#it was an asymptomatic case fortunately
Text
rant vent idk you could call it covid defeatism
SARS-2 is why I've lost faith in the world. I truly don't know what's going to become of me since I need mutual aid as a trans person and irl friends after psychological abuse left me isolated. What does it matter if I find these if the people providing them could die within days? Who will I rely on then? Every day the "mild covid" and asymptomatic cases lies dormant is a day closer to awakening, maybe mass awakening that I can only assume will lead to national outage. Maybe it'll creep up slowly but eventually we just might lose every trucker and our food and med stock. Public transport, we already have a shortage of bus driver's to match. I don't think about moving out anymore, or getting a job, independent life while being autistic, the dreams that kept me going in my darkest moments. I think I'll die or worse, starve, before I can get there, because if the people supposed to help me get there aren't taking the pandemic seriously then I can't take them seriously. I could die in the house with the family I always dreamed of escaping, and it's simultaneously okay and not okay. I used to dream of a cinematic mass virus death, striking fear into whoever is fortunate enough to keep living, and the politicians will announce a state of emergency. But I'm not so convinced anymore. Most of all I anticipate that everything around me will just fall apart as I'm left to wonder what myself or even anyone else can do, that is if I'm "fortunate" enough to "live" to see it all slowly bleed out. I feel so truly lost and hopeless. Everything I dreamed of has gone stale before me and left out to decompose. And the people around me treat it like it's still something I can nurture.
3 notes
·
View notes
Text
Heart Defects
Heart Defects
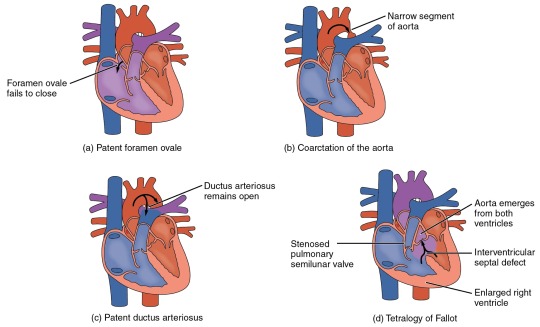
One very common form of interatrial septum pathology is patent foramen ovale, which occurs when the septum primum does not close at birth, and the fossa ovalis is unable to fuse. The word patent is from the Latin root patens for “open.” It may be benign or asymptomatic, perhaps never being diagnosed, or in extreme cases, it may require surgical repair to close the opening permanently. As much as 20–25 percent of the general population may have a patent foramen ovale, but fortunately, most have the benign, asymptomatic version. Patent foramen ovale is normally detected by auscultation of a heart murmur (an abnormal heart sound) and confirmed by imaging with an echocardiogram. Despite its prevalence in the general population, the causes of patent ovale are unknown, and there are no known risk factors. In nonlife-threatening cases, it is better to monitor the condition than to risk heart surgery to repair and seal the opening.
Coarctation of the aorta is a congenital abnormal narrowing of the aorta that is normally located at the insertion of the ligamentum arteriosum, the remnant of the fetal shunt called the ductus arteriosus. If severe, this condition drastically restricts blood flow through the primary systemic artery, which is life threatening. In some individuals, the condition may be fairly benign and not detected until later in life. Detectable symptoms in an infant include difficulty breathing, poor appetite, trouble feeding, or failure to thrive. In older individuals, symptoms include dizziness, fainting, shortness of breath, chest pain, fatigue, headache, and nosebleeds. Treatment involves surgery to resect (remove) the affected region or angioplasty to open the abnormally narrow passageway. Studies have shown that the earlier the surgery is performed, the better the chance of survival.
A patent ductus arteriosus is a congenital condition in which the ductus arteriosus fails to close. The condition may range from severe to benign. Failure of the ductus arteriosus to close results in blood flowing from the higher pressure aorta into the lower pressure pulmonary trunk. This additional fluid moving toward the lungs increases pulmonary pressure and makes respiration difficult. Symptoms include shortness of breath (dyspnea), tachycardia, enlarged heart, a widened pulse pressure, and poor weight gain in infants. Treatments include surgical closure (ligation), manual closure using platinum coils or specialized mesh inserted via the femoral artery or vein, or nonsteroidal anti-inflammatory drugs to block the synthesis of prostaglandin E2, which maintains the vessel in an open position. If untreated, the condition can result in congestive heart failure.
Septal defects are not uncommon in individuals and may be congenital or caused by various disease processes. Tetralogy of Fallot is a congenital condition that may also occur from exposure to unknown environmental factors; it occurs when there is an opening in the interventricular septum caused by blockage of the pulmonary trunk, normally at the pulmonary semilunar valve. This allows blood that is relatively low in oxygen from the right ventricle to flow into the left ventricle and mix with the blood that is relatively high in oxygen. Symptoms include a distinct heart murmur, low blood oxygen percent saturation, dyspnea or difficulty in breathing, polycythemia, broadening (clubbing) of the fingers and toes, and in children, difficulty in feeding or failure to grow and develop. It is the most common cause of cyanosis following birth. The term “tetralogy” is derived from the four components of the condition, although only three may be present in an individual patient: pulmonary infundibular stenosis (rigidity of the pulmonary valve), overriding aorta (the aorta is shifted above both ventricles), ventricular septal defect (opening), and right ventricular hypertrophy (enlargement of the right ventricle). Other heart defects may also accompany this condition, which is typically confirmed by echocardiography imaging. Tetralogy of Fallot occurs in approximately 400 out of one million live births. Normal treatment involves extensive surgical repair, including the use of stents to redirect blood flow and replacement of valves and patches to repair the septal defect, but the condition has a relatively high mortality. Survival rates are currently 75 percent during the first year of life; 60 percent by 4 years of age; 30 percent by 10 years; and 5 percent by 40 years.
In the case of severe septal defects, including both tetralogy of Fallot and patent foramen ovale, failure of the heart to develop properly can lead to a condition commonly known as a “blue baby.” Regardless of normal skin pigmentation, individuals with this condition have an insufficient supply of oxygenated blood, which leads to cyanosis, a blue or purple coloration of the skin, especially when active.
Septal defects are commonly first detected through auscultation, listening to the chest using a stethoscope. In this case, instead of hearing normal heart sounds attributed to the flow of blood and closing of heart valves, unusual heart sounds may be detected. This is often followed by medical imaging to confirm or rule out a diagnosis. In many cases, treatment may not be needed.
#atomic heart#science#biology#college#education#school#student#medicine#doctors#health#healthcare#nursing#physiology#pathology
3 notes
·
View notes
Text
Gallbladder Stone Treatment: Options and Innovations
Gallbladder stones, or gallstones, are hardened deposits of digestive fluid that can form in the gallbladder, a small organ beneath the liver. They can range in size from a grain of sand to a golf ball and can lead to significant pain and complications if not treated appropriately. Fortunately, various treatment options are available, from non-invasive methods to surgical procedures. This article will explore these treatment options, their effectiveness, and recent advancements in the field.
Understanding Gallstones
Gallstones can be classified into two types:
Cholesterol stones: These are the most common, accounting for about 80% of gallstones. They are primarily made of hardened cholesterol.
Pigment stones: These stones are smaller and darker, composed mainly of bilirubin, a substance produced from the breakdown of red blood cells.
Symptoms and Diagnosis
While some people with gallstones remain asymptomatic, others may experience:
Sudden and intense abdominal pain

Nausea and vomiting
Jaundice (yellowing of the skin and eyes)
Fever with chills (if an infection is present)
Diagnosis typically involves imaging studies such as ultrasound, CT scans, and MRIs, which can detect the presence and size of gallstones.
Treatment Options
Watchful Waiting
For asymptomatic patients, doctors often recommend a watchful waiting approach. Regular monitoring ensures that any emerging symptoms or complications can be addressed promptly.
