#Peutz-Jeghers syndrome
Text
Duodenal polyp a rare cause of repeated vomiting by Lahfidi Amal in Journal of Clinical and Medical Images, Case Reports

Clinical Image Description
A 50-year-old man without ATCD who suffers from dyspepsia and frequent vomiting, prompting him to seek medical help. There were no abnormalities found during the clinical evaluation. A CT scan of the abdomen was ordered to identify a duodenal polyp that was limiting the digestive light (Figure 1).
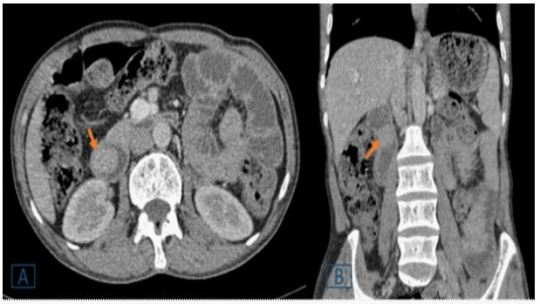
Figure 1: A duodenal endoluminal polyploid tissue process of 21 x 23 mm is shown on a transverse (A) and coronal (B) abdominal CT following contrast injection (orange arrow).
Peutz-Jeghers syndrome (PJS), juvenile polyposis, Cowden's disease, familial adenomatous polyposis, and Gardner's syndrome are polyposis syndromes that affect the duodenum [1]. Duodenal polyps are more common in children with polyposis syndromes, the majority of which are asymptomatic, according to a retrospective research in a pediatric population (aged 21 years) [2]. In the pediatric age group, duodenal polyps are seldom seen during standard high endoscopy (EGD) and radiographic investigations. In contrast, a recent study of adults using EGD and autopsy found a prevalence of up to 4.6 % [2]. Abdominal pain, vomiting, gastrointestinal bleeding, anemia, and intussusception or obstruction are among the symptoms [1, 2]. In comparison to the jejunum and ileum, duodenal disorders have received little attention in the imaging literature [1]. The exploration of the duodenum, which is still mostly examined by video endoscopy, has changed dramatically as a result of recent breakthroughs in imaging. However, advances in computed tomography (CT) and magnetic resonance imaging (MR) have made it easier to detect and characterize anomalies in the genesis of duodenal masses [1]. They are used to assess intraluminal content, the duodenum wall, and the extraduodenal area. The scanner, in combination with optimum intestinal distension and intravenous iodine contrast, provides for a thorough examination of the duodenum. Similarly, MRI has been demonstrated to be useful in diagnosing a wide spectrum of duodenal disorders when combined with duodenal distension and intravenous administration of a gadolinium-based contrast agent [1]. For the detection and characterization of a wide spectrum of duodenal lesions generating masses, CT remains the preferred imaging modality [1]. Large polyps (> 15 mm) might cause small intestinal blockage, thus it's important to keep an eye on them to see which ones need to be removed [1]. Protocols for monitoring are still being debated. Important polyps (big polyps with a proclivity for intussusception or blockage) are detected by endoscopy [1].
Surveillance in patients with polyposis syndromes was the most common reason for EGD; most of these patients were asymptomatic at the time of their EGD. In patients without polyposis syndrome, the most prevalent reason for EGD was stomach pain and vomiting [2]. CT and MRI can theoretically be used to monitor patients with many polyps and determine the best treatment, which could include endoscopic, enteroscopic, or surgical ablation, or a combination of these methods [1].
Competing Interests: The authors declare that they have no links of interest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#ATCD#frequent vomiting#dyspepsia#abnormalities#Peutz-Jeghers syndrome#polyposis syndromes#gastrointestinal#EGD#Lahfidi Amal#JCMICR
0 notes
Text
A better understanding of the causes of Black Gums
For many people, black gums might be an issue. Numerous variables, including heredity, lifestyle choices, and specific medical problems, may contribute to them. There are numerous choices if you're searching for a black gums treatment center in Mumbai. The causes of black gums and the various treatments at the closest dental clinic to grant road will be covered in this article.

Causes of Black Gums
Genetics
Due to their unique genetic composition, some people are born with inherently darker gums. Those with darker skin tones are more likely to experience this.
Smoking
One of the main causes of black gums is smoking. Over time, the gums may turn darker due to the nicotine and tar in cigarettes.
Inadequate Dental Hygiene
Inadequate dental hygiene can cause plaque and tartar to accumulate on teeth and gums. The gums may become irritated and turn darker as a result of this.
Certain drugs
As a side effect, some drugs, including tetracycline and minocycline, can cause the gums to get darker.
Medical Conditions
The gums may turn darker as a result of a number of illnesses, including Peutz-Jeghers syndrome and Addison's disease.
Melanin
The pigment that gives skin, hair, and eyes their color, melanin is a chemical that the body naturally creates. Gums that are dark brown or black may result from elevated melanin levels. Usually, there is no reason to be concerned if a person has always had extremely black gums because of melanin.
Smoker's Melanosis
Smoking can result in a darkening of the gums due to a disease known as smoker's melanosis. The melanin that the smoke deposited on the gums is the cause of this.
Specific Drugs
Black gums are a side effect of some medications, including antimalarial treatments, which can generate a condition known as drug-induced pigmentation.
Amalgam Tattoos
Amalgam tattoos can result in isolated patches of black, blue, or gray discolouration. They are caused by an accumulation of metal particles from dental fillings.
Treatment Options for Black Gums
There are various possibilities if you're searching for a dentist clinic in Grant Road or the closest dentist office in Mumbai for the treatment of black gums. The following are a few of the most popular forms of treatment:
Gum Depigmentation
This is a cosmetic surgery in which the outermost layer of the gums is removed to expose the healthier, lighter tissue beneath. Leading periodontists in Mumbai perform this treatment.
Laser Gum Care
A less intrusive substitute for conventional gum disease treatment is laser gum therapy. During this process, unhealthy tissue is removed using a laser, and the growth of good tissue is encouraged.
Maintaining Good Oral Hygiene
Black gums can be prevented and treated with proper oral hygiene. This entails flossing once a day, brushing twice a day, and scheduling routine cleanings and examinations at the dentist.
Give Up Smoking
Black gums can only be prevented and treated with quitting smoking. Although quitting can be difficult, there are a number of tools available to assist you, such as support groups and nicotine replacement treatment.
Medication Adjustment
Your doctor might be able to change your prescription or modify your dosage if your black gums are an undesirable consequence of one of your medications.
