#Vaginal Discharge - Causes and Prevention
Text
Treatments & Home remedies to treat excess vaginal discharge
Vaginal discharge is a common concern among women, often accompanied by feelings of discomfort and embarrassment. While some amount of discharge is considered normal, excessive or abnormal vaginal discharge can be indicative of an underlying issue. In this comprehensive guide, we will explore the causes of vaginal discharge, available treatment options, and effective home remedies to alleviate…

View On WordPress
#Home remedies for white vaginal discharge in women#Natural Remedies for White Discharge#Treatment of vaginal infections#Vaginal Discharge#Vaginal Discharge - Causes and Prevention#What are the 5 types of discharge?#What foods prevent white discharge?#What is normal vaginal discharge?#What is the best antibiotic for discharge?#Women&039;s Health
0 notes
Text
My dear lgbt+ kids,
Let's talk about vaginal yeast infections. They are super common and nothing to be ashamed of!
What is a yeast infection and what causes it?
Yeast is a type of fungus that naturally lives in multiple parts of your body, like your mouth and vagina. This is not a problem. It's supposed to be there! But it is a careful balancing act - if it becomes too much, you can get a yeast infection.
One of the most common ways this happens is by taking antibiotic medication. They do not only kill the bacteria that cause the infection you are treating, they also kill the "good" bacteria that usually keep the yeast in your vagina in check.
Other things that can throw you off balance are for example:
pregnancy
hormonal birth control
diabetes/uncontrolled blood sugar levels
the use of scented products (tampons, pads, deodorant, soap etc.)
douching (and excessive vaginal hygiene in general)
An untreated infection can be passed on during sex but it is not considered an STI. You can get a yeast infection even if you never had sex!
What are the symptoms?
Yeast infections typically cause itching in the vagina or vulva. You may also notice a thick, white, odorless discharge (comparable to the consistency of cottage cheese), redness, swelling, or a burning sensation (especially when you urinate).
(Yellow or greenish discharge or "fishy" smelling discharge are not typical symptoms of a yeast infection - if you notice those, you may have a bacterial infection instead.)
How can I treat a yeast infection? Do I need to see a doctor?
First things first: Please do not try any "home remedies" you may hear about (like putting yogurt or ice in your vagina) - these things do not help and can even make it worse!
Over-the-counter (OTC) medication is in most cases highly effective and quickly relieves you of uncomfortable symptoms. It's usually for topical use (a cream you use on your vulva, a pill you insert in the vagina, or a combination of both) but oral medication (a pill you swallow) is available as well.
It's essential to carefully read the instructions and take it for as long as you are supposed to (even if your symptoms have already faded or completely stopped!). If you stop taking it too early, the infection may return.
However, it's best to see a doctor if:
You suspect it may be a bacterial infection (see above). This requires a different treatment; taking antifungal OTC medication would be useless for a bacterial infection!
You are not sure if you really have a yeast infection
You tried OTC medication and the symptoms didn't go away (or even got worse)
You get more than four yeast infections within twelve months
You are pregnant (not all OTC medications are safe during pregnancy)
You don't need to be embarrassed or worry that your doctor will assume it's caused by a lack of hygiene. They know better. Seeing patients with yeast infections is routine for them - it's one of the most common reasons people go to their gynecologist!
Can I prevent yeast infections?
Some risk factors are out of your control but you can:
wash your vulva with plain warm water (instead of using soap, cleanser etc.)
avoid douching or "washing out" your vagina (you don't need to clean your vagina at all! It's self-cleaning)
avoid using deodorant on your vulva
avoid using scented tampons or pads
With all my love,
Your Tumblr Dad
584 notes
·
View notes
Text
Let's take a quick look at some of the body parts that women need to be acquainted with.
Here's a detailed illustration, lest you think the female reproductive system is some damn easy bake oven. But we're starting with the basics!
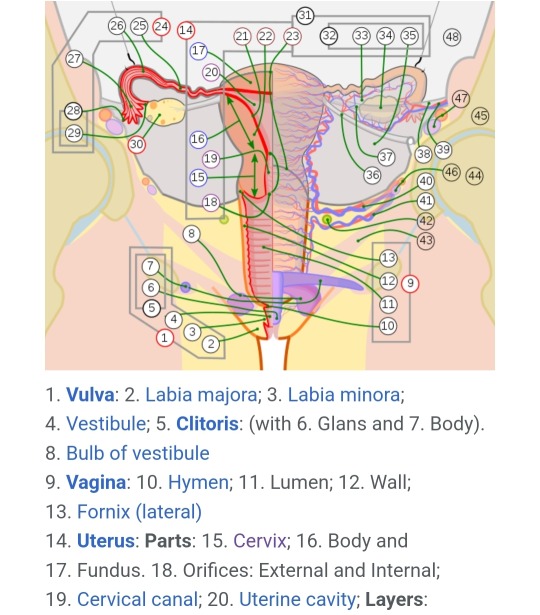
Bartholin's Glands: These are located on either side of the vaginal canal and emit mucus that ranges from almost watery to thick and gooey depending on the need. This mucus combines with the plasma produced by the vaginal walls during arousal. The mucus from the Bartholin's gland is acidic, ranging from 3.8-4.5 on the pH scale (7.0 is neutral).
Cervix: The cervix functions as a gate between the vagina and uterus. It is a deceptively small part of the system when "inactive" but it can dilate significantly to accommodate a fetus. While something inserted into the vagina may touch the outer opening of the cervix, the cervix sits closed most of the time, so you're at no risk of losing a tampon. The cervix opens a little bit during ovulation, menstruation, and childbirth.
Clitoris: Research into the functions of the clitoris has been extremely limited. It has both an internal and external aspect, with the external being located above the urethra, and the internal wrapping around either side of the vagina. The only known function is arousal and sexual stimulation, which also improves fertility.
Fallopian Tubes: The fallopian tubes catch eggs released during ovulation and hold them in the ampulla until the egg is either fertilized - when the then-zygote is sent into the uterus to attach - or not, and released during menstruation.
Labia Majora: The external set of labia is called the labia majora. The labia majora functions to protect the rest of the vulva, the urethra, and the vagina. The labia majora typically swells with blood and slightly parts during arousal.
Labia Minora: The labia minora are the small, inner set of skin folds going from the clitoris to the bottom of the vaginal opening. Like the labia majora, their role is to protect everything encased in them. Unlike with labia majora, it isn't common to grow hair on the labia minora, which may cause discomfort and ingrown hair, leading to infection risks.
Ovaries: Ovaries are small round-ish sacs that contain eggs, the female half of the human gamete. Every month, a new egg drops out of the ovaries and floats (hopefully) to the fallopian tubes. Ovaries aren't attached to the fallopian tubes, so sometimes the eggs just get released into the abdominal cavity. During sex, sperm typically also ends up in the abdominal cavity, and that's how we get extrauterine pregnancies (ectopic pregnancy). Even without a uterus or fallopian tubes, a woman with even just one ovary can still experience pregnancy. Ovaries are also one of the biggest hormone controlling mechanisms in the female body.
