#can elevated liver enzymes be cancer
Text
“I’m exhausted, nauseous and hurting”
- @texasred43
@texasred43 is back in the hospital because she has been nauseous for days and days. She can’t keep any food down due to the symptoms of her pancreatic cancer. And her liver enzymes are elevated, which indicates she may need another stent because the tumor is growing.
I’ll keep the Tumblrverse and the #tribe updated as best I can. Please keep her in your prayers. And if you can, please contribute to her GoFundMe to help her pay for these ongoing and ever-growing medical expenses.
https://gofund.me/4d810a58
41 notes
·
View notes
Text
There are multiple risk factors for the development of osteoporosis. These include but are not limited to advanced age, cigarette smoking, chronic glucocorticoid therapy, low body weight, previous fractures, history of rheumatoid arthritis, and excessive alcohol intake.
Antiepileptic drugs (AEDs) are associated with adverse effects on bone health. The AEDs most commonly associated with altered bone metabolism are those that induce the cytochrome P450 enzyme system. Specifically, the AED phenytoin has a direct inhibitory effect on intestinal calcium absorption and can stimulate osteoclastic bone resorption.
A score of less than -2.5 on DEXA scanning would indicate osteoporosis, a score of -1.0 to -2.5 would indicate osteopenia, and a score greater than -1.0 indicates normal bone density. Additionally, a fragility fracture (fracture from minor trauma such as a fall from a standing height or less) is diagnostic of osteoporosis without any further workup.
Bottom Line: The risk factors for osteoporosis include advanced age, cigarette smoking, chronic glucocorticoid therapy, physical inactivity, poor intake of calcium and vitamin D, body weight less than 127 lb, previous fractures, anticonvulsant use, hyperthyroidism, celiac disease, rheumatoid arthritis, and excessive alcohol intake.
The characteristic need for the child to use his hands to push himself to an upright position when arising from the floor is the Gower sign. It results from weakness in the proximal lower extremity muscles. Physical examination reveals pseudohypertrophy of the calf, lumbar lordosis, a waddling gait, shortening of the Achilles tendons, hypotonia, and hyporeflexia or areflexia. Patients usually use wheelchairs by age 12 or 13. Additional complications include delayed growth, dilated cardiomyopathy, increased fractures, progressive scoliosis with impaired pulmonary function, cognitive impairment, and eventual respiratory insufficiency.
Bottom Line: Elevated laboratory markers in the setting of Duchenne muscular dystrophy include serum creatine kinase, aspartate aminotransferase, and alanine transaminase.
COMBANK Insight: DMD is a progressive, myopathic disorder inherited in an X-linked, recessive fashion and caused by a defective gene on the X chromosome responsible for dystrophin production. Dystrophin normally serves to stabilize and prevent the breakdown of muscle fibers. Loss of dystrophin thus leads to muscle fiber degeneration, resulting in muscle weakness.
Wilson Disease, also known as hepatolenticular degeneration, is an autosomal recessive defect involving an ATPase, Cu2+ -transporting, β-polypeptide. In this disease state, copper is deposited in tissues of the brain, liver, kidneys, and Descemet membrane of the cornea (known as Kayser-Fleischer rings, which are seen in the exhibit). Parkinsonian-like tremor and dementia may be evident when the nervous system is affected. Renal tubular damage occurs in the kidneys and cirrhosis can develop in the liver. Diagnosis can be made with the observation of decreased serum ceruloplasmin. Treatment includes penicillamine, which creates a soluble complex with the metal that can be excreted through the urine.
Bottom Line: A Kayser-Fleischer ring is a golden brown ring observed in the Descemet layer of the cornea as a result of copper deposition and is seen in Wilson disease. Labs reveal low serum ceruloplasmin and treatment with penicillamine can stop the progression of this degenerative disease state.
The types of cancers that metastasize to the bone most commonly are lung, breast, thyroid, renal, and prostate. Multiple myeloma and lymphoma can both form lytic lesions from their origins within the marrow.
A SPEP and UPEP are sensitive for multiple myeloma and should be obtained along with a measurement of the patient's total protein and globulin levels.
Bottom Line: The initial workup of a new lytic lesion generally involves a CT chest/abdomen/pelvis, SPEP/UPEP, bone scan, basic labs, and mammogram or PSA
#osteoporosis#Duchenne muscular dystrophy#muscular dystrophy#Wilsons disease#multiple myeloma#cancer
3 notes
·
View notes
Text
Generic Arimidex
Arimidex is a brand name for anastrozole, a medication primarily used to treat breast cancer in postmenopausal women. It is a type of drug called an aromatase inhibitor, which works by reducing estrogen levels in the body. Since many breast cancers are estrogen-sensitive, lowering estrogen can help slow or stop the growth of these cancers. Here is a detailed breakdown of the generic drug anastrozole (Arimidex):
Mechanism of Action
Anastrozole works by inhibiting the enzyme aromatase, which is responsible for converting androgens (male hormones) into estrogens (female hormones) in the body. Since many breast cancers grow in response to estrogen, reducing the amount of estrogen in the body can help shrink or slow the growth of the tumor.
Uses
Breast Cancer Treatment: Mainly used for treating hormone receptor-positive breast cancer in postmenopausal women.
Prevention of Cancer Recurrence: Helps reduce the risk of breast cancer recurrence after surgery.
Occasional Off-Label Uses: May sometimes be prescribed for ovarian cancer or as part of treatment for infertility in some cases.
Side Effects
Common side effects of anastrozole include:
Hot flashes
Joint pain (arthralgia)
Osteoporosis: As estrogen helps maintain bone density, its reduction can increase the risk of bone thinning and fractures.
Fatigue
Nausea
Mood changes or depression
Increased cholesterol levels
Less common but serious side effects:
Heart disease or cardiovascular issues: Some studies have shown an increased risk of heart disease, particularly in women with pre-existing risk factors.
Liver function issues: In rare cases, anastrozole can cause liver enzyme elevations.
Severe allergic reactions: Rash, hives, and swelling (rare).
Contraindications
Pre-menopausal women: Not recommended for women who have not yet gone through menopause.
Pregnancy and Breastfeeding: Anastrozole can harm a developing fetus and is not recommended during pregnancy or while breastfeeding.
Severe liver or kidney disease: Requires caution in patients with significant liver or kidney impairment.
0 notes
Text
Essential Basic Health Check-Up Tests in Bhubaneswar for Early Detection and Prevention
Taking care of our health is no longer a luxury—it's a necessity. With the hustle and bustle of modern life, people often neglect their health until a serious issue arises. This is where the concept of a basic health check-up becomes crucial. Early detection and prevention are the keys to maintaining a healthy lifestyle, and in Bhubaneswar, several health check-up packages are available to help you stay ahead of potential health risks. These tests are simple, non-invasive, and designed to give you an accurate picture of your overall health.
If you're looking for basic health check-up packages in Bhubaneswar, this blog will guide you through the essential tests you should consider for early detection and prevention. We will also cover convenient options for those in Odisha who prefer health check-ups at home.
Why Basic Health Check-Ups Are Essential
Many serious health conditions, such as heart disease, diabetes, and certain cancers, develop without noticeable symptoms in the early stages. By the time you feel unwell, the condition may have already progressed. Regular health check-ups can catch these issues before they become severe, giving you time to take action and improve your health. Prevention is better than cure, and a basic health check-up test in Bhubaneswar can help you identify any early warning signs of illness.
Essential Basic Health Check-Up Tests
Here are some essential tests included in a basic health check-up package that focus on early detection and prevention:
1. Complete Blood Count (CBC)
A CBC is one of the most common tests included in any basic health check-up test in Bhubaneswar. It gives a detailed overview of the different types of cells in your blood—red blood cells, white blood cells, and platelets. Abnormal levels can indicate infections, anemia, immune system disorders, and other health conditions.