In Summary
Many people may be concerned about black gums, but there are a number of treatment options available. There are a number of possibilities in Mumbai if you're seeking for a facility that treats black gums, including The Maxfac facility. Treatment and prevention of black gums might also include changing medication, stopping smoking, and practicing proper oral hygiene.
#black gums treatment clinic in mumbai#nearest dental clinic#dental clinic in grant road#black gums#black gums treatment
1 note
·
View note
Text
What Causes the Presence of Dark Gums Around Your Teeth?

The occurrence of black or dark gums encircling teeth is a concern impacting both the aesthetics of one's smile and potentially signaling underlying health issues. While the natural shade of gums varies, the emergence of blackened areas disrupts the harmony between teeth and gums.
Several factors contribute to this discoloration. Excessive melanin, a natural pigment, can cause darkening of the gums. While some individuals might naturally have darker gums from birth, a shift from the usual pink to darker shades might indicate health concerns requiring medical attention.
Various health conditions could lead to blackened gums. Addison’s disease, affecting adrenal glands, may exhibit dark patches on gums, along with other symptomatic manifestations. Acute necrotizing ulcerative gingivitis, stemming from bacterial overgrowth, results in dark gums due to the accumulation of dead tissues, often accompanied by bleeding and foul breath.
Moreover, situations like amalgam tattoos, formed by displaced metal particles underneath oral tissues, or conditions such as Peutz-Jeghers Syndrome, a genetic disorder causing hyperpigmented patches, contribute to the discoloration of gums. Innocuous conditions like Blue Nevus or Eruption Hematoma during children's tooth eruptions can also lead to black spots on gums.
Recognizing black gums as a potential indicator of oral problems, systemic disorders, or even as side effects of medications and unhealthy habits like smoking is essential. Dentists offer various gum depigmentation or bleaching treatments akin to teeth whitening procedures to restore the natural pink hue of gums.
In essence, black gums often serve as a warning sign for underlying health issues, demanding professional assessment and attention. Whether stemming from oral conditions, medical ailments, or lifestyle choices, seeking dental advice and exploring suitable treatment options becomes crucial in restoring gum health and reviving a natural and radiant smile.
To know more, visit: https://www.aligndentalcare.lk/why-do-you-have-black-gums-around-your-teeth/
0 notes
Text
FDA grants first marketing authorization for a DNA test to assess predisposition for dozens of cancer types

- By U.S. Food and Drug Administration (FDA) -
On September 29, the U.S. Food and Drug Administration granted de novo marketing authorization for the Invitae Common Hereditary Cancers Panel, an in vitro diagnostic test that can help detect hundreds of genetic variants associated with an elevated risk of developing certain cancers.
The test can also help identify potentially cancer-associated hereditary variants in individuals with already-diagnosed cancer. The test, which is the first of its kind to be granted FDA marketing authorization, evaluates DNA extracted from a blood sample to identify variants in 47 genes known to be associated with an elevated risk of developing certain types of cancer.
“This test can assess multiple genes in a single test by using next-generation sequencing, which has proven helpful in providing insight into genetic variants with sensitivity and speed,” said Jeff Shuren, M.D., J.D., director of the FDA’s Center for Devices and Radiological Health. “Today’s action can provide an important public health tool that offers individuals more information about their health, including possible predisposition for certain cancers, which can help guide physicians to provide appropriate monitoring and potential therapy, based on discovered variants.”
According to the Centers for Disease Control and Prevention, there are more than 100 different documented types of cancer, a disease in which abnormal cells divide out of control and are able to invade other tissue. It is the second leading cause of death in the United States behind heart disease.
The Invitae Common Hereditary Cancers Panel can be used as a tool to help identify inherited causes of various types of cancers. Patients should speak with a healthcare professional, such as a genetic counselor, to discuss any personal/family history of cancer, as such information can be helpful in interpreting test results. Importantly, this test is not intended to identify or evaluate all known genes that can provide insight into predisposition for cancer.
For this prescription test, the specimen is collected at the point of care, such as a doctor’s office, and sent to a laboratory for testing. The clinical interpretation of the variants is based on evidence from published literature, public databases, prediction programs and Invitae’s internal curated variants database using Invitae's variant interpretation criteria consistent with those established by appropriate professional organizations or accredited boards. Some of the most clinically significant genes that the test identifies are: BRCA1 and BRCA2, which are genes with known associations to hereditary breast and ovarian cancer syndrome, Lynch syndrome associated genes (MLH1, MSH2, MSH6, PMS2 and EPCAM), CDH1 (mainly associated with hereditary diffuse gastric cancer, and lobular breast cancer) and STK11 (associated with Peutz-Jeghers Syndrome).
The FDA reviewed the Invitae Common Hereditary Cancers Panel under the FDA’s De Novo premarket review pathway, a regulatory pathway for low- to moderate-risk devices of a new type. To validate the performance, Invitae tested over 9,000 clinical samples, and achieved ≥99.0% accuracy for all tested variant types.
The risks associated with the test are mainly the possibility of false positive and false negative test results, as well as possible misunderstanding of the results. False negative test results may provide a false sense of assurance and these patients may not receive appropriate surveillance or clinical management. False positive test results could lead to inappropriate decision-making regarding healthcare and lifestyle, which can be associated with other undesirable clinical consequences. Further, since this test is not intended to identify or evaluate all known genes associated with a predisposition for cancer, and genetics are not the only factor in development of cancer, there is a risk of patients misunderstanding that they still have some risk of developing cancer following a negative test result. These risks are mitigated by the analytical performance validation, clinical validation and appropriate labeling of this test.
Along with this De Novo authorization, the FDA is establishing special controls that define the requirements related to labeling and performance testing. For example, accuracy for reporting of substitutions, insertions/deletions and copy number variants must be ≥99.0% for positive agreement and ≥99.9% for negative agreement with a validated orthogonal method. When met, the special controls, in combination with general controls, provide a reasonable assurance of safety and effectiveness for tests of this type.
Today’s action creates a new regulatory classification, which means that subsequent devices of the same type with the same intended use may go through FDA’s 510(k) premarket process, whereby devices can obtain marketing authorization by demonstrating substantial equivalence to a predicate device, which may save a developer time and expense compared to other review pathways.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
--
Source: U.S. Food and Drug Administration (FDA)
Read Also
Study: AI can forecast how well breast cancer treatment will work
0 notes
Text
Is colorectal cancer hereditary?

Yes, colorectal cancer can have a hereditary component. Here's more information:
Colorectal cancer can be influenced by both genetic and environmental factors. While the majority of cases are sporadic, meaning they occur without a strong family history, about 5-10% of colorectal cancer cases are linked to inherited genetic mutations.
