#Intensive Care Unit
Explore tagged Tumblr posts
Text
Everyone wish my aroace friend luck and a speedy recovery.
At 5am today, she got the call saying her donor was ready and that a car was coming to take her to London. Now, 16 hours later, she is having the operation done for her lung transplant.
I will not hear from her again until August due to the fact she will be put into intensive care and sedated.
For those of you who may remember, this is the same aroace friend who said "the only relationship I will ever be in is with my health, and it's a very toxic one". That quote is extremely ironic now.
Wish her luck!
#aroace#aromantic#asexual#friends#lung transplant#lung condition#transplant#operation#intensive care unit#I'm now officially the first person she has ever said “I love you” to#this is worrying#she better come out of this alive#or else I'm pole dancing down to hell and bringing her back
53 notes
·
View notes
Text
Duck or Treat?
A very Oktober Halloween(ish) Gift for the wonderful @ritualofcirice and her work Hazbin Hotel Imagines and Scenarios Chapter 3 : When Lucifer gave you your fiftieth Duck <3
While going Trick or Treat with Niffty an Halloween, Things not go as planned for you and you´re met with the Question - Duck or Treat.
Trigger Warning: NICU, premature Birth, Fear, Hospital Stay

“But Dazzle would look so cute in that costume” - a sigh escaped your lips as you demonstratively held up the little ketchup bottle-style costume and put all your persuasion, into convincing Charlie that Razzle or Dazzle could wear a costume for the annual Halloween. But the two bodyguards of the Princess of Hell were not keen and had hidden somewhere in the hotel.
“And Razzle would wear a matching outfit - ketchup and mustard” - were your additional words and with a reach into one of the bags on the floor, you conjured up the second costume intended for Razzle.
A Halloween mustard bottle outfit. It would have been such a great combination and in your opinion Razzle and Dazzle already looked cute in general... only the costumes would have made them even cuter.
“Darling? Maybe our demon cat told Razzle and Dazzle that you put the hamburger costume on her and wanted to take her trick or treating with Niffty?” - Lucifer gently placed a hand on your right shoulder. His words made sense.
“Oh yes, I think Razzle and Dazzle are hiding together with your cat, buuuuut Niffty is already excited, she hasn't talked about anything else for last days” - Charlie said with a smile and took both of the packed costumes from you.
“Maybe we can use one of the costumes for the baby , when it comes in a few months and celebrates its first Halloween?” - Charlie changed the subject and your hand automatically went to your Stomach, resting gently on the fabric of your dress.
“Four more months... maybe I should have dressed up as a duckling, hm Luci?” - you replied and with one hand you reached for Lucifer's to squeeze it gently.
The duck in the oven surprise was a few months ago and since that, you told almost everyone, the public's focus has been on you, more than ever.
And Charlie and Lucifer's concern for your well-being has increased.
But it's still four months until the birth date.
Nevertheless, the thought of all the holidays and special moments , that you could experience with your baby, the family and Lucifer enchants you. The little girl would be loved and protected by everyone.
"And what are you supposed to portray?" - came the question from Angel, who had sprinkled a little orange glitter in his hair for Halloween and an upcoming shoot for a Halloween spin-off in Valentino's studio.
"Isn't that obvious?" - Husk commented from the bar and you smiled at the grumpy bartender. He hadn't dressed up and you had already known it.
"Oh? And what exactly is the not so obvious?" - Angel countered cluelessly.
“A strawberry” - was Husk’s answer.
“I thought you were supposed to be a tomato… oh” - said Lucifer, surprised.
You reached into one of the bags again and a small strawberry handbag and a green hat completed your outfit.
“I was already wearing it , when we went through the entrance to the hotel, but it’s a bit warm here today… but yes, Husk is right. I’m a strawberry for Halloween” - you giggled and it was a simple Halloween costume. But sufficient.
“A pregnant strawberry, how cute!” - giggled Niffty, who came running into the entrance area of the hotel in her Halloween costume and the sight elicited an amused laugh from you. Charlie, Angel and Husk also had to smile.
Because Niffty had put a lot of effort into her costume. She had sewn it by hand and of course chose a bad boy from the last few decades.
