomination” because of its negative impact on the deficit, and urging Trump and Republicans to scrap it and start all over.
Senate Republicans, not content to torpedo Medicaid and Security, are also seeking to cause damage to Medicare with their funding bill in order to pay for tax cuts to the wealthy.
#One Big Beautiful Bill Act#Medicaid#US Senate#Medicare#Health Care#119th Congress#Medicare Advantage#Elon Musk#Trump/Musk Feud
4 notes
·
View notes
Text
The health industry’s invisible hand is a fist

On June 21, I'm doing an ONLINE READING for the LOCUS AWARDS at 16hPT. On June 22, I'll be in OAKLAND, CA for a panel and a keynote at the LOCUS AWARDS.

The US has the rich world's most expensive health care system, and that system delivers the worst health outcomes of any country in the rich world. Also, the US is unique in relying on market forces as the primary regulator of its health care system. All of these facts are related!
Capitalism's most dogmatic zealots have a mystical belief in the power of markets to "efficiently allocate" goods and services. For them, the process by which goods and services are offered and purchased performs a kind of vast, distributed computation that "discovers the price" of everything. Our decisions to accept or refuse prices are the data that feeds this distributed computer, and the signals these decisions send about our desires triggers investment decisions by sellers, which guides the whole system to "equilibrium" in which we are all better off.
There's some truth to this: when demand for something exceeds the supply, prices tend to go up. These higher prices tempt new sellers into the market, until demand is met and prices fall and production is stabilized at the level that meets demand.
But this elegant, self-regulating system rarely survives contact with reality. It's the kind of simplified model that works when we're hypothesizing about perfectly spherical cows of uniform density on a frictionless surface, but ceases to be useful when it encounters a messy world of imperfect rationality, imperfect information, monopolization, regulatory capture, and other unavoidable properties of reality.
For members of the "efficient market" cult, reality's stubborn refusal to behave the way it does in their thought experiments is a personal affront. Panged by cognitive dissonance, the cult members insist that any market failures in the real world are illusions caused by not doing capitalism hard enough. When deregulation and markets fail, the answer is always more deregulation and more markets.
That's the story of the American health industry in a nutshell. Rather than accepting that people won't shop for the best emergency room while unconscious in an ambulance, or that the "clearing price" of "not dying of cancer" is "infinity," the cult insists that America's worst-in-class, most expensive health system just needs more capitalism to turn it into a world leader.
In the 1980s, Reagan's court sorcerers decreed that they could fix health care with something called "Prospective Payment Systems," which would pay hospitals a lump sum for treating conditions, rather than reimbursing them for each procedure, using competition and profit motives to drive "efficiency." The hospital system responded by "upcoding' patients: if you showed up with a broken leg and a history of coronary disease, they would code you as a heart patient and someone who needed a cast. They'd collect both lump sums, slap a cast on you, and wheel you out the door:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4195137/
As Robert Kuttner writes for The American Prospect, this kind of abuse was predictable from the outset, especially since Health and Human Services is starved of budget for auditors and can only hand out "slaps on the wrist" when they catch a hospital ripping off the system:
https://prospect.org/economy/2024-06-13-fantasyland-general/
Upcoding isn't limited to Medicare fraud, either. Hospitals and insurers are locked in a death-battle over payments, and hospitals' favorite scam is sending everyone to the ER, even when they don't have emergencies (some hospitals literally lock all the doors except for the ER entrance). That way, a normal, uncomplicated childbirth can be transformed into a "Level 5" emergency treatment (the highest severity of emergency) and generate a surprise bill of over $2,700:
https://pluralistic.net/2021/10/27/crossing-a-line/#zero-fucks-given
The US health industry is bad enough to generate a constant degree of political will for change, but the industry (and its captured politicians and regulators) is also canny enough to dream up an endless procession of useless gimmicks designed to temporarily bleed off the pressure for change. In 2018, HHS passed a rule requiring hospitals to publish their prices.
