#splenic rupture
Text
Spontaneous Rupture of Wandering Spleen: Case Report by Mina Alvandipour in Journal of Clinical and Medical Images, Case Reports

Abstract
Keywords: Spleen; wandering spleen; ectopic spleen; splenic rupture.
Introduction
A wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2% [1]. wandering spleen is caused by either extreme laxity or absence of the normal ligaments that anchor the spleen to the left upper quadrant. Gravity also plays a role by allowing the spleen to descend into the lower abdomen attached by its vascular pedicle [2]. Symptoms depend on the degree of torsion and range from chronic abdominal pain in mild torsion to acute pain in severe torsion and infarction. Accurate clinical diagnosis is difficult because of the rarity of the condition and non-specific symptoms. Radiological evaluation includes usage of ultrasound, Doppler, abdominal CT or MRI depending upon availability or preference [3]. A wandering spleen can be either congenital or acquired. In the congenital condition the ligaments fail to develop properly, whereas in the acquired form the hormonal effects of pregnancy and abdominal wall laxity are proposed as determining factors .However, the precise etiology of the wandering spleen is not known [1]. We present a spontaneous rupture of a wandering spleen with severe torsion and infarction and abdominal pain without any history of trauma.
Case Report
A 25 years old female present to emergency unit with 2 week history of progressive abdominal pain, recurrent constipation ,vomiting and loss of appetite. There was no history of melena, fever, and hematochezia and weight loss. On examination there was periumbilical and epigastria tenderness and a firm and tender mass in the right side of the abdomen without muscle guarding and rebound tenderness. The vital sign and laboratory results were all within the normal ranges, except decreased hematocrit (hemoglobin-8.4). The plain abdominal radiograph was un-remarkable while abdominal ultrasonography with color Doppler showed absence of spleen in its normal location in the left upper abdomen. Also it detects a heterogeneous hypoechoic capsulated mass with diameter of 175mm in right lower abdomen. Other organs of the abdomen were normal. Abdominal pelvic CT scan with and without contrast was recommended and findings was Absence of the spleen in its normal position in the left hypochondrium, and presence of large diameter mass (splenomegaly)in the right sub hepatic area(Wandering spleen) . Other organs of the abdomen were normal. Contrast-enhanced computed tomography (CECT) of the abdomen revealed whirlpool sign near the umbilicus. The splenic parenchyma showed abnormal enhanced areas, suggestive of splenic torsion and infarction.
A final diagnosis was wandering spleen with torsion of the vascular pedicle and infarction. The patient underwent a total splenectomy. During the laparotomy, an enlarged and infarcted mass was seen in right side of abdomen. The characteristic “whirlsign” can be seen in the area of the splenic vascular pedicle, indicative of torsion. Histological examination confirmed total infraction of the wandering spleen. The postoperative course was uneventful, and the patient was discharged on the 4th day after the operation.
Discussion
A wandering spleen is a rare but well-known entity. The incidence is < 0.2%. It is more common in females than males between the second to fourth decade of life and children [4]. Splenic weight >500 g in more than 8 out of 10 cases [5]. Interestingly, it has been reported that one out of three cases of wandering spleen appears in children bellow the age of 10 years old [7].
Wandering is characterized by splenic hyper mobility that results from elongation or mal-development of its suspensory ligaments. It is also known as aberrant, floating, displaced, prolapsed, ptotic, dislocated or dystopic spleen. Ectopic spleen, splenosis and accessory spleens are separate clinical entities and must be distinguished from it [5]. If the pedicle is twisted in the course of movement of the spleen, blood supply may be interrupted or blocked, resulting in severe damage to the blood vessels .Acute splenic torsion compromises venous outflow, which causes congestion and impairment of arterial inflow. Pain is originated from the splenic capsular stretching with rapid splenic enlargement and localized peritonitis [6]. Etiology is congenital or acquired. In case of congenital anomaly, a failure occur in fusion of the dorsal mesogastrium with the posterior abdominal wall during the second month of embryogenesis. Acquired risk factors that predispose to wandering spleen include pregnancy, trauma and splenomegaly [7]. Splenic torsion is usually clockwise. Complications of splenic torsion include: gangrene, abscess formation, local peritonitis, intestinal obstruction and necrosis of the pancreatic tail, which can lead to recurrent acute pancreatitis [8].
Wondering spleen had nonspecific symptoms such as abdominal pain that make diagnosis extremely challenging. As a result, radiologists play a major role in the diagnosis of this condition and its complications. Torsion may occur acutely and present with infarction or peritonitis. Chronic intermittent torsion can lead to pain, splenomegaly, and functional splenectomy. Contrast-enhanced computed tomography (CT) is the best imaging tool to make this diagnosis, although ultrasound may be used as well. Imaging findings on CT include identification of a spleen in an abnormal location, or with an abnormal orientation in the left upper quadrant. Often the wandering spleen is identified as a “comma” shaped mass in abdomen, with no normal left upper quadrant spleen [9].
Laboratory investigations are non-specific. Thrombocytopenia, through a mechanism of spleen enlargement secondary to compression of the splenic pedicle is rarely found [7]. The clinical presentation of wandering spleen is variable; it is either asymptomatic or noted incidentally during physical and radiographic examination or presents as acute abdomen due to torsion with subsequent infarction. The most common presentation is a mass with non-specific abdominal symptoms or intermittent abdominal discomfort due to congestion resulting from torsion and spontaneous detorsion [10]. Today, the only recommended treatment for wandering spleen is operation [7]. Splenectomy is indicated for infracted spleen and sometimes for huge splenomegaly precluding splenopexy. Splenopexy is the choice of treatment if the spleen is not infarcted [6]. Splenic preservation is highly recommended for young patients—those under one year of age up to those in their thirties—who are at particular risk for overwhelming post-splenectomy sepsis [10]. This should be appropriately followed up by the prophylactic vaccines against post-splenectomy sepsis syndrome. Ideally they should be administered before surgery; however, in emergencies this is not always possible [1].
