#gabapentin without prescription
Explore tagged Tumblr posts
Text
just a little anecdote about disabilities & medication
had to go without my gabapentin, a medication i'm taking for nerve pain for about 2 weeks or so while i was struggling to get in contact with my doctor, and there was a mistake with it getting sent to the wrong pharmacy. gabapentin is a very good medication for a lot of people, myself included. i take 600 mg 3 times a day, which is the standard dose for nerve pain, and it works super well. it's honestly a great medication, as it helps with anxiety as well
whenever i'm on my gabapentin, i still feel some pain in my back, joints, and left arm, but when i'm not on it, holy fucking hell. sometimes i get used to what it's like on gabapentin and completely and totally forget what life is like without it. during those 2 weeks, my back seized up so bad i thought it was going to give out on me twice, even while using my rollator walker. the amount of squeezing pain i felt almost made me pass out at one point. the pain was causing my muscles to tense up, strangling my spine and my sciatic nerve at the same time, causing awful spidering pains that ran down my hips and legs. my left arm was almost unusable due to an injury i'm still recovering from. my entire left forearm was in absolute agony, i could barely use it.
sometimes when you're taking a maintenance medication for a long time, it can feel like it's not doing anything anymore. but trust me, it's still doing its job. if you aren't getting worse on a medication, chances are, it's working in ways that have become easy to overlook. obviously it's okay if you ever need to stop a medication. i've had to stop many that weren't helping, or making things outright worse. it's okay if a medication is making you feel like trash and you stop it. but if you ever feel like you can stop the medication because you feel better: don't. that's a sign that the medication is working. stay on it. you don't want to go back to what you were dealing with before. trust me. you want that quality of life.
good medications really can make the difference. it's not a bad thing to need prescription medications. some of them are genuinely life changing.
#disabled#disability#disability rights#disabilities#actually disabled#cripple punk#crip punk#cpunk#neuropunk#madpunk#health#our writing
155 notes
·
View notes
Text
Guess who was so rude to the vet that she’s not coming back without drugs on board!

Hiding, snarling, growling, yelling…
At least she didn’t bite. At least she used her words. I’m glad we have gabapentin (and trazodone! two drugs for overachieving dog!) for the next visit.
The whole vet visit took forever. First, a sick patient turned out to have a Huge Fucking Emergency, so the vet I was seeing assisted on that patient. This is not a problem, emergencies go before non-emergencies. It just took forever.
Then, it took a while for the vet to lure Momo out. (She used Churu.) Then she tried to touch Momo, and all hell broke loose. Then we had to wait for the prescription.
The plan is to do the exam and nail trim next time, when she’s all high. The vet wants to do x rays, too, but that would turn a $200 visit into an $800 visit to confirm or rule out arthritis that can be checked for with a physical exam.
Anyway, Momo wasn’t always like this, but her last two vet visits were for emergencies (not pleasant) so I think she’s really starting to associate the vet with pain and suffering. The drugs will be a good thing.
15 notes
·
View notes
Text
i ran out of sleep meds the other night and decided to try the gabapentin that's been sitting in our pie safe for over a year because google said it can help with sleep. my dog used to take it daily, so we have two bottles of the stuff. it didn't do a thing for my insomnia, but! i've been having the absolute worst pain in my jaw/neck/shoulders the last couple of weeks, and five minutes after i took the gabapentin, i could feel my jaw muscles relax. the pain wasn't completely gone, but it was the most relaxed my jaw had felt in days. so now i'm wondering how i can get a prescription for gabapentin without admitting that i'm an idiot who's been taking her dog's meds.
#personal#gonna have foot surgery in 1.5 weeks and i'm sure they're going to ask me at the pre-op what meds i'm taking#and i don't want to be like 'well i'm taking gabapentin but it wasn't actually prescribed to me'#but guys the pain gets so bad sometimes#lowkey i want to try my dog's other meds now
8 notes
·
View notes
Text
me, wanting to give my cat more gabapentin than his prescription says for sedation on a cross country road trip: am I allowed to do that without asking a vet?
me, realizing I will literally be a vet tomorrow: oh yeah
3 notes
·
View notes
Note
What meds would Y/N be on for her conditions?

What the Routine Carries
Summary: Managing chronic illness isn’t just about pills and prescriptions—it’s about vigilance, adaptation, and knowing yourself so deeply that you act before the fall. For Y/N, that means a regimen mapped around her unique mix of POTS, Ehlers-Danlos Syndrome, endometriosis, and chronic migraines. For Connor, it means being the steady hand beside her—refilling the med case, monitoring vitals, tracking patterns, and showing up every single day without question.

