#SARS-CoV-2 is not mild
Photo
https://www.news-medical.net/news/20220224/Study-reports-persistent-SARS-CoV-2-lingering-within-tissues-of-patients-with-long-COVID.aspx
https://www.nbcnews.com/health/health-news/long-covid-even-mild-covid-linked-damage-brain-months-infection-rcna18959
9K notes
·
View notes
Text
Testing positive for Covid requires sending a whole lot of notifications
Testing positive for Covid requires sending a whole lot of notifications
At the start of last weekend, two negative Covid tests in a row had me thinking that my sore throat was the result of too much conference socializing or maybe a summer cold. But then I self-tested one more time Sunday night, because I was set to fly to Denver the next afternoon for the Stream TV Show–and that positive result has since led to my having to notify more people than I might have…
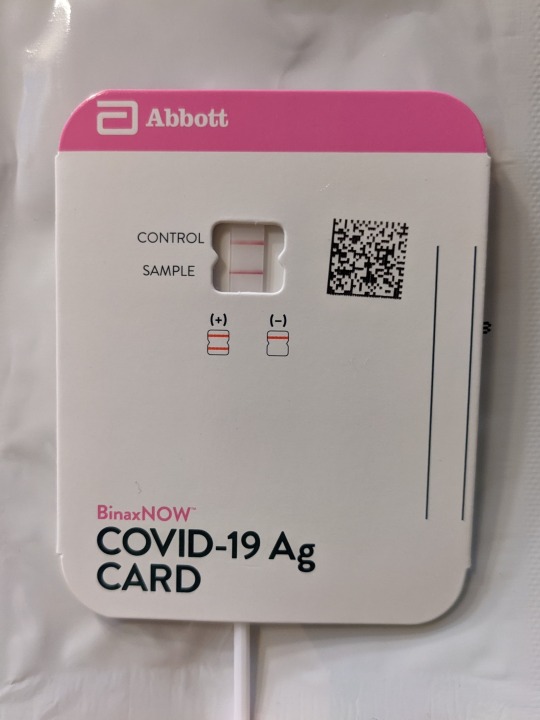
View On WordPress
#antigen test#cold or Covid?#common cold#conference#COVID vaccine#COVID-19#COVID-19 testing#COVIDWISE#exposure notification apps#mild Covid case#SARS-CoV-2
0 notes
Text
Updated vaccines against Covid-19 are coming, just as hospitalizations and deaths due to the virus are steadily ticking up again.
Today, the US Food and Drug Administration authorized new mRNA booster shots from Moderna and Pfizer, and a panel of outside experts that advises the Centers for Disease Control and Prevention voted to recommend the shots to everyone in the United States ages 6 months and older. Once Centers for Disease Control and Prevention director Mandy Cohen signs off on the recommendations and the vaccines are shipped, people can start getting the boosters.
The recommendation is projected to prevent about 400,000 hospitalizations and 40,000 deaths over the next two years, according to data presented at the meeting by CDC epidemiologist Megan Wallace.
This year’s mRNA vaccines are different from the 2022 booster in a key way. Last year’s shot was a bivalent vaccine, meaning it covered two variants: the original one that emerged in China in 2019, plus the Omicron subvariant BA.5, which was circulating during much of 2022. This fall’s booster drops the original variant, which is no longer circulating and is unlikely to return. It targets just the Omicron subvariant XBB.1.5, which was dominant throughout much of 2023.
Pfizer and Moderna’s vaccines work by introducing a tiny piece of genetic material called messenger RNA, or mRNA, that carries instructions for making SARS-CoV-2’s characteristic spike protein. Once it is injected, cells in the body use those instructions to temporarily make the spike protein. The immune system recognizes the protein as foreign and generates antibodies against it. Those antibodies stick around so that if they encounter that foreign invader again, they will mount a response against it.
Since the start of the Covid-19 pandemic, the virus has acquired new mutations in its spike protein and elsewhere. These mutations result in new variants and subvariants that diverge from the original virus. When enough mutations accumulate, these new versions can more easily evade the antibodies created by previous vaccine doses or infections.
The constantly evolving nature of the virus is the reason health regulators decided last year to update the original mRNA vaccines, which were designed against the version of the virus that first appeared in 2019. This year, once again, the virus has changed enough to warrant an updated booster.
In June, an advisory committee to the FDA recommended that this fall’s booster be a monovalent vaccine—targeting only the then-dominant XBB.1.5 subvariant.
At that meeting, committee members reviewed evidence suggesting that the inclusion of the original variant may hamper the booster’s effectiveness against newer offshoots. “The previous bivalent vaccine contained the ancestral spike and thus skewed immune responses to the old spike,” says David Ho, a professor of microbiology at Columbia University whose research, which is not yet peer-reviewed, was among the evidence the FDA panel reviewed. “This is what we call immunological imprinting, and it results in lack of immune responses to the new spike.” He thinks taking out the old variant should optimize the immune response.
But over the past few months, even newer Omicron offshoots have arrived. Currently, EG.5.1, or Eris, is the dominant one in the United States, United Kingdom, and China. Meanwhile, a variant called BA.2.86, or Pirola, has been detected in several countries. Pirola has raised alarm bells because it has more than 30 new mutations compared to XBB.1.5.
Even though the new boosters were formulated against XBB.1.5, they’re still expected to provide protection against these new variants. “The reason is, while antibodies are important in protection against mild disease, the critical part of the immune response that’s important for protecting against severe disease is T cells,” says Paul Offit, a professor of vaccinology at the University of Pennsylvania and member of the FDA’s vaccine advisory committee.
These cells are a different part of the immune response. Unlike antibodies, which neutralize a pathogen by preventing it from infecting cells, T cells work by eliminating the cells that have already been invaded and boosting creation of more antibodies. Both the Moderna and Pfizer-BioNTech Covid vaccines produce long-lasting T cells in addition to antibodies.
It’s why, Offit says, when the Omicron wave hit in late 2021 and peaked in January 2022, the US didn’t see a dramatic increase in hospitalizations and deaths even as cases rose significantly: People’s T cells kicked into gear, even when their antibodies didn’t recognize the Omicron variant.
“In some ways,” says Offit, when it comes to vaccine booster development, “it almost doesn’t matter what we pick to target” because the coronavirus has yet to evolve away from T cell recognition. “Everything works.”
Scientists think T cells are able to protect against severe Covid because they’re recognizing parts of the virus that have remained unchanged throughout the pandemic. “I suspect that as we continue to vaccinate, there are some conserved regions [of the virus],” says Jacqueline Miller, Moderna’s head of infectious diseases. “So even with the accumulation of mutations, we’re still building on previous immunity.”
