#Birth at Home Midwifery Services
Text
The Gillespie Approach's Craniosacral Fascial Therapy (CFT)
Betsy Richards, our practice’s senior apprentice, recently completed her Craniosacral Fascial Therapy training with the Gillespie Approach! She’s able to work with babies, children, and adults and, as a client of Betsy’s myself, I can say she has a lovely touch and does truly excellent work!
Here’s what Betsy has to say about it!
Have you ever seen a spiderweb and noticed how each of the strands…

View On WordPress
#Betsy Richards#Birth at Home Midwifery Services#Birth Trauma#Colic#CONSTIPATION#Craniosacral Fascial Therapy#Gillespie Approach#Headaches#Migraines#Oral Tethers#Reflux#Senior Apprentice#Torticollis
0 notes
Text
Title:
Labors of Love Birth Center, LLC
Description:
"Labors of Love Midwifery and Birth Center are your experts in natural birth, water birth and normal deliver of babies. Our midwives are here to better serve the mom's of Greenville, Spartanburg and the Upstate of SC. We can deliver you at your home birth, in a birth pool for a water birth, or at our birth center with state of the art SaniJet tubs. We believe birth to be a natural process not a medical event. You can choose what position to labor or birth in, who will attend you, and to not have tight bands around your belly for monitoring. Whether you want to have a natural birth at home or in a birth center, the philosophy is the same. Both are safe, satisfying and empowering for women and their families."
Website URL:
https://laborsoflovebirthcenter.com/
Maps URL:
https://maps.app.goo.gl/DBuMMTMSMW1kpCn1A
#Home birth#water birth#birth center#midwife#home birth midwife near me#home water birth#home birth midwife#home birthing options#midwifery birth center#midwifery care#midwife services
0 notes
Text
A Black couple living in Dallas say their 2-week-old daughter was taken from them because they decided to have a home birth with a midwife.
Home-births and midwifery services are increasingly sought out by Black pregnant people and families over traditional hospital settings amid a mounting maternal mortality crisis exacerbated by systemic medical racism. Black pregnant people are three to four times more likely than white pregnant people to die from pregnancy-related causes, per the CDC.
When Black pregnant people and families can’t feel safe seeking pregnancy and birth-related services from the hospital, and can’t feel safe choosing home births and home care options that draw police attention.
#horrific#stop kidnapping Black kids#Texas is the worst#CPS#black twitter#america was never great#twitter#police state#protect black children
7K notes
·
View notes
Photo

We ALL need to be sharing this story. In March, a Black, #Dallas based mother gave birth to a child at home. She was assisted by a Black midwife. The child has since been taken by Dallas Child Protective Services.
After the child's birth, Temecia Jackson (the child's mother) took her to a routine pediatric appointment, where it was discovered that the baby had jaundice. While the pediatrician advised that they go to the hospital for treatment, Jackson and her husband, Rodney, decided to treat the child at home with the assistance of their midwife. This is not uncommon.
The pediatrician had concerns over the type of light the Jacksons were using to treat their child, and eventually reported them to Dallas CPS. After harassing the family at 5am, on a separate date, police eventually arrested the father and took the child from the family's home. Yesterday, there was supposed to be a hearing for the baby to be reunited with her parents, but it was cancelled minutes before and rescheduled for April 20.
This is every parent's worst nightmare and is particularly horrible given the medical racism Black mothers face and the cross country war on midwifery. Rodney and Temecia are fighting for their baby girl and they need to know that we are too.
Please share this story far and wide. Also, The Afiya Center, a Black woman-led and Dallas based advocacy group, has started an emergency legal defense fund to support the Jacksons and other families facing similar situations.
DONATE HERE: https://secure.actblue.com/donate/taclegalfund
graphic via Cool Mamas Club
98 notes
·
View notes
Text
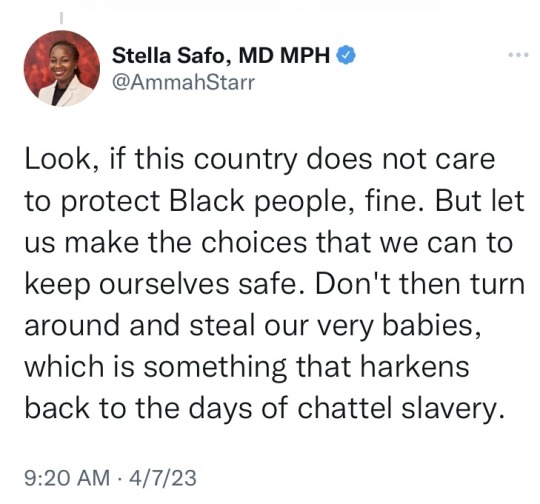
“So women with access to emergency care are the ones that live,” she said. “Women that don’t, die.”
https://www.washingtonpost.com/world/2024/01/21/gaza-childbirth/
JERUSALEM — Walaa didn’t expect the birth of her fourth child to spark abject fear. But by the time her contractions started, the whole family was frantic.
There were no ambulances to be seen in the streets of Gaza’s Rafah City, she said, now so crammed with displaced families that there was barely any food left available for the 27-year-old.
When her uncle Wissam, a doctor, reached the tent where she had lived for weeks in the cold, he said, he could see they had run out of time. “I’m having the baby now,” she kept telling him. It was dark, and she was scared.
His cellphone flashlight was all they had to see by.