Medications
Oral bile acid pills like ursodeoxycholic acid can help dissolve cholesterol gallstones. This treatment is usually reserved for patients who cannot undergo surgery and requires months or even years to be effective. It is most suitable for small, non-calcified stones.
Non-Surgical Procedures
Extracorporeal Shock Wave Lithotripsy (ESWL): This technique uses sound waves to break gallstones into smaller pieces that can be more easily passed or dissolved. It is rarely used today but can be an option for those who cannot have surgery.
Endoscopic Retrograde Cholangiopancreatography (ERCP): This is both a diagnostic and therapeutic procedure. It involves the insertion of an endoscope through the mouth to the small intestine to remove stones from the bile duct.
Surgery
Laparoscopic Cholecystectomy: This is the most common surgery for gallstones. It involves the removal of the gallbladder using a laparoscope, a thin tube with a camera. It is minimally invasive, has a short recovery time, and a high success rate.
Open Cholecystectomy: This traditional method involves a larger abdominal incision and is used when laparoscopic surgery is not feasible, such as in cases of severe inflammation, infection, or scar tissue from previous surgeries.

Advances in Treatment
Robotic-Assisted Surgery
Robotic systems like the da Vinci Surgical System offer greater precision, flexibility, and control than traditional methods. They enhance the surgeon’s ability to perform complex procedures with small incisions, reducing recovery time and complications.
Natural Orifice Transluminal Endoscopic Surgery (NOTES)
This innovative approach involves accessing the gallbladder through natural openings (mouth, vagina, or rectum) to perform surgery without external incisions, further minimizing recovery time and pain.
Enhanced Imaging Techniques
Advancements in imaging, such as high-definition endoscopes and improved MRI technology, allow for more accurate diagnosis and better planning of surgical interventions, reducing the risk of complications.
Lifestyle and Prevention
Preventive measures include maintaining a healthy weight, following a balanced diet low in fat and high in fiber, and regular physical activity. For those at high risk, such as individuals with a family history of gallstones, doctors may recommend more frequent monitoring and lifestyle adjustments.
Conclusion
The treatment of gallbladder stones has evolved significantly, offering patients various options based on the severity of their condition and overall health. From medications and non-surgical procedures to advanced surgical techniques, each treatment has its advantages and potential risks. Ongoing research and technological advancements continue to improve the outcomes and quality of life for those affected by gallstones. If you suspect you have gallstones or are experiencing symptoms, consult a healthcare provider to discuss the best treatment plan tailored to your needs.
#gallbladder stones#gallbladder stone treatment#gallbladder stone specialist#gallbladder surgery#gallbladder stone symptoms
0 notes
Text
Varicose Veins vs. Spider Veins: What’s the Difference?
Varicose veins and spider veins are common vascular conditions that affect millions of people worldwide, causing discomfort and aesthetic concerns. While they may seem similar at first glance, these two conditions have distinct characteristics, causes, and treatment approaches. In this informative guide, we’ll explore the differences between varicose veins and spider veins, shedding light on the nuances of each condition and the available Varicose Veins Treatment in Jaipur.
Understanding Varicose Veins
Varicose veins are enlarged, swollen, and twisted veins that typically appear blue or dark purple in color. They often develop in the legs and feet and are caused by faulty valves within the veins, which disrupt the normal flow of blood and lead to pooling. Factors such as genetics, age, obesity, pregnancy, and prolonged standing or sitting can increase the risk of developing varicose veins.
Common symptoms of varicose veins include:
Bulging, rope-like veins
Swelling in the legs or ankles
Aching or throbbing pain
Heaviness or discomfort in the legs
Itching or irritation around the affected veins
Understanding Spider Veins
Spider veins, also known as telangiectasia or thread veins, are smaller, superficial blood vessels that appear close to the skin’s surface. Unlike varicose veins, spider veins are typically red, blue, or purple in color and resemble a spider web or tree branch pattern. They can develop anywhere on the body but are most commonly found on the legs and face.
Spider veins are often associated with:
Hormonal changes (such as pregnancy or menopause)
Sun exposure
Injury or trauma to the skin
Genetics
Prolonged standing or sitting
Obesity
While spider veins are generally considered a cosmetic concern, they can sometimes cause symptoms such as itching, burning, or aching sensations.
Key Differences Between Varicose Veins and Spider Veins
Size and Appearance: Varicose veins are larger, bulging veins that may protrude from the skin’s surface and have a twisted or rope-like appearance. In contrast, spider veins are smaller, fine blood vessels that appear closer to the skin’s surface and often form a branching or spider web pattern.
Location: Varicose veins typically develop in the legs and feet, where the pressure on veins is higher due to gravity. Spider veins can occur anywhere on the body but are most commonly found on the legs, thighs, and face.
Symptoms: Varicose veins are more likely to cause symptoms such as pain, swelling, heaviness, or discomfort in the legs. Spider veins, on the other hand, are usually asymptomatic but may cause minor discomfort or itching in some cases.
Underlying Cause: Varicose veins are primarily caused by dysfunction of the valves within the veins, leading to impaired blood flow and pooling. Spider veins can result from various factors, including hormonal changes, sun exposure, genetics, or trauma to the skin.
Treatment Options for Varicose Veins and Spider Veins in Jaipur
Fortunately, individuals have access to a range of advanced treatment options for varicose veins and spider veins, provided by experienced Varicose Veins Doctors in Jaipur specializing in vascular health. Some common treatment modalities include:
Sclerotherapy: A minimally invasive procedure in which a special solution is injected into the affected veins, causing them to collapse and fade over time. Sclerotherapy is highly effective for treating both varicose veins and spider veins.
Endovenous Laser Ablation (EVLA): A procedure that uses laser energy to heat and seal off varicose veins, redirecting blood flow to healthier veins. EVLA is particularly suitable for larger varicose veins and offers excellent results with minimal discomfort and downtime.
Radiofrequency Ablation (RFA): Similar to EVLA, RFA involves using radiofrequency energy to heat and close varicose veins. This technique is often preferred for patients with underlying health conditions or who may not be suitable candidates for surgery.
Compression Therapy: Wearing compression stockings or socks can help improve blood circulation and alleviate symptoms associated with varicose veins and spider veins. Compression therapy is often recommended as a conservative Varicose Veins Treatment in Jaipur or as a complementary measure following vein procedures.
Laser Therapy: For spider veins, laser therapy can be an effective option for targeting and eliminating the affected blood vessels. This non-invasive treatment uses focused laser energy to heat and collapse the spider veins, gradually fading them from view.
Conclusion
In summary, while varicose veins and spider veins share some similarities, they are distinct vascular conditions with unique characteristics and causes. Understanding the key differences between varicose veins and spider veins is essential for accurate diagnosis and appropriate treatment. In Jaipur, individuals experiencing symptoms or cosmetic concerns related to varicose veins or spider veins can consult experienced Varicose Veins Doctors in Jaipur who offer a variety of advanced treatment options to restore vascular health and enhance overall well-being. If you’re dealing with varicose veins or spider veins, don’t hesitate to seek professional evaluation and personalized care to achieve optimal results and regain confidence in your appearance and comfort.
0 notes
Text
Debunking myths about gallbladder stones

The gallbladder — an unsung hero in our digestive system — often goes unnoticed until something goes wrong. In this blog, doctors at Vedam Gastro Hospital, one of the best gastro hospitals in Surat guide us in understanding gallstones — those tiny, yet mighty, crystalline deposits causing significant discomfort in the abdomen and help in debunking the myths that cloud our understanding of this vital organ’s issues.
