#AFib RVR
Explore tagged Tumblr posts
Text
Me: "What brings you to the ER today?"
Patient's family: "Their heart is going really fast. They drank an energy drink."
Me, internally: ....no, okay, stop that, maybe this is a four loko situation or panera lemonade or something, nip that eyeroll in the bud
Me: "How many? What kind?"
Patient's family: "One Celsius can"
Me:
Triage nurse, extremely, extremely tiredly: "just...i'll put the order in, just take them for the ekg."
Me, handing ekg to doctor: "here, from the lobby"
Doc: "whodis?"
Me: "tachycardia. After an energy drink"
Doc:
Me:
Doc: "...why"
Me: "happy new year"
Doc: "go home. Them, not you. You have to stay and suffer with us."
Me: "thanks"
Doc: "do not take that as incentive to bring me something interesting ok. No thu-rvr-days."
#we are so busy today#it has been a crescendo of fuckery today#several months ago literally four times in a row i walked back to hand him an ekg and all of them were afib rvr#by the third one he was like 'you're not allowed to do any more ekgs'
7 notes
·
View notes
Note
hii! what are the effects of prolonged tachycardia with fluctuating bpm ranging from 140-160 for around 30 minutes to a conscious patient? will it cause any brain damage?
The short answer is basically nothing and no.
Tachycardia is any heart rate above 100 in an adult. There are several different kinds of tachycardia, including sinus tachycardia, paroxysmal supraventricular tachycardia, atrial fibrillation with RVR, and ventricular tachycardia. Whether the tachycardia is bad for a person has to do with what kind of tachycardia it is, what the heart rate is, and how long the person is in that rhythm.
The first one we'll talk about is sinus tachycardia. Sinus tachycardia is a normal physiological response to the body's demand for more oxygen and nutrients. Sinus tach happens when someone has a fever, is dehydrated, has blood loss, is in shock, or is having a strong emotional response.
It's one of those things that doesn't need treated in and of itself, though figuring out and treating the cause is important. Once the cause is treated, the heart rate usually drops back down to normal.
There are also times when you intentionally bring the heart rate up above 100- for example, exercise. This is also considered sinus tachycardia. When you exercise, you want your heart rate to be in a target zone, which depending on age can be anywhere from 75-170bpm (the younger you are, the higher the target heart rate).
In the case of exercise, a heart rate of 140-160bpm for a half hour would be completely reasonable. In the case of dehydration or shock, you'd really need to fix the problem, but the heart rate itself isn't going to hurt anyone under about 60 who is otherwise healthy.
Paroxysmal Supraventricular Tachycardia (PSVT) is a condition in which the heart rate randomly increases into the high 100s-low 200s. This heart rate is so fast that the heart doesn't have time to fill with blood in between beats. Because of this, not as much blood is getting out of the heart to the brain and body, which means the person may feel faint, short of breath, or dizzy or even pass out.
People in PSVT may spontaneously convert back into a normal rhythm, or they may need a drug called adenosine given to change them back to a normal rhythm. Adenosine works kind of like a defibrillator- it briefly stops the heart in order to let it restart normally. If this happens frequently, someone may need an ablation- a procedure in which parts of the heart muscle that are causing the rapid heart rate are burned to permanently prevent future attacks.
In order to understand atrial fibrillation with RVR, you have to understand how the heart initiates beats normally. In the heart there are cells in a place called the SA pacemaker node, which send out small electrical signals that work to coordinate a beat across all the cells in the heart.
In atrial fibrillation, lots of cells outside this node try to initiate beats, which causes the top half of the heart to quiver. If a lot of these "beats" get through to the bottom of the heart, that's called Rapid Ventricular Response, or RVR. Afib RVR causes a rapid, irregular heart rate.
Afib RVR can cause the same problem as PSVT- namely that it causes the heart to beat so fast it can't refill with blood in between beats. Usually the first few times this happens the person converts out to a normal rhythm within about a week (or can be converted out with defibrillation or medications). Later this state can become permanent and has to be managed with medications that reduce the heart rate and blood thinners to prevent strokes and heart attacks, which happen because blood gets stuck and clots in the quivering upper part of the heart.