The humanitarian catastrophe caused by Israel’s three-month military campaign against Hamas in Gaza counts some 52,000 pregnant women among its greatest victims. As airstrikes push 1.9 million people into an ever-smaller corner of the besieged enclave, disease is spreading, famine is looming and levels of anemia are so high that the risk of postpartum hemorrhage has soared and breastfeeding is often impossible. Forty percent of pregnancies are high-risk, CARE international estimates.
Prenatal care is almost nonexistent — what remains of Gaza’s hospital network is on its knees, at 250 percent capacity and consumed with treating mass casualties from Israeli bombing. Far more women are giving birth outside of medical facilities — in displacement camps, even in the street — than inside them.
Damage to facilities and communications blackouts — the strip lost cellphone service for a week this month — have left Gaza’s health ministry unable to compilereliable data for infant or maternal mortality during the conflict. But doctors and aid groups say miscarriage and stillbirths have spiked.
“What we know about pregnancy-related complications is that it’s hard to prevent them in any setting, but the way that we save a woman and newborn’s life is we treat the complication quickly,” said Rondi Anderson, a midwifery specialist for the Project HOPE aid group.
“So women with access to emergency care are the ones that live,” she said. “Women that don’t, die.”
The only place that Wissam could find to deliver his terrified niece’s baby was a spot of cold earth between the tents. Aid workers hung bedsheets to give the woman a modicum of privacy. No one had been able to contact Walaa’s husband, and her mother was so scared that at times she had to look away. They cut the boy’s umbilical cord with an unsterilized scalpel and they filled tin cans with hot water to keep him warm. He weighed 7 pounds and Walaa named him Ramzy.
The family spoke on the condition that only their first names be used because they feared for their safety in the event that Israeli troops entered the town.

Baby Ramzy is 5 days old. (Loay Ayyoub for The Washington Post)
They fled their home in northern Gaza so abruptly that no one thought to grab clothes for the baby. This week, Ramzy was swaddled in a onesie outgrown by another child in the camp. He wailed as Walaa, still in pain from tearing during the birth, gingerly pulled herself upright.
The 16-year blockade imposed by Israel and Egypt after Hamas won control of Gaza had already made pregnancy and childbirth more difficult for expecting mothers. Before the current conflict, hospitals often lacked adequate equipment and training for neonatal staff, according to Medical Aid for Palestinians, and more than half of pregnant women were anemic.
Hamas fighters streamed out of the enclave on Oct. 7 to kill around 1,200 people in Israel and take another 240 hostage. Israel responded with a bombing campaign and ground war to eradicate Hamas, killing almost 25,000 Palestinians, most of them civilians, to date.
The South African legal team that accused Israel before the International Court of Justice this month of committing genocide during the conflict argued that the obstruction of lifesaving treatment since Oct. 7 amounts to preventing births.
A lawyer for Israel called allegations that it is obstructing the delivery of food, water, fuel and other supplies critical for Gaza “tendentious and partial,” and said it was working “around-the-clock” to help scale up the volume of aid making it into the enclave.
Hanaa al-Shawa, 23, gave birth to her first child, Ayla, during the coronavirus pandemic, and the little girl, she said, brought her family a “glimmer of hope.” Shawa and her husband Mustafa, 25, were ecstatic when they learned in July that another child was on the way. The war began in October, and the future they dreamed of fell apart. “I had felt overwhelming joy,” Shawa recalled. “I did not realize that this joy would turn into great suffering.”
Nearly 20,000 babies were born in Gaza during the first 105 days of the war, UNICEF reported Friday. Delays in the delivery of lifesaving supplies, the U.N. children’s agency said, have left some hospitals performing Caesarean sections without anesthetic. Spokeswoman Tess Ingram said she met a nurse at Gaza’s Emirati maternity hospital who had helped with postmortem caesarians on six dead women.
“Seeing newborn babies suffer while some mothers bleed to death should keep us all awake at night,” Ingram told reporters Friday. “In the time it has taken to present this to you, another baby was likely born, but into what?”
“Becoming a mother should be a time of celebration,” she said. “But in Gaza it’s another child delivered into hell.”
For the five pregnant women interviewed by Washington Post reporters, fear that mother or baby might not survive suffused their waking thoughts — and made appearances in nightmares, too.
Shawa and Mustafa left their home in Gaza City’s Yarmouk Street in the second week of October. The Israel Defense Forces had ordered 1.1 million people in northern Gaza to move south for what it described as their own safety.
“I was afraid that I would miscarry because of the power of the rockets,” she said.

Displaced Palestinian families from the northern and central Gaza Strip evacuate toward southern Gaza on Oct. 13. (Loay Ayyoub for The Washington Post)
Many pregnant women made the 20-mile journey from north to south on foot, their legs swollen and joints heavy as they carried their luggage, three women who made the journey told The Post.
When Ayla was born, her family had a room full of toys ready for her. The room in which Shawa’s second child, a girl, will spend her first weeks, in a friend’s home in the Tel al-Sultan area, is tainted with asbestos, she said.
“We carried Ayla here in just the clothes she was wearing, and we don’t even have anything warm for her,” Shawa said. “If I’m unable to provide for her, what will I do for my next child?”
Rising food scarcity and malnutrition can cause potentially life-threatening complications during childbirth and lead to low birth weight, wasting, failure to thrive and developmental delays.
Shawa said she had only eaten tinned food, with no access to fruit or vegetables, since she left her home three months ago. Doctors have said her iron levels are low and her blood pressure is high. Mustafa searches daily but has found no suitable medication to control it.
