#adenohypophysis
Text
How does one identify the location of the pituitary gland in the brain?
The pituitary gland, also known as the hypophysis, is a small, pea-sized gland located at the base of the brain. It is often referred to as the “master gland” because it controls the function of other endocrine glands in the body. Despite its small size, the pituitary gland plays a critical role in maintaining a wide range of bodily functions, including growth and development, metabolism, and…

View On WordPress
#adenohypophysis#Anatomy#brain#computed tomography#diagnosis#endocrine system#Health#hormones#imaging techniques#magnetic resonance imaging#nasal endoscopy#neurohypophysis#pituitary disorders#Pituitary gland#symptoms#treatment
0 notes
Text
A Review on Role of Prolactin in Birds
Abstract
In this article, we review the role of Prolactin, the parental hormone secreted by the adenohypophysis of the pituitary gland in
birds. Release of prolactin is regulated by the Ca+ dependent mechanism in birds. In lactating mammals, prolactin is associated
with regulation of milk production, whereas, in birds, this hormone is associated with incubation behaviour and broodiness. In
pigeons, is associated with the secretion of crop milk. Plasma concentration of prolactin and Luteinizing hormone varies with the
breeding cycle which determines the success of incubation in birds.
Keywords: Prolactin; Role; Birds
Authors: Violet BJ* and Kannan TA
0 notes
Photo

A helpful mnemonic to remember the functions of the hypothalamus.
2 notes
·
View notes
Text
Human Hormones and their properties
The Endocrine System is the collection of glands and organs that produce hormones which helps in the chemical co-ordination and integration in the human body. The following image shows various glands and their hormones.

Properties of hormones
These are discharged by endocrine organ (biogenic in source).
Their discharges is delivered straightforwardly into blood (aside from nearby hormones for example gastrin).
These are conveyed to remotely find explicit organs, called target organ.
These have explicit physiological activity (excitatory or inhibatory). These co-ordinate diverse physical, mental and metabolic exercises and look after homeostasis.
The hormones have low sub-atomic weight for example ADH has an atomic load of 600–2000 daltons.
These demonstration in extremely low focus for example around10–10 molar.
Hormones are non antigenic.
These are generally fleeting. So have a no camulative impact.
Some hormones are snappy acting for example adrenalin, while some acting gradually for example ostrogen of ovary.
Some hormones emitted in dormant structure called Prohormone for example Favorable to insulin.
Hormones are explicit. They are transporters of explicit data to their particular objective organ. Just those objective cell react to a specific hormone for which they have receptors.
Pituitary Gland (Hypophysis)
(1) Pituitory is known as hypophysis cerebri, its name pituitary was given by vesalius.
(2) Muller's organ of amphioxus and subneural organ of hardmania is homologous to pituitary of vertebrates.
Parts and segment
(1) Adenohypophysis (Anterior projection)
Pars distalis
Pars tuberalis
Pars intermedia
(2) Neurohypophysis (Posterior projection)
Pars nervosa
Infundibulum
Hypothalamus
1. Position and Structure: Hypothalamus is the floor of diencephalon. It is shaped of masses of dark issue, called hypothalmic cores, containing neurosecretory cells. It is associated with front pituitary projection by blood vessels of hypophyseal entryway framework and with the back pituitary flap by axons of its neurons, both going through the pituitary tail.
2. Hormones of hypothalamus: Neurosecretory cells of hypothalamus emit neurohormones called delivering factors (RF) or restraining factors (IF). These neurohormones are conveyed by hypophyseal gateway framework to adenohypophysis (essential objective organ) and animate or restrain the arrival of trophic hormones from adenohypophysis. These neurohormones are proteinous in nature and shaped of 3 – 20 amino acids.
Thyroid organ
1. The name "thyroid" was presented by Thomas Wharton (1656).
2. It is gotten from Greek "Thyreos" a shield.
3. Location: This is the biggest endocrine organ of our body. It is situated in our neck upon the ventral part of larynx (sound box or Adam's apple) and a couple of foremost most tracheal rings. It is a dim earthy colored and H-molded bilobed organ.