The last one, ventricular tachycardia, is the most dangerous because if not treated it can either become so fast virtually no blood is coming out of the heart (cardiac arrest) or become another dangerous rhythm called ventricular fibrillation (also cardiac arrest, but even worse).
This one is a life-threatening emergency and needs to be treated immediately with CPR (if the person is unconscious) defibrillation and medications.
This was a lot to answer your question, but all this to say that if your person is running 140s-160s because they're working out for a half hour, they're totally fine. If they're 140s-160s because of PSVT they're not fine but they're probably going to convert out of it with a medication or just time. If they're 140s-160s in RVR they're probably uncomfortable and need medical attention but they'll probably be alright. If they're in ventricular tachycardia, they need emergency care.
Of these, the only one that could really cause brain damage is the ventricular tachycardia, but it would have to be a lot faster than 140-160.
24 notes
·
View notes
Text
On Friday, I was chillin in bed then I randomly went into (supposed) Afib RVR that turned into SVT. I got hit with adenosine, fucking died for a few seconds, went into SVT again, got the defib pads slapped on my chest, and then converted back into a normal rhythm. Adenosine works but dear god what an awful, awful experience.
Never am I ever gonna say I want to die ever again. Holy shit. I'm alright though 👍🏼
#weird being a paramedic myself and being the patient like that was weird as fjck#anyway I SWEAR I thought it was so over for me like#my vision faded to white#akira screams into the void#I'm good tho#emergency medicine#ems
5 notes
·
View notes
Text
waiting awkwardly at bedside during a very long rapid response for afib/RVR
nursing: here, try blowing into this straw
resident: I don't think it's gonna do anything, he's in afib--
me: sshhhhh it gives the patient something to focus on
...
resident: ohh, I guess that's one of those attending insights huh?
9 notes
·
View notes
Text
Haven't been posting here because I've been dealing with some health stuff and had an "AFib with RVR" episode in a fucking AutoZone with a bpm of 190 which landed me in the hospital and now I'm feeling generally weird about life because Im sort of like a walking stroke risk rn until I can see a specialist next week(?). anyways.
11 notes
·
View notes
Text
Inside CVICU Nursing: A Veteran's Guide with Jeannie Cisney
In this interview, Kati chats with Jeannie Cisney, MSN RN. She is a 20+ year veteran of the CVICU (cardiovascular intensive care unit). We discuss:
The types of patients you’ll see in a CVICU
Her favorite and least favorite types of patients
A walkthrough of the patient pathway of a typical CABG patient
New grad vs. experienced nurse orientation experience into CVICU
Unexpected challenges of CVICU RNs
The advice she’d give her younger self
Jeannie is my co-author of Cardiac Confidence, a Crash Course for New Cardiac Nurses. To learn more and enroll, click here: https://courses.freshrn.com/p/cardiac-confidence
For a 14-page ECG cheatsheet: https://bit.ly/3Ws75NT
For a free mini-course on how to handle afib with RVR: https://courses.freshrn.com/p/afib-with-rvr
For my cardiac assessment checklist: https://bit.ly/4aV6RTO
For ALL of our cardiac content: https://www.freshrn.com/cardiac-nursing/
Learn more about the FreshRN All-Access Pass here - https://courses.freshrn.com/p/membership
To see our latest course catalog (med-surg, ICU, precepting, charge nurse, ortho, cardiac, neuro courses, and more), click here: https://courses.freshrn.com/
Get weekly tips, encouragement, stories from the bedside, and more - just for nursing students and new nurses at: https://www.freshrn.com/email-sign-up/
Connect With Me Online!