2. Blood Sugar Test
Monitoring your blood sugar levels is crucial, especially for detecting diabetes early. A fasting blood sugar test checks your glucose levels after not eating for several hours. This test can help detect prediabetes and diabetes, enabling early intervention to manage the condition effectively.
3. Lipid Profile
A lipid profile measures your cholesterol levels, including LDL (bad cholesterol), HDL (good cholesterol), and triglycerides. High cholesterol is a significant risk factor for heart disease, which is why this test is essential for anyone interested in preventing cardiovascular issues.
4. Thyroid Function Test
Thyroid health is often overlooked but plays a critical role in regulating metabolism, energy, and mood. Many health check-up packages in Bhubaneswar include a thyroid test package in Odisha, which assesses your T3, T4, and TSH hormone levels. This test can detect conditions such as hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid), both of which require medical intervention.
5. Liver Function Test (LFT)
Liver health is crucial for detoxifying your body and metabolizing nutrients. An LFT checks for enzymes and proteins in your blood that indicate how well your liver is functioning. Elevated levels can point to liver disease, fatty liver, or the effects of medications.
6. Kidney Function Test
Your kidneys filter waste from your blood and regulate various essential functions, including electrolyte balance and blood pressure. A kidney function test measures the levels of urea, creatinine, and other waste products in your blood to assess kidney health.
7. Electrocardiogram (ECG)
For those at risk of heart disease or with a family history of heart problems, an ECG is a non-invasive test that records the electrical activity of the heart. It can detect abnormalities in heart rhythm, which could be a sign of heart conditions.
8. Urine Routine Test
A simple urine test can provide valuable insights into your body's metabolic and kidney functions. It can detect infections, diabetes, dehydration, and other metabolic disorders.
9. Vitamin Deficiency Tests
Many people suffer from undiagnosed vitamin deficiencies, especially in essential nutrients like Vitamin D and B12. These deficiencies can lead to fatigue, mood disorders, and other health issues. Checking for vitamin deficiencies as part of your health check-up test packages in Odisha ensures that you are not missing out on any essential nutrients.
Choosing the Right Health Check-Up Package
With so many basic health check-up packages in Bhubaneswar, how do you choose the one that’s right for you? Here are some factors to consider:
1. Your Age and Risk Factors
If you're young and healthy, a basic package that covers the CBC, lipid profile, and blood sugar might suffice. However, if you're older or have a family history of certain conditions, you might want to opt for a more comprehensive package that includes tests for heart health, liver function, and thyroid health.
2. Customizable Packages
Some healthcare providers offer customizable health check-up packages. This means you can choose tests based on your personal health needs. For example, if you're particularly concerned about thyroid issues, you could add a thyroid test package in Odisha to your check-up plan.
3. Convenience
In today's world, convenience is key. Many healthcare centers offer health test packages at home in Odisha. This means that you can get all the essential tests done without leaving the comfort of your home. This is especially beneficial for individuals who have busy schedules or find it difficult to visit a healthcare facility.
4. Price and Value
While it might be tempting to opt for the most affordable package, it's essential to consider the value you're getting. A slightly more expensive package that includes critical tests like the thyroid test package in Odisha might be more beneficial in the long run.
Benefits of Health Check-Ups at Home
One of the most convenient options now available in Odisha is health test packages at home. This service allows healthcare professionals to visit your home, collect samples, and provide you with results without the hassle of visiting a clinic or hospital. Here are the main benefits:
Convenience: No need to travel or wait in lines at a diagnostic center. You can book a time that suits you.
Comfort: For elderly patients or those with mobility issues, getting tested at home is much more comfortable and stress-free.
Accuracy: Even at home, trained professionals collect samples with the same precision and hygiene standards as they would in a clinic.
Comprehensive Packages: Many service providers offer a wide range of tests, from basic CBCs to more specialized tests like thyroid or kidney function assessments.
At Diagnostic Point, for example, they offer health check-up test packages in Odisha that can be customized to include essential screenings, all performed at home by a team of experts.
When Should You Get a Basic Health Check-Up?
If you haven't had a check-up in the past year, now is the time to consider one. The frequency of health check-ups depends on your age, lifestyle, and medical history. Here are some general guidelines:
For young adults (18-39 years): A basic health check-up every 1-2 years is advisable. If you have risk factors such as smoking, obesity, or a family history of diabetes, you may want to consider more frequent check-ups.
For middle-aged adults (40-60 years): You should have a health check-up every year, especially to monitor cholesterol, blood sugar, and heart health.
For older adults (60+ years): An annual health check-up becomes even more important as the risk for chronic conditions increases with age.
Conclusion
Early detection and prevention are key components of maintaining a healthy lifestyle. By opting for a basic health check-up package in Bhubaneswar, you're taking a proactive step toward managing your health and preventing serious conditions from developing. Whether you visit a clinic or prefer the convenience of health test packages at home in Odisha, regular check-ups can make a significant difference in your long-term well-being.
Diagnostic Point offers a range of customizable health check-up test packages in Odisha, designed to meet the needs of every individual. Book your check-up today and invest in your future health.
#health test package at home in odisha#health check up test packages odisha#basic health check up test in bhuvneshwar#basic health check up packages bhuvneshwar
0 notes
Text
SGOT and SGPT: Indicators of Liver Health
By: Mrs Mayuri Mathur
Liver function tests, such as SGOT (serum glutamic oxaloacetic transaminase) and SGPT (serum glutamic pyruvic transaminase), play a crucial role in assessing liver health. Elevated levels of SGOT and SGPT can indicate liver damage or disease, making it essential to understand these markers and their implications for overall health.
Introduction
Liver function tests are blood examinations used to identify the underlying cause of symptoms and monitor liver health or damage. They assess the levels of specific enzymes and proteins in the bloodstream.
Some tests evaluate the liver's ability to perform its normal functions, such as producing proteins and eliminating bilirubin, a waste product found in blood. Other tests measure enzymes released by liver cells in response to injury or illness.

Liver function tests include:
Alanine transaminase (ALT) and aspartate transaminase (AST) are enzymes found in the liver that indicate liver cell damage when elevated.
Alkaline phosphatase (ALP) levels may rise due to liver damage or bone disease.
Albumin and total protein levels assess liver protein synthesis; low levels indicate liver disease or other conditions.
Bilirubin levels indicate liver function and may rise due to liver disease or bile duct blockage.
Gamma-glutamyltransferase (GGT) levels indicate liver or bile duct damage, while L-lactate dehydrogenase (LD) levels rise with liver damage.
Prothrombin time (PT) assesses blood clotting ability, often prolonged in liver disease or due to certain medications.
What are SGOT and SGPT?
SGOT (AST - Aspartate Aminotransferase) and SGPT (ALT - Alanine Aminotransferase)are important indicators of liver function. These enzymes are found in various tissues throughout the body, with the highest concentrations in the liver. When liver cells are damaged or destroyed, these enzymes are released into the bloodstream, causing their levels to rise in blood tests. The elevated levels of these enzymes may be indicative of:
Liver Diseases: Conditions like hepatitis (viral or alcoholic), cirrhosis, fatty liver disease, and liver cancer can cause elevated SGOT and SGPT levels.
Alcohol Consumption: Excessive alcohol intake can lead to liver inflammation and damage, increasing SGOT and SGPT levels.
Medications: Some medications, such as certain antibiotics, cholesterol-lowering drugs, and pain relievers, can elevate liver enzymes.
Obesity and Metabolic Syndrome: Conditions associated with insulin resistance, like obesity and metabolic syndrome, can lead to non-alcoholic fatty liver disease (NAFLD), elevating liver enzymes.
Liver Damage Progression: Persistently elevated SGOT and SGPT levels may indicate ongoing liver damage, potentially progressing to more severe conditions like cirrhosis or liver failure.
Cardiovascular Risk: Elevated SGOT levels have been linked to an increased risk of cardiovascular events, indicating broader health implications beyond liver health.