Pubic Hair: Beginning at the start of puberty, girls develop pubic hair. By womanhood, this hair typically comes from the pelvis all the way down, covering the labia majora, extending onto the inner thighs, and down and back over the perineum and up around the anus. Pubic hair is there to help us keep clean. Typically the texture is springy, coarse, and curled. This helps prevent detritus from reaching the inner labia and vagina, which can cause irritation and infection. Pubic hair also wicks sweat and moisture away from the vulva. This is a very important function as the vagina and vulva are typically a little wet, due to discharge, and that moisture needs to be removed as it is replaced.
Skene's Glands: Located on either side and slightly under the urethra, these glands can release an "ultrafiltrate" of blood plasma, but typically only during (a really good) orgasm in a phenomenon known as female ejaculation/squirting/gushing. This is not urine. Fun fact: The fluid from Skene's glands is sweet, and has a very high concentration of both glucose and fructose.
Uterus: The uterus is an interesting and multi-purpose structure. Most commonly referenced, the uterus holds a fetus, develops the placenta, and does most of the work in reproduction. However, the uterus also serves as a "weight bearing" organ helping to define and maintain the structure of the abdominal cavity. Newer research is also indicating that the uterus plays an important part in hormone control, and overall health - for example, a hysterectomy increases your chance of developing dementia later in life.
Vagina: The vagina is a tube-like muscle organ that connects up to the cervix. When 'at rest' the vagina is quite short, but when a woman is aroused it lengthens. (Average vagina depth directly correlates to average penis length within a group - if the average penis length is 4-5 inches, the average vaginal depth when aroused is 4-5 inches.) As it's made of muscle, the vagina is highly maneuverable and can be clenched and released whether to increase pleasure during stimulation, or to help push a baby out.
Vulva: The external portion of the female reproductive system, comprising of the labia majora, labia minora, vaginal opening, clitoris, urethra, and associated glands. Everything you can see is the vulva. (|i|) << all vulva.
29 notes
·
View notes
Note
Ok, so, Ive had this question for a while.
Can the clitoris ejaculate?
Because everytime I get wet there is always two different residues, an upper one which is a whiteish yellow color and the latter one which is a transparent white
okay, there's a yes and no answer to this depending on context.
In short, regardless of your sex, anyone can ejaculate! this is because the paraurethral glands (more commonly called the prostate) two inches into your urethra are responsible for secreting mucus during arousal/after arousal. This highly acidic (and somewhat sweet) substance is used to clean out the urethra before ejaculation and after sex. It's purpose is to clear out bacteria and prevent UTIs. For those who produce sperm, it clears out the urethra for safe passage for the sperm (also called precum).
When it comes to the clitoris, the answer would typically be no. However, that wouldn't include the experience of those with female congenital adrenal hyperplasia, an intersex condition usually assigned female at birth. One specific variation of this is when the urethra is intertwined with the clitoris, homogamous to the urethras relationship with the penis, and would imply that ejaculation would come from the clitoris region. If you are a vulva owner without that intersex variation, then the urethra is more commonly located just slightly below the clitoris, or the "upper one" as you referred to it.
The colour and variations of texture for the ejaculation vary from person to person, and as long as they are frequent to you and cause no discomfort, don't get caught up too much on if the consistency, colour, or smell is "wrong." It changes for each person depending on what part of their hormonal cycle they're in.
"female" ejaculation (though there's no reason to gender it, since everyone does it to some degree), is commonly observed as squirting. A huge debate on whether squirt juice is pee or not has been a discussion for what seems like forever; and the answer is it is NOT! squirt juice comes from the urethra and the paraurethral orifices (two smaller holes, located to the left and right on the vulvas' urethra). Not only does it look, smell, taste, and feel different from pee, it's an entirely different chemical compound and produces entirely different enzymes. squirting is not peeing.
As for the clear, white residue comes from the vaginal walls and the greater vestibular gland orifices (located to the left and right of the vaginal opening). It's typically clear and thins out more during and after arousal. This is used as a natural lubrication and is the liquid people are referring to when they say they are wet.
When you are not aroused or "wet," than it's typically a bit thicker in consistency and a bit more white. This is discharge, which is a combination of cervical mucus, vaginal mucus, and a lower concentration of both greater vestibular glands juices and paraurethral juices. As said above, what's normal completely varies person to person depending on what part of their cycle they are in.
Thanks for the ask, and thank you for your vulnerability! your elaboration helped me pin point exactly what you were asking so i could explain exactly what your situation was. If anyone else has any questions, similar to this or not, feel free to ask! i'm open to anon asks, so don't be shy to get a little personal or detailed. this is a shame a stigma free place. Any hate will be deleted and blocked.
22 notes
·
View notes
Text
Everything about gynecologist visit
A woman going to a gynecologist office
Many women may feel anxious or nervous about visiting a gynecologist for the first time, but it is an important step for their health and well-being. A gynecologist is a doctor who specializes in women's reproductive health, including the vagina, uterus, ovaries, and breasts. A gynecologist can perform routine exams, screenings, tests, and treatments for various conditions and concerns.
Here are some things to know before going to a gynecologist office:
- When to go: The American College of Obstetricians and Gynecologists (ACOG) recommends that girls have their first gynecologic visit between the ages of 13 and 15. This visit is usually an opportunity to get to know the doctor, ask questions, and learn about preventive care. After that, women should see their gynecologist at least once a year for a well-woman exam, which may include a pelvic exam, a Pap smear, a breast exam, and other tests depending on their age and risk factors. Women should also see their gynecologist if they have any symptoms or concerns related to their reproductive health, such as abnormal bleeding, pain, discharge, infection, contraception, pregnancy, menopause, or sexual health.
- How to prepare: Before going to a gynecologist office, women should make a list of any questions or concerns they have for the doctor. They should also review their medical history, family history, medications, allergies, and sexual history. They should avoid having sex, douching, or using tampons or vaginal products for 24 hours before the visit. They should wear comfortable clothes and underwear that are easy to remove. They should also bring their insurance card and identification.
- What to expect: During the visit, the gynecologist will ask about the woman's health history, menstrual cycle, sexual activity, contraception, and any symptoms or problems she may have. The gynecologist will then perform a physical exam, which may include checking the woman's weight, blood pressure, heart rate, and abdomen. The gynecologist may also perform a pelvic exam, which involves inserting a speculum into the vagina to look at the cervix and take samples for testing. The gynecologist may also insert one or two fingers into the vagina and press on the abdomen to feel the uterus and ovaries. The pelvic exam may cause some discomfort or pressure, but it should not be painful. The gynecologist may also perform a breast exam by feeling the breasts and underarms for any lumps or changes. The gynecologist will then discuss the results of the exam and tests with the woman and provide any recommendations or treatments. The woman can ask any questions or express any concerns she may have at this time.