Facebook: https://www.facebook.com/FreshRN
Twitter: https://twitter.com/Kati_Kleber
Pinterest: https://www.pinterest.com/Fresh_RN/
Instagram: https://www.instagram.com/kati_kleber/
TikTok: https://www.tiktok.com/@freshrn
Music credit: Keep My Cool by Benj Heard
Check out this episode!
3 notes
·
View notes
Text
Clinical Cardiac Nursing Concepts: Families in Crisis-Complex Health Problems I (Florida State College ICU – Plan of care Patient 1: newly admitted to ICU for pneumonia, hx: heart failure, COPD, renal disease, diabetes type 2 Strip indicates: Normal sinus rhythm, 80 bpm Assessment: pulses, shortness of breath, sugar Questions: medications? Oxygen at home? Recent hospitalization? Exertion on activity? Allergies? Onset of symptoms? Stage of COPD/ Heart failure? Where do you sleep (pillows?) Nursing interventions: 2L of oxygen, semi/high fowlers position, monitor LOC Expect vital signs to be: O2: 88-92. HR: 80. BP: elevated RR: increased Assessment findings expected: Lung auscultation (crackles), peripheral & respiratory edema, consolidation of chest x-ray Labs: CBC, BMP, Cardiac enzymes, BNP, possible ABG, urinalysis Diagnostics: Sputum culture, Chest Xray, Echocardiogram, Renal US Procedures: Medications: Mucomyst, Antibiotic, Diuretic (Furosemide), Pepcid, Beta blocker, ACE or ARB, Cardiac glycoside (Digoxin) Anticipated provider orders: Incentive spirometry, monitor intake and output, renal & cardiac diet (low fat, low sodium, DASH, Possible Venturi mask if O2 falling Consult: Cardiologist Patient 2: 55 years old, admitted 2 days ago for MI, stent placed, monitor for pseudo hematoma and infection-possible discharge home today. Strip: Symptomatic Bradycardia (40 bpm) Assess: verbal/ physical response, feel for diaphoresis, auscultate heart/ lungs, Vitals: HR: 40 BP: low Medications: beta blocker (when was last given), start Atropine 0.5 one time, IV fluids 500ml bolus Questions: Nursing interventions: stimulate, Educate: slow position changes Anticipated orders: Fluids, pacemaker Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Patient 3: SOB, extreme chest pressure, Vitals: hypertensive, tachycardiac, RR: 28, O2: 94 (Nasal cannula 3L) Monitor: STEMI Interventions: 12 lead EKG, MONA (morphine, oxygen, nitro, aspirin), LOC Assessment: chest pressure (men), epigastric, back pain & increasing fatigue (women), Labs: BMP, CBC, Cardiac enzymes, Coagulation, ABG’s, UA (drug toxicity) Procedures: Cardiac catheter (get consent), Patient 4: Palpitations, heart racing out of chest, pulse fast as fuck Monitor: SVT (Changes to Afib) Interventions: oxygen, IV access, try vagal maneuver, After vagal maneuver, went into AFIB (if AFIB and rapid, call is AFIB with RVR) Monitor: LOC (risk for stroke), Pulses (potential clot, MI), Medications: Anticoags (Warfarin, Eliquis), Diltiazem, FLECAINIDE, Possible heparin infusion (draw coags first) Diagnostics: TEE, Echocardiogram Labs: ABG, Cardiac enzymes, Coags Patient 5: Chest pain, SOB, dizziness, started a few minutes ago Monitor: Normal Sinus Rhythm Interventions: Oxygen, 12 lead EKG, Obtain IV, Blood Labs: Coags, CBC, BMP, Cardiac enzymes Possible causes: Anxiety, Heartburn, Esophageal spasm Patient 6: previous sinus rhythm, V-fib, now V-Tach V-tach with pulse: Cardioversion Patient 7: Asystole Assess patient, Check carotid pulse, non-shockable Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Call code: Epi 1 mg (2 mins CPR) Amiodarone 300mg (2 mins CPR) Epi 1 mg (2 mins CPR) Amiodarone 150mg (2 mins CPR) Epi 1m (2 mins CPR) Lidocaine 1mg/kg Assess H’s and T’s of ACLS Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Read the full article