4. Hormones of thyroid:
Thyroid organ secretes two iodinated hormones.
(a) Thyroxine: It is an iodine containing (6% iodine) amine hormone which is gotten from tyrosine amino corrosive. Chemically thyroxine is tetraidothyronine however likewise found as tri-iodothyronine. Emission of thyroxine is contrarily relative to the blood level of thyroxine (criticism system).
(b) Thyrocalcitonin (TCT): It is a long peptide hormone discharged by parafollicular by cells of thyroid organ (C-cells). It discharge is managed by expanded plasma level of calcium by criticism instrument.
5. Irregularities of thyroid organ
(a) Hypothyroidism: (Decreased segment of thyroxine from thyroid organ).
(b) Hypersecretion of thyroid hormones (Hyperthyroidism or thyrotoxicosis) : This may likewise be a hereditary imperfection, however for the most part it is given by interminable contaminations (flu, stiffness, tonsilitis, tuberculosis, measles, challenging hack, and so on.) pregnancy, admission of huge dosages of iodine, over-eating, and so forth. It results into an extensive increment in glucose and oxygen utilization by cells and the pace of oxidative digestion in the mitochondria.
Parathyroid organ
1. Hormones of parathyroid: Active hormone emitted by parathyroids is parathormone (PTH), additionally called Collip's Hormone (Phillips collip, 1925).
2. Irregularities of parathormones
(a) Hypoparathyroidism (Hyposecretion of parathormone)
(b) Hyperparathyroidism (Hypersecretion of parathormone)
Pancreas
1. Hormones of pancreas and their job:
(a) Insulin: Insulin manages how the body uses and stores glucose and fat.
(b) Glucagon: This is discharged by the alpha cells of islets of Langerhans. Its capacity is to hoist glucose level in blood when glucose is insufficient.
(c) Somatostatin and Pancreatic polypeptide: Modern physiologists have proposed that the d and F (PP) cells of pancreas separately discharge somatostatin (SS) and pancreatic polypeptide (PP). Somatostatin takes after the development hormone inhibitory hormone (GHIH) emitted by hypothalamus.
Thymus organ
1. Function of thymus organs
Thymus is haemopoietic, just as, an endocrine organ.
The significant capacity of thymus is to emit thymosin hormone, thymic humoral factor (THF), thymic factor (TF), thymopoietin.
Thymus is basic in neonatal (recently conceived) baby and postnatal kid for ordinary advancement of lymphoid organs and cell invulnerability.
Gonads
1. The gonads are the sex organs, the testicles and the ovary.
(i) Testes
The testis structure part of the male conceptive framework, and is where sperm and testosterone are created.
Elements of Testes
It animates the male conceptive framework to develop to full measure and become utilitarian.
It invigorates the arrangement of sperms (spermatogenesis) in the seminiferous tubules.
It additionally decides the male sexual conduct sex encourage, forceful conduct.
Under its impact protein anabolism increments.
(ii) Ovary
The ovary is a ductless conceptive organ in which the female regenerative cells are delivered.
2 notes
·
View notes
Text

🇺🇸 Patriotic Pituitary 🇺🇸
There's a little Red (acidophils) White (chromophobes) & Blue (basophils) in us all!
Happy 4th of July everyone!
i❤️histo
———
The pituitary gland (hypophysis) is the king of the endocrine glands! It is so important that it sits in its own throne on the floor of the skull called the sella turcica where is sends out hormones to control the entire body via the blood stream.
It has two distinct parts:
An anterior pituitary (adenohypophysis) which is glandular and colorful and a posterior pituitary (neurohypophysis) which is pale and subdued because it is composed of the axons of nerves that reside in the hypothalamus of the brain.
The patriotic adenohypophysis (shown here) constantly flies its red, white and blue flag. Cheering on the organs of the body by sending them signalling molecules.
The red cells are acidophils: they make Growth Hormone (to urge our bodies to grow) and Prolactin (to make sure milk is produced during pregnancy).