Saja Al-Shaer, 19, started to feel like she was too young to become a mother. Her weight had dropped below 110 pounds, she was anemic, and her husband had not managed to get her medication, either. “He spent three days knocking on the doors of pharmacies,” she said. “I do not know if I will see this child or not.”
In late December, doctors at the al-Aqsa Hospital, 11 miles to the north, received a pregnant woman whose high blood pressure caused eclampsia and bleeding to her brain, according to Deborah Harrington, a British obstetrician who volunteered at the hospital with a Medical Aid for Palestinians team.
The baby was delivered by a C-section, Harrington said. The mother was still on life support when the physician left two weeks later.
“These women are presenting it in much more extreme condition,” Harrington said. “They’re just not getting hypertensive treatment. They’re not being screened for diabetes. If they’re diabetic, they’re not getting treatment for their diabetes.
“They know that actually accessing care, as it often is for women in conflict, is really difficult and fraught with danger. At night, there is often no light, so moving around is really difficult. You can’t call an ambulance because there’s no signal. The women I saw were really frightened.”

Walaa with her uncle Wissam, who helped deliver her newborn son. (Loay Ayyoub for The Washington Post)
From the corner of the damp room where Walaa was tending to Ramzy on Friday, she worried about where they would find clean water or baby formula. Her family had looked everywhere for diapers, but come up empty. In Tel al-Sultan, Shawa was fixating on rumors that Israel’s army would direct them to evacuate again. The walking, the carrying, the sense that nothing around her was hygienic — it all frightened her.
But she had made one decision that no shortage or military orders could change. She would name her daughter after her sister-in-law, killed in an Israeli airstrike weeks earlier while trying to find shelter for her own children.
The girl, she said, would be called Heba. In Arabic, it means blessing from God.
Mahfouz reported from Cairo and Harb reported from London. Loay Ayyoub in Rafah contributed to this report.
#Gaza#Maternal and infant care in gaza#Delivering babies with the light from cellphones#52000 pregnant women#40% of pregnancies in gaza are high risk#Hospitals in gaza are at 250% capacity#Medical Aid for Palestinians#Caesarean sections without anesthetic#postmortem caesarians in a desperate bid to save the baby
14 notes
·
View notes
Text
Season 13 episode 2 & 3 combined rewatch
Phyllis teaching the student midwives about the privilege of attending to mothers during a home birth is a powerful scene. Joyce asks about the safety of hospital births and BOY has this question made people feel emotions ever since hospitals were an option for giving birth.
of course, the options for giving birth vary a lot from country to country and region to region. Having choice is so important and infrastructure for emergencies is equally vital. But I'm sure what nobody really wants is families having no safe option at all. Sadly that's what I see happening in too many regions. The hospital where my kid was born is no longer a hospital but a hospice. The town where she was born will no longer have a hospital with a maternity unit in the near future. The next hospital with one will be 20 minutes drive away. And while that is not too bad in comparison to other regions, it would have been too far for me back then. Nobody wants BBA situations in cars or on parking lots, and not everybody can stay home safely. Also, there are not enough midwives who attend home births because they would have to pay a fortune for insurance and they don't get paid enough to do so. Midwifery being a calling does not justify the low pay. With the high responsibility and skill level and especially working conditions they should all be paid much more.
Joyce shows how quickly she learns when attending to Edna. Giving her encouragement and valuing her work makes such a difference. Shelagh is adding her own experience with the repeated suggestion of financial aid. I remember the episode with young mother Marion who did not want help around the house, and then a fellow mother gave her the right nudge with the simple words "You're entitled."
The driving "lesson" with Matthew is supposed to be comic relief, but all it does is give mood whiplash after the heartbreaking scene with Edna feeding her son.
Is learning to drive harder when you're learning in a van? Fred's van seems a little more three-dimensional than the tiny green thing Trixie drove before.
Nancy and Joyce talking about their mould-experiences and how hospital is lovely and clean - germs resistant to antibiotics were not as common back then. it's a shame they became so widespread. Maybe Timothy's generation of doctors will learn to not give everyone precautionary antibiotics just because they can.
I'm growing more and more fond of Sister Veronica. She has the bite that Sister Evangelina brought to the table, and her knowledge of the different possibilities for help makes her highly valuable for Nonnatus House. Her "embellishments" are sometimes just the thing that is needed to bring the right people in or move an obstacle and that is a chaotic-good character trait with a lot of potential for entertainment.
effin ineffable? Colette dearest, that's another show.
social worker training in only 6 weeks? They must have needed them very badly. Today it's three years study at least where I live.
What I love about the newspaper shop as a location is that we're getting to see a lot more newspapers and magazines. The prop department can show off their skills, likewise with the sewing shop, but the paper shop sells an even wider range of wares and that means they can use almost everything in there.
The way that other candidate says the word "mayor" it sounds like "Mäher" in German and that's exactly the kind of gardening device that Fred injured himself on.
Rosalind with the nursing book and ideas for postnatal classes: of course new fathers also need a bit of looking after, but it's not the new mother who should have to do that. It should be friends and relatives and neighbours and I think especially other fathers. The only instance I can remember of fathers looking out for each other is the Fleming family when Derek goes for a pint with his national service friend after Christopher has died. Or maybe way back Tony Amos and his father-in-law.
Gillian's husband looks very much younger than her.
Trixie does use a particular voice on the phone with the shop. The theatricals of being a Lady are like a role that she steps into. Her actual self is showing clearly when she's comforting Violet and preparing her to see Fred in the hospital.