0 notes
Text
Travel RN - MS/Tele 48's
within same campus. Patient Population: High acuity Tele/M/S, Cardiac heavy, (Afib with RVR, Afib, flutter, blocks), heart cath… Apply Now
0 notes
Text
Read more on observation care from MCG paoer
downloaded in document section of Tablet
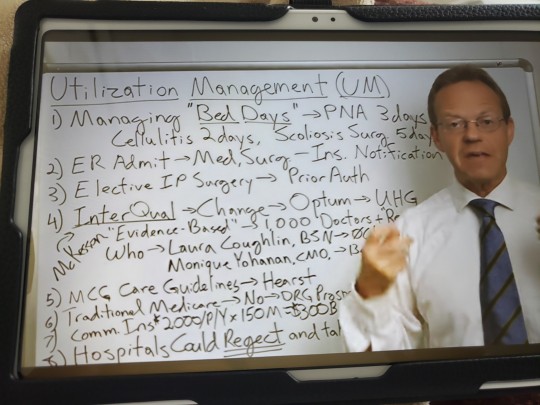
How money works
Managing bed days
Hospital goes to commercial payer
Approval of payment
Clinical crietria
Nurse gives report read doc notes
PNA 3 days, Cellulitis 2 days, Scoliosis 5 days
No one can predict
Takes turn for worse.
PNA goes to pneumonia edema Afib with Rvr
Dripper
Nurse calls again
Pays for 3 days, denies 2 days, pt gets bill for $20k
How do they get in hospital
Er
Ins notification
7 days a week 24 days
Case managers holidays
Did not notify
Elective surgery
Not emergency
PA for these many days
Who decides
#Interqual largest approval date associated with UHG, McKesson, evidence based. What evidence. Circular reasoning. Specific study, criteria, propertiary, registered non physician. 1000..break up, Laura Coughlin BSN no clinical evidence. Monique Yahannan.
#MCG care guidelines Milliman Care Guidelines
Hearst health. Media company.
Bed day standardization in healthcare
Traditional Medicare uses DRG.
How long you stay does not matter. Pay you x amt.
2k per member per year
300b commercial
100b Medicare Adv
400 b goes thru UM
1m providers managed by 1000 powerful MDs and NPs. Huge financial pacts
Who made them king
Negotiate. Hospital ve to agree.
Ins carriers are real sticlers
