#polyposis syndromes
Text
Duodenal polyp a rare cause of repeated vomiting by Lahfidi Amal in Journal of Clinical and Medical Images, Case Reports

Clinical Image Description
A 50-year-old man without ATCD who suffers from dyspepsia and frequent vomiting, prompting him to seek medical help. There were no abnormalities found during the clinical evaluation. A CT scan of the abdomen was ordered to identify a duodenal polyp that was limiting the digestive light (Figure 1).
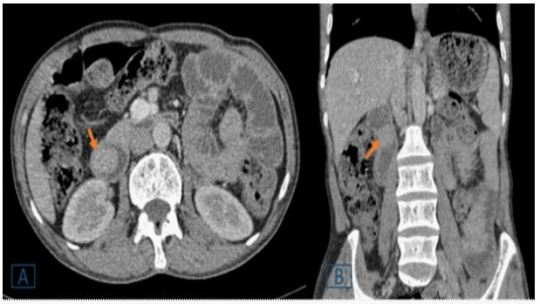
Figure 1: A duodenal endoluminal polyploid tissue process of 21 x 23 mm is shown on a transverse (A) and coronal (B) abdominal CT following contrast injection (orange arrow).
Peutz-Jeghers syndrome (PJS), juvenile polyposis, Cowden's disease, familial adenomatous polyposis, and Gardner's syndrome are polyposis syndromes that affect the duodenum [1]. Duodenal polyps are more common in children with polyposis syndromes, the majority of which are asymptomatic, according to a retrospective research in a pediatric population (aged 21 years) [2]. In the pediatric age group, duodenal polyps are seldom seen during standard high endoscopy (EGD) and radiographic investigations. In contrast, a recent study of adults using EGD and autopsy found a prevalence of up to 4.6 % [2]. Abdominal pain, vomiting, gastrointestinal bleeding, anemia, and intussusception or obstruction are among the symptoms [1, 2]. In comparison to the jejunum and ileum, duodenal disorders have received little attention in the imaging literature [1]. The exploration of the duodenum, which is still mostly examined by video endoscopy, has changed dramatically as a result of recent breakthroughs in imaging. However, advances in computed tomography (CT) and magnetic resonance imaging (MR) have made it easier to detect and characterize anomalies in the genesis of duodenal masses [1]. They are used to assess intraluminal content, the duodenum wall, and the extraduodenal area. The scanner, in combination with optimum intestinal distension and intravenous iodine contrast, provides for a thorough examination of the duodenum. Similarly, MRI has been demonstrated to be useful in diagnosing a wide spectrum of duodenal disorders when combined with duodenal distension and intravenous administration of a gadolinium-based contrast agent [1]. For the detection and characterization of a wide spectrum of duodenal lesions generating masses, CT remains the preferred imaging modality [1]. Large polyps (> 15 mm) might cause small intestinal blockage, thus it's important to keep an eye on them to see which ones need to be removed [1]. Protocols for monitoring are still being debated. Important polyps (big polyps with a proclivity for intussusception or blockage) are detected by endoscopy [1].
Surveillance in patients with polyposis syndromes was the most common reason for EGD; most of these patients were asymptomatic at the time of their EGD. In patients without polyposis syndrome, the most prevalent reason for EGD was stomach pain and vomiting [2]. CT and MRI can theoretically be used to monitor patients with many polyps and determine the best treatment, which could include endoscopic, enteroscopic, or surgical ablation, or a combination of these methods [1].
Competing Interests: The authors declare that they have no links of interest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#ATCD#frequent vomiting#dyspepsia#abnormalities#Peutz-Jeghers syndrome#polyposis syndromes#gastrointestinal#EGD#Lahfidi Amal#JCMICR
0 notes
Text
A huge, huge thank you to One Cancer Place for the monetary contribution for my rare disease chapter in the upcoming Positively Rare book to raise awareness and funds for rare disease! 🥰♥️
I’m about $800 away now from finishing my fundraising for my chapter! If you’d like to contribute towards my chapter, you can at
https://gofund.me/789579da
And as always, all help is greatly appreciated! 🫶
#medical#chronic illness#rare disease#familial adenomatous polyposis#familial polyposis#no colon#mental health#short gut syndrome#short bowel syndrome#author#book#crowdfunding#awareness#advocacy
6 notes
·
View notes
Text

The common types of hereditary cancer syndromes include:
1. Inherited Breast and Ovarian Cancer Syndrome (HBOC): HBOC primarily stems from mutations within the BRCA1 and BRCA2 genes. Females carrying these genetic alterations face notably heightened risks of breast and ovarian malignancies. Furthermore, BRCA mutations correlate with elevated susceptibilities to other cancers, such as prostate, pancreatic, and male breast cancer.
2. Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer, HNPCC): Lynch syndrome arises from mutations affecting genes responsible for DNA mismatch repair, notably MLH1, MSH2, MSH6, and PMS2. Those with Lynch syndrome exhibit increased predispositions to colorectal cancer, alongside risks of endometrial, ovarian, gastric, and urinary tract cancers.
3. Familial Adenomatous Polyposis (FAP): FAP manifests with the proliferation of numerous polyps within the colon and rectum, which pose a cancer risk if untreated. Primarily linked to mutations in the APC gene, FAP substantially heightens the likelihood of early-onset colorectal cancer.
4. Li-Fraumeni Syndrome (LFS): LFS, a rare hereditary cancer syndrome, arises from mutations in the TP53 tumor suppressor gene. Individuals with LFS confront elevated lifetime risks of various cancers, including breast cancer, sarcomas, brain tumors, and adrenal gland tumors, often occurring at a young age.
5. Hereditary Diffuse Gastric Cancer (HDGC): HDGC entails an escalated susceptibility to diffuse gastric cancer, characterized by infiltration of the stomach wall. This predisposition predominantly results from mutations in the CDH1 gene, which encodes a protein crucial for cell adhesion.
6. Cowden Syndrome (CS): CS stems from mutations in the PTEN gene and is typified by multiple noncancerous hamartomas, alongside heightened risks of developing diverse cancers, such as breast, thyroid, and endometrial cancers.
7. Hereditary Retinoblastoma (RB1): Hereditary retinoblastoma arises from mutations in the RB1 gene, leading to the formation of cancerous tumors in the retina, typically emerging in early childhood.
8. Von Hippel-Lindau Syndrome (VHL): VHL arises from mutations in the VHL gene and is characterized by the development of tumors and cysts in various organs, including the kidneys, adrenal glands, pancreas, and central nervous system.
If you have a family history of cancer, you should undergo regular cancer screenings for the early detection and management of cancer. You can undergo a regular full body health checkup at Jaslok Hospital Mumbai, which is one of the best hospitals in Mumbai for cancer screening and treatment.
#cancer#hereditary cancer#hereditary cancer syndrome#Lynch syndrome#inherited breast and ovarian cancer syndrome#familial adenomatous polyposis#full body health checkup#regular health checkups#cancer screening#health checkup packages
0 notes
Text

What is Colorectal Cancer?
