#End-Stage Kidney Disease
Text

Challenges in Re-Kidney Transplantation:
Re-kidney transplantation presents distinct challenges compared to initial kidney transplants. The development of antibodies against Human Leukocyte Antigens (HLA) due to sensitization from the first transplant escalates the risk of hyper-acute or acute rejection during re-transplantation. The presence of pre-existing HLA antibodies, known as donor-specific antibodies (DSA), makes finding a compatible donor more difficult and serves as a major obstacle to successful re-kidney transplantation. Furthermore, re-kidney transplantation can give rise to surgical challenges as patients may have adhesions or altered anatomy from the previous surgery. This can complicate the procedure, necessitating specialized techniques or experienced kidney transplant surgeons' involvement to address these complexities. Moreover, achieving the right balance in immunosuppressive regimens becomes crucial to prevent rejection while minimizing the risk of infection and other side effects. Both under-suppression and over-suppression of the immune system carry potential risks, respectively leading to acute rejection and graft failure or increased susceptibility to infections and malignancies.
Graft Survival in Re-Kidney Transplantation:
The success of re-kidney transplantation depends on various factors such as recipient and donor age, HLA matching, pre-transplant sensitization, and the duration between the first and second transplant. Notably, studies indicate that graft survival rates in re-kidney transplantation generally fall below those in primary kidney transplantation. However, advancements in immunosuppressive therapies, improved donor-recipient matching, and enhanced post-transplant care have positively impacted outcomes over time. Recent developments in transplantation have seen a growing emphasis on personalized medicine, wherein individual patient characteristics are considered when tailoring immunosuppressive regimens for optimal results. Additionally, progress in organ preservation techniques and the utilization of marginal or extended criteria donors have broadened the donor pool, providing greater access to kidney transplantation for patients seeking re-kidney transplantation.
There are some of the best doctors and hospitals in Bangalore available for the procedure of re-kidney transplantation. The total cost of kidney transplant in Bangalore will depend on a number of factors, like the doctor and hospital chosen for treatment, the reason for the failure of the previous kidney transplant, the health of the patient, and the type of donor used for kidney transplantation.
0 notes
Text
Peritoneal Dialysis: Definition, Types, and Benefits | TX Hospital Hyderabad
Peritoneal dialysis is a medical treatment for end-stage kidney disease. Learn about the two types of peritoneal dialysis, CAPD and APD, and their benefits over hemodialysis. TX Hospital Hyderabad offers state-of-the-art technology and top nephrologists to provide safe and effective peritoneal dialysis treatment options.
#Peritoneal dialysis#Continuous ambulatory peritoneal dialysis#Automated peritoneal dialysis#End-stage kidney disease#Nephrologists
0 notes
Text
Usefulness of American College of Cardiology/American Heart Association treatment-resistant hypertension criteria among end-stage kidney disease patients – A case series
Usefulness of American College of Cardiology/American Heart Association treatment-resistant hypertension criteria among end-stage kidney disease patients – A case series
image: Flickr
Article published in the J. Pharm. Pharmacogn. Res., vol. 10, no. 4, pp. 717-724, July-August 2022.
DOI: https://doi.org/10.56499/jppres22.1383_10.4.717
Shorouq Khader Abujadallah1, Seeba Zachariah1*, Rajaram Jagdale2,3
1College of Pharmacy, Gulf Medical University, Ajman, United Arab Emirates.
2Department of Nephrology, Thumbay University Hospital, Ajman, United Arab…