Replace with InterCare or McGQual.
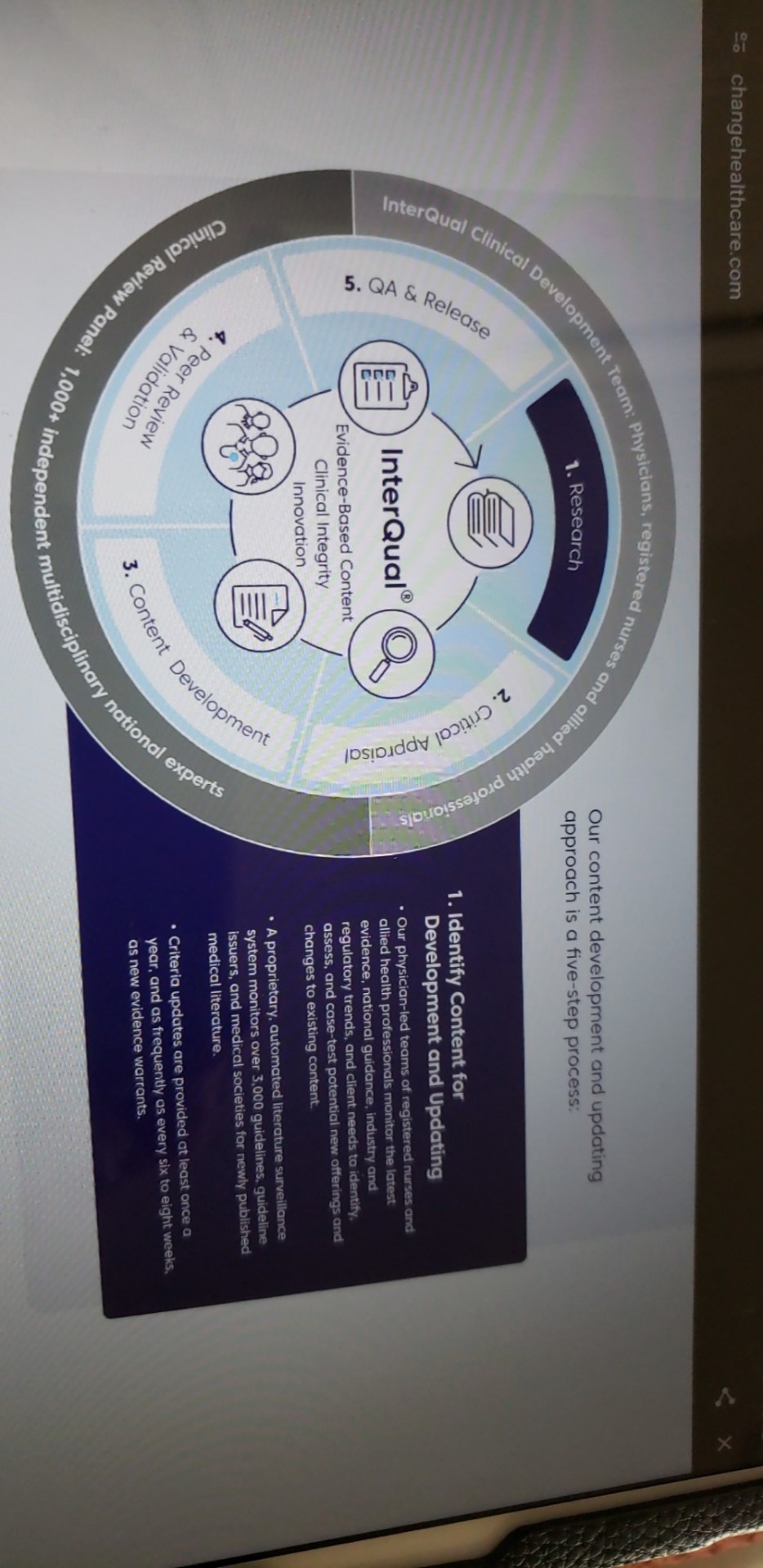
InterQual Evidence based content
Atrius health uses InterQual to make decision confidently about hospital at home for pts against inpatient hospital setting.
Review labs, imaging
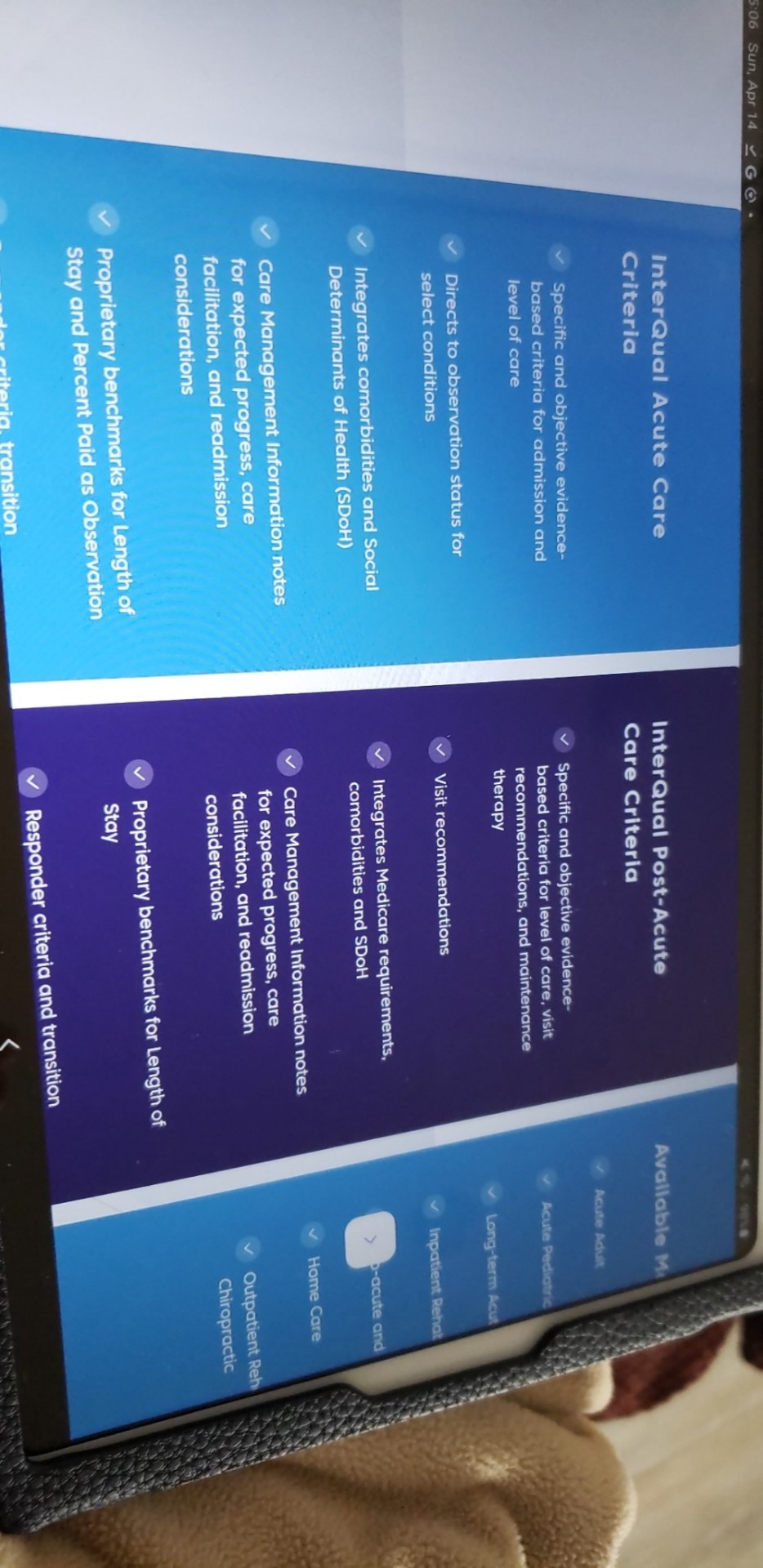
Available modules in Interqual
0 notes
Note
Huh. I’m a cardiology scribe and we use amiodarone all the time for stuff like afib w/ RVR and vfib or vtach. And yeah, I have a whole dot phrase in our medical record system just on its side effects and monitoring we have to do on it. It’s a beast, effective, but yeah, a mess. (It’s lipid-soluble, which is why it’s sticks around in the body for so long)
I had no idea lidocaine had a similar effect. I’m excited to do so research on this. Do we know if it works on the various SVTs of the world? I know adenosine is usually used for that (or diltazem/carvedilol, if that doesn’t work), but is there evidence this has a similar effect?
That mutuals tag game reminded me I wanted to ask you a medical question!
You said you're reading up on amio vs lido, and I was wondering what Lidocaine does in that regard?
Cause its typically seen as a numbing agent, but I know we have injections and lidocaine bags that we keep in the crash carts, though they're rarely used, so I was just curious what it's used for
Lidocaine is a sodium channel blocker, which can give it antiarrhythmic properties. It can be given for fatal tachycarrhythmias such as ventricular fibrillation and ventricular tachycardia. Amiodarone is typically the antiarrhtymic medication given refractory to defibrillation, but lidocaine is also an option. So the real issue is figuring out which one is better.
