#normal creatinine levels
Text
Recognising Creatinine Levels: An All-Inclusive Guide to Renal Health
Recognising Creatinine Levels: An All-Inclusive Guide to Renal Health
Kidneys are the vital organ that is responsible for removing extra fluids and waste from our blood, controlling blood pressure, and ensuring the balance of electrolytes. If kidney function is impaired, it causes kidney disease, which affects millions of people across the globe. Kidney diseases can be caused by a range of reasons, and diagnosis usually involves analyzing levels of creatinine in blood. The presence of high levels of creatinine may indicate kidney issues, and if not treated, kidney diseases can cause serious health problems.

Kidney Diagnosis and High Creatinine
The kidney disease diagnosis usually requires a series of tests, among which is assessing the level of creatinine in blood. Creatinine is a waste product created by muscles and then removed by kidneys. If the kidneys function optimally, they can maintain constant levels of creatinine. But, when kidney function is affected, and creatinine levels rise, it can be a sign of a decline. The presence of high levels of creatinine in the blood may indicate decreased kidney function, which could indicate an underlying kidney problem. The most common tests to determine levels of creatinine include urine and blood tests, with the estimated glomerular filter rate (eGFR) as an important indicator of kidney function.
High Creatinine Side Effects
The presence of high levels of creatinine is often an indication of kidney disease and may cause a wide range of uncomfortable and even life-threatening symptoms. Common side effects of high creatinine include:
The kidneys try to eliminate waste and keep electrolytes in balance; it could result in exhaustion and loss of energy.
Swelling: Kidneys play a vital role in maintaining our body's fluid equilibrium. If they're not functioning properly, extra fluid may build up and cause swelling, especially around the ankles, feet, and face.
Kidneys are a major factor in controlling blood pressure. If they're not functioning properly and their blood pressure rises, it can lead to and lead to hypertension.
Anemia: The kidney's function is impaired. It can affect the red blood cell production. This can result in anemia. This may cause weakness and fatigue.
Nausea and vomiting creatinine levels can cause the accumulation of waste materials in the bloodstream, which can cause sickness and nausea.
Itching: Kidney issues can cause the accumulation of substances that are not needed in the bloodstream, causing itching, skin itching, and rashes.
Natural Remedies for Kidney
Many people are looking into alternative treatments for kidney especially natural remedies for kidney disease. It's important to talk with a medical professional prior to commencing any kidney treatment. Natural remedies for kidney problems are:
Dietary changes: A diet containing less processed foods, salt, and saturated fats may help reduce the strain on kidneys. In addition, consuming more fresh vegetables and fruits can supply essential minerals and vitamins as well as support kidney health.
Hydration: Keeping hydrated is vital for good kidney health. A proper hydration regimen helps your kidneys eliminate waste and toxins. It is vital to regulate the amount of hydration you consume and to avoid excessive hydration since this can stress the kidneys.
Regular exercise: Keeping the right weight and completing regular physical exercise can aid in reducing blood pressure as well as improve kidney function in general.
Homeopathic Kidney Treatment
Kidney Treatment by homeopathy is a complete method of treatment that concentrates on enhancing the body's inherent healing capabilities. Homeopathic remedies are made by diluting natural substances. They are believed to work by stimulating the body's vital energy to restore equilibrium. Certain homeopathic remedies are utilized to help support kidney health and relieve symptoms of kidney disease. The remedies are tailored depending on the individual's symptoms and the constitution.
#best homeopathic medicine for creatinine#Kidney treatment by homeopathy#Low creatinine#normal creatinine levels#creatinine levels
0 notes
Text
#Kidney#creatinine#serum creatinine#normal creatinine levels#high creatinine level#what is creatinine?#creatinine means
0 notes
Text
hi guys! so i wanted to give you all this update as to why i have not been posting as much. for the past month i have been working at my job diligently, and at the same time ultimately concerned with my health and wellbeing. i know i made a post a while ago, saying that i was worried about my health and my kidney function, because i am a type 2 diabetic and kidney disease is common in my family. i have visited my new primary care doctor (for those who do not live in the US a primary care doctor is a healthcare provider that practices in general medicine and they are the individual i can go to to get check ups, vaccinations, referrals to specialists etc.) and a blood test as well as a urine test was done just last week.
the results of the blood test, my primary care doctor told me were fine. my urine test, to me told a different story, i noticed that my creatinine in my urine was low. it was at 17 when the reference range is 20 to 275 according to the lab test. anyways, i didn't ask them about my creatinine levels yet because i will be doing another visit with them at the end of this month to discuss over my results and what we will be doing as patient and doctor to make sure that i will be ok.
my blood sugar levels have been excellent. my respiratory is fine. my heart beat is normal. however i just have a really huge concern for my kidney function. until i get to see a kidney doctor who will do a test and the test informs me that i am well then i won't be worrying anymore. right now i am constantly stressing about my kidney function, i have been trying to distract myself with trying to finish writing requests, watching new anime shows, and going to the gym to put my mind off of it, but at the end of the night when my head hits my pillow it is all that i am thinking about.
i am writing this post to you guys, my followers and new followers, because i want for you all to know that i am still here. im still around, and i am trying my hardest to fulfill requests in my inbox and drafts. i am suffering right now from a really bad case of writer's block and stress. i think that is better to be transparent with you guys, and to let you all know what is going on with me.
i feel really bad that im not writing as often as i should be. i just hope, pray, and wish that this writer's block will go away and i will start writing again.
25 notes
·
View notes
Note
Ask for kidney function tests. Even if they did them. This sounds like my mom's end stage kidney disease & eventual cancer. *hugs* ♡
They keep repeating them and the only things coming up high are my MCH & MCHC levels (which are related to haemoglobin but I'm not anaemic (yet) as in my folate and b12 are fine) so I'm so confused myself haha.
My urea is verging on low and creatinine verging on high but nothing outside the "normal" limits (yet).
I'm so tired of arguing with them 😔 you guys advocate for me more than any doctor has! ♥️ I'll make sure they repeat everything soon tho x
12 notes
·
View notes
Text
Yeah. Knew it was gonna happen. Feeling mad about this.
Health-related vent with some info if your thyroid might be a messy bitch too. Just typing it out so my head doesn't blow up.
Myopathy in Hypothyroidism (quoth VeryWellHealth, I looked it up to make sure I wasn't hallucinating out of anger/relief)
Muscle weakness
Creatinine levels tend to be normal
Cramping (uncommon)
Rarely, issues with the muscles involved in swallowing and breathing (rare)
"Rarely, hypothyroidism can cause severe muscle symptoms. One example is Hoffman's syndrome. This is when a person develops muscle hypertrophy (enlarged muscles). It can lead to significant muscle stiffness, weakness, and pain."
Yeah. Ha. Yeah. In other news, in my body right now: 1)Hypertrophy of a muscle on the inside of my right thigh, causing constant pain and difficulty walking. 2)Shoulder that locked up the Winter of 2021 and continues to do so on a daily basis, making it difficult for me to type or draw. 3) Regular back spasms. 4) Occasional spasms of all kinds! 5) Sleep apnea that's resisting the CPAP.
And, if we count my mother, who died before she turned 70, all of the above, just in different places (with the exception of an apnea diagnosis, she never got one, she just had a horrible time sleeping) plus difficulty swallowing, weakness, falls, and brain fog. She had a million different diagnoses, and no follow up on any of them when she got no relief. To the best of my knowledge, nobody ever told her, "Hashimoto's, and Synthroid may not be enough to treat it."