- How to follow up: After the visit, the woman should follow any instructions or prescriptions given by the gynecologist. She should also contact the office if she has any questions or problems or if she does not receive her test results within a reasonable time. She should also schedule her next appointment as recommended by the gynecologist.
Going to a gynecologist office is an essential part of taking care of one's reproductive health. By knowing what to expect and how to prepare, women can have a positive and productive experience with their gynecologist.
2 notes
·
View notes
Text
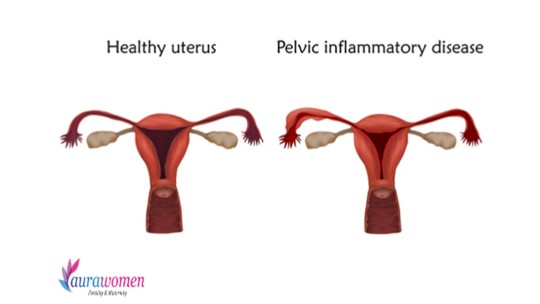
What is PID?
PID stands for "Pelvic Inflammatory Disease." It is a serious infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. PID is typically caused by untreated or undertreated sexually transmitted infections (STIs) such as chlamydia and gonorrhea but can also result from other infections. Common symptoms include lower abdominal pain, fever, unusual vaginal discharge, painful intercourse, and irregular menstrual bleeding. PID can lead to severe complications like infertility, chronic pelvic pain, and ectopic pregnancies. Early diagnosis and prompt treatment with antibiotics are crucial to prevent these complications. Regular STI testing and safe sexual practices can reduce the risk of PID.
#aurawomen#aura#ivf#iui#fertility#infertility#pregnancy#maternity#ivfsuccess#iuisuccess#pregnacy#pelvicinflamatory#pid#pid controller#ovulation pain
4 notes
·
View notes
Text
What are Sign and Risk Factor of Cervical Cancer ? Which Hospital Cerivcal Cancer Specialist in Delhi?
Cervical cancer is a significant health concern affecting women worldwide. While advancements in medical science have improved our understanding of the disease and its prevention, it remains crucial for women to be aware of the signs and risk factors associated with cervical cancer. Early detection can greatly increase the chances of successful treatment. In this article, we will explore the signs and risk factors of cervical cancer.
Signs of Cervical Cancer
Abnormal Vaginal Bleeding: One of the most common signs of cervical cancer is abnormal vaginal bleeding. This can manifest as bleeding between menstrual periods, after intercourse, or after menopause. Any unexplained vaginal bleeding should be promptly reported to a healthcare provider.
Pelvic Pain: Persistent, unexplained pelvic pain or discomfort can be a sign of cervical cancer. This pain may occur during intercourse or at other times and should not be ignored.
Pain During Intercourse: Pain or discomfort during sexual intercourse, known as dyspareunia, can also be indicative of cervical cancer. It may occur due to the growth of tumors in the cervix.
Unusual Vaginal Discharge: An unusual vaginal discharge that is watery, bloody, or has a foul odor may be a sign of cervical cancer. It is essential to differentiate between normal vaginal discharge and unusual changes.
Painful Urination: Cervical cancer Treatment in Delhi can sometimes cause urinary symptoms, including painful urination. However, this is less common than other symptoms and can also be caused by various other conditions.
Fatigue and Weight Loss: As with many cancers, cervical cancer can cause general symptoms like fatigue and unexplained weight loss. These symptoms are often seen in advanced stages of the disease.
Risk Factors of Cervical Cancer
Human Papillomavirus (HPV) Infection: HPV is the leading risk factor for cervical cancer. It is a common sexually transmitted infection that can lead to changes in cervical cells, potentially progressing to cancer over time. Vaccination against HPV is available and recommended for young individuals to reduce this risk.
Smoking: Smoking is a significant risk factor for cervical cancer. Women who smoke are more likely to develop the disease and have a higher chance of it progressing to an advanced stage.
Weak Immune System: A weakened immune system, often due to conditions like HIV/AIDS or immunosuppressive medications, can increase the risk of cervical cancer. A robust immune system helps the body fight off HPV infections.
Early Age of Sexual Activity: Engaging in sexual activity at an early age, particularly before the age of 18, increases the risk of exposure to HPV and, consequently, cervical cancer.
Multiple Sexual Partners: Having multiple sexual partners can increase the risk of HPV infection, which is a primary cause of cervical cancer. Cervical Cancer Doctor in Delhi
Family History: Women with a family history of cervical cancer may have a higher risk due to possible genetic factors or shared environmental exposures.
Oral Contraceptive Use: Long-term use of oral contraceptives (birth control pills) may slightly increase the risk of cervical cancer. However, this risk decreases after stopping their use.
Socioeconomic Factors: Limited access to healthcare and regular screenings can also increase the risk, as cervical cancer may not be detected in its early stages.
Sunrise hospital has the Cervical Cancer Specialist in Delhi.
2 notes
·
View notes
Text
Cervical cancer
Cervical cancer is a type of cancer that develops in the cervix, which is the lower part of the uterus that connects to the vagina. It is the fourth most common cancer in women worldwide and can affect women of all ages. However, it is most often diagnosed in women between 35 and years of age.
Causes of cervical cancer:
The main cause of cervical cancer is infection with human papillomavirus (HPV), a sexually transmitted virus. There are more than 100 different types of HPV, and some types can cause cervical cancer. Other factors that can increase the risk of cervical cancer include smoking, a weakened immune system, a family history of cervical cancer, and multiple sexual partners.
Symptoms of cervical cancer:
Cervical cancer does not necessarily cause symptoms in its early stages. As the cancer progresses, symptoms may include abnormal vaginal bleeding, pelvic pain or discomfort, pain during intercourse, and unusual vaginal discharge. It is important to note that these symptoms can be caused by other diseases, so it is important to consult a doctor to get a proper diagnosis.
Prevention and early detection of cervical cancer:
The most effective way to prevent cervical cancer is the HPV vaccine. The HPV vaccine protects against the types of HPV that cause most cases of cervical cancer, as well as against other types of HPV that can cause other types of cancer. The vaccine is recommended for males and females between 9 and 26 years of age.
Regular cervical cancer screening is also important for early detection. A Pap test is a test that checks for abnormal cells on the cervix. It is recommended that women start regular Pap tests from the age of 21. In addition, the new HPV test can also detect the presence of the virus that causes cervical cancer. Women should discuss with their healthcare provider which exams are right for them.