It seems like lidocaine is more effective based on some meta analyses that I’ve found, but I’m still trying to work things out. Because like, amio can also be used for stuff like a fib with RVR, whereas I’m trying to figure out if lidocaine is used for that as well. Also, amiodarone’s adverse effects suck and its pharmacokinetics show that it stays in the system for a while, whereas lidocaine seems less terrible in that regard, though lidocaine toxicity is a thing, so I’m trying to figure out which drug is the better one for the squad to stock and utilize for protocols.
But yeah! It’s interesting how things come and go in medicine, lidocaine used to be far more popular as an antiarrhythmic before Amiodarone became hugely popular, but now amio is becoming less popular and lidocaine is coming back. But because Amiodarone has been more traditionally used lately, that’s why lidocaine is hardly touched in the code cards.
…I’m still doing research, we’ll see, I’m drowning in articles and my brain is not focusing. But it’s super interesting! I can get more into detail if anybody wants, I love talking about this stuff, but yeah.
General gist: lidocaine can help stop the heart from doing bad fast rhythms. :)
9 notes
·
View notes
Text
Conflicted
So I got an admission this morning who was super hypoxic. She is a DNR/DNI and VERY sick at baseline. Literally all the problems (HfrEF, COPD, GI bleed, clotting disorder with active DVTs on heparin, PVD, HTN, HLD, GERD, RA, CAD, Afib, breast cancer).
She came to me on a BiPAP barely saturating 83%. The internist said they were concerned about aspiration and I was like "ok then BiPAP actually isn't a good option because it just shoves everything down." She is in Afib with RVR with HRs 140-160s though maintaining her BPs. She is extremely uncomfortable. I confirm that she doesn't want intubation. Then I switch her to high flow nasal cannula and she does better for maybe 20 minutes but ends up getting REALLY hypoxic. She got as low as 69%. So back on BiPAP she goes and she hangs out in the 75-85% range.
Now, interestingly, she is still alert and oriented even with such low saturations. I explain to her that I'll do all the respiratory/medical/non-invasive stuff I can but that ultimately to correct her hypoxia she would need intubation. She declines. I explain that she could die if her oxygen does not improve with BiPAP. She expressed understanding of this. I explain that I can keep giving her all her meds or she could opt to be comfortable. In the comfort case, I'd give her morphine and get rid of anything that doesn't support comfort. She said she wants to be comfortable and see her family.
So, I make her "comfort care", delete all the meds, then call her family and update them. The patient had this interesting affect/realization of "yes I know I've been slowly dying."
The thing I feel conflicted about is that I don't think I did a good enough job explaining her medical options. I kind of laid it out as either "this" (all the things) or "that" (comfort). Really, there can be an in between. I could still continue her antibiotics and such. I'm worried I jumped the gun and didn't explain things well enough. Also feel like I didn't discuss with her that the BiPAP would probably come off at some point. She expressed a wish to see her family and I explained to her that I wasn't sure if she would survive that long. I kept the BiPAP on to at least give her a chance of that.
I have a personal bias that I freely admit where I believe people with severe comorbidities who acutely decompensate should opt for comfort. I know that about myself, for better or worse. And I also know that sometimes when you give patients too many options it is overwhelming. Sometimes you have to be simplistic. I guess what I don't want to happen is have her family come and be like "well you just MADE her comfort when REALLY all she wanted was to breathe better."
When I left, my patient was sleepy after getting morphine but it did help her breathe better. Her tidal volumes are still trash but at least she was getting better saturations. It's not sustainable but at least she is cozy now.
I guess the other thing that pushed me in this direction was that the patient was DNR/DNI. So, she's not unaware of how sick she is. She clearly values a quality of life that doesn't involved unnecessary stuff. ...I just wish I was more explicit.
I guess I don't want it to seem like I gave up on her or didn't try. And I don't want it to seem like I misrepresented what was going on, though I could have been more clear that her respiratory issues could be due to a reversible cause and that she could do better, potentially, though I doubt that with her severe comorbidities.
