#hysteroscopy
Text
What are complications of hysteroscopy?
Hysteroscopy is a medical procedure that involves examining the inside of the uterus using a thin, lighted tube called a hysteroscope. It is commonly used for diagnostic and therapeutic purposes. While hysteroscopy is generally considered safe, like any medical procedure, it carries some risks and potential complications. These complications may include:
Infection: There is a risk of infection anytime an instrument is introduced into the body. However, the risk is relatively low with hysteroscopy. Antibiotics are sometimes prescribed before the procedure to minimize this risk.
Bleeding: Some degree of bleeding is normal after a hysteroscopy, but excessive bleeding can occur in rare cases. Women who are prone to bleeding disorders may be at a higher risk.
Perforation: There is a small risk of perforating the uterus or damaging other pelvic organs during the procedure. Perforation may require additional surgery to repair.
Fluid overload: During hysteroscopy, a liquid or gas may be used to expand the uterus for better visibility. In rare cases, the absorption of excessive fluid can lead to fluid overload, which may cause complications such as electrolyte imbalance or respiratory distress.
Allergic reaction: Some individuals may have an allergic reaction to medications or substances used during the procedure, such as anesthesia or the fluids used to expand the uterus.
Adverse reaction to anesthesia: If general anesthesia or sedation is used, there is a risk of complications related to the anesthesia, such as respiratory problems or allergic reactions.
Persistent pain: Some women may experience persistent pelvic pain or discomfort after the procedure.
Fertility issues: In rare cases, hysteroscopy may cause scarring or other damage to the uterine lining, potentially affecting fertility.
#best hospital#hysteroscopy#best hysteroscopy treatment in hyderabad#best gynecologist in india#top gynecologist in hyderabad
2 notes
·
View notes
Text
Recovering from my hysteroscopy! Everything went well, and I slept a lot yesterday and some more today 😴
I’m going to explain what to expect / how things went for me under the read more because I could NOT find any information other than absolute pain and it terrified me. Spoiler alert, it was not painful!
So for reference I live in Canada, and I had access to anesthesia both local and general ( I was sedated? (is that the word? half-asleep I guess) and they numbed my cervix). I cannot tell how the experience would be without anesthesia but definitely ask for it if you can. Also, if you receive medication make sure to have someone you can trust to be with you because I promise you you’ll be knocked out lmao (don’t drive seriously I could barely hold myself on my legs hospital drugs don’t fuck around)
For the preparation, you just need to be on an empty stomach for the procedure. Mine was done in the morning so I could eat when I got out. They ask routine questions and explain the procedure to you. I was also asked for a urine sample because they must do a pregnancy test. Then, they will put a catheter in your arm in order to administrate the sedation so if you are skirmish with needles like I am, request to lie down tho it is usually done in on the stretcher? hospital bed? so you should be fine.
Then, they carry you in the operation room. You’ll be seated like during a gynecological exam, with your legs up. They let you keep your blankets however. Now, I was nervous then so I had a panic attack but the staff was really nice and held my hand as the nurse administrated the medication. I don’t remember a thing from there and I woke up back in my room.
They let you wake up and gave me apple juice. I did not feel any pain at all. Be aware that there might be blood, and you may be bleeding (very light bleeding / spotting) for a few hours, especially if they removed polyps and/or fibroids). I was free to go pretty fast soon after, overall my appointment was at 8h30 in the morning and I was home by 10h. I slept all day however, make sure you get one or two days to rest depending on your ability to recover.
After the medication wore off, I could feel some cramps just like period cramps, but nothing I could not handle. I would suggest to take it slow and don’t make sudden move or exercise because it might be painful. I personally had my heated pad and it worked like a charm. You may also feel faint and weak, drink plenty of fluids and relax as much as you can. I personally didn't know how it would go so I took 2 days off work and its perfect. Follow your doctor recommendations! Mine were: for the next 3 days shower only (no baths) and nothing inserted in the vagina for 7 days (no sex, no diva cut/tampons, etc.) and that’s all!