Conclusion
In this case, splenectomy was done due to spleen infarction. Laparotomy was done in this case because of low experience at laparoscopy splenectomy. This report highlights the investigations and management necessary for a patient who presents with an ischaemic torted wandering spleen.
Acknowledgement: None.
Conflict of Interest: None.
Funds: None.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Spleen#wandering spleen#ectopic spleen#splenic rupture#Radiological#ultrasonography#Contrast-enhanced computed tomography#laparotomy#laparoscopy#Mina Alvandipour#JCMICR
0 notes
Text
Linda Fondren, 21 (USA 1974)
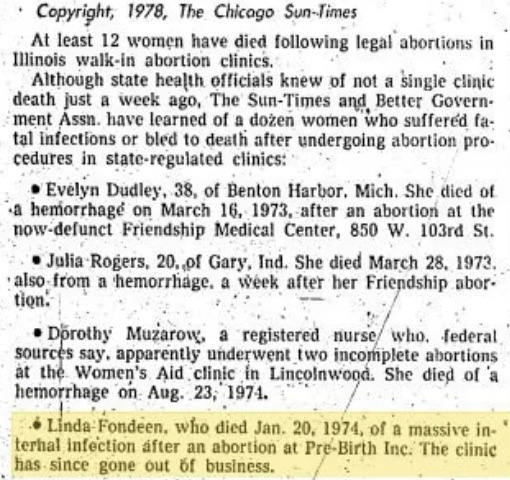
Linda Fondren was a single mother from Illinois who worked as a telephone operator. She was already caring for a small child when she discovered she was pregnant again. Linda was told that Roe v. Wade made abortion “safe and legal,” and it was thanks to this lie that she and her baby would lose their lives.
On the first New Year’s Day after Roe v. Wade, Linda underwent a legal abortion performed by Mohammad Pourtabib at Pre-Birth in Chicago. She bled afterwards, but the facility did not give her any follow-up care. An ambulance finally took her to the hospital, but she was already in shock. Doctors had to give her an emergency hysterectomy.
Linda had a terrible internal infection in addition to the bleeding. Doctors attempted to save her, but fluids were building up in her chest from the infection. During an attempt to drain the fluid on January 16, her spleen finally ruptured. She died on January 20 of massive infection with a coroner’s diagnosis of "hemoperitoneum with splenic rupture following hysterectomy and earlier dilatation and curettage [abortion]."
Linda’s survivors sued for her death. She was buried on January 25 in Burr Oak Cemetery. Fortunately for the women of Illinois, the negligent facility that killed her closed down.
According to a local newspaper’s exposé (which slightly misspelled her last name), Linda was one of at least 12 women killed by legalized abortion at walk-in abortion facilities in the state of Illinois alone in the time period analyzed. State officials had no knowledge of any of the deaths just a week before the newspaper published their report in 1978. This means that it’s possible that none of them were counted by the CDC’s statistics as maternal deaths from legal abortion.
Chicago Sun-Times “The Abortion Profiteers” Exposé 1978
Cook County Circuit Court Case No. 74L 12514
Death Certificate No. 601804
Chicago Tribune 8-17-74, 8-21-74
Chicago Today 8-5-74, 8-16-74
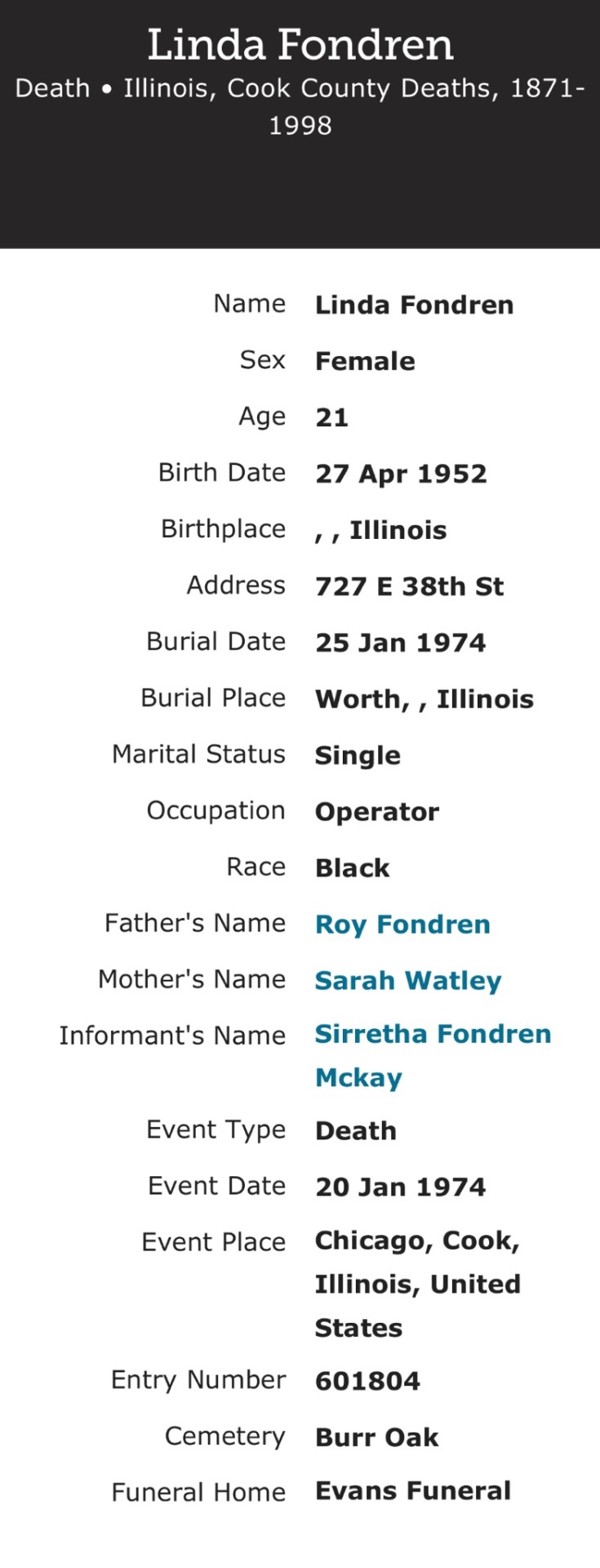
"Illinois, Cook County Deaths, 1871-1998," database, FamilySearch (https://familysearch.org/ark:/61903/1:1:Q2MN-438W : 18 March 2018), Linda Fondren, 20 Jan 1974; citing Chicago, Cook, Illinois, United States, source reference , record number , Cook County Courthouse, Chicago; FHL microfilm .