People who have hybrid immunity—that is, have had a Covid infection and have also been vaccinated—seem to have the best immune responses to new variants, she says, which suggests that previous exposure shapes and improves immune responses to new variants. Preliminary studies show that antibodies generated by previous infections and vaccinations should be capable of neutralizing Pirola.
Earlier this month, Moderna issued a press release saying that clinical trial data showed that its updated booster generated a strong immune response against Pirola, as well as the more prevalent Eris variant.
In a statement to WIRED, Pfizer spokesperson Jerica Pitts said the company continues to closely monitor emerging variants and conduct tests of its updated monovalent booster against them. Data presented at Tuesday’s CDC meeting showed that Pfizer-BioNTech’s updated booster elicited a strong neutralizing antibody response against both Eris and Pirola.
The FDA expects that Covid-19 vaccines will continue to be updated on an annual basis, unless a completely new variant emerges that requires a different approach. “We will always be a little behind the virus,” says Ho. “In this instance, we won’t suffer too much, but that might not be the case going forward. Surveillance is imperative.”
814 notes
·
View notes
Text
SALUD: ¿PORQUE, NO TODOS SE CONTAGIAN CON EL COVID-19?
SALUD: ¿PORQUE, NO TODOS SE CONTAGIAN CON EL COVID-19?
HEALTH: WHY DOES NOT EVERYONE GET COVID-19?
El SARS-CoV-2 es un ejemplo extremo del misterio de la infección: puede matar a algunos y pasar desapercibido para otros. SARS-CoV-2 is an extreme example of the mystery of infection: it can kill some and go unnoticed by others.Un estudio ejecutado por la Universidad de Bristol en Reino Unido sobre la transmisión del coronavirus por el aire apunta que…

View On WordPress
#ASYMPTOMATIC WITH MILD DISEASE#HASTA QUE MOMENTO SE PUEDE CONTAGIAR=#HEALTH#LAS VACUNAS#lomasleido#PERSONAS SUPER INMUNES#PORQUE NO TODOS SE CONTAGIAN CON EL COVID.19?#SALUD#SARS-COV-2#THE CHILDADVANTAGE
0 notes
Text
COVID-19's long-term effects on the body: an incomplete list
COVID’s effect on the immune system, specifically on lymphocytes:
NYT article from 2020 (Studies cited: https://www.biorxiv.org/content/10.1101/2020.05.18.101717v1, https://www.biorxiv.org/content/10.1101/2020.05.20.106401v1, https://www.unboundmedicine.com/medline/citation/32405080/Decreased_T_cell_populations_contribute_to_the_increased_severity_of_COVID_19_, https://www.medrxiv.org/content/10.1101/2020.06.08.20125112v1)
https://www.biorxiv.org/content/10.1101/2022.01.10.475725v1
https://www.science.org/doi/10.1126/science.abc8511 (Published in Science)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9057012/
https://www.forbes.com/sites/williamhaseltine/2022/04/14/sars-cov-2-actively-infects-and-kills-lymphoid-cells/
https://www.cleveland.com/news/2022/10/in-cleveland-and-beyond-researchers-begin-to-unravel-the-mystery-of-long-covid-19.html
SARS-CoV-2 infection weakens immune-cell response to vaccination: NIH-funded study suggests need to boost CD8+ T cell response after infection
https://www.merckmanuals.com/professional/hematology-and-oncology/leukopenias/lymphocytopenia
https://thetyee.ca/Analysis/2022/11/07/COVID-Reinfections-And-Immunity/
Dendritic cell deficiencies persist seven months after SARS-CoV-2 infection
https://www.frontiersin.org/articles/10.3389/fimmu.2022.1034159/full
https://www.n-tv.de/politik/Lauterbach-warnt-vor-unheilbarer-Immunschwaeche-durch-Corona-article23860527.html (German Minister of Health)
Anecdotal evidence of COVID’s effects on white blood cells:
https://twitter.com/DrJohnHhess/status/1661837956875956224
https://x.com/TristanVeness/status/1661565201345564673
https://twitter.com/TristanVeness/status/1689996298408312832
Much more if you speak to Long Covid patients directly!
Related information of interest:
China approves Genuine Biotech's HIV drug for COVID patients
COVID as a “mass disabling event” and impact on the economy:
https://www.ctvnews.ca/health/report-says-long-covid-could-impact-economy-and-be-mass-disabling-event-in-canada-1.6306608
https://x.com/inkblue01/status/1742183209809453456?s=20
COVID’s impact on the heart:
https://www.dailystar.co.uk/news/world-news/deadly-virus-could-lead-heart-31751263 (Research from: Japan's Riken research institute)
https://www.brisbanetimes.com.au/national/queensland/unlike-flu-covid-19-attacks-dna-in-the-heart-new-research-20220929-p5bm10.html
https://www.mdpi.com/2077-0383/12/1/186
https://medicalxpress.com/news/2023-04-mild-covid-effects-cardiovascular-health.html
https://publichealth.jhu.edu/2022/covid-and-the-heart-it-spares-no-one
https://www.bhf.org.uk/informationsupport/heart-matters-magazine/news/coronavirus-and-your-health/is-coronavirus-a-disease-of-the-blood-vessels (British Heart Foundation)
COVID’s effect on the brain and cognitive function:
https://www.openaccessgovernment.org/article/brain-infection-by-sars-cov-2-lifelong-consequences/171391/
https://www.cidrap.umn.edu/covid-19/study-shows-covid-leaves-brain-injury-markers-blood
https://www.theguardian.com/world/2020/jul/08/warning-of-serious-brain-disorders-in-people-with-mild-covid-symptoms
Cognitive post-acute sequelae of SARS-CoV-2 (PASC) can occur after mild COVID-19
Neurologic Effects of SARS-CoV-2 Transmitted among Dogs
https://journals.lww.com/nsan/fulltext/2022/39030/neurological_manifestations_and_mortality_in.4.aspx
https://www.salon.com/2023/06/17/new-evidence-suggests-alters-the-brain--but-the-extent-of-changes-is-unclear/
https://www.scientificamerican.com/article/covid-virus-may-tunnel-through-nanotubes-from-nose-to-brain/
https://neurosciencenews.com/post-covid-brain-21904/
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
https://medicalxpress.com/news/2022-08-covid-infection-crucial-brain-regions.html
https://news.ecu.edu/2022/08/04/covid-parkinsons-link/
Covid as a vascular/blood vessel disease:
https://www.salon.com/2020/06/01/coronavirus-is-a-blood-vessel-disease-study-says-and-its-mysteries-finally-make-sense/
https://www.salon.com/2023/12/27/brain-damage-caused-by-19-may-not-show-up-on-routine-tests-study-finds/
https://www.nih.gov/news-events/news-releases/sars-cov-2-infects-coronary-arteries-increases-plaque-inflammation
https://www.mdpi.com/2077-0383/12/6/2123
https://www.sciencedaily.com/releases/2021/10/211004104134.htm (microclots)
Long Covid:
Post-COVID-19 Condition in Canada: What we know, what we don’t know, and a framework for action
https://www.ctvnews.ca/health/coronavirus/more-than-two-years-of-long-covid-research-hasn-t-yielded-many-answers-scientific-review-1.6235227
https://www.cbc.ca/news/canada/london/cause-of-long-covid-symptoms-revealed-by-lung-imaging-research-at-western-university-1.6504318
https://www.cbc.ca/news/canada/montreal/long-covid-study-montreal-1.6521131
https://news.yale.edu/2023/12/19/study-helps-explain-post-covid-exercise-intolerance
Other:
- Viruses and mutation: https://typingmonkeys.substack.com/p/monkeys-on-typewriters
Measures taken by the rich and world leaders
Heightened risk of diabetes
https://jamanetwork.com/journals/jama/fullarticle/2805461
https://www.nature.com/articles/d41586-022-00912-y
Liver damage:
https://timesofindia.indiatimes.com/city/mumbai/46-of-covid-patients-have-liver-damage-study/articleshow/97809200.cms?from=mdr
tl;dr: covid is a vascular disease, not a respiratory illness. it can affect your blood and every organ in your body. every time you're reinfected, your chances of getting long covid increase.