Sunday nights in their apartment were quiet.
The kitchen island would be cleared of mail, mugs, and surgical journals. Y/N would sit in her hoodie and fuzzy socks with a heating pad wrapped around her hips, sipping ginger tea while Connor sorted the contents of her weekly med organizer—double-lock lids, color-coded rows, four time slots a day.
He knew her routine better than anyone. And he never missed a step.
Morning Meds (8:00 a.m.)
First, he started with Midodrine, a 10 mg dose taken thirty minutes before she planned to stand up for the day. It helped raise her blood pressure and keep her upright—a cornerstone med for managing her POTS.
Next came Fludrocortisone, a tiny 0.1 mg tablet that helped her body retain sodium and water. She always took it with salted Gatorade or electrolyte water, chased with something salty—usually pretzels or saltines if her stomach cooperated.
Then Magnesium glycinate, 400 mg. This one helped with both migraines and EDS-related muscle cramping. They’d learned the glycinate version was easier on her gut after trying citrate, which made things worse.
He always added Vitamin D3, 2000 IU, which Ava insisted she needed regularly to support her bones and joints—especially during endo flares when pain confined her to bed.
Her oral contraceptive, taken continuously, was critical. It helped suppress endometriosis flares by stopping her cycle altogether. If she missed even one dose, the bleeding and pain could return with a vengeance.
Some mornings, depending on her symptoms, he’d include a small dose of Propranolol—10 to 20 mg. She only took it if her heart rate was running too high. “You’re in the 140s again,” Connor would murmur gently, and she’d nod, knowing he was watching closely.
Lastly, Pepcid—20 mg to help settle her stomach and prevent reflux, especially important with so many meds that caused GI issues. That one came with breakfast.
Midday Routine (Around Noon)
This part was all about keeping her upright and balanced through the second half of the day.
She’d take 1 to 2 grams of salt tablets with at least 16 ounces of water or a Nuun tab dropped into Gatorade. This combo helped maintain her blood volume and prevented afternoon crashes.
On high pain days or if her joints felt especially unstable, Connor handed her Naproxen, 220 to 440 mg. She always took it with food, otherwise it flared her stomach. She hated it, but it helped with endo flare stiffness and EDS joint pain, especially in her knees and hips.
Evening Meds (6:00 to 7:00 p.m.)
Evenings were all about slowing down her nervous system and managing pain that built throughout the day.
Connor would hand her Gabapentin, usually 300–600 mg depending on her symptoms. It helped with pelvic nerve pain and endo-related spasms. She took it with dinner, right before they curled up on the couch with a blanket and her Kindle.
Next was Amitriptyline, 10 to 25 mg. Ava had prescribed it as a low-dose tricyclic for both migraine prevention and chronic pain modulation. It helped her fall asleep and stay asleep—something she hadn’t been able to do for years before she met Connor.
They’d added a calcium-magnesium combo supplement as well, meant to support muscle and joint health and balance some of the nutrient depletion that came from her higher med load.
Bedtime Meds (10:00 p.m.)
If the day had been a flare day—especially one where her back or legs had gone into spasm—Connor would bring her Cyclobenzaprine, 5 to 10 mg. It helped her muscles finally release.
Some nights, if she was anxious or wired from pain, Will had approved a low dose of Trazodone, 25 to 50 mg, to help her sleep without feeling groggy in the morning.
As-Needed Meds (Always Nearby)
Y/N never left home without Zofran ODT, 4–8 mg. The melt-in-your-mouth kind. Nausea was one of her worst enemies—whether from migraines, endo, or sudden POTS crashes—and Zofran was one of the few things that worked quickly.
For acute migraines, she kept a Sumatriptan auto-injector in her work bag and bedside drawer. If it got to the point where oral meds wouldn’t stay down, Connor would help her administer the injection. He’d sit beside her in the dark, whispering, “You’re okay. Just breathe.”
During heavy bleeding episodes from endo, especially breakthrough cycles, she used Tranexamic Acid (TXA). Oral doses worked sometimes, but when the bleeding got bad—really bad—Connor had standing orders to administer the IV form through her port.
They also kept Toradol injections and Ativan available for severe flares that became unbearable. Ava trusted Connor to use clinical judgment. Will made him promise to track every dose.