The white cells are chromophobes: they don’t have a clearly understood function in the pituitary.
The blue cells are basophils: they produce Thyroid Stimulating Hormone (TSH - which excites the secretory cells of the thyroid gland), Follicle Stimulating and Luteinizing Hormone (FSH, LH - these are important in reproductive processes in the body) and Adrenocorticoptrophic Hormone (ACTH - which excites the secretory cells of the adrenal cortex).
#histology#anatomy#pathology#science#4th of july#independence day#med school#med student#vet science#vet school#premed#med lab#nursing#nurse#dental student#dental school#dental#histotech#histopathology#endocrine#pituitary#ihearthisto
116 notes
·
View notes
Text
TAFAKKUR: Part 12
Your Endocrine System: Part 1
We are now approaching the end of the series of organs that told you about themselves. They have been pointing out the seal of God on them, and celebrating themselves as they manifest the beauties and the delicacies of God’s art. Thus, they have not only expanded your knowledge, but also guided people to the truth of God’s Oneness, stressing that natural and biological causes alone can never be an explanation for their splendid creation.
Each of your organs told you about its perfect structure and how it functioned within your body system. Let us think that each organ is a musical instrument. No matter how splendid and artful a musical instrument is, its true value is understood only among other orchestra instruments as they perform a wonderful concert. Your body is like that orchestra, where hundreds of instruments play together. In addition to the perfect structure of each organ, more importantly all the organs have to work together perfectly as a team. The success of an orchestra depends on how the instruments play in harmony with each other. The conductor of an orchestra is the person who ensures that harmony. The orchestra members carefully watch the conductor and play according to his arm movements, sometimes louder or softer, sometimes pausing or breaking into a very loud introduction. That is how a perfect concert can be performed.
In order to achieve such harmony, the organs in your body need a system that works just like a good orchestra conductor. This “regulating system,” which has to maintain the perfect harmony and order of the ongoing activities in your body, has two sub-units: One is the brain and the nervous system, and the other is me; your endocrine system (hormonal system). Since I work as a system that consists of many organs, from now on I will refer to myself as “us.” Each of us adjusts itself to the whole system by carefully watching the movements and works of the other organs. At our head are the brain and nervous system, which act as the general control center. However, it cannot carry out the regulating and controlling task alone; it needs our help.
The most basic principle that your body has to follow in order to maintain its health is keeping the inner medium stable in a dynamic balance while responding to varying environmental conditions properly. This is also known as homeostasis. For the inner medium to be kept stable, it is first of all important to be aware of the changes that are happening in the outer world, which is initially done by your sense organs. The signals related to the changes in the outer world are sent to your brain and nervous system through the sense organs. Afterwards, the signals are evaluated, and then they are sent to the related organ so that the proper reaction is produced and the inner balance can be regained. While all the activities regarding growth and reproduction are carried out, the inner medium should be kept stable at the same time (homeostasis). In order for all these activities to be performed continuously, you need inner secretion glands, which are small, but highly important.
The most important of all your organs that constitute the endocrine system is called the Pituitary (hypophysis) gland, which is recognized as the commander of all these organs and situated in your brain. The other secretion glands included in my system are the thyroid, parathyroid, suprarenal (adrenal) gland, epiphysis, pancreas, testicles, and ovarium. Now, these small but very important organs of mine will respectively talk about themselves and demonstrate the perfect program and the sensitive balance within which they work. You are the one who will draw the necessary lessons from this.
In all tissues, there are specific recipient molecule groups that respond to a particular hormone. Each hormone is programmed to stimulate its target cells, which contain those special recipient molecule groups that start doing their specific work. The principal functions of my endocrine system are: to enable growing; to regulate the necessary reproduction process in an ordered manner; and to carry out the physiological processes in the body in a relatively stable medium. I guess your amazement, admiration, love, and apprehension will increase when you hear about my secretion glands. Now, here comes the hypophysis.
My name is Hypophysis (the Pituary Gland)!