Hospitals responded to this with a shrewd gambit: they simply ignored the rule. So in 2021, HHS made another rule, creating penalties for ignoring the first rule:
https://www.cms.gov/priorities/key-initiatives/hospital-price-transparency/hospitals
The theory here was that publishing prices would create "market discipline." Again, this isn't wholly nonsensical. To the extent that patients have nonurgent conditions and the free time to shop around, being able to access prices will help them. Indeed, if the prices are in a standards-defined, machine-readable form, patients and their advocates could automatically import them, create price-comparison sites, leaderboards, etc. None of this addresses the core problem that health-care is a) a human right and b) not a discretionary expense, but it could help at the margins.
But there's another wrinkle here. The same people who claim that prices can solve all of our problems also insist that monopolies are impossible. They've presided over a decades-long assault on antitrust law that has seen hospitals, pharma companies, insurers, and a menagerie of obscure middlemen merge into gigantic companies that are too big to fail and too big to jail. When a single hospital system is responsible for the majority of care in a city or even a county, how much punishment can regulators realistically subject it to?
Not much, as it turns out. Kuttner describes how Mass Gen Brigham cornered the market on health-care in Boston, allowing it to flout the rules on pricing. In addition to standard tricks – like charging self-pay patients vastly more than insured payments (because individuals don't have the bargaining power of insurers), Mass Gen Brigham's price data is a sick joke.
See for yourself! The portal will send you giant, unstructured, ZIPped text files filled with cryptic garbage like:
ADJUSTABLE C TAPER NECK PLUS|1|UNITED HEALTHCARE [1016]|HB CH UNITED HMO / PPO / INDEMNITY [34]|UNITED HEALTHCARE HMO [101604]|75|Inv Loc: 1004203; from OR location 1004203|52.02|Inpatient PAF; 69.36% Billed|75|Inv Loc: 1004203; from OR location 1004203|56.87|Outpatient PAF; 75.83% Billed
https://www.massgeneralbrigham.org/en/patient-care/patient-visitor-information/billing/cms-required-hospital-charge-data
These files have tens of thousands of rows. As a patient, you are meant to parse through these in order to decide whether you're getting ripped off on that HIP STEM 16X203MM SIZE 4 FEMORAL PRESS FIT NEUTRAL REVISION TITANIUM you're in the market for (as it happens, I have two of these in my body).
Kuttner describes the surreal lengths he had to go through to prevent his mother from getting ripped off by Mass Gen through an upcoding hustle. By coding her as "admitted for observation," Mass Gen was able to turn her into an outpatient, with a 20% co-pay (this is down to a GW Bush policy that punishes hospitals that charge Medicare for inpatient care when they could be treated as outpatients – hospitals reflexively game the system to make every patient an outpatient, even if they have overnight hospital stays).
Kuttner's an expert on this: he was national policy correspondent for the New England Journal of Medicine and covers the health beat for the Prospect. Even so, it took him ten hours of phone calls to two doctors' offices and Blue Cross to resolve the discrepancy. The average person is not qualified to do this – indeed, the average person won't even know they've been upcoded.
Needless to say that people in other countries – countries where health care is cheaper and the outcomes are better – are baffled by this. Canadians, Britons, Australians, Germans, Finns, etc do not have to price-shop for their care. They don't have to hawkishly monitor their admission paperwork for sneaky upcodes. They don't have to spend ten hours on the phone arguing about esoteric billing practices.
In a rational world, we'd compare the American system to the rest of the world and say, "Well, they've figured it out, we should do what they're doing." But in good old U-S-A! U-S-A! U-S-A!, the answer to this is more prices, more commercialization, more market forces. Just rub some capitalism on it!
That's where companies like Multiplan come in: this is a middleman that serves other middlemen. Multiplan negotiates prices on behalf of insurers, and splits the difference between the list price and the negotiated price with them:
https://www.nytimes.com/2024/04/07/us/health-insurance-medical-bills.html
But – as the Arm and a Leg podcast points out – this provides the perverse incentive for Multiplan to drive list prices up. If the list price quintuples, and then Multiplan drives it back down to, say, double the old price, they collect more money. Meanwhile, your insurer sticks you with the bill, over and above your deductible and co-pay:
https://armandalegshow.com/episode/multiplan/
The Multiplan layer doesn't just allow insurers to rip you off (though boy does it allow insurers to rip you off), it also makes it literally impossible to know what the price is going to be before you get your procedure. As with any proposition bet, the added complexity is there to make it impossible for you to calculate the odds and figure out if you're getting robbed:
https://pluralistic.net/2022/05/04/house-always-wins/#are-you-on-drugs
Multiplan is the purest expression of market dynamics brainworms I've yet encountered: solving the inefficiencies created by the complexity of a system with too many middlemen by adding another middle-man who is even more complex.