A serial killer costume.
Michael Myers.
She had styled her hair a little messier and the dark suit that was typical for Michael Myers had been changed into a knee-length dark two-piece dress and heels along with one of the kitchen knives, which completed her Halloween outfit.
“Exactly, Niffty… or should I say Michael Myers?” - you said to Niffty who gave you a proud smile and a few moments later a Halloween bucket appeared in both your free hand and Niffty’s hand.
“Don’t forget to smile Ladies!”, said Alastor from the reception before he and his shadow wrapped themselves in a dark cloud and disappeared.
“Alastor wanted to record a special podcast for Halloween… unfortunately he’s not coming with us”, explained Niffty and rustled the bag once.
“Oh, he’s already put some sweets in the bags. How nice of him”, you said happily and heard Lucifer quietly grinding his teeth.
“Could be poisoned and….”
“Daaad! Alastor is really trying to be nice!”
“Char-Char it….”
“Dad! Would he try to poison Niffty or the mother of my little sister and your daughter?”
“No?”
You could hear Lucifer wanting to say something else, but the ringing of his cell phone interrupted him. He let go of your hand, walked a few steps away and talked on the phone for a moment.
“I'm afraid I'll have to join you later... there's a meeting scheduled with my brothers and sisters... I'd really like to skip it, I told Asmodeus and Leviathan , that we wanted to go trick or treating with Niffty and....” - Lucifer had a pained expression on his face, but you completely understood. He was the king of hell, one of the seven deadly sins, and had obligations and duties that he had to fulfill.
“No problem Luci, we'll take care of ourselves and I think with Michael Myers by my side , nothing can happen to me”, you said lovingly and gave him a kiss on the cheek. If he has to go to this meeting, then so be it.
Lucifer smiled gratefully and then said goodbye.
You say goodbye to Charlie, who waves to you and Niffty as you leave the hotel, and then you set off with the little cyclops in your Halloween costumes, to visit the first shops and houses to do the well-known trick or treating.
It was something completely different to on earth.
Treat came first and usually something ends in flames or chaos if you have crappy candy... or don't open the door in the first place.
The children of hell, however, had a special position, got lots of candy and soon Niffty's little bucket was filled with lots of candy, a card for teeth cleaning at a Dentist Place, a poisonous green apple and a bracelet with a spider web design.
You also got a few things as a companion... candy and a saying like - well, pretty strawberry all alone? Niffty had scared the guy when she rang the bell and hit the air with the kitchen knife. She really took her role seriously. You shouldn't underestimate Michael Myers and the Strawberry Duo.
"What about the house? Does it belong to someone?", you nod once to an old building on the outskirts of the city, which was dilapidated and didn't look like it belonged to anyone...but appearances are deceptive, because as soon as you asked the question, a Hellborn with a broad smile appeared on the ground with a little yellow smoke.
"May I recommend our latest scare project to these costumed Halloween visitors? A Hunted House! For just a small entrance fee, there is an almost hour-long tour of scares and horror!", the Hellborn said mysteriously.
"Oh, that sounds exciting. Do you want to do that?", Niffty grabbed your free hand and you couldn't say no.
Maybe it was because of the baby fever, that was flaring up or because the cyclops was so small, but the pleading expression on Niffty's face triggered something in you that made you nod.
“A haunted house, huh? Let's see if we can scare the ghosts there!” - were your words, and after paying the entrance fee, the spooky fun could begin.
You ignore the slight stomach ache , that makes you grimace when you enter. That's probably from eating sweets. According to Niffty, that's part of a trick or treating trip. And you ate a lot of them as you went from house to house.
The Hellborn hadn't under-promised, the haunted house was much darker and scarier on the inside than it seemed.
There were scare actors, hidden rooms... spooky decorations and something that looked like the shadow of a real ghost.
The goal was to find a way to the exit through the labyrinth of rooms, stairs, secret rooms and hiding places. And it was fun... to get scared and discover the little details of the haunted house... the fog that suddenly appeared enveloped it in an even scarier atmosphere.
Up to the point where you and Niffty parted ways.