Hydration & POTS Fluid Management
Daily, she drank at least 2 to 3 liters of fluids—usually broken down into high-sodium Gatorade, Nuun tablets, or Liquid I.V.
On bad days, Connor administered 1–2 liters of IV saline through her port. He flushed it first, monitored her response, and kept a chart of how long it took for her vitals to stabilize. She hated needing it. He never judged her when she did.
Connor’s Role
He kept everything organized in a locked kit—one at home, one in his locker at Med, one in a go-bag for overnight stays or trips.
He checked her vitals quietly—early in the morning, after showers, before long walks. If she got pale or quiet, he didn’t ask. He just brought her fluids and wrapped a cool cloth behind her neck.
And every Sunday night, he sat across from her, sorting meds into little plastic squares that looked ordinary but carried so much of their life.
Because every dose was a promise.
Every vial, every pill, every IV line—
Was him saying: I see you. I believe you. I’m not going anywhere.
Not even on the hard days.
Especially not on the hard days.

#fluff#connor rhodes#connor rhodes x reader#connor rhodes imagine#yn halstead#chicago med#connor rhodes x halstead reader#sevasey51
6 notes
·
View notes
Text
g-ddamn fucking pharmacy is gaslighting me about my gabapentin scrip. somehow the last refill was written at half my actual dose. so i ran out in 2 weeks and then the pharmacy refused to fix it without another doctors appt, even though i Just Did That for this incorrect prescription. and there somehow "isn't a record of a prescription for [correct dosage]" even thought i've been taking it for years.
#i am in so much pain.#im just gonna stop going to this place this is fucking ridiculous#newt needs a text post tag#newt's medical posting
5 notes
·
View notes
Note
Hey, I sent an ask earlier asking about help with medications for migraines and I now see a bunch of your past resource posts. Thank you for taking the time to write and post about your experiences.
I was prescribed sumatriptan a few months ago, but haven't taken it often because it makes me feel dizzy, fatigued, lightheaded, and gives me brain fog. But I've been taking 50mg and never considered decreasing the dose! I plan to try 25mg now. I've been relying on ibuprofen, excedrin, and cannabis to treat pain which isn't great for my long term health. If you have any more suggestions, they are more than welcome and very appreciated
I guess I have 2 new questions, if you'll have em :)
1. So far I haven't found any of your posts that discuss preventative options. Do you have experience with these? What was your experience like?
2. Healthline says that one shouldn't cut or crush the tablet. Based on your posts, I assume your experience with doing this is fine, but I wanted to make sure before trying it.
Genuinely thank you for any help you may be able to give me. I downloaded the keeler method because of your recommendation.I appreciate it🐝
hi! some folks definitely get some gnarly side effects from sumatriptan. i was told by my physician that cutting the pill in half is fine, and i've been cutting the pills for 10 years without issue. but take that with a grain of salt, i'm obviously not a chemist lol. you may also want to ask your doctor about other triptans (rizatriptan, zolmitriptan, etc). it's possible that you'll react similarly to all triptans, but maybe there's an option that you'll tolerate better.
there are many options for migraine preventatives, which i have been exploring for 7 or 8 years now. keep in mind that my experience comes from living in the US with private health insurance. i can't speak to how you'd go about this in a different country or if you're uninsured, etc. also keep in mind that health insurance might not approve you for preventatives (especially the newer, better ones) unless you've been diagnosed with chronic migraine (meaning, 15 or more migraine days per month).
something i highly recommend to everyone suffering from regular headaches is to start taking magnesium. start at a lower dose (200mg daily), which you can increase to 400-600mg. magnesium is affordable, accessible and well-tolerated by most people, and is shown to be effective at preventing migraines. the main side effect is a laxative effect, so proceed cautiously if you have problems with that.
as far as prescriptions go, older migraine preventatives fall into three classes: antidepressants (usually amitryptaline), anticonvulsants (topiramate is a common one), and blood pressure medications. newer (and better, but more expensive) preventatives are: botox injections and CGRP inhibitors. in most cases, you'll need to jump through hoops to get these better preventatives. health insurance usually requires that you try and fail two of the three classes of old-school preventative before approving you for botox or CGRPs.
i've tried amitryptaline (did nothing; also, i don't tolerate antidepressants well) and three different anticonvulsants (topiramate, gabapentin and lamotrigine). i had horrible reactions to the anticonvulsants, with side effects like constant brain fog, tingling in my extremities, changes to how food tasted, increased headaches, and a full-body rash, to name a few. i don't say this to discourage anyone from trying these preventatives--in fact, many folks have great results with them. but they're medications used to stop seizures. they're heavy duty and the side effects should be weighed against their benefit.