Colorectal cancer is a neoplastic disease of the large intestine from Ileo-cecal junction till the rectum. Unregulated growth of their cell lining lead to polyps and cancers.
The exact cause of colorectal cancer is not known, but several factors can increase risk of developing colorectal cancer.
Age: Elderly people are at risk of colorectal cancer. It is most common in people over 50 years of age.
Family history: People with history of colorectal cancer in family (first degree relatives) are at increased risk.
Genetic factors: They are associated with some hereditary syndromes like lynch syndrome, familial Adenomatous polyposis, etc.
Lifestyle factors: A diet rich in red and processed meats and low in fibres or lacking fruits and vegetables can increase risk of colon cancer. Obesity, reduced physical activity, alcohol consumption or smoking also increase risk of colorectal cancer.
Medical Conditions: Certain medical conditions like inflammatory bowel disease (Crohn’s disease and ulcerative colitis) can increase the risk of colorectal cancer.
It is important to note that having one or more risk factors does not mean that a person will develop cancer. Regular screening tests such as stool occult blood and colonoscopy, can help to detect as well as prevent it at the early stage.
#Colorectal cancer#colon cancer#colorectal cancer#bowel cancer#sigmoid colon#rectal cancer#colorectal#stage 4 colon cancer#colon cancer treatment#adenocarcinoma colon#stage 4 bowel cancer#malignant neoplasm of colon#colon health#colorectal cancer treatment#bowel cancer treatment#the colon#colorectal carcinoma#rectal cancer treatment#rectal adenocarcinoma#sigmoid cancer#large intestine cancer#colonic neoplasm#rectal tumor#colon tumor#carcinoma colon#colorectal adenocarcinoma#large colon#cancer intestinal#colon rectum#sigmoid colon cancer
4 notes
·
View notes
Text
Genetic mutations: Inherited gene mutations, like Lynch syndrome or familial adenomatous polyposis (FAP), can increase colon cancer risk.
Age: Most cases occur in people over 50.
Diet: A diet high in red or processed meats and low in fruits and vegetables may raise the risk.
Family history: Having close relatives with colon cancer increases the likelihood.
Lifestyle factors: Lack of physical activity, smoking, and heavy alcohol use can contribute to colon cancer.
Inflammatory bowel disease: Conditions like Crohn’s disease or ulcerative colitis can raise the risk of colon cancer over time.
Obesity: Excess body weight is linked to a higher chance of developing colon cancer.
#Colon Cancer Surgery in India#Low Cost of Colon Cancer Treatment India#Top Oncologist For Colon Cancer India#Top Colon Cancer Treatment Hospital of India#Top Surgeons for Colon Cancer Treatment India#Affordable Cost of Colon Cancer Treatment India
1 note
·
View note
Text
What Diseases Can Be Detected by a Colonoscopy?
When it comes to maintaining digestive health, a colonoscopy is one of the most crucial diagnostic tools available. This procedure, which involves the examination of the colon and rectum using a flexible tube with a camera, can detect a range of diseases and conditions that might otherwise go unnoticed. Whether you're seeking the best colonoscopy centre in Ghaziabad & Delhi or the best gastroenterologist in Ghaziabad & Delhi, understanding what a colonoscopy can reveal is vital for making informed health decisions.

Diseases and Conditions Detected by a Colonoscopy:
Colorectal Cancer:
Early Detection: Colonoscopy is renowned for its ability to detect colorectal cancer early, often before symptoms appear. By identifying precancerous polyps or tumors at an early stage, colonoscopy can significantly improve the chances of successful treatment and recovery.
Polyps:
Types of Polyps: Colon polyps are growths on the inner lining of the colon. While some polyps are benign, others can develop into cancer over time. Colonoscopy helps in identifying different types of polyps, including adenomatous polyps, which are more likely to become cancerous.
Inflammatory Bowel Disease (IBD):
Conditions Included: This includes Crohn’s disease and ulcerative colitis. Colonoscopy can reveal inflammation, ulcers, and other signs of these chronic conditions, helping to guide treatment and management strategies.
Diverticulosis and Diverticulitis:
Understanding the Conditions: Diverticulosis is characterized by small pouches that can form in the colon wall, while diverticulitis occurs when these pouches become inflamed or infected. Colonoscopy can diagnose these conditions and help determine the appropriate treatment.
Irritable Bowel Syndrome (IBS):
Diagnostic Role: While IBS is typically diagnosed based on symptoms, colonoscopy can help rule out other conditions with similar symptoms, ensuring a correct diagnosis.
Rectal Bleeding:
Investigation of Symptoms: Rectal bleeding can be caused by a range of issues, from hemorrhoids to more serious conditions like cancer. A colonoscopy provides a direct view of the colon to pinpoint the cause of bleeding.
Colonic Obstruction:
Detecting Blockages: Colonoscopy can help identify the presence and cause of blockages in the colon, which might be due to tumors, scar tissue, or other obstructions.
Familial Conditions:
Genetic Testing and Screening: For individuals with a family history of colon cancer or hereditary conditions like Familial Adenomatous Polyposis (FAP), colonoscopy plays a crucial role in early detection and preventive care.
Choosing the Right Centre and Specialist:
For accurate diagnosis and effective treatment, selecting the right medical centre and specialist is essential. If you're looking for the best colonoscopy centre in Ghaziabad, it's important to consider factors like the centre’s reputation, the technology used, and patient reviews. A well-regarded centre will offer state-of-the-art equipment and a comfortable environment, enhancing the overall experience.
Similarly, consulting with the best gastroenterologist in Delhi can make a significant difference. A top gastroenterologist will not only provide expert care but also offer valuable advice on managing and preventing gastrointestinal diseases. They will ensure that the colonoscopy is performed with precision and that any findings are communicated clearly with appropriate follow-up recommendations.
Conclusion:
A colonoscopy is a powerful diagnostic tool that can detect a variety of diseases and conditions, from colorectal cancer to inflammatory bowel disease. By choosing the best colonoscopy centre in Ghaziabad and consulting with the best gastroenterologist in Ghaziabad & Delhi, you ensure that you receive the highest standard of care. Regular screenings and timely diagnoses can make a significant difference in managing digestive health and preventing serious conditions.
#Best Gastroenterologist in Noida Extension#Best Endoscopy Clinic in Ghaziabad#Best Endoscopy Centre in Ghaziabad#Best Endoscopy Centre in Indirapuram#Best Colonoscopy Centre in Indirapuram#Best Colonoscopy Centre in Ghaziabad#Best Endoscopy Centre in Noida#Best Endoscopy Centre in Delhi#Best Colonoscopy Centre in Noida#Best Colonoscopy Centre in Delhi
0 notes
Text
What Types of Medical Procedures Are Used to Treat Rectal Cancer?
Rectal Cancer is a malignancy that originates in the cells of the rectum, which is the final segment of the large intestine, connecting the colon to the anus. It typically develops slowly over time, starting as small growths called polyps on the inner lining of the rectum. While not all polyps become cancerous, some may progress into cancer if left untreated.

CAUSES AND RISK FACTORS:
Several factors may contribute to the development of Rectal Cancer. These include:
Age: The risk of Rectal Cancer increases with age, with the majority of cases diagnosed in individuals over 50 years old.