Myth 1: Only the Elderly Get Gallstones
Contrary to popular belief, gallstones aren’t exclusive to the elderly. While age increases the likelihood, even younger individuals can develop them due to various factors, including diet, genetics, obesity, and rapid weight loss.
Myth 2: Gallstones Only Cause Pain
Yes, gallstones are notorious for causing intense pain, known as biliary colic. However, their impact extends beyond discomfort. If a stone blocks the bile duct, it can lead to complications like cholecystitis (inflammation of the gallbladder), pancreatitis (inflammation of the pancreas), or jaundice.
Myth 3: Removing the Gallbladder Disrupts Digestion
A very senior Gastroenterologist at Vedam Gastro Hospital explains that the gallbladder’s primary function is to store and concentrate bile produced by the liver, aiding fat digestion. After gallbladder removal (cholecystectomy), bile drips continuously into the intestine, facilitating digestion. While some individuals may experience mild digestive changes post-surgery, most adapt without major disruptions.
Myth 4: Diet Doesn’t Affect Gallstones
High-cholesterol and high-fat diets are culprits in gallstone formation. Excessive intake of saturated fats prompts the liver to excrete more cholesterol into bile, leading to imbalances that form gallstones. Conversely, diets rich in fibre, vegetables, fruits, and healthy fats can help prevent gallstones.
Diet significantly influences gallstone development. Choosing a balanced diet, moderating fat intake, focusing on healthy fats, and maintaining a healthy weight are key factors in reducing the risk of gallstones. While diet isn’t the sole factor, it is a crucial player in the prevention of gallstone formation and supports overall gallbladder health.
Myth 5: All Gallstones Need Immediate Treatment
Not all gallstones warrant immediate action. Asymptomatic gallstones, found incidentally during medical tests for unrelated issues, may not require treatment. However, in case of severe pain or discomfort, medical intervention is necessary to prevent further complications.
Myth 6: Medication Dissolves Gallstones Completely
Medication for gallstones aims to dissolve cholesterol-based stones over time by altering bile composition. Ursodeoxycholic acid (UDCA) is a common medication used for this purpose. It works by reducing the cholesterol content in bile, gradually dissolving small cholesterol stones over several months to years. However, this approach has limitations. It’s effective mainly for small, cholesterol-based stones and may take a long duration to work. Not all stones respond to medication, particularly larger or pigment stones. Additionally, there’s a risk of stone recurrence once treatment stops. Close monitoring and adherence to the prescribed regimen are crucial. While medication can be an option for certain cases, surgical intervention remains the primary treatment for symptomatic or larger gallstones that don’t respond to medication.
Myth 7: Gallstones Only Require Surgical Treatment
Dr. Ronak Malani, a senior gastro surgeon at one of the best stomach hospitals in Surat, confirms that alternative treatments, such as shock wave lithotripsy (using shock waves to break up stones) can be opted for in cases where surgery isn’t possible for a patient.
Myth 8: Pregnancy Doesn’t Influence Gallstones
Pregnancy significantly increases the risk of gallstones due to hormonal changes that affect how the gallbladder functions. The risk persists during the postpartum period. Fortunately, most gallstones discovered during pregnancy remain asymptomatic and may not require immediate action.
Myth 9: All Symptoms Point to Gallstones
Gallstone symptoms, like abdominal pain, nausea, and vomiting, overlap with various digestive issues. However, not all abdominal discomfort stems from gallstones. A thorough examination by a healthcare professional is essential for an accurate diagnosis.
Myth 10: Once Gallstones Are Removed, They Won’t Return
Dr. Pravin Borasadia, one of the best stomach specialists in Surat, says that in rare cases recurrence is possible even after gallstone removal. Lifestyle modifications, including dietary changes and maintaining a healthy weight, can significantly reduce the likelihood of their reappearance.
In Brief:
Debunking the myths surrounding gallstones is crucial for a better understanding of their nature, prevention, and treatment. While some misconceptions exist, awareness, lifestyle modifications, and timely medical intervention remain our best defences against gallbladder issues. Consultation with the best healthcare professionals helps navigate these myths, ensuring accurate information and appropriate management of gallstone-related concerns.
0 notes
Text
An Introduction to Dental Bone Spurs
Bony growths on the teeth, gums, or jawbone are known as dental bone spurs. They can be unpleasant and uncomfortable, making everyday tasks such as eating, drinking, and speaking difficult. Fortunately, there are a variety of therapies available to assist manage and alleviate the pain produced by dental bone spurs. This page will go through the causes, side effects, identification, and therapies that are available.

What exactly are dental bone spurs?
Tori, or dental bone spurs, are benign bony growths that can form in the mouth, most usually on the palate (the roof of the mouth) or the lower jaw (the mandible). They are typically asymptomatic and can be of various sizes and shapes.
How Do You Spot Dental Spurs?
Tori are frequently detected during routine dental examinations or through radiographic imaging. Here are some pointers to help you figure it out.
They are mainly distinguishable by their location and appearance.
They frequently develop on the tongue side of the lower jaw or along the palate of the upper jaw.
These growths resemble little, spherical bone lumps that might vary in size.
When handled, they feel firm and bony, similar to the surrounding bones.
Dental bone spurs are usually asymptomatic, but if they cause pain or interfere with oral function, consult a dentist for a proper diagnosis and treatment options.
What is the cause of dental bone spurs?
Dental bone spurs can develop for a variety of reasons. The following are some of the factors that may contribute to the formation of dental bone spurs:
Genetics
Bite and tooth misalignment Bruxism (teeth grinding or clenching)
Age
Trauma
Habits of the Mouth
Irritation that lasts a long time
Dental bone spurs vary in size and location, and not all of them require treatment. If you have any concerns, see a dentist or oral surgeon for an evaluation and treatment options.
What dental treatment is available for dental spurs?
In most cases, it will vanish on its own. If they are causing significant problems, your dentist may recommend one of the following treatments:
Alveoloplasty
This is a surgical procedure used to smooth the jawbone edges after the tooth was extracted. This can help to keep bone spurs at bay.
Surgical removal of a bone spur
A minimally invasive approach is utilized to remove the bone spur. It is usually performed under local anesthesia.
Antibiotics
If the bone spur becomes infected, your dentist may prescribe antibiotics to you.
Pain killers
Pain and inflammation can be relieved with over-the-counter pain medications such as ibuprofen or acetaminophen.
Conclusion
In conclusion, Because of heredity, habits, biting irregularities, and age, it causes discomfort or difficulties in oral tasks. Fortunately, serious health problems caused by oral bone spurs are rare. If you have dental bone spurs that cause you pain or interfere with your oral health, you should seek professional assistance. A dentist can evaluate the situation, give management recommendations, and ensure that your dental health is emphasized. Dental bone spurs can be effectively treated in most cases with the proper guidance and care, allowing you to maintain a healthy and comfortable smile.
To get full details, read the full blog : https://www.dramarnathansdentalcare.com/an-overview-of-dental-bone-spurs/
For More Tips & Details Visit
Website : https://www.dramarnathansdentalcare.com/
Facebook : https://www.facebook.com/people/DrAmarnathans-Dental-Care/100063667464980/
Twitter : https://twitter.com/dramarnathan
Instagram : https://www.instagram.com/dr_amarnathans_dental/
#Dental Bone Spurs#tori#dental#dentistry#tori amos#tori spring#dental treatment#dental treatment for bone spurs#bony growth#mouth bony growth#bone spurs#dental health#dental care#oralcare
0 notes
Text
A Stress-Free Solution to Avoiding a COVID Spread- Same Day Results Covid Testing
Living in the era of COVID-19 pandemic has brought about new rules, regulations, and safety measures that we must adopt in our personal lives and working environments. One of the vital tools we can use is getting tested for COVID-19. Testing is essential in helping to regulate the outbreak of the virus. However, waiting for test results can be one of the most anxiety-inducing moments in the process. Fortunately, same-day results Covid testing in Chicago has recently become accessible to solve that problem, making the diagnosis process quicker, easier, and stress-free for people.