I am appointed as the commander of all your glands. Therefore, I am situated in a very firm place at the lower brain. I am an organ that is as small as a bean and that weighs only a few grams, but I have got so many talents. I have two parts. The first is my frontal lobe (adenohypophysis) which secretes most of the hormones. Our Creator has given key roles to the hormones of my frontal lobe to direct secretion activities of other endocrine glands. For example, thyrotropin hormone is arranged in such a way that it affects the thyroid gland and stimulates it for secretion. The unbalance in my thyrotrophic secretion affects the function of Thyroid gland negatively. If it is secreted too much, hyperthyroid; if it is secreted too little, hypothyroid illnesses emerge. In both cases, some problems occur during metabolism. Adrenocorticotropic hormone is created to arrange the activities at the adrenal cortex. Follicular stimulating hormone has two very important roles. The first one is regulating the secretion of estrogen, which is one of the female hormones. The second one is maintaining the physiological activities in the maturation of sperm cells in males, as well as the egg cells in females, for the continuation of human generation. The Luteinizing hormone together with the Estrogen stimulates the secretion of other sexual hormones (progesterone and testosterone).
When you were born, you were 20 inches tall. Now you are almost 6 ft tall. Both your height and your hands and feet grew. Meanwhile, your head and body got bigger proportionally. Another important secretion of yours that controls your growth appropriate to your age is somatotropin hormone. If, for some reason, my working balance got deteriorated, and this hormone secreted less, you would be like a dwarf, or some of your parts would be unbalanced with your body and abnormally short. If this hormone were secreted too much, then you would get into gigantism due to abnormally large growth. Together with gigantism illness, several problems occur; i.e., heart and blood pressure problems, muscle weaknesses, and problems regarding immunity and general metabolism.
Other hormones that are secreted from my frontal lobe are prolactin hormones, which help milk glands develop in expecting mothers, and melanocyte stimulating hormone, which stimulates the pigment cells that give color to your skin. However, these two hormones have no relation with the other hormonal glands.
The lipoprotein molecule of my melanocyte stimulating hormone helps the morphine substances, known as encephalin and endorphin, to be synthesized. You can call these two substances naturally inherent drugs. These secreted substances help you to bear several physical pains. The secretion of my hormones has direct relation with your nervous system and psychological well-being.
Although formed in the hypothalamus part of the brain, one of the hormones that is secreted after being stored in my back lobe (Neurohipofiza) is oxytocin, and the other one an antidiuretic hormone called vasopressin. Oxytocin makes the smooth muscles work. In particular, it stimulates the contractions at uterus during labor and delivery, and it also stimulates the secretions of milk canals by making them contract. Vasopressin enables blood vessels to shrink, causes the blood pressure to increase, and also reduces the production of urine by increasing the transition of water to blood through the kidneys. Hence, it prevents dehydration in hot and dry weather. In the deficiency of the secretion of this hormone, an illness called diabetes insipidus will occur and water metabolism will be deteriorated. I have more amazing features to tell, but I should not be selfish. I think it is time for Thyroid to speak.
#allah#god#muhammad#prophet#sunnah#hadith#quran#ayah#islam#muslim#muslimah#hijab#help#dua#salah#pray#prayer#revert#convert#reminder#religion#welcome to islam#how to convert to islam#new muslim#new revert#new convert#revert help#convert help#islam help#muslim help
2 notes
·
View notes
Text
Vocabulary (pt.dccxliii)
Words taken from the AMA Manual of Style: A Guide for Authors and Editors, 10th edition, by the editors of JAMA and the Archives journals (Oxford University Press, 2007):
allograft (n.)
a tissue graft from a donor of the same species as the recipient but not genetically identical.
actinomycin D (n.)
a chemotherapy medication used to treat a number of types of cancer.
adenohypophysis (n.)
the anterior glandular lobe of the pituitary gland.
angina (n.)