Hopefully this helps someone out there ;v;)/ courage, take a deep breath, it’ll be okay 💕
3 notes
·
View notes
Text
OMMG i got to see a real cannulated resection hysteroscope i love you womens center
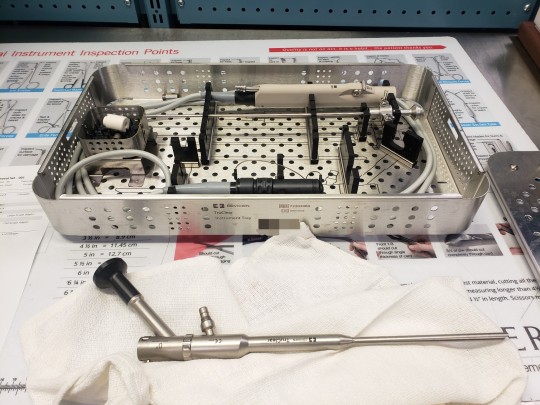
#blind abortions are cringe we're all about visual abortions and miscarriage tissue removals around here btw#surgical instruments#ignore the white adapter in the pan whoever did this up before me was an idiot#hysteroscopy#sterile processing
3 notes
·
View notes
Text
The Advantages of HYSTEROSCOPY
No incisions
Accurate diagnosis
Swift recovery
Targeted treatment
Consult Now
Visit - https://www.drgayatrigynaecologist.com
Location - https://maps.app.goo.gl/XBdy5beCLPqfHvYZ8
Follow us on
Facebook: https://www.facebook.com/drgayatrikarsoni/
Twitter: https://twitter.com/DrGayatrikar
Instagram: https://www.instagram.com/drgayatrigynecologist/
Linkedin: https://www.linkedin.com/in/dr-gayatri-kar-soni-01b9932b6/
#Hysteroscopy#NoIncisions#AccurateDiagnosis#SwiftRecovery#TargetedTreatment#MinimallyInvasive#WomensHealth#Gynecology#AdvancedDiagnostics#QuickRecovery#PrecisionMedicine#ReproductiveHealth
0 notes
Text
Hysteroscopy: Your Inner Uterus, Unveiled!

Ever wondered what goes on inside your amazing uterus? A Hysteroscopy lets you take a peek! It's a minimally invasive procedure that uses a nifty tool called a hysteroscope to examine the inside of your uterus.
Think of the hysteroscope as a super-skinny camera on a stick. Imagine it – it's inserted through your vagina and cervix, giving your doctor a clear view of the uterine lining. Here's why a hysteroscopy might be on the menu:
Diagnosis Detective: Having abnormal uterine bleeding? Unexplained pelvic pain? A hysteroscopy can help identify the culprit, whether it's fibroids, polyps, or scar tissue.
Fix-It Mission: Not just for looking, a hysteroscopy can also be used for minor surgical procedures. This tool helps remove small fibroids, take tissue samples for tests, or fix uterine malfunctions. This tool is used in such procedures.
Key things to remember:
It's usually an outpatient procedure, meaning you go home the same day.
Recovery is quick, though you might experience some cramping or spotting.
️ Talk to your doctor to see if a hysteroscopy is right for you.
Hysteroscopy – a helpful tool for diagnosing and treating uterine concerns!
Read More - https://crystaivf.com/blogs/hysteroscopy-in-hindi/
0 notes
Text
Just got out of having a hysteroscopy.
Not. Fun.
1 note
·
View note
Text

Diagnosis of uterine fibroids:
To diagnose uterine fibroids, a thorough evaluation begins with a detailed medical history and pelvic examination. Imaging techniques like transvaginal ultrasound, MRI, or CT scans are utilized to visualize the fibroids' size, number, and location. Additional procedures like hysteroscopy or biopsy might be necessary to confirm the diagnosis and rule out other conditions like endometrial cancer.
Treatment Options:
Tailored to individual needs, treatment options for uterine fibroids consider factors such as symptom severity, fertility desires, and overall health. Options include:
1. Observation: For small, asymptomatic fibroids or those nearing menopause, a watchful waiting approach involving regular monitoring without intervention may be recommended.
2. Medications: Hormonal medications like GnRHa, birth control pills, or progestin-releasing IUDs can alleviate symptoms such as heavy bleeding and pelvic pain. NSAIDs may also be used for pain relief.
3. Minimally invasive procedures: Techniques like UAE, myomectomy (performed through open surgery, laparoscopy, or hysteroscopy), and endometrial ablation are available to treat fibroids while preserving the uterus.
4. Surgery: In severe cases where conservative measures fail, hysterectomy (total, subtotal, or radical) may be advised as a definitive treatment.