She either killed herself shortly after yet another surgery, or aspirated her own vomit and died with no help from the pain meds they gave her. "Issues with muscles involved in swallowing and breathing," yes.
This is my life. This has been my whole life. Optimistically speaking, this has taken half my life, and my circumstances are irreparably different because of it. Might I have had children if I knew my mom's lifelong physical and mental health issues were down to an under-treated thyroid? Maybe! And if they'd been treating mine, my uterus and ovaries probably wouldn't have been so screwed up they needed to be yanked out and thrown away. Might I have been able to hold down a job and had a career without that constant pain and anxiety? Who knows! Might I have had enough strength to keep pushing and get published traditionally, thus being absorbed and rewarded by the broken system I've devoted my total-lack-of-notoriety to fighting and working without? Beats me! Would I still have two living parents and some ability to get closure for what I went through growing up? A riddle for the ages!
If my new doctor sticks with it and finds something that works for me, this is all the marbles. I did not over-state how important this was. This is my quality of life, for the rest of my life. But I look back, and there's so much I've already lost that I'll never get back. It's just gone.
Before this, there was nothing to stop me from being unable to eat, or breathe, or move, and going out just like my mom. Her story would've been mine - only mine would've been shorter. Going down the generations, my grandmother had a lot of these issues, just less severe. It was getting worse. The Agent Orange they dropped on my dad surely did not help. I was able to figure out what was going on thanks to internet access, but I couldn't get anyone to confirm it or treat me. I fought like hell, and it took someone who loved me to intervene on my behalf. Someone with a Y chromosome. And now I still need One Good Doctor to see me through. Just one, out of all of 'em. Please, Lord, just the one.
If you got a little extra in you, God, I could use a few more - this gremlin has been ripping up my health for a long time and there's consequences - but maybe I won't die choking on my own vomit in 25 years if just this one works out.
This isn't me. You know that? I've been sick my whole life. I still am. I have no idea if the broken coping mechanisms I developed to deal with this are gonna go away. I don't know who I am. I'm not a ball of anxiety in constant pain that can't hold down a job, but I have no idea who I am.
I hope I get to meet me at some point.
Geez, and I hope you like me too.
3 notes
·
View notes
Text
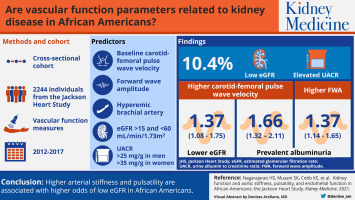
Understanding African American and non-African American eGFR laboratory results
Understanding why eGFR laboratory reports include African American and non-African American results
Glomerular filtration rate (GFR) is the best way to measure how well your kidneys are working, but this test is complicated and cannot be easily done in a doctor’s office. To get around this, laboratories use mathematical equations to estimate the glomerular filtration rate instead of measuring it. This is why laboratories report estimated GFR or eGFR.
Two commonly used estimating equations for eGFR are the CKD MDRD (Modification of Diet in Renal Disease) and the CKD EPI (Chronic Kidney Disease Epidemiology Collaboration) equations. Using these math equations, eGFR is calculated from the amount of creatinine in the blood.
Creatinine is a waste product that comes from the normal wear and tear on your body’s muscles and also from the foods you eat. Everyone has creatinine in their bloodstream. However, creatinine levels can differ between people. This reason for this difference may not only be related to kidney disease – it may be affected by several other factors, such as age, sex, and body weight.
Race was originally included in eGFR calculations because clinical trials demonstrated that people who self-identify as Black/African American can have, on average, higher levels of creatinine in their blood. It was thought the reason why was due to differences in muscle mass, diet, and the way the kidneys eliminate creatinine. Since a patient’s race is not always used when laboratory tests are ordered, laboratories used different eGFR calculations for African American and non-African American and included both numbers in their lab results.
The use of race in calculating eGFR has been a subject of debate. Race is not a biological concept, but a social construct. Using race as a factor for calculating eGFR does not account for the diversity within communities of color. Also, people who self-identify as multiracial might not want to be put in a single racial bucket.
What is the NKF doing to address concerns about using race in measuring eGFR?
In 2020, the National Kidney Foundation (NKF) and the American Society of Nephrology (ASN) formed a joint task force to review the use of race in eGFR calculations. On September 23, 2021, the Task Force announced a new race-free calculation for estimating eGFR. The National Kidney Foundation is working with the nation’s laboratories to get this new calculation into use as quickly as possible. The NKF is also creating materials to show how this new equation may impact patient care.
How is eGFR used?
Estimated GFR is one of the key tests for diagnosing kidney disease. The earlier kidney disease is detected, the better the chance of managing it or keeping your condition from getting worse. Your eGFR informs healthcare professionals about your kidney function and helps them to recommend the best treatments for you. For instance, eGFR results are used in the following ways:
Confirming that kidney function is normal for a potential living kidney donor
Making sure the right dose of medicine is used
Enrollment in clinical trials that use kidney function as an inclusion or exclusion criterion
Making sure the right type of imaging tests and dyes are used
When to refer someone to a nephrologist or kidney doctor
If and when to plan for dialysis
When to start an evaluation for a kidney transplant
Although the NKF alone cannot solve all inequalities, the NKF is working to help identify, confront and reverse them. NKF advocates for making affordable healthcare more available and making sure that communities of color are not left behind. NKF’s CARES helpline is available to all people with kidney disease. NKF’s educational offerings include the impact of kidney disease on diverse communities, and the reasons why communities of color have been disproportionately affected by COVID-19. NKF is committed to continuing its work to address inequalities in kidney health.

#gfr#african american#kemetic dreams#african#africans#lab test#laboratory#health#clincial#clinical laboratory test market
7 notes
·
View notes
Text
Does Metformin, a glucose-lowering drug, hurt the kidneys?
Metformin is a biguanide compound that reduces blood sugar mainly by reducing hepatic glucose output, improving insulin resistance, and reducing glucose absorption in the small intestine. It is currently one of the world's most widely used oral hypoglycemic drugs. Drug safety evaluation studies have found that Metformin has a good safety profile, no carcinogenic or mutagenic effects, and no evidence that Metformin can increase the risk of lactic acidosis. Medicilon has a professional team and experience in preclinical drug safety evaluation services, providing high-quality data and a fast turnaround time to support all drug safety evaluation studies.
Many patients are concerned about the effects of long-term metformin use on the kidneys. The drug does not directly damage the kidneys but can lead to drug accumulation when taken by patients with existing kidney damage. Both the Chinese Guidelines for the Prevention and Treatment of Type 2 Diabetes (2017 edition) and the Expert Consensus on the Clinical Application of Metformin (2016 edition) suggest that Metformin is the drug of choice for the treatment of type 2 diabetes in the absence of contraindications and intolerance, and should always be retained in the glucose-lowering regimen.
1, Benefits of Metformin.
Metformin can reduce hyperglycemia with no hypoglycemic effect on those with regular blood sugar; the drug has the following benefits in addition to hypoglycemia.
(1), Metformin has the effect of reducing body weight.
(2) Metformin has apparent cardioprotective effects and reduces the risk of cardiovascular disease in newly diagnosed and established type 2, diabetes patients.
(3) Metformin can improve lipid synthesis, metabolism, and lipid profile.