A trapdoor had opened under your feet and pulled you down to a lower floor... into the basement and Niffty's outraged cries had been swallowed up by the dark walls of the basement.
Nothing had happened to you when you hit the floor, a mattress had been provided and a few flashlights had been switched on for the visitors to light up the way in the darkness. You weren't afraid. The relationship with Lucifer and moving into the king's castle had given you a little more self-confidence.
When you turned the next corner and met a scar actor in a zombie outfit with one eye hanging out, you were frightened and let out a surprised scream... but you didn't expect the intense stomach pain that brought your body to its knees.
An intense pain took your breath away. For a moment, everything went everything goes black. The colors start to fade and the zombie comes a few steps closer, waving his axe in front of you and making... zombie noises.
"Aaaaaah!"- you scream, full of fear.
Real fear... something is wrong... your body is clearly signaling that something is wrong... and that it has nothing to do with the haunted house.
When something warm runs down your legs, you are confused... before a new threshold of pain causes you to scream louder, scared and panicked.
Tears form in your eyes and at that moment the scare actor , also realizes that something is wrong and contacts the owner of the haunted house via walkie talkie.
Only when the new wave of pain hits do you guess the reason.
It wasn't the zombie scare actor's great performance... that was premature labor.
But… it was much too early and… you instinctively push… a reaction from your body, while around you quick steps approached the basement… you are now lying on your back on the cold floor… another scream escapes you as your hands search for something to hold on to, but you can’t get a hold of anything, expect the gold ground.
Another contraction causes you to push, the panic and fear for your baby manifests itself in your brain. This isn’t how it should be… you… you… should have four more months left....four months of pure Happyness and looking forward to be a parent....to promise Lucifer he is going to be a good dad, he did a very good job with charlie after all....to have late night Walks in the Park with Lucifer, to kiss him good morning and in renturn he first gaves you a kiss on the forehead, and than a kiss on the stomach for the little baby girl.
It was much too early!
The next wave of pain exhausts you… your vision blurs and you feel, only half awake, how Niffty rushes to your side and grabs your hand, begging you to stay with her… the ambulance is on the way and you would be going to the hospital… but your eyes closed too fast....it went dark too fast.
Bright light blinds you as you open them again. The voices of the nurse and doctors are so loud. Your hand automatically goes to your stomach... your now flat stomach. Where is your BABY!? In a panic, you want to jump up and flee from the hospital bed, but a kind nurse stops you and the doctor treating you takes away your fear.
***
“There we have our patient again, don't worry, her little daughter is fine... she is in an incubator in the premature baby ward of the hospital, we will take her to her right away. Please rest” said the doctor.
She... is alive? Your baby, who was born four months early... survived? Was she okay? What happend to Niffty?
“How... what... and Niffty?”
What had happened to Niffty... was she still in the haunted house?
“Your companion threatened our head doctor, if he doesn't provide the best possible treatment and a single room for you and the baby... he will suffer...a lot” - was the nurse's answer with a slightly tortured laugh.
“If…if they’re afraid of Niffty, they’re scared of my Partner”
Lucifer would be terribly worried…hopefully he had finished his meeting with the other sins…damn overthinking and people pleasing…another habit of yours.
You were soon taken to your private room and were able to see your baby for the first time.
The incubator frightened you…all the tubes and wires the baby was connected to, the beeping monitors and equipment monitoring her vital signs…the feeding tube that had been put in…the little body rising and falling as she breathed and the fact that she had come into this world too early.
Tears welled up in your eyes and you were scared. Terribly scared.
The nice nurse and doctor, however, assured you that the technological standards and the chances of survival were good, even for hell.
And as the partner of the King of Hell, you would take extra good care of Mother and baby.
You were told what to look out for, how important it was that no germs got into the incubator and that you should make physical contact with the baby as soon as possible, talk to her a lot, sing to her...caring for you and your premature baby , would be unusual for both of you...but you were in good hands.
Your body, after you had assured yourself that the heart rate on one of the screens remained constant...craved rest...and you dared to go into a restless sleep. Sleep that your body desperately needed.
Several hours later, you were woken up by the gentle sounds of an all too familiar violin.