How did you choose your couch? I got mine because I liked the outrageous color. Should I get a new one, it'll have to be one that can open up into a guest bed.
I had a look into how hip problems in newborns are treated today and the kind of hip problem Stephanie has is found in 2-3 newborns. The devices to treat the condition look a good deal more comfortable than the one we saw on the show. Some baby carriers can also help in keeping baby in the right position, with the legs and bottom in kind of an M shape.
they fooled me the first time I watched the episode when the doctors rushed to help the man in the bed beside Fred, and again when I rewatched the scene. Sister Monica Joan sunk into deepest prayer reminded me of how many decades of her life she must have spent praying. Would heaven hear her prayers all the more loudly because of it? Kind of like when Trixie called the shop as Lady Aylward to make them open up late. "This is the most senior nun of the entire order of midwives, don't you dare take our friend from this earth before his time!"
Mrs. Wallace is growing on me. We might not agree on religion, but I respect her sense of community and her attitude towards helping anyone who comes her way. I feel like she is the Miss Higgins of her church, keeping everyone in order.
Miss Higgins! her contribution this week will flow into a different post.
Reggie's idea with bringing Italian food to the hospital is fabulous!
4 notes
·
View notes
Text

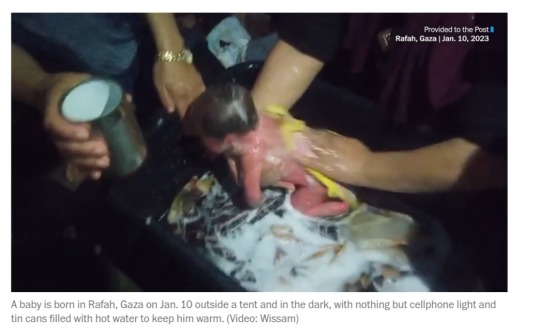
On May 6th 1870 Sir James Simpson, Scottish physician, died.
Born in Bathgate, the son of a baker. Simpson attended the University of Edinburgh from the age of only 14, graduating in 1832. He was appointed to a Chair of Midwifery at the same institution in 1840, quickly establishing the position of this subject as a popular and essential part of medical education. He was a pioneer in the use of anaesthetics, particularly chloroform, developing its use in surgery and midwifery. He introduced ether to obstetric practice in 1847, but in a search for something better, Simpson tried different anaesthetic agents with his colleagues by inhaling their vapours around the dinner table at his home.
He championed the use of chloroform against medical, moral and religious opposition. It was not until Queen Victoria used this anaesthetic during the birth of Prince Leopold that its use became generally accepted. Simpson also pioneered obstetric techniques and responsible for much reform of hospital practice while working at the Infirmary in Edinburgh. In 1866 Simpson became the first person to be knighted for services to medicine.
Simpson is buried in Warriston Cemetery in Edinburgh. Around 1700 medical colleagues and public figures joined his funeral procession and more than 100,000 people lined the route to the cemetery.
He is remembered by the Simpson Memorial Maternity Pavilion in Edinburgh, the most westerly of Princes Street Gardens statue is of the man himself.
7 notes
·
View notes
Text
The Vital Contributions of Nurses and Midwives to Ireland’s Health Sector

Nurses and midwives form the backbone of Ireland's healthcare system, providing essential care across a wide range of settings and populations. Their contributions are fundamental to the health and well-being of the nation, impacting everything from individual patient outcomes to the overall efficiency and effectiveness of the healthcare system. This article explores the vital roles that nurses and midwives play in Ireland's health sector and the profound impact of their work.
1. Frontline Care Providers
Nurses and midwives are often the primary point of contact for patients within the healthcare system. They deliver critical frontline care in hospitals, clinics, community settings, and homes. From administering medications and performing medical procedures to offering emotional support and patient education, nurses and midwives ensure that patients receive comprehensive care tailored to their individual needs.
The hands-on care provided by nurses and midwives is essential for the day-to-day functioning of healthcare services, ensuring that patients receive timely and compassionate care.
2. Promoting Public Health
Beyond individual patient care, nurses and midwives are instrumental in promoting public health in Ireland. They lead vaccination campaigns, conduct health screenings, and educate communities on disease prevention and healthy living. Public health nurses, in particular, work closely with communities to address health disparities, focusing on vulnerable populations such as the elderly, children, and those with chronic conditions.
Nurses and midwives play a crucial role in public health initiatives that prevent disease and promote wellness, reducing the overall burden on the healthcare system.
3. Supporting Maternal and Child Health
Midwives are central to the provision of maternal and child healthcare in Ireland. They support women through pregnancy, childbirth, and the postnatal period, ensuring safe and positive birth experiences. Midwifery-led care models are associated with lower intervention rates, improved maternal satisfaction, and better outcomes for mothers and babies.
Midwives are essential in ensuring the health and well-being of mothers and children, contributing to the long-term health of the population.
4. Addressing Healthcare Inequalities
Nurses and midwives are at the forefront of efforts to address healthcare inequalities in Ireland. They provide care to underserved populations, including those in rural areas, marginalized communities, and individuals with limited access to healthcare. By offering culturally competent care and advocating for patients' rights, nurses and midwives help to ensure that everyone in Ireland has access to quality healthcare.
The work of nurses and midwives in addressing healthcare inequalities is crucial for building a fair and just healthcare system in Ireland.