Family history: A family history of colorectal cancer or certain hereditary conditions, such as familial adenomatous polyposis (FAP) or Lynch syndrome, can elevate the risk.
Dietary Factors: Consuming a diet high in red and processed meats, and low in fiber, fruits, and vegetables may increase the risk of Rectal Cancer.
Lifestyle Choices: Factors like smoking, excessive alcohol consumption, and a sedentary lifestyle have been linked to an increased risk of Colorectal Cancer.
Inflammatory Bowel Disease (IBD): Chronic conditions like ulcerative colitis or Crohn’s disease affecting the colon and rectum may raise the risk of developing Rectal Cancer over time.
SYMPTOMS
The symptoms of Rectal Cancer can vary depending on the stage and location of the tumor. Common signs and symptoms include:
Persistent changes in bowel habits, such as diarrhea or constipation
Rectal bleeding / the presence of blood in the stool.
Abdominal discomfort or pain, including cramps or bloating
Unexplained weight loss
Fatigue or weakness
A feeling of incomplete bowel emptying
Rectal pain or discomfort
Iron Deficiency Anemia resulting from blood loss.
HOW TO TREAT IT?
SURGERY
Surgery is often the primary treatment for Rectal Cancer, particularly in early-stage disease. The goal of surgery is to remove the Tumour and any surrounding tissue affected by cancer while preserving bowel function and quality of life. Several surgical procedures may be employed, depending on the stage and location of the cancer:
Local Excision: This minimally invasive procedure is suitable for small, early-stage Tumours confined to the inner layers of the rectal wall. It involves the removal of the Tumour and a small margin of surrounding tissue through the rectum.
Low Anterior Resection (LAR): LAR is performed for Tumours located in the upper part of the rectum. It involves removing the affected portion of the rectum and reconnecting the remaining healthy bowel to the anus.
Abdominoperineal Resection (APR): APR is reserved for Tumours located in the lower part of the rectum or close to the anus. It involves the removal of the entire rectum, anus, and surrounding tissue, with the creation of a permanent colostomy.
Total Mesorectal Excision (TME): TME is a meticulous surgical technique used to remove the rectum and surrounding lymph nodes while preserving the integrity of the Mesorectal tissue. The goal is to lower the chances of cancer returning and enhance long-term results.
CHEMOTHERAPY:
Chemotherapy utilizes potent medications to eliminate or slow the growth of cancer cells. It may be recommended before or after surgery, depending on the stage and aggressiveness of the cancer. Neoadjuvant chemotherapy is administered before surgery to shrink the Tumour and make it more manageable for surgical removal. Adjuvant chemotherapy is given after surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
RADIATION THERAPY:
Radiation therapy uses high-energy beams to target and destroy cancer cells. It may be used alone or in combination with chemotherapy (Chemo radiation) to shrink Tumours before surgery, reduce the risk of local recurrence, or treat metastatic disease. Radiation therapy can also be employed as palliative treatment to alleviate symptoms and improve quality of life in advanced cases.
TARGETED THERAPY:
Targeted therapy drugs are designed to interfere with specific molecules involved in cancer growth and progression. In Rectal Cancer treatment, targeted therapy may involve medications that target the vascular endothelial growth factor (VEGF) or epidermal growth factor receptor (EGFR), among others. These drugs can be used in combination with other treatments to improve outcomes, particularly in advanced or metastatic disease.
IMMUNOTHERAPY:
Immunotherapy utilizes the immune system’s capabilities to identify and eradicate cancer cells. While still relatively new in the realm of Rectal Cancer treatment, immunotherapy shows promise in certain cases, particularly for cancers that express specific biomarkers such as microsatellite instability-high (MSI-H) or deficient mismatch repair (DMMR). Immunotherapy drugs may be used alone or in combination with other treatments to enhance the body’s immune response against cancer cells.
CONCLUSION
Rectal Cancer is a significant health concern worldwide, but advancements in early detection and treatment have improved survival rates and quality of life for many patients. Awareness of risk factors, regular screening, and prompt medical evaluation of symptoms are essential for the timely diagnosis and management of Rectal Cancer. At our Oncology department, with a multidisciplinary approach involving surgery, chemotherapy, and radiation therapy, along with ongoing research into immunotherapies, there is hope for continued progress in the fight against Rectal Cancer.
To learn more about our services and treatments, Schedule an appointment today or call 0491 251 5717.
#Oncology department#radiation therapy#rectal cancer#cancer#hospital#private hospitals#multispecialty hospitals
0 notes
Text
NAILS IN HEALTH AND DISEASE.
The nails are present at the end of each finger tip on the dorsal surface.The main function of nail is protection and it also helps for a firm grip for holding articles.It consists of a strong relatively flexible keratinous nail plate originating from the nail matrix. Under the nail plate there is a soft tissue called nail bed.Between the skin and nail plate there is a nail fold or cuticle.Normal healthy nail is slight pink in colour and the surface is convex from side to side.Finger nails grow 1 cm in three months and toe nails take 24 months for the same.
Importance of nails in disease diagnosis:
The colour ,appearance,shape and nature of the nails give some information about the general health and hygiene of a person . Nails are examined as a routine by all doctors to get some clues about underlying diseases.Just looking at nails we can makeout the hygiene of a person.The abnormal nail may be congenital or due to some diseases.The cause for changes in the nail extend from simple reasons to life threatening diseases.Hence the examination by a doctor is essential for diagnosis .Some abnormal findings with probable causes are discussed here for general awareness.
1) Hygiene:-
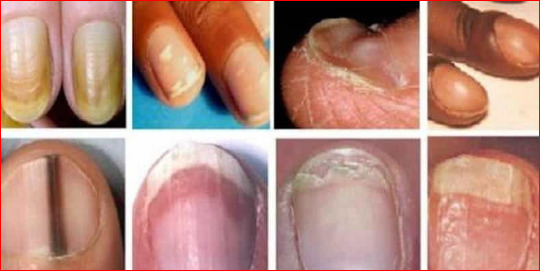
2) Colour of the nails:-
a) Nails become pale in anaemia.
b) Opaque white discolouration(leuconychia) is seen in chronic renal failure and nephrotic syndrome.
c) Whitening is also seen in hypoalbuminaemia as in cirrhosis and kidney disorders.
d) Drugs like sulpha group,anti malarial and antibiotics ect can produce discolouration in the nails.
e) Fungal infection causes black discolouration.
f) In pseudomonas infection nails become black or green.
g) Nail bed infarction occures in vasculitis especially in SLE and polyarteritis.
h) Red dots are seen in nails due to splinter haemorrhages in subacute bacterial endo carditis, rheumatoid arthritis, trauma, collagen vascular diseases.
i) Blunt injury produces haemorrhage and causes blue/black discolouration.
j) Nails become brown in kidney diseases and in decreased adrenal activity.
k) In wilsons disease blue colour in semicircle appears in the nail.
l) When the blood supply decreases nail become yellow .In jaundice and psoriasis also nail become yellowish.
m) In yellow nail syndrome all nails become yellowish with pleural effusion.