Impact on Women:
Living with uterine fibroids can significantly affect a woman's physical, emotional, and social well-being. Chronic symptoms like pelvic pain and excessive bleeding can disrupt daily life and work performance. Uncertainty regarding fertility and pregnancy outcomes can lead to anxiety and depression. Financial burdens may also arise from medical costs and lost wages due to missed workdays.
Doctors suggest undergoing a regular full body health checkup for the early detection and management of conditions like uterine fibroids.
#uterine fibroids#pelvic pain#excessive menstrual bleeding#medical history#pelvic examination#transvaginal ultrasound#CT scans#MRI scans#hysteroscopy#biopsy#endometrial cancer#menopause#myomectomy#full body health checkup#regular health checkups
0 notes
Text
#Hysteroscopy#Types of Hysteroscopies#Best Gynecologist in Chennai#Gynecologist in Chennai#kauvery hospital#healthcare#healthy#healthcare blog#healthcare news
0 notes
Text

Hands-On Laparoscopic Training Centre the medicity
In the realm of modern medicine, technological advancements have revolutionized surgical procedures, making them more precise, minimally invasive, and patient-friendly. One such groundbreaking innovation is the advent of laparoscopic surgery. Laparoscopy, also known as minimally invasive surgery, has redefined surgical practices by utilizing small incisions and specialized instruments, offering patients quicker recovery times, reduced pain, and minimal scarring.
At the forefront of laparoscopic training stands The Medicity, a pioneering institution dedicated to providing hands-on laparoscopic training to medical professionals. This cutting-edge training center boasts state-of-the-art facilities and an expert team committed to equipping surgeons with the skills necessary to excel in this specialized field.
The Medicity: A Hub of Laparoscopic Excellence
Located in the heart of innovation, The Medicity stands as a beacon of excellence in laparoscopic training. Its curriculum is meticulously crafted to blend theoretical knowledge with practical expertise, ensuring that participants gain a comprehensive understanding of laparoscopic procedures.
State-of-the-Art Training Facilities
The Medicity houses advanced training facilities equipped with the latest laparoscopic equipment and simulators. These facilities simulate real surgical environments, providing trainees with hands-on experience that bridges the gap between theory and practice. Participants have access to cutting-edge tools and technology, allowing them to hone their skills under the guidance of experienced mentors.
Comprehensive Curriculum
The curriculum at The Medicity covers a wide array of laparoscopic procedures across various specialties, including but not limited to general surgery, gynecology, urology, and bariatric surgery. Trainees undergo a structured learning program that encompasses didactic lectures, live surgical demonstrations, and extensive hands-on practice sessions. This holistic approach ensures that participants gain a thorough understanding of laparoscopic techniques and procedures.
Expert Faculty and Mentorship
The success of The Medicity's training programs is attributed to its esteemed faculty comprising seasoned surgeons and experts in the field of laparoscopy. These mentors bring a wealth of practical experience and theoretical knowledge, guiding participants through every step of their learning journey. Their mentorship plays a pivotal role in shaping competent and confident laparoscopic surgeons.
Empowering Future Healthcare Professionals
The impact of laparoscopic surgery on patient outcomes cannot be overstated. By providing comprehensive training, The Medicity empowers healthcare professionals to adopt innovative surgical techniques that benefit patients by reducing postoperative complications, minimizing hospital stays, and accelerating recovery times.
Conclusion
The Medicity's Hands-On Laparoscopic Training Centre is a testament to the institution's commitment to advancing medical education and enhancing patient care. Through its state-of-the-art facilities, comprehensive curriculum, and expert faculty, it continues to shape the future of laparoscopic surgery, preparing a cadre of skilled surgeons to meet the evolving needs of the healthcare industry.
1 note
·
View note
Text
Hysteroscopy Treatment/ Services in Pune| Ashakiran Hospital
The technique of hysteroscopy enables your doctor to examine the internal of your uterus in order to identify and address the causes of atypical bleeding. Ashakiran Hospital in Narayanpeth Pune is renowned for providing the best Hysteroscopy Treatment in Pune. The hospital has been provided with modern technology and qualified hysteroscopy specialists that guarantee patients receive top-notch medical care.
#Hysteroscopy#Hysteroscopy cost in pune#Hysteroscopy Treatment in Pune#Hysteroscopy Services in Pune#Hysteroscopy cost in Baner#Hysteroscopy cost in Deccan#Hysteroscopy cost in Narayanpeth
0 notes
Text
Can Hysteroscopy Treat Asherman's Syndrome?