View On WordPress
#antihypertensive#blood pressure control#end-stage kidney disease#hemodialysis#resistant hypertension
0 notes
Text
:(
#he's not sick or anything no worries everything is fine#but smooch aka dried pickle man is just...#getting older#he's 13#which isn't super old for an indoor cat with superior vet care but it is low end lifespan#and he has stage 3 kidney disease AND IBD so like that has to take a toll#and i've noticed lately that he has been slowing down#not like lethargic or anything#just#sleeping more often#being a little slower#bothering his brothers less#and it guts me to see him age even a little#i cried about it today#he's due for his annual and he gets ALL the bloods and prodding to make sure he's chugging along and i expect everything will be fine#he's just getting up there and i'm not ready for that#he's a pillar of my world
45 notes
·
View notes
Text
I have a headache and I wish I could take naproxen instead of useless Tylenol
#Tylenol's the only kidney-safe OTC painkiller#but it doesn't do SHIT#ESRD#end stage renal disease#headache#owwww#tylenol
4 notes
·
View notes
Text
https://gofund.me/6732cec4
Behind every dope ass woman is one hell of a story💚🪄🌻
#black girl magic#national kidney foundation#chronic kidney failure#esrd#ckd#organ donation#kidney transplant#end stage renal disease#Pediatric Nurse#registered nurse#chronic illness#chronic pain#gofundme#fundrasier#john hopkins hospital#black nurses matter#black nurses rock
30 notes
·
View notes
Text
I started dialysis a few months ago, after ending up in hospital with a creatinine of 15.4.
And I’m sitting here, looking at this machine that leashes me each evening, and it’s a little miracle of science that I’m alive, that I can continue to be alive, in the comforts of my own home, with a dedicated team of professionals available 24/7 to support me: I have doctors, nurses, a dietitian, a social worker, a finance/insurance coordinator…and then the transplant team is even bigger. It’s wild. Truck drivers who come into the house and stack boxes for me, even.
And in the U.S. it’s covered immediately with Medicare, by federal law. Because I’d die without it.
So it can be done. This could be how we handle diabetes. Cancers. This could extend to others, who will die without intervention.
So I am so very lucky(?) to have a terminal chronic disease that is handled like this. Don’t get me wrong, having any chronic illness is exhausting, and there are nights when I feel burdened at the thought of hooking up, but then I remind myself how damn lucky I am (for both the technology and the supports) and then I am enraged that it isn’t common sense for a government to not let its population just die from treatable things…
#dialysis#chronicillness#kidney disease#end stage renal failure#medical insurance#stupid government#it is not that hard#just give everyone medical insurance
1 note
·
View note
Text
Compassionate Care for Chronic Kidney Disease: A Nursing Perspective
Chronic Kidney Disease (CKD) is a progressive loss of kidney function over time. Managing CKD is not just about slowing the progression of the disease but also about enhancing the quality of life for those affected. Nurses play a crucial role in this process, providing care that is as compassionate as it is competent. This blog post will explore the nursing interventions and desired outcomes that…

View On WordPress
#AChronic Kidney Disease#Blood Pressure Control#CKD Complications#CKD Management#CKD Progression#Dialysis Support#End-Stage Renal Disease#Fluid Management#Kidney Disease Education#Kidney Function Monitoring#medication adherence#Nurse#nurses#Nursing#Nursing Care Plan#Nursing Interventions#Pain Management in CKD#palliative care#patient education#psychosocial support#Quality of Life with CKD
0 notes
Text