"United States Social Security Death Index," database, FamilySearch (https://familysearch.org/ark:/61903/1:1:J2B5-4PK : 9 January 2021), Linda Fondren, Jan 1974; citing U.S. Social Security Administration, Death Master File, database (Alexandria, Virginia: National Technical Information Service, ongoing).
"United States, Social Security Numerical Identification Files (NUMIDENT), 1936-2007", database, FamilySearch (https://www.familysearch.org/ark:/61903/1:1:6KQQ-G1JM : 10 February 2023), Linda Fondren, .
#black lives matter#tw abortion#pro life#victims of roe#unsafe yet legal#tw murder#tw ab*rtion#abortion#abortion debate#death from legal abortion#tw blo0d#tw negligence#tw neglect
6 notes
·
View notes
Text
so, for anyone who's been following me since I started here, or even before, and have been wondering about me...
2013 • traumatizing breakup, bounce back after discovering Markiplier's content
2014 • diagnosed with ADHD, actively freelancing
2015 • pretty good year overall...
2016 • dad diagnosed with Leukemia (AML) in May & almost died from splenic rupture - are air lifted to another hospital & I stay with him until July, living in the cancer ICU waiting room
2017 • stopped freelancing, mental health gets bad - dad had stroke, seizures, partially blind, muscle atrophy, cancer is only briefly in remission
2018 • I get a part time job at grocery store, have daily panic attacks & develop POTS, become mostly bedridden - dad's cancer is deemed terminal
2019 • dad died on Dec 12, at 10:40~10:45pm, I was home alone when it happened. the memory is burned into my brain permanently. I have PTSD.
2020 • have panic attacks & break downs at work, pandemic is brewing in Jan, quit my job in Feb, had another very traumatic breakup, then realize I can't draw anymore... but am able to get out of bed more & spend the summer hiking A LOT...but get COVID-19 in Nov, was sick for 28 days (mom was sick for 2 mos)
2021 • start exposure therapy for my drawing problems, (negative conditioning by trauma while in hospital with dad,) not much hiking anymore, lose a friend, finally find a medication that relieves my chronic anxiety, but long-covid sets in
2022 • I've become pretty much a total sedentary shut-in with declining health. had to go on Medicaid. spent the entire year trying to get a new therapist. long-covid is making POTS worse. nightmares about my dad being sick. multiple mental health crises to the point of feeling suicidal. yet...gradually able to draw again, though literally every aspect of my recovery has been improving at a snails pace. still spending most of my time in bed... trying to figure out how to move on with my life...
that's not everything, but I don't feel like going into too much detail because like I said, I've literally got nightmares. so hey. twitters dying. I'm back. 🫥
14 notes
·
View notes
Note
hey babe, i hope you’re okay. the past 16 hours have been really wild. my dog of 8 years had to be put down yesterday bc she had a tumor in her spleen that ruptured- she was also an older dog so it would be harder on her if we put her through surgery and chemo. we all knew that she would pass soon bc she was getting old but we didn’t expect it to be so soon. what break my heart the most is that her tumor didn’t rupture until my mom and i got home-we were out of town and got back home a few hours before ended up taking her to the vet. it makes me think that she “waited” for until before eventually passing. i miss her so much and i hope she’s okay but i know she’s in a better place.
hope you’re doing okay, hug your pets extra tight for me.
-🦉
I am so sorry to hear about your baby :( splenic tumors are shitty little surprises that are realllllly good at hiding until the last second. I've been there personally and professionally and it SUCKS all the way around, especially when you're forced to make BIG decisions very quickly.
There isn't a single doubt that she loves you round the moon and back a thousand times over. That's the beauty of the human-animal bond. The single hardest part of being a pet owner is having to make decisions on their behalf but choosing to give her a dignified passing in light of her poor prognosis is fair and kind. It's a decision made out of love and compassion.
Even with those thoughts in mind - Grief is to be expected and an important part of healing. My heart is broken for you, friend. I am sending you alllllllll the biggest, warmest hugs right now <3 please let me know if you ever feel like you or anyone in your family might need any pet loss resources and I can forward those over to you! Love you LOTS little owlet <3
#tw: pet loss#tw: medical#🦉 anon#i'm squeezing you sooooo tight#one day you'll have to send pics of your sweet baby
3 notes
·
View notes
Text
The Best Hospitals and Surgeons for Spleen Surgery in Delhi
Spleen surgery, or splenectomy, is a critical procedure often performed to treat conditions such as splenic rupture, splenic tumours, or haematological disorders. In Delhi, patients have access to some of the best hospitals and surgeons with advanced facilities and specialised expertise for spleen surgery.