Yes, hysteroscopy is a commonly used and effective treatment for Asherman's Syndrome. Asherman's Syndrome, also known as intrauterine adhesions, involves the formation of scar tissue inside the uterus, often resulting from previous uterine surgeries, infections, or other trauma. Hysteroscopy is a minimally invasive surgical procedure that allows direct visualization of the uterine cavity using a thin, lighted tube called a hysteroscope.
Key points about hysteroscopy for Asherman's Syndrome treatment:
1-Identification and Assessment:
Hysteroscopy enables the surgeon to identify and assess the extent of intrauterine adhesions. The hysteroscope is inserted through the cervix into the uterus, providing a clear view of the uterine lining.
2-Adhesion Removal:
The surgeon can use specialized instruments through the hysteroscope to precisely cut or lyse (break) the adhesions. This aims to restore the normal architecture of the uterine cavity.
3-Minimally Invasive Nature:
Hysteroscopy is minimally invasive, meaning it is performed without the need for abdominal incisions. This results in less postoperative pain, a shorter recovery time, and reduced risk of complications compared to traditional open surgery.
4-Improved Uterine Cavity:
Successful hysteroscopic treatment improves the structure of the uterine cavity, creating a more favorable environment for embryo implantation and pregnancy.
5-Enhanced Fertility:
For women experiencing fertility issues due to Asherman's Syndrome, hysteroscopic treatment can enhance fertility by addressing the underlying cause of intrauterine adhesions.
6-Postoperative Care:
Following the procedure, postoperative care may involve hormonal therapy to promote endometrial regrowth and prevent the recurrence of adhesions. Close monitoring and follow-up are essential.
While hysteroscopy is a valuable and often successful treatment for Asherman's Syndrome, the degree of success can vary based on factors such as the severity of adhesions and individual patient characteristics. It's important for individuals considering this treatment to have a thorough discussion with their healthcare providers to understand the potential benefits, risks, and postoperative care requirements.
For more information, consult Dr. Neha Lalla one of the Best Gynecologist in Dubai or you can contact us on 97142122599.
#gynaecologist in dubai#best indian gynaecologist in dubai#dr. neha lalla#gynecologist#best indian gynaecologist in dubai.#Hysteroscopy#Asherman's Syndrome#Finding the Best Gynecologist in Dubai
0 notes
Text
Medcy IVF - Leading Fertility Clinic In AP And Telangana

Embark on Your Journey to Parenthood with the Medcy IVF clinic. With our advanced fertility treatments and compassionate care, we help you achieve your dream.
#ivf center near me#ivf center#fertility clinic near me#fertility center near me#the fertility clinic#fertility center#near me ivf center#ivf near me#best ivf center near me#best fertility hospitals in vijayawada#best ivf center in vijayawada#best fertility clinic near me#ivf centers in vijayawada#laparoscopic surgery#hysteroscopy#ivf#ivf treatment#iui treatment#iui treatment cost#embryo vitrification#myomectomy#myomectomy surgery#vitrification#assisted hatchng#semen bank#egg donation#oocyte donation#preimplantation genetic screening#fertility enhancing surgery#ovarian drilling
1 note
·
View note
Text
Diagnostic Hysteroscopy

Introduction
Hysteroscopy is a medical procedure that has revolutionized the field of gynecology and women's health. It allows doctors to visualize the inside of the uterus and diagnose various uterine conditions and abnormalities. In this blog post, we will explore the ins and outs of diagnostic hysteroscopy, its purpose, the procedure itself, and what to expect during and after the examination.
What Is Diagnostic Hysteroscopy?
Diagnostic hysteroscopy is a minimally invasive procedure used by gynecologists to examine the inside of a woman's uterus. It is typically recommended when a patient presents with certain symptoms or conditions that require a closer look at the uterine cavity. This procedure helps diagnose and identify issues such as abnormal bleeding, recurrent miscarriages, pelvic pain, or unexplained infertility.
The Purpose of Diagnostic Hysteroscopy
Identifying Uterine Abnormalities: One of the primary purposes of diagnostic hysteroscopy is to identify structural abnormalities within the uterus. These can include polyps, fibroids, septums, adhesions, or abnormal tissue growth that may be causing symptoms or fertility problems.