Treatment of cervical cancer:
Treatment of cervical cancer depends on the stage of the cancer and other factors such as the woman's age and general health. Treatment options may include surgery, radiation therapy, chemotherapy, or a combination of these treatments.
In summary, cervical cancer is a common female cancer that can be prevented by vaccination and detected early by regular screening. Women should consult with their health care provider to determine appropriate screening and vaccination. If cervical cancer is diagnosed, early treatment can lead to a better outcome.
For more information Visit: www.oncorelief.in
#Cervical cancer#Women's health#Cancer prevention#Cancer screening#HPV vaccine#Pap test#HPV test#Cancer treatment#Early detection#Health education#Gynecologic oncology#Oncology nursing#Reproductive health#Sexually transmitted infections#Public health#Medical research#Health advocacy#Patient support#Survivorship
2 notes
·
View notes
Text
What is the use of Progynova Tablet?
Progynova 1 MG Tablet is a form of female sex hormone, estrogen.
It is used to relieve symptoms occurring after menopause such as vaginal dryness/burning/itching, hot flashes, etc. and prevents osteoporosis (a condition in which bone becomes weak and fragile).
Progynova 1 MG Tablet shows side effects like stomach pain, headache, changes in weight, oedema (swelling) of legs, breast tenderness, mood alterations including anxiety and depressed mood.
Inform your doctor if these side effects become severe or persist for a long time.
Progynova 1 MG Tablet can be taken with or without food. Take it at the same time every day for the ease of remembering.
Your doctor will decide the dosage of this medicine based on the indication you are taking it for.
Progynova 1 MG Tablet is not recommended for use if you have abnormal/unusual vaginal bleeding.
Inform your doctor if you have any kidney problems, diabetes, or any other medical conditions.
Do not take this medicine if you are pregnant or planning a pregnancy.
Inform your doctor if you are breastfeeding to understand its benefits and the risk to your infant.

Side effects
Major & minor side effects for Progynova 1 MG Tablet
Breast pain and tenderness
Vomiting
Weight gain
Dizziness
Depression
Back pain
Headache
Vaginal discharge with no odor
Swelling of face, lips, eyelids, tongue, hands and feet
Discharge from the nipple
Change in the texture of breast skin and nipples
Uses of Progynova 1 MG Tablet
What is it prescribed for?
Post menopausal symptomsA post-menopausal symptom is a group of symptoms that you experience after menopause (end of menstrual cycles). These symptoms may include vaginal dryness/itching, hot flushes, irritability, and mood swings. Progynova 1 MG Tablet works by balancing the level of hormones (chemical messengers) that cause these symptoms in your body.
Postmenopausal osteoporosisPostmenopausal osteoporosis is a condition that causes weak and fragile bones due to decreased levels of estrogen in your body. Its symptoms are back pain, change in posture, etc. Progynova 1 MG Tablet is used to prevent and treat the symptoms of osteoporosis in women who have reached menopause.
Hormonal replacement therapyProgynova 1 MG Tablet is used as Hormonal replacement therapy to relieve symptoms associated with menopause. This includes mood swings, hot flushes, decreased urge to have sex and vaginal dryness. You are advised to use this medicine only upon your doctor's advice.
When not to use?
Allergy
Avoid taking Progynova 1 MG Tablet if you are allergic to it. Allergic reactions are rare; however, contact your doctor immediately if you experience symptoms like rashes, itching/swelling (particularly of your face/tongue/throat), severe dizziness, and breathing difficulty, etc.
Undiagnosed vaginal bleeding
Progynova 1 MG Tablet is not recommended for use if you have an abnormal vaginal bleeding episode that has not been diagnosed by your doctor. If you have any menstrual abnormalities, consult your doctor first before taking this medicine.
Heart and blood vessel disorder
Progynova 1 MG Tablet is not recommended if you have an active or history of stroke (brain damage due to blocked blood flow) or heart attack. This medicine should also be avoided if you have an active or previous blood clotting issue. Progynova 1 MG Tablet can lead to an increase in clot formation if taken in higher doses and thus can worsen your condition.
Estrogen-dependent tumor
Progynova 1 MG Tablet is not recommended if you have cancer that is sensitive to oestrogens, such as breast and cancer of the endometrium (womb lining), or if you are suspected of having it.
Liver Tumours
Liver tumours are types of cancer that form in the liver. Progynova 1 MG Tablet is not recommended in liver tumours because long term use of this medicine may worsen your condition.
Porphyria
Porphyria is a disorder resulting from the accumulation of certain chemicals related to blood cell proteins. Progynova 1 MG Tablet is not recommended in the presence of porphyria.
0 notes
Text
Pregnancy increases vaginal discharge due to various hormonal and physiological changes. Here are some reasons why:
1. *Hormonal fluctuations*: During pregnancy, estrogen levels surge, stimulating the cervix to produce more mucus. This increased mucus production leads to more vaginal discharge.
2. *Cervical ectropion*: Pregnancy hormones can cause the cervix to protrude into the vagina, leading to an increase in cervical mucus production.
3. *Increased blood flow*: Pregnancy increases blood flow to the pelvic area, including the vagina, which can lead to more discharge.
4. *Vaginal pH changes*: The vaginal pH becomes more alkaline during pregnancy, which can lead to an overgrowth of bacteria, resulting in increased discharge.
5. *Immune system changes*: Pregnancy suppresses the immune system to prevent it from attacking the fetus, which can lead to an overgrowth of bacteria and increased discharge.
6. *Pressure on the urethra*: The growing uterus can put pressure on the urethra, leading to increased urine frequency and, in some cases, increased vaginal discharge.
7. *Prostaglandins*: Pregnancy hormones stimulate the production of prostaglandins, which can cause smooth muscle contractions, leading to increased vaginal discharge.
It's important to note that while increased vaginal discharge during pregnancy is normal, it's essential to distinguish it from abnormal discharge, which can be a sign of an underlying infection. If you have concerns or notice any unusual changes, it's always best to consult your healthcare provider.
0 notes
Text
The best way to Stay clear of STDs: Important Prevention Strategies
Sexually transmitted illnesses (STDs) are a major public wellness worry, influencing thousands and thousands of people globally. Preventing STDs is important for retaining sexual overall health and Total properly-becoming. Below’s an in depth guide regarding how to steer clear of STDs by way of informed decisions and preventive measures. For further insights and precious recommendations on how to keep Harmless from STDs, like expert recommendations and up-to-day info on avoidance and treatment, be sure to take a look at our substantial resource web site at https://www.gopusa.com/central-pa-drag-queen-activist-charged-with-25-counts-of-child-pornography-police/ . Your health and perfectly-remaining are our top rated precedence—continue to be informed and keep shielded.
In depth Comprehension of STDs
STDs include things like a range of bacterial infections like chlamydia, gonorrhea, syphilis, HIV, herpes, and HPV. These bacterial infections may cause serious health issues if still left untreated, which includes infertility, Long-term soreness, and a heightened danger of other bacterial infections. Recognizing the significance of prevention may result in more healthy sexual practices.