3) Shape of nails:-
a) Clubbing: Here tissues at the base of nails are thickened and the angle between the nail base and the skin is obliterated. The nail becomes more convex and the finger tip becomes bulbous and looks like an end of a drumstick. When the condition becomes worse the nail looks like a parrot beak.
Causes of clubbing:-
Congenital Injuries
Severe chronic cyanosis
Lung diseases like empyema,bronchiactesis,carcinoma of bronchus and pulmonary tuberculosis.
Abdominal diseases like crohn’s disease,polyposis of colon,ulcerative colitis,liver cirrhosis ect…
Heart diseases like fallot’s tetralogy,subacute bacterial endocarditis and ect..
b) Koilonychia:-
Here the nails become concave like a spoon.This condition is seen in iron deficiency anaemia.In this condition the nails become thin,soft and brittle.The normal convexity will be replaced by concavity.
c) Longitudinal ridging is seen in raynaud’s disease.
d) Cuticle becomes ragged in dermatomyositis.
e) Nail fold telangiectasia is a sign in dermatomyositis ,systemic sclerosis and SLE.
4) Structure and consistancy:-
a) Fungal infection of nail causes discolouration,deformity,hypertrophy and abnormal brittleness.
b) Thimble pitting of nail is charecteristic of psoriasis ,acute eczema and alopecia aereata.
c) The inflamation of cuticle or nail fold is called paronychia.
d) Onycholysis is the seperation of nail bed seen in psoriasis,infection and after taking tetracyclines.
e) Destruction of nail is seen in lichen planus,epidermolysis bullosa.
f) Missing nail is seen in nail patella syndrome.It is a hereditary disease.
g) Nails become brittle in raynauds disease and gangrene.
h) Falling of nail is seen in fungal infection,psoriasis and thyroid diseases.
5) Growth:-
Reduction in blood supply affects the growth of nails. Nail growth is also affected in severe ilness. when the disease disappears the growth starts again resulting in formation of transverse ridges.These lines are called Beau’s lines and are healpful to date the onset of illness.
The Importance of Learning How to Earn Money from Famous Tutorials
0 notes
Text
Understanding the Risk Factors for Secondary Cancers
Secondary cancers, also known as second primary cancers or metachronous cancers, are new, unrelated cancers that develop in individuals who have previously been diagnosed with cancer. While surviving cancer is a significant achievement, it's essential to be aware of the risk factors for secondary cancers. Let's explore what these risk factors are and how individuals can take steps to reduce their risk.
What Are Secondary Cancers?
Secondary cancers occur when new cancerous cells develop in tissues or organs unrelated to the original cancer diagnosis. These cancers are not recurrences or metastases of the original cancer but are entirely new primary cancers. For example, a person who has been successfully treated for breast cancer may develop a secondary cancer, such as lung cancer, years later.
Risk Factors for Secondary Cancers:
Previous Cancer Treatment: Certain cancer treatments, such as radiation therapy and chemotherapy, can increase the risk of developing secondary cancers. Radiation therapy exposes healthy cells to ionizing radiation, which can damage DNA and increase the likelihood of mutations that lead to cancer. Similarly, some chemotherapy drugs can cause DNA damage and increase the risk of secondary cancers.
Genetic Predisposition: Individuals with certain genetic conditions, such as Li-Fraumeni syndrome, hereditary retinoblastoma, and familial adenomatous polyposis, have an increased risk of developing multiple cancers over their lifetime. These genetic conditions can predispose individuals to the development of primary and secondary cancers.
Environmental and Lifestyle Factors: Environmental factors, such as exposure to carcinogens like tobacco smoke, asbestos, and ultraviolet radiation from the sun, can increase the risk of developing cancer. Lifestyle factors, including smoking, excessive alcohol consumption, poor diet, and lack of physical activity, can also contribute to the development of secondary cancers.
Age: The risk of developing secondary cancers tends to increase with age. As individuals live longer, they may be exposed to additional risk factors and accumulate genetic mutations that increase the likelihood of developing cancer.
Hormonal Factors: Hormonal factors, such as hormone replacement therapy (HRT) and oral contraceptive use, can influence the risk of developing certain types of secondary cancers. For example, long-term use of estrogen-only HRT has been associated with an increased risk of developing endometrial cancer.
Immune Suppression: Individuals with weakened immune systems, such as organ transplant recipients and those living with HIV/AIDS, are at an increased risk of developing secondary cancers. A compromised immune system may be less effective at detecting and eliminating cancerous cells, allowing them to proliferate and form new tumors.
Prevention and Management:
While some risk factors for secondary cancers cannot be modified, there are steps individuals can take to reduce their risk:
Follow-up Care: Regular follow-up care with healthcare providers is essential for cancer survivors. This includes routine screenings, physical examinations, and laboratory tests to detect any signs of recurrence or new cancers early.
Healthy Lifestyle Choices: Adopting a healthy lifestyle can help reduce the risk of developing secondary cancers. This includes maintaining a balanced diet rich in fruits, vegetables, and whole grains, engaging in regular physical activity, avoiding tobacco products, limiting alcohol consumption, and protecting the skin from sun exposure.
Genetic Counseling and Testing: Individuals with a family history of cancer or known genetic predispositions may benefit from genetic counseling and testing. These services can help identify individuals at increased risk of developing cancer and inform personalized screening and prevention strategies.
Minimize Environmental Exposures: Minimizing exposure to known carcinogens and environmental toxins can help reduce the risk of developing cancer. This includes avoiding tobacco smoke, limiting exposure to ultraviolet radiation from the sun, and following safety precautions in occupational settings with potential chemical exposures.
Conclusion:
While surviving cancer is a significant achievement, cancer survivors need to be aware of the risk factors for secondary cancers. Understanding these risk factors and taking proactive steps to reduce them can help individuals live healthier, longer lives. By following recommended screening guidelines, adopting a healthy lifestyle, and minimizing exposure to known carcinogens, cancer survivors can take control of their health and reduce their risk of developing secondary cancers. If you or someone you know is a cancer survivor, it's essential to discuss any concerns or questions about secondary cancer risk with a healthcare provider. With knowledge, awareness, and proactive management, individuals can minimize their risk and continue to thrive after cancer.
#best oncologist in Hyderabad#best oncologist in Hyderabad India#oncology specialist in Hyderabad#oncologist in Hyderabad#top 10 oncologist in Hyderabad#best cancer doctor in Hyderabad#top oncologist in Hyderabad#best medical oncologist in Hyderabad#best surgical oncologist in Hyderabad#surgical oncologist in Hyderabad#medical oncologist in Hyderabad#best oncology surgeon in Hyderabad#radiation oncologist in Hyderabad#oncology#radiation therapy#cancer hospital#oncology specialist in bangalore#oncology specialist in hyderabad#top oncologist in hyderabad#Oncology Doctors in Hyderabad#Oncology Doctors#Oncologists near me#best oncology doctors in hyderabad#best oncologists in hyderabad#oncologists near me#oncologists near hyderabad#best cancer doctors in hyderabad#cancer doctors near me#best radiation oncologists in hyderabad#radiation oncologists near me
0 notes
Text
Understanding Gastrointestinal Surgeries: Common Procedures and Their Benefits

Gastrointestinal (GI) surgeries are crucial interventions for treating a variety of conditions affecting the digestive tract. These surgeries can range from minimally invasive procedures to complex operations that address severe ailments. As a surgical gastro oncologist in Pune, Dr. Snita Sinukumar specializes in these life-saving procedures. This article aims to provide an in-depth understanding of common gastrointestinal surgeries and their benefits.