Click here and read more about that :Why Patients Choose the Best Bariatric Surgeon in Delhi NCR for Weight Loss Surgery

Top Hospitals for Spleen Surgery in Delhi:
Max Super Specialty HospitalKnown for its multidisciplinary approach, Max Hospital offers advanced laparoscopic and minimally invasive splenectomy procedures. The hospital is equipped with state-of-the-art technology and a well-trained team of specialists.
Medanta – The MedicityA highly reputed institution in Delhi NCR, Medanta is known for its excellent surgical team, especially in the areas of organ surgeries. They use cutting-edge technology and advanced minimally invasive techniques to ensure faster recovery and better patient outcomes.
Fortis Escorts Heart InstituteWhile renowned for its cardiovascular care, Fortis Escorts also provides excellent general and specialized surgery services, including spleen surgery. Their expertise in laparoscopic surgery ensures a high success rate with minimal post-operative complications.
Sir Ganga Ram HospitalSir Ganga Ram Hospital has a strong general surgery department with renowned surgeons experienced in splenectomies. Their facilities are well-suited for patients with both routine and complex spleen issues.
Notable Surgeons:
Dr. Tarun Mittal – Known for his experience in minimally invasive surgeries, Dr.Mittal has successfully performed surgeries in Sir Ganga ram Hospital.
Dr. Pradeep Chowbey – A pioneer in laparoscopic surgeries, Dr. Chowbey has performed several complex spleen surgeries and is one of the top choices for patients at Max Hospital.
Dr. Anil Sharma – Based at Sir Ganga Ram Hospital, Dr. Sharma specializes in gastrointestinal and spleen surgeries, with excellent patient feedback for his skill and compassionate care.
0 notes
Note
What kind of creature is that?? (genuinely have no idea)
i think you're talking about the splenectomy? if you aren't my apologies—but it's the extremely diseased spleen of a dog (i think about lab-sized). splenic tumors can be undetected for literal years, but they will eventually rupture and kill them quickly due to the extreme blood loss that occurs. we can perform life-saving surgery, but it usually entails blood transfusions (luckily, we can auto-transfuse in a lot of hemoabdomen [blood in the abdominal cavity] cases) and fast intervention. we like to take them out early to avoid all that stress, and because they're more likely to metastasize the longer they're in the body.
that was the spleen of a dog who was lucky, because we caught it before it ruptured, but unlucky because his incision had to be huge to accommodate that size. it ended up being almost 6 kilograms.
0 notes
Text
Splenic Rupture_Sound therapy session_Sounds of nature

Splenic rupture, a serious medical condition often caused by trauma to the abdomen, requires prompt medical attention and intervention. Conventional treatments for splenic rupture typically involve surgery, blood transfusions, and close monitoring to ensure a successful recovery. However, in recent years, the integration of alternative therapies, such as resonant frequency sound therapy (RFST), as an adjunct to conventional medicine has garnered attention for its potential benefits in promoting healing and overall well-being for patients with splenic rupture.
Resonant frequency sound therapy is a non-invasive treatment modality that utilizes sound waves at specific frequencies to stimulate the body's natural healing processes. The therapy is based on the principle of resonance, which posits that when two objects vibrate at the same frequency, they can exchange energy efficiently. In the context of sound therapy, this principle is applied to the human body, with the goal of promoting healing and wellness.
There are several potential benefits of using RFST as an adjunctive treatment for splenic rupture in combination with conventional medicine:
1. Pain Management: Patients recovering from splenic rupture often experience significant pain. RFST has been shown to help manage pain and discomfort, potentially reducing the need for high doses of pain medication and promoting a more comfortable recovery process.
2. Stress Reduction: The recovery period following splenic rupture can be emotionally and psychologically challenging for patients. RFST has been found to promote relaxation and reduce stress, potentially enhancing the overall well-being of patients during the recovery process.
3. Enhanced Healing Response: RFST may aid in promoting the body's natural healing processes. By stimulating the body at a cellular level, it has the potential to support the healing of damaged tissues and contribute to a more efficient recovery.
4. Improved Sleep Quality: Many patients recovering from splenic rupture experience sleep disturbances. RFST has been shown to improve sleep quality, which is crucial for the body's healing and recovery processes.
5. Overall Well-Being: Integrating RFST with conventional treatments may contribute to the overall well-being of patients, offering a holistic approach to healing that addresses not only the physical aspects of recovery but also the emotional and psychological aspects.
It is important to note that while RFST shows promise as an adjunctive treatment for splenic rupture, it is not a replacement for conventional medical interventions.
The integration of alternative therapies like RFST with conventional medicine underscores the evolving landscape of healthcare, emphasizing a holistic approach to patient care.
In conclusion, resonant frequency sound therapy, when used as an adjunctive treatment in combination with conventional medicine, holds potential benefits for patients recovering from splenic rupture. Its ability to manage pain, reduce stress, enhance healing, improve sleep quality, and contribute to overall well-being makes it a promising addition to the spectrum of treatment options available to patients.
#ResonantFrequencySoundTherapy#SplenicRupture#AdjunctiveTreatment#TraditionalMedicine#SoundTherapyBenefits#HolisticHealing#AlternativeTherapies#MedicalAdjuncts#IntegrativeMedicine#healthcareinnovations
0 notes
Text
Introduction
Ruptured spleen traumatic, also known as splenic rupture, is a condition where the spleen is damaged or torn due to trauma or injury. The spleen is an important organ located in the upper left side of the abdomen, and it plays a crucial...
#Mirari #MirariDoctor #MirariColdPlasma #ColdPlasma
0 notes
Text
Spontaneous Rupture of Wandering Spleen: Case Report by Mina Alvandipour in Journal of Clinical and Medical Images, Case Reports

Abstract
Keywords: Spleen; wandering spleen; ectopic spleen; splenic rupture.