Lucifer sat by the baby's incubator and hummed the song - Hush little Baby - quietly accompanied by the music on the violin.
Another reason besides the hormones and the event that caused your inner dams to collapse and made you start to cry.
Silent…quietly just so as not to interrupt your partner's beautiful violin playing…but Lucifer notices it and is quickly at your side…apologizes to you so many times, even though he has done nothing wrong.
He is super careful, gives you several gentle kisses on the cheek and head of hair and swears to make the owner of the Haunted House suffer for putting you into premature labor.
“Luci….my Love, I don’t think it was the Haunted House’s fault….there are many reasons for a premature birth….we’ll be fine….will you stay with us….just a little bit, please Luci? I….am scared”, you whisper and grab your partner’s hands.
Lucifer stayed overnight.
The King of Hell had slept in a chair and you had woken up in a panic almost every time the machines used to monitor your daughter’s vital functions started beeping loudly.
Something else you’ll have to get used to…future false alarms, from the technical equipment while your baby is sleeping peacefully.
The nurses and the doctor treating you, are doing their best to take away your fear and worry...but mother and baby still have to stay in the hospital for a while...and it will be almost two weeks before Charlie and Vaggie can visit the intensive care unit.
"Naaaaaaw, she's so small and cute! Look at her Vaggie!", - cooed Charlie and could hardly tear himself away from the incubator and quietly talk to her little sister in baby talk , while Vaggie stood next to her partner.
Now that your body was feeling a little better, you sat down on one of the armchairs on Lucifer's lap and laid your head on his shoulder.
Your partner had been with you as often as possible at night, trying to support you where he could...and of course placed the large - congratulations it's a girl - gift basket from Ozzie and Fizzy in the room.
The sympathy for the birth of the other deadly sins was so heartwarming and the congratulations cards from the hotel residents, had made you cry tears of joy.
The public knew nothing about the premature princess. Lucifer, together with Queen Bee and Charlie, had silenced the media for the time being... you should enjoy and use the few weeks of peace that you still have left... because media hype and photos for the press were out of place.
"We don't have a name yet but... her middle name should be Charlotte" - you say and snuggle up to Lucifer, who lovingly strokes your hair. Which causes Charlie to let out an even more touched naaaaaw.
"Babe, we still have something for mother and child remember?", said Vaggie after another fifteen minutes in which Charlie had only looked devotedly at the sleeping baby in the incubator.
"Oh yes, of course... surprise!" - Charlie handed you a small bag.
You recognized the logo of the Halloween outfitter immediately.
Curiously, you reached into the bag and were able to pull out a set of three Halloween costumes.
"But these are..."
“Duck family costumes!” - Lucifer finished your sentence enthusiastically.
“Then you have a mama duck, daddy duck and baby duck for the coming next years Halloween!” - Charlie listed enthusiastically.
You didn't miss the fact that the princess' eyes started to light up when you said the word baby. Well, sounds like if someone start to get baby fever?
“Thanks Charlie and Vaggie... it's perfect!” - you thanked him and Lucifer also expressed his thanks.
“Then we already have a theme for the next year coming Halloween” - you said and looked lovingly at the baby duck costume... it would be a long time before your baby would fit into it.
“No haunted houses for the both you!” - Lucifer said seriously straight away.
You give him a loving kiss on the mouth and add the following sentence.
“I was thinking more of something like - Duck or Treat?”