(4) Metformin significantly improved liver serological enzyme profile and metabolic abnormalities in patients with non-alcoholic fatty liver.
2, Adverse reactions and countermeasures
The main adverse reactions of Metformin are diarrhea, nausea, vomiting, gastric distension, and other gastrointestinal responses, which mainly occur in the early stage of treatment (the majority happen in the first ten weeks). Most patients can gradually tolerate them, or their symptoms disappear as the duration of treatment increases. Start taking small doses, gradually increase the amount, adjust the quantity at the right time, take with meals, and choose enteric preparations and other methods, which can reduce gastrointestinal reactions.
Three 、Does Metformin hurt the liver and kidney?
Metformin has no hepatic and renal toxicity; Metformin is absorbed through the gastrointestinal tract for blood circulation, almost does not combine with plasma albumin, does not go through liver metabolism, does not compete with liver P450 enzymes, and does not degrade in the body, but acts directly on the liver and muscle, reducing hepatic glucose isomerism and increasing muscle glucose enzymes. Therefore, Metformin is not hepatotoxic.
Metformin is mainly excreted from the urine in its original form by the kidneys and is cleared rapidly, with approximately 90% clearance in 12-24h. The renal clearance of Metformin is about 3.5 times higher than that of creatinine, and renal tubular excretion is the main route of metformin clearance. Therefore, Metformin itself is not harmful to the kidney.
However, caution should be exercised when using Metformin in people with impaired liver and kidney function. Metformin should be avoided when serum transaminases exceed three times the upper limit of normal, and patients with renal insufficiency need to adjust the dose by estimating the level of glomerular filtration rate. Clinicians or pharmacists can assess the above.
4, long-term use of Metformin, the need for appropriate supplementation of vitamin B12
Studies have shown that: the incidence of vitamin B12 deficiency in glucose patients using Metformin is 5.8%, while the incidence of vitamin B12 deficiency in glucose patients not using Metformin and people without diabetes is 2.4% and 3.3%, respectively. Therefore, long-term metformin users should monitor vitamin B12 concentration regularly and increase the intake of vitamin B12-rich foods appropriately (vitamin B12 is mainly contained in animal proteins, such as meat, animal liver, fish, shellfish, eggs, etc.) to prevent and correct vitamin B12 deficiency. If this condition occurs, vitamin B12 should be supplemented in an appropriate amount under the guidance of professional doctors.
Five 、Stop taking Metformin 48 hours before and after doing a CT examination
Diabetic patients should stop taking Metformin 48 hours before and after doing enhanced CT because it is necessary to play contrast agent before doing CT. The contrast agent belongs to macromolecular substances excreted through the kidneys. If you retake Metformin, it will increase the burden on the kidney and cause contrast nephropathy.
6, the icing on the cake: combined with other glucose-lowering drugs
There are several different drugs when taking glucose-lowering drugs, often more than Metformin. This is because the combination of glucose-lowering medications mutually increases the hypoglycemic effect, improves insulin resistance, or reduces adverse reactions.
All diabetic patients should choose the appropriate hypoglycemic drugs according to their different conditions and pay attention to the indications and contraindications of each type of drug. At the same time, it is essential to emphasize that diet therapy and diet control are the cure for diabetic patients and must be adhered to for life. Diet therapy should not be relaxed or abandoned because of oral hypoglycemic drugs or increased dosages of hypoglycemic medications.
3 notes
·
View notes
Text
Reviewing questions
Courvoisier sign is a palpable gallbladder on physical examination and is usually associated with biliary or pancreatic malignancy. Physicians should suspect malignancy in a patient with obstructive jaundice, weight loss, and a history of smoking.
PBC involves granulomatous destruction of the intrahepatic ducts within the portal triads, without affecting the extrahepatic ducts. It is an autoimmune disorder that mainly affects middle-aged women and can increase the risk of developing hepatocellular carcinoma.
Ursodeoxycholic acid has been shown to slow the progression of PBC and is the most important medical therapy. Multiple mechanisms have been proposed including protection of injured cholangiocytes against toxic effects of hydrophobic bile acids and inhibition of apoptosis of hepatocytes. However, the exact mechanism is unknown. Ursodeoxycholic acid does not improve pruritis, which is when cholestyramine or diphenhydramine can be prescribed. Liver biochemical testing will usually show improvement within 3 months of starting therapy. The majority of patients will see sustained improvement with this therapy. For those who do not show improvement, a liver transplant can be considered. Liver transplantation has shown very promising results in patients with end-stage PBC and should be offered after medical therapies have failed.
Geographic tongue, also known as benign migratory glossitis, is an inflammatory condition of the tongue secondary to an unknown etiology. Its key characteristic includes red patches with white borders on the dorsal surface of the tongue, which may mimic the design of a map. The lesions on the tongue are known to change location, shape, and pattern over time and may occur recurrently. The patchy areas are spots in which the local loss of the filiform papillae leads to the depapillation of the tongue. It may be seen more commonly in individuals with eczema, psoriasis, and reactive arthritis. Patients typically present asymptomatically, though common symptoms are usually mild and may include burning or increased sensitivity to certain food and drinks. The diagnosis is typically made clinically, and cultures or biopsies are necessary only in uncertain or persistent cases. Treatment is conservative and may include topical and systemic analgesics.
Alcoholic cirrhosis with signs of portal HTN (ascites and varices). Most patients with clinically apparent ascites will require diuretic therapy in addition to dietary sodium restriction. Diuretic therapy typically consists of treatment with spironolactone and furosemide in a ratio of 100:40 mg per day, with doses titrated upward as needed. Dietary sodium restriction and diuretic therapy are effective in approximately 90 percent of patients with cirrhosis and ascites. Concomitant treatment with both medications can mobilize moderate ascites more rapidly than if added sequentially. Also, using a combination of spironolactone and furosemide in a ratio of 100:40 mg usually maintains normokalemia. Spironolactone may be used alone only in severe alcoholic hepatitis with profound hypokalemia. Furosemide is still added once the potassium normalizes and potassium replacement is no longer needed. The response to diuretics should be carefully monitored on the basis of changes in body weight, laboratory tests, and clinical assessment. Patients on diuretics should be weighed daily; the rate of weight loss should not exceed 0.5 kg/day in the absence of edema and should not exceed 1 kg/day when edema is present. Serum potassium, blood urea nitrogen (BUN), and creatinine levels should be serially followed. In the setting of hyponatremia, diuretics should be stopped when the mean arterial pressure falls to 82 mmHg or below. Making sure that potassium is repleted may also help treat hyponatremia.
T5-T9 is where the sympathetic viscerosomatic reflex for the liver (and other components of the upper GI system) is located.
Bottom Line: Ascites has a stepwise treatment beginning with alcohol cessation, NSAID avoidance, and salt restriction. If this fails, then therapy with spironolactone and furosemide can be utilized followed by large volume paracentesis with albumin infusion. TIPS is the next step, and if this does not achieve a positive response, then liver transplant is the next choice.
The etiology of the ascites can be established through measurement of the serum-ascites albumin gradient. SAAG = serum albumin – ascites albumin. A SAAG greater than 1.1 indicates the ascitic fluid is a transudate and may be related to portal hypertension, which can be seen in splenic vein thrombosis, schistosomiasis, cirrhosis, hepatic metastases, right heart failure, constrictive pericarditis, or Budd-Chiari syndrome. An SAAG less than 1.1 indicates the fluid is an exudate and may be from protein leakage into the peritoneal cavity, which can be caused by nephrotic syndrome, TB, or peritoneal malignancies.