(in full: angina pectoris) pain in the chest brought on by exertion, owing to an inadequate blood supply to the heart.
attenuation (n.)
the reduction of the force, effect, or value of something.
ascorbic acid (n.)
a vitamin found in citrus fruits and green vegetables, essential in maintaining healthy connective tissue, a deficiency of which results in scurvy.
aphasia (n.)
the loss of ability to understand or express speech, owing to brain damage.
autograft (n.)
a graft of tissue from one point to another of the same person’s body.
ancylostomiasis (n.)
a hookworm infection of the small intestine, often leading to anemia.
antirejection therapy (n.)
drugs used to prevent organ or tissue transplant rejection.
1 note
·
View note
Photo

Product name : Sermorelin
Alias: GRF 1-29 NH2, Sermorelin Acetate Hydrate
CAS: 86168-78-7
Sequence: H-Tyr-Ala-Asp-Ala-Ile-Phe-Thr-Asn-Ser-Tyr-Arg-Lys-Val-Leu-Gly-Gln-Leu-Ser-Ala-Arg-Lys-Leu-Leu-Gln-Asp-Ile-Met-Ser-Arg-NH2
MF: C149H246N44O42S
MW: 3357.96
Purity: 99%
Specification: 2mg/vial
Appearance: White Lyophilized Powder
Standard: USP
Method of Analysis: HPLC
Storage: Lyophilized peptides although stable at room temperature for 3 months, should be stored desiccated below -18° C. Upon reconstitution of the peptide it should be stored at 4° C between 2-21 days and for future use below -18° C.
Sermorelin Description
Sermorelin, in comparison, is not governed by the same strict laws of medical use and this is largely due to its safety profile. For this reason, sermorelin is much more accessible and is commonly prescribed by doctors in anti-aging and wellness clinics in conjunction with other releasing peptides such as GHRP-2 and GHRP-6.
Sermorelin acetate is a releasing peptide used for diagnostic evaluation of pituitary function and also for increasing growth in children. Off label usage of sermorelin acetate may include acute or age-related grow hormone insufficiency.
Sermorelin is a synthetic (man-made) version of a naturally occurring substance that causes release of grow hormone from the pituitary gland. Grow hormone is naturally produced by the pituitary gland and is necessary for growth in children. In children who fail to grow normally because their bodies are not producing enough grow hormone, this medicine may be used to increase the amount of grow hormone produced by the pituitary gland.
Sermorelin Applications
Sermorelin Acetate, also known as GRF 1-29, is a hormone produced by the brain that stimulates the production and release of Grow Hormone. Sermorelin Acetate was first developed in the 70s, which is thought to be the shortest fully functional fragment of GHRH and has been used as a test for Grow Hormone secretion. It is often used extensively in Anti-aging Therapy along with Test in men. Sermorelin Acetate affects a more primary source of failure in the GH neuroendocrine axis, has more physiological activity, and its use for adult hormone deficiency is not restricted.
Sermorelin is a GHRH peptide analogue. Its peptide sequence is comprised of 29 amino acids. This sequence is a portion of the endogenous human GHRH, and is currently considered to be the shortest synthetic peptide that possesses the full array of functional GHRH activity. Due to this fact, sermorelin is considered to be a grow hormone secretagogue .
Sermorelin has been used during research to stimulate the secretion of grow hormone from the adenohypophysis. The anterior pituitary secretes trophic hormones. Sermorelin has also been used in research stimulation tests to assess for pituitary sufficiency in relation to the secretion of the grow hormone.
1 note
·
View note
Link
Forevercenturymed.com: Body Growth Medicine For Male, Buy Genotropin, HGh For Sale Online, Hgh Increase Height, Order Hgh adenohypophysis cells is a peptide hormone.
#Pharmaceutical HGH For Sale#Body Growth Medicine For Male#Buy Genotropin#HGh For Sale Online#Hgh Increase Height#order hgh
1 note
·
View note
Text
Organoid Culture - Pluripotent Stem Cells or Adult Stem Cells
Previously, we discussed organoids and its generation, But a researcher new to this field have to learn how to establish an organoid culture. First of all, we will expalin origin of the organoids. Then we will study whether adult stem cells (ASCs) or pluripotent stem cells (PSCs) are better choice.