avoid being infected. reduce the amount of viral load you're exposed to.
the gap between what the scientific community knows and ordinary people know is massive. collective action is needed.
#putting this somewhere at least as reference for... somebody hopefully#covid#disability#y'all. it is bleak out there but some very good people are doing their best to help#we need as many people aware and helping as possible
460 notes
·
View notes
Text
Now we know how COVID attacks your heart
Even patients with mild COVID symptoms could face a higher risk of developing heart disease and stroke
By Sanjay Mishra Nov 07, 2023 04:08 PM 5 min. read
Scientists have noticed that COVID-19 can trigger serious cardiovascular problems, especially among older people who have a buildup of fatty material in their blood vessels. But now a new study has revealed why and shown that SARS-CoV-2, the virus that causes COVID-19, directly infects the arteries of the heart.
The study also found that the virus can survive and grow inside the cells that form plaque—the buildup of fat-filled cells that narrow and stiffen the arteries leading to atherosclerosis. If the plaque breaks, it can block blood flow and cause a heart attack or a stroke. The SARS-CoV-2 infection makes the situation worse by inflaming the plaque and increasing the chance that it breaks free.
This can explain long-term cardiovascular effects seen in some, if not all, COVID-19 patients.
SARS-CoV-2 virus has already been found to infect many organs outside the respiratory system. But until now it hadn't been shown to attack the arteries.
"No one was really looking if there was a direct effect of the virus on the arterial wall," says Chiara Giannarelli, a cardiologist at NYU Langone Health, in New York, who led the study. Giannarelli noted that her team detected viral RNA—the genetic material in the virus—in the coronary arteries. “You would not expect to see [this] several months after recovering from COVID.”
Mounting evidence now shows that SARS-CoV-2 is not only a respiratory virus, but it can also affect the heart and many other organ systems, says Ziyad Al-Aly, a clinical epidemiologist at Washington University in St. Louis. Al-Aly's research has shown that the risk of developing heart and cardiovascular diseases, including heart failure, stroke, irregular heart rhythms, cardiac arrest, and blood clots increases two to five times within a year of COVID-19, even when the person wasn't hospitalized.
"This important study links, for the first time, directly the SARS-CoV-2 virus with atherosclerotic plaque inflammation," says Charalambos Antoniades, chair of cardiovascular medicine at the University of Oxford, United Kingdom.
Virus triggers the inflammation in plaque
A recent study of more than 800,000 people led by Fabio Angeli, a cardiologist at University of Insubria in Varese, Italy, has shown that COVID-19 patients develop high blood pressure twice as often as others. More worrying is that the risk of cardiac diseases can also rise for patients who suffered only mild COVID symptoms.
"I saw a patient who now has a defibrillator, and she didn't even have a severe [COVID] illness," says Bernard Gersh, a cardiologist at Mayo Clinic, Rochester, Minnesota.
Wondering whether the cardiovascular damage during COVID was due to the virus directly attacking the blood vessels, the NYU team analyzed autopsied tissue from the coronary arteries and plaque of older people who had died from COVID-19. They found the virus was present in the arteries regardless of whether the fatty plaques were big or small.
"The original finding in this study is that the virus was convincingly found in the plaque in the coronary artery," says Juan Carlos Kaski, a cardiovascular specialist at St George's, University of London, who was not involved in the study.
The NYU team found that in the arteries, the virus predominantly colonized the white blood cells called macrophages. Macrophages are immune cells that are mobilized to fight off an infection, but these same cells also absorb excess fats—including cholesterol from blood. When microphages load too much fat, they change into foam cells, which can increase plaque formation.
To confirm that the virus was indeed infecting and growing in the cells of the blood vessels, scientists obtained arterial and plaque cells—including macrophages and foam cells—from healthy volunteers. Then they grew these cells in the lab in petri dishes and infected them with SARS-CoV-2.
Giannarelli found that although virus infected macrophages at a higher rate than other arterial cells, it did not replicate in them to form new infectious particles. But when the macrophages had become loaded with cholesterol and transformed into foam cells, the virus could grow, replicate, and survive longer.
"We found that the virus tended to persist longer in foam cells," says Giannarelli. That suggests that foam cells might act as a reservoir of SARS-CoV-2. Since more fatty buildup would mean a greater number of foam cells, plaque can increase the persistence of the virus or the severity of COVID-19.
Scientists found that when macrophages and foam cells were infected with SARS-CoV-2 they released a surge of small proteins known as cytokines, which signal the immune system to mount a response against a bacterial or viral infection. In arteries, however, cytokines boost inflammation and formation of even more plaque.
"We saw that there was a degree of inflammation [caused] by the virus that could aggravate atherosclerosis and cardiovascular events," says Giannarelli.
These findings also confirm previous reports that measuring inflammation in the blood vessel wall can diagnose the extent of long-term cardiovascular complications after COVID-19, says Antoniades.
"What this study has found is that plaque rupture can be accelerated and magnified by the presence of the virus," says Kaski.
Understanding heart diseases after COVID
While this new research clearly shows that SARS-CoV-2 can infect, grow, and persist in the macrophages of plaques and arterial cells, more studies are needed to fully understand the many ways COVID-19 can alter cardiac health.
"The NYU study identifies one potential mechanism, especially the viral reservoir, to explain the possible effects" says Gersh. "But It's not going to be the only mechanism."
This study only analyzed 27 samples from eight elderly deceased patients, all of whom already had coronary artery disease and were infected with the original strains of virus. So, the results of this study do not necessarily apply to younger people without coronary artery disease; or to new variants of the virus, which cause somewhat milder disease, says Angeli.