Consistent Use of Condoms
Utilizing condoms in the course of every sexual experience, which include vaginal, anal, and oral intercourse, is one of the most effective techniques to stop STDs. Condoms act as a barrier that forestalls the Trade of bodily fluids, therefore considerably lowering the risk of transmitting infections. Ensure proper utilization To maximise their usefulness.
Vaccination as a Preventive Device
Vaccines are offered for certain STDs, for instance HPV and hepatitis B. The HPV vaccine is recommended for both equally males and females, ideally ahead of they become sexually Energetic. The hepatitis B vaccine is an element on the plan vaccination plan for youngsters but can be administered at any age. These vaccines deliver very long-expression safety towards these infections.
Mutual Monogamy
Remaining in a mutually monogamous marriage where by both of those companions are examined and confirmed for being free of STDs can greatly cut down the risk of an infection. This entails both of those partners agreeing to own sexual relations only with one another. Trust, honesty, and normal testing are essential components of the preventive tactic.
Common STD Screening
Regimen STD tests is significant, particularly when you have got numerous sexual associates or engage in unprotected sex. Several STDs don't exhibit fast signs or symptoms, so standard screening assures early detection and procedure. Early procedure can avert extreme health and fitness complications and minimize the potential risk of transmission to others.
Open up Interaction with Companions
Discussing sexual wellbeing, STD status, and Harmless sex tactics together with your companion(s) is essential. This dialogue should include subjects like earlier sexual historical past, screening frequency, and the use of safety. Genuine and open up communication fosters have faith in and promotes safer sexual tactics.
Staying away from Large-Possibility Behaviors
Specific behaviors, like possessing various sexual companions or participating in unprotected sexual intercourse, improve the possibility of STDs. Minimizing the amount of sexual associates and constantly using protection can appreciably lower this hazard. Currently being selective and careful with sexual encounters is often a useful method of prevention.
Recognizing Signs or symptoms of STDs
Whilst numerous STDs could be asymptomatic, it’s vital to acknowledge the likely signs of infection. Indicators might contain strange discharge, sores or bumps, itching, and suffering throughout urination. Getting vigilant about these signs or symptoms and looking for healthcare tips promptly can avoid troubles along with the unfold of bacterial infections.
Beyond Condoms: Further Defense
As well as condoms, other protecting measures can reduce the chance of STDs. Dental dams can be utilized for the duration of oral sexual intercourse to prevent the exchange of bodily fluids. Additionally, practising very good hygiene and staying away from the sharing of private products like razors and towels may also help stop infections.
Educating Yourself and Other folks
Training is a strong Device in STD avoidance. Remain knowledgeable by way of respected sources for example Health care providers, general public health corporations, and educational packages. Knowledge the pitfalls, signs and symptoms, and preventive steps empowers you for making knowledgeable choices and promote sexual health.
Trying to find Specialist Health care Advice
When you have any fears or indicators connected to STDs, seeking Experienced Health care assistance is vital. Healthcare suppliers can give screening, therapy, and counseling, assisting you handle and forestall bacterial infections successfully. Typical Examine-ups and consultations can offer peace of mind and maintain sexual wellness.
Respecting Boundaries and Supporting Each Other
In relationships, it’s essential to respect each other’s boundaries and assist safe sexual intercourse practices. Encouraging and working towards mutual regard and comprehension can boost your romance and make sure the two companions’ health and security. A cooperative method of sexual well being strengthens believe in and well-getting.

In conclusion, avoiding STDs will involve a combination of Safe and sound sexual intercourse methods, typical testing, vaccination, and open conversation. By adopting these strategies, you'll be able to protect yourself along with your associate from your pitfalls affiliated with STDs, making certain a healthier and satisfying sexual lifestyle. Training and proactive actions will be the cornerstones of successful STD avoidance, fostering a culture of wellbeing and responsibility in sexual relationships.
1 note
·
View note
Text
7 Signs It’s Time to See a Gynaecologist
Women often prioritize the health of their loved ones over their own, but it’s crucial to remember that self-care is not selfish. Regular check-ups with a gynaecologist play a vital role in maintaining overall well-being. Knowing when to schedule a visit to the best multispecialty hospital can make a significant difference in catching potential health issues early on.

Thangam Hospital of PMRC is the best multispecialty hospital in Palakkad that delivers a comprehensive range of preventive, acute, and outpatient services. Our hospital, located in Palakkad, Kerala, is ideal for people seeking treatment for various ailments, because of its excellent infrastructure and our commitment to maintaining the highest standards of safety, cleanliness, integrity, and honesty.
The obstetrics team from the Department of Obstetrics and Gynaecology are trained and experienced in handling all sorts of complexities related to Gynaecology. We have experienced and expert doctors and nursing staff, available 24×7 in our department to deal with major gynaecological issues.
In this blog post, we will explore seven signs that indicate it’s time to see a gynaecologist.
Irregular Menstrual Cycles:
Irregular periods can be a common occurrence for many women, but persistent irregularities may be a cause for concern. If your menstrual cycle suddenly becomes irregular, too frequent, or unusually heavy, it’s essential to consult with a gynaecologist. Irregularities can be indicative of hormonal imbalances, polycystic ovary syndrome (PCOS), or even due to menopause.
Irregular menstrual cycles in women of a certain age group are occasionally misinterpreted as signs of menopause. This misunderstanding can lead to a failure in identifying potential risks of ovarian, uterine, or cervical cancers.
Unexplained Pelvic Pain:
Pelvic pain that isn’t related to your menstrual cycle or occurs outside of normal cramping can be a red flag. Persistent or severe pelvic pain may be a sign of conditions such as endometriosis, pelvic inflammatory disease (PID), or ovarian cysts. A gynaecologist can help diagnose the cause of the pain and recommend appropriate treatment.
Abnormal Vaginal Discharge:
Changes in the colour, consistency, or odour of vaginal discharge can be signs of infection or other reproductive health issues. If you notice any unusual changes, it’s crucial to seek medical attention promptly. A gynaecologist can perform tests to identify the cause and prescribe appropriate medications if necessary.
Painful Intercourse:
Experiencing pain or discomfort during intercourse is not normal and should not be ignored. It could be due to a variety of factors, including infections, hormonal imbalances, or conditions like vaginismus. A gynaecologist can help identify the underlying cause and recommend appropriate treatment options.
Concerns About Birth Control:
If you are experiencing side effects from your current method of birth control or are considering a change in contraception, it’s a good time to consult with your gynaecologist. They can provide information on various birth control options, address concerns, and help you find a method that suits your individual needs and lifestyle.