Same-Day Results Covid Testing Explained
Same-day results COVID testing is a revolutionary diagnostic technique that has recently gained tremendous popularity. The process involves employing sophisticated molecular biology methods to spot the presence of the SARS-CoV-2 virus, which triggers the infection. This highly effective testing approach can provide exact results in hours, making testing more accessible and efficient.
Such testing relies on a complex process that involves high-tech laboratory equipment and a team of skilled professionals. The polymerase chain reaction (PCR) technique is at the center of this process, which efficiently amplifies small snippets of the virus's genetic material to facilitate its identification. This process of detection is so sophisticated that it can identify even the tiniest traces of the virus, making it an excellent tool for spotting asymptomatic carriers.
The speed at which it delivers the diagnosis results makes same-day results COVID testing even more effective and sought-after. Unlike traditional COVID-19 testing methods that require samples to be sent to laboratories for assessment, same-day results COVID testing can provide results on the spot. It is particularly useful for people who must travel or attend events requiring medical clearance certificates.
The availability of same-day results COVID testing has also revolutionized the healthcare industry, especially in the fight against the pandemic. With this technique, hospital emergency departments can quickly screen patients for COVID-19, reducing the waiting time for results and improving the overall efficiency of the healthcare system. Additionally, businesses and schools can use this approach to screen employees and students, ensuring everyone is safe and healthy.
Benefits of Same-Day Results Covid Testing
The main advantage of same-day Covid testing is quick results, which frees an individual from the anxiety of waiting for the results. The prompt test results help individuals self-isolate immediately if they test positive or return to work if they test negative, ensuring that everyone surrounding them is much safer. This quick and stress-free testing method also ensures that more people get tested and get their results, reducing the spread of the virus.
Convenience of Same-Day Results Covid Testing
Same-day results Covid testing is also incredibly convenient. Testing centres and facilities with same-day results are set up all over the U.S.A., which helps people get tested more quickly and easily. At-home testing lets individuals get tested with a simple sample collection without needing a clinic visit. Test results are delivered via phone or email in just a few hours or less, making it easy for individuals to self-isolate if necessary.
Cost of Same-Day Results Covid Testing
The cost of the testing varies from provider to provider and facility to facility. In most cases, health insurance plans will cover the cost of testing, including same-day results. In the U.S.A., the CARES Act requires that most insurance plans include COVID-19 testing without coinsurance or copays. At-home tests may not be deeply discounted, but insurance companies may cover the costs mostly.
Same-day results from Covid tests have transformed the way we test for COVID-19. Not only is the testing process quicker and less stressful, but it is also more accessible and efficient. These tests are a game-changer in the fight against the spread of COVID, allowing for the early detection of the virus, quick response, and self-isolation. It is essential to remember that same-day results Covid testing can make our lives, work, and communities safer. Contact Xpress Covid Testing to get instant and accurate results from your Covid test on the same day. The reputable facility offers same-day results covid testing in Chicago by collaborating with certified laboratories.
0 notes
Text
Hernia Treatment
Hernias are a common health problem that affects millions of people every year. They occur when an organ or tissue protrudes through a weak spot in the muscle or connective tissue. Hernias can be very painful and can cause other complications if left untreated. Fortunately, there are several effective treatments available for hernias in Miami, FL. In this blog post, we will explore some of the most common hernia treatments in Miami and discuss how to choose the right treatment for you.
Types of hernias
Before we dive into the treatment options, let's take a quick look at the different types of hernias.
Inguinal hernia: This is the most common type of hernia and occurs when the intestine or bladder protrudes through the inguinal canal in the groin area.
Hiatal hernia: This type of hernia occurs when part of the stomach protrudes through the diaphragm and into the chest.
Umbilical hernia: This type of hernia occurs when the intestine or abdominal tissue protrudes through a weak spot near the belly button.
Incisional hernia: This type of hernia occurs at the site of a previous surgical incision, where the muscle tissue may be weaker.
Hernia Treatment Options in Miami
Watchful Waiting: For small, asymptomatic hernias, watchful waiting may be an option. This means monitoring the hernia with regular check-ups to ensure that it doesn't get worse or cause any complications.
Lifestyle Changes: In some cases, lifestyle changes such as losing weight or avoiding heavy lifting may be enough to manage the symptoms of a hernia.
Medications: If the hernia is causing discomfort or pain, over-the-counter pain relievers such as ibuprofen or acetaminophen may be recommended.
Hernia Belt: A hernia belt is a special belt designed to support the area around the hernia and prevent it from protruding. This can be helpful in managing symptoms and preventing the hernia from getting worse.
Surgery: Surgery is the most common treatment for hernias that are causing symptoms or complications. There are two main types of hernia surgery: open surgery and laparoscopic surgery.
Open Surgery: In open surgery, the surgeon makes a large incision in the affected area to access and repair the hernia. This type of surgery is generally recommended for larger hernias or hernias that have recurred after a previous surgery.
Laparoscopic Surgery: In laparoscopic surgery, the surgeon makes several small incisions in the abdomen and uses a small camera and specialized surgical instruments to repair the hernia. This type of surgery is generally recommended for smaller hernias or hernias that have not recurred after a previous surgery.
Choosing the Right Hernia Treatment
Choosing the right hernia treatment depends on several factors, including the type and size of the hernia, the severity of the symptoms, and the overall health of the patient. Your doctor will work with you to determine the best treatment option for your specific needs.
If you are experiencing symptoms of a hernia, such as pain or discomfort in the affected area, it is important to seek medical attention as soon as possible. Delaying treatment can lead to complications such as obstruction or strangulation of the affected tissue, which can be life-threatening.
Conclusion
Hernias can be a painful and frustrating health problem, but with the right treatment, they can be effectively managed. If you are experiencing symptoms of a hernia, don't wait to seek medical attention. A qualified healthcare provider can help you determine the best treatment option for your needs and ensure that you receive the care you need to get back to your normal activities. With the right treatment, you can get relief.
0 notes
Text
WHAT IS A BULGING DISC AND WHAT ARE THE TOP TREATMENT OPTIONS

A bulging disc is when the soft cushioning material between the vertebrae of your spine begins to push out of the center of the disc, which can cause pain and discomfort in other parts of your body. This condition is known as a herniated or bulging disc. Depending on where it is located, a bulging disc can cause nerve impingement, back pain, neck pain, and even numbness or tingling in the arms or legs.
Fortunately, there are a variety of treatment options available for those suffering from bulging discs. Chiropractic care in Westchase is often used to help strengthen the muscles around the spine and improve the range of motion. Exercises may include stretches, core strengthening, or yoga.
WHAT IS A BULGING DISC?
A bulging disc is a medical condition that can cause severe pain and discomfort. It occurs when the vertebrae in your spine are pressed against the discs between them, causing them to bulge out of shape. Bulging discs are a common cause of back pain, especially in adults over the age of 30. A bulging disc occurs when the gel-like center of the disc pushes out between the vertebrae, causing a bulge in the disc that can put pressure on nearby nerves, causing pain, discomfort, and potentially decreased mobility. It can also occur if you have a degenerative condition such as osteoporosis or arthritis that weakens the bones in your spinal column.