5. Driving Innovation and Improvement
Nurses and midwives are increasingly taking on leadership roles and driving innovation within the healthcare sector. Advanced nurse practitioners, nurse educators, and nurse researchers are leading efforts to improve care delivery, develop new treatment protocols, and implement evidence-based practices. Their work contributes to the continuous improvement of healthcare services, ensuring that the Irish healthcare system remains responsive to changing needs and challenges.
The leadership and innovation of nurses and midwives are key to advancing the quality and efficiency of healthcare in Ireland.
6. Education and Mentorship
The sustainability of Ireland's healthcare workforce relies heavily on the education and mentorship provided by experienced nurses and midwives. They play a critical role in training the next generation of healthcare professionals, sharing their expertise, and guiding students and junior staff in developing the skills and knowledge necessary for their roles.
The mentorship and education provided by nurses and midwives ensure the ongoing development of a skilled and capable healthcare workforce in Ireland.
7. Resilience in Crisis
The resilience and adaptability of nurses and midwives have been especially evident during times of crisis, such as the COVID-19 pandemic. Their ability to manage complex and high-pressure situations, often at great personal risk, has been crucial in maintaining healthcare services during challenging times. Their unwavering commitment to patient care, even under the most difficult circumstances, underscores their vital role in the health sector.
The resilience of nurses and midwives in the face of crises ensures that healthcare services can continue to operate effectively, even in the most challenging of circumstances.
Nurses and midwives are the cornerstones of Ireland’s health sector, providing essential care, promoting public health, and driving innovation and improvement. Their contributions extend far beyond patient care, influencing every aspect of the healthcare system and ensuring that it remains responsive, equitable, and effective. As Ireland continues to face new healthcare challenges, the vital roles of nurses and midwives will only become more significant. Their dedication and expertise are indispensable to the health and well-being of the nation, making them true pillars of Ireland’s healthcare system.
0 notes
Text
Checking out the World of Nursing: A Comprehensive List of Essential Nursing Positions
**Title: Exploring the World of Nursing: A Comprehensive List of Essential Nursing Positions**
**Introduction:**
Nursing is a dynamic and rewarding field that offers a wide range of career opportunities for those passionate about healthcare. From bedside care to administrative roles, nursing positions encompass various specialties and settings. In this article, we will explore a comprehensive list of essential nursing positions, highlighting the responsibilities, requirements, and potential career paths within each role.
**Essential Nursing Positions:**
1. **Registered Nurse (RN):**
– Responsibilities: Providing patient care, administering medications, collaborating with healthcare team members.
– Requirements: Bachelor’s degree in Nursing, passing the NCLEX-RN exam.
– Career Path: Advanced practice nurse, nurse manager, clinical nurse specialist.
2. **Licensed Practical Nurse (LPN):**
– Responsibilities: Assisting RNs with patient care, monitoring vital signs, administering medications.
– Requirements: Diploma or certificate in nursing, passing the NCLEX-PN exam.
– Career Path: Moving up to become an RN, specializing in a specific area such as geriatrics or pediatrics.
3. **Certified Nursing Assistant (CNA):**
– Responsibilities: Assisting with daily activities, monitoring patients’ condition, providing emotional support.
– Requirements: Completion of a state-approved training program.
– Career Path: Further education to become an LPN or RN, specializing in areas like oncology or critical care.
4. **Nurse Practitioner (NP):**
– Responsibilities: Diagnosing and treating patients, prescribing medications, providing patient education.
– Requirements: Master’s degree in Nursing, passing national certification exams.
– Career Path: Specializing in areas like family practice, women’s health, or mental health.
5. **Certified Registered Nurse Anesthetist (CRNA):**
– Responsibilities: Administering anesthesia during surgical procedures, monitoring patient vital signs.
– Requirements: Master’s degree in Nurse Anesthesia, passing the national certification exam.
– Career Path: Working in hospitals, surgical centers, or private practices.
6. **Nurse Midwife:**
– Responsibilities: Providing prenatal care, attending births, offering postpartum care.
- Requirements: Master’s degree in Nurse Midwifery, passing national certification exams.
– Career Path: Working in hospitals, birthing centers, or offering home birth services.
7. **Clinical Nurse Educator:**
– Responsibilities: Developing and delivering educational programs for nurses, assessing learning needs.
– Requirements: Master’s degree in Nursing Education or related field.
– Career Path: Advancing to leadership roles in nursing education or professional development.
**Benefits of Pursuing Nursing Positions:**
- Job security and stability in a growing field.
– Competitive salaries and potential for advancement.
– Opportunities for specialization in areas of interest.
– Fulfilling work that makes a positive impact on patients’ lives.
**Practical Tips for Aspiring Nurses:**
– Research different nursing positions to find the right fit for your skills and interests.
– Pursue additional certifications or advanced degrees to expand your career options.
– Network with other healthcare professionals to learn about job opportunities and mentorship programs.
– Stay up to date on current healthcare trends and best practices in nursing.
