#creatinine means
Text
#Kidney#creatinine#serum creatinine#normal creatinine levels#high creatinine level#what is creatinine?#creatinine means
0 notes
Text
I got bored, frankly, it's annoyance if anything, of going to my university library. To remedy that I've been going to a public library branch and today it really made my day!
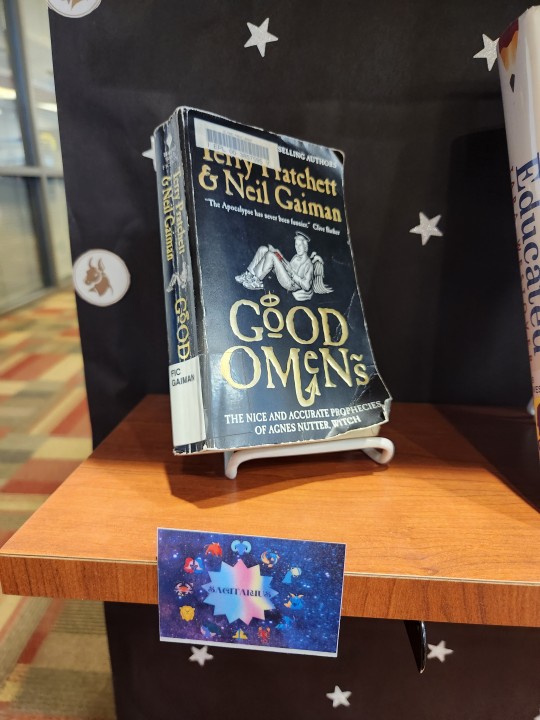
They had a display about book recommendations based on zodiac signs. I always find zodiac themed items a little funny, and naturally, I wanted to see what would be deemed a good Sagittarius, my own zodiac sign, recommendation. I had actually been looking for my libraries collection of Neil Gaiman books the day before and was disappointed when GO wasn't there. Well, now I know why. 🥰
Anyways I spent the last 30 minutes before I had to leave reading and giggling to myself. 🤭
#i do think they should have put it under Libra#but i mean i guess its whatever#i honestly did a double-take cause like wtf!?!#i was so invested in my NPN notes that GO was the very last thing on my mind#my literal thought process went from#doo do doo creatinine kinase is found in skeletal and heart muscle and brain tissue clickity clack#*i look up cause idk if a woman passing by was gonna stop to ask me something but she didnt so i take a quick look around*#oh GO#clickity clack#GOOD OMENS?!?! 🤯#and then i finished studying for the day and went to get it and got a dirty look from an old man cause he thought i was inappropriately#dressed. like my dude disrespectfully im here on my own time and i wanna grab the book ive been wanting to read for a long time now#i can finally drive myself around and be out of the house for quite a bit longer than if my parents were to pick me up and give me a ride#everywhere i need to go. i dressed comfy for myself and no one else. you can go if it bothers you that much#whoa didnt expect to get into that...my bad y'all#i digress im really happy i got my hands on go. now i have a book im really looking forward to at the end of my study sessions.#good omens 2#good omens#crowley#OMG Y'ALL AND ITS THE CROWLEY VERSION MY HEART!!#“get humans wet and staring into each others eyes va-voom! sorted”#me too crowley me too#the power of getting humans wet and staring into each others eyes#ok this is getting longer than i was originally intending
4 notes
·
View notes
Text
Understanding Microalbumin Creatinine Ratio: A Comprehensive Guide To Kidney Health
Are you familiar with the microalbumin creatinine ratio, a crucial parameter in the world of kidney health? In this comprehensive guide, we will delve into the significance of this ratio, how it aids in evaluating kidney health, and its role in detecting early signs of kidney damage. We'll explore the normal ranges, its importance for individuals with conditions like diabetes or high blood pressure, and the straightforward formula for calculating it. Let's embark on a journey to understand how the microalbumin creatinine ratio plays a vital role in maintaining healthy kidneys.
#protein in urine#creatinine test#kidney function test#urine test#renal function test#creatinine meaning#albumin creatinine ratio#albumin creatinine#microalbumin normal range#microalbumin creatinine ratio#what is microalbumin
0 notes
Text
here's a perfect example of how medical misogyny kills women
for anyone who can't watch the video, he's basically saying that high levels of creatinine can indicate kidney problems, which is why it's key feature for determining who needs a liver transplant first. the issue with this is that it doesn't account for creatinine-to-muscle ratios, meaning that men typically have artificially higher numbers because they typically have more muscle mass. while women's numbers may look low, they're actually high in relation to their muscle mass. basically, the system was designed based on male bodies
949 notes
·
View notes
Text
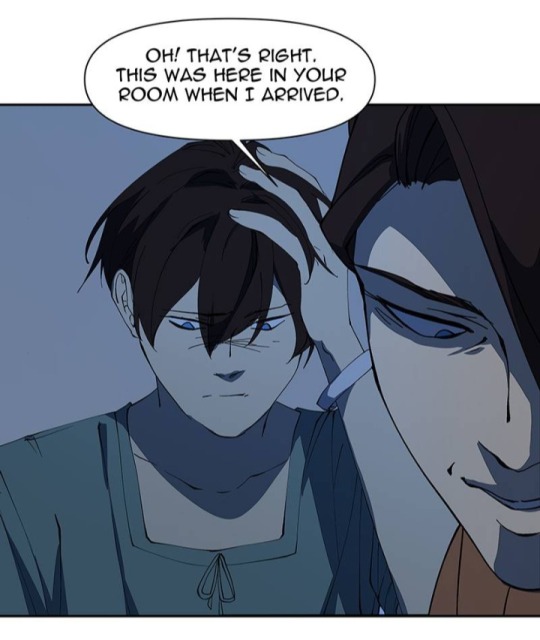
I LOVE YOO 220 Thoughts
1. What excites me the most on this episode is, we got a glimpse of how Yui abused Nol in the past! (Not that I enjoy seeing Nol being abused, far from it, but I'm glad we finally see the plot moving) This is the discussion back in ep 150:

And with today's episode, we now see how Yui utilizes her power as the owner of the hospital: interfering with the doctors and nurses' decision, having their license revoked if they try to defy her, rewarding them with money -or anything- if they do as she say... Of course Yui's hand would stay clean if everyone is too scared of her! It really give us a glimpse of how she abused Nol in the past. Ugh. Now I wonder, did he also had the nurse he's close with removed from his sight because of Yui? Did she also gaslighted him into thinking it's his fault? 😒
Hearing Yui's argument is laughable actually. When a patient is unconscious, a doctor has the right to do some tests based on medical judgement in order to reach the correct diagnosis for the right treatment, because a sleeping patient can't tell the doctor what's wrong with them afterall. She has no right to veto as a mother too(?), since Kousuke is already an adult. Now, whether the CEO of the hospital has the right to revoke a medical lisence based on personal opinion -- or not, I can't tell because I don't know the laws. But well, money and power goes a long way, sadly.
2. At least Nol wakes up with the person he care by his side. Kousuke wakes up with no one in sight, and the sound of arguments outside. Quimchee just loves hammering down Kousuke's sign of neglection, huh. As much of an asshole Kousuke is, he's still the victim of abuse just like Nol :(
3.

AW NAH BITCH, STAY AWAY FROM JAYCE. STAY AWAY FROM NOL. JUST GO AWAY, NO ONE WANTED YOU HERE.
4. Now, about the reason why Yui is so adamant not letting Kousuke be tested by a literal professional. Many people has guessed it's because Yui doesn't want anyone to find out Kousuke is not Rand's biological son, but I don't think we're there yet. Hansuke mentioned basic tests; as far as I know, the basic, standard tests don't include blood-type test or DNA test. It usually only covered the potentials of:
Irregularity in blood (haemoglobin, platetet, RBC counts)
Infection (WBC, Lymphocyte counts)
Liver disfunction (AST, ALT)
Kidney disfunction (Creatinin, Urea, Bilirubin)
Diabetes (blood sugar)
Cholesterol-based illness (LDL, HDL, triglycerides)
Irregularity in electrolytes (Na, K, Cl, Ca)
And that's the gist of it. There's not much to get, unless Yui doesn't want anyone to find out Kousuke is actually diabetic? Maybe she inserted diabetes medicines inside his food? Kousuke did say they have personal chefs, maybe they also received Yui's order. I kinda doubt it though, this seem like a stretch.
It's a different story if Hansuke wanted to check the possible substance inside Kousuke's body, though. Hansuke suspected Kousuke is under the influence; it's the easiest answer that could explain Kousuke's abnormal behavior.