"We do not know if this will happen in people who have been vaccinated," says Kaski. "There are lots of unknowns."
It is also not clear whether and to what extent the high inflammatory reaction observed in the arteries of patients within six months after the infection, as shown in the new study, will last long-enough to trigger new plaque formation. "New studies are needed to show the time-course of the resolution of vascular inflammation after the infection," says Antoniades.
COVID patients should watch for any new incidence of shortness of breath with exertion, chest discomfort, usually with exertion, palpitations, loss of consciousness; and talk to their physician about possible heart disease.
374 notes
·
View notes
Text
“Imaging revealed white matter lesions in the subcortical frontal and parietal lobes, in 71% of cases. Cognitive impairment was present in 46% of this group.”
The first "S" in "SARS" means "Severe." "Mild covid" is an oxymoron.
#mask up#covid#covid 19#covid isn't over#pandemic#covid conscious#long covid#covid is airborne#wear a mask#coronavirus
53 notes
·
View notes
Text

🎇 NYE COVID-19 RED ALERT - AVOID CROWDS & MASK UP 🎆
You wouldn't know it from our governments, but Turtle Island, aka the US & Canada, are in the worst spike of illness and deaths since 2020's deadly Omicron surge.
That means it's more dangerous to go to a New Years party this weekend than it's been for approximately 96.4% OF THE ENTIRE PANDEMIC. It's bad out there tonight, and your odds of staying healthy after an unmasked gathering are NOT good.

The more people at your party, the higher the chance you'll catch COVID-19. You may think it's worth the risk, since many people appear to have "mild" infections, but that's not the whole story.
The first 2 weeks of COVID-19, aka the "acute phase", are just the beginning. Even if you don't need emergency hospitalization, or even if you never have any symptoms at all, the virus SARS-CoV-2 responsible for COVID-19 silently turns your immune system against you and shreds the lining of your circulatory and nervous systems. This can permanently elevate your risk of heart attacks, strokes, digestive problems, and even life-changing disabling disorders like ME/CFS.
And even if you escape relatively unscathed, you could pass the virus onto loved ones who WILL get hit hard, and survive with new life-long disabilities, or not survive at all.

COVID-19 never left, and our healthcare systems are NOT looking out for us. We have to take care of each other. Please, please rethink going out to that party tonight. If you can't avoid socializing, please protect yourself as much as you can:
Wear WELL-FITTING respiratory masks like N95s & KN94s
Use nasal sprays before & after, & CPC mouthwash after
Gather outdoors whenever possible
Get good air circulation indoors with air filters like CR Boxes, or open windows for outside air (bundle up if it's cold)
More resources on these tips, and how to reduce the damage if you do get sick, can be found on this COVID Safety Roundup list. All graphics courtesy of the Pandemic Mitigation Collection and Dr. Michael Hoebert, from their website. Hoebert further breaks down the data on his twitter too.
You can also ask me any particular questions and I'll do my best to help! We all deserve to survive this, and we'll do it together.
#covid 19#long covid#still masking#mask up#actually disabled#covid isn't over#covid19#new year#happy new year#new years eve
89 notes
·
View notes
Text
About 16 million people in the United States have Long Covid, a poorly understood disorder that causes body aches, headaches, fatigue, insomnia, brain fog and other symptoms long after an initial infection with COVID-19. For some, the symptoms are mild, but for other they are so severe they become disabling.
Why do some people quickly recover from Covid, while about one in five have lingering symptoms?
A new animal study found that thousands of genes involved in nervous system function are affected by SARS-CoV-2, and may cause lasting damage to dorsal root ganglia, the spinal nerves that carry pain and other sensory messages to the brain. Scientists believe that genetic damage may be what causes Long Covid.
“Several studies have found that a high proportion of Long Covid patients suffer from abnormal perception of touch, pressure, temperature, pain or tingling throughout the body. Our work suggests that SARS-CoV-2 might induce lasting pain in a rather unique way, emphasizing the need for therapeutics that target molecular pathways specific to this virus,” explains co-author Venetia Zachariou, PhD, chair of pharmacology, physiology & biophysics at Boston University’s Chobanian & Avedisian School of Medicine. (Read more at link)
123 notes
·
View notes
Text


Guys this is driving me nuts. This is not true. I understand why you might think this is true, since a recent study seemed to conclude this and it was covered by every news outlet on the planet, but it is not.
This is the study: Acute and postacute sequelae associated with SARS-CoV-2 reinfection. It was published in Nature Medicine, which is a very reputable journal. The study itself is fine. The headlines covering it were very misleading. Here’s the problem.
The study was observational only. You’re familiar with “correlation vs. causation”? This type of study can only find correlations. It cannot conclude that COVID reinfection causes an increased risk of hospitalization, severe disease, etc. It is equally possible (and much more plausible IMO!) that reinfection occurs more frequently in people who already have higher health risks. The study cannot differentiate between the two.
The study was also done using VA records. This means that any mild COVID infection or positive COVID test that did not result in an encounter with the VA health system would not have been captured in the study. They were already only looking at people who had severe enough COVID -- and severe enough reinfections -- that they sought medical treatment.
Furthermore -- any COVID exposure that did not result in infection due to acquired immunity would, naturally, not have been captured. Because COVID infection absolutely confers natural immunity.
Check out this other recent (Nov. 3, 2022) study: Immune Imprinting and Protection against Repeat Reinfection with SARS-CoV-2. It was published in the New England Journal of Medicine, probably the most prestigious medical journal out there. They’re studying unvaccinated people in Qatar who have -- guess what -- natural immunity from prior COVID infection(s).
“Omicron infection induces strong protection against a subsequent omicron infection.2,4 In the present cohort study, an additional, earlier infection with non-omicron SARS-CoV-2 was found to strengthen this protection against a subsequent omicron infection. The earlier pre-omicron infection may have broadened the immune response against a future reinfection challenge.
“Confers immunity” and “induces strong protection against” does not mean you will never get COVID. This is the same fallacy that anti-vaxxers use to justify not getting the vaccines. It’s still possible to get COVID, but with some combination of vaccines and prior infections, you will have memory immune cells that will greatly reduce your chances of severe disease.