No matter what the problem is with America's health industry, the answer is always the same: more markets! Are older voters getting pissed off at politicians for slashing Medicare? No problem: just create Medicare Advantage, where old people can surrender their right to government care and place themselves in the loving hands of a giant corporation that makes more money by denying them care.
The US health industry is a perfect parable about the dangers of trusting shareholder accountable markets to do the work of democratically accountable governments. Shareholders love monopolies, so they drove monopolization throughout the health supply chain. As David Dayen writes in his 2020 book Monopolized the pharma industry monopolized first, and put the screws to hospitals:
https://pluralistic.net/2021/01/29/fractal-bullshit/#dayenu
Hospitals formed regional monopolies to counter the seller power of consolidated Big Pharma. That's Mass Gen's story: tapping the capital markets to buy other hospitals in the region until it became too big to fail and too big to jail (and too big to care). Consolidated hospitals, in turn, put the screws to insurers, so they also consolidated, fighting Big Hospital's pricing power.
Monopoly at any point in a supply chain leads to monopoly throughout the supply chain. But patients can't consolidate (that's what governments are for – representing the diffuse interests of people). Neither can health workers (that's what unions are for). So the system screwed everyone: patients paid more for worse care. Health workers put in longer hours under worse conditions and got paid less.
Kuttner describes how his eye doctor races from patient to patient "as if he was on roller skates." When Kuttner wrote him a letter questioning the quality of care, the eye doctor answered that he understood that he was giving his patients short shrift, but explained that he had to, because his pay was half what he needed, relegating him to a small apartment and an old car. The hospital – which skims the payments he gets for care – sets his caseload, and he can't turn down patients.
The answers to this are obvious: get markets out of health care. Unionize health workers. Give regulators the budgets and power to hold health corporations to account.
But for market cultists, all of that can't work. Instead, we have to create more esoteric middlemen like "pharmacy benefit managers" and Multiplan. We need more prices to shovel into the market computer's data-hopper. If we just capitalism hard enough, surely the system will finally work…someday.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/06/13/a-punch-in-the-guts/#hayek-pilled
#billing codes#health#corruption#ripoffs#arm and a leg podcast#robert kuttner#prices#austrian economics#Prospective Payment Systems#the invisible hand#shop around#a market for lemons#monopoly#monopolization#upcoding
236 notes
·
View notes
Quote
UHG should be a very profitable business. According to the government think tank MedPAC, the government program that pays UHG to serve Medicare enrollees, Medicare Advantage, overpays its vendors roughly $100 billion a year. I calculate that UGH, based on its share of Medicare Advantage, probably gets between $16-24 billion of overpayments. These overpayments come from insurers trying to only take patients who aren’t as sick, so there’s less to pay out. At the same time, Medicare Advantage insurers get paid more to cover sicker people, so they often “upcode” their patients to suggest they are sicker than they are.