This is just some wild theory but I suspect Yui inserted some antipsychotic drugs in his drink or food (remember the family chefs?) to keep Kousuke in check. If Hansuke finds out about it, it will reveal that Yui has been hiding the fact that Kousuke has some mental disorder, and that could jeopardize his position as the new CFO; that's why Yui doesn't want a blood work. Just a guess 💀
Btw, this is Shinae on episode 14 LMAO

Oh Shinae. Now this doesn't seem like a joke anymore ☠️
Oh. WAIT.


💀💀💀
5. [Yui: what has you scrambling around in distress?] [Kou: I can't recall... ] [Yui: Aww that's too bad...]
Look at that sinister smile. She is DELIGHTED Kousuke forgets. Since Yui knew he hit his head on the wall, I think it's safe to assume(?) she knows Kousuke was looking at patient record earlier. She knows which name that triggers him. Does it mean she doesn't want Kou to find out about Nessa (further, what she did to her)? Has Yui always used Kou's "ignorance" (memory issue) about Nessa's fate to let him mock Nol about her disappereance?
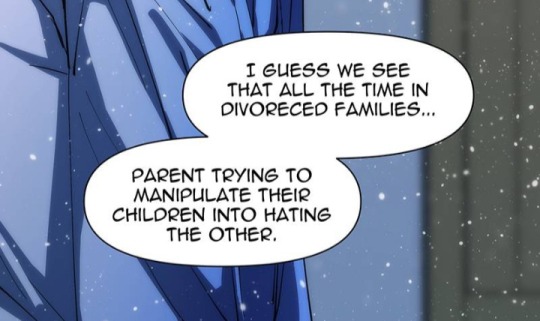
Nol you couldn't be more right. I look forward to see Kou finding out he has been mocking Nol's mom's absence when it's his own "dear mother" who "killed" her. The devastation...
6. I still don't get why would Yui throw away Rand's gift. If anything, I think it'd benefit her more if she give it to Kousuke. Something like: praising him, how he's done such a good job being a CFO that his father would give him an early expensive present, gaslight him into thinking it's not enough, but just a little more until he'd truly acknowledge him, etc. I thought he'd be easier to manipulate if he get enough reward (which he clearly didn't get)? It feels like Yui's manipulation is getting old. Idk, I thought a goal would be much sweeter if he get to taste it, so he'd work even harder. But so far, he didn't taste any of it.
But then it hit me. If Kousuke sees the real present, he'd know his father does care about him. He won't need Yui anymore, he'd start to rely on Rand, as in, the person. And Yui doesn't want that. She wants Kousuke to be fully in her control, she wants him to keep relying on Rand's image by her words; that Rand is a cold man who doesn't care about his family unless Kousuke surpassed him. She just... never let Kousuke to be free. (Which is why I realized Nol has the potential to be a much scarier manipulator than Yui, but that's another topic for another day).
7. Yui touching Kousuke's injured hand without apologizing is such a psychopath thing to do: lacking of guilt or empathy.
8. BAHAHA since we're almost at the end of the year, it's nice to see the reference of earlier episode!


Though, could this be a foreshadowing? If Shinae really becomes Kousuke's assistant in the future, would she be included in the future hospital inspection? Would she play a role in uncovering Nol and Kousuke's mistreatment in the hospital? Lol.
9. MEG!! AOEBJDDJ I hope she would return the gift to Kousuke, just like Shinae who return the bible to Nol! Kousuke needs to know Rand is more caring than he seemed and Yui is much more wicked than he thought! This is probably Meg's role as the member of the Black Team: to open Kousuke's eyes that he still has people who care for him as who he is.
And that's it! See you next week 👋
#i love yoo#ily#ily 220#i love yoo webtoon#line webtoon#quimchee#kousuke hirahara#yui hirahara#ily theory#ily analysis
61 notes
·
View notes
Text
Psittacosis
Let's open with a case report, like we're on an episode of house.
Case Report
35 yo otherwise well, suddenly presents with 2/52 of high fevers and a headache (usually this means > 39)
a/w chills and rigours, responsive to medication/presumably panadol and intermittent (would resolve then come back)
no respiratory symptoms
She had neutrophilia and intrestingly, a CRP of merely 30.
CXR revealed nonspecific consolidation in 2 lobes, they followed this up with a CT revealing pretty impressive ground glass opacities (or GGOs)

She was empirically treated on IV tazocin only (I'm used to atypical coverage empirically started if there's even a whiff of resp, which she may not have had symptoms but her CXR confirms this)
eventually she was on referred to the authors, who felt her CT findings with consistent with psittacosis and treated her with doxycycline which resolved her symptoms in 48 hrs
on further history, it was revealed that she had parrots at home, one had died 2 days preceding her symptoms and she was sleeping next to its body at night (crazy)

What is it:
psittacosis is a zoonoses (transmitted by animals, animals = reservoirs), in this case, transmitted by birds. Orthinoses if birds in general, but psittacosis if referred to macaws, parrots etc. YOu can also catch it from chickens and turkeys.
Some what related is Bird fancier's lungs. Which just sounds fancy.. I'm sure it's just an old term.

Bird fancier's lung refers to a hypersensitivty pneumonitis (ILD) caused by bird exposure. DIfferent disease process, but birds is the come denominator. INhaled bird particles
Psittacosis specifically refers to the infective disease process caused by a bacteria. It was 'identified" or reported in the 1870s, when a cluster of 7 swiss patients developed the same symptoms and found to have possessed tropical birds.
Similarly, in the 1930s there was an outbreak in the US with a mortality of up to 20% (80% in pregnant women), also attributed to parrots from South America.
Eventually, with further scientific development, the causative pathogen was identified as chlamydia psittaci, an atypical intracellular organism.
Psittacosis is a significant differential to consider in community acquired pneumonia as it has a high mortality if left untreated. But it is rare, and causes about 1% of cases in the US. Part of this is due to improved hygiene practices and strict importation guidelines of tropical birds.
It's spread through the inhalation of dust with either dried faeces or respiratory secretions from infected birds.
Clinical features
Variable! but the key thing on history is birds
incubation time can be anywhere from 2 days to 20
Flu-like (fevers/chills/myalgias/arthralgias/malaise/headache)
high fevers is key
respiratory symptoms - does not always present as per the case report, and can be mild on spectrum (dry cough) to more severe
if systemic, can also get photophobia, deafness and epistaxis
Rare (particularly where doxycycline or azith are prescribed at a low threshold): hepatosplenomegaly (look out for LFTs), GI symptoms (remember CAP can present with diarrhoea, nausea/vomiting --> always do a CXR)
even rarer: endocarditis or myocarditis, encephalitis or hepatitis (usually the complications of untreated disease)