There are several hereditary syndromes that can increase the risk of developing colorectal cancer:
1. Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer or HNPCC):
Lynch syndrome is the most common inherited cause of colorectal cancer. It is caused by mutations in certain genes that are responsible for DNA repair. People with Lynch syndrome have a significantly higher risk of developing colorectal cancer, as well as other types of cancer such as endometrial, ovarian, and stomach cancers.
2. Familial Adenomatous Polyposis (FAP):
FAP is characterized by the development of hundreds to thousands of polyps in the colon and rectum. If left untreated, these polyps can turn into cancer. FAP is caused by mutations in the APC gene. Individuals with FAP usually develop colorectal cancer at a younger age.
3. MYH-Associated Polyposis (MAP):
MAP is caused by mutations in the MYH gene. Similar to FAP, it leads to the development of multiple polyps in the colon and an increased risk of colorectal cancer.
4. Peutz-Jeghers Syndrome:
This syndrome is characterized by the development of polyps in the digestive tract and pigmented spots on the skin and mucous membranes. People with this syndrome have an increased risk of various cancers, including colorectal cancer.
5. Juvenile Polyposis Syndrome:
This rare syndrome causes the development of polyps in the digestive tract during childhood. While the risk of colorectal cancer is increased, it also elevates the risk of other types of cancer.
6. Other Syndromes:
There are several other rare hereditary syndromes that can increase the risk of colorectal cancer, such as MUTYH-associated polyposis (MAP), Cowden syndrome, and Gardner syndrome.
It's important to note that having a family history of colorectal cancer doesn't necessarily mean you will develop the disease, but it does increase your risk. If you have a family history of colorectal cancer or suspect a hereditary syndrome, it's advisable to consult a genetic counselor and discuss appropriate screening and prevention strategies. Regular screenings and early detection are crucial in managing the risk associated with hereditary forms of colorectal cancer.
For more information, Consult Dr. Chintamani Godbole as he provides the Best Colorectal Surgeon in Mumbai
#drchintamanigodbole
#colorectal surgeon in mumbai.
#colon cancer treatment in mumbai
0 notes
Text
Understanding the Prevalence of Small Intestine Cancer
Introduction:
Small intestine cancer, also known as small bowel cancer, is a rare type of cancer that affects the tissues of the small intestine. While it may not receive as much attention as other types of cancer, understanding its prevalence is crucial for raising awareness and ensuring early detection and treatment. In this article, we will delve into the incidence, risk factors, and prognosis of small intestine cancer to shed light on its prevalence in the general population.
Incidence and Prevalence:
Small intestine cancer is considered a rare malignancy, accounting for approximately 1% to 2% of all gastrointestinal cancers. According to statistics, there are approximately 10,000 to 15,000 new cases of small intestine cancer diagnosed each year worldwide. While the incidence varies geographically, it is estimated that around 3,000 cases are diagnosed annually in the United States.
Risk Factors:
Identifying the risk factors associated with small intestine cancer can help individuals and healthcare professionals understand the likelihood of developing the disease. Several factors have been linked to an increased risk of small intestine cancer, including:
Age: The risk of developing small intestine cancer tends to increase with age, with the majority of cases occurring in people over the age of 60.
Gender: Men are slightly more prone to small intestine cancer compared to women.
Genetic conditions: Inherited disorders such as familial adenomatous polyposis (FAP), Lynch syndrome (hereditary nonpolyposis colorectal cancer), and Peutz-Jeghers syndrome increase the risk of small intestine cancer.
Crohn’s disease: Individuals with long-standing Crohn’s disease affecting the small intestine may have an elevated risk.
Celiac disease: People with celiac disease, a chronic digestive disorder, have a slightly higher risk of developing small intestine cancer.
Radiation exposure: Prior radiation therapy for other cancers in the abdomen or pelvis can increase the risk of small intestine cancer.
Prognosis and Survival Rates:
The prognosis for small intestine cancer depends on various factors, including the stage at diagnosis, the size and location of the tumor, and the overall health of the patient. Unfortunately, small intestine cancer is often diagnosed at an advanced stage due to the non-specific nature of its early symptoms, leading to a lower survival rate compared to some other cancers.
The five-year survival rate for small intestine cancer varies depending on the stage at diagnosis. On average, the five-year survival rate for localized small intestine cancer is around 70%. However, this rate drops to approximately 40% for cases where the cancer has spread to regional lymph nodes and further decreases to about 5% for distant metastatic disease.
Conclusion:
Small intestine cancer is a rare form of cancer that affects the tissues of the small intestine. While its prevalence is relatively low compared to other cancers, it is essential to be aware of its risk factors and symptoms. Early detection and timely treatment can significantly improve the prognosis and survival rates for individuals diagnosed with small intestine cancer. Maintaining a healthy lifestyle, undergoing regular screenings, and consulting with healthcare professionals can contribute to the early detection and better management of this rare malignancy.
0 notes
Text
Ayushman Day Care Centre For Lip Hyperpigmentation
What Is Lip Hyperpigmentation Surgery?
Lip Hyperpigmentation refers to the darkening of the skin on the lips beyond the normal range of pigmentation. This condition is caused by an increase in the production of melanin, which is the pigment that gives colour to our skin, hair, and eyes.
Lip hyperpigmentation can occur due to a variety of reasons, including exposure to the sun, hormonal changes, certain medications, smoking, and underlying medical conditions such as Addison's disease and Peutz-Jeghers syndrome.

What Is The Purpose Of Lip Hyperpigmentation Surgery?
The purpose of hyperpigmentation treatment is to reduce or eliminate the excess pigmentation in the skin, resulting in a more even skin tone. This can be done through various methods, depending on the cause and severity of the hyperpigmentation.
The main goal of hyperpigmentation treatment is often cosmetic, as many people with hyperpigmentation feel self-conscious about the appearance of their skin. However, in some cases, hyperpigmentation may be a symptom of an underlying medical condition, such as melasma or certain autoimmune disorders, and treating hyperpigmentation may also improve the underlying condition.
What Are The Benefits Of Lip Hyperpigmentation Surgery?
here are some of the benefits of lip hyperpigmentation at the Skin & Cosmetology Centre.
Improved Appearance:- One of the most significant benefits of lip hyperpigmentation surgery is that it can improve the appearance of the lips.
Boosted Self-Confidence:- For many people, having hyperpigmentation on their lips can be a source of insecurity and lower their self-esteem.
Permanent Results:- Unlike topical treatments or other temporary solutions, lip hyperpigmentation surgery can provide permanent results, meaning you won't need to keep applying creams or undergoing treatments to maintain the results.