Other recent studies have been looking at a phenomenon called “immune imprinting”, which describes the fact that your body would much rather use existing memory immune cells to defend against a very closely related variant of something it has already encountered, rather than make a whole fresh batch of very similar immune cells perfectly specific to the new variant. This has implications for the efficacy of the new bivalent booster vaccines that include the Omicron variant -- it’s possible that the two variants are too similar and including Omicron in the booster isn’t particularly useful. This recent pre-print study -- Immunogenicity of the BA.5 Bivalent mRNA Vaccine Boosters -- compared the old monovalent boosters with the new bivalent boosters that include Omicron, and found that there wasn’t actually that much difference. Both increased antibody levels against both original COVID and Omicron (yes, even the booster that didn’t include Omicron did that, because basically everyone has been exposed to Omicron at this point and has antibodies against it, and the antibodies seem to be similar enough that they all trigger together). But both boosters increased antibodies against original COVID far more powerfully than they increased antibodies against Omicron, because everyone’s first exposure (in the study) was to original COVID, so those are the immune memory cells your body has the most of to begin with. They conclude:
Our findings suggest that immune imprinting by prior antigenic exposure5 may pose a greater challenge than currently appreciated for inducing robust immunity to SARS-CoV-2 variants.
This is tricky! This could help explain why Omicron infections are still so prevalent despite pretty good coverage with really good vaccines against original COVID (though bivalent booster coverage is pretty abysmal in the US at least, so hard to say). This does not mean that natural immunity "doesn't work" with COVID and it certainly doesn't mean that "reinfection just makes you get worse and worse".
COVID is not great. You should avoid getting it and if you get it you should definitely avoid spreading it. If you have risk factors for getting severe COVID, you should really avoid getting it, and if you have those risk factors then you already knew that. But it is not a case of “natural immunity does not exist, every subsequent reinfection only gets worse and worse forever until you die”. This is anti-science alarmism. I understand that something along these lines was in a hundred different newspapers recently but I hope this explains why that reporting was misleading and ultimately wrong.
#covid#sorry this is long and nuanced i am just getting itchy with how many fact-free covid posts i have been seeing sorry
287 notes
·
View notes
Text
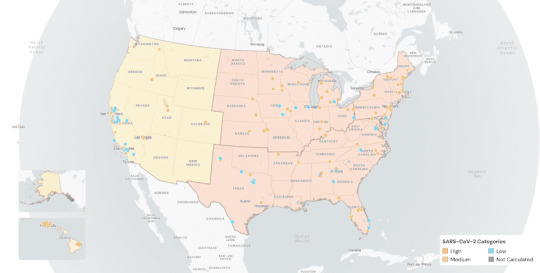
The Weather (according to Wastewater)
SARS-CoV-2 levels in wastewater are being reported by Biobot again as they file an appeal with the CDC. For now, we will use the map below from WastewaterSCAN, another source for wastewater surveillance. One quarter of the nation’s wastewater testing sites remain shut down while the appeal is being processed, creating an overall gap in data reliability that we could continue to experience for several months to come. We anticipate releasing another COVID map depicting transmission levels developed by the People’s CDC in the coming weeks.
According to WastewaterSCAN, nationally, COVID wastewater levels are at medium while the Northeast, Midwest, and the South are high since their last update from October 31, 2023. Across the US, COVID wastewater levels are at 239.7 Pepper mild mottle virus (PMMoV) Normalized on October 31, 2023, down from a peak of 430.5 PMMoV Normalized on August 28, 2023, but slightly up from 201.8 PMMoV Normalized on October 18, 2023. PMMoV normalization differs from how Biobot normalizes data, so the raw numbers are not directly comparable with Biobot’s.

Wins
On October 27-29, #namingthelost hosted a memorial at St Mark’s Church in-the-Bowery in NYC in order to name, honor, and mourn the individuals that we have lost and continue to lose due to COVID and COVID-related complications. On their homepage, #namingthelost states “We know it didn’t have to be this way, that our country’s leaders made choices that risked our lives. We know we can choose a different way forward that is about caring for all of us.”
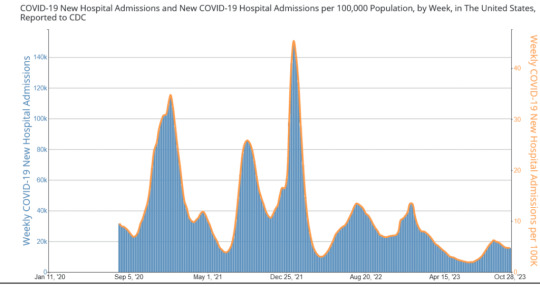
Hospitalizations and Deaths
New weekly hospitalizations associated with COVID have stopped dropping, staying at a constant of over 15,000 hospitalizations for the past three weeks including the week of October 28, 2023. According to the CDC’s COVID Data Tracker, there have been another 4,000 reported deaths from COVID in the past month of October. We mourn these 4,000 individuals as this is not “normal.” A reminder that the lives and livelihoods of everyone in our entire society continue to remain at stake. Do not lower your standards as many in society, especially those in the business sector, normalize this ongoing atrocity as they demand for a return to on-site work even though most people prefer the option of remote work. Continue to demand layers of protection such as high-quality masking, ventilation, filtration, and testing, in all settings to prevent ongoing COVID infections, hospitalizations, Long COVID, and death.
Vaccines and Treatment
Do not wait to get an updated COVID vaccine for those 6 months and older! Multiple options are available including Pfizer, Moderna, or Novavax. Access continues to be challenging especially for those with certain health insurance plans or who are uninsured. Lack of interest and access difficulties have likely all contributed to a low uptake of only 3.5% of Americans receiving the most recent and updated COVID vaccine. The Bridge Access program ensures no-cost access and you can find a location as determined by the federal government, but be sure to call ahead and ask to ensure local participation.
Similarly, federal funding for COVID treatment options, such as Paxlovid and Lagevrio, have transitioned from the federal government to health insurance plans on November 1, 2023. Individuals with Medicare or Medicaid will have access through the end of 2024 and those uninsured will have access at least through the end of 2028 via the federal government, but limited information has been provided. Test to Treat locations continue to provide no-cost access to those without insurance while Pfizer’s Patient Assistance Program can also provide no-cost access to Paxlovid (Nirmatrelvir–Ritonavir). If your health insurance plan does not cover COVID treatments such as Paxlovid, you can participate in the Co-Pay Savings Programs offered by Pfizer, which drops the cost out-of-pocket down to 140 dollars.
Long COVID
The scientific understanding of Long COVID continues to grow with a recent study demonstrating that viral persistence may potentially affect some individuals resulting in Long COVID. However, another study that compared Long COVID outcomes among patients who received Paxlovid at the Veterans Health System did not observe lower rates of Long COVID after treatment. A guaranteed treatment for Long COVID remains to be determined while the primary approach in avoiding this is to employ layers of protection such as consistently using a high quality mask or respirator in order to lower the risk, ultimately preventing a COVID infection.