Fever, jaundice, right-upper-quadrant abdominal pain (the Charcot triad), altered mental status, and hypotension (the Reynolds' pentad) are characteristic symptoms of acute cholangitis. Stones in the common bile duct are a leading cause of obstructive jaundice. Endoscopic retrograde cholangiopancreatography (ERCP) is the most appropriate next step in managing the case of a pt who presents with acute cholangitis in the setting of biliary obstruction. Cholangitis is potentially life-threatening, and resuscitative measures, including administration of intravenous fluids and antibiotics, commonly targeted against Escherichia coli, Klebsiella species, and Enterobacteriaceae, should be done initially. After hemodynamic stability is achieved, ERCP is the treatment of choice for biliary decompression and stone extraction in patients with normal anatomy (unaltered by surgery, such as roux-en-y). In patients who have had roux-en-y gastric bypass or other major upper-gastrointestinal surgery, external biliary decompression, such as with percutaneous transhepatic cholangiogram, may need to be considered.
Sphenopalatine ganglion (SPG) release may help stimulate parasympathetic activity and improve secretions to the eyes and mouth. The SPG is associated with both sympathetic and parasympathetic activity in the head and face. The SPG is an autonomic-nervous-system ganglion that relays mixed cranial nerves innervating the upper airways. The SPG is situated in the pterygopalatine fossa, posterior to the posterior wall of the maxillary sinus and inferior to the junction of the body of the sphenoid, the greater wing and pterygoid process of the sphenoid, lateral to the perpendicular plate of the palatine bone, and medial to the pterygomaxillary fissure. It receives parasympathetic and sympathetic sensory afferents via fibers derived from the accessory branch of the facial nerve and the maxillary branch of the trigeminal nerve (V2). It distributes these fibers to the nasal mucosa, lacrimal glands, nasopharynx, and soft palate, including some of the upper-airway dilator muscles. Parasympathetic stimulation results in increased secretions (lacrimation, rhinorrhea, mucus production) (students should remember "rest and digest"), whereas sympathetic stimulation results in decreased secretions. Intraoral myofascial therapy of the SPG is widely used in osteopathic practice for the management of nasal obstruction and chronic rhinitis. The SPG release technique will help increase lacrimation and mucosal secretions. Most likely, this will also initially cause rhinorrhea but will most quickly lead to improvement of this patient's xerostomia and keratoconjunctivitis sicca. A rare syndrome called burning mouth syndrome is often treated with injections and osteopathic manipulative therapy to the sphenopalatine ganglia. With such treatment, patients with this condition generally report improvement in pain, dysgeusia, and xerostomia.
Ischemic colitis commonly presents with crampy abdominal pain and sudden rectal bleeding in the setting of colonic hypoperfusion from any source (dehydration, sepsis, cardiogenic shock), and these low-flow states can be exacerbated by underlying vascular disease.
A patient with a history of significant vascular disease presenting with sudden-onset abdominal cramping and hematochezia is concerning for the development of ischemic colitis. This is a common complication of colonic hypoperfusion, generally in the watershed areas of the colon (areas between the large arterial supply branches), which are most susceptible to variability in blood flow. When flow is insufficient to provide for the needs of cellular metabolism, ischemia develops. In this case (as commonly occurs in real life), the most likely trigger was working in the heat without adequate fluid resuscitation. This resulted in relative intestinal hypotension, likely exacerbated by underlying microvascular disease. In acute colonic ischemia, patients experience a sudden onset of abdominal cramping and tenderness over the affected areas of the abdomen. This is often associated with an urgent need to defecate. Rectal bleeding is mostly associated with left-sided colonic involvement and does not have to be present to make a diagnosis of acute ischemic colitis. Labs consistent with ischemic colitis include: lactic acidosis, fever, leukocytosis, or thrombocytopenia. If there is transmural involvement of the colon, colon perforation with localized or generalized peritonitis may be present, though this is less often the case. Ischemic colitis can be categorized as nonocclusive, which is typically transient, or occlusive. Nonocclusive ischemic colitis can occur in patients that are dehydrated or hypotensive, as in the setting of sepsis or cardiogenic shock. It usually affects the watershed areas of the colon, such as the splenic flexure and rectosigmoid junction. Occlusive ischemic colitis can result from embolic or thrombotic arterial occlusion, which may be from atrial fibrillation or iatrogenically from instrumentation.
Bottom Line: Gilbert syndrome is caused by reduced bilirubin conjugation resulting in episodic isolated unconjugated hyperbilirubinemia and often presents during adolescence.
COMBANK Insight: It is important to note for testing purposes that unconjugated bilirubin may not be reported in lab results. It is measured by subtracting the direct (or conjugated) bilirubin from the total bilirubin. It may also be referred to as indirect bilirubin.
2 notes
·
View notes
Text
Treatment for Kidney Failure: Effective Solutions for Managing End-Stage Renal Disease

Bharat Homeopathy Kidney Treatment Hospital
Your kidneys may not be functioning properly if you have a chronic kidney disease. Kidneys are filters in your body. They filter toxins, wastes and excess water from your blood. Also, they help with red blood cells and bone health. Your kidneys will not be able to remove waste when they stop working. This causes waste to accumulate in your blood. You will likely experience many difficulties. To prevent kidney problems, it is important to receive kidney failure treatment without dialysis that does not involve dialysis.
What is acute renal injury?
Acute kidney injury (AKI) is a temporary decrease in kidney function that lasts less than three months. This condition is usually a rapid onset and can be triggered by taking too many kidney problem medication. Patients may also decide to continue dialysis to help heal their kidneys if they have kidney diseases or injuries. Homeopathy is the only permanent cure available for chronic kidney disease treatment. Many patients who suffer from acute kidney injury recover completely and lead normal lives. If enough damage is done, there's a higher chance that chronic kidney disease (or ongoing kidney problems) will develop in the future. Chronic kidney disoder can be difficult to treat because of this. As soon as the first signs of kidney failure are recognised, a patient can avoid any problems by taking the right homeopathic treatment.
Complications of CKD
They can be complications of chronic kidney disease treatment. If they're addressed promptly, they can prevent this condition from developing into a serious condition.
Hypertension: The most damaging consequence of CKD is elevated blood pressure, which is thought to accelerate the decline of renal function.
Anaemia: Anaemia is a different consequence. It occurs when the kidneys are unable to make adequate red blood cells, which results in weakness and fatigue.
Diseases of the bone, such as CKD, may also trigger bone problems. The kidneys are accountable for ensuring calcium and phosphorus levels. If the kidneys fail to perform as they should, bones become weaker, which increases the chance of breaking.
What is chronic kidney disease?
Chronic kidney disease (CKD) is a condition where your kidneys are damaged and cannot remove blood as they should. High blood pressure and diabetes are two of the main causes of kidney disease. Your healthcare professional may perform tests to diagnose the cause of your kidney disease. Treatment for kidney failure may differ depending on the underlying cause of your kidney disease. Only tests can determine if there is kidney damage. It is vital to be examined if you have a medical history of heart disease, high blood pressure or diabetes, as well as kidney disease. Treatment of kidney failure is more effective if you start early. Follow these tips to take care of your kidneys:
Control the conditions that are causing your problems
You should be careful if you have a chronic health condition that can trigger CKD. For example, diabetes or high blood pressure. Follow your doctor's advice and follow the cure for chronic kidney disease.