Understanding Dialysis:
Dialysis stands as a remarkable medical intervention, effectively mimicking the essential functions of the kidneys by removing waste products, excess fluid, and toxins from the bloodstream. This process is vital for maintaining the body's overall health and preventing the accumulation of harmful substances that can lead to severe complications. Broadly categorized into hemodialysis and peritoneal dialysis, each approach offers distinct advantages and considerations, catering to the diverse needs and preferences of patients.
Hemodialysis:
Hemodialysis represents a widely utilized form of renal replacement therapy, involving the extracorporeal circulation of blood through a specialized machine known as a hemodialyzer. This sophisticated apparatus functions as an artificial kidney, facilitating the removal of waste products and excess fluid from the blood while restoring electrolyte balance. Hemodialysis sessions typically occur several times a week at designated dialysis centers, necessitating the establishment of reliable vascular access through arteriovenous fistulas, grafts, or central venous catheters.
The procedural intricacies of hemodialysis encompass a comprehensive array of considerations, including blood flow rates, dialysate composition, and ultrafiltration targets. Despite its efficacy in achieving adequate clearance of metabolic waste, hemodialysis may pose certain challenges such as the risk of hypotension, muscle cramps, and vascular access-related complications. Furthermore, adherence to a strict dietary regimen and fluid restriction is essential to optimize treatment outcomes and minimize potential adverse effects.
Peritoneal Dialysis:
In contrast to hemodialysis, peritoneal dialysis harnesses the permeable nature of the peritoneal membrane lining the abdominal cavity to facilitate the exchange of solutes and fluids. This modality entails the instillation of a sterile dialysis solution into the peritoneal cavity via a surgically implanted catheter, allowing for the passive diffusion of waste products and excess fluid across the peritoneal membrane. Subsequently, the spent dialysate is drained from the abdomen, completing a cycle of peritoneal dialysis.
The versatility and convenience of peritoneal dialysis render it an attractive option for many patients, offering greater autonomy and flexibility in managing their treatment regimen. Home-based peritoneal dialysis affords individuals the opportunity to undergo therapy while maintaining their daily routines and minimizing disruptions to their lifestyle. Nevertheless, meticulous attention to infection control practices, including proper catheter care and aseptic technique during exchanges, is imperative to mitigate the risk of peritonitis and other infectious complications.
Doctors suggest undergoing a full body health checkup at regular intervals in case of dialysis patients to check the side effects associated with dialysis, its impact on the general health of the patient, and early management of the complications associated with the procedure.
#dialysis#end stage kidney disease#end stage renal disease#hemodialysis#peritoneal dialysis#full body health checkup#regular health checkups
0 notes
Link
End stage of Renal disease happens to be the last stage of acute or chronic renal failure. read about Causes, Symptoms, Treatment of End stage Renal disease
#End Stage renal Disease#Causes ESRD#Symptoms ESRD#nephrologist in Ahmedabad#Nephrology Doctor#kidney diseases#Kidney Specialist in Ahmedabad
0 notes
Link
#end stage kidney disease#end stage disease in pet#cats#my cats#kidney#chronic#renal acute renal#symptoms#stages#treatment#diagnosis#usa#chronic disease
0 notes
Text
#kidney transplant#kidney damage#End stage kidney diseases#Polycystic kidney disease#Kidney cancer#Kidney inflammation#Chronic glomerulonephritis#Reaction to anesthesia#Blood clots#Rejection to donor's kidney#Kidney transplant treatment in India#medical treatment#Expert urologist#surgeon#physician and doctors#medical tourism in india#best doctors in india
0 notes
Text
Frustrated by lack of relatable ESRD posts
I really really wish there were more posts about End Stage Renal Disease and everything related to it from other people who also live with it. Stuff about our experiences with kidney failure and dialysis and doctors and the diets they put us on and co-morbid illnesses and just everyday mundane stuff and what it's like to live with this condition. Cause most of the time when I'm looking up ESRD, I just find stuff about pets who have it, or posts from doctors or medical institutes or some study about some supposedly innovative thing in the nephrology world. I crave more relatable content from other humans who have ESRD, because it feels like there's hardly enough out there and I'm tired of it
#end stage renal disease#ESRD#chronic illness#disability#dialysis#life with kidney failure#kidneys#terminal illness
1 note
·
View note
Text

Shoutout to my GOD-mama for my cup! It’s most definitely a coffee ☕️ kind of day.
https://gofund.me/6732cec4
#ThisNurseNeedsAKidney#ClickTheLink#DonateLife#ShareYourSpare#PediatricNurse#black girl magic#black girls rock#black nurses matter#black nurses rock#esrd#ckd#chronic kidney disease#kidney failure#end stage renal disease#dialysis#john hopkins hospital#atypical hus#Atypical Hemolytic Uremic Syndrome#chronic pain#chronic illness#spoonie#gofundme#healing#happy juneteenth#juneteenth#support black people#support black women#registered nurse#organ donor#organ donation
12 notes
·
View notes
Text
The text for all of the screenshots below will be included after the screenshots at the end of this post.