THE END
AO3
#hazbin hotel characters#Lucifer x Reader#Lucifer x You#established relationship#hazbin hotel x reader#Halloween#Trick or Treat#Duck or Treat#Haunted House#Good Friend Niffty#pregnant#razzle hazbin hotel#dazzle hazbin hotel#charlie morningstar#vaggie hazbin hotel#parent lucifer morningstar#hospital#intensive care unit#premature baby ward#premature birth#fear#fanfiction#ao3 fanfic#hellaverse#angel dust#hazbin husk#spooky season#michael myers#halloween costumes#alastor the radio demon
48 notes
·
View notes
Text


ICU & ED simulation training -challenging but great experience!💪
#tmedic#studyblr#medicine#medblr#medblr community#emergency medicine#intensive care unit#intensive medicine#my stuff#studyspread#med school#medical university#anesthesiology#medical training#year5#med#uniblr#cpr#resuscitation#clinical medicine#icu care#medical blog#study medicine#aspiring docblr
45 notes
·
View notes
Text

From a little over 4 years ago. I was in a serious motorcycle accident, killed my girlfriend who was riding with me and nearly killed as I was brought back twice. I was in the hospital for almost 4 months, with 5 weeks of that in ICU. My left was amputated above the elbow because of the accident. Due to severe internal injuries, had to have colostomy. The colostomy just got reversed in April. Been a long road, but thankful and very lucky to be alive
#disabled#lesbian#limb loss#motorcycle accident#hospital stay#intensive care unit#colostomy#ostomate#ostomy reversal#lucky to be alive#my story
8 notes
·
View notes
Text
I am an occupational therapist working at a hospital. We are fighting for better working conditions to FINALLY get some relief. All the pressure and distress is captivating and harmful for all of us. Nurses, doctors, therapists, and every single person working in the german health care system. We could do so much better if the system would let us. But we need fair payment, more employees, and a fucking personal life.
And I feel hope. I really do. I am willing to fight for a better future. And we will fucking get it.
#germany#health care#therapist#we are fighting for society#intensive care unit#occupational therapy#ergotherapie#unions#union work#verdi#let the flame burn higher#gesundheitssystem#i have hope
6 notes
·
View notes
Text
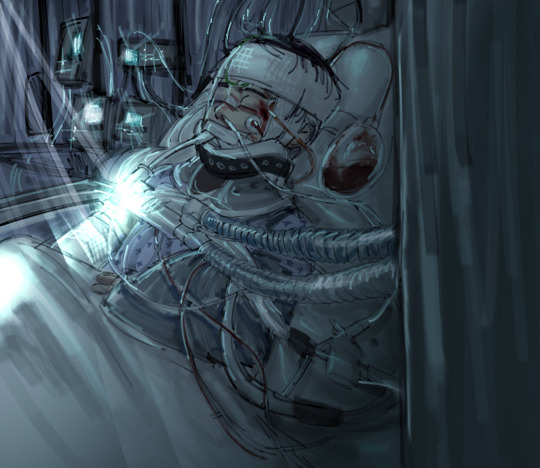
I.C.U., Pandora
#cw hospital#tw hospital#art#digital art#character design#oc#my oc#oc lore#oc trauma#hospital#intensive care unit#cw injury#original character#carboncopycomic
14 notes
·
View notes
Text
Btw, turned out that yes BUT the chocolate was worth it, i tell ya


I can't help myself😭




#digital#art#furry#artwork#drawing#furry art#anthro#furry anthro#canine#dog#samoyed#hot chocolate#sip#comics#winter#holidays#yed#hot drink#dog moment#hospital#ambulance#intensive care unit
2K notes
·
View notes
Text
Air Hostess : ವೆಂಟಿಲೇಟರ್ ನಲ್ಲಿದ್ದ ಗಗನಸಖಿಯ ಮೇಲೆ ಆಸ್ಪತ್ರೆ ಸಿಬ್ಬಂದಿಯಿಂದ ಲೈಂಗಿಕ ದೌರ್ಜನ್ಯ: ಗುರುಗ್ರಾಮದಲ್ಲಿ ನಡೆದ ಆಘಾತಕಾರಿ ಘಟನೆ....!