Smoking: Smoking is associated with an advanced risk for heart disease. This in turn, increases the likelihood of chronic kidney disease (CKD). This illness can lead to heart attacks or strokes. Quitting smoking can help you to become healthier and reduce your risk of some serious illnesses.
Eat healthy food to reduce your risk of kidney disease. Healthy diet will help you maintain a healthy cholesterol level and blood pressure. Eat lots of fruits and vegetables.
Smoking and alcohol consumption must be stopped. Moreover, you should only take your medications as prescribed by your doctor. High creatinine Kidney problems can be prevented by using high creatinine treatment.
Drink plenty of water in accordance with the recommendations of your physician. Healthy food is crucial for the proper functioning of your kidneys. However, over-hydration can be detrimental.
Regular checkups: According to your doctor's advice, drink plenty of water. Healthy food is essential for your kidneys to function properly. However, too much water can be harmful.
Visit your doctor regularly to have your kidneys examined and to check your overall health.
Bharat Hmeopathy Treatment
Bharat Homeopathy, the best hospital in the medical field for Treatment for kidney failure. It is known for its success in treating kidney diseases and the use of natural remedies. It is a well-known hospital that has a reputation for treating chronic kidney disease. Our experts provide detailed advice on a range of kidney ailments.
We believe that natural remedies can combat kidney disease. Bharat Homeopathy places a great deal of importance on comfort and ease of recovery when developing nutrition programs based on medical history.Call Bharat homeopathy immediately to ensure your kidneys are receiving the treatment needed to function properly. We are here to help you achieve your ideal health. Our best kidney doctor is available to help you begin kidney failure treatment without dialysis.
0 notes
Text
Does Diabetes affect the kidneys?
Diabetes is a condition that lasts forever and makes a person's blood sugar too high due to insulin issues. The primary sugar that the body uses to create energy is glucose. More individuals are being diagnosed with a condition that, if left untreated, can result in severe health issues—among them, kidney damage.
About 40% of individuals with diabetes might eventually suffer from diabetic kidney disease, also referred to as diabetic nephropathy.

How does diabetes affect the kidneys?
Elevated blood sugar levels raise the force within the sensitive filtering apparatus in the kidney (the glomeruli), leading to more harm to the filters. This harm results in elevated blood pressure, the escape of protein into the urine, and (over time) ongoing harm to the kidneys, culminating in complete kidney failure. If the damage is severe, the kidneys might stop working properly, making it necessary for a person to get dialysis or a new kidney to survive.
In type 1 diabetes, the development of diabetic kidney disease might span over a decade. Nonetheless, for the elderly with type 2 diabetes, who might have pre-existing kidney damage due to high blood pressure or heart conditions, diabetes seems to accelerate kidney deterioration significantly earlier. Hence, it's crucial that your physician keeps an eye on your kidney's well-being and that you make an effort to maintain your kidney health.
Kidney damage can start 5-10 years before symptoms appear. Severe cases may cause fatigue, headache, irregular heartbeat, nausea, and poor appetite. Infections are common.
Risk elements for diabetic kidney disease encompass:
Lack of control over elevated blood sugar levels (hyperglycemia).
Lack of control over elevated blood pressure (hypertension).
High levels of cholesterol in the blood.
Genetic predisposition to diabetes and kidney disease.
Being overweight.
Smoking.
How is kidney disease diagnosed?
To determine if you have kidney disease, check the creatinine levels in your blood. This measurement helps in calculating your glomerular filtration rate (GFR), which indicates if your kidneys are functioning properly. Additionally, a urine test is conducted to detect the presence of protein albumin in your urine.
Treatment options
Kidney damage can be managed with medical care if it is detected early. As the level of protein in the urine increases, the condition of the kidneys will gradually deteriorate.
Control your blood pressure
Controlling blood pressure below 130/80 mm Hg is key to slowing kidney damage. ACE inhibitors or angiotensin II receptor blockers may be prescribed to protect kidneys from microalbuminuria. Medications may also be prescribed for normal blood pressure. To choose the best course of action, speak with a provider.

SIMPLE TECHNIQUE TO HELP MANAGE BLOOD SUGAR
Control your blood sugar level
Controlling blood sugar levels through healthy eating, exercise, and medication can slow kidney damage. Some diabetes medicines prevent nephropathy better than others. Check and record blood sugar levels regularly. Pick the medication that will work best for you.
Alternative Methods to Safeguard Your Kidneys
Attend your scheduled medical check-ups and tests consistently.
Consume all your prescribed medications, such as ACE inhibitors and ARBs, which could safeguard your kidneys or slow disease advancement.
Strive to keep a balanced way of living. This involves consuming a well-balanced diet, engaging in physical activity, ensuring adequate rest, managing stress, and keeping your weight within a healthy range.
Quit (or avoid beginning) smoking or using any tobacco items, and restrict your consumption of alcohol.
Untreated diabetic kidney disease can lead to severe problems. This condition is irreversible and may progress to end-stage kidney failure, necessitating a kidney transplant for survival.
Starting treatment early is the most effective method to slow down the advancement and stop additional harm. Discuss with your physician strategies to prevent or control diabetes to prevent kidney disease from occurring.
0 notes
Text
Comprehending Chronic Kidney Disease (CKD)
The kidneys are vital organs for filtering waste and excess fluids from the blood. Kidney problems, whether acute kidney injury (AKI) or chronic kidney disease (CKD), can lead to a range of health issues, including swelling due to kidney failure. While conventional treatments are commonly prescribed, more individuals are exploring alternative approaches to kidney health, including homeopathy kidney treatment.
Understanding Kidney Function and Kidney Conditions
Before discussing homeopathic remedies, it is essential to understand the role of the kidneys and the distinction between acute and chronic kidney conditions.
Kidney Function:
The kidneys perform several crucial functions in the body, including the filtration of waste products, maintenance of fluid balance, regulation of electrolytes, and secretion of hormones that control blood pressure. When the kidneys are impaired, these functions can be compromised, leading to a buildup of waste in the body and other health complications.
Acute Kidney Injury (AKI):
AKI is a sudden loss of kidney function that typically occurs as a result of an injury, infection, or certain medications. It is characterized by a rapid decline in kidney function, leading to an accumulation of waste products in the bloodstream. Acute kidney injury
requires immediate medical attention and can sometimes be reversible with timely intervention.
Chronic Kidney Disease (CKD):
CKD, on the other hand, is a long-term condition where the kidneys gradually lose their ability to function over time. It progresses through stages, and in advanced cases, it can lead to kidney failure, also known as end-stage renal disease (ESRD). Chronic kidney disease
often requires lifelong management and may ultimately necessitate dialysis or kidney transplantation.
Swelling Due to Kidney Failure
One common and distressing symptom of kidney failure is swelling, medically referred to as edema. Edema occurs when excess fluid accumulates in the body, leading to swelling in various areas, including the hands, legs, face, and abdomen. This swelling due to kidney failure can be uncomfortable and impact a person's quality of life. Homeopathic remedies may offer a gentle approach to alleviate edema associated with kidney failure.
Homeopathy for Kidney Health
Homeopathy is a holistic system of medicine that focuses on treating the individual and addressing the underlying causes of health issues. Homeopathic medicine for kidney disease are made from highly diluted natural substances and aim to stimulate the body's innate healing abilities.