Common Gastrointestinal Surgeries
1. Appendectomy
An appendectomy is the surgical removal of the appendix, typically performed to treat appendicitis, an inflammation of the appendix. This is often an emergency procedure to prevent the appendix from rupturing and causing peritonitis, a severe abdominal infection.
Benefits:
Immediate relief from pain and symptoms of appendicitis.
Prevention of life-threatening complications like peritonitis and sepsis.
2. Cholecystectomy
A cholecystectomy is the removal of the gallbladder, commonly performed to treat gallstones and gallbladder disease. This can be done via traditional open surgery or laparoscopically.
Benefits:
Relief from pain and digestive issues caused by gallstones.
Reduced risk of gallbladder cancer and other complications.
3. Colectomy
A colectomy involves the removal of all or part of the colon. This procedure is used to treat various conditions, including colorectal cancer, diverticulitis, and inflammatory bowel disease (IBD).
Benefits:
Effective treatment for colorectal cancer, potentially preventing its spread.
Relief from symptoms of diverticulitis and IBD, improving quality of life.
Reduction in cancer risk for patients with familial adenomatous polyposis (FAP) or Lynch syndrome.
4. Gastrectomy
A gastrectomy is the surgical removal of part or all of the stomach. This procedure is commonly used to treat stomach cancer, severe ulcers, and other stomach disorders.
Benefits:
Effective removal of cancerous tissues, which can be life-saving.
Relief from chronic ulcers and other severe stomach issues.
Improved prognosis for patients with early-stage stomach cancer.
5. Pancreaticoduodenectomy (Whipple Procedure)
The Whipple procedure is a complex surgery used to treat pancreatic cancer, bile duct cancer, and other conditions. It involves the removal of the head of the pancreas, part of the small intestine, the gallbladder, and the bile duct.
Benefits:
Increased survival rates for patients with pancreatic cancer.
Relief from symptoms caused by tumors in the pancreas, bile duct, or duodenum.
Potential for curative treatment in early-stage pancreatic and bile duct cancers.
6. Hemorrhoidectomy
A hemorrhoidectomy is the surgical removal of hemorrhoids, which are swollen veins in the rectum and anus that cause discomfort and bleeding.
Benefits:
Permanent relief from hemorrhoid symptoms.
Improved quality of life and daily comfort.
Advanced Minimally Invasive Techniques
Minimally invasive surgeries, such as laparoscopic and robotic surgeries, have revolutionized the field of gastrointestinal surgery. These techniques involve smaller incisions, which lead to numerous benefits over traditional open surgery.
Benefits:
Reduced Pain and Discomfort: Smaller incisions result in less postoperative pain.
Faster Recovery: Patients typically experience quicker recovery times, allowing them to return to normal activities sooner.
Lower Risk of Infection: Smaller wounds decrease the risk of postoperative infections.
Reduced Scarring: Minimally invasive techniques result in less noticeable scars, which can be cosmetically favorable for patients.
The Role of Gastrointestinal Surgeries in Cancer Treatment
Gastrointestinal surgeries play a critical role in the treatment of various cancers, including colorectal, stomach, pancreatic, and liver cancers. Surgical intervention can be curative, especially when the cancer is detected early.
Colorectal Cancer Surgery
Colorectal cancer surgery often involves removing the cancerous part of the colon or rectum along with surrounding lymph nodes. In some cases, a colostomy may be required.
Benefits:
Potentially curative if the cancer is localized.
Reduction in cancer symptoms and prevention of metastasis.
Stomach Cancer Surgery
For stomach cancer, partial or total gastrectomy is performed. The extent of the surgery depends on the cancer’s location and stage.
Benefits:
Removal of the tumor and affected tissues, which can be life-saving.
Improved chances of long-term survival and quality of life.
Pancreatic Cancer Surgery
The Whipple procedure is the most common surgery for pancreatic cancer, aimed at removing the tumor and preventing the spread of the disease.
Benefits:
Increased survival rates, especially when combined with other treatments like chemotherapy.
Reduction in symptoms caused by the tumor.
Postoperative Care and Recovery
Postoperative care is crucial for the success of gastrointestinal surgeries. Patients typically require a combination of rest, diet modifications, and gradual physical activity to ensure proper healing.
Key Aspects of Postoperative Care:
Pain Management: Effective pain control through medications and other methods.
Nutritional Support: Special diets to promote healing and prevent complications.
Follow-Up Care: Regular check-ups to monitor recovery and detect any complications early.
Conclusion
Gastrointestinal surgeries are vital procedures that address a range of conditions from appendicitis to cancer. With advancements in surgical techniques, particularly minimally invasive methods, patients experience numerous benefits, including reduced pain, faster recovery, and improved outcomes. As a surgical gastro oncologist in Pune, Dr. Snita Sinukumar provides expert care, utilizing these advanced techniques to enhance patient health and quality of life.
For those considering gastrointestinal surgery, understanding these common procedures and their benefits can help in making informed decisions about their health care. Whether it’s for emergency conditions like appendicitis or complex cases like pancreatic cancer, gastrointestinal surgeries offer significant benefits that can lead to life-saving outcomes and improved overall well-being.
#surgical oncologist in pune#women's cancer treatment in pune#oncologist in pune#head and neck cancer treatment in pune#cancer specialist in pune#Surgical Gastro Oncologist in Pune
0 notes
Text
Duodenal polyp a rare cause of repeated vomiting by Lahfidi Ama in Journal of Clinical and Medical Images, Case Reports

Clinical Image Description
A 50-year-old man without ATCD who suffers from dyspepsia and frequent vomiting, prompting him to seek medical help. There were no abnormalities found during the clinical evaluation. A CT scan of the abdomen was ordered to identify a duodenal polyp that was limiting the digestive light (Figure 1).
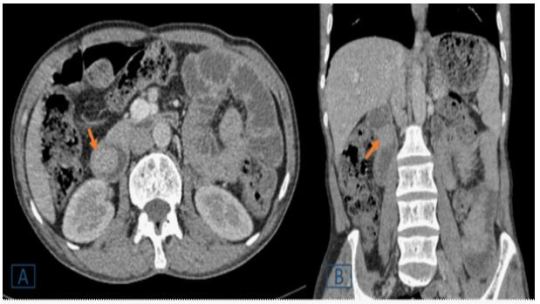
Figure 1: A duodenal endoluminal polyploid tissue process of 21 x 23 mm is shown on a transverse (A) and coronal (B) abdominal CT following contrast injection (orange arrow).