Investigating Unexplained Symptoms: Women who experience abnormal uterine bleeding, pelvic pain, or recurrent miscarriages may undergo hysteroscopy to determine the underlying cause of these symptoms.
Assessing Fertility Issues: In cases of unexplained infertility, hysteroscopy can be a valuable tool to examine the uterine cavity for any issues that could affect a woman's ability to conceive and carry a pregnancy to term.
The Diagnostic Hysteroscopy Procedure
Preparation: Before the procedure, patients may receive general or local anesthesia, depending on their comfort level and the doctor's recommendation. Anesthesia ensures that the patient is comfortable and pain-free during the examination.
Insertion of Hysteroscope: A hysteroscope is a thin, flexible tube with a light and camera at the tip. It is gently inserted into the vagina and guided through the cervix into the uterine cavity. The camera allows the doctor to visualize the uterine walls and the structures inside.
Visualization and Diagnosis: The doctor carefully examines the uterine lining and any abnormalities or issues are identified and documented. This real-time visualization is crucial for an accurate diagnosis.
Treatment If Necessary: In some cases, diagnostic hysteroscopy can transition into operative hysteroscopy if the doctor needs to remove or treat any identified issues, such as polyps or fibroids. This is typically done during the same procedure.
What to Expect During and After the Procedure
During the procedure, patients may experience some discomfort or mild cramping. However, anesthesia helps manage any pain, and the discomfort is usually minimal. The procedure itself typically takes about 20-30 minutes, although this can vary depending on the complexity of the case.
After the procedure, patients may experience some mild spotting or discharge for a few days. They can usually return to their normal activities within a day or two. Doctors may provide specific post-procedure instructions to ensure a smooth recovery.
Potential Benefits and Risks of Diagnostic Hysteroscopy
Before undergoing a diagnostic hysteroscopy, it's essential to understand both the potential benefits and risks associated with the procedure:
Benefits:
Accurate Diagnosis: Diagnostic hysteroscopy provides a direct view of the uterine cavity, allowing for precise diagnosis of uterine abnormalities, which might otherwise go undetected through other imaging methods.
Minimally Invasive: Compared to traditional open surgery, hysteroscopy is minimally invasive. This means smaller incisions, reduced pain, and quicker recovery times.
Treatment in the Same Session: If an issue is identified during the diagnostic hysteroscopy, it can often be addressed immediately, eliminating the need for a separate surgical procedure.
Risks:
Infection: As with any medical procedure, there is a minimal risk of infection, particularly if the instruments used are not properly sterilized. This risk is relatively low but should be discussed with your healthcare provider.
Bleeding: Some women may experience minor bleeding or spotting after the procedure. This is usually temporary and resolves on its own.
Uterine Perforation: In rare cases, the hysteroscope could accidentally puncture the uterine wall. This risk is minimized by the skill and experience of the healthcare provider.
Adverse Reaction to Anesthesia: While rare, adverse reactions to anesthesia can occur. Patients should discuss their medical history and any concerns with their healthcare provider before the procedure.
Failed Procedure: In some instances, it may not be possible to complete the hysteroscopy due to anatomical issues or other factors. In such cases, alternative diagnostic methods may be necessary.
Before undergoing a diagnostic hysteroscopy, your healthcare provider will discuss these potential risks and benefits with you, taking into consideration your individual health status and the reasons for the procedure. It's important to ask any questions or express any concerns you may have during this discussion to ensure you are well-informed and comfortable with the decision.
In conclusion, diagnostic hysteroscopy is a valuable diagnostic tool in gynecology that allows for the direct visualization of the uterine cavity. It is a relatively safe and minimally invasive procedure that can provide essential information for diagnosing and addressing various uterine conditions and reproductive health issues. If recommended by your healthcare provider, don't hesitate to undergo this procedure to gain clarity about your reproductive health and potentially receive timely treatment if needed. Always follow your doctor's guidance and post-procedure care instructions for the best possible outcome.
Follow-Up and Care after Diagnostic Hysteroscopy
After undergoing a diagnostic hysteroscopy, it's crucial to follow specific care instructions to ensure a smooth recovery and optimal results. Here are some essential post-procedure considerations:
Rest and Recovery: You may experience mild discomfort, cramping, or spotting after the procedure. Plan to rest for the remainder of the day, and consider taking over-the-counter pain relievers as recommended by your healthcare provider.