I mean...she was SO hypoxic and not making improvement. 100% FiO2 on BiPAP. 84% SpO2. Not sustainable.
So. Here is anxiety Poppen, sitting and worrying about it. I shared my concerns with the day team and they said they would readdress everything. It's not like we can't add her meds back on if she wants more workup. It's just...when I sit and think about it...I could have ultrasounded her heart and lungs. I could have done more investigating instead of being like "shit your saturations have been less that 84% basically since you got here (2 hours) this looks like this is it." I literally told her that I was worried she was actively dying and she was like, "I know, I have been."
*sigh* I don't typically take work home with me in this way. I think since I have started my ICU job in February I've had 2 other occasions where I came home being like "did I make the right decision?"
I feel like in her case, with how sick she is as baseline that comfort is the best option. And she said she wanted that. I guess I just feel like I didn't give her enough information to make the most informed decision. :-/
Update/Edit: bless the day team for contacting me and telling me that family was in agreement and that the patient wouldn't want any more intervention. I think this just serves as a learning point for me to be more clear. I can explain in between options without making it complicated. I'll be more diligent about this, especially in emergent situations, in the future.
#pa-c#physician assistant#physician associate#pre-pa#pre paid#critical care#icu medicine#medicine#caspa#originstory#palliative care#palliative medicine
14 notes
·
View notes
Text
That moment when you think the patient is gonna be a simple covid pneumonia but you just keep on finding things like afib with rvr and mildly elevated trops then hyponatremia now he had a 2pt drop in Hg in a week and its just... omfg
6 notes
·
View notes
Conversation
table rounding w hangry
Me: Alrighty, in Room 1, we have Mr. Smith. He is a 63y/o male with a history of Afib and Takotsubo cardiomyopathy who presented with flash pulmonary edema and DVT. Cardiology is following. Following extensive diuresis and an increase in his home metoprolol, he is no longer in RVR and now satting mid-90s on room air. Once we get the prior auth on his Lovenox, he can go home.
Attending: Perfect.
Me: He also has an adorable bulldog at home.
Attending: Ah.
Me: Okay, next up in Room 2, we have Ms. Jones. She is a 74y/o female who received allogeneic stem cell transplant about 2 months ago and presented with rash and diarrhea suspicious for diarrhea. Heme/Onc is following. She is on Methylprednisolone with significant improvement in stool volume, now putting less than 500ml out. Her rash originally was ~50% BSA and is now about 20%. She will be discharged on Prednisone taper, pending Heme/Onc recs.
Attending: Good.
Me: And she has a little goldendoodle at home.
Attending: Nice.
Me: All right. Then in Room 3 is Ms. Williams. She is a 67y/o female who presented with urosepsis secondary to new kidney stone. She's had a wild hospital course and was extubated just 2 days ago. It appears that she also is now deaf. We've consulted ENT, and they suspect vestibular neuritis. I reached out to them to ask about starting steroids. She likely will not be returning home for at least another 48hrs while we sort this out.
Attending: I see.
Me: She has a giant derpy mutt at home.
Attending: I take it that you like dogs.
Surrounding coworkers: [in unison] YEP!
48 notes
·
View notes
Link
Check it out! We’ve got another Instagram question panel series for you! Please let us know what you think. Happy Studying!
#FOAMed#Meded#wpw#Afib#Vfib#rvr#deltawaves#diagnosis#usmle#usmlestep1#usmle step1#usmlestep2ck#usmlestep3#stepprep#step1prep#medschool#medschoolblog#medstudent#medstudentblog#medstudy#medstudyblog#medstudyblr#studygram
0 notes
Text
2nd day being pulled to the unit for coverage.
I'm exhausted.
Not so much from the covid pts, but the stupid questions from the medicine interns
"should we get PT/OT on this pt who's paralyzed?"
Almost going to be a medicine senior and can't manage afib with rvr
Do I put the drips on sign out that aren't running?

3 notes
·
View notes