Increased risk groups:
pet shop owners
bird owners
farmers
zoo, lab workers where birds are kept, vets, avian quarantine station workers
poultry handlers/workers
So ask if they live or work with birds, or had recent exposure.
INvestigations
serology is gold standard - so looking for antibodies in blood tests
it's intracellular - so hard to culture if even possible on standard blood cultures
elevated ESR/CRP may see LFT derangement and creatinine rise in systemic illness
CXR- usually lower lobe changes, if CT is done, you can get pulmonary infiltrates with GGOs
Treatment:
usual culprits for atypical coverage: azithromycin 3 days or doxycycline 100 mg BD for 14/7
Differentials
always broad if systemic features only (also consider IE and other causes of sepsis)
with resp symptoms - legionella, Q fever, mycoplasma, tularaemia (except for tularaemia, the rest are also covered by doxycycline)
In clinical practice, I'm so used to just having atypicals on board for any cases of atypical pneumonia. I really take it for granted. But will consider this differential more myself in cases of PUO - but I feel like there should be at least CXR findings regardless.
Anyway, prognosis is very good so long as it is treated.
Sources:
CDC guidelines
Case Report: Importance of Clinical history in Psittacosis
StatPearls
Wiki
#psittacosis#chlamydia psittaci#community acquired pneumonia#infectious diseases#infectious disease#medblr
9 notes
·
View notes
Text
creatinine kinase levels are still elevated 8 months later which means some muscle in my body (or my fucking brain) has been deteriorating and leaking into my blood this whole time. and like my skeletal muscles seem fine so that doesn't bode well for my brain
but guess who does not have toxoplasmosis. not to brag but turns out i love my cats an inordinate amount without pathogen influence....
5 notes
·
View notes
Text
join me in pell (piss hell)
Let's talk kidneys!
Your kidneys are situated:
Inferior to the liver and the suprarenal glands
Superior to the ureters
Anterior to the posterior wall of abdomen and diaphragm
Posterior to the peritoneum (sack with yer guts in it)
Their job is to:
Regulate blood ions (like sodium) and control blood pH
Maintain blood volume (by extracting or conserving water)
Secrete hormones
Excrete toxic waste (urea, ammonia, creatinine…)
Guess what shape they are. Go on, guess.
YEAH THAT’s RIGHt – IT’S BEAN TIME, BITCHEs

[CW: beneath the cut you will find CT images of kidney trauma]
(and here is some very basic anatomy, sketched on… that same bean)
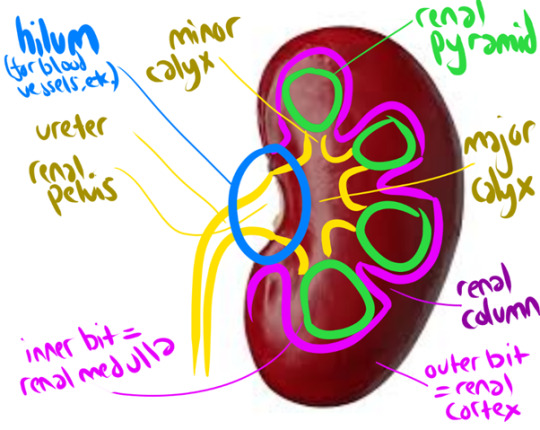
The renal cortex + renal pyramids together form the PARENCHYMA, aka the functional bit of the kidneys (aka where your peepee is made)
But HOW is that peepee made, I hear you cry?
Lemme introduce you to my good friend
The Nephron
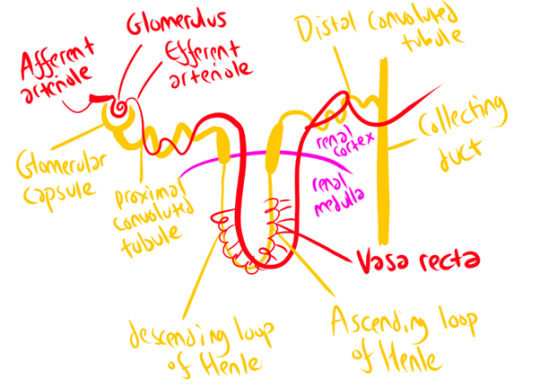
The afferent arteriole carries blood to the Glomerulus (which isn’t actually some weird DnD spell – just a knot of arteries surrounded by the Glomerular Capsule!) This arteriole then slims down considerably to form the efferent arteriole. This pressure increase forces loads of waste products and water out of the bloodstream into the glomerular capsule – but the holes in the arteriole wall are too small to release blood cells, plasma proteins, and other large molecules. This part of the nephron is called the ‘corpuscle’ (again, not a DnD spell). It’s where your blood plasma gets filtered!
The arteriole then follows the nephron around its windy path, wrapping around it at several points – notably the proximal/distal convoluted tubules, and the Vasa Recta that runs parallel to the Loop of Henle. To horrifically simplify a complex process, this provides lots of opportunities for secretion (Bad Stuff to be squeezed out of the blood – those dangerous ions and waste products we talked about earlier!) and selective reabsorption (Good Stuff (water) gets squeezed back in). It’s a careful balancing act, orchestrated in part by hormones! The end result (theoretically) is that all the stuff you DON’T want is shlorped into the nephron as urine, and all the water you need is shlorped back into the blood.
Once your kidneys have produced your peepee, it takes a fun rollercoaster ride through a series of ducts and tubes! Collecting duct -> papillary duct -> minor calyx -> major calyx -> renal pelvis -> ureter -> urinary bladder -> urethra -> you know the rest.
Your kidneys produce 180 litres of fluid a day (aka, a hell of a lot) but most of this is reabsorbed in these little nephrons, with water & useful solutes going back into the bloodstream! As a result, you only pee about 1-2 litres a day (though I swear I feel closer to the 180 litres some days)
Because kidneys are SOOOO important (your body does NOT like to be full of urea/ammonia/sodium, or acid!) they’re really, really vascular (lots of blood supply). They receive up to 25% of your resting cardiac output! So, when you’re just chilling, literally 25% of your blood is being gobbled by those hungry, hungry kidneys!
This means the kidney is VULNERABLE TO TRAUMA.
Although kidney trauma can be picked up on Ultrasound, we will take anyone who has suffered abdominal trauma through to CT, as you get better pictures there! We usually use a multiphase protocol – a longer scan, basically – to show us the extent of the injury, with a non-contrast phase (shows calculi clearly), an arterial phase (evaluates any injury to the renal arteries), a nephographic phase (shows renal lesions clearly), and a delayed phase (shows bleeding and injuries to the urinary collection system). Basically, contrast quickly moves to your kidneys from your blood stream, and filters through the collection system – so if we give a bolus of contrast and watch it flood through the renal arteries, then wait a little while, we can see how the kidneys are processing it or if it’s spilling into the surrounding space.
Kidney trauma is graded from 1 (no laceration but a haematoma (bruise) within the kidney capsule) to 5 (kidney torn away from renal vascular system and dying as a result, actively bleeding, structure of kidney shattered). Here’s a grade 5 (Left (looks like the right side of the image)) in comparison to the normal healthy kidney (Right (looks like the left side of the image)). Note the massive visible laceration + huge haematoma!