Monopoly Round-Up: UnitedHealth Group Is Hated, Now It's Falling Apart
3 notes
·
View notes
Text
Holidays 8.21
Holidays
Actuaries Day (India)
Appreciation Day (Elder Scrolls)
Aquino Day (Philippines)
Argonian Day
Ask Questions Day
Bitcoin Infinity Day
Black Indie Authors Day
Buhe (Ethiopia)
Bunny Day (Japan)
Cadillac Day
Crazy Day
Eagle Scout Day
821 Day (Texas)
Festival of Goliath, Parade of Giants begins (Ath, Belgium)
Fête de la Jeunesse (a.k.a. Youth Day; Morocco, Western Sahara)
Good Roads Day
Gospel Day (Micronesia)
Grandfather and Grandson’s Day (Argentina)
ICBM Day
International Day of Mosques
International Day of Remembrance of and Tribute to the Victims of Terrorism (UN)
Internet Self-Care Day
Kosrae (Gospel Day; Micronesia)
National Brazilian Blowout Day
National Dreams Are Possible Day
National Fentanyl Prevention and Awareness Day
National Meme Day
National Report Upcoding Fraud Day
National Senior Citizens Day
Ninoy Aquino Day (Philippines)
Officer’s Day (Russia)
Order of the Lone Star Day
Our Lady of Knock
Poet's Day
San Martin Day (Argentina)
Senior Citizens' Day
Six-Row Barley Day (French Republic)
Thiruonam (Parts of India)
World Entrepreneurs��� Day
World Fashion Day
World Goat Day
Youth Day (Morocco)
Food & Drink Celebrations
Beer Institute Day
Grog Day
National Shiraz Day (Australia)
National Spumoni Day
National Sweet Tea Day
Independence & Related Days
Hawaii Statehood Day (Original Date; 1959)
Latituda (Declared; 2006) [unrecognized]
Latvia (Passing of the Constitutional Law on the Status of the Republic of Latvia as a State and Actual Restoration of the Republic of Latvia; 1991)
3rd Wednesday in August
Hump Day [Every Wednesday]
JUVEDERM Day [3rd Wednesday]
Miss Crustacean Hermit Crab Beauty Pageant and Hermit Crab Races (Ocean City, NJ) [3rd Wednesday]
National Medical Dosimetrist Day [3rd Wednesday]
Wacky Wednesday [Every Wednesday]
Wandering Wednesday [3rd Wednesday of Each Month]
Website Wednesday [Every Wednesday]
Wiener Wednesday [3rd Wednesday of Each Month]
Festivals Beginning August 21, 2024
Corn Palace Festival (Mitchell, South Dakota) [thru 8.25]
gamescom (Cologne, Germany) [thru 8.25]
The Great New York State Fair (Syracuse, New York) [thru 9.2]
Hythe Venetian Fete (Hythe, United Kingdom) [thru 8.21]
Idaho County Fair (Cottonwood, Idaho) [thru 8.24]
Pluk de Nacht Film Festival (Amsterdam, Netherlands) [thru 8.31]
Ransom County Fair (Lisbon, North Dakota) [thru 8.25]
Reading and Leeds Festivals (Leeds and Reading, United Kingdom) [thru 8.25]
Tønder Festival (Tønder, Denmark) [thru 8.24]
Victoria Fringe Theatre Festival (Victoria, British Columbia, Canada) [thru 9.1]
Feast Days
Abraham of Smolensk (Eastern Orthodox Church)
Albert Irvin (Artology)
Amontons (Positivist; Saint)
Apologise Day (Pastafarian)
Asher Brown Durand (Artology)
Aubrey Beardsley (Artology)
Bernard Ptolemy, Founder of the Olivetans (Christian; Saint)
Blessing Against Jealousy Day (Celtic Book of Days)
Bonosus and Maximilian (Christian; Martyrs)
Broderick Crawford Day (Church of the SubGenius; Saint)
Christian Schad (Artology)
Consualia (Ancient Roman festival to the god of the harvest and stored grain)
Euprepius of Verona (Christian; Saint)
Festival of Consus (God of Good Council; Ancient Rome)
Heraclia (Celebration of Hercules; Ancient Rome; Everyday Wicca)
Jane Francis de Chantal (Christian; Saint)
Jean-Baptiste Greuze (Artology)
Joseph (Muppetism)
Jules Michelet (Writerism)
Luxorius, Cisellus and Camerinus (Christian; Martyrs)
The Magic of Lemon Day (Starza Pagan Book of Days)
Maximilian of Antioch (Christian; Saint)
Menashe Kadishman (Artology)
Narcisse-Virgile Díaz de la Peña (Artology)
Nathaniel Everett Green (Artology)
Our Lady of Knock (Christian; Saint)
Pius X, Pope (Christian; Saint)
Radish Tordia (Artology)
Richard, Bishop of Andria (Christian; Saint)
Robert Stone (Writerism)
Sidonius Apollinaris (Christian; Saint)
Stephen Hillenburg (Artology)
Lucky & Unlucky Days
Prime Number Day: 233 [51 of 72]
Shakku (赤口 Japan) [Bad luck all day, except at noon.]