Family Planning and Pregnancy:
If you are planning to start a family or are currently pregnant, regular visits to a gynaecologist are essential for a healthy pregnancy and childbirth. Your gynaecologist can guide preconception care, monitor your pregnancy, and address any concerns or complications that may arise.
Conclusion:
Prioritizing your reproductive health is a crucial aspect of self-care. If you’re experiencing any of the signs mentioned above or have concerns about your reproductive health, it’s time to schedule an appointment with a gynaecologist. Regular check-ups from Thangam Hospital of PMRC, the best Multispecialty hospital in Palakkad detect potential issues early on and contribute to maintaining overall well-being.
Thangam, the best Gynaecology hospital in Palakkad deals with aspects of PCOS & infertility, complications during pregnancy and childbirth, as well as various other diseases of the female reproductive system.
If you have any concerns or need professional guidance on your reproductive health, our experienced team is here to provide comprehensive care and support.
Schedule an appointment today with us to ensure a healthier tomorrow.
#gynaecologist#gynaecologist doctor#gynaecology#best Gynaecology hospital in Palakkad#best Gynaecology hospital#hospital#multispecialty hospital
0 notes
Text
Cervical cancer: understanding its impact, symptoms, and stages for early detection and prevention.
Cervical cancer is a significant health concern affecting women worldwide. It arises from abnormal cell growth in the cervix, the lower part of the uterus that connects to the vagina. Understanding the symptoms and stages of cervical cancer is crucial for early detection and effective treatment.
What is Cervical Cancer?
Cervical cancer develops when cells in the cervix undergo abnormal changes, typically caused by human papillomavirus (HPV) infection. While HPV is common and often clears on its own, persistent infection with high-risk HPV strains can lead to the development of cervical cancer over time. Regular screening tests, such as Pap smears and HPV tests, can help detect abnormal changes in the cervix early, allowing for timely intervention.
Symptoms of Cervical Cancer
In its early stages, cervical cancer may not cause noticeable symptoms. However, as the disease progresses, women may experience:
Abnormal vaginal bleeding, such as between periods, after sex, or after menopause.
Pelvic pain or discomfort during intercourse.
Unusual vaginal discharge that may be watery, bloody, or foul-smelling.
Pain in the lower back or pelvis.
It is essential to promptly consult a healthcare professional if any of these symptoms occur, as early detection significantly improves treatment outcomes.
Stages of Cervical Cancer
Cervical cancer is typically classified into different stages based on the extent of the disease. These stages include:
Stage 0 (carcinoma in situ): Abnormal cells are confined to the surface layer of the cervix and have not invaded deeper tissues.
Stage I: Cancer is confined to the cervix but has not spread to surrounding tissues.
Stage II: Cancer has spread beyond the cervix to nearby tissues, such as the upper vagina or pelvic wall.
Stage III: Cancer has spread to the lower vagina, pelvic wall, or nearby lymph nodes.
Stage IV: Cancer has metastasized to distant organs, such as the bladder, rectum, or lungs.
The stage of cervical cancer guides treatment decisions and prognosis, with earlier stages generally associated with better outcomes.
Prevention and Screening
Preventing cervical cancer involves a multifaceted approach that includes vaccination against HPV, regular cervical cancer screening, and adopting healthy lifestyle habits. The HPV vaccine is highly effective at preventing infection with the most common HPV strains responsible for cervical cancer. Additionally, routine screenings, such as Pap smears and HPV tests, can detect precancerous changes in the cervix early, allowing for timely intervention before cancer develops.
SmartCare Diagnostics Pvt Ltd: Empowering Women's Health
SmartCare Diagnostics Pvt Ltd is at the forefront of promoting women's health by offering state-of-the-art diagnostic services and innovative healthcare solutions. Through advanced technologies and a patient-centric approach, SmartCare is committed to early detection and prevention of cervical cancer. From comprehensive screening tests to personalized treatment plans, SmartCare prioritizes the well-being of every individual, ensuring access to high-quality healthcare services.
In collaboration with healthcare providers and communities, SmartCare strives to raise awareness about cervical cancer prevention and the importance of regular screenings. By empowering women with knowledge and resources, SmartCare aims to reduce the burden of cervical cancer and improve health outcomes for generations to come.
The Importance of Awareness and Education
Raising awareness about cervical cancer and its prevention is crucial in combating the disease. Educational campaigns aimed at promoting HPV vaccination and regular screenings play a vital role in empowering women to take charge of their health. Additionally, providing accurate information about risk factors, symptoms, and available treatment options can help dispel myths and misconceptions surrounding cervical cancer.
Barriers to Screening and Treatment
Despite the availability of screening tests and effective treatment options, various barriers prevent women from accessing cervical cancer prevention and care services. These barriers may include limited access to healthcare facilities, lack of awareness about the importance of screenings, cultural stigma, and financial constraints. Addressing these barriers requires a concerted effort from policymakers, healthcare providers, and community organizations to ensure equitable access to cervical cancer prevention and treatment services for all women.
The Role of Technology in Cervical Cancer Prevention
Advancements in technology have revolutionized cervical cancer prevention and screening methods. Digital health platforms and mobile applications enable women to access information about cervical cancer prevention, schedule screenings, and receive reminders for follow-up appointments. Additionally, telemedicine services facilitate remote consultations with healthcare providers, particularly in underserved areas where access to healthcare facilities is limited.
Support Services for Women with Cervical Cancer
A diagnosis of cervical cancer can be emotionally and psychologically challenging for women. Support services, such as counseling, support groups, and patient advocacy organizations, play a crucial role in providing emotional support, guidance, and resources to women and their families throughout their cancer journey. These services help women cope with the physical and emotional toll of the disease, navigate treatment decisions, and improve their quality of life.
Conclusion
Cervical cancer is a preventable and treatable disease, particularly when detected early through regular screenings. By raising awareness, promoting HPV vaccination, and ensuring access to screening and treatment services, we can reduce the burden of cervical cancer and save lives. SmartCare Diagnostics Pvt Ltd is dedicated to empowering women's health and contributing to the fight against cervical cancer through innovative diagnostic solutions and comprehensive healthcare services.
#best diagnostic centre#healthcare#healthylifestyle#service provider#smartcare#smartcarelabs#SmartCare Diagnostics Pvt Ltd#smarthealth#SmartCare
0 notes
Text
How Should One Do Istinjah Properly?
Question
I take very long in the bathroom and then miss prayers. I spend 30 min on the toilet and 20 making wudu’. I fill my lotaa (jug) 4-5 times to wash for urine. Should every part be rubbed? Must inner thighs be washed in Istinjah? What if vaginal discharge touched them, and I do not know?
Is it sufficient to pour water on the inner thighs? Is it permissible to sit on the toilet with legs open to avoid anything touching your thighs? Will this cause splashes when urinating? I am worried that vaginal discharge mixed with water will splash my inner thighs during Istinjah.