Loooooads of other stuff can go wrong with your kidneys too – but that’s a whole other post! Which I will make, one day soon, because it's super fascinating!
(Have you ever heard of a stag horn calculus? It will put you off holding onto your pee FOR LIFE. If you're sitting there kinda needing the loo but not going... GO NOW. PLEASE.)l
18 notes
·
View notes
Text
Nothing in my day-to-day job shows me the limits of modern medicine like vancomycin does. And it makes me insane.
(extremely long, somewhat incoherent nerd rant below the cut)
See, vanc is really good at, like, three things: treating MRSA (when given IV), treating ampicillin-resistant enterococcus (when given IV), and treating c diff (when administered orally ONLY). Most every use outside of that, like when it’s used to treat methicillin-susceptible staph aureus for “penicillin allergic patients” (don’t get me started on PCN allergies), actually has data that it increases risk of morbidity and mortality (i.e. harm and DEATH).
Unfortunately, due to the prevalence of multi-drug resistant organisms, vancomycin is empiric therapy for a lot of presumed infections. And it's a lot more difficult to actually tell if someone has an infection than you'd think. A lot of medical conditions imitate each other and when time is of the essence to identify what's going on, the most ethical thing is to start an antibiotic and rule out infection as the hospitalization continues. Lab techniques have gotten a lot quicker: I can remember 8 years ago, it would take 3 days just to identify what microbe the patient had in their presumed infection. These days, anno domini 2023, PCR comes back in a matter of hours, identifying gram positive/gram negative staph/strep/bacilli/etc, and it's the sensitivities that take 2-3 days. (Don't get me started on contaminated cultures.) But even with improvements in lab technique, we might not culture any microbe at all or the provider might keep vancomycin on "just in case" because we don't know IF the patient is infected, WHAT they're infected with, or if the infection will get better with a different drug.
And vancomycin is terrible on kidneys. Extremely nephrotoxic. It isn’t as bad as the 80s when the drug first came out and was called Mississippi Mud colloquially, but it will fuck the patient up if not monitored closely.
But finding the correct dose for each patient in a timely manner is nigh impossible. This is because vancomycin is renally eliminated. We have to mathematically estimate how well the kidneys are working. Unfortunately, our mathematic equation is next to useless if you are:
-Less than 50 kg
-Shorter than 5 foot tall
-Have a BMI of more than 40
-Are an adult younger than 45 (twenty-year-olds get astronomical doses that would be destructive in an older patient)
-Are older than 65 (the official definition of 'geriatric', i'm relatively sure)
-Are female (this is really only applicable if the patient is less than 50 kg or older than 65 - think: little old frail lady - we have absolutely no fucking idea how their kidneys are doing until we order the serum drug level. It is next to impossible to accurately dose vancomycin in little old ladies on the first try.)
-Are missing limbs (lots of leg amputations in the older and impoverished diabetic population!!)
-Have a lot of muscle mass (think bodybuilder or really tall guys)
Fun fact: we estimate renal function by looking at height, weight, age, birth gender (few, if any, studies on trans patients taking HRT), and a lab value called serum creatinine. Creatinine is a byproduct of muscle metabolism, I don't know the fine details, but we can generally estimate how well kidneys are working by seeing how much creatinine is in the blood: low creatinine usually means kidneys are excreting it as they 'should' be. High creatinine means there's something wrong, the kidneys aren't able to excrete it as efficiently as they 'should' be. But the effect of low muscle mass and high muscle mass haven't been studied enough to be able to adjust our mathematical equation to compensate for them. And with high BMI: we often overestimate their renal function because we don't know how to estimate their muscle mass vs their body fat.
(I work out in the boonies. ~70% of our patients have diabetes. ~80% of our patients have a BMI of greater than 35. So what I'm trying to say here is: we are shooting in the fucking dark when we're estimating the renal function of the vast majority of our patients.)
Complicating this: vancomycin is useless until it reaches steady-state concentration in therapeutic range. On one side of this problem: a lot, if not most, medical providers assume that vancomycin starts working its magic from the first dose. So we sometimes get orders for "vancomycin 1 gram now and see how the patient is doing in the morning". That isn't going to solve jack shit! That's just going to increase the incidence of microbial resistance!!
OR, like in the multiple situations I dealt with this afternoon, you make an educated guess on what regimen is going to work for the patient. You get a level 48 hours after the dose starts. And you find out that you fucking guessed wrong and the patient is subtherapeutic. It has been two fucking days and the patient hasn't started being treated for their (presumed) infection yet!! And we've increased the possibility of microbial resistance! *muffled screaming in frustration*
So what I'm trying to say here is: on almost every presumed infection that comes into the hospital (which we're guessing like 30%? 50%? of the time), we're starting an extremely toxic drug, oftentimes 100% guessing what regimen will be therapeutic, only finding out in 2 days that it is not therapeutic, and it can sometimes take days and days to titrate the dose sufficiently to find a therapeutic regimen. And sometimes we're really fucking unlucky and we destroy the patient's kidneys temporarily (or permanently! but kidneys can be very resilient so that's thankfully rare) because we guessed a regimen that's too high!! This is a fucking nightmare!!!!!!!!
And if all of this wasn't bad enough, we don't really have any drugs that do what vancomycin does therapeutically. We have things that can be used to cover some of what vancomycin does, but nothing that's equivalent AND less toxic.
Like, to fix this situation, we need:
-Better education to providers on what drugs are appropriate empiric therapy for different presumed infections (we're working on it, we are working on it)
-Better ways to estimate kidney function (there needs to be more research on kidney function in patients with BMI greater than 35!! And little old ladies!! And patients with low body weight and high body weight and amputations and...)
-Better prognostic tools to tell 1. when the patient is infected (looking at you, sepsis!!!) 2. what they're infected with
-Less-toxic antibiotics AND/OR better ways to treat infection (this would be the evolution of medicine as we know it)
And I want to be clear: vancomycin isn't bad. It's an extremely effective tool when used correctly but we often either don't have enough data to use it correctly or the provider doesn't understand that this tool is fucking useless for the job they're trying to perform.
#some days i'm just smacked in the face by the limits of modern medicine#there is so much we don't know!!!#we're doing the best we can!!!#negativity#personal#us healthcare#i understand other hospitals will have a different experience than this#but my corporation is extremely stingy and we get all the new grads#so educating providers and nurses is a never-ending wheel at my facility#and we don't treat anything complicated except orthopedic surgeries#some days I just get overwhelmed by how little we know#if you can guess my profession on the first try please keep it to yourself i'm trying to maintain a low profile here okay#also if you ask me medical questions don't expect an answer#i was a Cs Get Degrees student all I know i've learned on the job and I don't know shit
6 notes
·
View notes
Text
This is a PSA-
Just because one of your lab values is outside of a normal range does not actually indicate something is wrong. Nearly every human on the planet, including healthy ones, will have a couple of labs outside of “normal” limits. Just because your physician didn’t explain to you why your creatinine was low doesn’t mean they missed something.
21 notes
·
View notes
Note
Hi Wayfaring! My dad found out that he has kidney disease from his autoimmune disease getting worse. We hear a lot of terms like kidney function % and protein being in his urine. Would you please do a lil rundown on kidney disease and what these things mean? Can kidney function improve and can the cells regrow or is it just that he needs to stop it getting worse because they can’t be repaired? Thank you :)
Ok, here’s some basic definitions for kidney disease:
- GFR or creatinine clearance: a number indicating how well the kidneys are filtering proteins and other wastes out of the blood. A normal GFR would be >60. When they’re talking about % of normal kidney function that’s more of a layman’s term and isn’t as specific.
- chronic kidney disease: broken down into stages defined by GFR or creatinine clearance. Stages 1 and 2 are essentially normal kidney function. Stage 3 (3a is a GFR of 45-59. 3b is GFR of 30-44) is where we start having to adjust dosages on certain drugs because the kidneys don’t clear them as quickly as normal. Stage 5 (GFR of <15) is end stage renal failure, where a person would be on dialysis and/or a transplant list.
- protein being in the urine is basically from leaky filters. There are lots of things that can cause protein in the urine.