Introduction
A wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2% [1]. wandering spleen is caused by either extreme laxity or absence of the normal ligaments that anchor the spleen to the left upper quadrant. Gravity also plays a role by allowing the spleen to descend into the lower abdomen attached by its vascular pedicle [2]. Symptoms depend on the degree of torsion and range from chronic abdominal pain in mild torsion to acute pain in severe torsion and infarction. Accurate clinical diagnosis is difficult because of the rarity of the condition and non-specific symptoms. Radiological evaluation includes usage of ultrasound, Doppler, abdominal CT or MRI depending upon availability or preference [3]. A wandering spleen can be either congenital or acquired. In the congenital condition the ligaments fail to develop properly, whereas in the acquired form the hormonal effects of pregnancy and abdominal wall laxity are proposed as determining factors .However, the precise etiology of the wandering spleen is not known [1]. We present a spontaneous rupture of a wandering spleen with severe torsion and infarction and abdominal pain without any history of trauma.
Case Report
A 25 years old female present to emergency unit with 2 week history of progressive abdominal pain, recurrent constipation ,vomiting and loss of appetite. There was no history of melena, fever, and hematochezia and weight loss. On examination there was periumbilical and epigastria tenderness and a firm and tender mass in the right side of the abdomen without muscle guarding and rebound tenderness. The vital sign and laboratory results were all within the normal ranges, except decreased hematocrit (hemoglobin-8.4). The plain abdominal radiograph was un-remarkable while abdominal ultrasonography with color Doppler showed absence of spleen in its normal location in the left upper abdomen. Also it detects a heterogeneous hypoechoic capsulated mass with diameter of 175mm in right lower abdomen. Other organs of the abdomen were normal. Abdominal pelvic CT scan with and without contrast was recommended and findings was Absence of the spleen in its normal position in the left hypochondrium, and presence of large diameter mass (splenomegaly)in the right sub hepatic area(Wandering spleen) . Other organs of the abdomen were normal. Contrast-enhanced computed tomography (CECT) of the abdomen revealed whirlpool sign near the umbilicus. The splenic parenchyma showed abnormal enhanced areas, suggestive of splenic torsion and infarction.
A final diagnosis was wandering spleen with torsion of the vascular pedicle and infarction. The patient underwent a total splenectomy. During the laparotomy, an enlarged and infarcted mass was seen in right side of abdomen. The characteristic “whirlsign” can be seen in the area of the splenic vascular pedicle, indicative of torsion. Histological examination confirmed total infraction of the wandering spleen. The postoperative course was uneventful, and the patient was discharged on the 4th day after the operation.
Discussion
A wandering spleen is a rare but well-known entity. The incidence is < 0.2%. It is more common in females than males between the second to fourth decade of life and children [4]. Splenic weight >500 g in more than 8 out of 10 cases [5]. Interestingly, it has been reported that one out of three cases of wandering spleen appears in children bellow the age of 10 years old [7].
Wandering is characterized by splenic hyper mobility that results from elongation or mal-development of its suspensory ligaments. It is also known as aberrant, floating, displaced, prolapsed, ptotic, dislocated or dystopic spleen. Ectopic spleen, splenosis and accessory spleens are separate clinical entities and must be distinguished from it [5]. If the pedicle is twisted in the course of movement of the spleen, blood supply may be interrupted or blocked, resulting in severe damage to the blood vessels .Acute splenic torsion compromises venous outflow, which causes congestion and impairment of arterial inflow. Pain is originated from the splenic capsular stretching with rapid splenic enlargement and localized peritonitis [6]. Etiology is congenital or acquired. In case of congenital anomaly, a failure occur in fusion of the dorsal mesogastrium with the posterior abdominal wall during the second month of embryogenesis. Acquired risk factors that predispose to wandering spleen include pregnancy, trauma and splenomegaly [7]. Splenic torsion is usually clockwise. Complications of splenic torsion include: gangrene, abscess formation, local peritonitis, intestinal obstruction and necrosis of the pancreatic tail, which can lead to recurrent acute pancreatitis [8].
Wondering spleen had nonspecific symptoms such as abdominal pain that make diagnosis extremely challenging. As a result, radiologists play a major role in the diagnosis of this condition and its complications. Torsion may occur acutely and present with infarction or peritonitis. Chronic intermittent torsion can lead to pain, splenomegaly, and functional splenectomy. Contrast-enhanced computed tomography (CT) is the best imaging tool to make this diagnosis, although ultrasound may be used as well. Imaging findings on CT include identification of a spleen in an abnormal location, or with an abnormal orientation in the left upper quadrant. Often the wandering spleen is identified as a “comma” shaped mass in abdomen, with no normal left upper quadrant spleen [9].
Laboratory investigations are non-specific. Thrombocytopenia, through a mechanism of spleen enlargement secondary to compression of the splenic pedicle is rarely found [7]. The clinical presentation of wandering spleen is variable; it is either asymptomatic or noted incidentally during physical and radiographic examination or presents as acute abdomen due to torsion with subsequent infarction. The most common presentation is a mass with non-specific abdominal symptoms or intermittent abdominal discomfort due to congestion resulting from torsion and spontaneous detorsion [10]. Today, the only recommended treatment for wandering spleen is operation [7]. Splenectomy is indicated for infracted spleen and sometimes for huge splenomegaly precluding splenopexy. Splenopexy is the choice of treatment if the spleen is not infarcted [6]. Splenic preservation is highly recommended for young patients—those under one year of age up to those in their thirties—who are at particular risk for overwhelming post-splenectomy sepsis [10]. This should be appropriately followed up by the prophylactic vaccines against post-splenectomy sepsis syndrome. Ideally they should be administered before surgery; however, in emergencies this is not always possible [1].
Conclusion
In this case, splenectomy was done due to spleen infarction. Laparotomy was done in this case because of low experience at laparoscopy splenectomy. This report highlights the investigations and management necessary for a patient who presents with an ischaemic torted wandering spleen.