Take Action
HICPAC, the federal committee that advises the CDC and DHHS on infection control practices in healthcare, met on November 2-3 and voted on draft documents, which continue to fail to protect patients and healthcare workers from COVID infections. We provided a nationwide virtual space to protest the CDC HIPCAC meeting on Thursday, November 2nd. Multiple members of the People’s CDC were recognized to provide public comments to members of HICPAC during the meeting. We also submitted the following official statement this week as our comment. We provide instructions and asked you to also submit a comment to them using our recommendations in response to their terrible decision via email to [email protected] by 11:59 pm on Monday, November 6th to include in their meeting minutes (date has passed). The next steps of their process will include the publication of draft documents in the Federal Register, which can be reviewed and commented on by the general public.
Lastly, local groups are a primary opportunity to impact your community. Get involved locally and join a local group.
#op#covid#long covid#covid isn't over#covid 19#covid-19#coronavirus#pcdc#people's cdc#pandemic#covid news#covid19#public health#covid pandemic#medical#medical news#img#described in alt text
18 notes
·
View notes
Text
Chinese Hospitals Are Housing Another Deadly Outbreak
In Beijing and other megacities in China, hospitals are overflowing with children suffering pneumonia or similar severe ailments. However, the Chinese government claims that no new pathogen has been found and that the surge in chest infections is due simply to the usual winter coughs and colds, aggravated by the lifting of stringent COVID-19 restrictions in December 2022. The World Health Organization (WHO) has dutifully repeated this reassurance, as if it learned nothing from Beijing’s disastrous cover-up of the COVID-19 outbreak.
There is an element of truth in Beijing’s assertion, but it is only part of the story. The general acceptance that China is not covering up a novel pathogen this time appears reassuring. In fact, however, China could be incubating an even greater threat: the cultivation of antibiotic-resistant strains of a common, and potentially deadly, bacteria.
Fears of another novel respiratory pathogen emerging from China are understandable after the SARS and COVID-19 pandemics, both of which Beijing covered up. Concerns are amplified by Beijing’s ongoing obstruction of any independent investigation into the origins of SARS-CoV-2, the virus that causes COVID-19—whether it accidentally leaked from the Wuhan lab performing dangerous gain-of-function research or derived from the illegal trade in racoon dogs and other wildlife at the now-infamous Wuhan wet-market.
Four years ago, during the early weeks of the COVID-19 outbreak, Beijing failed to report the new virus and then denied airborne spread. At pains to maintain their fiction, Chinese authorities punished doctors who raised concerns and prohibited doctors from speaking even to Chinese colleagues, let alone international counterparts. Chinese medical statistics remain deeply unreliable; the country still claims that total COVID-19 deaths sit at just over 120,000, whereas independent estimates suggest the number may have been over 2 million in just the initial outbreak alone. Now, Chinese doctors are once again being silenced and not communicating with their counterparts abroad, which suggests another potentially dangerous cover-up may be underway.
We don’t know exactly what is happening, but we can offer some informed guesses.
The microbe causing the surge in hospitalization of children is Mycoplasma pneumoniae, which causes M. pneumoniae pneumonia, or MPP. First discovered in 1938, the microbe was believed for decades to be a virus because of its lack of a cell membrane and tiny size, although in fact it is an atypical bacterium. These unusual characteristics makes it invulnerable to most antibiotics (which typically work by destroying the cell membrane). The few attempts to make a vaccine in the 1970s failed, and low mortality has provided little incentive for renewed efforts. Although MPP surges are seen every few years around the world, the combination of low mortality and difficult diagnostics has meant there is no routine surveillance.
Although MPP is the most common cause of community-acquired pneumonia in school children and teenagers, pediatricians such as myself refer to it as “walking pneumonia” because symptoms are relatively mild. Respiratory Syncytial Virus (RSV), influenza, adenoviruses, and rhinoviruses (also known as the common cold) all cause severe inflammation of the lungs and are far more common causes of emergency-room visits, hospitalization, and death in infants and young children. Why should MPP be acting differently now?
One contributing factor to the severity of this outbreak may be “immunity debt.” Around the globe, COVID-19 lockdowns and other non-pharmaceutical measures meant that children were less exposed to the usual range of pathogens, including MPP, for several years. Many countries have since seen rebound surges in RSV. Several experts agree with Beijing’s explanation that the combination of winter’s arrival, the end of COVID-19 restrictions, and a lack of prior immunity in children are likely behind the surging infections. Some even speculate that that substantial lockdown may have particularly compromised young children’s immunity, because exposure to germs in infancy is essential for immune systems to develop.
In China, MPP infections began in early summer and accelerated. By mid-October, the National Health Commission had taken the unusual step of adding MPP to its surveillance system. That was just after Golden Week, the biggest tourism week in China.
Infection by two diseases at the same time can make things worse. The usual candidates for coinfection in children—RSV and flu—have not previously caused comparable surges in pneumonia. One difference this time is COVID-19. It is possible that the combination of COVID-19 and MPP is particularly dangerous. Although adults are less susceptible to MPP due to years of exposure, adults hospitalized for COVID-19 who were simultaneously or recently coinfected by MPP had a significantly higher mortality rate, according to a 2020 study.
Infants and toddlers are immunologically naive to MPP, and unlike COVID-19, RSV, and influenza, there is no vaccine against MPP. It seems implausible that no child (or adult) has died from MPP, yet China has not released any data on mortality, or on extrapulmonary complications such as meningitis.
Most disturbing, and a fact being downplayed by Beijing, is that M. pneumoniae in China has mutated to a strain resistant to macrolides, the only class of antibiotics that are safe for children less than eight years of age. Beyond discouraging parents to start ad hoc treatment with azithromycin, the most common macrolide and the usual first-line antibiotic for MPP, Beijing has barely mentioned this fact. Even more worrying is that WHO has assessed the risk of the current outbreak as low on the basis that MPP is readily treated with antibiotics. Broader azithromycin resistance in MPP is common across the world, and China’s resistant strain rates in particular are exceptionally high. Beijing’s Centers for Disease Control and Prevention reported macrolide resistance rates for MPP in the Beijing population between 90 and 98.4 percent from 2009 to 2012. This means there is no treatment for MPP in children under age eight.
Fears over a novel pathogen are already abating. After all, MPP is rarely lethal. But antimicrobial resistance (AMR) is. Responsible for 1.3 million deaths a year, AMR kills more people than COVID-19. No country is immune to this growing threat. Since China, where antibiotics are regularly available over the counter, leads the world in AMR, it is inconceivable that this issue hasn’t yet come up, particularly during WHO’s World AMR Awareness week, from Nov. 18 to Nov. 24.
Any infectious disease physician would want to know: Did WHO asked China the obvious question—what is the level of azithromycin resistance of M. pneumonia in the current outbreak—and include the answer in its risk assessment? Or did it ask about resistance to doxycycline and quinolones, antibiotics that can be used to treat MPP in adults? Even if WHO did ask, China isn’t telling, and WHO isn’t talking.
China’s silence isn’t surprising. Its antibiotic consumption per person is ten times that of the United States, and policies for AMR stewardship are predominantly cosmetic. While surveillance is China’s strong point, reporting is not.