Kidney function can improve depending on what is damaging it. In the case of an autoimmune disease, it typically clogs up the filtration system with antibodies, so as the antibodies decrease, the filtration improves. The problem comes when things get so clogged up that the tissue can’t get adequate oxygen and dies. That would not be reversible and the kidney does not regenerate like the liver does. Knowing whether the damage was permanent or not would really require a kidney biopsy. Ultimately with kidney disease you try to slow down progression of disease as much as possible to prevent having to move to dialysis or transplant.
15 notes
·
View notes
Text
Medical Abbreviations on Pharmacy Prescriptions
Here are some common medical abbreviations you may see on pharmacy prescriptions:
qd - once a day
bid - twice a day
tid - three times a day
qid - four times a day
qh - every hour
prn - as needed
pc - after meals
ac - before meals
hs - at bedtime
po - by mouth
IV - intravenous
IM - intramuscular
subQ - subcutaneous
mL - milliliter
mg - milligram
g - gram
mcg - microgram
stat - immediately, right away
NPO - nothing by mouth
cap - capsule
tab - tablet
susp - suspension
sol - solution
amp - ampule
inj - injection
Rx - prescription
C - Celsius
F - Fahrenheit
BP - blood pressure
HR - heart rate
RR - respiratory rate
WBC - white blood cell
RBC - red blood cell
Hgb - hemoglobin
Hct - hematocrit
PT - prothrombin time
INR - international normalized ratio
BUN - blood urea nitrogen
Cr - creatinine
Ca - calcium
K - potassium
Na - sodium
Cl - chloride
Mg - magnesium
PO2 - partial pressure of oxygen
PCO2 - partial pressure of carbon dioxide
ABG - arterial blood gas
CBC - complete blood count
BMP - basic metabolic panel
CMP - comprehensive metabolic panel.
ECG - electrocardiogram
EEG - electroencephalogram
MRI - magnetic resonance imaging
CT - computed tomography
PET - positron emission tomography
CXR - chest x-ray
CTX - chemotherapy
NSAID - nonsteroidal anti-inflammatory drug
DMARD - disease-modifying antirheumatic drug
ACE - angiotensin-converting enzyme
ARB - angiotensin receptor blocker
SSRI - selective serotonin reuptake inhibitor
TCA - tricyclic antidepressant
ADHD - attention deficit hyperactivity disorder
COPD - chronic obstructive pulmonary disease
CAD - coronary artery disease
CHF - congestive heart failure
DVT - deep vein thrombosis
GI - gastrointestinal
UTI - urinary tract infection
OTC - over-the-counter
Rx - prescription
OD - right eye
OS - left eye
OU - both eyes.
TID - thrombosis in dementia
TDS - ter die sumendum (three times a day)
BOM - bilaterally otitis media (infection in both ears)
BT - body temperature
C&S - culture and sensitivity
D/C - discontinue or discharge
D/W - dextrose in water
ETOH - ethyl alcohol
FUO - fever of unknown origin
H&P - history and physical examination
I&D - incision and drainage
I&O - intake and output
KVO - keep vein open
N&V - nausea and vomiting
PERRLA - pupils equal, round, reactive to light and accommodation
PR - per rectum
QAM - every morning
QHS - every bedtime
QOD - every other day
S/P - status post (after)
TPN - total parenteral nutrition
UA - urinalysis
URI - upper respiratory infection
UTI - urinary tract infection
VO - verbal order.
XRT - radiation therapy
YOB - year of birth
BRBPR - bright red blood per rectum
CX - cervix
DVT - deep vein thrombosis
GB - gallbladder
GU - genitourinary
HCV - hepatitis C virus
HPI - history of present illness
ICP - intracranial pressure
IVP - intravenous pyelogram
LMP - last menstrual period
MRSA - methicillin-resistant Staphylococcus aureus
MVA - motor vehicle accident
NKA - no known allergies
PEG - percutaneous endoscopic gastrostomy
PRN - pro re nata (as needed)
ROS - review of systems
SOB - shortness of breath
TAH - total abdominal hysterectomy.
TIA - transient ischemic attack
Tx - treatment
UC - ulcerative colitis
URI - upper respiratory infection
VSD - ventricular septal defect
VTE - venous thromboembolism
XR - x-ray
w/c - wheelchair
XRT - radiation therapy
ASD - atrial septal defect
Bx - biopsy
CAD - coronary artery disease
CKD - chronic kidney disease
CPAP - continuous positive airway pressure
DKA - diabetic ketoacidosis
DNR - do not resuscitate
ED - emergency department
ESRD - end-stage renal disease
FFP - fresh frozen plasma
FSH - follicle-stimulating hormone.
GCS - Glasgow Coma Scale
Hct - hematocrit
Hgb - hemoglobin
ICU - intensive care unit
IV - intravenous
JVD - jugular venous distension
K - potassium
L - liter
MCH - mean corpuscular hemoglobin
MI - myocardial infarction
Na - sodium
NGT - nasogastric tube
NPO - nothing by mouth
OR - operating room
PCN - penicillin
PRBC - packed red blood cells
PTT - partial thromboplastin time
RBC - red blood cells
RT - respiratory therapy
SOA - short of air.
SCD - sequential compression device
SIRS - systemic inflammatory response syndrome
STAT - immediately
T - temperature
TPN - total parenteral nutrition
WBC - white blood cells
ABG - arterial blood gas
A fib - atrial fibrillation
BPH - benign prostatic hypertrophy
CBC - complete blood count
CO2 - carbon dioxide
COPD - chronic obstructive pulmonary disease
CPR - cardiopulmonary resuscitation
CT - computed tomography
CXR - chest x-ray
D5W - dextrose 5% in water
Dx - diagnosis
ECG or EKG - electrocardiogram
EEG - electroencephalogram
ETO - early termination of pregnancy.
FHR - fetal heart rate
GSW - gunshot wound
H&P - history and physical exam
HCG - human chorionic gonadotropin
I&D - incision and drainage
IBS - irritable bowel syndrome
ICP - intracranial pressure
IM - intramuscular
INR - international normalized ratio
IOP - intraocular pressure
LFT - liver function test
LOC - level of consciousness
LP - lumbar puncture
NG - nasogastric
OA - osteoarthritis
OCD - obsessive-compulsive disorder
OTC - over-the-counter
P - pulse
PCA - patient-controlled analgesia
PERRLA - pupils equal, round, reactive to light and accommodation.
PFT - pulmonary function test
PICC - peripherally inserted central catheter
PO - by mouth
PRN - as needed
PT - physical therapy
PT - prothrombin time
PTSD - post-traumatic stress disorder
PVC - premature ventricular contraction
QD - once a day
QID - four times a day
RA - rheumatoid arthritis
RICE - rest, ice, compression, elevation
RSI - rapid sequence intubation
RSV - respiratory syncytial virus
SBP - systolic blood pressure
SLE - systemic lupus erythematosus
SSRI - selective serotonin reuptake inhibitor
STAT - immediately
TB - tuberculosis
TIA - transient ischemic attack.
TID - three times a day
TKO - to keep open
TNTC - too numerous to count
TPN - total parenteral nutrition
URI - upper respiratory infection
UTI - urinary tract infection
V-fib - ventricular fibrillation
V-tach - ventricular tachycardia
VA - visual acuity
WNL - within normal limits
AED - automated external defibrillator
ARDS - acute respiratory distress syndrome
BID - twice a day
BP - blood pressure
BUN - blood urea nitrogen
CAD - coronary artery disease
CHF - congestive heart failure
CVA - cerebrovascular accident
D/C - discontinue
DKA - diabetic ketoacidosis.
DM - diabetes mellitus
DVT - deep vein thrombosis
EGD - esophagogastroduodenoscopy
ER - emergency room
F - Fahrenheit
Fx - fracture
GI - gastrointestinal
GTT - glucose tolerance test
HCT - hematocrit
Hgb - hemoglobin
HRT - hormone replacement therapy
ICP - intracranial pressure
IDDM - insulin-dependent diabetes mellitus
IBS - irritable bowel syndrome
IM - intramuscular
IV - intravenous
K - potassium
KVO - keep vein open
L&D - labor and delivery
LASIK - laser-assisted in situ keratomileusis.
ROM - range of motion
RT - radiation therapy
Rx - prescription
SCD - sequential compression device
SOB - shortness of breath
STD - sexually transmitted disease
TENS - transcutaneous electrical nerve stimulation
TIA - transient ischemic attack
TSH - thyroid-stimulating hormone
UA - urinalysis
US - ultrasound
UTI - urinary tract infection
VD - venereal disease
VF - ventricular fibrillation
VT - ventricular tachycardia
WBC - white blood cell
XRT - radiation therapy
XR - x-ray
Zn - zinc
Z-pak - azithromycin (antibiotic).
AAA - abdominal aortic aneurysm
ABG - arterial blood gas
ACS - acute coronary syndrome
ADL - activities of daily living
AED - automated external defibrillator
AIDS - acquired immunodeficiency syndrome
ALS - amyotrophic lateral sclerosis
AMA - against medical advice
AML - acute myeloid leukemia
APAP - acetaminophen
ARDS - acute respiratory distress syndrome
ASCVD - atherosclerotic cardiovascular disease
BPH - benign prostatic hyperplasia
BUN - blood urea nitrogen
CABG - coronary artery bypass graft
CBC - complete blood count
CHF - congestive heart failure
COPD - chronic obstructive pulmonary disease
CPAP - continuous positive airway pressure
CRF - chronic renal failure.
CT - computed tomography
CVA - cerebrovascular accident
D&C - dilation and curettage
DVT - deep vein thrombosis
ECG/EKG - electrocardiogram
EEG - electroencephalogram
ESRD - end-stage renal disease
FSH - follicle-stimulating hormone
GERD - gastroesophageal reflux disease
GFR - glomerular filtration rate
HbA1c - glycated hemoglobin
Hct - hematocrit
HIV - human immunodeficiency virus
HPV - human papillomavirus
HTN - hypertension
IBD - inflammatory bowel disease
IBS - irritable bowel syndrome
ICU - intensive care unit
IDDM - insulin-dependent diabetes mellitus
IM - intramuscular.
IV - intravenous
LFT - liver function test
MI - myocardial infarction
MRI - magnetic resonance imaging
MS - multiple sclerosis
NPO - nothing by mouth
NS - normal saline
OCD - obsessive-compulsive disorder
OSA - obstructive sleep apnea
PCOS - polycystic ovary syndrome
PMS - premenstrual syndrome
PPD - purified protein derivative
PSA - prostate-specific antigen
PT - prothrombin time
PTT - partial thromboplastin time
RA - rheumatoid arthritis
RBC - red blood cell
RSV - respiratory syncytial virus
SLE - systemic lupus erythematosus
TB - tuberculosis.
It is important to remember that medical abbreviations can vary based on location and specialty.
Healthcare professionals should use medical abbreviations with caution and only when they are familiar with their meanings.
Patients should always communicate any questions or concerns they have about their medications or medical care to their healthcare provider or pharmacist to ensure they receive safe and accurate medical care.