Acknowledgement: None.
Conflict of Interest: None.
Funds: None.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Spleen#wandering spleen#ectopic spleen#splenic rupture#ligaments#Radiological#abdominal pain#CECT#splenopexy#Mina Alvandipour#JCMICR
0 notes
Text
Spontaneous splenic rupture due to Peliosis and the association with malignancy: A case series and literature review
CMLHope.Com http://dlvr.it/SvXZV9
0 notes
Text
Clinician's tactics
Something physicians seem to be belittling about the side effects or what could happen during the briefing of the procedure is that “Major complications after donating stem cells are rare, but fatalities and life-threatening events such as deep vein thrombosis, splenic rupture, and cardiac arrest have been reported.” (Kisch and Forsberg).
This is something that physicians seem to leave out and or briefly mention in order not to scare or intimidate the donor.
" Negative effects since the transplant were also reported (21%) {...} and reported wishing they had been more informed of the possible side effects prior to the transplant." (Wiener et al.)
The donor is then blindsided by how much this can actually affect them and their sibling mentally and physically. The donor must have all the information before consenting to donate.
0 notes
Text
Know About Your Favorite Bollywood Actors and their Health Issues
Credit: Google
Being a star doesn’t come with all the comfort. It comes with so many pros and cons of a lavish life. Bollywood stars also suffer from serious health issues.
Working for 18 hours and traveling all over the world is not that easy. And the extremely hectic schedule of these Stars affects their health badly.
Here is the list of Bollywood Celebs with their health issues.
1.Salman Khan

The Bhaijaan of Bollywood was diagnosed with a neauopathic disorder ‘Trigeminal Neuralgia’ in the year 2011. This causes intense pain in jaws and cheeks. After which he was held with a surgery.
Also read: Bahubali Not Well? Read What Happened to Prabhas !!
2.Sonali Bendre

In the year 2018, she was diagnosed with cancer. She went New York for her treatment and was recovered from the disease.
3.Amitabh Bachchan
While shooting for his movie Coolie in 1982, he got injured which caused him splenic rupture. Which led him into coma. In the 2000 he also suffered from TB.
4.Hrithik Roshan
In the year 2013, he underwent a brain surgery. As he was having several injuries in the skull. The blood clots developed in his head during filming his movie Bang Bang.
5.Samantha Ruth Prabhu

She has recently posted on her social media account about her several health related issues. She is suffering from autoimmune condition. And she said, she will be fine within a couple of months.
6.Shah Rukh Khan
He has undergone over 6 shoulder surgeries. Due to which he has also been into depression for a long while.
7.Deepika Padukone

She has openly talked about her depression in media. Deepika has done phenomenal work in the film industry. But she says that depression made her suffer a lot and she has battled a long period of time. Also, she took a step to open a centre for mental health to help people who are facing depression.
Also read: Best Healthy Alternatives of Coffee to Boost Your Energy
0 notes
Text
Best Splenectomy Doctors in Faridabad
What is Splenectomy ?
A splenectomy is a surgical procedure that partially or completely removes the spleen

What are indications for Splenectomy ?
When it becomes very large such that it becomes destructive to platelets/red blood cells
Lymphomas
Certain cases of Splenic abscess
Certain cases of wandering spleen
Splenic vein thrombosis with bleeding gastric varices
Idiopathic thrombocytopenic purpura
Trauma
Following spontaneous rupture
For long-term treatment of congenital erythropoietic porphyria (CEP) if severe hemolytic anemia develops
What are the various ways of Splenectomy?
Laparoscopy is the preferred procedure in cases where the spleen is not too large and when the procedure is elective.
Open surgery is performed in trauma cases or if the spleen is enlarged.
Vaccination for pneumococcus, H. influenza and meningococcus should be given pre-operatively if possible to minimize the chance of overwhelming post-splenectomy infection (OPSI), a rapid-developing and potentially fatal type of septicaemia
What are the side effects of Splenectomy?
Increased risk of sepsis due to encapsulated organisms (such as S. pneumoniae and Haemophilus influenzae
An increase in blood leukocytes can occur following a splenectomy.
The post-splenectomy platelet count may rise to abnormally high levels (thrombocytosis), leading to an increased risk of potentially fatal clot formation
Splenectomy may also lead to chronic neutrophilia
A splenectomy also results in a greatly diminished frequency of memory B cells and increased risk of infection.
For More about Laparoscopic Splenectomy, you can reach directly to Dr. Mradul Garg at +91-9560413585
0 notes
Text
Stuff I Learned: Surgical Recall I
Chapter 1: Introduction
Allen’s test: check for patency of the ulnar artery before placing radial arterial line or performing ABG
Blumer’s shelf: metastasis to rectouterine or rectovesical pouch
Boas’ sign: right subscapular pain from cholelithiasis
Carcinoid triad (FDR)
Flushing
Diarrhea
Right heart failure
Homan’s sign: calf pain on forced dorsiflexion in DVT
Skull base fracture
Raccoon eyes: periorbital ecchymosis bilaterally = anterior cranial fossa
Battle’s sign: post-auricular ecchymosis over mastoid process = middle cranial fossa
CSF rhinorrhea/otorrhea
Hemotympanum
Splenic rupture
Ballance’s sign: dull LUQ; right RUQ
Kehr’s sign: severe left shoulder pain (diaphragmatic irritation
Acute appendicitis
Obturator sign: pain upon internal rotation of leg with hip and knee flexed
Psoas sign: pain upon hip extension with knee fully extended (psoas inflammation)
Rovsing’s sign: RLQ pain upon LLQ palpation
Pheochromocytoma
PHEochromocytoma
PHE
Palpitations
Headache
Episodic diaphoresis
PHEnoxybenzamine: alpha blocker, always before beta blocker to treat
10% bilateral, 10% malignant, 10% in children, 10% extra-adrenal, 10% familial
Hypocalcemia
Chvostek’s sign: twitching on tapping of facial nerve
Trousseau’s sign: carpal spasm after forearm occlusion with BP cuff
#let the learning begin#stuff i learned#surgical recall#pheochromocytoma#hypocalcemia#splenic rupture#skull base fracture#surgery#revision#textbook notes
1 note
·
View note
Note
Hello person that i really dont know. about that hurt comfort dialog prompts. 1 and 11 with bakudeku or tododeku, Ill let you choose hehehehe
Hello, person that I absolutely do not know anything about, I’m gonna do BakuDeku with 11 because I will fill this goddamn tag by myself if I have to, damn it. (I was gonna follow up with TodoDeku with 1, but it got too long so fuckit. Also, there’s a whole other story in the tags, you should read them all, lmao).