Dangerous Levels of SGOT and SGPT
An SGOT to SGPT ratio exceeding 2 strongly suggests the presence of alcoholic hepatitis and cirrhosis. The ratio of SGOT to SGPT shows a significant increase in patients diagnosed with alcoholic hepatitis and cirrhosis (2.85 +/- 0.2) compared to those with postnecrotic cirrhosis (1.74 +/- 0.2), chronic hepatitis (1.3 +/- 0.17), obstructive jaundice (0.81 +/- 0.06), and viral hepatitis (0.74 +/- 0.07).
Regular monitoring of SGOT and SGPT levels is crucial for early detection and management of liver diseases. Elevated levels can indicate ongoing liver damage, prompting further investigation and treatment to prevent complications.
Educational and Healthcare Interventions:
Educational and healthcare interventions for managing SGOT (AST) and SGPT (ALT) levels focus on promoting liver health through education, lifestyle changes, and medical management. Here's a comprehensive approach:
Education on Liver Function: It is crucial to understand the roles of SGOT and SGPT in liver function. Educate patients on how these enzymes reflect liver health and why monitoring their levels is essential.
Healthy Lifestyle Guidance: Provide dietary recommendations emphasizing a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limit saturated fats, sugars, and processed foods. Encourage portion control and regular meal times.
Medication Review: Review medications and supplements to identify any that may affect liver function. Adjust or monitor dosages as necessary under medical supervision.
Screening and Monitoring: Establish protocols for regular liver function tests to monitor SGOT and SGPT levels. This allows early detection of liver abnormalities and timely intervention.
Treatment of Underlying Conditions: Address underlying conditions such as viral hepatitis, fatty liver disease, or autoimmune disorders promptly. Tailor treatment plans to manage these conditions effectively.
Health Promotion: Promote overall health and well-being through stress management techniques, adequate hydration, and regular physical activity. These practices support liver function and overall health.
Patient Empowerment: Empower patients with knowledge and resources to take an active role in managing their liver health. Provide educational materials, support groups, and access to healthcare professionals for ongoing guidance.
Collaborative Care Approach: Foster collaboration between healthcare providers, specialists, dietitians, and mental health professionals to offer comprehensive care. This approach ensures holistic management of SGOT and SGPT levels.
Lifestyle Tips for Managing SGOT and SGPT Levels:
Healthy Diet: Consume a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Limit saturated fats, sugars, and processed foods. Drink plenty of water to help flush toxins from your body and support overall liver function.
Limit Alcohol: Excessive alcohol consumption can elevate SGOT and SGPT levels. If you drink, do so in moderation or avoid alcohol altogether.
Weight Management: Maintain a healthy weight through regular exercise and a balanced diet. Obesity can contribute to fatty liver disease, leading to elevated liver enzymes.
Medication Management: Some medications can increase SGOT and SGPT levels. Always take medicines as prescribed and inform your healthcare provider of any ongoing supplements or over-the-counter drugs.
Avoid Toxins: Minimize exposure to environmental toxins and chemicals that can harm the liver. Use protective gear if working with chemicals.
Monitor health Regularly: Regular check-ups with your healthcare provider can help monitor liver function. Discuss any concerns about SGOT and SGPT levels and follow recommended screening guidelines.
Healthy Habits: Quit smoking if you smoke, as it can worsen liver health. Stress-reduction techniques like yoga or meditation can be incorporated to manage stress, which can impact liver function.
Follow Medical Advice: Follow your healthcare provider's recommendations for managing SGOT and SGPT levels, including any necessary medications, lifestyle changes, or dietary adjustments.
Conclusion
Understanding the significance of liver function tests encourages proactive healthcare behaviors. Medical and healthcare education and disease awareness empower individuals to make informed decisions about their health and promotes early detection of liver disorders, facilitates prompt intervention, and ultimately improves outcomes by preventing complications associated with liver disease.
Adopting proactive and preventive strategies can help manage and prevent elevated SGOT and SGPT levels, promoting better liver health and overall well-being. Always consult your healthcare provider for personalized advice based on your specific health needs.
0 notes
Text
Pazopanib HCL: A Powerful Tyrosine Kinase Inhibitor for Cancer Treatment
Pazopanib HCL is a cutting-edge medication used in the treatment of advanced renal cell carcinoma (RCC) and soft tissue sarcoma. As a tyrosine kinase inhibitor, it plays a crucial role in managing these challenging cancers by targeting the mechanisms that enable tumor growth and spread.
What is Pazopanib HCL?
Pazopanib HCL is an effective tyrosine kinase inhibitor that helps manage advanced renal cell carcinoma and soft tissue sarcoma. This medication works by inhibiting key tyrosine kinases involved in cancer progression, thus hindering tumor growth and metastasis.
Buy Pazopanib HCL to access this powerful treatment option and take a step towards managing your cancer effectively.
Mechanism of Action
Pazopanib HCL works by blocking multiple tyrosine kinases, including:
Vascular Endothelial Growth Factor Receptors (VEGFRs)
Platelet-Derived Growth Factor Receptors (PDGFRs)
Fibroblast Growth Factor Receptors (FGFRs)
By inhibiting these receptors, pazopanib disrupts angiogenesis, the process through which tumors develop their blood supply. This disruption reduces the growth and spread of tumors, leading to decreased tumor vascularity and increased necrosis.
Benefits and Advantages
Here’s why buying pazopanib HCL could be a valuable choice for managing advanced RCC and soft tissue sarcoma:
Broad-Spectrum Inhibition: Pazopanib targets multiple pathways involved in tumor growth and angiogenesis, offering a comprehensive approach to cancer treatment.
Convenient Oral Administration: Its oral formulation makes it easy to take, improving patient compliance and convenience.
Effective Symptom Management: By slowing cancer progression and reducing tumor size, pazopanib helps improve patients' quality of life and potentially extends survival.
Side Effects and Risks
While pazopanib is effective, it can cause side effects that need monitoring:
Hypertension: Elevated blood pressure may occur, requiring careful management to avoid cardiovascular issues.
Hepatotoxicity: Liver toxicity, indicated by elevated liver enzymes, may necessitate regular monitoring of liver function.
Cardiac Toxicity: Potential cardiac side effects include QT interval prolongation, arrhythmias, and heart failure, particularly in those with preexisting cardiovascular conditions.
Gastrointestinal Issues: Pazopanib may cause diarrhea, nausea, and vomiting, which might require supportive care or dose adjustments.
About MedicaPharma
MedicaPharma is a leading distributor of high-quality active pharmaceutical ingredients (APIs), providing products to hospitals, pharmacies, research institutes, and universities worldwide. When you buy pazopanib HCL from us, you are choosing a supplier committed to excellence in pharmaceutical quality and safety.
Why Choose MedicaPharma?
At MedicaPharma, we pride ourselves on supplying GMP-certified products with logistics that comply with GDP regulations. This ensures that when you buy pazopanib HCL, you receive a product of the highest standard, supporting your treatment journey effectively.
Request a Quote Today
If you’re interested in buying pazopanib HCL, contact us for a quote and more information about how our high-quality products can meet your needs. Let MedicaPharma assist you in accessing this essential medication for managing advanced renal cell carcinoma and soft tissue sarcoma.
Choose MedicaPharma for reliable, high-quality pharmaceutical solutions and take control of your cancer treatment with confidence.
0 notes
Text
Retevmo: Uses, Dosage, Side Effects, Warnings
Retevmo, with its active component selpercatinib, is designed to treat adults who suffer from specific cancer conditions. These include locally advanced or metastatic non-small cell lung cancer (NSCLC) with a RET gene fusion, and locally advanced or metastatic solid tumors with a RET gene fusion. It also targets advanced or metastatic medullary thyroid cancer (MTC) with a RET mutation. The drug operates by inhibiting kinase activity, which is crucial in halting the progression of cancer cells. Additionally, Retevmo is approved for pediatric patients aged 12 and older who have advanced medullary thyroid cancer. In India, Retevmo cost in India is available at a relatively low cost and can be purchased with a valid prescription from numerous suppliers. Indian Pharma Network, known for distributing reliable generic medicines, is one of the prominent distributors of Retevmo.