Peutz-Jeghers syndrome (PJS), juvenile polyposis, Cowden's disease, familial adenomatous polyposis, and Gardner's syndrome are polyposis syndromes that affect the duodenum [1]. Duodenal polyps are more common in children with polyposis syndromes, the majority of which are asymptomatic, according to a retrospective research in a pediatric population (aged 21 years) [2]. In the pediatric age group, duodenal polyps are seldom seen during standard high endoscopy (EGD) and radiographic investigations. In contrast, a recent study of adults using EGD and autopsy found a prevalence of up to 4.6 % [2]. Abdominal pain, vomiting, gastrointestinal bleeding, anemia, and intussusception or obstruction are among the symptoms [1, 2]. In comparison to the jejunum and ileum, duodenal disorders have received little attention in the imaging literature [1]. The exploration of the duodenum, which is still mostly examined by video endoscopy, has changed dramatically as a result of recent breakthroughs in imaging. However, advances in computed tomography (CT) and magnetic resonance imaging (MR) have made it easier to detect and characterize anomalies in the genesis of duodenal masses [1]. They are used to assess intraluminal content, the duodenum wall, and the extraduodenal area. The scanner, in combination with optimum intestinal distension and intravenous iodine contrast, provides for a thorough examination of the duodenum. Similarly, MRI has been demonstrated to be useful in diagnosing a wide spectrum of duodenal disorders when combined with duodenal distension and intravenous administration of a gadolinium-based contrast agent [1]. For the detection and characterization of a wide spectrum of duodenal lesions generating masses, CT remains the preferred imaging modality [1]. Large polyps (> 15 mm) might cause small intestinal blockage, thus it's important to keep an eye on them to see which ones need to be removed [1]. Protocols for monitoring are still being debated. Important polyps (big polyps with a proclivity for intussusception or blockage) are detected by endoscopy [1].
Surveillance in patients with polyposis syndromes was the most common reason for EGD; most of these patients were asymptomatic at the time of their EGD. In patients without polyposis syndrome, the most prevalent reason for EGD was stomach pain and vomiting [2]. CT and MRI can theoretically be used to monitor patients with many polyps and determine the best treatment, which could include endoscopic, enteroscopic, or surgical ablation, or a combination of these methods [1].
Competing Interests: The authors declare that they have no links of interest.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Peutz-Jeghers syndrome#juvenile polyposis#computed tomography#gastrointestinal bleeding#vomiting#endoscopy#enteroscopic#Lahfidi Ama#JCMICR
0 notes
Text
Check out my latest RareDisease.net article!
#medical#chronic illness#rare disease#familial adenomatous polyposis#familial polyposis#short gut syndrome#short bowel syndrome#disability
2 notes
·
View notes
Text
Is Colon Cancer Hereditary

Colon cancer is a prevalent and potentially fatal disease, so understanding the causes and risk factors is critical. The link between genetics and colon cancer is a major source of anxiety, with many people concerned about their family history and how it affects their vulnerability to the disease.
This article delves into the complex relationship between genetics and colon cancer, addressing the riddles behind its inherited origins.
Several inherited factors influence the development of colon cancer. Inherited illnesses like familial adenomatous polyposis (FAP) and Lynch syndrome raise the likelihood of acquiring this form of cancer. Genetic mutations in genes such as MLH1, MSH2, MSH6, PMS2, EPCAM, MUTYH, and STK11 can all contribute to the development of colon cancer.
Family history is also a major factor in determining colon cancer risk. Individuals with a first-degree relative diagnosed with colon cancer are more likely to develop the disease themselves. However, not all occurrences of colon cancer are hereditary. Nonetheless, individuals with an inherited vulnerability may benefit from earlier and more frequent screening.
0 notes
Text
Continuing Education Activity
Esophagogastroduodenoscopy (EGD) is a diagnostic endoscopic procedure used to visualize the oropharynx, esophagus, stomach, and proximal duodenum.
It is one of the most common procedures for gastroenterologists.
This activity describes the diagnostic and therapeutic capabilities of upper endoscopy and highlights the role of the interprofessional team in looking after patients with pathology of the upper digestive tract.
Objectives :
Identify the indications for esophagogastroduodenoscopy.
Describe the technique for performing upper endoscopy.
Review the complications associated with esophagpgastroduodenoscopy.
Explain interprofessional team strategies for improving care coordination and communication to advance the appropriate and safe use of esophagogastroduodenoscopy to improve patient outcomes.
Introduction
Esophagogastroduodenoscopy (EGD) is a diagnostic endoscopic procedure that includes visualization of the oropharynx, esophagus, stomach, and proximal duodenum.
It is one of the most common procedures that a gastroenterologist performs.
Anatomy and Physiology
Esophagus
The esophagus is located posterior to the trachea and begins distal to the cricoid cartilage and ends at the cardiac orifice of the stomach.
It ranges in diameter from 4 to 6 mm and in length from 9 to 10 cm in the term infant to approximately 25 cm in the adult.
The change in the mucosa color from pale- to reddish-pink marks the transition from the esophagus and gastric epithelium (Z line).
Stomach
The stomach is usually located beneath the diaphragm and is approximately 40 cm distal to the incisors in an adult.
The area of the stomach where the esophagus enters is known as gastric cardia.
The portion of the stomach above the junction of the esophagus and stomach is known as fundus. It is visible in a retroflexed endoscopic view.
The majority of the stomach is known as stomach body.
Along the lesser curvature of the stomach is the incisura which divides the gastric body from the antrum. Endoscopically, the transition from the body to the antrum is from rugae to flat mucosa. The pylorus is the muscular opening between the lower end of the stomach and duodenum bulb.
Duodenum
The duodenum extends from the pylorus to the duodenojejunal angle.
The duodenum bulb is an expanded region immediately distal to the pylorus.
The duodenum then forms a C-shaped loop and endoscopically turns posteriorly and to the right for 2.5 cm, then inferiorly for 7.5 to 10 cm (descending portion), then anteriorly and to the left for approximately 2.5 cm, and finally connects to the jejunum at the level of ligament of Treitz.
Indications
Diagnostic
Persistent upper abdominal pain or pain associated with alarming symptoms such as weight loss or anorexia.
Dysphagia, odynophagia or feeding problems.
Intractable or chronic symptoms of GERD.
Unexplained irritability in a child.
Persistent vomiting of unknown etiology or hematemesis.
Iron deficiency anemia with presumed chronic blood loss when clinically an upper gastrointestinal (GI) source is suspected or when colonoscopy is normal.
Chronic diarrhea or malabsorption.
Assessment of acute injury after caustic ingestion.
Surveillance for malignancy in patients with premalignant conditions such as polyposis syndromes, previous caustic ingestion, or Barrett esophagus.
Therapeutic
Foreign body removal.
Dilation or stenting of strictures.
Esophageal variceal ligation.
Upper GI bleeding control.
Placement of feeding or draining tubes.
Management of achalasia (botulinum toxin or balloon dilation).
Contraindications
Absolute Contraindications
Perforated bowel.
Peritonitis.
Toxic megacolon in an unstable patient.
Relative Contraindications
Severe neutropenia.
Coagulopathy.