Organoids have great potential in research of organ development, disease modeling, drug screening and, precision and regenerative medicine[4]. Different tissue-derived organoids have successfully been generated from adult stem cells (ASCs) and pluripotent stem cells (PSCs). They can proliferate indefinitely in culturing conditions and have shown the ability to differentiate and re-organise mimicking the organ of origin[8].
The composition and organization of cells within organoids is dictated by the identity of the tissue being grown which in turn affects the overall size and shape of the organoid[1]. Since different cell types originate from different developmental stages and have different differentiation fates, the origin of the cell population is particularly important when studying the mechanisms of organoid formation.

Figure 1. ASCs and PSCs-derived organoid culture protocols[1]
A: ASC-derived organoids are grown from healthy or tumourous tissue biopsies. Tissues are processed into a single cell suspension which is directly embedded in an extracellular matrix. Media containing numerous growth factors, which vary dependent on the tissue being grown, is added and regularly changed until organoids have expanded.
B: PSC-derived organoids originate with 2D cultures of PSC’s that are grown into aggregates/spheroids. At this point, they may be embedded in an extracellular matrix and expanded to maturity using a growth factor rich media that is specific to the tissue of interest.
PSCs-derived organoids
PSC-derived organoids are mainly used to study organogenesis and developmental events that lead to tissue formation[9]. Organoids derived from PSCs are promising platforms for modeling organs for which tissue samples are not readily available, such as the brain, and for simulating the developmental process of organogenesis. Some types of organoids can only be generated from PSCs, including neurectodermal organoids, such as optic cup and brain organoids, and mesodermal kidney organoids.
Endoderm-derived epithelial organoids, such as gastrointestinal and respiratory organoids, can also be generated from PSCs. PSCs can be differentiated into endodermal progenitors, which are then embedded in ECM-protein-rich matrices, in which they mature under appropriate stimuli to form structures similar to native organs.
In contrast to their ASC-derived analogues, they also contain a mesenchymal layer and are usually larger, but, once established, they cannot be easily propagated by simple passaging[11].
Organoids generated from PSCs are (neurectoderm) retinal organoids, brain organoids, adenohypophysis organoids, cerebellar organoids; (endoderm) stomach organoids, small intestinal organoids, liver organoids, lung and thyroid organoids; (mesoderm) kidney[2].

Figure 2. Schematic of the Various Organoids that Can Be Grown from PSCs and the Developmental Signals that Are Employed[2]
However, PSC-derived organoids very rarely reach an adult tissue stage in vitro and usually resemble fetal-stage tissues. One possible reason for the limited maturation of PSC-derived organoids is the fact that development towards more mature cell types requires continuous culture for periods of time that typically exceed the capacity of the actual culturing methodologies. Another possibility is that, in contrast to ASC-derived organoids, cells in PSC-derived organoids are missing crucial interactions with other co-developing cell types because of our limited capacity to fully reconstruct embryonic developmental processes in vitro[9].
ASCs-derived organoids
ASCs-derived organoids are established by directly dissociating tissues of interest and culturing under conditions of tissue-specific growth factors for extended periods of time. The first organoids to be established are small intestinal organoids marked with Lgr5+ (Intestinal Organoid Culture Medium). For most ASCs-derived organoids, Wnt activators (Wnt3a , R-spondins , or the small molecule GSK3 inhibitor CHIR-99021) are key components and that Lgr5+ stem cells invariably appear in such specific culture medium[2].