SYMPTOMS OF BULGING DISC IN WESTCHASE
A bulging disc can cause several different types of symptoms depending on where it is located in your spine and what nerves are affected by the pressure. Some common symptoms include:
• Lower back pain
• Neck pain
• Tingling or numbness in limbs or other parts of the body
• Muscle weakness or stiffness in certain areas
• Difficulty bending or moving certain parts of the body
• Pain that radiates down into your legs or arms
It’s important to note that not all bulging discs will cause symptoms. In some cases, they may remain asymptomatic until they become herniated discs which require more aggressive treatment. It’s important to pay attention to how your body feels and to recognize any changes that could signal something more serious than just normal aches and pains from everyday activities.
CAUSE OF BULGING DISC IN WESTCHASE
The most common cause of a bulging disc is aging. As we get older, our bones and muscles naturally become weaker as wear and tear take their toll over time. This weakening can cause the discs between our vertebrae to not hold up as well as they once did, leading to a bulging disc.
Here are some of the cases of Bulging Discs:
Age-related Wear and Tear
As we age, our intervertebral discs naturally become weakened due to general wear and tear. This weakening can cause them to bulge outwards when too much pressure is put on them. The most common type of age-related bulging disc occurs in the lower back (lumbar region).
Injury or Trauma
Injury or trauma to the spine can also cause a disc to bulge outwards. The most common types of injuries that can lead to a bulging disc are falls, motor vehicle accidents, sports injuries (especially contact sports), and heavy lifting. In some cases, even minor incidents such as sneezing or coughing can lead to a slipped disc if there is already existing weakness in that area due to age-related wear and tear or another underlying medical condition.
Underlying Medical Conditions
Some underlying medical conditions can increase your risk of developing a bulging disc. These include obesity, osteoporosis, diabetes, rheumatoid arthritis, scoliosis, spondylolisthesis (when one vertebra slips over another), and spinal stenosis (narrowing of the spaces within your spine). If you have any of these underlying medical conditions, it’s important to talk with a chiropractic doctor at Optim Chiropractic in Westchase about ways to reduce your risk of developing a bulging disc.
Lifestyle Factors
Certain lifestyle factors can also increase your chances of developing a bulging disc. Poor diet, lack of exercise, smoking, and excessive alcohol consumption can all contribute to weak muscles that put extra strain on your spine and make it more likely for you to develop a bulging disc. Being overweight can also put extra pressure on your spine that increase your chances of developing a disc issue as well.
TOP TREATMENT OPTIONS OF BULGING DISC IN WESTCHASE
Alternative Treatments
There are alternatives to traditional medicine pharmaceutical treatments that can be used to help relieve symptoms associated with bulging discs such as acupuncture, chiropractic care, massage therapy, and yoga/stretching exercises. Chiropractors at Optim Chiropractic specialize in diagnosing and treating conditions related to the musculoskeletal system such as bulging discs.
Chiropractors use manual adjustment techniques, massage therapy, ultrasound, electric stimulation, non-surgical spinal decompression, and other treatments to help reduce pain and restore mobility in the affected area. Additionally, chiropractors may provide advice on lifestyle changes that can help prevent future issues or flare-ups.
Physical Therapy or Exercise Therapy
Physical therapy is one of the most common treatments for bulging discs. Through physical therapy, patients have access to a wide range of exercises and stretch that can help improve strength and flexibility in the affected area as well as reduce pain and discomfort. Physical therapists also educate patients on proper posture and body mechanics to help prevent future injuries or complications.
Epidural Injections
Epidural injections are another option for treating bulging discs. During an epidural injection, medicine is injected directly into the spine near the affected area to reduce inflammation and pain in that part of the body. These injections typically include steroids or anesthetic agents that work to provide immediate relief from discomfort caused by a bulging disc. While this method may not be suitable for everyone, it does offer short-term relief for those who find it helpful.
Medications
When conservative treatments like physical therapy are not enough to provide relief from a bulging disc, medications may be necessary to reduce inflammation and decrease pain levels. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce swelling and ease discomfort. In more severe cases, stronger prescription medications such as muscle relaxants or even narcotic pain relievers may be prescribed by your primary care doctor if necessary.
Hot and Cold Therapy
Hot and cold therapy can be used to treat bulging discs by reducing inflammation and providing temporary relief from pain. The heat increases blood circulation, which helps relax tight muscles in the affected area. This can reduce pressure on the disc, leading to less pain. On the other hand, applying cold compresses to the affected area can reduce swelling by constricting blood vessels. This can also help numb the area so you don’t feel any discomfort.
CHIROPRACTIC CARE IN TREATING BULGING DISC IN WESTCHASE

Chiropractic care is an effective treatment option for those suffering from bulging disc pain in Westchase. Through spinal manipulation techniques combined with lifestyle changes like exercise modifications or dietary adjustments, chiropractic doctor Dr. Mike Whitlow is able to provide relief from the discomfort associated with bulging discs as well as promote overall healing of the affected area(s).
If you’re experiencing any type of discomfort due to a bulging disc issue in Westchase and Tampa, contact us today at (813) 475-4150 to learn more about how we can help you manage your symptoms through chiropractic care!
0 notes
Text
STORY AT-A-GLANCE
The 2022 U.S. Vaccine Damage Report revealed a sobering glimpse into the true carnage that occurred at the hands of the COVID-19 shot campaign
COVID-19 shots resulted in 300,000 excess deaths, 26.6 million injuries and 1.36 million disabilities
Total economic costs due to the shots are estimated at $147.8 billion, including $89.9 billion from related injuries, $52.2 billion from disabilities and $5.6 billion from excess deaths
A preprint systematic review found the mRNA-based COVID shots increased the risk of myocarditis, with a mortality of about 1 to 2 per 200 cases
Evidence of serious neurological harms, including Bell’s palsy, Guillain-Barré syndrome, myasthenic disorder and stroke, which are likely due to an autoimmune reaction, was also found from the shots
We're beginning to see the fallout from the mass COVID-19 shot campaign, which has been referred to as the "greatest violation of medical ethics in the history of medicine, maybe humanity."1
Former BlackRock analyst and fund manager Edward Dowd is one of the few trying to get the word out about COVID-19 shot risks, and he's been using data and statistics to prove his point and publicize the undeniable increase in deaths and disability among young, healthy adults that has occurred since the shots' widespread rollout.2
This group — the 148 million employed Americans between the ages of 18 and 643 — is typically a healthy crowd. This is why private insurance companies love to sell group life insurance policies to large Fortune 500 corporations and mid-sized companies —they hardly ever have to pay out on a claim. But this is changing.
Dowd's 2022 U.S. Vaccine Damage Report4 revealed a sobering glimpse into the true carnage that occurred at the hands of the COVID-19 shot campaign, and its results are striking.
300K Excess Deaths, Millions of Injuries, Billions in Costs
Dowd and colleagues published their 2022 Vaccine Damage Project at their website, Phinance Technologies.5 It revealed the following estimated human and economic costs:6Human CostEconomic Cost
26.6 million injuries
1.36 million disabilities
300,000 excess deaths
Total: $147.8 billion
Injuries: $89.9 billion
Disabilities: $52.2 billion
Excess deaths: $5.6 billion
To put this into perspective, John Leake writes on Courageous Discourse, "Note that this death count in one year is 5.2 times the number of men killed in 10 years of combat in Vietnam," adding:7
The report included data from employed individuals between the ages of 16 and 64, and categorized the impact into four broad groups:
No effect or asymptomatic
Mild to moderate outcome including a temporary or short-term, long-term or permanent injury
Severe outcome that leads to a disability
Extreme outcome leading to death
While group 1 was the largest, comprising an estimated 82% of the population, the authors pointed out that these groups are dynamic, and individuals in one group could move into another, particularly in the case of progressing from no or minor injury to severe injury, such as we've seen with elite athletes suddenly dropping dead on the field:8
'The Multiplier Effects Are Massive'
The effects in the report are only what can currently be measured, and are likely to also be fluid. In terms of economic effects, for instance, the report notes that mortuary companies are likely to benefit while life insurers will be harmed, leading to a reallocation of resources.