**Conclusion:**
There are countless opportunities awaiting those who choose to explore the world of nursing. From entry-level positions like CNAs to advanced practice roles such as NPs and CRNAs, the field of nursing offers diverse career paths for individuals with a passion for healthcare. By understanding the responsibilities, requirements, and potential career paths within various nursing positions, aspiring nurses can make informed decisions about their professional journey and take steps towards a rewarding and fulfilling career in nursing.
youtube
https://nursingcertificationcourses.com/checking-out-the-world-of-nursing-a-comprehensive-list-of-essential-nursing-positions/
0 notes
Text
Legal Issues
Despite being invited to develop birthing plans, women worldwide continue to be excluded from participating in the design and evaluation of maternity care. This becomes evident as some countries have legislation which make it illegal or nearly impossible for healthcare providers to offer home birth services or midwifery-led birth centers (Sadler et al. 2016:48). In the many countries that do not practice informed maternity services, care is driven by local beliefs about childbirth and professional or organizational cultures (Sadler et al. 2016:48). Even in settings where out-of-hospital births are legal, planning and experiencing one can be extremely difficult and challenging for families and professionals. The biomedical model of care has a complex historical construction “with a consistent set of internal beliefs, rules and practices which responds to and reproduces gender ideologies across health professionals, the legal system and the state” (Sadler et al. 2016:50). Birthing women as a group are systematically disbelieved as a result of the implicit bias that women are less rational than men and lack certain epistemic capacities, which are historically grounded ideas about the uterus and the female reproductive system (Cohen Shabot 2021:642).
Though placed on feminist and public policy agendas, the issue of obstetric violence continues to be overlooked by medical and legal professionals and institutions. Through the “Organic Law on the Right of Women to a Life Free of Violence,” Venezuela became the first country to formally define the concept of obstetric violence as “the appropriation of women's body and reproductive processes by health personnel, which is expressed by a dehumanizing treatment, an abuse of medicalization and pathologization of natural processes, resulting in a loss of autonomy and ability to decide freely about their bodies and sexuality negatively impacting their quality of life” (Sadler et al. 2016:50). Since then, there has been resistance from health professionals from the concept of violence as it is contrary to their ethos. The framing of obstetric violence as a matter of violence and as a human rights violation allows us to acknowledge that practitioners and institutions are often unwittingly socialized to accept invisible forms of violence as normal happenings in reproductive care.
Birthing women become secondary elements in the birthing scenario under the law (Diaz-Tello 2016; Jardim and Modena 2018). The personal value that physicians and health attorneys ascribe to the fetus corresponds with their strong willingness to seek court-appointed procedures and interventions over the protest of an unwilling patient (Diaz-Tello 2016:60). Fetal interests become more compelling, which contribute to the violent policing of gender norms. Institutional rules separate women from social and cultural contexts, making them and others discredit their physiological capacity to give birth. Though guaranteed equal protection, women continue to experience gender discrimination throughout the birthing process. According to common tort law, anyone subjected to unconsented touching, regardless if for medical purposes, may sue for battery in most jurisdictions (Diaz-Tello 2016:59). There is no current law to protect this right for pregnant women. Those who do take legal action face issues with statutes of limitations or with healthcare providers, institutions, and courts reading in exceptions, preventing them from achieving legal progress.
Worldwide, women continue to be excluded from participating in the design and evaluation of maternity care as the current model fails to provide appropriate, evidence-based care. This becomes evident as some countries have legislation which make it illegal or nearly impossible for healthcare providers to offer home birth services or midwifery-led birth centers (Sadler et al. 2016:48). In settings where out-of-hospital births are legal, planning and experiencing one can be extremely difficult and challenging for families and professionals.
Legal case studies have revealed tragic occurrences and experiences of unconsented procedures and coercion. Studies of women who have pursued legal action after such violations and the outcomes of their cases demonstrate that the courts often favor the practitioners and healthcare systems over human rights (Logan et al. 2022:759). Forced cesarean surgery is a violent act that takes place in a setting where women are inferior to their doctors and other medical staff. In a society where women’s capacity for pregnancy has been historically used to sanction their exclusion from full citizenship; obstetric violence is more than a case of battery (Diaz-Tello 2016:59). Out of fear and insecurity about obstetric processes, birthing women become dependent and submissive, subjected to the wills of the professionals, holding them hostage to the violent cycle of obstetric violence (Jardim and Modena 2018:8).
Modern case law rejects the notion that pregnant women have any lesser entitlement to the fundamental right to bodily autonomy than any other person under the constitution (Diaz-Tello 2016:61). Still, women continue to experience limitations due to a lack of enforcement, lack of rights-based training among healthcare providers, and a failure to address infrastructural weaknesses (Diaz-Tello 2016:62). Practitioners significantly overestimate liability risks and irrationally prioritize fetal health, ascribing low value to any injury or failure of informed consent for pregnant women. This, along with the hesitation of legal authorities to criminally charge physicians, makes hospitals feel comfortable in making threats and intervening. There are rarely successful prosecutions for obstetric violence (Cohen Shabot 2021; Diaz-Tello 2016; Jardim and Modena 2018; Lokugamage and Pathberiya 2017; Sadler et al. 2016).
Of the few obstetric violence cases which have been taken to trial, each only lasted a matter of minutes (Diaz-Tello 2016). The juries sided with the hospitals, agreeing that the physicians had made the best possible choices for the mothers and their babies. To suggest that pregnant patients were to have the same rights as others, given the connotations the pregnant status invokes as that of hysteria, irrationality, and unreasonableness, would be naive and foolish. For the pregnant patients, there is a right to consent to the surgeries and procedures suggested by the medical professionals, but not a right to refuse them (Diaz-Tello 2016:59).