Comparison of Pluripotent Stem Cells and Adult Stem Cells
Although both PSCs and ASCs-derived organoids can grow long-term in culture conditions, they differ markedly in developmental stages, cell types, and complexity.AdvantagesLimitationsESC/iPSC-based organoidsPotential to generate organoids for any type of tissue including ones difficult to access (eg, human brain organoids) Ability to form organoids consisting of heterotypic lineage cells, which is closer to the physiologicalstatus
Resource availability through existing iPSC banks
Capacity to study diseases manifesting at various human developmental stagesOrganoid generation protocols are more complex and time consuming in general
Resultant organoids are immature and less functional in general, and may need additional culture for maturationASC-based organoidsRobust protocols available for long-term culture and cryopreservation of several types of organoids
Protocols require fewer steps and generally less time overall
Recapitulate original tissue phenotypes more consistently
Malignant organoids (tumoroids) can be generated tooNeed organ samples containing stem cells to begin
Figure 3. Comparison between PSC(ESC/iPSC)-based organoids and ASC-based organoids[3]
Gastrointestinal organoids derived from ASCs contain only organ-specific epithelial cells and stem cells, whereas organoids derived from PSCs contain epithelial and mesenchymal cells, including fibroblasts and smooth muscles because PSCs can differentiate into multiple cell types.
While PSC-based organoids exploit developmental processes for their establishment, ASCs can be forced to form organoids by creating conditions that mimic the stem cell niche environment during physiological tissue self-renewal or during damage repair[2]. Although both retain the genetic information of original cells, ASC-based organoids tend to reproduce the original tissue phenotype directly. In contrast, organoids derived from PSC(ESC/iPSC) seem to have an ability to form more complex structures, likely due to their pluripotency potential. In a practical sense, ASC-based organoid protocols are simpler than ESC/iPSC-based organoids, because ASCs are already committed to organ-specific differentiation[3].

Since organoids-unlike cell lines-ideally represent all cellular components of a given organ, they are theoretically well suited for infectious disease studies, particularly of pathogens that are restricted to human beings and are dependent on specialized cell types[2]. In accordance with this global trend, the organoid industry continues to grow throughout the world, and organoid research and the market for organoids have been boosted by the demand for efficient and rapid drug development in response to the COVID-19 pandemic[4].
Related products
Wnt3a
Wnts are involved in regulating cell development, proliferation, differentiation, adhesion, polarity, cell-cell communication, survival and self-renewal. Wnt3a is one of the most critical morphogens in organoid cultures.
EGF
Epithelial tissue growth factor EGF binds to its receptor and induces proliferative changes. EGF is a factor required for the organoids culture of gastrointestinal tract, liver, thyroid, and brain etc.
R-spondin-1
R-spondin-1 plays a role in stem cell self-renewal and activation of Wnt signaling. It induces proliferation of intestinal crypt epithelial cells, healing of intestinal epithelial, renewal of intestinal epithelial stem cells, and is a key factor for the maintenance and proliferation of mouse/human stem/progenitor cells in organoids.
Noggin
Noggin is an endogenous inhibitor for bone morphogenetic proteins (BMP), regulating cell differentiation, proliferation and apoptosis. It is one of the most basic factors in organoid culture.
BMP-2, BMP-4
BMPs play crucial role in embryogenesis, development and maintenance of tissue homeostasis.
CHIR-99021
Selective GSK3 inhibitor for the generation of organoids. CHIR99021 + Valproic acid or CHIR99021 + LDN-193189, can synergistically promote the maintenance of
Lgr5+ ISCs in a self-renewing and undifferentiated state, resulting in ISCs-enriched cultivation.
Valproic acid
Inhibitor of HDAC; in organoid cultures, the combination of Valproic acid and CHIR99021 synergistically promote the maintenance of Lgr5+ ISCs in a self-renewing and undifferentiated state, resulting in ISCs-enriched cultivation.
LDN-193189
A selective BMP type I receptor inhibitor with IC50 of 5 nM and 30 nM for ALK2 and ALK3, respectively.
IWP-2
Inhibitor of Wnt processing and secretion with IC50 of 27 nM.
DAPT
Inhibits Notch 1 signaling and induces cell differentiation.
All products from MCE are only used for scientific research or drug registration applications, we do not provide products and services for human use.
References
[1]. Nino Iakobachvili, Peter J Peters. Humans in a Dish: The Potential of Organoids in Modeling Immunity and Infectious Diseases. Front Microbiol. 2017 Dec 5;8:2402.