Answer
I pray that this situation improves for you and that you stop paying attention to waswasah (baseless misgivings).
Using four or five jugs of water is way too much water. Although there is no set amount, one large jar (lotaa) is usually too much.
Every part does not have to be rubbed, nor is rubbing obligatory. However, scholars advise that one use the middle finger of the left hand to remove the filth in the rear.
Inner thighs don’t require washing during Istinjah.
If you don’t know that vaginal discharge affects your inner thighs, you don’t need to wash them. Certainty is not removed by doubt.
If the vaginal discharge does affect the inner thighs, one can pour water and rub to remove it. However, most vaginal discharge is pure, so it doesn’t require removal.
Sit on the toilet with the legs open when relieving oneself is permissible. What causes splashing is different for everyone. A woman can gently push her skin down (the pelvic area where the pubic hair is) to prevent urine from splashing out onto the seat.
Vaginal discharge mixed with urine should not splash on the thighs when washing oneself. If something does splash, assume it is pure water. You may be seeing more splashes because you are using so much water.
Pouring water during rubbing and drying should take a minute or two. The same is with wudu’. So urinating, washing, and performing wudu’ should take five minutes. Please keep working on this until it is down to the desired timing.
Also, take a course on obligatory knowledge to fight off this waswasa. It is the best weapon you can have. The Shaytan is succeeding when he whispers to you to prolong your time in the bathroom because you end up missing prayers. Make up those prayers and don’t succumb to his tricks. Please see the link below for complete detail on this topic.
Kindly see this article:
How to Deal With Waswasah Regarding Purity According to the Shafi’i School?
Hope this helps, In shaa Allah!
[Ustadhah] Shazia Ahmad
Checked and Approved by Shaykh Faraz Rabbani
Ustadha Shazia Ahmad lived in Damascus, Syria for two years where she studied ‘aqidah, fiqh, tajweed, tafseer, and Arabic language. She then attended the University of Texas at Austin, where she completed her Masters in Arabic langage. Afterward, she moved to Amman, Jordan, where she studied fiqh, Arabic, and other sciences. She later moved back to Mississauga, Canada, where she lives with her family.
REFERENCES:
0 notes
Text
Experts recommend women see a gynecologist at least once a year. ~ Toni Weschler, MPH
“Toni Weschler introduced the Fertility Awareness Method (FAM) in 1995 — a natural and effective birth control option — women still barely understood their menstrual cycles.”
Your menstrual cycle is not something that should be shrouded in mystery. ~ Toni Weschler
“Cervical fluids have two jobs:
• Assisting the sperm toward the egg.
• Preventing the sperm from entering the cervix.”
“Cervical fluids have two jobs:
• Assisting the sperm toward the egg.
• Preventing the sperm from entering the cervix.
The condition of cervical secretions can signal fertile times or hint at dysfunction. That said, FAM is essential knowledge for healthcare professionals and menstruating women to prevent any reproductive oddities. The method can detect problems such as:
• Lack of ovulation
• Late ovulation
• Infertile cervical fluid
• Hormonal imbalances
• Miscarriages”
“Most contraception aids demonstrate side effects, some of which are detrimental to female health:
• Oral contraceptives increase the risk of breast and cervical cancer.
• Intrauterine devices (IUDs) can cause chronic inflammation and painful menstruation.
• Diaphragms, cervical caps, and sponges can provoke vaginal infections.”
“FAM encourages observation of vaginal discharge during ovulation. For instance, changes in cervical fluid patterns are natural during that period. A wetter and stickier cervical fluid indicates high fertility, which happens days before ovulation. Another way to confirm a pregnancy is by observing your waking temperature. Rising body heat usually indicates successful ovulation, while estrogen lowers the physical temperature before the egg’s release.”
“You'll also notice an increase in cervical fluid before egg release. Increased progesterone causes an excess of non-fertile cervical fluid that prevents sperm from further entry.
Examine your cervical fluids right after your period.
• Focus on vaginal sensation; does it feel dry, sticky, or wet?
• Check if it stretches or breaks.”
“The most common female reproductive diseases include:
• Ovarian cysts
• Endometriosis
• Polycystic Ovarian Syndrome (PCOS)”
“The two most familiar types of cysts are functional and follicular cysts. The former develops within the body’s regular functions but continues growing beyond the normal size, causing irregular menstrual cycles. As for the latter, follicular cysts originate from egg follicles that enlarge into a cyst, preventing ovulation. Follicular cysts can resolve independently but may still cause chronic pelvic pain; progesterone injections or surgery can successfully treat these fluid-filled sacs.”
“During endometriosis, the waste products of menstruation remain inside the uterus, growing as cysts. The early stages of endometriosis can be challenging to detect as it takes time to accumulate the leftover uterine tissue and blood remnants. So, most of the time, it has already spread all over the ovary before doctors diagnose the condition.”
“p olycystic ovarian syndrome affects 5% to 10% of fertile women, presenting long-term health risks. The most common symptoms include:
• Irregular cycles lasting over 35 days
• Abnormally frequent cervical fluid release
• Facial or excessive hair
• Obesity
• Inability to conceive
Hormonal birth control and lifestyle changes can help manage the condition, but further professional intervention is necessary.”
The age of menopause is likely to concur in women of the same biological family. ~ Toni Weschler, MPH
“Fertility starts to diminish about thirteen years before menopause. If you'd like to preserve your eggs, seek testing for endometriosis, PCOS, and ovarian cysts. If any of these conditions come up on the radar, you must address them before pregnancy. In addition to aging, these ailments can significantly harm your fertility.”
…Women are fertile for only a fraction of the time men are. ~ Toni Weschler
“Any woman looking to have children in the future must check her ovaries early to know the number of fertile eggs left. The Anti-Mullerian Hormone (AMH) test and the Antral Follicle Count are standard fertility tests suitable for women of childbearing age. In addition, safe sex also reduces the chances of contracting STIs, preventing the scarring of fallopian tubes and preserving more fertile eggs.
If you plan to have children in your 30s or later, egg-freezing technologies may help you.”
“Whenever a woman is ready, she undergoes in vitro fertilization (IVF) to conceive a child artificially. However, the success rate of IVF is still low.
People looking to freeze their eggs must avoid surgery on their ovaries to prevent their mature eggs from scarring.”
“Male health is equally vital for smooth pregnancy and childbirth. That said, men must check their fertility as regularly as their opposite-sex partners.
The most common tests for male fertility are:
• Semen analysis
• Sperm penetration
• Sperm DNA
A semen analysis is the most common test to determine sperm activity. To perform it, urologists collect the semen and count the exact number of sperm with normal shape and motility.”
“men and women can improve their reproductive health by, first and foremost, changing their lifestyles. Lowering caffeine, nicotine, and alcohol consumption or cutting it out completely is a good start. Focus more on low-carb and low-glycemic diets and drink at least eight cups of non-caffeinated liquids daily.