Air Hostess – ಗುರುಗ್ರಾಮದ ಖಾಸಗಿ ಆಸ್ಪತ್ರೆಯೊಂದರಲ್ಲಿ ವೆಂಟಿಲೇಟರ್ನಲ್ಲಿ ಚಿಕಿತ್ಸೆ ಪಡೆಯುತ್ತಿದ್ದ ಗಗನಸಖಿಯ ಮೇಲೆ ಆಸ್ಪತ್ರೆ ಸಿಬ್ಬಂದಿಯಿಂದ ಲೈಂಗಿಕ ದೌರ್ಜನ್ಯ ನಡೆದಿರುವ ಆಘಾತಕಾರಿ ಘಟನೆ ಬೆಳಕಿಗೆ ಬಂದಿದೆ. ರೋಗಿಯ ಆರೋಗ್ಯವನ್ನು ಕಾಪಾಡಬೇಕಾದ ಸಿಬ್ಬಂದಿಯೇ ಈ ಕೃತ್ಯಕ್ಕೆ ಒಳಗಾ��ಿರುವುದು ಸಾರ್ವಜನಿಕರಲ್ಲಿ ತೀವ್ರ ಆಕ್ರೋಶಕ್ಕೆ ಕಾರಣವಾಗಿದೆ. ಆರೋಪಿಗಳನ್ನು ಬಂಧಿಸಿ ಅವರ ವಿರುದ್ದ ಕಠಿಣ ಕ್ರಮ ತೆಗೆದುಕೊಳ್ಳುವಂತೆ ಆಗ್ರಹ ವ್ಯಕ್ತವಾಗುತ್ತಿದೆ. Air Hostess – ಘಟನೆಯ…
#critical condition patient#emotional hospital image#female patient#hospital bed with equipment#hospital ICU room#hospital monitoring equipment#hospital scene#ICU patient#Indian woman hospital#intensive care unit#medical care#medical emergency#patient life support#realistic hospital setup#serious health condition#tracheostomy tube#unconscious woman hospital bed#ventilator machine#ventilator support#woman on ventilator
0 notes
Text
0 notes
Text
2024-2032 Intensive Care Unit Market Revenue, Demand & Key Players
The Intensive Care Unit Market Revenue was valued at $7.30 billion in 2023 and is projected to grow significantly, reaching $10.82 billion by 2032. This growth, at a CAGR of 4.49% during the forecast period of 2024-2032, is driven by advancements in critical care technologies, increasing prevalence of chronic diseases, and the growing demand for specialized healthcare services globally.

Key Growth Drivers
The increasing global burden of critical illnesses, coupled with advancements in intensive care technology, is propelling the growth of the Intensive Care Unit (ICU) market. The rising incidence of cardiovascular diseases, respiratory disorders, and infectious diseases has led to a greater demand for ICU facilities equipped with state-of-the-art equipment.
Moreover, the integration of artificial intelligence (AI) and machine learning (ML) into ICU systems is enhancing patient monitoring and decision-making processes. These technologies allow healthcare providers to predict patient outcomes, optimize resource utilization, and improve overall care quality. The shift toward value-based care models further highlights the importance of ICUs in delivering high-quality, cost-effective patient care.
Regional Insights
North America leads the ICU market due to its advanced healthcare infrastructure, increasing geriatric population, and significant investments in healthcare technologies. Europe closely follows, with government initiatives to enhance healthcare facilities and address the growing demand for critical care services. Meanwhile, the Asia-Pacific region is expected to witness rapid growth due to rising healthcare awareness, increasing healthcare spending, and the prevalence of critical diseases.
Get Free Sample Report@ https://www.snsinsider.com/sample-request/3519
Market Outlook
As healthcare providers worldwide focus on enhancing critical care services, the ICU market is poised for sustained growth. Key trends include the adoption of portable ICU equipment, the development of smart ICUs leveraging IoT (Internet of Things) technologies, and increasing collaborations between technology providers and healthcare organizations. These advancements are expected to address the rising global demand for ICU facilities and ensure better patient outcomes.
About Us
SNS Insider is one of the leading market research and consulting agencies that dominates the market research industry globally. Our company's aim is to give clients the knowledge they require in order to function in changing circumstances. In order to give you current, accurate market data, consumer insights, and opinions so that you can make decisions with confidence, we employ a variety of techniques, including surveys, video talks, and focus groups around the world.
Contact Us
Akash Anand – Head of Business Development & Strategy Email: [email protected] Phone: +1-415-230-0044 (US) | +91-7798602273 (IND)
#Intensive Care Unit#Intensive Care Unit Market#Intensive Care Unit Market Size#Intensive Care Unit Market Share#Intensive Care Unit Market Growth#Market Research
0 notes
Text

🌟 Key Topics for the EDIC Exam: Intensive Care Essentials 🌟
Get ready to ace the European Diploma in Intensive Care Medicine (EDIC) exam! Here's a quick guide to the must-know areas:
A.Cardiovascular System: Master hemodynamic monitoring, shock types (septic, cardiogenic, hypovolemic, anaphylactic), and arrhythmias management.