Meanwhile, in terms of economic costs, milder damage is associated with greater cost, since a larger portion of working age individuals are affected. For instance, those with mild to moderate injury made up a sizeable 18% of the population. According to the report:9
Further, many other economic costs are harder to account for, such as a worker who's still at work but not able to work to their full potential. When these types of scenarios are factored in, the damages could be even more massive. Dowd tweeted:11

Download this Article Before it Disappears
Download PDF
Systematic Review Reveals Serious Harms
A preprint systematic review of papers with data on serious adverse events associated with COVID-19 shots again points to significant risks.12 The review was conducted by Maryanne Demasi, Ph.D., a former medical scientist with the University of Adelaide and former reporter for ABC News in Australia and Professor Peter Gøtzsche, a Danish physician-researcher who co-founded the Cochrane Collaboration in 1993.
It included 18 systematic reviews, 14 randomized trials and 34 other studies, noting that "most studies were of poor quality" and additional randomized trials are needed. Still, their review revealed multiple red flags, including:13
Adenovirus vector vaccines increased the risk of venous thrombosis and thrombocytopenia
mRNA-based shots increased the risk of myocarditis, with a mortality of about 1 to 2 per 200 cases
Evidence of serious neurological harms, including Bell's palsy, Guillain-Barré syndrome, myasthenic disorder and stroke, which are likely due to an autoimmune reaction, was found
Severe harms, defined as those that prevent daily activities, were underreported in the randomized trials
Severe harms were very common in studies of booster doses after a full round of shots and in a study of vaccination of previously infected people
Further, not only have drug regulators and public health authorities been slow to follow up on safety signals showing serious harms from the shots, Demasi notes, but, "Population-wide recommendations for COVID vaccination and boosters ignore the negative benefit to harm balance in low-risk groups such as children and people who have already recovered from covid-19 (natural immunity)."14
Australian Safety Report — 24-Fold Increase in Adverse Events
It's can be difficult to parse out adverse effects from COVID-19 shots and those due to COVID-19 infection. The Western Australia Vaccine Safety Surveillance (WAVSS) 2021 Report, however, shows a unique viewpoint that made this possible. At the time, there was virtually no COVID-19 circulating in the community, yet the area had a 90% vaccination rate among those 12 years and over.15 Umbrella News reported:16
So, what happened in an area of the world that had very few COVID-19 cases and very high rates of COVID-19 shots? An "exponential increase" in reports of adverse events following immunization (AEFI), such that it necessitated changes to the vaccine safety surveillance program at the department in order to manage them.17 According to the report:18
As Umbrella News reported, the peak of AEFI reports coincided with the rollout of shot mandates, culminating in a rush of hospitalizations that strained area hospitals:19
Other standouts from WA's report include a 35% increase in myocarditis and a 25% increase in pericarditis compared to background rates. "Shockingly," Umbrella News noted, "the risk of pericarditis in the age group in the age group 25 to 29 years old was 53.5 cases per 100,000 doses of Spikevax. It is perhaps unsurprising that chest pain was the fifth most common reported AEFI for COVID vaccines in 2021."20
COVID Shot Efficacy 'Grossly Overestimated'
While the risks of adverse effects have been downplayed, the efficacy of COVID-19 shots has been overstated from the beginning. Writing in the Journal of Evaluation in Clinical Practice, a research team revealed that multiple biases, including background infection rates and cross-overs from unvaccinated to vaccinated in the early days of the campaign, led to an overstatement of COVID-19 shots' effectiveness.21
"We conclude that "real-world" studies using methodologies popular in early 2021 overstate vaccine effectiveness," the study notes.22 Board-certified internist and cardiologist Dr. Peter McCullough explained that from the lack of efficacy alone, the shots should be removed from the market. And the case gets even stronger when you factor in the significant number of related disabilities and deaths:23
0 notes
Text
WHAT IS A BULGING DISC AND WHAT ARE THE TOP TREATMENT OPTIONS

A bulging disc occurs when the soft cushioning material between the vertebrae of your spine starts to push out, which can cause pain and discomfort in other parts of your body. This condition is known as a herniated or bulging disc. Depending on where it is located, a bulging disc can cause nerve impingement, back pain, neck pain, and even numbness or tingling in the arms or legs.
Fortunately, there are a variety of treatment options available for those suffering from bulging discs. Chiropractic care in Dubuque is often used to help strengthen the muscles around the spine and improve the range of motion. Exercises may include stretches, core strengthening, or yoga.
What is a Bulging Disc?
A bulging disc is a medical condition that can cause severe pain and discomfort. It occurs when the vertebrae in your spine press against the discs between them, causing them to bulge out of shape. Bulging discs are a common cause of back pain, especially in adults over the age of 30. A bulging disc occurs when the gel-like center of the disc pushes out between the vertebrae, causing a bulge that presses on nearby nerves, causing pain and discomfort as well as decreased mobility in some cases. It can also occur if you have a degenerative condition such as osteoporosis or arthritis that weakens the bones in your spinal column.
Symptoms of Bulging Disc in Dubuque
A bulging disc can cause several different types of symptoms depending on where it is located in your spine and what nerves are affected by the pressure. Some common symptoms include:
• Lower back pain
• Neck pain
• Tingling or numbness in limbs or other parts of the body
• Muscle weakness or stiffness in certain areas
• Difficulty bending or moving certain parts of the body
• Pain that radiates down into your legs or arms
It’s important to note that not all bulging discs will cause symptoms. In some cases, they may remain asymptomatic until they become herniated discs which require more aggressive treatment. It’s important to pay attention to how your body feels and to recognize any changes that could signal something more serious than just normal aches and pains from everyday activities.
Cause of Bulging Disc in Dubuque
The most common cause of a bulging disc is aging. As we get older, our bones and muscles naturally become weaker as wear and tear take their toll over time. This weakening can cause the discs between our vertebrae to not hold up as well as they once did, leading to a bulging disc.
Here are some of the cases of Bulging Discs:
Age-related Wear and Tear
As we age, our spine discs naturally become weakened due to general wear and tear. This weakening can cause them to bulge outwards when too much pressure is put on them. The most common type of age-related bulging disc occurs in the lower back (lumbar region). Other types may occur in different parts of the spine.
Injury or Trauma
Injury or trauma to the spine can also cause a disc to bulge outwards. The most common types of injuries that can lead to a bulging disc are falls, motor vehicle accidents, sports injuries (especially contact sports), and heavy lifting. In some cases, even minor incidents such as sneezing or coughing can lead to a slipped disc if there is already existing weakness in that area due to age-related wear and tear or another underlying medical condition.
Underlying Medical Conditions
Some underlying medical conditions can increase your risk of developing a bulging disc. These include obesity, osteoporosis, diabetes, rheumatoid arthritis, scoliosis, spondylolisthesis (when one vertebra slips over another), and spinal stenosis (narrowing of the spaces within your spine). If you have any of these underlying medical conditions, it’s important to talk with a chiropractic doctor at Tri-States Chiropractic Health and Injury Care in Dubuque about ways to reduce your risk of developing a bulging disc.
Lifestyle Factors
Certain lifestyle factors can also increase your chances of developing a bulging disc. Poor diet, lack of exercise, smoking, and excessive alcohol consumption can all contribute to weak muscles that put extra strain on your spine and make it more likely for you to develop a bulging disc. Being overweight can also put extra pressure on your spine that increase your chances of developing a disc issue as well.
Top Treatment Options of Bulging Disc in Dubuque
Alternative Treatments
There are also alternative treatments that can be used to help relieve symptoms associated with bulging discs such as acupuncture, chiropractic care, massage therapy, and yoga/stretching exercises. Chiropractors at Tri-States Chiropractic Health and Injury Care specialize in diagnosing and treating conditions related to the musculoskeletal system such as bulging discs.