Severe thrombocytopenia or impaired platelet function.
Increased risk of perforation including connective tissue disorders, recent bowel surgery or bowel obstruction.
Aneurysm of the abdominal and iliac aorta.
Equipment
Gastroscopes
The standard gastroscopes have a diameter of 10 mm with an instrument channel of 2.8 mm. In children weighing less than 10 kg, endoscopes smaller than 6 mm in diameter for routine endoscopy should be used.
A gastroscope with a large operating channel measuring 3.8 to 4.2 mm is useful in severe acute upper GI bleeding.
High-definition gastroscopes with optical zoom should be available to screen for pre-malignant gastric or duodenal lesions.
Accessories
The biopsy forceps (standard and jumbo) are needed for tissue sampling. For retrieval of a foreign body during esophagogastroduodenoscopy (EGD), rat tooth forceps, alligator forceps, retrieval net, polypectomy snare, overtubes of esophageal and gastric lengths, and a foreign body protector hood should be available. Additional equipment may be required if therapeutic procedures are anticipated.
Preparation
Routine endoscopy in children and adults is usually performed in an outpatient setting using parenteral or general anesthesia.
Occasionally, endoscopy is necessary at the hospital bedside or in an operating room.
Diet :
Preparation for elective upper endoscopy procedure involves a period of fasting.
As per American Society for Anesthesiologists (ASA) guidelines, patients should fast a minimum of 2 hours after ingestion of clear liquids and 6 hours after ingestion of light meals.
In emergency situations or in conditions where gastric emptying is impaired, the potential for pulmonary aspiration of gastric contents must be considered to determine (1) level of sedation, (2) whether endotracheal intubation should be considered to protect the airway or (3) whether the procedure should be delayed.
Medications :
Most medications can be continued and are usually taken with a small sip of water before endoscopy, although diabetes medications need to be adjusted due to the period of fasting before the procedure.
American Society for Gastrointestinal Endoscopy (ASGE) guidelines should be followed for decisions regarding the management of anti-thrombotic agents or for the use of antibiotic prophylaxis in at-risk patients before the endoscopy.
Sedation and Monitoring
Sedation is used in most patients not only to minimize discomfort but also to provide amnesia for the procedure.
All patients undergoing upper endoscopy require pre-procedural evaluation to assess their risk for sedation and to manage potential problems related to pre-existing health conditions.
The choice of sedation varies from conscious sedation delivered by the proceduralist or monitored anesthesia care provided by an anesthesiologist, and preferences for one type of sedation over another are largely based on training and available local resources.
For routine upper endoscopy, many endoscopists utilize intravenous sedation using propofol.
For therapeutic endoscopic procedures such as foreign body removal or in patients in whom cooperation is not anticipated, including very young patients, general anesthesia may be required.
ASGE guidelines recommend routine monitoring of vital signs in addition to clinical observation for changes in cardiopulmonary status during all endoscopic procedures performed under sedation.
Informed consent
Patients, parents, or legal guardians should provide informed consents before the Esophagogastroduodenoscopy (EGD) and for the administration of sedation.
Technique or Treatment
Handling the Endoscope
The endoscope is mostly held in the left hand.
The control section of the endoscope should rest comfortably in the palm of the left hand.
The thumb controls up or down movement of the tip of the endoscope using a large wheel.
The index finger and, at times, the middle finger control the suction, air, and water valves.
The right hand is used to advance and withdraw the endoscope and its axial rotation.
The right hand is also used to insert instruments such as biopsy forceps, cytology brushes, needles for injection, hemostatic clips, polypectomy snares, foreign body retrieval instruments, and syringes for irrigation via the biopsy channel.
Esophageal Intubation
For esophagogastroduodenoscopy (EGD), patients are typically placed in left lateral decubitus with neck flexed forward.
A bite block is placed in the mouth before the endoscope is inserted into the oral cavity.
The endoscope is introduced into the mouth and to the base of the tongue under direct visualization.
The tip of the scope is then gently angulated downward until the vocal cords, epiglottis, both piriform sinuses, and cricoarytenoid cartilages are visualized.
The scope is then passed behind and to the right of the arytenoid cartilage towards the upper esophageal sphincter.
The upper esophageal sphincter is passed under direct visualization, often with application of gentle pressure while insufflating air.
Esophagus and Esophagogastric junction
After intubating the esophagus, the scope is advanced down the esophagus lumen while simultaneously examining the mucosa for any inflammation, ulcerations, furrowing, varices, narrowing or strictures.
The location of the esophagogastric junction should be noted.
The squamocolumnar junction, also referred as Z-line, is the area where the squamous epithelial lining of the esophagus (pale pink colored) meets the columnar lining mucosa of the stomach (salmon-colored).
The level of the Z-line should also be noted. If the Z-line is displaced proximal to the gastroesophageal junction, biopsies should be taken to evaluate for Barrett esophagus.
Stomach
The stomach is entered after passing the esophagogastric junction.
Once the stomach is entered, any residual gastric secretions should be suctioned, and air is insufflated to improve visualization.
The endoscope is then advanced while torquing to the right. The endoscope is advanced along the lesser curvature towards the pylorus, but to fill the greater curvature with the endoscope is usually necessary before the cannulation of the pyloric canal.
The pylorus is a small opening with radiating folds around it.
To pass through the pylorus, the endoscope is positioned in front of the pylorus, and a little air and gentle pressure should be applied against the orifice.
Duodenum
After passing through the pylorus, the endoscope enters the duodenum bulb.
The duodenum bulb should be examined on endoscope insertion rather than during withdrawal as passage of the instrument can cause possible mucosal changes.
After all four quadrants of the bulb are inspected the scope is advanced to the posterior aspect of the bulb; here the duodenum turns right sharply and takes downward turn. To pass the superior flexure of the duodenum and enter the second part of the duodenum, the instrument is advanced using the dials and shaft torque, usually down and to the right followed by an upward spin of the dial.
The superior flexure of the duodenum is often passed blindly and examined on the way back.
The lower part of the second portion of the duodenum is reached by straightening the endoscope, in other words, pulling the endoscope slowly backward while maintaining the view of the lumen. This maneuver reduces the loop along the greater curvature of the stomach and, paradoxically, advances the endoscope into the distal duodenum.
The duodenum distal to the bulb has distinctive circular rings called valvulae conniventes.
The ampulla of Vater is found in the second portion of the duodenum and examined while withdrawing the endoscope.
After careful examination of the duodenum, pylorus, and antrum, the endoscope is retroflexed to visualize the gastric cardia and fundus.
The endoscope is then returned to a neutral position.
Once the stomach has been fully inspected, and biopsies, if necessary, are obtained, the endoscope is then withdrawn.
Before leaving the stomach, air should be suctioned.
The esophagus is again examined on withdrawal of the endoscope.
The average duration of a diagnostic EGD is 5 to 10 minutes under optimal sedation conditions.
Tissue sampling is obtained from suspicious lesions during EGD, although many gastroenterologists perform routine biopsies from designated sites, as a clinically significant disease may be present in an apparently normal looking mucosa.
Specimens obtained include biopsies, brushings of mucosal surface, and polypectomy.