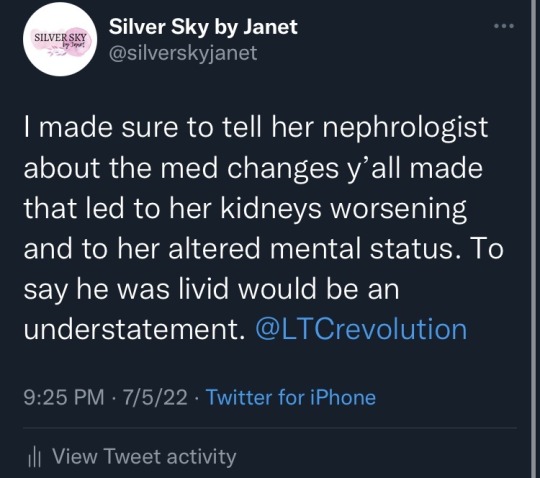

Between 3:27 and 3:37 PM CDT on July 4, 2022, while at my mom’s bedside in the emergency room of Huntsville Hospital, I made and updated a thread about my mom’s stay at Whitesburg Gardens, a Signature HealthCARE facility and how their actions led to my mom needing to be at the emergency room.
At 3:27:
I’m not saying the @LTCrevolution rehab my mom has been at for almost two weeks has made her kidneys, heart, and lungs significantly worse, but I’m not saying it hasn’t.
(Her labs that they twiddled their thumbs on ordering are totally saying it though.)
When we kept asking when they’d get her back on her medicine, they had to wait for a pharmacy to fill it. They still haven’t got her on one BP med and her bicarb medicine dose is too low vs what she’s supposed to be on.
When we kept asking when they’d check her creatinine, potassium, CBC, etc., they’d tell us “probably tomorrow” until the dietician ordered it—6 days into the stay.
When they got the CBC back, the next morning they sent her to get a blood transfusion. They didn’t monitor her closely after she got back.
When mom was lethargic on Saturday, a symptom that her CKD is worsening and/or that she may have respiratory acidosis, it took me calling the front desk TWICE to get them to call an ambulance.
An. Hour. After. I. Called. The. Last. Time.
When she couldn’t breathe and was coughing last night, the nurse refused to check on her. All. Night. Long.
She sent a message for mom to sit up through a CNA. Sitting up didn’t help. Two nebulizer treatments this morning didn’t help.
Now mom is at the ER (for the third time in a week and the second in three days) because she couldn’t oxygenate properly.
Her creatinine is up to 4.4 from 3.5 the day she went in.
Her CO2 went up by 4, into the high territory within the first week.
Her ProBNP is at 5055 pg/mL. Higher than at discharge.
Her potassium is high enough for her to probably need a potassium binder.
Her kidneys are now bad enough that she may need dialysis and I am so beyond pissed. One of her previous roommates made a comment last week that “it’s like they’re trying to kill us” and it kinda feels like they are.
At 3:37:
There have been incidents where they would stand in front of her and mock her for being unable to stand up. She was having trouble standing because CKD, heart, and lung problems cause muscle weakness and fatigue.
They responded at 8:32 AM CDT on July 5, 2022:
Silver Sky by Janet, we at Signature take all of your concerns very seriously, and we work hard to serve you, our residents, and their families. The care of our residents is our top priority. Please contact our CAREline at (888) 392-8886 -Sincerely, Signature HealthCARE
I responded at 9:42 PM CDT on July 5, 2022:
The name is Janet, but I’m not surprised you have a form response/bot for your replies @LTCrevolution since that was the same way that y’all apparently handled 1-star reviews on Google reviews for Whitesburg Gardens.
I made sure to tell her nephrologist about the med changes y’all made that led to her kidneys worsening and to her altered mental status. To say he was livid would be an understatement. @LTCrevolution
As of around 11:30 PM CDT on July 5, her creatinine is still at 4.4 mg/dL and her potassium has gone up to 5.4 mmol/L. Her systolic blood pressure and diastolic blood pressure keep taking turns on the systolic being high with the diastolic being normal and the systolic being normal with the diastolic being high. She’s having trouble with her vision and her hearing that she wasn’t having before. She cannot feel areas of her body she could feel before two days ago. She is confused. She struggles with words. She is scared. She is combative. I don’t know if this is a temporary mental status change. I don’t know if her kidneys will rebound. I don’t know what will happen next, but I know that all of these changes in her labs and her personality and her new status as an end-stage renal disease patient are a result of the actions taken at Whitesburg Gardens.
Update (July 6, 2022 at 5:51 pm CDT): She has developed pancytopenia as a result of the mismanagement of her CKD. This means her red blood cell, white blood cell, and platelet counts are too low, and her body can no longer produce the erythropoietin needed to protect her blood cells from being attacked. She will need a second surgery for her dialysis fistula sometime soon and she may need emergency access while that heals.
#kidney failure#end stage renal disease#elder abuse#nursing home#caregiver#signature healthcare#skilled nursing facility#family#disabled#disability#neuropathy#twitter#hypertension#heart failure#whitesburg gardens#huntsville#alabama#ckd
0 notes
Text
Allow inhibitors of SGLT-2-protect your kidneys: diabetes will thank you for life
Allow inhibitors of SGLT-2-protect your kidneys: diabetes will thank you for life
Diabetes is the leading driver of kidney disease, a potentially fatal condition affecting millions people wordlwide. Diabetes damages the kidneys by preventing the organs from effectively filtering wastes and excess fluids from the body. Because symptoms such as nausea, vomiting, sleep disturbances and swollen limbs are common and nonspecific to kidney disease, most people don’t realize they have…

View On WordPress
#angiotensin#blood glucose#cell signaling#cellular energy#cellular stress#dapagliflozin#diabetes drug#end-stage kidney failure#kidney disease#lisinopril#osmotic stress#rosiglitazone#signal transduction
0 notes