B. Respiratory System: Get a grip on mechanical ventilation, ARDS treatment, and handling respiratory failure.
C.🩺 Renal System: Learn all about AKI, electrolyte imbalances, and renal replacement therapies like CRRT.
D.🧠 Neurological System: Know your TBI protocols, stroke management strategies, and handling status epilepticus.
E.🦠 Infectious Diseases: Be ready for sepsis and septic shock, and prevent nosocomial infections like VAP and CRBSI.
F.💊 Pharmacology: Perfect sedation and analgesia techniques, and practice antibiotic stewardship.
G.🤝 Ethics & End-of-Life Care: Navigate complex ethical dilemmas and provide compassionate end-of-life care.
Nail these topics and you're on your way to EDIC success! 🚀
0 notes
Text
Sahayog Hospital Pioneering Specialized Healthcare Excellence in Gondia
In the heart of Gondia, Maharashtra, Sahayog Hospital stands tall as a best hospital in gondia beacon of hope and healing for the community. With a steadfast commitment to providing exceptional healthcare services, Sahayog Hospital has emerged as the premier destination for specialized medical care in the region. From advanced brain and heart care to a wide array of super specialty services, the hospital is dedicated to ensuring superior clinical outcomes and patient satisfaction.
#Best Heart Hospital in Gondia#Best Critical Care Hospital in Gondia#Intensive Care Unit#Gastrointestinal Surgeon in Gondia
0 notes
Text
Transfer to ICU
Written sitting in corridor outside ICU Leah continued to find breathing difficult and has now been transferred to the Intensive Care Unit. Nic & I are in the relatives waiting area & have been told that it will be 30 or 40 minutes before we’re allowed to see her. I’m not used to being separated from Leah when she’s ill and I’m finding it very difficult – I feel that my role as a mother is to be…
View On WordPress
0 notes
Text
#intensive critical care unit in nagpur#intensive care unit#super speciality hospital in nagpur#best hospital in nagpur#hospital in dighori#hospital in nagpur
0 notes
Text
Today one of my clients died after two hours of cpr. I never thought this human was going to die in our hospital. It caught me off guard and now I am feeling everything and nothing at all. I am sad and empty but also dedicated to do what makes me happy. Because life can be over in just a blink of the eye.
#health care#hospital#intensive care unit#occupational therapy#occupational therapist talking to you#life is so precious#do what makes you happy#it can be over in a blink of an eye#the client was only 35#i dont know what to say#death is a certain companion#i am familiar with clients dying#but not like this#tw death
1 note
·
View note
Text
হিট স্ট্রোকে আক্রান্ত, দুবাইতে হাসপাতালের ICU-তে রয়েছেন অভিনেতা রাকেশ বাপাট
‘হিটস্ট্রোক’-এ আক্রান্ত ‘তুম বিন’ অভিনেতা রাকেশ বাপাট। গুরুতর অসুস্থ অবস্থায় তিনি দুবাইয়ের একটি হাসপাতালে ভর্তি রয়েছেন। এই মুহূর্তে তিনি হাসপাতালের ICU-রয়েছেন বলে খবর। মঙ্গলবারই রাকেশ বাপাট ইনস্টাগ্রাম হ্যান্ডেলের মাধ্যমে নিজের অসুস্থতার খবর শেয়ার করেন। মঙ্গলবার রাকেশ বাপাটের সোশ্যাল মিডিয়ায় যে ছবিটি পোস্ট করা হয় তাতে তাঁর হাতের একটি ছবি ছিল। যেখানে দেখা যায়, অভিনেতাকে চ্যানেলের মাধ্যমে IV…

View On WordPress
#Bollywood#dubai#Entertainment#Heat Stroke#Intensive Care Unit#Raqesh Bapat#অভিনেতা রাকেশ বাপাট#দুবাই#বিগ বস-১৫#রাকেশ বাপাট#হিট স্ট্রোক
0 notes