9 notes
·
View notes
Text
Intro
I recently found out that my beloved cat who's been in my life for 12 years has developed renal insufficiency. The vet wants me to put her on a Kidney Care Diet, and we're slowly making the change to that.
In the meantime, she is still well. By that I mean, she hasn't really shown any signs or symptoms yet. I dread the day that I start to see them.
The most painful part of this whole thing is anticipatory grief. I grew up without an emotionally available home and she has been my only source of unconditional love and emotional support. So far, she has been with me through 2 moves, 4 jobs, traveling out of the country and within, 12 holidays, and from the beginning of college to now. I always knew I would outlive her, but I assumed that she would simply grow older, without having to live with a terminal illness at the same time.
I'm trying to find others who are in the same boat as me, and while I see and hear advice to enjoy her company right now, and to take it one day at a time, and to 'live in the moment', those are easy to say but hard to bear. I love her more than anything. I almost lost her 2 times in the past, the second time being the most recent, just a week before I found out about her condition. I was devastated, imagining the worst, spending 4 days and nights crying, grieving, dealing with anxiety, having no appetite. I did everything, putting up posters, talking to neighbors, calling for her at dawn and dusk. Sleep become my only comfort, because then I don't have to deal with my worst enemy - my own intrusive thoughts.
But, I found her, 4 days later. I took her to the vet to make sure she was okay. And in the bliss ignorance of the week that followed, I felt like my entire world, which has stopped, started to revolve again.
And then two days ago, I got a phone call from the vet.
They found that her Creatinine was 2.5, and that her SDMA, a biomarker for renal function, was 16. Both values were slightly out of the reference range.
I again felt devastated, especially after hearing about all the changes, the things she may go through as this irreversible condition slowly progresses. I want to know so I can be prepared, but there's much overwhelming information, and it's paradoxical to me how she is seemingly doing well outwardly, while inside, her kidneys are no longer working as well as they were before.
Thus, I wanted to write all my feelings and thoughts down, as a way for me to cope. I know she doesn't fully understand why I've been sniffling and crying so much, and why my behavior has changed, but I'd like to imagine that she has noticed a change, and if she did understand everything, she wouldn't want me to feel sad because I know she loves me.
This is the start of my coping and grieving journey. Please feel free to follow if you are on the same road. But please, above all else, be kind.
2 notes
·
View notes
Note
Hey, I'm so sorry I don't mean to push but each morning I check to see if there's any update on This love is bad. Your writing is terrific, I fear the day you'll post part 5 of This love is bad because I know it'll be the end of this amazing serie but I can't wait to know how it is going to go! xx
HI MY LOVEE! First of, tysm for appreciating my work! 🥹🥹🥹 AND U CALLED MY WRITING TERRIFIC I AM SMILING FROM EAR TO EAR AT THE MOMENT!
Okie so I’m gonna use this ask as a sort of update about why I’m writing slow. also I’m gonna talk about body dysmorphia so if this triggers u, you can just skip 🤍
So life update, I’m slowly working on the remaining 2 or 3 chapters of the series but as I said, it’s slow bcos of the workload of graduate school aaaaaand my how do I call this hmm inflammation(???) in my knees. I went to the ortho doctor today and finally had them check since they’ve been hurting for weeks now during my workout. Then I had my blood chem tested etc etc.
So even when I stand or sit or drive or walk or even lie down, they hurt but not constantly. The doc said I am lucky to not have that part or the knee completely destroyed bcos we don’t have transplant for that now. And so I have to rest for 4-8 weeks. I’m taking meds now. Also the blood chem thingy, my sugar is a bit low and my creatinine is a bit low. SO I NEED TO EAT MORE PROTEIN PER THE DOCTOR SKSKSK
so moving on to the body dysmorphia talk, I grew up thin. Like borderline malnourished thin bcos I didn’t like eating. But then my parents brought me to the doctor etc etc and I was prescribed back then a vitamins for me to eat more. Then I was borderline obese. Then puberty came and I slimmed down a bit but was still a chubby girl. Then only when I graduated college did I start loving my body bcos I was constantly working out. To the point that I run everyday, and did jumping rope 1000 times a day. Soooo my knees kind of took the hit. I didn’t like the feeling I get when I go on a long time without working out. I feel like i was gaining weight when in reality, i wasn’t. So long story short, I have to learn to love me and not the image i see in the mirror. It’s kind of taking a toll on my health.
Here’s me, still standing despite the pain mwahahahaha