rearrangement (in NSCLC or thyroid cancers). The retevmo dosage is tailored according to the patient's body weight, which is assessed before starting the treatment. Patients who weigh less than 50 kg are advised to take 120 mg, whereas those who weigh 50 kg or more should take 160 mg. This medication must be prescribed by a healthcare professional, and the treatment should be closely monitored by a qualified medical expert to ensure its effectiveness and safety.Retevmo contains the active ingredient selpercatinib, and its prescription is based on identifying a specific RET gene mutation (in the case of MTC) or a transfection gene
Retevmo capsules should be administered orally twice daily, approximately every 12 hours, and continued until there is either disease progression or severe toxicity. The medication can be taken with or without food, except when used with a proton pump inhibitor. It's important that the capsules are swallowed whole, without crushing or chewing them. If a dose is missed, it should be taken at least six hours after the previous dose. Proper adherence to these guidelines ensures the medication's efficacy and safety.
Selpercatinib, the active ingredient in Retevmo, is a potent RET inhibitor and belongs to the tyrosine kinase inhibitor class of cancer therapies. Retevmo 80 mg hard gelatin capsules are available for oral use. It effectively blocks the activity of abnormal proteins that are produced due to mutations in the RET gene. These proteins can cause uncontrolled cell growth and division, leading to tumor development. By inhibiting these proteins, selpercatinib reduces the growth and spread of cancer cells. Its affordability and efficacy make selpercatinib accessible to patients, offering a critical option for those battling specific types of cancer driven by RET gene mutations.
Although Retevmo is an effective cancer treatment, it can cause a range of retevmo side effects, from mild to severe. Common side effects include loss of appetite, headache, dizziness, prolonged QT interval, high blood pressure, abdominal pain, diarrhea, nausea, vomiting, constipation, dry mouth, rash, fever, fatigue, edema, and bleeding. Blood tests may show changes in liver enzymes, decreased platelet and white blood cell counts, decreased magnesium levels, and increased creatinine levels. About one in ten patients experience these side effects. The most frequently reported major adverse effects are stomach pain, hypersensitivity, diarrhea, and elevated liver enzymes, which indicate liver stress.
#retevmo 40 mg capsule price in india#buy retevmo 40 mg capsule#retevmo in india#retevmo importer in noida#buy retevmo capsules online
0 notes
Text
Unraveling the Complexity: Exploring Pancreatic and Biliary Diseases
Introduction:
The pancreas and biliary system are integral components of the digestive system, playing crucial roles in digestion, nutrient absorption, and waste elimination. However, diseases affecting these organs can lead to significant morbidity and mortality if left untreated. In this blog, we will delve into the intricacies of pancreatic and biliary diseases, their causes, symptoms, diagnosis, and treatment modalities.
Pancreatitis:
Pancreatitis, inflammation of the pancreas, can be acute or chronic and is often triggered by factors such as gallstones, alcohol consumption, medications, or genetic predisposition. Acute pancreatitis manifests with sudden onset severe abdominal pain, nausea, vomiting, and elevated pancreatic enzymes. Chronic pancreatitis is characterized by recurrent episodes of abdominal pain, weight loss, and pancreatic insufficiency. Diagnosis involves clinical evaluation, imaging studies such as CT scans, and laboratory tests. Treatment aims to relieve symptoms, prevent complications, and address underlying causes through pain management, dietary modifications, enzyme replacement therapy, and, in severe cases, surgery.
Gallstone Disease:
Gallstone disease, one of the most common biliary disorders, occurs when gallstones form in the gallbladder or bile ducts. These stones can obstruct the flow of bile, leading to symptoms such as abdominal pain (biliary colic), nausea, vomiting, and jaundice. Diagnosis is typically made through imaging studies such as ultrasound or CT scans. Treatment options include lifestyle modifications, medications to dissolve stones, and surgical removal of the gallbladder (cholecystectomy) in symptomatic cases.
Biliary Obstruction:
Biliary obstruction occurs when the flow of bile from the liver to the small intestine is impaired, leading to jaundice, dark urine, pale stools, abdominal pain, and itching. Common causes of biliary obstruction include gallstones, tumors (benign or malignant), strictures, or inflammation of the bile ducts. Diagnosis involves imaging studies such as MRCP (magnetic resonance cholangiopancreatography) or ERCP (endoscopic retrograde cholangiopancreatography) to visualize the biliary tract. Treatment depends on the underlying cause and may include endoscopic interventions, surgical procedures, or palliative measures to relieve symptoms.
Pancreatic Cancer:
Pancreatic cancer is a highly aggressive malignancy with a poor prognosis, often diagnosed at an advanced stage due to nonspecific symptoms and lack of effective screening tools. Common symptoms include abdominal pain, jaundice, weight loss, and new-onset diabetes. Diagnosis involves imaging studies such as CT scans, MRI, and endoscopic ultrasound (EUS), followed by tissue biopsy for confirmation. Treatment options may include surgery, chemotherapy, radiation therapy, and targeted therapies, depending on the stage and extent of the disease.
Pancreatic and biliary diseases encompass a range of conditions affecting the pancreas and the biliary system, including the gallbladder, bile ducts, and associated structures. These diseases can be complex and challenging to diagnose and manage due to their often nonspecific symptoms and potential for severe complications.
Pancreatic Diseases
Acute Pancreatitis:
Definition: A sudden inflammation of the pancreas that can be mild or life-threatening.
Causes: Gallstones, chronic alcohol use, certain medications, and high triglyceride levels.
Symptoms: Severe abdominal pain, nausea, vomiting, fever, and a swollen abdomen.
Diagnosis: Elevated serum amylase and lipase levels, abdominal ultrasound, CT scan.
Treatment: Hospitalization for fasting, IV fluids, pain management, and treating the underlying cause (MDLinx) (MGMA Homepage).
Chronic Pancreatitis:
Definition: Long-term inflammation of the pancreas that leads to permanent damage.
Causes: Chronic alcohol consumption, genetic predisposition, and autoimmune conditions.
Symptoms: Chronic abdominal pain, malabsorption, weight loss, and diabetes.
Diagnosis: Imaging studies (CT, MRI), pancreatic function tests, and endoscopic ultrasound.
Treatment: Pain management, enzyme supplements, dietary changes, and addressing complications like diabetes (MDLinx) (MGMA Homepage).
Pancreatic Cancer:
Definition: Malignant tumor of the pancreas, often with poor prognosis.
Symptoms: Jaundice, weight loss, diabetes, and upper abdominal pain.
Diagnosis: Imaging (CT, MRI, endoscopic ultrasound), biopsy, and blood tests (CA 19-9).
Treatment: Surgery (Whipple procedure), chemotherapy, radiation therapy, and palliative care (MDLinx) (MGMA Homepage).
Biliary Diseases
Cholelithiasis (Gallstones):
Definition: Formation of stones within the gallbladder.
Symptoms: Often asymptomatic; can cause biliary colic, nausea, and vomiting if stones block ducts.
Diagnosis: Ultrasound, CT scan, and sometimes MRCP (magnetic resonance cholangiopancreatography).
Treatment: Dietary changes, pain management, and possibly cholecystectomy (surgical removal of the gallbladder) (MDLinx) (MGMA Homepage).
Cholecystitis:
Definition: Inflammation of the gallbladder, often due to gallstones blocking the cystic duct.
Symptoms: Severe right upper abdominal pain, fever, nausea, and vomiting.
Diagnosis: Ultrasound, HIDA scan, and blood tests showing elevated white blood cells.
Treatment: Hospitalization, antibiotics, fasting, IV fluids, and cholecystectomy (MDLinx) (MGMA Homepage).
Choledocholithiasis:
Definition: Presence of gallstones in the common bile duct.
Symptoms: Jaundice, dark urine, pale stools, and biliary colic.