Minimal Scarring:- The surgery is typically done with a CO2 laser, which can help to minimize scarring and achieve a smoother, more uniform appearance.
Is Lip Hyperpigmentation Surgery Safe?
lip hyperpigmentation surgery can be a safe and effective way to improve the appearance of your lips. It is essential to have a thorough consultation with your surgeon and carefully follow their pre-operative and post-operative instructions to ensure the best possible outcome.
What To Do For Recovery After Surgery?
Here are some general tips for recovery after surgery in Skin & Cosmetology Centre Dwarka Sector 12.
Rest and Avoid Strenuous Activities:- You should avoid strenuous activities and rest for the first few days after surgery to allow your body to heal.
Keep Your Lips Clean:- Your plastic surgeon will provide you with instructions on how to clean your lips after surgery.
Apply Ice Packs:- Applying ice packs to the lips can help to reduce swelling and discomfort.
Take Pain Medication:- Your surgeon may prescribe pain medication to help manage discomfort during the recovery period. Follow their instructions on how to take the medication, and avoid taking any additional pain relievers without their approval.
Conclusion
In conclusion, Lip Hyperpigmentation refers to the darkening of the skin on the lips, which can be caused by a variety of factors. While it is typically a harmless condition, some people may choose to undergo treatment to reduce the pigmentation and achieve a more even skin tone.
#ayushman skin & cosmetology centre in dwarka sector 12#ayushman skin & cosmetology centre in dwarka#ayushman skin & cosmetology centre#ayushman skin & cosmetology#skin & cosmetology centre in dwarka Sector 12.#Skin & Cosmetology centre dwarka#skin & cosmetology centre.
0 notes
Text
What is stomach cancer? What are the symptoms and treatment methods? 2023
New Post has been published on https://bankakredin.com/what-is-stomach-cancer-what-are-the-symptoms-and-treatment-methods-2023/
What is stomach cancer? What are the symptoms and treatment methods? 2023
Stomach cancer is caused by abnormal division of cells in the stomach. The stomach is a muscular organ located in the upper part of the abdominal cavity on the left side just below the ribs. Oral food is delivered to the stomach via the esophagus. Foods reaching the stomach can be kept in the stomach for a while. They are then destroyed and digested.
The stomach consists of four parts: the “cardia”, to which the esophagus is connected and called the stomach gate, the “fundus”, which is the upper part of the stomach, the “corpus”, which is the body of the stomach, and the “pylorus”, which connects the stomach to the small intestine. Gastric cancer, also known as gastric cancer, can originate from any part of the stomach. In most parts of the world, the most common site of stomach cancer is the body of the stomach. However, in the United States, the most common site of gastric cancer initiation is the gastroesophageal junction, where the stomach and esophagus connect.
Stomach cancer is a slowly progressive disease. It mostly occurs in people between the late 60s and 80s.
What Are the Types of Stomach Cancer?
Gastric cancer originates from the glandular cells that cover the inner surface of the stomach at a rate of 95%. Stomach cancer can progress and spread to the stomach wall and even to the blood or lymphatic circulation.
Gastric cancer is named according to the cell from which it originates. Some common stomach cancers are as follows:
Adenocarcinoma : The most common type of stomach cancer. The tumor is formed from the glandular structure that covers the inner surface of the stomach.
Lymphoma : It originates from lymphocyte cells in the immune system.
Sarcoma : It is a type of cancer originating from adipose tissue, connective tissue, muscle tissue or blood vessels.
Metastatic cancer : It is a type of cancer whose primary cancer tissue is not in the stomach, which is seen as a result of the spread of other cancers such as breast cancer, lung cancer or melanoma to the stomach.
Other types of stomach cancer, such as carcinoid tumor, small cell carcinoma, and squamous (squamous) cell carcinoma, are less common.
What are the Causes of Stomach Cancer?
The mechanism that triggers the uncontrolled growth and proliferation of cells in the stomach and leads to cancer is not fully known. However, it has been determined that there are some factors that increase the risk of gastric cancer. One of these is H. pylori bacteria, which can cause a widespread asymptomatic infection and stomach ulcers. Gastritis, which is defined as inflammation of the stomach, pernicious anemia, which is a long-lasting anemia, and polyps, which are structures protruding from the stomach surface, increase this risk. Other factors that increase the risk of stomach cancer are given below:
To smoke
Being overweight or obese
Excessive consumption of smoked and salty foods
Consuming too much pickle
drinking alcohol regularly
Having stomach surgery due to ulcer
A blood group
Epstein-Barr virus infection
some genes
Working in the coal, metal, timber or rubber industry
asbestos exposure
Having a family history of stomach cancer
Having Familial Adenomatous Polyposis (FAP), Hereditary Nonpolyposis Colorectal Cancer (HNPCC)-Lynch Syndrome, or Peutz-Jeghers Syndrome
Stomach cancer begins when cells in the stomach change their DNA, which is the genetic material. These changes allow cancer cells to divide and live very quickly while healthy cells die. Over time, cancer cells combine and wash away healthy tissue. Thus, it can spread to other parts of the body.
What are the Symptoms of Stomach Cancer?
The most common symptom of stomach cancer is weight loss. The patient has lost 10% or more of his body weight in the last 6 months. The following symptoms can be counted as early signs of stomach cancer:
Indigestion
feeling bloated after eating
burning sensation in chest
mild nausea
Loss of appetite
Symptoms such as indigestion or a burning sensation in the chest alone do not indicate cancer. However, if the complaints are too many and more than one symptom is seen, the patient is examined in terms of risk factors for gastric cancer and some tests may be requested.
As the tumor size increases, the complaints become serious. The following serious symptoms can be seen in the later stages of stomach cancer:
Stomache ache
seeing blood in the stool
Vomiting
Weight loss for no apparent reason
difficulty swallowing
Yellowish eye whites and yellowish skin color
swelling in the stomach
constipation or diarrhea
Weakness and fatigue
chest pain
The above-mentioned complaints are more serious and require a doctor’s consultation.
How is Stomach Cancer Diagnosed?
There is no screening test for stomach cancer. In the last 60 years, there has been a decrease in gastric cancer cases. However, people with a family history or syndromes that pose a risk for stomach cancer should go to routine controls. The patient’s medical history is taken and begins with a physical examination.
If the doctor deems it necessary, he may order some tests such as:
Tumor Markers: Blood level of substances known as cancer markers (CA-72-4, carcinoembryonic antigen, CA 19-9)
Endoscopy: The stomach is looked at with the help of a thin and flexible tube and a camera.