Despite Spring Festival, the Chinese celebration of the Lunar New Year and another peak travel period, approaching in February 2024, WHO hasn’t advised any travel restrictions. It should have learned the danger of accepting Beijing’s statements at face value. Four years ago, Beijing’s delay enabled more than 200 million people to travel from and through Wuhan for Spring Festival. That helped COVID-19 go global. Since China’s AMR rates are already so high, importing AMR from other countries isn’t a major concern for China. Export is the issue, and China’s track record in protecting other countries is abysmal.
Rather than repeating the self-serving whitewashing coming from Beijing, WHO should be publicly pressing China about the threat of mutant microbes. Halting AMR is essential. Before antisepsis and antibiotics, surgery was a treatment of last resort. Without antibiotics, we lose 150 years of clinical and surgical advances. Within ten years, we are at risk of few antibiotics being effective. It may not be the novel virus that people were expecting, but the next pandemic is already here.
13 notes
·
View notes
Note
Hi, I'd like to know if there's a SARS-Cov-2 vaccine for cats and/or dogs? A quick google told me one for mink was considered in '21, but nothing about pet species. I'm thinking of getting a cat and would like to avoid playing the worst pingpong. Yes, I'm vaccinated, but it is known that even vaccinated people can get and pass on the infection, including to their pets.
gettingvetted here.
No, there is not a vaccine available. That's because while cats and dogs *can* get COVID-19, they typically have very mild or no symptoms at all and have NOT been proven to transmit the virus back to humans or to other pets (outside of extremely close, unnatural confinement in small cages with deliberate airflow to and from other cats).
63 notes
·
View notes
Text
ID: Person with long brown hair in white cowl neck white knit sweater holding coffee cup with Greek style design. Video is captioned.
New crucial information from David Putrino of the Putrino Laboratory, and the Mount Sinai long covid clinic. Leading expert, and facility on the front of this disease.
Take aways:
Vaccination as of 2024, according to this information does not prevent long covid.
I'd like to include other sources state vaccines reduce long covid by percentages, though no higher than 68.7%. It is important to also factor the dwindling and low rates of vaccination as of 2024 (17%), and highly mutagenic, immune evasive and contagious nature of SARS-CoV-2.
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(23)00414-9
https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people-booster-percent-pop5, (completed primary series + updated bivalent booster)
https://ourworldindata.org/grapher/covid-variants-bar?time=earliest
https://www.nature.com/articles/s41579-023-00878-2 "Like most RNA viruses, coronaviruses evolve rapidly"
The point being, while it is encouraged to get vaccinated, vaccination alone is not sufficient to robustly protect individuals or the general population from infection or development of virus associated disease/long covid.
Literature and resources on the full inventory of mitigation methods, please read my pinned post or search for the December 2023 update.
Many long covid sufferers, especially now, have multiple vaccinations, are median age 38, had mild feeling or even asymptomatic infection and were not hospitalized.
Note: mild infection does not mean harmless, and segments and statements from Mount Sinai and Dr. David Putrino illustrate why.
Furthermore, while it is my personal opinion mild and asymptomatic infection is quite likely a sign of immune evasion, there is some other evidence and real world examples that may support my hypothesis. - Admin/mod
You can listen to the whole interview here: https://www.bayarealyme.org/blog/long-covid-what-we-have-learned-about-chronic-illness-from-the-front-lines/
#SARS-CoV-2#SARS CoV 2#covid-19#covid 19#covid#long covid#Ongoing pandemic#pandemic#public health#news#February 2024#Month of February#February#David Putrino#Putrino Lab#Mount Sinai#Long covid clinic
6 notes
·
View notes
Text
From the report by Beth Mole, posted 29 Feb 2024:
In a lengthy background document, the agency laid out its rationale for consolidating COVID-19 guidance into general guidance for respiratory viruses—including influenza, RSV, adenoviruses, rhinoviruses, enteroviruses, and others, though specifically not measles. The agency also noted the guidance does not apply to health care settings and outbreak scenarios.
"COVID-19 remains an important public health threat, but it is no longer the emergency that it once was, and its health impacts increasingly resemble those of other respiratory viral illnesses, including influenza and RSV," the agency wrote.
The most notable change in the new guidance is the previously reported decision to no longer recommend a minimum five-day isolation period for those infected with the pandemic coronavirus, SARS-CoV-2. Instead, the new isolation guidance is based on symptoms, which matches long-standing isolation guidance for other respiratory viruses, including influenza.
"The updated Respiratory Virus Guidance recommends people with respiratory virus symptoms that are not better explained by another cause stay home and away from others until at least 24 hours after both resolution of fever AND overall symptom are getting better," the document states. "This recommendation addresses the period of greatest infectiousness and highest viral load for most people, which is typically in the first few days of illness and when symptoms, including fever, are worst."
The CDC acknowledged that the eased isolation guidance will create "residual risk of SARS-CoV-2 transmission," and that most people are no longer infectious only after 8 to 10 days. As such, the agency urged people to follow additional interventions—including masking, testing, distancing, hygiene, and improving air quality—for five additional days after their isolation period.
"Today’s announcement reflects the progress we have made in protecting against severe illness from COVID-19," CDC Director Dr. Mandy Cohen said in a statement. "However, we still must use the commonsense solutions we know work to protect ourselves and others from serious illness from respiratory viruses—this includes vaccination, treatment, and staying home when we get sick."
Overall, the agency argued that a shorter isolation period would be inconsequential. Other countries and states that have similarly abandoned fixed isolation times did not see jumps in COVID-19 emergency department visits or hospitalizations, the CDC pointed out. And most people who have COVID-19 don't know they have it anyway, making COVID-19-specific guidance moot, the agency argued.
In a recent CDC survey, less than half of people said they would test for SARS-CoV-2 if they had a cough or cold symptoms, and less than 10 percent said they would go to a pharmacy or health care provider to get tested. Meanwhile, "The overall sensitivity of COVID-19 antigen tests is relatively low and even lower in individuals with only mild symptoms," the agency said.
The CDC also raised practical concerns for isolation, including a lack of paid sick leave for many, social isolation, and "societal costs."
The points are likely to land poorly with critics.
“The CDC is again prioritizing short-term business interests over our health by caving to employer pressure on COVID guidelines. This is a pattern we’ve seen throughout the pandemic,” Lara Jirmanus, Clinical Instructor of Medicine at Harvard Medical School, said in a press release last month after the news first broke of the CDC's planned isolation update. Jirmanus is a member of the People's CDC, a group that advocates for more aggressive COVID-19 policies, which put out the press release.
Another member of the group, Sam Friedman, a professor of population health at NYU Grossman School of Medicine, also blasted the CDC's stance last month. The guidance will "make workplaces and public spaces even more unsafe for everyone, particularly for people who are high-risk for COVID complications," he said.