Chiropractors use manual adjustment techniques, massage therapy, ultrasound, electric stimulation, and other treatments to help reduce pain and restore mobility in the affected area. Additionally, chiropractors may provide advice on lifestyle changes that can help prevent future issues or flare-ups
Physical Therapy or Exercise Therapy
Physical therapy is one of the most common treatments for bulging discs. Through physical therapy, patients have access to a wide range of exercises and stretches that can help improve strength and flexibility in the affected area and reduce pain and discomfort. Physical therapists also educate patients on proper posture and body mechanics to help prevent future injuries or complications.
Epidural Injections
Epidural injections are another option for treating bulging discs. During an epidural injection, medicine is injected directly into the spine near the affected area to reduce inflammation and pain in that part of the body. These injections typically include steroids or anesthetic agents that work to provide immediate relief from discomfort caused by a bulging disc. While this method may not be suitable for everyone, it does offer short-term relief for those who find it helpful.
Medications
When conservative treatments like physical therapy are not enough to provide relief from a bulging disc, medications may be necessary to reduce inflammation and decrease pain levels. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce swelling and ease discomfort. In more severe cases, stronger prescription medications such as muscle relaxants or even narcotic pain relievers may be prescribed by your doctor if necessary.
How Hot and Cold Therapy Works
Hot and cold therapy can be used to treat bulging discs by reducing inflammation and providing temporary relief from pain. The heat increases blood circulation, which helps relax tight muscles in the affected area. This can reduce pressure on the disc, leading to less pain. On the other hand, applying cold compresses to the affected area can reduce swelling by constricting blood vessels. This can also help numb the area so you don’t feel any discomfort.
Chiropractic Care in Treating Bulging Disc in Dubuque
Chiropractic care in Dubuque is an effective treatment option for those suffering from bulging disc pain. Through spinal manipulation techniques combined with lifestyle changes like exercise modifications or dietary adjustments, chiropractic doctor Dr. Peter Lynch can provide relief from the discomfort associated with bulging discs and promote overall healing of the affected area(s).
If you’re experiencing any type of discomfort due to a bulging disc issue in Dubuque, contact us today at (563) 635-6599 to learn more about how we can help you manage your symptoms through chiropractic care!
0 notes
Text

From A Journal of the Plague Year by Daniel Defoe. Defoe was only 5 years old during the Great Plague of 1665, and the narrative is fictional, and it has been debated whether it is more fiction or more documentary. Perhaps it supplants In Cold Blood as the first nonfiction novel🤔. In either case, he did extensive research, had second hand accounts, and primary documentary sources to create what seems to be a fascinating account of the contagion. I’ve only just been sampling it and look forward to reading it through.
Some fascinating observations include the reliance on the superstitious constructs: finding portentous meaning in a comet or the configuration of clouds, the reliance on religion, astrologers, fortune tellers and other charlatans, the belief in the power of amulets, charms, and other worthless preservatives. Another phenomenon during the bubonic plague was the proliferation of medical quacks & mountebanks selling potions of useless and sometimes harmful ingredients to the gullible masses.
Other interesting points include: the denialism that plague would affect their communities with such severity, the general lack of individual planning, the great difficulty of maintaining the isolation of afflicted citizens, the problem of asymptomatic infected persons who unwittingly spread disease, the fearful mistrust towards each other, the attrition of healthcare workers and the premature letting down of precautionary measures once the mortality rates declined. It’s amazing that the general consensus of the plague that it was a judgment from god for their sins and yet be grateful to the same god for saving others. Of course the reason for this mindset was their abject ignorance of medical science in the 17th C and the resulting overwhelming fear and helplessness. Fortunately we now have advanced medical science to mitigate morbidity and mortality and to make inroads into weaning ourselves from religion and other forms of superstition. Unfortunately there are still ignorant and evil people who ignore science and propagate harmful misinformation and conspiracy theories for profit and political gain, much to the detriment of the poorly educated.
0 notes
Text
Debunking myths about gallbladder stones

The gallbladder — an unsung hero in our digestive system — often goes unnoticed until something goes wrong. In this blog, doctors at Vedam Gastro Hospital, one of the best gastro hospitals in Surat guide us in understanding gallstones — those tiny, yet mighty, crystalline deposits causing significant discomfort in the abdomen and help in debunking the myths that cloud our understanding of this vital organ’s issues.
Myth 1: Only the Elderly Get Gallstones
Contrary to popular belief, gallstones aren’t exclusive to the elderly. While age increases the likelihood, even younger individuals can develop them due to various factors, including diet, genetics, obesity, and rapid weight loss.
Myth 2: Gallstones Only Cause Pain
Yes, gallstones are notorious for causing intense pain, known as biliary colic. However, their impact extends beyond discomfort. If a stone blocks the bile duct, it can lead to complications like cholecystitis (inflammation of the gallbladder), pancreatitis (inflammation of the pancreas), or jaundice.
Myth 3: Removing the Gallbladder Disrupts Digestion
A very senior Gastroenterologist at Vedam Gastro Hospital explains that the gallbladder’s primary function is to store and concentrate bile produced by the liver, aiding fat digestion. After gallbladder removal (cholecystectomy), bile drips continuously into the intestine, facilitating digestion. While some individuals may experience mild digestive changes post-surgery, most adapt without major disruptions.
Myth 4: Diet Doesn’t Affect Gallstones
High-cholesterol and high-fat diets are culprits in gallstone formation. Excessive intake of saturated fats prompts the liver to excrete more cholesterol into bile, leading to imbalances that form gallstones. Conversely, diets rich in fibre, vegetables, fruits, and healthy fats can help prevent gallstones.
Diet significantly influences gallstone development. Choosing a balanced diet, moderating fat intake, focusing on healthy fats, and maintaining a healthy weight are key factors in reducing the risk of gallstones. While diet isn’t the sole factor, it is a crucial player in the prevention of gallstone formation and supports overall gallbladder health.
Myth 5: All Gallstones Need Immediate Treatment
Not all gallstones warrant immediate action. Asymptomatic gallstones, found incidentally during medical tests for unrelated issues, may not require treatment. However, in case of severe pain or discomfort, medical intervention is necessary to prevent further complications.
Myth 6: Medication Dissolves Gallstones Completely
Medication for gallstones aims to dissolve cholesterol-based stones over time by altering bile composition. Ursodeoxycholic acid (UDCA) is a common medication used for this purpose. It works by reducing the cholesterol content in bile, gradually dissolving small cholesterol stones over several months to years. However, this approach has limitations. It’s effective mainly for small, cholesterol-based stones and may take a long duration to work. Not all stones respond to medication, particularly larger or pigment stones. Additionally, there’s a risk of stone recurrence once treatment stops. Close monitoring and adherence to the prescribed regimen are crucial. While medication can be an option for certain cases, surgical intervention remains the primary treatment for symptomatic or larger gallstones that don’t respond to medication.
Myth 7: Gallstones Only Require Surgical Treatment
Dr. Ronak Malani, a senior gastro surgeon at one of the best stomach hospitals in Surat, confirms that alternative treatments, such as shock wave lithotripsy (using shock waves to break up stones) can be opted for in cases where surgery isn’t possible for a patient.
Myth 8: Pregnancy Doesn’t Influence Gallstones
Pregnancy significantly increases the risk of gallstones due to hormonal changes that affect how the gallbladder functions. The risk persists during the postpartum period. Fortunately, most gallstones discovered during pregnancy remain asymptomatic and may not require immediate action.