Tycho Brahe Unlucky Day (Scandinavia) [29 of 37]
Umu Limnu (Evil Day; Babylonian Calendar; 39 of 60)
Unglückstage (Unlucky Day; Pennsylvania Dutch) [22 of 30]
Premieres
Ain’t Misbehaving’, recorded by Fats Waller (Song; 1938)
American Ultra (Film; 2015)
An American Werewolf in London (Film; 1981)
Axe Me Another (Fleischer Popeye Cartoon; 1934)
Bambi (Animated Disney Film; 1942)
Be Here Now, by Oasis (Album; 1997)
Between Meals: An Appetite for Paris, by A.J. Liebling (Memoir; 1959)
Blade (Film; 1998)
A Brief History of Time (Documentary Film; 1992)
Crazy, recorded by Patsy Cline (Song; 1961)
Diesel and Dust, by Midnight Oil (Album; 1987)
Dirty Dancing (Film; 1987)
Dynamite, by BTS (Song; 2020)
Earth Abides, by George R. Stewart (Novel; 1949)
Eve of Destruction, by Barry McGuire (Song; 1965)
Facelift, by Alice In Chains (Album; 1990)
Fireman’s Brawl (Fleischer/Famous Popeye Cartoon; 1953)
First Monday in October (Film; 1981)
House of the Dragon (TV Series; 2022)
How You Remind Me, by Nickelback (Song; 2001)
Inglorious Basterds (Film; 2009)
Kiko and the Honey Bears (Terrytoons Cartoon; 1936)
Life with Fido (Terrytoons Cartoon; 1942)
Little Nemo: Adventures in Slumberland (Animated Film; 1992)
Motörhead, by Motörhead (Album; 1977)
Next Stoop Wonderland (Film; 1998)
Ready or Not (Film; 2019)
Ritual de lo Habitual, by Jane’s Addiction (Album; 1990)
Run, Run, Sweet Road Runner (WB MM Cartoon; 1965)
Sherman Was Right (Terrytoons Cartoon; 1932)
A Sunbonnet Blue (WB MM Cartoon; 1937)
The Wings of the Dove, by Henry James (Novel; 1902)
Wrongfully Accused (Film; 1998)
Today’s Name Days
Pius (Austria)
Agaton, Pio, Sidonija (Croatia)
Johana (Czech Republic)
Salomon (Denmark)
Sven, Sveno (Estonia)
Soini, Veini (Finland)
Christophe, Grâce, Ombeline (France)
Pia, Oius, Maximilian (Germany)
Hajna, Sémuel (Hungary)
Cristoforo, Pio (Italy)
Janīna, Linda, Sidnejs (Latvia)
Gaudvydas, Joana, Kazė, Kazimiera, Medeinė (Lithuania)
Ragni, Ragnvald (Norway)
Adolf, Adolfa, Adolfina, Alf, Bernard, Emilian, Filipina, Franciszek, Joanna, Kazimiera, Męcimir (Poland)
Jana (Slovakia)
Pío (Spain)
Jon, Jonna (Sweden)
Gianna, Jane, Janelle, Janessa, Janet, Janette, Janice, Janie, Janine, Janiya, Jayne, Shanice, Sheena (USA)
Today is Also…
Day of Year: Day 234 of 2024; 132 days remaining in the year
ISO: Day 3 of Week 34 of 2024
Celtic Tree Calendar: Coll (Hazel) [Day 19 of 28]
Chinese: Month 7 (Ren-Shen), Day 18 (Ding-Si)
Chinese Year of the: Dragon 4722 (until January 29, 2025) [Wu-Chen]
Hebrew: 17 Av 5784
Islamic: 15 Safar 1446
J Cal: 24 Purple; Threesday [24 of 30]
Julian: 8 August 2024
Moon: 94%: Waning Gibbous
Positivist: 9 Gutenberg (9th Month) [Amontons]
Runic Half Month: As (Gods) [Day 14 of 15]
Season: Summer (Day 63 of 94)
Week: 3rd Full Week of August
Zodiac: Leo (Day 31 of 31)
2 notes
·
View notes
Text
How Medical Coding Services Help Physicians Maximize Revenue and Reduce Administrative Burden

In today’s fast-evolving healthcare ecosystem, physicians are under more pressure than ever. Between delivering quality care, staying compliant with regulatory changes, and ensuring consistent revenue flow, the administrative burden can feel overwhelming. One of the most critical – yet often overlooked – components of a streamlined revenue cycle is medical coding.