Im not on a hiatus! I’m just taking this time to rest and love myself more. But rest assured I’m still writing and even have new series coming! I love u all and let’s all love ourself as hard as we love other people.
6 notes
·
View notes
Text
I need to read about dosing and management of lithium. There is a lot of stuff you have to monitor for pts taking lithium and I don't feel comfortable prescribing it. But I don't have time to read this right now. Will look at this later and fix with page breaks: Laboratory tests and monitoring — Before prescribing lithium and during ongoing treatment, laboratory tests need to be obtained because lithium can adversely affect several organ systems. Management of abnormal test results and adverse effects resulting from lithium are described elsewhere in the topic, as is management of a positive pregnancy test. (See 'Renal' below and 'Thyroid' below and 'Parathyroid' below and 'Cardiac' below and 'Pregnancy' below.) Prior to beginning lithium, the following tests should be obtained [47-51]: ●Urinalysis, blood urea nitrogen, creatinine, thyroid function studies, and calcium. ●Pregnancy test for women of childbearing potential. ●Electrocardiogram for patients with risk factors for coronary heart disease, including diabetes mellitus, hypertension, dyslipidemia, and cigarette smoking. (See "Overview of established risk factors for cardiovascular disease".) Lithium levels should be checked five to seven days after the dose is changed. In addition, a lithium level should be checked if a dose increase is under consideration and a level has not been measured for at least two weeks. Patients on steady doses should have their levels checked every 6 to 12 months. In addition to checking lithium levels during ongoing treatment, renal, thyroid, and parathyroid function should be monitored as follows [10,44,47-51]: ●Urinalysis, blood urea nitrogen, and creatinine every two to three months during the first six months of therapy, and every 6 to 12 months thereafter. (See "Renal toxicity of lithium".) ●Thyroid function tests once or twice during the first six months, and every 6 to 12 months thereafter or more frequently in higher risk patients. (See "Lithium and the thyroid".) ●Serum calcium is monitored yearly. MANAGING LITHIUM ADVERSE EFFECTS Lithium can cause many acute and long-term adverse effects that are not necessarily associated with toxicity [52]. Some adverse effects, such as weight gain and cognitive impairment, are more likely to be associated with nonadherence than other adverse effects, such as nausea, polyuria/polydipsia, and tremor [44]. Severe or a sudden worsening of side effects may be a sign of lithium toxicity. (See 'Lithium toxicity' above and "Lithium poisoning".) General strategies — General strategies for managing adverse effects of lithium include [44]: ●Watchful waiting – Tolerance to some side effects (eg, nausea and tremor) can eventually occur, but is unlikely with other adverse effects (eg, weight gain). ●Changing the time of administration. ●Lowering the dose; however, dose reductions risk compromising efficacy. ●Changing to a different lithium formulation (immediate or slow release). ●Dividing the daily dose to take smaller amounts more often, to decrease peak serum levels. ●Treating adverse effects with a second drug (eg, diuretic for polyuria/polydipsia). ●Discontinuing lithium and switching to a different drug if adverse effects are intolerable and cannot be managed. Strategies for managing specific adverse effects are discussed in the sections below. Renal — Renal function is adversely affected by lithium and thus monitored with laboratory tests [50]. (See 'Laboratory tests and monitoring' above.) Adverse renal effects are often functional and reversible, but may eventually progress to structural, permanent changes [44,53,54]. As an example, a study examined the impact of long-term lithium treatment (mean duration 18 years) on glomerular filtration rate in 312 bipolar disorder patients (mean age = 56 years) [55]. Extended lithium exposure reduced the estimated glomerular filtration rate by approximately 30 percent more than that associated with aging alone. Additional risk factors for decreased estimated glomerular filtration rate were higher serum lithium concentrations, longer exposure, lower initial estimated glomerular filtration rate, general medical comorbidity, and older age. None of the patients developed end-stage kidney disease. Abnormal renal function tests are managed in collaboration with a nephrologist to determine the need for further testing, a reduction in the dose of lithium, or switching to an alternative medication for treating bipolar disorder. Additional information about lithium and renal toxicity is discussed separately. (See "Renal toxicity of lithium".) Polyuria and polydipsia — Polyuria is often defined as urinating more than three liters in 24 hours [44]. Polyuria and polydipsia have been observed in up to 70 percent of lithium treated patients; potential risk factors include longer duration of treatment, higher serum lithium concentrations, episodes of lithium toxicity, and use of other psychotropic medications. Polyuria and polydipsia may be a symptom of nephrogenic diabetes insipidus. (See "Renal toxicity of lithium", section on 'Nephrogenic diabetes insipidus'.) Clinicians should attempt to prevent polyuria at the onset of lithium treatment by [44]: ●Administering lithium once per day ●Maintaining lithium serum concentrations as low as possible ●Avoiding episodes of lithium toxicity For patients who develop polyuria, diuretics (eg, the potassium-sparing diuretic amiloride) may decrease polyuria, but caution must be used because many diuretics alter serum lithium concentrations; lithium doses may need to be adjusted and lithium levels checked more often [44]. Use of diuretics that decrease potassium levels necessitates measuring potassium levels and possibly administering potassium supplements. Specific interactions of lithium with other medications may be determined using the Lexicomp drug interactions tool included in UpToDate. Thyroid — Thyroid function is adversely affected by lithium and thus monitored with laboratory tests (see 'Laboratory tests and monitoring' above); lithium can cause goiter, hypothyroidism, chronic autoimmune thyroiditis, and possibly hyperthyroidism. The adverse effects of lithium on thyroid function and their management are reviewed separately. (See "Lithium and the thyroid".) Neither pretreatment hypothyroidism (presumably treated adequately with T4) nor lithium-induced hypothyroidism is a contraindication to lithium therapy [44,56]. Reasonable recommendations are to monitor serum thyrotropin and if it rises much above the upper value of normal, to start T4 while continuing the lithium. Consultation with an endocrinologist may also be indicated. (See "Clinical manifestations of hypothyroidism" and "Treatment of primary hypothyroidism in adults".) Parathyroid — Lithium may cause hypercalcemia, elevated serum parathyroid hormone, and hyperparathyroidism [44,50]. Patients with lithium-induced hypercalcemia and hyperparathyroidism are generally asymptomatic [57]. An elevated calcium level should prompt a serum parathyroid hormone concentration. If the hormone level is abnormal, an endocrine consult is obtained. Hypercalcemia, hyperparathyroidism secondary to lithium, and measurement of serum calcium are discussed separately. (See "Pathogenesis and etiology of primary hyperparathyroidism", section on 'Lithium therapy' and "Primary hyperparathyroidism: Diagnosis, differential diagnosis, and evaluation", section on 'Serum calcium' and "Primary hyperparathyroidism: Management".) Tremor — Lithium tremor is common; pooled results from multiple studies suggest that the prevalence is approximately 25 percent [58]. The pathogenesis may involve lithium-induced accumulation of iron in the substantia nigra [59]. Tremor secondary to lithium is classified as an action tremor, and subcategorized as an exaggerated physiologic tremor. Lithium tremors are also subclassified as a postural tremor that occurs when a specific posture, such as holding the arms outstretched or while standing, is voluntarily maintained. (See "Overview of tremor".) Onset of lithium tremor typically occurs when the drug is started or titrated up, but tremor can appear at any time during treatment [44,58]. Lithium tremor is generally symmetric, limited to the hands or upper limbs, and nonprogressive. The frequency of the involuntary rhythmic oscillation of the hands is approximately 10 Hertz. Factors that increase the risk of tremor include higher lithium doses and serum concentrations, anxiety, caffeine, medications (eg, antiarrhythmics, beta-adrenergic agents, carbamazepine, and valproate), emotional and physical stress, fatigue, and older age. The differential diagnosis of lithium tremor includes metabolic abnormalities, benign essential tremor, Parkinson disease, and lithium toxicity [58]. Tremor caused by lithium toxicity is more coarse and severe than is otherwise observed in patients treated with lithium; in addition, lithium toxicity may affect body parts other than the upper extremity, and is likely to occur with other symptoms of toxicity. (See 'Lithium toxicity' above and "Lithium poisoning", section on 'Signs and symptoms'.) Clinicians evaluating lithium tremor should obtain a history, physical examination, and laboratory tests (including a serum lithium concentration), to rule out other causes of tremor [58]. Additional information about the evaluation of lithium tremor is discussed separately. (See "Overview of tremor", section on 'Evaluation'.) Watchful waiting is a reasonable approach to lithium tremor because it often is relatively mild and resolves over time [44,58]. Management of lithium tremor that is troublesome and/or persistent starts with modifying aggravating factors (eg, decreasing caffeine intake). In addition, it may help to change the lithium preparation from long acting to short acting, or to a different salt (ie, from carbonate to citrate), or to divide the daily dose to take smaller amounts more often. For lithium tremor that still persists and causes moderate to severe functional problems, we suggest add-on pharmacotherapy (eg, beta blockers such as propranolol) [44,58]. Alternatively, the total daily dose of lithium can be reduced if feasible. Choosing and administering add-on pharmacotherapy for lithium tremor is discussed separately in the context of essential tremor. (See "Essential tremor: Treatment and prognosis".) Nausea — Nausea secondary to lithium is observed in 10 to 20 percent of patients [44]. Management strategies include the following, listed from most to least preferable: ●Taking lithium with food or after meals. ●Using a sustained release formulation of lithium (to decrease peak serum concentrations because nausea may be related to higher peak levels). ●Dividing the daily dose to take smaller amounts more often (to decrease peak serum concentrations). ●Treatment with a second drug. (See "Approach to the adult with nausea and vomiting", section on 'Antiemetics and prokinetics'.) ●Reducing the total daily dose. Nausea often abates over time, which allows patients to resume a higher dose and once daily dosing [44]. Vomiting secondary to lithium is uncommon and can indicate lithium toxicity, especially in the context of other adverse effects, such as coarse tremor and ataxia [44]. (See 'Lithium toxicity' above.) Loose stools/diarrhea — Lithium-induced loose stools/diarrhea is seen in up to 10 percent of patients [44]. Higher serum lithium concentrations (eg, greater than 0.8 mEq/L [0.8 mmol/L]) may correlate with loose stools/diarrhea; thus, management strategies include: ●Using an immediate-release formulation of lithium (to avoid distal absorption of the drug). ●Treatment with a second drug. (See "Approach to the adult with chronic diarrhea in resource-abundant settings", section on 'Symptomatic therapy'.) ●Reducing the daily dose. Weight gain — Lithium can cause weight gain through several mechanisms, such as carbohydrate craving, increased thirst, and fluid consumption, water retention related to salt retention, and reduced metabolism secondary to hypothyroidism. A meta-analysis of five randomized trials compared lithium with placebo in patients with bipolar disorder; four trials lasted to 12 or 18 months (n = 899 patients) and one trial lasted 3 months (n = 325) [50]. Clinically significant weight gain, defined as an increase >7 percent from baseline, occurred in nearly twice as many patients treated with lithium than placebo (relative risk 1.9, 95% CI 1.3-2.8). In addition, weight gain is relatively distressing, compared with other adverse effects [44]. Preventing and managing weight gain during lithium treatment is based upon nonspecific measures [44]: ●Discussing the likelihood of weight gain at the outset of treatment. ●Encouraging patients to drink low caloric drinks when thirsty. ●Dietary strategies, exercise, and drug therapy. (See "Obesity in adults: Overview of management", section on 'Drug therapy'.) ●Treating polyuria/polydipsia-induced weight gain with a diuretic, and treating hypothyroidism-induced weight gain with thyroid supplementation. (See "Renal toxicity of lithium", section on 'Treatment' and "Treatment of primary hypothyroidism in adults".) Cognitive impairment — Lithium-induced cognitive impairment appears to be one of the most distressing adverse effects of the drug and often leads to nonadherence [10,44]. Cognitive dysfunction secondary to lithium needs to be distinguished from the cognitive impairment that is associated with bipolar disorder per se, including patients who are euthymic or depressed [44,60]. Concomitant medications (eg, antipsychotics, antidepressants, and benzodiazepines) may also contribute to cognitive dulling that occurs in patients receiving lithium. In addition, it appears that the neurocognitive effects are worse at higher doses and are cumulative over time. Cognitive impairment that is due to bipolar disorder itself is discussed separately. (See "Bipolar disorder in adults: Clinical features", section on 'Neurocognitive function'.) Multiple cognitive domains are adversely affected by lithium. As an example, a meta-analysis of six studies included patients with remitted mood disorders (n = 326, primarily bipolar disorder) and found that use of lithium was associated with small to moderate impairment of immediate verbal learning and memory, creativity, and psychomotor performance [61]. However, lithium may preserve other domains of neurocognition [60]. Management strategies include dividing the daily dose to take smaller amounts more often; in addition, lowering the dose of lithium may help, because cognitive dulling may be dose related [44]. Among patients receiving polypharmacy, especially complex psychotropic regimens that include three or more drugs, discontinuing one or more drugs may improve cognitive dysfunction without exacerbating mood symptoms. Adding stimulants such as modafinil and armodafinil may possibly help, but there is no high quality evidence to support this approach. Sexual dysfunction — Lithium-induced sexual dysfunction appears to be common. One study assessed clinically stable patients with bipolar disorder who were treated with lithium for an average of 10 years (n = 100 patients; mean age 44 years); 85 percent were receiving lithium monotherapy and the mean dose in the entire sample was 800 mg/day [62]. Sexual dysfunction across multiple domains (eg, arousal, sexual drive, and penile erection/vaginal lubrication) was present in 37 percent and was associated with poor adherence. Risk factors for sexual dysfunction included older age and the presence of other adverse effects. Management strategies, beyond the general strategies for managing adverse effects (see 'General strategies' above), are discussed in the context of treating the general population of patients with sexual dysfunction. (See "Treatment of male sexual dysfunction" and "Overview of sexual dysfunction in women: Management".) Cardiac — Lithium may rarely cause cardiac dysrhythmias in patients without pre-existing cardiac disease [36,52,63]. In addition, lithium may lead to the following abnormalities on the electrocardiogram, which may anticipate the onset of dysrhythmias [52]: ●Repolarization abnormalities of the T wave or ST segment. ●Findings consistent with sinus node dysfunction. (See "Sinus node dysfunction: Epidemiology, etiology, and natural history", section on 'Other'.) ●An unmasked or modulated Brugada pattern. (See "Brugada syndrome: Clinical presentation, diagnosis, and evaluation", section on 'Provoking factors'.) These electrocardiogram findings should prompt a cardiology consult. PREGNANCY Although lithium is generally regarded as teratogenic due to increased risks of cardiac defects (eg, Ebstein anomaly) [64-66], many authorities consider the absolute risk small [67-71]. The use of lithium during pregnancy and risks of lithium exposure during pregnancy and breastfeeding are discussed separately. (See "Bipolar disorder in women: Preconception and prenatal maintenance pharmacotherapy", section on 'Refractory patients' and "Teratogenicity, pregnancy complications, and postnatal risks of antipsychotics, benzodiazepines, lithium, and electroconvulsive therapy", section on 'Lithium' and "Breastfeeding infants: Safety of exposure to antipsychotics, lithium, stimulants, and medications for substance use disorders", section on 'Lithium'.)
2 notes
·
View notes
Text
Treatment For Kidney Failure: Guide for Alternative Medication to Avoid Dialysis For Kidney Failure