When it comes to kidney health, homeopathy can offer several potential benefits:-
Symptom Management:
Homeopathic remedies can help manage the symptoms associated with kidney conditions, including high creatinine levels, swelling, high blood pressure, and urinary issues. By addressing these symptoms, individuals may experience improved comfort and well-being.
Individualized Treatment:
Homeopathic treatment is highly individualized, with remedies chosen based on the specific symptoms, constitution, and emotional state of the patient. This personalized approach takes into account the unique aspects of each person's condition.
Minimal Side Effects:
Homeopathic remedies are highly diluted and generally well-tolerated, making them a gentle and safe option for individuals with kidney conditions. They can be used alongside conventional treatments if necessary.
Homeopathic Remedies for Kidney Conditions
Several homeopathic remedies may be recommended for individuals dealing with kidney issues, including those with swelling due to kidney failure. These remedies are chosen based on the patient's specific symptoms like creatinine and constitution.
It's important to consult a qualified homeopathic practitioner to assess your specific condition and prescribe the most suitable remedy.
Conclusion
Homeopathy offers a natural and holistic approach to managing kidney conditions, including acute kidney injury, chronic kidney disease, and the associated swelling due to kidney failure. While it may not replace conventional medical kidney treatments in all cases, it can be a valuable complementary therapy or an alternative for those seeking a gentler and less invasive approach to kidney care. If you or a loved one are dealing with kidney-related issues, consider consulting a qualified homeopath to explore the potential benefits of kidney treatment by homeopathy in your journey to better kidney health. Effective treatment requires individualized assessment and guidance from a healthcare professional experienced in homeopathy.
If you want to know for kidney treatment homeopathy, then you can visit my original blog. The link has been provided below:
https://bharathomeopathy.com/disease/kidney-failure-treatment
#chronic kidney disease (CKD)#Low creatinine#High creatinine levels#normal creatinine levels#creatinine levels#Kidney treatment by homeopathy#Kidney treatment
0 notes
Text
Comprehensive Urine Assessment for Health Monitoring | H.R. Diagnostic

Understanding the Importance of a Urine Assessment
A urine assessment, often referred to as a urinalysis, is a key diagnostic tool. It helps in detecting various health conditions. From kidney disorders to infections, it offers insights into a person’s health. Therefore, it's essential to understand its importance and how it benefits your health.
What is a Urine Assessment?
A urine assessment involves analyzing urine samples to check for various markers. These markers include proteins, glucose, and blood cells. Each of these components can indicate different health issues. For example, the presence of protein may suggest kidney damage. However, glucose in urine can be a sign of diabetes. By evaluating these elements, healthcare professionals can diagnose and monitor various conditions.
Why is a Urine Assessment Important?
Urine assessments are crucial because they provide early warnings about underlying health conditions. Often, symptoms of diseases like kidney disease, diabetes, or urinary tract infections (UTIs) are not noticeable until the condition has progressed. However, with a routine urine test, these issues can be detected early, allowing for timely intervention.
Common Conditions Detected Through a Urine Assessment
Urine assessments can detect a range of health issues. Here are some common conditions that can be identified:
1. Kidney Disease
Kidney function is essential for filtering waste from the blood. When the kidneys are not functioning properly, waste products may accumulate in the body. This can be detected through abnormal levels of protein or creatinine in the urine.
2. Diabetes
High glucose levels in urine can indicate diabetes. Early detection through a urine assessment can lead to better management and prevention of complications.
3. Urinary Tract Infections (UTIs)
UTIs are common and can be easily identified through the presence of bacteria, white blood cells, or blood in the urine. Early treatment can prevent the infection from spreading to the kidneys.
4. Liver Disorders
Urine assessments can also reveal liver issues. For instance, bilirubin in the urine may indicate liver damage or disease.
How is a Urine Assessment Conducted?
A urine assessment is a simple and non-invasive procedure. Here is a step-by-step breakdown of the process:
Collection: A urine sample is collected in a clean container. It is important to provide a midstream sample for accuracy.
Visual Examination: The color and clarity of the urine are observed. Cloudy or dark-colored urine may indicate infections or dehydration.
Chemical Examination: Test strips are used to check for various substances in the urine. These include glucose, protein, ketones, and pH levels.
Microscopic Examination: Under a microscope, the urine is examined for cells, bacteria, and crystals.
Preparing for a Urine Assessment
For accurate results, preparation is key. Here are some tips to ensure the effectiveness of your urine assessment:
Stay Hydrated: Drink enough water before the test, but avoid excessive amounts.
Avoid Certain Foods: Foods like beets and berries can change the color of urine. Therefore, avoid them before the test.
Inform Your Doctor: If you're on medication or supplements, inform your doctor, as these can affect the test results.
Interpreting the Results
After the urine assessment, understanding the results is crucial. However, it's best to discuss the findings with a healthcare professional for accurate interpretation.
Normal Results: Clear, light yellow urine with no abnormal substances indicates good health.
Abnormal Results: Any abnormality, such as the presence of blood, protein, or glucose, may indicate an underlying issue that requires further investigation.
Regular Urine Assessments for Health Maintenance
Routine urine assessments should be part of your regular health check-up. They help in early detection and prevention of various diseases. However, they should not replace other diagnostic tests. A comprehensive approach, combining different tests, is essential for accurate health monitoring.
Benefits of a Regular Urine Assessment
Regular urine assessments come with multiple benefits:
Early Detection: Identifying potential health issues early can lead to prompt treatment.
Monitoring Chronic Conditions: For those with chronic conditions like diabetes, regular urine tests help monitor the effectiveness of treatments.
Preventive Care: Regular assessments can help prevent diseases by identifying risk factors early.
Choosing the Right Diagnostic Center
Selecting the right diagnostic center for your urine assessment is incredibly important. First and foremost, you need a facility that provides accurate results; therefore, professional care is essential. Additionally, H.R. Diagnostic stands out as a trusted name in health assessments. Not only do we use state-of-the-art equipment, but we also have experienced professionals on hand, ensuring precise and timely results. Moreover, whether you’re coming in for a routine check-up or investigating a specific concern, we are here to support you every step of the way. Therefore, you can trust us to meet your health assessment needs with the utmost care and efficiency.
Why Choose H.R. Diagnostic for Your Urine Assessment?
At H.R. Diagnostic, we prioritize your health. Here’s why you should choose us:
Advanced Technology: Our facility is equipped with the latest diagnostic tools, ensuring accurate and reliable results.
Experienced Staff: Our team of healthcare professionals is skilled and knowledgeable, providing top-notch care.
Comprehensive Services: Beyond urine assessments, we offer a wide range of diagnostic services, making us your one-stop destination for all health-related needs.
Patient-Centered Care: We focus on providing a comfortable and stress-free experience for our patients.
Conclusion
A urine assessment is more than just a routine test; it is a powerful tool for maintaining your health. Whether you're monitoring an existing condition or seeking early detection, this simple test can provide valuable insights. Therefore, make it a part of your regular health routine. At H.R. Diagnostic, we're here to support you every step of the way, ensuring you get the best care possible.
Don't wait for symptoms to appear. Book your urine assessment today and take control of your health!
Read More…..
Author Bio:
Simi Gajala has been working in digital marketing since 2018, amassing 6 years of experience. Currently Working as a Digital Marketing Executive at H.R. Diagnostics. Simi specializes in SEO, SMO, Google Ads, Meta Ads, and blogs & content writing, Boosting Brands, Increasing Visibility, And Enhancing Online Performance.