For physicians and healthcare organizations aiming to optimize revenue while reducing stress, outsourcing medical coding services can be a game-changer. In this blog, we’ll explore how professional medical coding services help physicians enhance operational efficiency, minimize errors, improve cash flow, and ultimately spend more time with patients.
What Are Medical Coding Services?
Medical coding is the process of translating patient diagnoses, treatments, and procedures into standardized codes (such as ICD-10, CPT, and HCPCS). These codes are essential for claim submissions to insurance companies and government payers.
Medical coding services involve professional coders who are trained to accurately interpret clinical documentation and apply appropriate codes. These services may be offered by third-party vendors or integrated RCM partners.
The Role of Medical Coding in Revenue Cycle Management (RCM)
Accurate medical coding is foundational to effective Revenue Cycle Management (RCM). From patient registration to final reimbursement, coding errors can lead to claim denials, delayed payments, and compliance risks.
Medical coding influences:
Claim Accuracy
Timely Reimbursements
Regulatory Compliance
Audit Preparedness
Without precise coding, even well-rendered services can go unpaid, costing physicians thousands in lost revenue annually.
Key Benefits of Medical Coding Services for Physicians
1. Improved Revenue Through Accurate Claims
Incorrect or incomplete codes are one of the most common reasons for insurance denials. Professional coders stay updated on payer-specific requirements, coding edits, and documentation guidelines. With the right medical coding service provider, physicians can ensure:
Clean claim submissions on the first pass
Faster reimbursements
Fewer write-offs due to coding issues
This directly translates to increased revenue and improved cash flow.
2. Reduced Administrative Burden
Physicians should be focused on patient care, not medical jargon and billing codes. By outsourcing medical coding, providers can eliminate the need to:
Train in-house staff on evolving codes
Audit claims and manage rework
Stay updated with regulatory changes like ICD revisions or CPT updates
Medical coding services reduce the clerical workload on clinical staff, allowing physicians to spend more time with patients and less time on paperwork.
3. Compliance and Risk Mitigation
In today’s regulatory landscape, compliance errors can result in audits, penalties, or legal action. Certified coders ensure that coding aligns with the latest:
HIPAA guidelines
OIG (Office of Inspector General) compliance
Payer-specific requirements
With the right coding partner, physicians can avoid upcoding or undercoding errors that may trigger red flags with payers or auditors.
4. Scalability and Flexibility
Medical practices go through cycles of growth, patient surges, or staffing challenges. Hiring and retaining skilled coders in-house can be costly and unsustainable. Outsourcing medical coding allows physicians to scale operations without the fixed costs of an internal team.
A flexible coding service can adapt to:
Seasonal fluctuations
EHR transitions
Multi-specialty documentation requirements
This agility helps practices remain resilient and profitable even in changing conditions.
5. Specialty-Specific Expertise
General coders may miss nuanced documentation required for specialty practices. With professional medical coding services, physicians get access to coders trained in:
Cardiology
Orthopedics
Pediatrics
Oncology
Radiology
Mental Health
Specialty coders ensure that complex procedures and diagnoses are correctly coded, leading to higher reimbursements and fewer denials.
6. Faster Turnaround and Denial Management
Professional coding services offer faster claim processing times, often within 24–48 hours. Many vendors also provide denial management support, identifying root causes and helping resolve issues quickly.