0 notes
Text
VBAC Private Midwives
In anticipation of a HBAC (home birth after cesarean) I have shortlisted some Gold Coast private midwives that are experienced with VBAC (vaginal birth after cesarean). I can't wait to connect with them when the time comes!
https://birthingmum.com.au/
0 notes
Text
Welcoming Life: The Beauty of In-Home Midwifery Care
In the journey of childbirth, there's a serene beauty in welcoming life within the comfort and familiarity of one's own home. As modern healthcare evolves, so do our choices in birthing experiences. In recent years, the resurgence of in-home midwifery care has captured the hearts of many expectant parents, offering a deeply personalized and empowering alternative to traditional hospital births.
In-home midwifery care embodies a holistic approach to childbirth, emphasizing the sacredness and natural rhythm of the birthing process. It celebrates the innate strength of women and honors the profound connection between mother and child. At the heart of this movement lies a commitment to empowering individuals to reclaim ownership of their birthing experiences, guided by the compassionate support of skilled midwives.
The Rise of In-Home Midwifery Care
In an era marked by technological advancements and medical interventions, the resurgence of in-home midwifery care represents a return to simplicity and intimacy in childbirth. This shift is driven by a growing desire among expectant parents to cultivate a sense of autonomy and agency in their birthing journey. With a focus on personalized care and individualized support, in-home midwifery services offer a refreshing alternative to the often impersonal and regimented atmosphere of hospital births.
Empowering Birthing Experiences
Central to the philosophy of in-home midwifery care is the belief that childbirth is a natural, transformative experience that should be approached with reverence and respect. Unlike traditional hospital settings, which can be fraught with medical interventions and bureaucratic protocols, in-home births provide a serene and familiar environment where individuals can labor and deliver according to their own instincts and preferences.
Through personalized prenatal care, continuous labor support, and gentle postpartum guidance, midwives facilitate a deeply empowering birthing experience that prioritizes the physical, emotional, and spiritual well-being of both mother and baby. By fostering a sense of trust and collaboration, midwives empower individuals to make informed decisions about their care and actively participate in the miraculous journey of bringing new life into the world.
The Role of Sacred Birth Midwifery
At the forefront of the in-home midwifery movement is Sacred Birth Midwifery, a beacon of compassionate care and unwavering support for expectant families. With a deep reverence for the sacredness of birth, Sacred Birth Midwifery embodies the essence of in-home midwifery care, offering comprehensive services tailored to the unique needs and desires of each individual.
Through a holistic approach that encompasses prenatal education, labor assistance, and postpartum care, Sacred Birth Midwifery creates a nurturing environment where families can embrace the transformative journey of childbirth with confidence and grace. By honoring the innate wisdom of the body and the profound bond between mother and baby, Sacred Birth Midwifery redefines the birthing experience as a sacred rite of passage, filled with beauty, strength, and boundless love.
In embracing the beauty of in-home midwifery care, we reclaim the power to shape our own birthing experiences and usher new life into the world with reverence and joy. As we honor the sacredness of birth and embrace the wisdom of generations past, we pave the way for a future where every individual can welcome life in a manner that is truly empowering and unforgettable.
Visit Sacred Birth Midwifery to learn more about their compassionate in-home midwifery services and embark on a journey of empowerment and celebration.
0 notes
Text
Home Birth Midwives - Your Partners in Safe and Supported Birth
At Avenir Life Midwifery, we understand that choosing to have a home birth is a deeply personal decision. It's about creating a birthing experience that feels safe, supported, and empowering for you and your family. That's why our team of experienced home birth midwives is here to be your partners every step of the way.
Home Birth Midwives play a crucial role in providing compassionate and personalized care throughout the entire birthing journey. From the initial consultation to postpartum support, our midwives are dedicated to ensuring that you feel confident and informed every step of the way.
When you choose Avenir Life Midwifery for your home birth, you can expect comprehensive and holistic care that prioritizes your physical, emotional, and mental well-being. Our midwives take the time to get to know you and your unique needs, allowing them to tailor their approach to best support you during labor and delivery.
One of the key benefits of working with home birth midwives is the comfort and familiarity of giving birth in your own home. This environment allows you to relax and feel more in control, which can lead to a smoother and more positive birthing experience for both you and your baby.
Safety is always our top priority at Avenir Life Midwifery. Our midwives are highly trained professionals who have extensive experience in managing home births and responding to any unexpected situations that may arise. We work closely with you to create a comprehensive birth plan that addresses your individual needs and preferences while ensuring the safety and well-being of you and your baby.
Throughout your pregnancy and birth, our midwives provide continuous support and guidance, helping you to feel empowered and confident in your body's ability to give birth naturally. We believe that every woman deserves to have a birth experience that is respectful, empowering, and supported, and we are committed to helping you achieve that with our home birth services.
In conclusion, home birth midwives at Avenir Life Midwifery are your partners in safe and supported birth. With our compassionate care, personalized approach, and commitment to safety, we are here to support you in achieving the home birth experience you desire. Contact us today to learn more about our home birth services and how we can help you create the birth experience of your dreams.
For more information visit our website: https://www.avenirlifemidwifery.com.au/
Contact Info:
Avenir Life Midwifery
Email: [email protected]
Tel: 0423 300 110
0 notes
Text
Best college offering GNM in Bangalore
General Nursing and Midwifery (GNM) is a vital area of healthcare that offers diverse career opportunities for individuals interested in nursing and midwifery. Here's an overview of the career opportunities available to GNM graduates:
1. Staff Nurse: GNM graduates can work as staff nurses in hospitals, clinics, nursing homes, and other healthcare facilities. They provide direct patient care, administer medications, monitor vital signs, and assist with medical procedures under the supervision of registered nurses or physicians.