0 notes
Text
Kidney Health: Chronic Kidney Disease Treatment Naturally-Bharat Homeopathy
About Treatment for kidney failure

Our kidneys work continuously to keep us healthy. Despite their small size, these organs play a vital role in filtering waste, regulating fluid balance and ensuring our well-being. But what happens if they start to malfunction? Illnesses such as acute kidney injury (AKI) and chronic kidney disease (CKD) can put our health at risk. Apart from abdominal pain, the patient may have to face many problems. Kidney disease should be identified and examined immediately, and if it is the initial stage of the disease, then Treatment for kidney failure should be started so that it can be prevented from becoming more serious.
Diet for kidney Health?
If you are suffering from kidney disease and want to find a chronic kidney disease treatment very soon. So it is obvious that you need a good cure for chronic kidney diseases, but at the same time, it is essential to focus on your diet because diet for kidney patients has a great impact on the patient, and diet plays an important role in making the medicines effective. So you will need to change the way you eat. Now, you will have to make your diet routine not like that of a normal person but from the perspective of curing the disease and becoming free from this serious disease.
We will tell you that there are many things for kidney patients that, along with foods for healthy kidneys, are very beneficial for their kidney problems. You can enjoy food items like poha, upma, porridge, sago, and plain oats.
Include low-sodium foods like ginger, carrot, and bottled gourd vegetables. Low potassium foods: parwal, tinda, capsicum, brinjal, cauliflower, cabbage. Protein-rich foods like melon seeds and watermelon seeds, as well as tur moong dal and makhana, should be in your diet. But you have to avoid cucumbers, meat, potatoes, Rice, Avocados, Tomatoes, and Whole wheat Bread.
Food & fruits for healthy kidneys
Kidneys help eliminate toxins from our bodies and maintain the levels of many minerals, such as sodium, potassium, and acids. Many fruits are very good to consume, and some are very beneficial for patients. If you want to cure for chronic kidney disease, Keeping all these things in mind, we will tell you some of the best fruits for patients with this condition.
Berries: Blueberries, strawberries, and cranberries are high in antioxidants and vitamins, promoting overall renal health.
Apples: High in fibre and anti-inflammatory compounds, apples help maintain renal health.
Fish: omega-3 fatty acids, fish like salmon and mackerel reduce inflammation and support cardiovascular health.
Watermelon and melon contain a high amount of water, which is good for urine formation.
Avoid pomegranate seeds and eat only the red part Because it puts you at risk of developing stones.
Guava also contains good amounts of potassium and phosphorus. Also, you should not eat guava seeds.
You can include peach in your diet, but diabetic patients will have to avoid it.
Having discussed various fruits and foods beneficial for kidney patients, let's now proceed further to understand the role that dry fruits play in their lives.
Best treatment for healthy kidneys
Are you troubled by kidney problems and are looking for better kidney failure treatment without dialysis? Our Bharat homeopathic treatment of kidney is a better option for you; homeopathy treatment has many benefits, the first of which is a side-effect-free homeopathic high creatinine treatment that is completely prepared from herbs. Secondly, in the process of your treatment, our Bharat Homeopathy doctors know your complete medical history, and after that, your treatment is started, which is done keeping in mind your root causes. If you want a good body and healthy kidneys, then it is mandatory for you to adopt better treatment.
0 notes
Text
Understanding Kidney Function Tests: Why They Matter and How RML Pathology Can Help

The kidneys play a vital role in maintaining overall health by filtering waste and excess fluids from the blood, regulating blood pressure, balancing electrolytes, and producing essential hormones. When the kidneys aren't functioning properly, it can lead to a range of serious health issues, including chronic kidney disease (CKD) and kidney failure. Early detection through kidney function tests is crucial in preventing further damage and managing kidney-related conditions effectively.
What is a Kidney Function Test?
A Kidney Function Test (KFT) is a group of tests that assess how well your kidneys are working. These tests typically measure levels of waste products, electrolytes, and other substances in the blood and urine that the kidneys normally filter out. Here’s a breakdown of the key tests involved:
Serum Creatinine Test: This blood test measures the level of creatinine, a waste product of muscle metabolism. Elevated levels of creatinine may indicate impaired kidney function.
Glomerular Filtration Rate (GFR): GFR is an estimate of how much blood passes through the glomeruli (tiny filters in the kidneys) each minute. It’s derived from serum creatinine levels and is used to assess the stage of kidney disease.
Blood Urea Nitrogen (BUN) Test: BUN measures the amount of nitrogen in your blood that comes from the waste product urea. Higher than normal levels may suggest that the kidneys are not filtering effectively.
Urine Albumin Test: This test checks for the presence of albumin, a type of protein, in the urine. Protein in the urine can be an early sign of kidney damage.
Electrolyte Levels: Tests for sodium, potassium, and other electrolytes help assess the balance of fluids and electrolytes in your body, which the kidneys regulate.
Why Kidney Function Tests are Essential
Kidney diseases often progress slowly and silently, with few noticeable symptoms until the condition is advanced. Regular kidney function tests are essential for:
Early Detection: Identifying kidney damage or dysfunction at an early stage allows for timely intervention, potentially slowing the progression of disease.
Monitoring Chronic Conditions: For individuals with conditions like diabetes, hypertension, or a family history of kidney disease, regular kidney function tests are crucial for monitoring kidney health.
Guiding Treatment: The results of kidney function tests can help doctors tailor treatment plans, manage medications, and make lifestyle recommendations to protect kidney health.
Who Should Get a Kidney Function Test?
While everyone should consider getting a kidney function test as part of routine health check-ups, it is especially important for those who:
Have high blood pressure or diabetes
Have a family history of kidney disease
Are over the age of 60
Are experiencing symptoms like swelling in the legs or ankles, frequent urination, or fatigue
RML Pathology: Your Trusted Partner for Kidney Function Testing
At RML Pathology, we understand the importance of accurate and timely diagnostics in maintaining your health. Our Kidney Function Test panel is designed to provide comprehensive insights into your kidney health, helping you take control of your well-being.
Why Choose RML Pathology?
State-of-the-Art Technology: Our laboratory is equipped with advanced diagnostic technology to ensure precise and reliable results.
Experienced Professionals: Our team of skilled pathologists and technicians is dedicated to delivering high-quality care and accurate diagnoses.
Convenient Services: We offer home sample collection services, making it easy and convenient for you to get tested from the comfort of your home.
Comprehensive Reporting: Our detailed reports provide you with a clear understanding of your kidney health, enabling informed discussions with your healthcare provider.
How to Book Your Kidney Function Test
Booking your Kidney Function Test with RML Pathology is simple and hassle-free. You can visit our website at www.rmlpathology.com or call us at 7991602001 to schedule your test. Our team is available to assist you with any questions and guide you through the process.
By choosing RML Pathology, you’re taking a proactive step towards safeguarding your kidney health. Remember, early detection is key to preventing and managing kidney disease effectively. Don’t wait for symptoms to appear—schedule your Kidney Function Test today and take control of your health.
Stay Informed, Stay Healthy, with RML Pathology.