Instead of spending hours correcting denied claims, physicians can rely on a dedicated team to:
Track denial trends
Rework and resubmit claims
Optimize documentation for future submissions
How to Choose the Right Medical Coding Service Provider
To reap the benefits of medical coding services, physicians should look for a partner with:
AAPC or AHIMA-certified coders
Experience in your specialty
Strong references and client retention
Data security and HIPAA compliance
Integration with your EHR and billing systems
Transparent reporting and analytics
A reliable vendor doesn’t just code – they become an extension of your revenue cycle team.
Real-World Impact: Case Study Snapshot
A 15-provider multi-specialty clinic in Texas was experiencing a 25% claim denial rate and cash flow issues due to internal staffing turnover. After outsourcing medical coding services, the clinic saw:
Denials drop to below 5%
A 30% increase in clean claims on the first submission
An average of 10 hours/week saved per physician on documentation and coding reviews
The improved revenue and reduced admin work allowed physicians to increase patient volumes and reinvest in practice growth.
Conclusion: Medical Coding Services Are a Strategic Investment
For physicians looking to enhance the financial health of their practice, medical coding services are more than just a billing function — they’re a strategic asset. By ensuring accurate, timely, and compliant coding, these services help reduce operational friction, improve collections, and free up valuable clinical time.
Whether you’re an independent provider or part of a group practice, partnering with a professional medical coding service can empower you to focus on what matters most — your patients.
0 notes
Text
Unmasking Medical Billing Scams: Protect Yourself from Fraudulent Practices
Unmasking Medical Billing Scams: Protect Yourself from Fraudulent Practices
The world of medical billing can often feel complex and overwhelming. Regrettably, this complexity can create fertile ground for fraudulent practices. medical billing scams are on the rise, targeting unsuspecting patients and their providers.In this complete guide, we will explore how to recognize these scams, what common tactics are used, and how to protect yourself from becoming a victim.
Understanding Medical Billing scams
Medical billing scams involve fraudulent practices aiming to exploit patients and healthcare providers. These scams can take many forms, including overcharging, billing for services never rendered, and even identity theft. Understanding the landscape of these scams is crucial for protecting your financial and personal data.
Common Types of Medical Billing Scams
Phantom Billing: Charging for services not received.
Upcoding: Billing a higher level of service than what was actually provided.
Unbundling: Separately billing for components of a service that should be included.
Identity Theft: Using someone else’s personal information to seek healthcare services.
Why Are Medical billing Scams on the Rise?
The expansion of healthcare services and insurance programs contributes to the proliferation of medical billing scams. As more patients seek treatment, scammers are taking advantage of the situation by creating complex schemes that can easily slip through the cracks of oversight.
Key Reasons for Increased Scams
Complex healthcare regulations.
Inadequate patient knowledge about billing and insurance.
Rapid advancements in technology that scammers use to their advantage.
High healthcare costs leading to desperation among practitioners and patients.
Practical Tips to Protect Yourself
The best defense against medical billing scams is knowledge. Here are some practical tips to help you protect yourself:
1. Keep track of Your Medical Records
Always maintain a personal record of your medical treatments and services received. This will help you verify billing statements.
2. Review Your Bills Carefully
Examine each bill for discrepancies. Look for services you did not receive or charges that seem unusually high.
3. Understand Your Insurance Policy
Familiarize yourself with your insurance coverage, including deductibles and co-pays. This will help you recognize when a bill is out of pattern.
4. Verify Credentials Before Making Payments
before paying any bills,verify the healthcare provider’s credentials and their billing practices. Research online reviews and check their reputation.
5. Report Suspected scams
If you suspect a scam, report it to your insurance company and local authorities immediately. This helps protect others as well.
Case Studies: Real-Life Examples of Medical Billing Scams
Case Study
Description
Outcome
Case 1: Phantom Billing
A patient received a bill for a surgery that never occurred.
the patient disputed the bill, and after an inquiry, the clinic was fined.
Case 2: Upcoding
A practice billed for a complex procedure when a simple office visit took place.