Specimens are sent for histological, cytological, or microbiologic analysis based upon the type of the sample and clinical situation.
Complications
Complications following esophagogastroduodenoscopy (EGD) are rare, occurring in less than 2% of patients.
These could be related to sedation, endoscopy, and complications related to diagnostic or therapeutic maneuvers.
The most frequent and serious complications of sedation are cardiopulmonary.
Adverse events from over sedation include hypoxemia, hypoventilation, hypotension, airway obstruction, arrhythmias, and aspiration.
The complications following diagnostic EGD include infection, bleeding, duodenal hematoma, and bowel perforation.
The risk of bleeding following EGD with biopsy is 0.3%. Post mucosal biopsy bleeding can occur as intraluminal hemorrhage or intraluminal hematoma.
A duodenal hematoma is a rare complication of EGD with an unknown incidence and seems to occur more often in children than adults.
Bowel perforation occurs in less than 0.3 % of cases, and infection is rarely reported.
Complications typically are identified in the first 24 hours after the procedure.
Bleeding presents with hematemesis or bloody output from the gastrostomy tube.
Perforation is identified due to fever, tachycardia, abdominal pain or discomfort.
An abdominal x-ray should be done to reveal extra-luminal air.
Conservative therapy with bowel rest and antibiotics is the typical treatment, although some patients might require surgical repair.
Clinical Significance
Esophagogastroduodenoscopy (EGD) has become a key element in the diagnosis and treatment of esophageal, gastric, and small-bowel disorders.
The many accepted indications for EGD include evaluation of dysphagia, GI bleeding, peptic ulcer disease, medically refractory GERD, esophageal strictures, celiac disease, and unexplained diarrhea.
During EGD evaluation, diagnostic biopsies can be performed as well as therapies to achieve hemostasis and dilation for significant strictures.
If properly performed, it is generally a safe and well-tolerated procedure. EGD's availability and use in the pediatric population have increased.
Decisions surrounding the conditions and time for EGD use in children remain more of an art than a science, and additional critical review of this tool's use is needed to maximize results and minimize risk.
Enhancing Healthcare Team Outcomes
In the pediatric population, endoscopy is typically performed by a pediatric endoscopist with the medical knowledge and technical competency specific to perform safe and effective GI procedures in this population.
The American Society for Gastrointestinal Endoscopy (ASGE) published practice modification guidelines to provide guidance regarding performing endoscopy in infants and children.
If it is not possible for a pediatric-trained endoscopist to perform the procedure, an adult-trained endoscopist should perform endoscopic procedures in children in coordination with a pediatrician and pediatric specialists.
During endoscopic procedures, procedural and resuscitative equipment appropriate for pediatric use should be readily available.
If sedation is needed for the procedure, personnel trained specifically in pediatric life support and airway management should also be readily available.
In symptomatic children with known or suspected caustic ingestion, endoscopy should be performed within 24 hours.
It is recommended to perform emergent foreign body removal of esophageal button batteries as well as two or more rare-earth neodymium magnets.
0 notes
Text

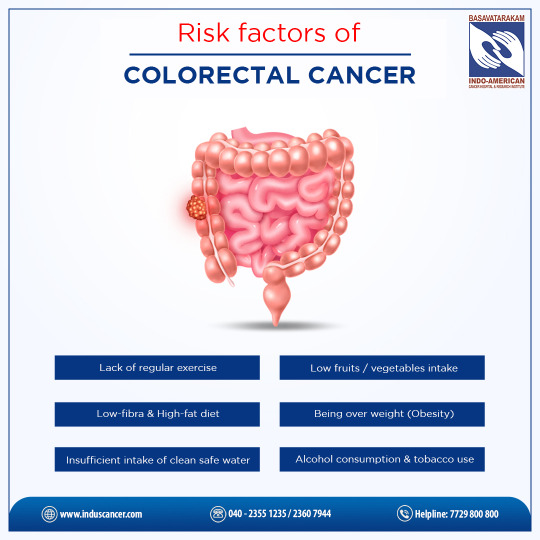
What is Colorectal Cancer?
Colorectal cancer, also known as bowel cancer, occurs in the colon or rectum, forming malignant growths. These growths, called tumors, can invade and damage nearby tissues and spread to other parts of the body.

Age: The risk of colorectal cancer increases with age, with most cases diagnosed in individuals over 50.
Family History: A family history of colorectal cancer or polyps increases the risk, especially if a close relative was diagnosed before age 50.
Personal History: Individuals with a history of colorectal cancer, polyps, or inflammatory bowel disease (such as Crohn's disease or ulcerative colitis) are at higher risk.
Lifestyle Factors: Poor diet (low in fiber, high in red or processed meats), lack of physical activity, obesity, smoking, and heavy alcohol consumption can increase the risk.
Genetics: Some inherited gene mutations, such as Lynch syndrome and familial adenomatous polyposis (FAP), can significantly increase the risk of colorectal cancer.
Race and Ethnicity: African Americans have a higher risk of colorectal cancer than other racial or ethnic groups.
Early detection through regular screenings, such as colonoscopies, can greatly improve treatment outcomes. If you're concerned about your risk or have symptoms, don't hesitate to reach out to our expert team at Basavatarakam Indo American Cancer Hospital.
We're here to support you every step of the way. Stay informed, stay proactive, and together, let's fight colorectal cancer!
#ColorectalCancerAwareness#knowthefacts#earlydetection#BasavatarakamHospital#IndoAmericanCancerHospital#IndoAmericanHospitalHyderabad#BasavatarakamCancerHospital#best cancer treatment in india#best cancer hospital#indo american cancer hospital#best cancer hospitals in india#basavatarakam hospital#indo american hospital#basavatarakam cancer hospital#best cancer specialist in india#basavatarakam#basavatarakamcancerhospital basavatarakam
1 note
·
View note
Text
Can genetics influence the risk of colon cancer?

Absolutely, genetics can play a crucial function in figuring out one's susceptibility to colon cancer. If a near member of the family has had it, the threat increases. Specific gene mutations, like in Lynch syndrome or familial adenomatous polyposis (FAP), heighten the probability. However, genetics isn't the sole component; lifestyle picks be counted too. Regular screenings, retaining a wholesome diet rich in fiber, and guidance clean of tobacco and immoderate alcohol can drastically mitigate those risks. Understanding your family records and adopting a proactive approach, combining genetic factors with a healthful lifestyle, can considerably lower the threat of growing colon cancer. Dr. Mohit Agarwal is the best oncologist in Delhi. He emphasized that a family history of the disorder will increase vulnerability. Regular checkups with an oncologist in Delhi, like Dr. Agarwal, especially for those with genetic predispositions, can hit upon and control risks early. Find the best cancer specialist in Delhi for personalized care near you.
#best cancer specialist in delhi#oncologist in delhi#best oncologist in delhi#best breast cancer treatment#best medical oncologist in delhi#best oncology doctor in delhi#best oncologist in shalimar bagh#best oncologist doctor near me#dr mohit agarwal fortis shalimar bagh#medical oncologist in delhi
0 notes