Upper Gastrointestinal System X-ray: A limy liquid called barium is given to the patient and the stomach is visualized on the direct X-ray.
Computed Tomography: It is an imaging device that creates detailed images with the help of X-ray rays.
Biopsy: It is examined pathologically by taking a sample from the abnormal tissue of the stomach. The definitive diagnosis is biopsy and the type of cancer is determined by the pathology result.
How Is Stomach Cancer Treatment?
The most important factor determining the treatment of gastric cancer is the stages of gastric cancer. Stomach cancer stages; It is determined by the size of the tumor, whether it has spread to the lymph node, whether it has spread to a place other than the stomach.
Stage 0 : It is the presence of unhealthy cells that have the potential to turn into cancer cells in the epithelial layer covering the inner surface of the stomach. A cure is achieved by removing part or all of the stomach with surgery. Along with the stomach, the lymph nodes near the stomach, which are an important part of the immune system in our body, are also removed.
Stage 1: At this stage, there is a cancer cell in the stomach and may have spread to the lymph nodes. As in stage 0, some or all of the stomach and lymph nodes in the nearby region are removed with surgery. Chemotherapy or chemoradiotherapy may be added to treatment before or after surgery. It is used before surgery to reduce the size of the cancer and to remove more with surgery, and when done after surgery, it is used to kill the remaining cancer cells after surgery. Chemotherapy is drugs that aim to kill cancer cells. In addition to drugs, chemoradiotherapy aims to kill cancer cells by making use of the high energy of the rays with radiotherapy.
Stage 2 : The cancer has spread to the deeper layers of the stomach and lymph nodes. Similar to stage 1 treatment, the main treatment in stage 2 consists of pre- or post-surgical chemoradiotherapy and surgery.
Stage 3 : Cancer has spread to all layers of the stomach, as well as to nearby organs such as the spleen and colon. The entire stomach is removed with surgery and chemotherapy is given. However, although this treatment does not provide a definitive cure, it relieves the patient’s symptoms and pain.
Stage 4 : Cancer has spread to organs far from the stomach, such as the brain, lungs, and liver. Curing is much more difficult, the goal is to relieve symptoms.
What Can Be Done to Prevent Stomach Cancer?
Some of the measures that can be taken to prevent stomach cancer are listed below:
quit smoking
Treating a stomach ulcer
Eating a healthy diet with fiber-rich foods
not consuming alcohol
Using pain relievers and medications like aspirin cautiously
If you have a lot of stomach ailments or if you have serious complaints such as seeing blood in the stool or losing weight quickly, it is recommended that you apply to health institutions and get support from specialist physicians.
stomach cancer,are stomach cancer symptoms intermittent,are stomach cancers curable,are stomach cancer and colon cancer related,are stomach cancer symptoms constant,are stomach cancer symptoms persistent,are stomach cancer lumps painful,what are stomach cancer symptoms,what are stomach cancers,what are stomach cancer treatments,what are stomach cancer chemo,can stomach cancer be cured,can stomach cancer kill you,can stomach cancer be detected by blood test,can stomach cancer cause diarrhea,can stomach cancer cause weight gain,can stomach cancer be seen on ct scan,can stomach cancer cause back pain,can stomach cancer cause itchy skin,can stomach cancer cause shortness of breath,
#are stomach cancer and colon cancer related#are stomach cancer lumps painful#are stomach cancer symptoms constant#are stomach cancer symptoms intermittent#are stomach cancer symptoms persistent#are stomach cancers curable#can stomach cancer be cured#can stomach cancer be detected by blood test#can stomach cancer be seen on ct scan#can stomach cancer cause back pain#can stomach cancer cause diarrhea#can stomach cancer cause itchy skin#can stomach cancer cause shortness of breath#can stomach cancer cause weight gain#can stomach cancer kill you#stomach cancer#what are stomach cancer chemo#what are stomach cancer symptoms#what are stomach cancer treatments#what are stomach cancers
0 notes
Text
Peutz-Jeghers syndrome is an autosomal dominant disorder. There are two manifestations of Peutz-Jeghers syndrome: pigmented mucocutaneous macules and multiple hamartomatous gastrointestinal polyps, which are usually benign but may produce symptoms or become malignant. Polyps begin to grow in the first decade of life and most patients become symptomatic between the age of 10 and 30. Gastrointestinal symptoms can be caused by obstruction from intussusception or occlusion of the lumen by polyps, abdominal pain caused by infarction, acute or chronic rectal bleeding from ulceration, and extrusion of polyps through the rectum. About 50% of these patients will have an intussusception during their lifetime, most often in the small bowel. The treatment is surgical removal of the polyps if they become symptomatic or if they are very large. Intussusception presents with colicky abdominal pain, vomiting, currant jelly stools, abdominal tenderness, and palpable abdominal mass. It is the most common cause of bowel obstruction in the first two years of life. In adults intussusception is considered to be caused by a mass until proven otherwise. A common location of intussusception is the ileocecal junction.
Bottom Line: Patients with Peutz-Jeghers syndrome have pigmented mucocutaneous macules and hamartomatous polyps of the gastrointestinal tract. Nearly half of all these patients will have an intussusception during their lifetime.
2 notes
·
View notes
Text
Duodenal polyp a rare cause of repeated vomiting by Lahfidi Ama in Journal of Clinical and Medical Images, Case Reports

Clinical Image Description
A 50-year-old man without ATCD who suffers from dyspepsia and frequent vomiting, prompting him to seek medical help. There were no abnormalities found during the clinical evaluation. A CT scan of the abdomen was ordered to identify a duodenal polyp that was limiting the digestive light (Figure 1).
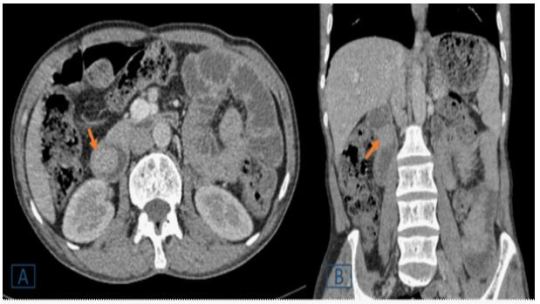
Figure 1: A duodenal endoluminal polyploid tissue process of 21 x 23 mm is shown on a transverse (A) and coronal (B) abdominal CT following contrast injection (orange arrow).