The explosion was loud enough to pierce through Izuku’s eardrums, and for a while, all he could hear was ringing, and his own frantic heartbeat. Katsuki was nowhere in sight, nor was the villain they’d been fighting for what seemed like a lifetime now. Deku wanted to believe that his partner had won, but he would not be able to tell until he saw him.
But when the smoke cleared, Katsuki still stood, tall and fierce and victorious. The villain laid at his feet, no longer a threat. When Izuku looked at him, the light from the fiery sunset behind him cast a halo around his imposing figure.
And then, Katsuki stumbled. It was slight, and he caught himself, but Izuku noticed it; he knew his partner for so long and in so many ways that it would have been impossible to miss it.
“Kacchan?” he called, preparing to race forward when Bakugo’s hand in the air stopped him.
“Stay where you are, Deku!” he demanded, panting heavily.
“Are you okay?” Izuku asked, plainly disregarding his demand.
“Are you blind or just stupid?” Bakugo barked dryly. “Do I look like I’m on the fucking ground?”
“You’re hurt, though,” Deku remarked, taking a few steps forward regardless. Indeed, there was something unnerving about the slow-bleeding wounds on Bakugo’s arms, the sheen of sweat on his face, his heaving chest and his pale face. “Let me see your wounds.”
“For fuck’s sake, they’re just scratches!” his partner growled. “Now stay the fuck away from me! Don’t you have anything better to do!?”
“Kacchan, calm down!”
“I am calm! Shut the fuck up!” Even for Bakugo Katsuki, this felt like a whole new level of defensiveness. The last time that Izuku had seen him this anxious, he’d revealed his biggest secret to him and they’d decked it out in the training grounds after dark. “Go away, Deku!”
“What is wrong with you!?” No longer heeding restraint, Izuku rushed forward. In response, Bakugo spun around to stomp off, and that went as well as Izuku expected it.
Katsuki turned around, swayed in his spot, and stumbled a few steps until his face met with the ground.
“Kacchan!”
Izuku’s horror did not abate when his partner made weak efforts to stand up, clearly having trouble with his balance. All else forgotten, he rushed towards him.
“Don’t you fucking dare, Deku!” Katsuki spat, arms shaking with the simple effort of pulling himself up. From up close, his skin was white, almost yellow. He breathed heavily through his nostrils as if to bite down the pain. “Get the fuck away from me!”
“You’re hurt, Kacchan! Let me help you!” Deku insisted, jumping to his side and kneeling. For his efforts, he only got a weak punch to the face that sent both of them to the ground.
“I don’t… need… your goddamn help!” Bakugo insisted with a growl, trying to push himself up on his elbows at least. A grunt of pain escaped him, but when Izuku made a move to help him up, he persistently glared at him. That didn’t stop his partner from grabbing his face, sticky with the sickly sheen of sweat. Bakugo’s eyes eyes were clouded.
Izuku saw anger in them, he saw desperation, but he also saw pain and he also saw fear. He never saw fear in Bakugo’s eyes; ever.
“Tell me where it hurts,” he demanded firmly, even as Bakugo pulled away from his grip and shakily got on his knees. “Damn it, Kacchan, stop being so prideful and tell me what’s wrong with you!”
“Don’t…” Bakugo cut himself off with a stifled cry of pain, suddenly clutching at his left side and doubling over. “Fuck… fuck!”
“Kacchan!” Deku didn’t think, just moved. He put his hands where Katsuki was gripping his side, and the problem immediately became obvious to him.
Bakugo’s abdomen was rock solid.
Of course, it was rock solid every day thanks to Katsuki’s intense training regiment, but distended and stretched as it was, it was anything but normal.
“Oh god.” Blood drained from Izuku’s face like it was draining from Bakugo’s body. “You’re bleeding.”
“No… No shit,” Bakugo grunted, pressing down hard on his side. “Broken ribs… cut something…”
“We need to get you to a medic, now!” Izuku hurried him, grabbing his shoulders to help him up. He got a weak slap to his arms for his trouble.
“Don’t… Don’t touch me. I can… do it myself,” Katsuki grunted, but only got a knee off the ground before he was tumbling forward again. This time, Deku was ready, and caught him.
He didn’t know if his arms were the solace for which Bakugo’s body yearned, for the moment he fell against Izuku’s chest, he went limp.
“Kacchan?” Urgently shot up in Izuku’s brain immediately as the dead weight pressed onto him. “Kacchan! Answer me!”
“Don’t…” Katsuki mumbled, words chewed up and almost indiscernible. His face was no longer a yellowish pale, but more like a foreboding grey. Whatever was bleeding was bleeding very fast.
Deku tried to gather his bearings, but his mind could not hold itself together. Not with Katsuki like this in his arms. He felt like a rag doll when Deku tilted his head up to look at him, eyes closed and pale lips parted. Against Deku’s chest, Bakugo’s heart hammered away fiercely, and when Izuku clutched him tightly in his arms, his heart almost gave out as well.