Diagnosis: MRCP, ERCP (endoscopic retrograde cholangiopancreatography), and ultrasound.
Treatment: ERCP to remove stones, and possibly cholecystectomy to prevent recurrence (MDLinx) (MGMA Homepage).
Primary Sclerosing Cholangitis (PSC):
Definition: Chronic disease causing inflammation and scarring of the bile ducts.
Symptoms: Jaundice, itching, fatigue, and episodes of cholangitis.
Diagnosis: MRCP, ERCP, liver biopsy, and blood tests showing elevated liver enzymes.
Treatment: Symptom management, bile acid therapy, and eventually liver transplantation in advanced cases (MDLinx) (MGMA Homepage).
Diagnostic Techniques
Imaging: Ultrasound, CT scan, MRI, MRCP, and ERCP are crucial for visualizing the pancreas and biliary system.
Laboratory Tests: Blood tests to check liver function, pancreatic enzymes (amylase, lipase), and tumor markers (e.g., CA 19-9).
Biopsy: Fine-needle aspiration or surgical biopsy for histological examination.
Conclusion:
Understanding pancreatic and biliary diseases requires a multidisciplinary approach involving gastroenterologists, radiologists, and surgeons. Timely diagnosis and appropriate treatment are crucial to manage these conditions effectively and prevent complications.
For further reading and detailed information, you can explore the following resources:
MDLinx on Gastroenterology
Gastroenterology & Hepatology Journal
Medical Group Management Association (MGMA)
Pancreatic and biliary diseases pose significant challenges in clinical practice, requiring a multidisciplinary approach for effective management. Early recognition of symptoms, timely diagnosis, and appropriate treatment interventions are essential for improving outcomes and quality of life for patients affected by these conditions. Through ongoing research, advances in diagnostic techniques, and therapeutic innovations, healthcare providers continue to strive towards better understanding, prevention, and treatment of pancreatic and biliary diseases, offering hope to patients and their families facing these complex challenges.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference
Short Name: 14GHUCG2024
Dates: December 17-19, 2024
Venue: Dubai, UAE
Email: [email protected]
Visit: https://gastroenterology.universeconferences.com/
Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/
Register here: https://gastroenterology.universeconferences.com/registration/
Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/
Call Us: +12073070027
WhatsApp Us: +442033222718

0 notes
Text
Understanding Your Liver Health: SGOT & SGPT Tests at PACE Hospitals
Your liver is a vital organ responsible for filtering toxins from your blood,
producing proteins, and regulating numerous bodily functions. Regular monitoring of your liver health is crucial for early detection and management of potential problems. At PACE Hospitals, we offer SGOT & SGPT Test in Hyderabad as a key part of our comprehensive liver function assessment.
What are SGOT & SGPT Tests?
SGOT (Serum Glutamic-Oxaloacetic Transaminase): Also known as AST (Aspartate Aminotransferase), SGOT is an enzyme found in various tissues throughout the body, including the liver, heart, muscles, and kidneys.
SGPT (Serum Glutamate Pyruvate Transaminase): Also known as ALT (Alanine Aminotransferase), SGPT is an enzyme primarily found in the liver.
These tests measure the level of these enzymes in your blood. When liver cells are damaged or inflamed, SGOT and SGPT leak into the bloodstream, causing elevated levels in the test results.
Why are SGOT & SGPT Tests Important?
Elevated SGOT or SGPT levels can be an indicator of various liver conditions, including:
Hepatitis (viral infection of the liver)
Fatty liver disease
Cirrhosis (scarring of the liver)
Liver cancer
Early detection of liver problems is crucial for effective treatment and management. These tests can also help assess the severity of existing liver disease and monitor the effectiveness of treatment.
What to Expect During the Test:
A simple blood draw is performed by a qualified healthcare professional at PACE Hospitals.
No special preparation is typically required.
The results are usually available within a few days.
What to Do After the Test:
Your doctor at PACE Hospitals will discuss the results with you and explain their significance.
If your SGOT or SGPT levels are elevated, further tests may be needed to determine the underlying cause.
Your doctor will recommend the most appropriate course of treatment based on the diagnosis.
Benefits of Getting Tested at PACE Hospitals:
Experienced Doctors: Our team of qualified gastroenterologists and hepatologists are experts in diagnosing and treating liver diseases.
Advanced Technology: We utilize advanced laboratory equipment for accurate and timely test results.
Holistic Care: We focus on providing comprehensive care plans that address your individual needs.
Maintaining Healthy Liver Function:
Practice a healthy lifestyle with a balanced diet and regular exercise.
Maintain a healthy weight.
Limit alcohol consumption.
Avoid smoking.
Get vaccinated against hepatitis A and B.
Early detection and intervention are key to managing liver health. Schedule an appointment at PACE Hospitals today to discuss your liver health and get SGOT & SGPT tests if recommended by your doctor.
0 notes
Text
#Celiac Disease! What is it?
Celiac disease is an autoimmune disorder triggered by gluten ingestion. It results in damage to the intestinal lining and causes symptoms such as diarrhea, fatigue, weight loss, bloating, and anemia. Here are some key points about Celiac disease:
Symptoms:
Digestive symptoms (for adults) may include:
Diarrhea
Bloating
Abdominal pain
Constipation
Weight loss
Other symptoms (both adults and children) can include:
Anemia (due to decreased iron absorption)
Loss of bone density (osteoporosis) or softening of bones (osteomalacia)
Itchy, blistery skin rash (dermatitis herpetiformis)
Headaches, fatigue, mood changes
Nervous system problems (numbness, tingling, balance issues)
Joint pain
Reduced spleen function (hyposplenism)
Elevated liver enzymes
Causes:
Celiac disease is an autoimmune disorder triggered by an extreme reaction to foods containing gluten (found in wheat, barley, and rye).
Genetic factors (HLA-DQ2 or HLA-DQ8 variants) play a role.
Environmental triggers (pregnancy, surgery, viral infection) can also contribute.
Complications:
Lactose intolerance
Malnutrition
Increased risk of cancer
Neurological issues
Loss of calcium and bone density
Infertility and miscarriage
Diagnosis:
Blood tests (elevated celiac disease antibodies)
Genetic testing (HLA variants)
Intestinal biopsy
Treatment:
Strict gluten-free diet
Lactose-free diet
Multivitamins and calcium supplements
Remember to consult a healthcare provider if you experience symptoms related to Celiac diseas



For individuals with Celiac disease, adhering to a gluten-free diet is essential to manage the condition and prevent damage to the small intestine. Here are some guidelines for foods to include and avoid:
Foods to Include:
Naturally Gluten-Free Foods:
Fruits
Vegetables
Meat and poultry
Fish and seafood
Dairy
Beans, legumes, and nuts
Gluten-Free Grains and Alternatives:
Rice
Corn (maize)
Soy
Potato
Tapioca
Beans
Quinoa
Millet
Buckwheat
Arrowroot
Amaranth
Teff
Flax
Chia
Gluten-free oats
Gluten-Free Products:
Look for products labeled as ‘gluten-free’ including breads, pastas, and snacks.
Foods to Avoid:
Gluten-Containing Grains and Their Derivatives:
Wheat
Barley
Rye
Triticale
Malt
Brewer’s yeast
Processed Foods that may contain gluten unless labeled ‘gluten-free’:
Breads
Pastas
Cereals
Baked goods
Snack foods
Sauces and gravies
Beer and other malt beverages
Tips for Managing a Gluten-Free Lifestyle:
Read Food Labels Carefully: Look for ‘gluten-free’ certification or the absence of gluten-containing ingredients.
Be Aware of Cross-Contamination: Even gluten-free foods can be contaminated if processed on the same equipment as gluten-containing products.
Dining Out: Choose restaurants that offer gluten-free options and communicate your dietary needs clearly to the staff.
It’s important to consult with a healthcare provider or a dietitian specialized in Celiac disease to ensure you’re getting all the necessary nutrients while following a gluten-free diet.