As for women, p remenstrual syndrome (PMS) and menopause are prevailing hormonal battles, with the most popular treatments including:
• Prescribed medications like diuretics, antidepressants, or mood stabilizers
• Osteopathy
• Hormone therapy
• Natural alternatives”
“Women going through menopause have to deal with:
• Sexual desire and sensitivity loss
• Lower energy
• Increased pubic hair
• Poor calcium levels
Furthermore, acupuncture and acupressure can harmonize your hormones and help you enter menopause with ease. The most important thing to remember is that menopause may jumble your hormones for a while, but it doesn’t steal your sensuality.
Did you know? A female is born with a lifetime’s worth of eggs.”
“Finally, it's worth reminding women that they don't have to give early birth to satisfy societal norms. Either way, you’re safe to freeze your eggs and have children when you’re mentally and financially ready.
Try this:
• Monitor your cervical fluid: An egg-white color signals upcoming or a recently finished ovulation.
• Try a luteinizing hormone (LH) urine test. This hormone spikes 24 hours before egg release.
• A slight increase in body temperature follows the fertile window. Measure your body heat regularly at the same time to notice a temperature change.”
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
I wanted to share this thought-provoking idea with you 🤗
Start discovering thousands of them on the Headway app today 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=quote&af_siteid=summary_text
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
I wanted to share this thought-provoking idea with you 🤗
Start discovering thousands of them on the Headway app today 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=insight&af_siteid=summary_text
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
I wanted to share this thought-provoking idea with you 🤗
Start discovering thousands of them on the Headway app today 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=quote&af_siteid=summary_text
My highlight from Taking Charge of Your Fertility on the Headway app. Start making yours 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=highlight&af_siteid=highlights
I wanted to share this thought-provoking idea with you 🤗
Start discovering thousands of them on the Headway app today 👇
https://headway.onelink.me/9USK?pid=app_referral&af_web_dp=https%3A%2F%2Fweb.get-headway.com%2Fbook%2F&c=insight&af_siteid=summary_text
0 notes
Text
CERVICAL FIBROIDS
Cervical myomas (also known as cervical fibroids) are smooth, round benign tumors composed mostly of muscle tissue. These fibroids are present in the cervix, the lower part of the uterus, and are rare. They are usually accompanied by uterine fibroids, in the larger upper part of the uterus. Based on their location, cervical myomas can be classified as extra cervical (sub-serosal myoma) and intracervical. Cervical fibroids can further be anterior, posterior, lateral, and central depending on their position.
There are different types of uterine fibroids depending on where they’re located and how they attach. Specific types of uterine fibroids include:
Intramural fibroids: Intramural fibroids are the most common type and they are embedded into the muscular wall of your uterus.
Submucosal fibroids: These fibroids grow under the inner lining of your uterus.
Subserosal fibroids: Subserosal fibroids grow under the lining of the outer surface of your uterus. They can become quite large and grow into your pelvis.
Pedunculated fibroids: These are the least common type of fibroids and they attach to your uterus with a stalk or stem. They’re often described as mushroom-like because they have a stalk and then a wider top.
However, they can cause serious problems in some cases, especially if they are large. They may block part of the urinary tract or prolapse through the cervix and into the vaginal canal. Prolapsed myomas may develop ulcers, which could cause abnormal bleeding or infection.
Causes:
Most cervical fibroids eventually cause symptoms. It’s unclear why fibroids develop. A couple of different factors may influence their formation:
Hormones: The ovaries produce estrogen and progesterone. These hormones cause the uterine lining to regenerate during each menstrual cycle and stimulate the growth of fibroids.
Family history: Fibroids may run in the family. If your mother, sister, or grandmother has a history of this condition, you may develop it as well.
Risk factors:
People are at greater risk of developing fibroids if they have one or more of the following risk factors:
Due to their family history
If they are 30 years or above
Body weight is high.
The surgical treatment of cervical leiomyomas poses more difficulty; due to the risk of intraoperative Hemorrhage and the potential injuries because of contiguity and dislocation of adjacent organs.
Symptoms:
Mild cervical myomas may not cause any problems while moderate to severe myomas may cause one or more of these symptoms:
1. Painful or excessive bleeding during the period.
2. Bleeding between your periods.
3. Menstrual clots.
4. Anemia, as a result of heavy bleeding, accompanied by fatigue
5. A feeling of fullness in your lower belly (abdomen)/bloating.
6. Frequent urination (this can happen when a fibroid puts pressure on your bladder).
7. Dyspareunia
8. Low back pain and pain in the pelvis.
9. Constipation or feeling pressure on your rectum.
10. Long-term (chronic) vaginal discharge.
11. Inability to pee or empty your bladder.
12. Increased abdominal distention (enlargement), causes your abdomen to look pregnant.
The symptoms of uterine fibroids usually stabilize or go away after you’ve gone through menopause because hormone levels decline within your body.
Treatment:
Small myomas that do not cause symptoms may not need to be treated. However large fibroids/myomas that are causing pain, bleeding, or urinary problems can be surgically removed via myomectomy. Depending on the size and location of the cervical fibroid/myomas, the doctor may perform one of three procedures.
Drug therapy may be an option for some women with fibroids/myomas. Heavy bleeding and painful menstrual cycle caused by fibroids/myomas may be controlled with medications. They may not prevent the growth of cervical myomas. Surgery may not be avoidable. Drug treatment for fibroids includes the following options:
Birth control pills (oral contraceptives) and other types of hormonal birth control methods: These drugs often are used to control heavy bleeding and painful periods.
Gonadotropin-releasing hormone (GnRH) agonists: These drugs stop the menstrual cycle and can shrink fibroids. They sometimes are used before surgery to reduce the risk of bleeding.
Progestin intrauterine device (IUD): An option for women with myomas that does not distort the inside of the uterus. It reduces heavy and painful bleeding. The medication does not treat the myomas.
Laparoscopy
A procedure in which the surgeon conducts the operation through one or more tiny incisions near the belly button. A thin, flexible, lighted instrument, called a laparoscope, helps the doctor to see the surgical site.
Laparotomy
It is an open surgical procedure in which the surgeon removes the myomas through a larger abdominal incision.
Hysterectomy
Complete surgical removal of the uterus and sometimes the ovaries. If the fibroids are very large, this may be the surgeon’s only option. After a hysterectomy, the female patient can no longer become pregnant.
conclusion:
These are the fibroids that are present in the cervix and different factors like hormonal imbalance or family history might be the cause. Anemia and pain in the abdomen are the common symptoms. The basic treatment is myomectomy, in some cases, mediation is used. Treatments like laparoscopy, laparotomy, and hysterectomy are surgical procedures to remove fibroids.
0 notes