Avoid Certain Activities: Your doctor will likely advise you to abstain from sexual intercourse, tampon use, and strenuous activities for a specific period after the procedure, typically for about a week. This helps prevent infection and reduces the risk of complications.
Monitor for Complications: While complications are rare, it's essential to be vigilant about any unusual symptoms. Contact your healthcare provider immediately if you experience severe pain, heavy bleeding, fever, or any signs of infection.
Follow-Up Appointments: Depending on the findings of the hysteroscopy, your doctor may schedule a follow-up appointment to discuss the results, potential treatment options, or any additional steps that may be necessary.
Birth Control: If you are not trying to conceive, discuss birth control options with your healthcare provider, as some treatments that may follow diagnostic hysteroscopy could affect fertility or pregnancy.
Healthy Lifestyle: Maintain a healthy lifestyle with a balanced diet and regular exercise. These factors can contribute to overall reproductive health.
Emotional Support: Coping with a diagnosis or treatment plan can be emotionally challenging. Seek support from loved ones or consider speaking with a mental health professional if you need emotional support during this time.
Understanding the results of your diagnostic hysteroscopy is crucial, as it will guide any further steps in your treatment journey. Your healthcare provider will discuss the findings and potential treatment options with you, tailoring the approach to your specific situation.
In some cases, treatment may involve hysteroscopic surgery to remove uterine polyps, fibroids, adhesions, or other identified issues. These procedures are generally minimally invasive, which means they come with fewer complications and a shorter recovery period compared to traditional open surgery.
In conclusion, diagnostic hysteroscopy is a valuable tool for gynecologists to assess and diagnose uterine abnormalities and reproductive health issues. It provides a clear view of the uterine cavity and allows for timely interventions when necessary. By following your healthcare provider's recommendations for post-procedure care and any subsequent treatments, you can take proactive steps towards managing and improving your reproductive health. Remember that open communication with your healthcare team is essential to address any concerns or questions you may have throughout this process.
1 note
·
View note
Text
Hysteroscopy Set Manufacturer
Hysteroscopy Set Manufacturer
Hysteroscope set is an essential part of the toolbox of any gynaecologist, hence it is always available in any of the clinics. These sets are required for gynaecologists to look into the womb of females for any complication related to the uterine problem for example to diagnose the abnormal uterine bleeding, uterine fibroids, and polyps. After continuous miscarriage, the doctors usually recommend hysteroscopy treatment. Hysteroscopy is the visual inspection inside the womb of the woman so the instruments for the procedure have been made carefully under the specified guidelines. Generally, two types of the Hysteroscopes that have been used in the medical industry worldwide which are flexible and rigid both are available in a different sizes.
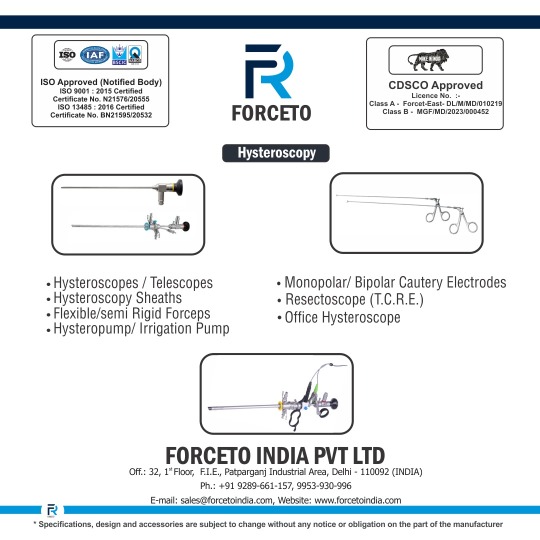
We here at Forceto India continuously develop the new products for use in hospitals, by gynaecologists and medical specialists.
Hysteroscope Telescope
Hysteroscopy Sheath
Flexible and Semi Rigid Forceps
Hysteroscopy and Irrigation Pump
Monopolar and Bipolar Cautery Electrode
Resectoscope
Office Hysteroscope
If you are searching for a Hysteroscopy Set, you can visit our website or you can call our contact no +91-92896 61157.
Reference:
Hysteroscopy Set
#health#healthcare#forcetoindia#forceto india#hospital#hospital india#health services#forceto#hysteroscopy#hysteroscopy set
0 notes