0 notes
Text
Malaria presents with periodic flu-like symptoms and should be suspected in any ill patient with a history of travel from an endemic region. Diagnosis is primarily made by examining thick and thin blood smears for speciation and percent parasitemia. All malarial species produce intra-erythrocytic rings (trophozoites). Rapid antigen testing may also be available and can distinguish between P. falciparum and P. vivax. Treatment with chloroquine is standard for mild-to-moderate disease. Due to chloroquine resistance, however, artemisinin combination therapy (ACT) is commonly used. ACT options include dihydroartemisinin, artesunate, mefloquine, or artemether in combination with other antimalarials (eg, piperaquine or mefloquine).
Severe disease should be treated with intravenous artesunate. The anti-hypnozoite drug primaquine is also necessary for P. vivax and P. ovale because of their ability to cause relapse due to dormant hypnozoite forms within the liver. To prevent acute hemolysis, it is important to test for glucose-6-phosphate dehydrogenase deficiency prior to initiating primaquine. Of note, P. falciparum is known to produce fulminant disease, including hemolytic anemia, renal failure, pulmonary edema, central nervous system disease, hypoglycemia, liver failure, and lactic acidosis. Rapid treatment is therefore essential to prevent poor outcomes.
Gonorrhea is diagnosed with NAAT of a swab or culture on Thayer-Martin media. Once the samples have been obtained, the patient can be initiated on antimicrobial therapy. The standard therapy would be ceftriaxone 250 mg intramuscularly (IM) as a single dose, plus azithromycin 1 g orally (due to increasing resistance) or doxycycline 100 mg orally twice daily for 7 days.
Wilson disease results in inappropriate deposition of copper in the liver, brain, and other tissues due to impaired clearance of copper into the bile. It is an autosomal-recessive disease affecting chromosome 13. Signs and symptoms are the consequence of cirrhosis, basal ganglia deterioration, and deposition of copper in other tissues, causing hepatic failure, neurologic abnormalities, hemolytic anemia, and Kayser-Fleischer rings around the iris.
Basic labs will reveal hemolytic anemia (decreased hemoglobin and hematocrit with elevated bilirubin as well as decreased haptoglobin and increased reticulocyte count) and elevated liver enzymes due to liver inflammation and cirrhosis. Decreased ceruloplasmin (less than 20 mg/dL) and low serum copper concentration are consistent with Wilson disease and should prompt confirmatory workup, including 24-hour urine copper excretion. Low serum copper levels may seem paradoxical; however, it should be remembered that ceruloplasmin is the primary copper binding protein and is responsible for the majority of copper contained in the serum. Low ceruloplasmin results in a low total serum copper, despite the fact that total-body copper is in excess. This excess, while not measurable in the serum at a specific point in time, is measurable as increased urinary excretion over the course of the day, which is why a 24-hour urine copper is needed.
Kayser-Fleischer rings are present in 50% of patients with active liver disease but without any neurologic involvement. When neurologic symptoms present (dysarthria, dystonia, tremor, parkinsonism, choreoathetosis, ataxia, cognitive impairment), Kayser-Fleischer rings are present in 98% of patients.
Gastric cancer presents with left supraclavicular lymphadenopathy. Left supraclavicular adenopathy (known as the Virchow node) suggests an abdominal source, such as the stomach, gallbladder, or pancreas.
In any patient with an upper GI bleed, it is important to ask for recent anticoagulation use and a history of prior bleeding or endoscopy as up to 60% of recurrent GI bleeding is from the same lesion. Other important considerations in the history include: if the patient has a history of H. pylori, cirrhosis, odynophagia, or the use of antiplatelet agents.
Esophageal varices and peptic ulcers are common and easily treatable causes of bleeding in pts with cirrhosis.
Bottom Line: The most common causes of upper GI bleeding include peptic ulcer disease, severe or erosive gastritis/duodenitis/esophagitis, esophagogastric varices, portal hypertensive gastropathy, angiodysplasia, Mallory-Weiss syndrome, mass lesions (polyps/cancers).
Besides varices, other major complications of cirrhosis include ascites, spontaneous bacterial peritonitis, hepatic encephalopathy, hepatocellular carcinoma, hepatorenal syndrome, hepatopulmonary syndrome, however, in patients with acute decompensation due to upper GI bleeding, the most urgent conditions to evaluate for include the development of hepatic encephalopathy, SBP, and hepatorenal syndrome.
Bottom Line: A patient with cirrhosis and acute upper GI bleeding should have 2 large-bore IVs or a large-bore, single-lumen central catheter placed, be resuscitated with IV fluids, transfused blood as needed, started on an IV proton pump inhibitor drip, an IV octreotide drip, and IV antibiotics for SBP prophylaxis, and will generally require ICU admission. An EGD should be performed within 24 hours of admission, but ideally as soon as possible, once the patient is hemodynamically stable.
Management of critical patients with upper GI bleeding generally follows the same trajectory. Get as much history as possible to localize risk factors for bleeding and options to inform immediate pharmacologic treatment (PPI vs octreotide vs both). Give blood and fluids. Consult gastroenterology for EGD. If the patient cannot undergo EGD or this is not available or had a recent EGD with bleeding that is not amenable to further endoscopic therapy, consult IR for embolization.
Those patients found to have SBP should receive hepatorenal syndrome prophylaxis with albumin on days 1 (1.5g/kg) and 3 (1g/kg) of admission if they meet the criteria.
Multiple trials evaluating the effectiveness of prophylactic antibiotics in cirrhotic patients hospitalized for GI bleeding suggest an overall reduction in infectious complications and possibly decreased mortality. Antibiotics may also reduce the risk of recurrent bleeding in hospitalized patients who bled from esophageal varices.
Diagnose pheochromocytoma with urine metanephrine and normetanephrine levels. The most appropriate drug therapy prior to adrenalectomy for suspected pheochromocytoma consists of phenoxybenzamine followed by the addition of propranolol (if needed for heart rate control). Preoperative treatment for surgical resection of pheochromocytoma involves alpha-receptor blockade. This can be followed by beta-receptor blockade if needed for further heart rate control, usually 2 to 3 days before surgery.
7 to 14 days of phenoxybenzamine and 2 to 3 days of propranolol prior to surgery (if needed for heart rate control), with the continuation of propranolol perioperatively. The most important aspect of treatment in patients with pheochromocytoma with respect to preoperative antihypertensive therapy is alpha-receptor blockade. Alpha-receptor blockade prevents the hypertensive effect of overstimulation by the catecholamines released from the adrenal medulla. Beta-receptor blockade should follow, which prevents rebound tachycardia (goal heart rate should be 60-80/min) in the setting of unopposed alpha blockade. The clinical guidelines from the Journal of Clinical Endocrinology and Metabolism released in 2014 currently support the use of alpha-blockers for blood pressure control prior to surgery. Beta-blockers can be added afterward if needed. Of note, selective alpha-1-receptor blockers, such as prazosin or doxazosin, may be used instead of phenoxybenzamine in certain situations, such as in patients who have significant benign prostatic hyperplasia and may already be on low doses of these medications or if the patient cannot tolerate the first-line agents listed above. Metoprolol can also be administered instead of propranolol or atenolol.
There is a rule of 10's associated with pheochromocytoma: 10% are extra-adrenal, 10% are bilateral, 10% are malignant, and 10% occur in children. Some people add that 10% will recur after excision within 10 years and 10% will be found after a significant stroke. It was previously thought that about 10% were familial; however, that number has been adjusted upward as more and more genetic and familial diseases have been linked with the development of pheochromocytoma. It is now thought that about 40% of pheochromocytomas are associated with some kind of underlying genetic predisposition. Malignant pheochromocytomas are biologically and histologically indistinguishable from benign pheochromocytomas. The only way to determine malignancy is to observe local infiltrative disease or find evidence of metastatic spread. Thus, even benign pheochromocytomas found on excision will need clinical follow-up.