Myth 9: All Symptoms Point to Gallstones
Gallstone symptoms, like abdominal pain, nausea, and vomiting, overlap with various digestive issues. However, not all abdominal discomfort stems from gallstones. A thorough examination by a healthcare professional is essential for an accurate diagnosis.
Myth 10: Once Gallstones Are Removed, They Won’t Return
Dr. Pravin Borasadia, one of the best stomach specialists in Surat, says that in rare cases recurrence is possible even after gallstone removal. Lifestyle modifications, including dietary changes and maintaining a healthy weight, can significantly reduce the likelihood of their reappearance.
In Brief:
Debunking the myths surrounding gallstones is crucial for a better understanding of their nature, prevention, and treatment. While some misconceptions exist, awareness, lifestyle modifications, and timely medical intervention remain our best defences against gallbladder issues. Consultation with the best healthcare professionals helps navigate these myths, ensuring accurate information and appropriate management of gallstone-related concerns.
0 notes
Text

Comparing the 2% so-called case fatality rate of SARS-CoV2 with the widely reported 0.1% case fatality rate of the seasonal flu is like comparing apples to orangutans. In the latter case, the study’s authors note that the denominator (and numerator) value includes estimated presumed mild cases that didn’t seek medical attention, which is a vast number. In the former case, the denominator reflects only those that are test-confirmed, presumably because most of them were sick enough to warrant being tested in the first place (keep in mind that test kits are in very limited supply).
In all likelihood, however, given the one-off infections that are being detected in disparate locations, thousands if not millions have already had mild or asymptomatic SARS-CoV2. If an estimate of untested cases had been included in the denominator (and numerator)—as had been done in the case fatality rate for seasonal flu, the case fatality rate of SARS-CoV2 would probably be far below the reported 2%. The same selection bias likely skews the widely reported case fatality rates of SARS-CoV1 (9.6%) and MERS (36%).
Keep in mind that terms like SARS and MERS are tautologically self-referential. They are branded as memes through the process of taking a group of patients who are unfortunately close to dying from a viral respiratory infection, then measuring the death rate among those close to dying. Though it’s hardly the ideal comparison, the analogous exercise would be taking the estimated 12,000 to 79,000 deaths from the annual seasonal flu in America then dividing by the 140,000 and 960,000 hospitalizations each year from the seasonal flu. The median case of these numbers would yield a case fatality rate of about 10% for the seasonal flu. Fortunately, the public, scientists and the CDC mentally account for the true flu prevalence, including mild cases, to be between 9.3 million to 49 million per year, which dramatically deflates the case fatality rate for the seasonal flu by 50 fold.
0 notes
Text
Bird flu is a huge problem now – but we’re just one mutation away from it getting much worse | Devi Sridhar
New Post has been published on https://petnews2day.com/pet-news/bird-news/bird-flu-is-a-huge-problem-now-but-were-just-one-mutation-away-from-it-getting-much-worse-devi-sridhar/
Bird flu is a huge problem now – but we’re just one mutation away from it getting much worse | Devi Sridhar
Lockdowns are a horrible experience, but fortunately one that is in the past now. Unless, that is, you’re a domestic bird in Britain. Since 7 November, a UK directive has instructed all farmers to keep their birds indoors as part of a stringent measure to stop the spread of avian flu, or the H5N1 virus. This measure is intended to avoid infection of domestic birds from wild birds, and will result in tens of millions of chickens, ducks, geese and turkeys being brought inside for the foreseeable future. We’ve also seen island birds affected, resulting in the shutdown of human visitors to the Isle of May in Scotland for five weeks, among other measures.
Avian flu is known as one of the most infectious diseases: the R number, which was often discussed for the spread of Covid-19, can be as high as 100 for avian flu, meaning one bird can infect as many as 100 others. And the past few months have seen exponential spread of the virus, with Britain and Europe hit especially hard. A lab in Surrey that tests samples says it has seen a 600% increase in cases in the past three months.
Why is this outbreak causing concern not just among scientists but also poultry farmers and government officials? Currently, avian flu outbreaks have been limited in humans because the virus doesn’t spread easily between us. But this is a ticking timebomb. A mutation that makes this virus circulate more easily between humans is possible. This would be a gamechanger and raise the risk to humans considerably. And the more chances the virus has to jump into a human and mutate, the more likely it is a dangerous strain will emerge that could set off the next pandemic.
While humans have been infected by birds, they are usually workers on poultry farms and those in close contact with infected birds, and even these instances have been rare. For example, on 3 November, two farm workers in Spain tested positive; it was the second known infection of humans in Europe since 2003. Infection is usually through handling sick or dead birds.
Infected birds have the flu virus in their saliva, blood, mucus and faeces, and humans can get infected if they get this virus into the eyes, nose or mouth, or inhale droplets in close range (you can’t get infected with avian flu by eating fully cooked poultry or eggs). And this virus is not mild. The fatality rate is thought to be high in humans: the World Health Organization estimate is roughly 60% for H5N1. We currently have no vaccine to use in humans; nor does the seasonal flu vaccine work against avian flu.
But while the chance of human transmission is a future worry, right now the virus is affecting people’s livelihoods and farms, and putting hundreds of millions of domestic and wild birds in danger. Outbreaks in chickens can kill the entire local population; in other birds, such as ducks and geese, the disease is often mild or even asymptomatic. Ducks have even been called the “Trojan horses” for the virus, given their ability to carry it and infect others while remaining unaffected themselves.
Bird flu is highly infectious and poses a high risk to chickens and turkeys. As a result, if a farm tests positive for bird flu, the entire flock is culled. This can lead to hundreds of thousands to millions of pounds in lost income, and places enormous strain on poultry farms. It also has implications for the price and availability of turkeys and chickens going into Thanksgiving and Christmas. And, of course, it is a tremendous loss of bird life.
The heart of the issue is how we raise and treat animals, and their interactions with humans. Poultry are often kept in difficult conditions where they are packed into close quarters and diseases easily pass through them. Some experts think that this more infectious strain developed in an industrial factory environment, where animals are kept in close quarters and viruses have the chance to circulate and mutate.
And this is not just an issue with avian flu, but other infectious diseases as well. In places such as China and India, antibiotics are freely given to animals in order to prevent infection (especially in industrial farming) and to make them as large as possible. A survey of chicken farmers in China found that they all used antibiotics. The rationale here is cheap and fast meat to meet the growing demand in emerging economies.
But this creates its own problems. Feeding antibiotics to animals can lead to the emergence of resistant bacterial strains, and then humans such as farmers becoming infected with antibiotic-resistant infections. These then circulate in humans and reduce the effectiveness of one of the most powerful drugs in modern medicine. Chemotherapy, infections and surgeries of all kinds have become safer because of antibiotics. If the drugs don’t work, these procedures become high-risk and life-threatening, as they used to be in the pre-antibiotic era. And as we’ve learned, all it takes is for a person to get on a plane with a novel infectious disease for it soon to become a problem for everywhere else in the world.
The major infectious disease threats in humans tend to come from animals: think of Sars-CoV-2, Sars, Mers, Ebola … the list goes on. There are more than a million viruses circulating in the animal kingdom, and it would be a fool’s errand to try to stop that circulation. But we can limit the chances these have to jump into the human population, and limit their circulation in domestic animals. This requires taking the animal-human interface seriously, and knowing that while it’s a major economic, animal welfare and farming problem now, the situation becoming even worse is just a mutation away.
0 notes
Text
i will get to writing soon hopefully !! i know i revamped this blog n then Dipped but i will write !!
#tbd.#* out.#covid mention in the tags !!#anyways ive been rlly tired lately#even tho ive been getting enough sleep#so we think it might be post covid effects n whatnot.........#it was an asymptomatic case fortunately#tho constant fatigue n chest pains are. Not fun lol!
0 notes