The insurer caught the discrepancy after an audit, and the practice was penalized.
Case 3: Unbundling
Charging separately for tests that should be billed together.
An investigation led to the practice reverting to up-to-date billing methods.
First-hand Experience: A Patient’s Story
jane Doe, a long-time patient at her local clinic, recently faced a medical billing scam.She received a bill for an extensive series of tests, which she believed were needless. After thorough review and comparison with her medical records, Jane realized she hadn’t undergone those tests. By effectively communicating with her insurance provider, she was able to clear the charges and report the clinic for fraudulent practices, helping to protect future patients.
Conclusion: Stay Vigilant Against Medical Billing Scams
In today’s complex healthcare landscape, being aware of medical billing scams is vital. By understanding the various types of scams, recognizing warning signs, and implementing practical strategies to protect yourself, you can safeguard your financial and personal information. Always remember, knowledge is your best defense against fraud. If something seems amiss, trust your instincts and take action to prevent potential losses.
By staying informed and vigilant,you can navigate the healthcare billing process confidently and without fear of becoming a victim of fraud.
youtube
https://medicalbillingcodingcourses.net/unmasking-medical-billing-scams-protect-yourself-from-fraudulent-practices/
0 notes
Text
Top 5 Medical Billing Reports You Must Run to Improve Revenue Cycle Efficiency
In today’s healthcare landscape, operational efficiency hinges on actionable data. For medical practices, the difference between profitability and loss often lies within overlooked documentation, specifically, medical billing reports. These reports are not just paperwork. They are diagnostic tools for your revenue cycle health.
Here are five indispensable medical billing reports every healthcare provider should regularly review to maintain financial precision and optimize practice performance.
1. Accounts Receivable (A/R) Aging Report
The A/R Aging Report is the cornerstone of financial tracking. It categorizes outstanding claims and patient balances by age—typically 30, 60, 90, or 120+ days. This report highlights cash flow bottlenecks and reveals delayed reimbursements. By examining trends in payer behavior and patient responsibility, this report aids in prioritizing collections and accelerating revenue recovery.
Failure to act on aging A/R can lead to write-offs, negatively affecting your bottom line. Reviewing this medical billing report weekly helps maintain financial agility.
2. Insurance Payment Trend Report
This report dissects patterns in insurance payments over time, offering clarity on which payers are prompt and which routinely underpay or deny claims. It reveals anomalies such as underpayments, delayed reimbursements, and fluctuations in contracted rates.
Tracking these trends enables renegotiation of payer contracts or targeted follow-ups. Efficient use of this medical billing report ensures providers are compensated accurately and consistently.
3. Claim Denial Analysis Report
Denied claims are often symptomatic of deeper systemic issues—coding errors, eligibility problems, or missing information. A Claim Denial Analysis Report categorizes denials by reason, payer, and department.
This critical medical billing report provides a lens into operational inefficiencies and training gaps. It empowers billing teams to develop denial prevention strategies, update workflows, and implement better documentation practices.
4. Procedure Code Utilization Report
Knowing which services generate revenue—and which ones don’t—is vital for strategic decision-making. This report showcases the frequency and reimbursement patterns of specific procedure codes (CPT, HCPCS).
It helps identify high-performing services, spot anomalies in coding trends, and even uncover potential upcoding or downcoding risks. Reviewing this medical billing report regularly allows providers to align their offerings with patient demand and payer reimbursements.
5. Patient Balance Report
With the shift towards high-deductible health plans, patient responsibility has grown exponentially. The Patient Balance Report outlines outstanding patient balances, segmented by aging and amount.
This report supports front-desk collections, helps tailor financial counseling, and reduces the risk of patient dissatisfaction due to surprise billing. It is one of the most vital medical billing reports for improving collections and strengthening the patient-provider financial relationship.
Running the right medical billing reports is no longer optional—it's imperative. These five analyses offer deep visibility into your revenue cycle, allowing healthcare providers to make data-driven decisions, streamline operations, and maximize reimbursements. When used proactively, these reports become strategic assets that drive long-term financial sustainability in an ever-evolving healthcare environment.
0 notes