Chronic kidney disease
Our kidneys are constantly working to ensure that we are healthy. Despite their tiny dimensions, they perform a crucial role in the removal of waste, controlling the balance of fluids and maintaining our wellbeing. Conditions like acute kidney injuries (AKI), as well as chronic kidney diseases (CKD), could cause health risks for us. Along with abdominal pain, the sufferer might be faced with a variety of issues. Kidney diseases should be recognised and evaluated immediately. When it is the first stage of the illness, Treatment for kidney failure needs to be initiated to ensure that it is avoided from getting worse.
DIET for kidney health?
If you suffer from kidney disease, you need to get an effective chronic kidney disease treatment immediately. This means that you require a suitable cure for chronic kidney disease; however, it is crucial to pay attention to the diet you eat because eating habits for patients with kidney disease have significant effects on the patient. Moreover, diet plays a significant role in ensuring that medications are efficient. Therefore, you must alter the way you eat. The next step is to change your diet to be different from that of an ordinary person, but rather from the standpoint of taking care of the illness and gaining freedom from this deadly disease.
We'll tell our readers that there are plenty of things that kidney patients can do which, in addition to diets for healthy kidneys, are extremely beneficial to those suffering from kidney issues. There are many foods like poha, upma, porridge, sago, and plain oats.
Include foods with low sodium, such as carrots, ginger and gourds that are bottled. Low potassium foods: parwal, tinda, capsicum, brinjal, cauliflower, cabbage. Protein-rich foods such as watermelon seeds and melon seeds, along with makhana and tur moong dal, should be part of your diet. However, you must stay clear of cucumber meat, potatoes, rice, avocados, tomatoes, and whole wheat bread.
Fruits and food items for healthy kidneys
Kidneys assist in eliminating the body of toxins and keep the levels of a variety of minerals, like potassium, sodium and acids. Numerous fruits are great to eat, and some are extremely beneficial to patients. If you want to cure for chronic kidney disease, Keeping all these things in mind, we will tell you some of the best fruits for patients with this condition.
Strawberries, blueberries and cranberries are packed with antioxidants and vitamins. They can help improve overall health of the kidneys.
Apples are rich in fibre and are anti-inflammatory substances. They aid in maintaining renal health.
Fish: High in Omega-3-rich fatty acids, fish such as mackerel or salmon help reduce inflammation and improve the health of your cardiovascular system.
Melons and watermelons have large amounts of water. This helps in the formation of urine.
Do not eat pomegranate seeds, and consume only the red portion because it increases the high risk for developing stone.
Guava also has high levels of phosphorus and potassium. It is also recommended not to consume seeds from guava.
Peaches can be included in your daily diet. However, diabetics must be careful about it.
We've discussed a variety of foods and fruits that are beneficial to people suffering from kidney disease. We can look into the role that dried fruit plays in the lives of patients.
The best solution for healthy kidneys
Are you suffering from kidney issues and looking for a more effective kidney failure treatment without dialysis? We have the solution for you. Bharat homeopathic treatment for kidney problems is the best choice for you. Homeopathy treatment offers many advantages, one of which is that it is a completely non-toxic high creatinine treatment that is made entirely using herbal extracts. Additionally, during the course of treatment, the Bharat Homeopathy physicians will know your complete medical history before the treatment begins, keeping in mind the root cause of your condition. If you're looking to have a strong kidney and a healthy body, it is imperative to follow a better treatment regimen.
0 notes