[2]. Hans Clevers. Modeling Development and Disease with Organoids. Cell. 2016 Jun 16;165(7):1586-1597.
[3]. Noriko Watanabe, Katherine E Santostefano, Naohiro Terada, et al. A pathologist's perspective on induced pluripotent stem cells. Lab Invest. 2017 Oct;97(10):1126-1132.
[4]. Hanbyeol Lee, Jeong Suk Im, Da Bin Choi, Dong-Hun Woo. Trends in the global organoid technology and industry: from organogenesis in a dish to the commercialization of organoids. Organoid 2021;1:e11.
[5]. Kai Kretzschmar, Hans Clevers. Organoids: Modeling Development and the Stem Cell Niche in a Dish. Dev Cell . 2016 Sep 26;38(6):590-600.
[6]. Onur Basak, Joep Beumer, Hans Clevers, et al. Induced Quiescence of Lgr5+ Stem Cells in Intestinal Organoids Enables Differentiation of HormoneProducing Enteroendocrine Cells. Cell Stem Cell. 2017 Feb 2;20(2):177-190.e4.
[7]. Claudia Corrò, Laura Novellasdemunt, et al. A brief history of organoids. Am J Physiol Cell Physiol. 2020 Jul 1;319(1):C151-C165.
[8]. Angela L Caipa Garcia 1, Volker M Arlt, David H Phillips. Organoids for toxicology and genetic toxicology: applications with drugs and prospects for environmental carcinogenesis. Mutagenesis. 2021 Jun 19;geab023.
[9]. Giuliana Rossi, Andrea Manfrin, Matthias P Lutolf. Progress and potential in organoid research. Nat Rev Genet. 2018 Nov;19(11):671-687.
[10]. Maarten H Geurts, Jelte van der Vaart, Hans Clevers, et al. The Organoid Platform: Promises and Challenges as Tools in the Fight against COVID-19. Stem Cell Reports. 2021 Mar 9;16(3):412-418 .
[11]. Xiaolei Yin, Benjamin E Mead, Jeffrey M Karp, Oren Levy, et al. Engineering organoids. Cell Stem Cell. 2016 Jan 7;18(1):25-38.
0 notes
Text
Adenohypophysis = anterior pituitary.
Neurohypophysis = posterior pituitary.
0 notes
Photo
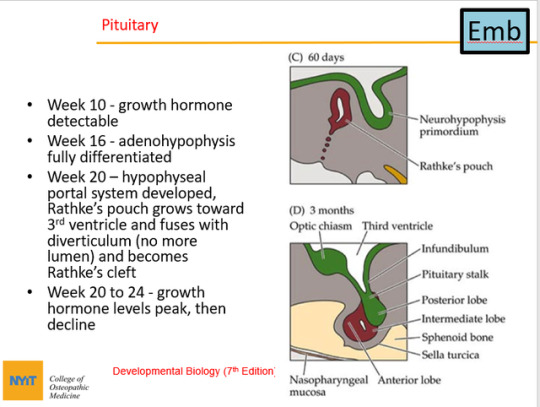
So basically, the pituitary gland forms from neural ectoderm (neurohypophysis), which descends from the brain to the roof of the mouth, and surface ectoderm (adenohypophysis), which comes from the roof of the mouth and moves superiorly. They fuse. So there are 2 cell types that make up the pituitary gland. Rathke’s pouch is the surface ectodeum of the stomodeum (mouth) that folds in.
Wikipedia:
In embryogenesis, Rathke’s pouch is an evagination at the roof of the developing mouth in front of the buccopharyngeal membrane. It gives rise to the anterior pituitary (adenohypophysis), a part of the endocrine system.
Rathke’s pouch, and therefore the anterior pituitary, is derived from ectoderm.
The pouch eventually loses its connection with the pharynx giving rise to the anterior pituitary. The anterior wall of Rathke’s pouch proliferates, filling most of the pouch to form pars distalis and pars tuberalis. The posterior wall forms pars intermedia.
1 note
·
View note