Most authors advocate obtaining 24-hour fractionated urine metanephrines if the clinical suspicion is low, and serum metanephrines if the clinical suspicion is high. Serum metanephrines have a decreased specificity, and positive testing may result in unnecessary imaging and follow-up, which is why it is not recommended as the first-line test for all patients.
HAs, diaphoresis, HTN = pheo
Gastrinoma (Zollinger-Ellison) - initial test that should be ordered is a fasting serum gastrin level. If elevated, it should be followed by a secretin infusion test. Somatostatin-receptor scintigraphy is the imaging test of choice as it detects for primary or metastatic lesions. Treatment includes intravenous (IV) proton pump inhibitors and surgical resection. Zollinger-Ellison syndrome is also associated with multiple endocrine neoplasia (MEN) type 1. MEN 1 is also known as Werner's syndrome and presents with the 3 Ps: parathyroid tumors; pituitary tumors, including prolactinoma; and pancreatic endocrine tumors, including insulinomas, vipomas, glucagonomas, and Zollinger-Ellison syndrome.
The initial test of choice for Zollinger-Ellison syndrome is a fasting serum gastrin (off proton pump inhibitors). The diagnosis is confirmed with a secretin infusion test. It is associated with MEN1.
2 notes
·
View notes
Text
Generic Arimidex
Arimidex is a brand name for anastrozole, a medication primarily used to treat breast cancer in postmenopausal women. It is a type of drug called an aromatase inhibitor, which works by reducing estrogen levels in the body. Since many breast cancers are estrogen-sensitive, lowering estrogen can help slow or stop the growth of these cancers. Here is a detailed breakdown of the generic drug anastrozole (Arimidex):
Mechanism of Action
Anastrozole works by inhibiting the enzyme aromatase, which is responsible for converting androgens (male hormones) into estrogens (female hormones) in the body. Since many breast cancers grow in response to estrogen, reducing the amount of estrogen in the body can help shrink or slow the growth of the tumor.
Uses
Breast Cancer Treatment: Mainly used for treating hormone receptor-positive breast cancer in postmenopausal women.
Prevention of Cancer Recurrence: Helps reduce the risk of breast cancer recurrence after surgery.
Occasional Off-Label Uses: May sometimes be prescribed for ovarian cancer or as part of treatment for infertility in some cases.
Side Effects
Common side effects of anastrozole include:
Hot flashes
Joint pain (arthralgia)
Osteoporosis: As estrogen helps maintain bone density, its reduction can increase the risk of bone thinning and fractures.
Fatigue
Nausea
Mood changes or depression
Increased cholesterol levels
Less common but serious side effects:
Heart disease or cardiovascular issues: Some studies have shown an increased risk of heart disease, particularly in women with pre-existing risk factors.
Liver function issues: In rare cases, anastrozole can cause liver enzyme elevations.
Severe allergic reactions: Rash, hives, and swelling (rare).
Contraindications
Pre-menopausal women: Not recommended for women who have not yet gone through menopause.
Pregnancy and Breastfeeding: Anastrozole can harm a developing fetus and is not recommended during pregnancy or while breastfeeding.
Severe liver or kidney disease: Requires caution in patients with significant liver or kidney impairment.
0 notes
Text
Jaundice fever — symptoms, causes, prevention, myths, diagnosis, treatments and faqs — All you need to know about jaundice
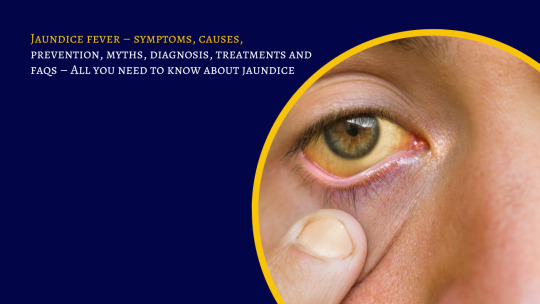
Overview
Jaundice is a medical condition where the person’s skin becomes highly yellowish and the eyes whiten and discolour due to the elevation of bilirubin in their blood. Jaundice is most common among young children but it can affect people of any age.
Bilirubin occurs when there is any kind of breakdown in the red blood cells of the human body.
If anyone is seen with pale yellow skin and Eyes or if they go through dark and yellow colour urination, it is a sure sign of Jaundice.
Jaundice occurrence is a cause of many things and a poor Lifestyle causes the generation of an amount of bilirubin in the body.
Someone who is taking regular drugs without the prescription of their doctor may have a higher risk of generating jaundice or people going for substance abuse like alcohol
and smoking are more prone to getting affected by the disease. However, the disease is easily preventable if you are following a Healthy lifestyle,
having a properly balanced diet managing stress, having Limited consumption of alcohol, exercising regularly, having protected and safe sex and going for a regular medical check-up can easily reduce the risk getting affected by any kind of disease in themselves.
What are the various Signs and symptoms to detect jaundice in my child or anyone else?
Jaundice is caused when your body starts secreting excess amounts of bilirubin in the red blood cells of your body.
The symptoms to detect jaundice include the following-
• Pale, yellowish colour of your skin and Eyes
• Dark and yellowish urine
• Change in the structure of your stool passage
• Mild or moderate level fever
• Continuous irritated and tickled skin
• Nausea
• Vomiting
• Diarrhoea
• Appetite loss
• Unexpected weight loss
• Restlessness and dizziness
Did you see medical attention for Jaundice treatment?
Medical attention is needed if your child or anyone else faces a yellowish skin texture of your body which does not improve within 2–3 days or maximum within a week. Also, if you don’t experience the yellow skin colour of your body but experience the other following symptoms explained above still you should go for a medical consultation at least once.
What are the various causes and diseases which are associated with Jaundice?
Myth — jaundice is a normal diseasJaundice is caused by the secretion of bilirubin in your body but there are many other states of the body which can result in jaundice. Some of them include the following –
• Lack of enzymes in your body
• Brain haemorrhage
• Sepsis issues
• Biliary atresia
• Abnormal function of your liver
• Suffering from other viral infection
The three stages of Jaundice in a person’s body –
• Pre-hepatic stage of jaundice — pre-hepatic jaundice occurs before the secretion of bilirubin in the liver. The disease can lead to autoimmune disorders like nausea, diarrhoea and malaria.
• Hepatic stage of jaundice — the hepatic stage is said to be when the condition starts generating inside the liver which can cause hepatitis and liver disease.
• Post-hepatic stage of Jaundice — when the medical state arises after the secretion of bilirubin in the liver causing bladder issues and cancer it is the hepatic stage.
What are the risk factors associated with Jaundice?
Some of the factors that increase the risk of Jaundice in a person include the following –
• Your age — Although jaundice can affect people of any age children are more prone to jaundice.
• Your race — people of East Asia are found to get jaundice more easily than people in other parts of the world.
• Premature birth of your child
• Lesser Breastfeeding
What are the complications associated with jaundice — Jaundice can lead to various kinds of complications in one’s body like –
• Kernicterus — kernicterus is a medical condition which leads to permanent damage to the human brain. The disease leads to hearing loss vision loss on controlled body movement and unhealthy tooth enamel.
• Acute bilirubin encephalopathy — this is also the disease which is most common in children. The disease affects your brain and can lead to abnormalities like fever and inability to walk and learn new things in children.
Is jaundice preventable?
How can I prevent jaundice?
Yes, jaundice is preventable by taking very few precautionary measures in your everyday life. these include the following –
• Maintain a healthy weight
• Limit alcohol and smoking
• Stay hydrated. Drink plenty of fluids
• Have a properly balanced diet with an adequate amount of high-fibrous foods
• Exercise regular
• Practice yoga and meditation
• Learn to manage your stress in this busy lifestyle
What are the various common myths created about jaundice?
e like others.
Fact — jaundice is not a disease but a medical condition where your body starts secreting excess amounts of bilirubin.