Peutz-Jeghers syndrome (PJS), juvenile polyposis, Cowden's disease, familial adenomatous polyposis, and Gardner's syndrome are polyposis syndromes that affect the duodenum [1]. Duodenal polyps are more common in children with polyposis syndromes, the majority of which are asymptomatic, according to a retrospective research in a pediatric population (aged 21 years) [2]. In the pediatric age group, duodenal polyps are seldom seen during standard high endoscopy (EGD) and radiographic investigations. In contrast, a recent study of adults using EGD and autopsy found a prevalence of up to 4.6 % [2]. Abdominal pain, vomiting, gastrointestinal bleeding, anemia, and intussusception or obstruction are among the symptoms [1, 2]. In comparison to the jejunum and ileum, duodenal disorders have received little attention in the imaging literature [1]. The exploration of the duodenum, which is still mostly examined by video endoscopy, has changed dramatically as a result of recent breakthroughs in imaging. However, advances in computed tomography (CT) and magnetic resonance imaging (MR) have made it easier to detect and characterize anomalies in the genesis of duodenal masses [1]. They are used to assess intraluminal content, the duodenum wall, and the extraduodenal area. The scanner, in combination with optimum intestinal distension and intravenous iodine contrast, provides for a thorough examination of the duodenum. Similarly, MRI has been demonstrated to be useful in diagnosing a wide spectrum of duodenal disorders when combined with duodenal distension and intravenous administration of a gadolinium-based contrast agent [1]. For the detection and characterization of a wide spectrum of duodenal lesions generating masses, CT remains the preferred imaging modality [1]. Large polyps (> 15 mm) might cause small intestinal blockage, thus it's important to keep an eye on them to see which ones need to be removed [1]. Protocols for monitoring are still being debated. Important polyps (big polyps with a proclivity for intussusception or blockage) are detected by endoscopy [1].
Surveillance in patients with polyposis syndromes was the most common reason for EGD; most of these patients were asymptomatic at the time of their EGD. In patients without polyposis syndrome, the most prevalent reason for EGD was stomach pain and vomiting [2]. CT and MRI can theoretically be used to monitor patients with many polyps and determine the best treatment, which could include endoscopic, enteroscopic, or surgical ablation, or a combination of these methods [1].
Competing Interests: The authors declare that they have no links of interest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Peutz-Jeghers syndrome#juvenile polyposis#computed tomography#gastrointestinal bleeding#vomiting#endoscopy#enteroscopic#Lahfidi Ama#JCMICR
0 notes
Text
TBC is done! My giant comic project is also done, and I'm both pleased and a little distressed: what am I going to do with my time now? Finish up my dozens of older projects? That's not very me.
I thought the ending would feel very bittersweet - I've been in a bit of a distressed kind of Mood about the game lately, not helped by the community's reaction to the ending - but no, I'm actually fairly satisfied with it, and I'm pleased that a great deal of the ending was ultimately left ambiguous. It leaves room for everyone to come to what conclusions they want, and with stories, that always feels the best.
In health news: I attended my dermatology visit, which was very stressful going in, and significantly less so coming out. The doctor apparently saw my chart, and got very excited, because autoimmunal pancreatitis is rare, and he thought that I must have it from IGG4, if I was having skin issues. So he brought in his entire gaggle of medical ducklings..
.. and then got disappointed to realise that I do not have IGG4 symptoms, which is a surprise to me, haha. Pancreatitis is so hard to research! I know I have autoimmunal, but I did not realise there was even a difference between hereditary and IGG4-based pancreatitis in the first place. He still used it as an opportunity to drill his students on pancreatitis, though, which was fun, and educational to me as well, haha.
He also gave me a referral to a pancreatric specialist with his network, too, which is nice: I went to Cleveland to get seen by one of the state's Top Specialists, per google and my GP, and said specialist was very thrown over the fact I didn't have substance-based pancreatitis. Very thrown, and kind of judgemental! Meanwhile, this doctor's first words after interrogating me on pancreatitis for his students were: "oh, you must get people thinking you abuse alcohol a lot, huh?"
It's very nice to have a doctor.. not assume I am lying, or immediately jumping to negative conclusions, lol. Very nice, and unfortunately, very rare! But his network actually handles autoimmunal and hereditary pancreatitis, and I am so relieved that there is potentially an end to sight in dealing with this. He seemed very certain there were multiple treatment options involving pills, rather than surgery, for it. I'm crossing my fingers!
Also crossing my fingers that, for all that I'm pleased over him inexplicably hyperfocusing in on my pancreatitis, he is not entirely correct on his diagnosis of my skin issue? He looked over the dark spots, asked a lot about family history and my grandfather's mysterious abdominal surgeries, and then immediately said, oh, this is almost undoubtedly Peutz-Jeghers Syndrome, and I probably just hadn't noticed any of the symptoms in the past, because pancreatitis is a good way to mask it, but my bizarre lip spots are pretty indicative of it. So go to the gastro he was referring me to, get the pancreatitis checked, and get testing for the PJS, so it can be treated!
And in the meanwhile, don't freak out! :)
Because, as he lovingly informed his ducklings, patients always look these things up on their phones and then spend the next three months freaking the fuck out.
And who am I, but a stereotype?
I'm not letting mysef froth over it too much, haha, or at least, I'm trying not to! Darcel and I do have markers for it, per Promethease, but that isn't necessarily reliable, and it's certainly not a diagnosis of anything. Still, I keep eyeing that, and then eyeing Cleveland Clinic's cheery note that "the lifetime risk of developing any sort of cancer is estimated to be as high as 93 percent", and midkey frothing. I would really just like to be healthy! I do not want to have to memorise how to spell fucked up German disorders! Going into an appointment to ensure I do not have cancer, and getting told "you don't have cancer! but eventually you might! :)" is not my favorite activity!
But if I do have it, whatever, lol. This shit is what preventative care is for, I suppose, and if I have to make time to go and get checked out regularly, I'll make do. The health complications and risks seem as if they primarily come down to not having preventative care, which is something I can work with.
#d. rambles#the mysterious fainting waif disease#more like 'the mysterious flaming trash bag in your apartments dumpster disease' at this point lmao#I am so glad I did not plan on having kids because yeah nooo.