But, the CDC argues that the threat of COVID-19 is fading. Hospitalizations, deaths, prevalence of long COVID, and COVID-19 complications in children (MIS-C) are all down.
COVID-19 vaccines are safe and effective at preventing severe disease, death, and to some extent, long COVID—we just need more people to get them.
Over 95% of adults hospitalized with COVID-19 in the 2023–2024 respiratory season had no record of receiving the seasonal booster dose, the agency noted.
Only 22% of adults got the latest shot, including only 42% of people ages 65 and older. In contrast, 48% of adults got the latest flu shot, including 73% of people ages 65 and older. But even with the crummy vaccination rates for COVID-19, a mix of past infection and shots have led to a substantial protection in the overall population.
The CDC even went as far as arguing that COVID-19 deaths have fallen to a level that is similar to what's seen with flu. "Reported deaths involving COVID-19 are several-fold greater than those reported to involve influenza and RSV. However, influenza and likely RSV are often underreported as causes of death," the CDC said.
In the 2022–2023 respiratory virus season, there were nearly 90,000 reported COVID-19 deaths.
For flu, there were 9,559 reported deaths, but the CDC estimates the true number to be between 18,000 and 97,000.
In the current season, there have been 32,949 reported COVID-19 deaths to date and 5,854 reported flu deaths, but the agency estimates the real flu deaths are between 17,000 and 50,000.
"Total COVID-19 deaths, accounting for underreporting, are likely to be higher than, but of the same order of magnitude as, total influenza deaths," the agency concluded.
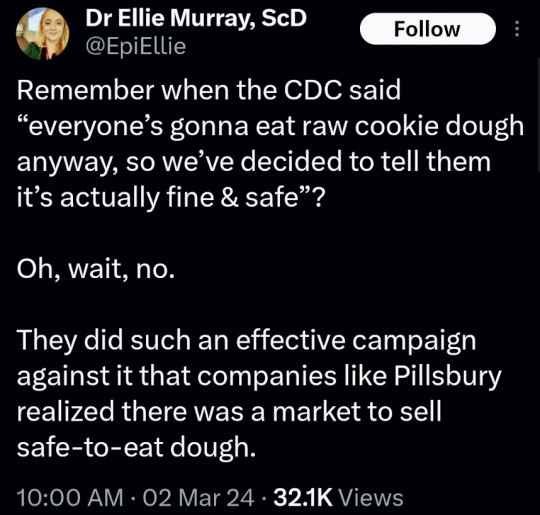
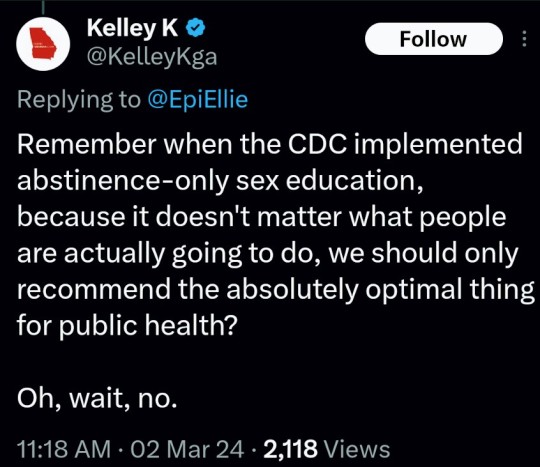
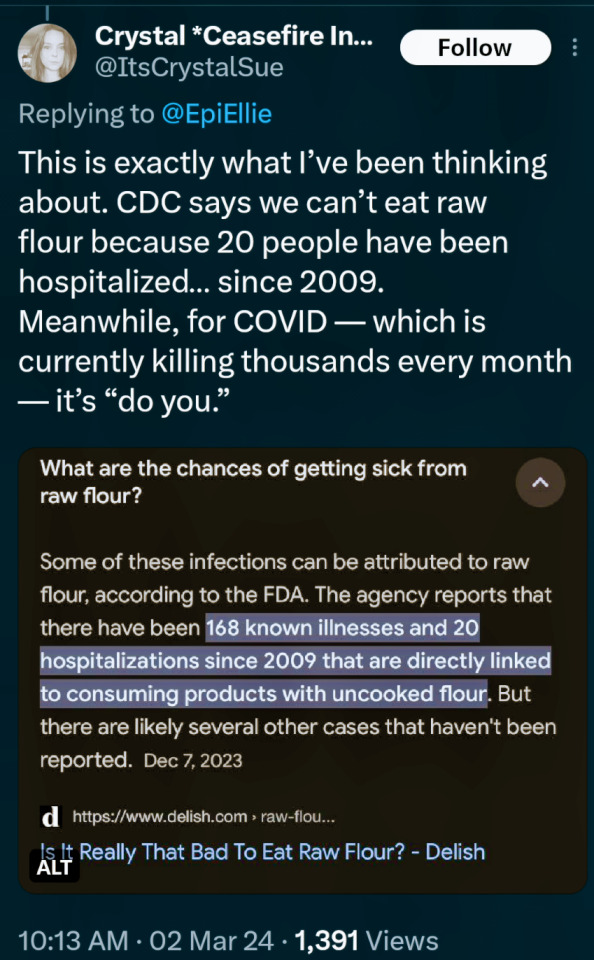
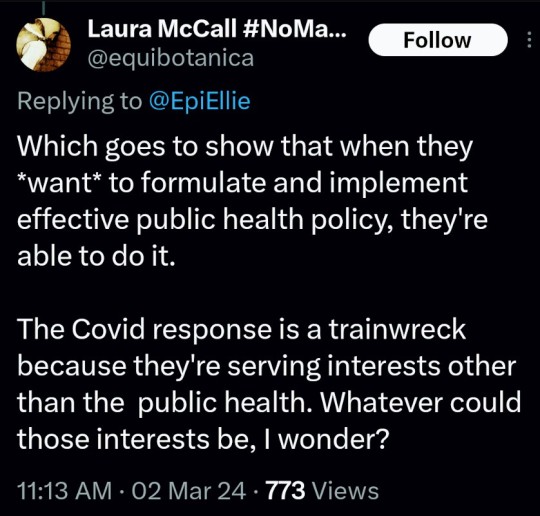
(say no to raw dough: CDC)
#please stay safe#the vaccines are safe#yes the covid shot is safe#covid is not a hoax#covid causes permanent long term damage to your body even if you're healthy#news#scicomm#science#ars technica#covid--19#coronavirus#beth mole#pandemic#the cdc#centers for disease control#5 day covid isolation#yes you should stay home for at least 5 days if you test positive for covid#Open windows to ventilate indoor space with outdoor air to prevent virus transmission#Wear a mask that doesn't touch your lips#keep distance from others
5 notes
·
View notes