“Someone, please help!” he cried out blindly, weaving a hand into the hair at the nape of Katsuki’s neck, pressing his forehead into the crook of his neck as if his touch could warm up the cold body in his arms. “Please! Please help him!”
But nobody could hear him, and nobody came. At that moment, in their world, there existed no more heroes. Only Izuku and Katsuki. Only Deku and Kacchan, children, and powerless. Izuku’s hands no longer could reach him.
He clutched Bakugo’s body and let tears run down his face.
“Someone please help!” he repeated, glancing around him desperately. “He’s going to die!” Saying it out loud made it much more real. Bakugo was tough, and Deku trusted him to fight on, but the fight ran out of him with every ounce of blood in his abdomen.
“D-De… ku… don’t…” Bakugo breathed out against Izuku’s neck, his desperate gasps for air almost physically painful to hear.
His fingers made creases in Katsuki’s arms when he clutched tighter, white markings dotting his skin in the wake of Deku’s realization.
There were no more heroes, just him, and Katsuki.
And just like he always had and always would, he still wanted to reach out and bring his Kacchan back from the brink.
“Full Cowl!” Before he knew it, unbridled power was rushing through his legs, threatening to break every bone in his body-again. He barely managed to twist the cap on his power before he was shooting off the ground, leaving dust in his wake. Villains and heroes be damned, Izuku only had one thing on his mind.
He had to save Kacchan.
It took him less than a minute to arrive where the ambulances were parked, paramedics working on treating a few civilians caught in the crossfire. Izuku’s flashy entrance worked in catching their attention; when he landed hard enough to crack the asphalt, all eyes turned to him.
“Please!” he tried again, Katsuki’s body limp against him. “Please, help him!”
And they did, finally. In the minute it took for Katsuki to be ripped away from him and secured on a stretcher, Izuku had cried out his name at least three times.
Bakugo did not respond, laying lifelessly on the stretcher as they wheeled him into the ambulance. Deku did not hesitate to follow, and nobody stopped him. Perhaps it was the sight of his face, eyes rimmed red and incessant tears carving tracks through the dirt smudged on his cheeks. Perhaps it was the sound of his breaking voice, the way he repeated Bakugo’s name so reverently, his cries a prayer to every cruel god that tried to take Katsuki away from him.
Perhaps it was the way he held Bakugo’s hand, fingers entwined and clutched tightly between his own, for if Bakugo could no longer hold on, then Izuku vowed to hold on for both of them.
“I can’t lose you, Kacchan,” he pleaded, watching Katsuki’s shallow breathing fog up the oxygen mask. The ambulance hit a bump, and the stretcher rattled.
Bakugo cracked one eyelid open, just enough for Izuku to see that he was still there, and that he was still fighting. His lips moved to make up a word, and Izuku momentarily removed the oxygen mask to hear it.
“De…ku…” Katsuki rasped out weakly, as if Izuku’s name would be the last thing he ever said. “Don’t…”
“Stop refusing my help, Kacchan.” Izuku’s heart squeezed, and he squeezed Katsuki’s hand in return.
He froze when Katsuki squeezed back, so weak that Izuku could have missed it. But he wouldn’t. He would never.
“Don’t…” Bakugo’s eyes slipped shut again, his pale face going slack. Izuku was hit with the sudden realization that he would never be able to save every person that needed his help. “Don’t… let… me… go…”
But Deku could still help the ones that called his name.
And therefore, Izuku would not let go.
#bakudeku#katsudeku#bnha#boku no hero academia#my hero academia#bnha fanfic#drabble#fanfiction#fanfic#bakugo katsuki#midoriya izuku#cin answers#cin's writing#musical prince#bakugo has a splenic rupture by the way and he's going into uncompensated shock#the more u know#he could very well die or could very well live#matt i know youre gonna headcanon as him dying in the ambulance haha#I STILL THINK HE LIVES#he gets to the operating room and they open his abdomen up and blood LITERALLY gushes out of him in fountains#his heart stops twice during the surgery and they shock him back into sinus tachycardia#they finally remove his spleen and tie off his arteries and transfuse like... 27 units of blood into him lmao#and the blood-covered surgeons and nurses announce that it's finished#and deku is just watching all of this unfold from the observation area and just freaking. the. fuck out.#like straight up terror man it's way past a lil bit of anxiety#he's never been this scared in his life#and then todoroki arrives in a hurry like 'yo uraraka told me u were in the hospital dude what happened'#and deku just collapses in his arms and screams and todoroki is like.... ummmm.... pat pat?#cause he's so relieved that kacchan is still alive but whaaaaatttt the fuck just happened#and what if he doesnt wake up from the anesthesia
11 notes
·
View notes
Text
thesis statement: people in general tend to think of bodies as static, and interpret symptoms as the result of predictable external forces acting upon the body.
e.g. “my dog is lethargic because he ate a bunch of fruit from the tree in the yard” vs the reality that the dog was bleeding internally from a ruptured splenic hemangiosarcoma.
the default assumption is that whatever is happening to you (or your sister, or your cat) can be explained using knowledge you already possess- it’s cold outside, there’s mold in her house, he was stung by a bee. you know these things, so you assume that one of them must be causing new symptom X.
but the disquieting reality is that bodies are constantly changing, and we frequently can’t perceive those changes directly. diagnostic testing exists precisely because there are so many more ways for bodies to get fucked up than you can possibly imagine, and most of them are not at all within your control. that’s scary, but I also find it comforting. if you believe that you have total control over your health with yoga and crystals and protein powder, illness becomes a personal failing rather than an intrinsic part of having a body. who wants to live like that?
301 notes
·
View notes