8 notes
·
View notes
Text
post ain't long it's wrong, can't study till dawn? yawn
100 days of productivity
day 44 + 45
CVS/RS
rheumatoid pleural effusions closely mimic complicated parapneumonic effusion on analysis, w/ ph <7.2, marked ↑LDH and notably glucose <30 (in fact glucose >30 almost rules out rheumatoid effusion)
in afib, digoxin will slow ventricular rate but is unlikely to cardiovert the rhythm
itraconazole in ABPA causes a 50% reduction in steroid dose and 25% reduction in anti-aspergillus IgE, and either partial or complete resolution of CXR infiltrates or improvement in PFTs/exercise tolerance
TRALI can happen as early as 15 minutes into the transfusion apparently?????
mesothelioma is an abject death sentence. The most you can do for patients beyond stage 1 is chemotherapy (limited survival benefit with platinics), radiotherapy to biopsy/thoracoscopy tracts only and surgery (lung-sparing debulking ± pleurodesis for recurrent effusions; radical surgery has shown no survival benefit)
mild tachy + broad qRs in haemodynamically stable pt s/p PCI for MI → likely to be LBBB developing; watch and wait
CNS/Ophthal/Psych
PSP looks similar to parkinson's bc it affects the opposite pathway as parkinsons (striatonigral vs nigrostriatal)
the best response you can get from deep brain stimulation for parkinsons = the best response you got from medication; DBS will NOT add a greater response compared to maximum medical therapy
without any other information, parkinson's ssx w/ dementia WITHIN 1 year of onset, it's Lewy body dementia; if it's more than 1 year, it's parkinson's w/ 2° dementia
choroidal neovascularisation with NO OTHER fundal signs: wet mac degen > diabetic retinopathy
focal dystonias are better treated with botox than with medication
SAH is unlikely to cause cranial nerve palsies other than III and maybe VI; pituitary apoplexy presents similarly with very severe headache/projectile vomiting/AMS, while affecting nerves III, IV, V-1 and VI
MS relapse: 500 mg PO or 1 g IV methylpred x5 days
there is no difference in risk of progression to Korsakoff when Wernicke is treated w/ glucose first vs w/ thiamine first
Endocrine/Repro
hyperaldosteronism: hyperplasia > adenoma
acute alcohol consumption can trigger hypoglycaemic events as the liver uses up NAD+ for each step of the alcohol detox pathway, where NAD+ is an important cofactor for the malate-oxalate shuttle used in gluconeogenesis
cinacalcet's major indication is hyperparathyroidism taht can't be corrected w/ surgery (eg, unfit pts)
Rheum/Derm/Immuno
topical steroid potency: hydrocortisone < clobetasol butyrate, betamethasone valerate low-dose < betamethasone valerate high-dose, fluticasone propionate < clobetasol propionate
onycholysis: trauma, tinea (infections), thyrotoxicosis, tetracyclines
pseudoxanthoma elasticum is assoc w/ mitral prolapse, renovascular htn, PVD, CAD, GIT bleeds and retinal vessel abnormalities
IgE values are normally distributed, so about 2.5% of the pop has raised IgE and 2.5% has reduced
s/p parathyroidectomy → acute drop in PTH → bones that are used to high levels of PTH experience a relative hypoPTHism → ↑blastic ↓clastic activity → acute bony uptake of calcium, PO4 and importantly magnesium = hungry bone syndrome (replace calcium and magnesium!)
carpal tunnel pain can radiate retrogradely to the forearm and sometimes even the arm
periarticular osteoporosis → RA
punched out erosions in juxtaarticular bone → gout
GIT
Peutz-Jeghers: small bowel hamartomas → intussusception, colorectal cancer, pigmented lesions (classically perioral/mucosal, but also palms/soles)
pernicious anaemia: parietal cell Abs (common) > intrinsic factor Abs (specific)
haemochromatosis: venesection → keep ferritin <50 and transferrin sat <50%
passing stools frequently, elevated inflammatory markers, ↑faecal calprotectin, PPI but not in demographic for IBD → take a colonoscopy and biopsy, this is probably microscopic colitis (and PPIs can trigger at any age)
liver biopsy is not indicated for Gilbert's—it is sufficient to do routine CBCs/LFTs w/ bilirubin analysis
pancreolauryl (fluorescein dilaurate) is quite nonspecific and will not pinpoint the exact pancreatic disease
hep A can be precided by short diarrhoeal illness`
in an IBD (esp UC) pt who comes >10 yrs after initial symptoms with recent change in bowel habits, offer urgent colonoscopy to r/o ca colon BEFORE starting on treatment
Onc/Haem
MTX + antifolate antibiotics: makes sense not to give them together—they can cause fulminant marrow failure
leukaemia can very rarely lead to acute painful scrotal swelling
5q- syndrome = myelodysplasia, but with thrombocytosis; diff from essential thrombocythaemia by anaemia with normal reticulocyte count and leukopaenia in the former
radiotherapy is a primary modality of tx in retinal, CNS, skin, oesophageal, cervical, vaginal and prostatic tumours; it is adjuvant in all other tumours
the commonest presentations of CMV s/p txp are pneumonia or pulmonary infiltrates
Renal/Biochem
SIADH causing drugs - SIADH Causes Poor Voiding: Sedatives (barbiturates), Indomethacin (NSAIDs), Antidepressants (TCAs/SSRIs), thiazide Diuretics, 1st gen antiHistamines, Cyclophosphamide/antiConvulsants, 1st gen antiPsychotics, Vinca alkaloids
malaria: irreversible nephrosis (esp memb or FSGS) > nephritis
2° syphilis: reversible nephritis > nephrosis
even if the patient doesn't qualify for ACEis/ARBs for HTN, give them first-line anyway if concomitant renal disease
kidney size difference >1 cm is significant
for drugs that will be dialysed out on dialysis days, dose them immediately after dialysis on those days
only urge incontinence is not primarily managed with pelvic floor exercises
Pharm/Toxo
valproate ADRs - VALPROATE: Vomiting, Alopecia/Anorexia, Liver tox, Pancreatitis/PCOS, Redistributed fat (weight gain/lipodystrophy), Oedema, hyperAmmonaemia/Ataxia, Tremor/Thrombocytopaenia, Enzyme inhibitor
opioid withdrawal: methadone is the best single tx and avoids needing to give multiple drugs to cover ssx (eg, clonidine + dextromethorphan + loperamide)
aminoglycosides preferentially affect proximal tubular cells
the classic pattern of symptoms in both cotton workers and workers at factories that process nitrates is that of 'Monday disease'
toxicities for which measuring the blood levels is indicated - SLIME TiPP: Salicylates, Lithium, Iron, Methanol, Ethylene glycol, Theophylline, Paraquat, Paracetamol
amphetamine tox → hyponatraemia due to water retention, worsened by the excessive thirst; hyperkalaemia → rhabdo; hypokalaemia not seen because amphetamines tho sympathetomimetic do not have affinity for the β2 receptor like cocaine does
#100 days of productivity#studyblr#studying#med school#medblr#mine#long post#very long post#don't be mad that i f-#i love that vine so much tbh
18 notes
·
View notes
Text
Gastric Outlet Obstruction as an Aggravation of Peutz- Jeghers Syndrome: Case Report - BJSTR Journal
Gastric Outlet Obstruction as an Aggravation of Peutz- Jeghers Syndrome: Case Report by Marcelo Zamorano* in Biomedical Journal of Scientific & Technical Research
https://biomedres.us/fulltexts/BJSTR.MS.ID.006160.php
The Peutz-Jeghers Syndrome (PJS) is a rare autosomal dominant disease characterized by macules of mucocutaneous pigmentation and hamartomatous intestinal polyps. Some signs of the PJS appear in childhood, usually with abdominal pain. In some cases, patients can develop complications. In this article, we report a case of a patient with PJS that reached the emergency room after presenting a concomitant gastric outlet obstruction (GOO). The patient underwent through an endoscopic polypectomy, followed by a laparotomy and an intraoperative enteroscopy. The symptoms were controlled and the extraction of hamartomatous intestinal polyps were achieved, culminating with an intestinal segment resection with muscle atrophy and posterior gastrojejunostomy. There is evidence of PJS cases related to other conditions that developed abnormal scenarios such as biliary obstruction or cecal appendix polyps. However, the association between PJS and GOO and a concomitant delimited intestinal aperistalsis has not been reported. Thus, this case report shows the possible association between the PJS and GOO, whose cause is the intraluminal occupation of the duodenum by polyps and the synergy of the symptoms given by the atrophy of the jejunum muscle.