Contact Information:
Address: B-171, Nirala Nagar, Lucknow - 226020
Website: www.rmlpathology.com
Phone: 7991602001, 7991602002
#KidneyHealth#RMLPathology#KidneyFunctionTest#HealthCheckup#PreventiveCare#StayHealthy#Diagnostics#ChronicKidneyDisease#KidneyDiseaseAwareness#PathologyServices
1 note
·
View note
Text
Albumin & Creatinine Tests Market Unlimited Opportunities for New Companies, Forecast to 2024-2032

The Reports and Insights, a leading market research company, has recently releases report titled “Albumin & Creatinine Tests Market: Global Industry Trends, Share, Size, Growth, Opportunity and Forecast 2024-2032.” The study provides a detailed analysis of the industry, including the global Albumin & Creatinine Tests Market Size share, trends, and growth forecasts. The report also includes competitor and regional analysis and highlights the latest advancements in the market.
Report Highlights:
How big is the Albumin & Creatinine Tests Market?
The albumin and creatinine tests market size reached US$ 1,284.5 million in 2023. Looking forward, Reports and Insights expects the market to reach US$ 4,344.9 million in 2032, exhibiting a growth rate (CAGR) of 14.5% during 2024-2032.
What are Albumin & Creatinine Tests?
The albumin and creatinine tests are standard methods for evaluating kidney function and detecting early signs of kidney damage. The albumin test measures the levels of albumin, a blood protein, while the creatinine test measures creatinine, a muscle waste product. Normally, the kidneys prevent albumin from entering the urine and maintain stable creatinine levels. However, if kidney function is impaired, albumin may appear in the urine, and creatinine levels may increase. These tests are typically conducted together, either as a urine test (albumin-to-creatinine ratio) or a blood test, providing a comprehensive assessment of kidney health.
Request for a sample copy with detail analysis: https://www.reportsandinsights.com/sample-request/2045
What are the growth prospects and trends in the Albumin & Creatinine Tests industry?
The albumin and creatinine tests market growth are driven by various factors and trends. The market for albumin and creatinine tests is expanding as kidney disorders become more prevalent and early diagnostic tools are increasingly sought after. These tests play a critical role in assessing kidney function and identifying conditions like chronic kidney disease. Market growth is driven by factors such as an aging population, lifestyle shifts leading to kidney-related issues, and advancements in diagnostic technology. Moreover, the growing emphasis on preventive healthcare and the significance of routine health screenings are also contributing to the increased demand for albumin and creatinine tests. Hence, all these factors contribute to albumin and creatinine tests market growth.
What is included in market segmentation?
The report has segmented the market into the following categories:
By Type
Urine Albumin Tests
Urine Creatinine Tests
Glycated Albumin
Micro Albumin Test
Blood and Serum Creatinine Tests
By Product
Cartridges
Cartridges for POC Analyzers
Cartridges for Table-Top Analyzers
Dipsticks Kits
Analyzers
Reagents
Other Consumables
By Application
Kidney Disease Diagnosis
Diabetes
High Blood Pressure
Kidney Screening
Others
By End-User
Hospitals Clinics
Diagnostic Laboratories
Research Laboratories Institutes
By Region
North America
United States
Canada
Europe
Germany
United Kingdom
France
Italy
Spain
Russia
Poland
Benelux
Nordic
Rest of Europe
Asia Pacific
China
Japan
India
South Korea
ASEAN
Australia New Zealand
Rest of Asia Pacific
Latin America
Brazil
Mexico
Argentina
Middle East Africa
Saudi Arabia
South Africa
United Arab Emirates
Israel
Rest of MEA
Who are the key players operating in the industry?
The report covers the major market players including:
Abbott
Roche Diagnostics
Fujifilm Wako Pure Chemical Corporation
Nova Biomedical
Ortho Clinical Diagnostics
Danaher
Siemens Healthcare Gmbh
Promocell Gmbh
Sysmex Corporation
Thermos Fisher Scientific Holdings, Inc.
View Full Report: https://www.reportsandinsights.com/report/Albumin & Creatinine Tests-market
If you require any specific information that is not covered currently within the scope of the report, we will provide the same as a part of the customization.
About Us:
Reports and Insights consistently mееt international benchmarks in the market research industry and maintain a kееn focus on providing only the highest quality of reports and analysis outlooks across markets, industries, domains, sectors, and verticals. We have bееn catering to varying market nееds and do not compromise on quality and research efforts in our objective to deliver only the very best to our clients globally.
Our offerings include comprehensive market intelligence in the form of research reports, production cost reports, feasibility studies, and consulting services. Our team, which includes experienced researchers and analysts from various industries, is dedicated to providing high-quality data and insights to our clientele, ranging from small and medium businesses to Fortune 1000 corporations.
Contact Us:
Reports and Insights Business Research Pvt. Ltd.
1820 Avenue M, Brooklyn, NY, 11230, United States
Contact No: +1-(347)-748-1518
Email: [email protected]
Website: https://www.reportsandinsights.com/
Follow us on LinkedIn: https://www.linkedin.com/company/report-and-insights/
Follow us on twitter: https://twitter.com/ReportsandInsi1
#Albumin & Creatinine Tests Market share#Albumin & Creatinine Tests Market size#Albumin & Creatinine Tests Market trends
0 notes
Text
Understanding the DLPL Fever Profile Test
The DLPL (Dr Lal Pathology Lab) fever profile test is a comprehensive diagnostic tool designed to identify the root causes of fever, one of the most common symptoms of a wide range of medical conditions. This profile includes a series of tests that examine various bodily fluids and functions to provide a detailed overview of the potential infectious or inflammatory processes at work.
What is Included in the DLPL Fever Profile Test?
The specific tests included in a fever panel may vary based on the patient's symptoms or as suggested by the physician. Typically, it encompasses:
Complete Blood Count (CBC): This test measures different components of the blood, including red and white blood cells and platelets. It helps detect infections, inflammation, and other hematological conditions.
Erythrocyte Sedimentation Rate (ESR): ESR measures how quickly red blood cells settle at the bottom of a test tube. A faster-than-normal rate may indicate inflammation in the body.
C-Reactive Protein (CRP): CRP levels rise in response to inflammation. High levels can suggest an acute inflammatory process or infection.
Liver Function Tests (LFTs): These tests assess the health of the liver by measuring levels of enzymes, proteins, and substances produced or cleared by the liver.
Renal Function Tests (RFTs): These tests evaluate kidney performance by measuring levels of waste products like urea and creatinine in the blood.
Blood Cultures: To detect the presence of bacteria or fungi in the blood, indicating a bloodstream infection.
Urinalysis: This test checks for signs of infection, kidney disease, and other medical conditions by examining the appearance, concentration, and content of urine.
When Should You Consider the DLPL Fever Profile Test?
At the start of an infection or during the incubation phase, a person may feel lethargic or have a fever. It is recommended to visit a doctor and get tested at this point to determine the exact cause. Persistent or unexplained fever warrants a detailed investigation to rule out serious underlying conditions.
Benefits of the DLPL Fever Profile Test
Comprehensive Diagnosis: The test covers a wide range of potential causes of fever, providing a holistic view of the patient's health.
Early Detection: Identifies infections and inflammations early, allowing for prompt treatment.
Guided Treatment: Helps physicians tailor treatments based on specific findings, improving patient outcomes.
Conclusion
The DLPL fever profile test is an essential tool in the diagnostic arsenal for managing fevers. By providing a thorough analysis of various biomarkers and organ functions, it aids in identifying the precise cause of fever, ensuring that patients receive appropriate and timely treatment. For anyone experiencing persistent or severe fever symptoms, consulting a healthcare provider and considering a DLPL fever profile test could be a crucial step toward recovery.
0 notes