Myth — jaundice is a very serious medical state
Fact — this is a partial myth. Yes, jaundice left untreated can lead to various severe complications but the death rate of Jaundice is very low and every person suffers from jaundice at least once in their lifetime so it’s quite common and easy to get rid of.
Myth — exposure to sunlight can solve the jaundice
Fact — this is a big myth. Exposure to sunlight to someone suffering from jaundice can worsen the state as it can lead to sunburn and dehydration.
How do doctors diagnose jaundice?
In most cases, diagnosis of Jaundice is not needed as the pale skin texture answers everything. But doctors still go for your examinations for confirmation. these examinations include the following-
• Blood analysis
• Urine test
• Physical test
• Skin test with transcutaneous bilirubin meter
• Stool sample ( if necessarily needed )
Study the pre-health issues of the person
Read More:-
1 note
·
View note
Text
Shedding Light on Gallbladder Cancer: Risk Factors and Prevention
Gallbladder cancer is a relatively rare but deadly form of cancer that develops in the gallbladder—a small, pear-shaped organ located in the upper right portion of the abdomen. The gallbladder stores and concentrates bile produced by the liver and released into the small intestine to help with fat digestion. While not very common, gallbladder cancer poses serious health risks and requires urgent medical intervention for treatment. This in-depth article aims to provide comprehensive information about gallbladder cancer, including risk factors, symptoms, diagnostic tests, staging, treatment options and prevention strategies.
What is Gallbladder Cancer?
Gallbladder cancer, also known as cholangiocarcinoma, occurs when abnormal and uncontrolled cell growth develops in the epithelial lining of the gallbladder. These cancerous cells form tumors that can destroy healthy gallbladder tissue and spread to other organs if left undetected and untreated. Gallbladder cancer is considered an aggressive form of cancer as it often does not show obvious symptoms until reaching an advanced stage. The majority of gallbladder cancers are diagnosed at a late stage when the probability of long-term survival is quite low.
Risk Factors for Gallbladder Cancer
Several factors are known to increase the risk of developing gallbladder cancer. Age is a significant risk factor, with most gallbladder cancers occurring in people over 60 years of age. Women are also at a slightly higher risk than men. Other prominent risk factors include gallstones, infection of the gallbladder (cholecystitis), obesity, smoking, and family history of gallbladder cancer. People with conditions like porcelain gallbladder or gallbladder polyps are also known to face elevated risk. Chronic inflammation caused by these risk factors is believed to damage gallbladder cells over many years and increase cancer risk.
Symptoms of Gallbladder Cancer
Early stage gallbladder cancer often does not present any perceivable symptoms. As the cancer progresses and spreads, the following signs and symptoms may develop:
- Continuous pain in the upper right or middle section of the abdomen
- Jaundice or yellowing of skin and whites of eyes
- Loss of appetite and unintended weight loss
- Fever
- Nausea or vomiting
- Enlarged lymph nodes in neck region
- Fatigue
- Abdominal swelling or lump
- Pain under ribs on right side of body
Diagnostic Tests for Gallbladder Cancer
When gallbladder cancer is suspected based on symptoms and medical history, doctors perform some imaging tests and laboratory workups to confirm diagnosis:
- Abdominal ultrasound examines gallbladder thickness and mass formation
- CT scan provides detailed images of organs and lymph nodes
- MRI scan uses magnetic fields to produce detailed pictures of soft tissues
- ERCP enables direct visualization and biopsy of gallbladder
- Blood test to check bilirubin, alkaline phosphatase and liver enzyme levels
- Biopsy involves surgically removing gallbladder tissue sample for examination under microscope
Staging Gallbladder Cancer
0 notes
Text
What You Need To Know About Bile Duct Cancer
Bile duct cancer, also known as cholangiocarcinoma. It is a rare form of cancer. It often affects older adults and has usually spread beyond the bile ducts by the time it’s diagnosed. February month is celebrated the Bile Duct Cancer Awareness Month worldwide. On this occasion. Dr. Srivatsan Gurumurthy, a Robotic & Laparoscopic Surgeon in Chennai provides valuable information about bile duct cancer. He explains the bile duct cancer, it’s symptoms, types, and treatment options available of the bile duct cancer. Most people receive a cholangiocarcinoma diagnosis after the cancer has already spread outside of their bile ducts. It’s difficult to treat and the prognosis (chance of recovery) is usually poor. However, a growing number of targeted therapies and clinical trials are starting to change that.
Types of bile duct cancers by location:
Bile duct cancer (cholangiocarcinoma) can start in any part of the bile duct system. Based on where the cancers start(see the picture below), they’re grouped into 3 types:
Intrahepatic bile duct cancers
Perihilar (also called hilar) bile duct cancers
Distal bile duct cancers
Symptoms of Bile Duct Cancer:
Jaundice
Abdominal Pain
Itching (Pruritus)
Unexplained Weight Loss
Fatigue
Pale-colored Stools
Dark Urine
Diagnosis of Bile Duct Cancer:
Medical History and Physical Examination: Dr Srivatsan Gurumurthy will interrogate about the existent’s symptoms, medical history, and any procurators that could elate the threat of corrosiveness conduit cancer. Dr Srivatsan Gurumurthy will also guide a thorough physical examination to identify gesticulations similar to hostility, abdominal pain, and detectable lumps
Blood Tests: Blood tests may be performed to assess liver function and to check for elevated levels of certain substances, such as bilirubin and liver enzymes.
Liver function tests: These liver tests check your blood for high levels of substances that might indicate your liver isn’t working as it should or there is a bile duct blockage, such as elevated liver enzymes.
CT Scan (Computed Tomography): Dr Srivatsan Gurumurthyutilizes improved imaging ways to gain detailed cross-sectional images of the tummy, abetting in the identification of abnormalities in the liver and corrosiveness tubes. also, glamorous Resonance Imaging (MRI), a system analogous to a CT checkup, is assumed by Dr Srivatsan Gurumurthy to induce detailed images, especially salutary for imaging soft napkins.
Ultrasound: This imaging system uses sound swells to produce images of the liver and corrosiveness tubes and can support identifying blockages or abnormalities.
Endoscopic Retrograde Cholangiopancreatography (ERCP): This imaging system uses sound swells to produce images of the liver and corrosiveness tubes and can support identifying blockages or abnormalities.
Treatment of Bile Duct Cancer:
Treatment options encompass a combination of surgical procedures, chemotherapy, radiation therapy, and additional supportive measures.
Surgery:
Resection: This involves surgically removing the tumor and conterminous towel, frequently involving a partial liver resection( hepatectomy) or, in improved cases, the exclusive liver.
Whipple Procedure: For tumors near the pancreas or in the common bile duct, a Whipple procedure (pancreatoduodenectomy) may be conducted to excise affected portions of the pancreas, duodenum, bile ducts, and, at times, a portion of the stomach.
Liver Transplant: In specific instances, a liver transplant may be contemplated for selected patients diagnosed with early-stage bile duct cancer.
Chemotherapy: entails the administration of medicines to exclude or stymie the excrescency of cancer cells. It can be assumed pre or post-surgery to target residual cancer cells or to condense excrescences before surgical intervention.
Radiation Therapy:
Employs high-dynamism shafts to target and annihilate cancer cells. Its quittance can be foreign or internal, contingent on the excrescence’s position. Radiation remedy is constantly exercised in confluence with surgery or chemotherapy.
If you are one of the many people who suffer from a bile-duct disorder, you may be looking for a doctor who can help you get your life back on track. There are many different physicians who specialize in treating bile duct disorders, but if you want the best possible care, you should choose Dr. Srivatsan Gurumurthy, he gives the best bile duct disorder treatment in Chennai. Dr. Srivatsan Gurumurthy is a highly skilled and experienced doctor who has devoted his career to treating bile-duct disorders. He has a deep understanding of the medical issues that can cause these diseases, and he is passionate about providing his patients with the best possible care. If you are suffering from a bile duct disorder, don’t hesitate to contact Dr. Srivatsan Gurumurthy . He will help you get your life back on track.
0 notes