For more articles on Journals on Biomedical Science please click here
bjstr
Follow on Twitter : https://twitter.com/Biomedres01
Follow on Blogger :https://biomedres01.blogspot.com/
Like Our Pins On : https://www.pinterest.com/biomedres/
#Journals on Medical Drug and Therapeutics#Medical Humanities#Behavioral Medicine Journals#Journals on Emergency Medicine#Nano Medicine
0 notes
Text
Periodontics
This department specializes in the care and prevention of gum related diseases. In common terms the department for the deep cleaning of teeth and gums
Deep scaling
This deep cleaning has two parts. Scaling is when your dentist removes all the plaque and tartar (hardened plaque) above and below the gumline, making sure to clean all the way down to the bottom of the pocket.
Crown Lengthening
During the dental crown lengthening procedure, excess gum and bone tissue is reshaped to expose more of the natural tooth. This can be done to one tooth, to even your gum line, or to several teeth to expose a natural, broad smile.
Operculectomy
is the removal of the flap of gum overlying a tooth.
Frenectomy
A frenectomy is a surgical procedure typically performed under local anesthetic that removes or loosens a band of muscle tissue that is connected to the lip, cheek or floor of the mouth. There are two types of frena; the lingual frenum and the labial frenum.
Gingivectomy
A gingivectomy is necessary when the gums have pulled away from the teeth creating deep pockets. The pockets make it hard to clean away plaque and calculus. Gingivectomy is usually done before gum disease has damaged the bone supporting the teeth.
Flap surgery
Gingival flap surgery is a procedure in which the gums are separated from the teeth and folded back temporarily to allow a dentist to reach the root of the tooth and the bone.
LANAP
Laser-assisted new attachment procedure (LANAP) is a surgical therapy for the treatment of periodontitis, intended to work through regeneration rather than resection.
Augmentation
A dental implant is an artificial tooth root that is placed into your jaw to hold a replacement tooth or bridge
Oral pigmentation
is a relatively common condition that may involve any portion of the oral cavity. Multiple causes are known, and they may range from simple iatrogenic mechanisms, such as implantation of dental amalgam, to complex medical disorders, such as Peutz-Jeghers syndrome.
Depigmentation
It iis the lightening of the skin or loss of pigment. ... The pigment loss can be partial (injury to the skin) or complete (caused by vitiligo). It can be temporary (from tinea versicolor) or permanent (from albinism).
De sensitization
There is nothing worse than being unable to enjoy the foods and drinks you love. Whether it is sipping on something hot or eating something cold, tooth sensitivity can impact your quality of life. Instead of avoiding the foods you really want to eat, you could benefit from tooth desensitization.

0 notes
Text
Genetic Counseling and Testing for Colorectal Cancer in Young Adults: Mini-Review by Ethem Unal in PRJFGS - Lupinepublishers

Colorectal cancer (CRC) has one of the largest proportions of familial cases. Two to 5% of all colon cancers arise in the setting of inherited syndromes, including Lynch syndrome (hereditary nonpolyposis colorectal cancer [HNPCC]), familial adenomatous polyposis (FAP), attenuated FAP, MUTYH-associated polyposis (MAP), and certain hamartomatous polyposis conditions like Peutz-Jeghers syndrome (PJS) and juvenile polyposis syndrome (JPS). All of these conditions are inherited, autosomal dominant disorders, except MAP, which is autosomal recessive [l]. Although clinical similarities do exist, each has different cancer risks, characteristic clinical features, and separate genetical etiologies. In addition to these syndromes, up to 30 % of colon cancers exhibit increased familial risk, likely related to inheritance. A number of less penetrant, but possibly more frequent susceptibility genes have been identified for this level of inheritance. Determination of predisposing genes allows for accurate risk assessment and more precise screening approaches. Examples include common polymorphisms in genes that regulate metabolism or genes that are regulated by environmental or other genetic factors.
https://www.lupinepublishers.com/forensic-and-genetics-journal/fulltext/PRJFGS.MS.ID.000109.php
#forensic#genetic sciences#lupine publishers#open access journals#genetic factors#autosomal disorders#genes#polymorphism#predisposing genes#familiar cases
2 notes
·
View notes
Text
Medical Conditions For Black Gum
Certain medical conditions can cause oral changes, including black gums. Only a medical professional can diagnose these conditions through appropriate testing.
Acute Necrotizing Ulcerative Gingivitis, a severe gum infection, can cause gums to turn black or grey.
Addison’s Disease is a disorder that affects adrenal glands and can cause dark spots on the gums and lips.
Oral Cancer can alter the color of your gums, though it generally appears as a black spot rather than overall discoloration.
Peutz-Jeghers Syndrome, a genetic condition, appears as dark blue or brown freckles that usually appear during childhood. The freckles generally fade over time, but people with Peutz-Jeghers could be at greater risk for developing cancer.
Are you asking yourself why are my gums dark? Know the reason for gums getting black by booking an appointment with the best Manhattan Beach dentists and get outstanding treatment for all your dental issues.
0 notes