2. Community Health Nurse: Community health nurses work in community settings, such as health centers, schools, and residential facilities, to provide healthcare services to individuals and families. They conduct health assessments, provide health education, and promote preventive care initiatives to improve community health outcomes.
3. Midwife: GNM graduates can pursue a career as midwives, providing care to pregnant women, mothers, and newborn babies before, during, and after childbirth. Midwives assist with prenatal care, labor and delivery, and postpartum care, and they play a crucial role in ensuring safe and positive birth experiences for women and their families.
4. Critical Care Nurse: GNM graduates with specialized training and experience may work as critical care nurses in intensive care units (ICUs), emergency departments, or trauma centers. Critical care nurses provide specialized care to critically ill or injured patients, including monitoring vital signs, administering life-saving interventions, and collaborating with multidisciplinary teams to stabilize patients' conditions. GNM college in Bangalore

5. Pediatric Nurse: Pediatric nurses specialize in providing healthcare services to infants, children, and adolescents. They work in pediatric hospitals, clinics, and pediatricians' offices, caring for patients with a wide range of medical conditions and developmental needs. Pediatric nurses administer vaccinations, perform developmental assessments, and provide support to families during challenging times.
6. Geriatric Nurse: Geriatric nurses specialize in caring for older adults, including those with age-related health issues, chronic conditions, or complex medical needs. They work in nursing homes, assisted living facilities, and geriatric clinics, providing personalized care, managing medications, and promoting the health and well-being of elderly patients.
7. Public Health Nurse: Public health nurses work in government agencies, non-profit organizations, and community health centers to address public health issues and promote population health. They develop and implement health education programs, conduct disease surveillance, and collaborate with community partners to improve access to healthcare services and reduce health disparities.
for more details: The best college for GNM in Bangalore
0 notes
Text
The Role of Midwives in Supporting Home Birth Experiences
In the realm of childbirth, the support and expertise provided by midwives are invaluable, particularly in the context of home births. As expectant parents increasingly seek personalized and holistic birthing experiences, midwifery services play a pivotal role in facilitating safe and empowering home births. This article delves into the significant contributions of midwives, focusing on their role in supporting home birth experiences, particularly in the vibrant community of the Gold Coast, where Avenir Life Midwifery shines as a beacon of personalized care and support.
Home birth midwives are dedicated professionals who specialize in assisting families through the journey of giving birth in the comfort of their own homes. Their role extends far beyond the delivery room, encompassing comprehensive prenatal care, continuous support during labor, and postnatal care for both mother and baby. One of the primary benefits of engaging a home birth midwife is the continuity of care they offer, building a trusting relationship with the expectant family throughout the entire childbirth process.
Avenir Life Midwifery, a leading provider of midwifery services on the Gold Coast, exemplifies this commitment to personalized care. With a team of highly skilled and compassionate midwives, Avenir Life is dedicated to honoring the preferences and wishes of each family while ensuring the safety and well-being of mother and baby during home births. From the initial consultations to the joyful moment of welcoming a new life into the world, Avenir Life Midwifery stands by families every step of the way.
Midwives from Avenir Life bring a wealth of experience and expertise to home birth settings, equipped to handle a wide range of scenarios with confidence and grace. Their comprehensive prenatal care includes regular check-ups, personalized birth planning, and education on nutrition, exercise, and childbirth techniques. Throughout labor, home birth midwives provide continuous emotional and physical support, employing techniques such as massage, breathing exercises, and positioning to facilitate a smooth and comfortable birthing experience.
Postnatally, midwives from Avenir Life continue to offer invaluable support, assisting with breastfeeding, newborn care, and maternal recovery. They provide regular home visits to monitor the health and well-being of both mother and baby, offering guidance and reassurance during the critical postpartum period. Through their unwavering dedication and compassionate care, Avenir Life Midwifery helps families navigate the transition to parenthood with grace and resilience.
In conclusion, the role of midwives in supporting home birth experiences cannot be overstated. From prenatal care to postnatal support, midwifery services play a vital role in ensuring safe, empowering, and personalized childbirth experiences. In the vibrant community of the Gold Coast, Avenir Life Midwifery stands as a trusted partner for families seeking the highest standard of care and support during home births. With their unwavering dedication and commitment to excellence, Avenir Life Midwifery is reshaping the landscape of childbirth, one joyful home birth at a time.
For more information visit our website: https://www.avenirlifemidwifery.com.au/
Contact Info:
Avenir Life Midwifery
Email: [email protected]
Tel: 0423 300 110
0 notes
Text
Midwifery: Not Just For Hippies Anymore
There has been a recent upsurge in the popularity of midwifery and alternative options in childbirth. Pregnant and childbearing women are increasingly seeking to customize their birthing experiences by incorporating elements of both the mainstream medical model and the midwifery model of care. In this paper, I use data obtained through in-depth interviews to examine the ways in which a collective of birthworkers; midwives, doulas, childbirth educators, and lactation consultants construct their identity in an attempt to appeal to the consumption patterns of this potential clientele. Refuting stereotypical notions of midwives and other birthworkers as being a part of a radical fringe, this group seeks to attract a larger, more mainstream client base by providing services that can be consumed by women choosing a more medical birth. Instead of insisting upon non-medicated, midwife-directed home birthing, this collective defines themselves as different from traditional midwifery in a number of important ways. Specifically, these birthworkers incorporate elements of the medical model into their practice and employ the rhetoric of professionalism, individualized care, non-biased information, neutrality and non-judgment, and informed choice.
0 notes