botox (injected every three months by my neurologist) worked amazingly for about 6-8 months, and at its best i was only getting one or two migraines a week (which for me is great). but over the last six months, it stopped working as well and i was back to getting 10-15 migraine days per month. i would have liked to keep getting botox while pursuing other options, but insurance wants you to try monotherapies first. so i stopped botox and i'm in the process of getting approved to try aimovig (a CGRP inhibitor that you inject yourself once a month). there are other CGRPs that are in tablet form, like nurtec. CGRPs work remarkably well for lots of people, so i'm hopeful.
as a final note to this very long post lol, if you're able to get a referral to a neurologist or, better yet, a neurologist with a migraine/chronic pain specialty, i highly recommend doing so!
20 notes
·
View notes
Text
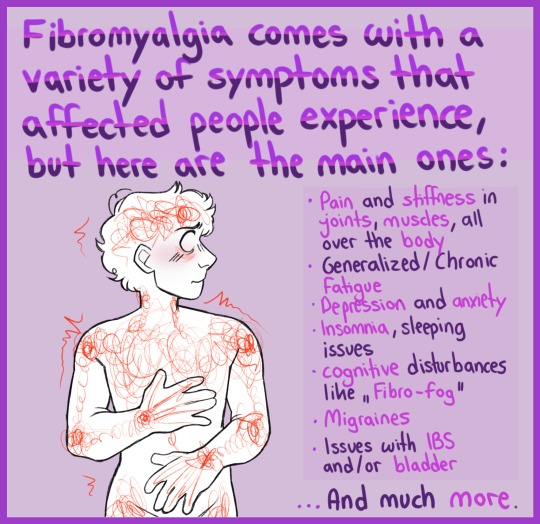
Some fibro thoughts:
I am in my early 50s. I was diagnosed with fibromyalgia about 10 years ago but have had symptoms and on and off treatment for those symptoms since my early 20s. For the last 10 years I have had naproxen prescribed and omeprazole prescribed to try and protect my stomach. Previous to that I didn’t have a PPI prescribed alongside my NSAIDs. Last year I was diagnosed with small stomach ulcers (an incidental finding when checking for other things) and my naproxen was stopped. So for the last year or so I have continued on gabapentin (slowly titrating the dose upwards to compensate for the lack of naproxen. I also take paracetamol 3-4 times a day. NICE (UK health guidance) means they won’t prescribe me opioids. So my pain relief options are limited.
The naproxen worked really well for me and I have really really missed it. A little while ago I got a referral to the pain clinic and had a good long consultation with a specialist pain doctor. I was hoping for another medication option. There isn’t one. I already have dry needling once a month and this or acupuncture is one of the things they suggest. He also suggested a TENS machine. This has made a huge difference. It’s still not as good as naproxen but it’s so much better than before.
The ‘prescription’ for the TENS is to use it on the sorest parts of my back, neck thighs etc for at least 20 minutes four times a day. He said to turn it up until you can’t bear it and then turn it down one. I thought I would find this hard to manage enough times in the day but I’m actually using a lot more than the minimum. There has been noticeably less stiffness and pain in my pelvis. I still haven’t quite cracked using it on my shoulders in a way that helps and doesn’t overwork the muscles but I’ll get there.
I can sometimes go a day without it but any longer than that I really notice the difference. I crave the electric shocks 😄
Obviously my kids had to have a play with my TENS when I got it. There was a lot of screaming from teen 1 but teen 2 really likes it.
All in all I highly recommend.
5 notes
·
View notes
Text
Very personal but important question(s?) regarding chronic health issues and disability
So I’ve had fibromyalgia and Gastroparesis for about a decade now, and I try my best to self-manage these issues (in addition to the expensive meds they give me that don’t really provide relief), but it becomes severely difficult for me to work a full schedule, particularly when my job drains me physically, mentally, and emotionally. I spend my days off in complete recovery mode, absolutely bed-ridden, afraid to do anything social or physical, because I risk going into a total Fibro meltdown. Which is a nightmare, but I’ll spare you the details.
I’ve been considering applying for partial disability because I think working 3 or 4 days instead of 5 or 6 would be much better for most humans, honestly, but particular for someone like me who deals with chronic nausea, discomfort, and pain on the daily. I’ve been putting it off for ages though because I know that disability can be very difficult to get and a horrible process and I can’t work myself up to it or afford a disability lawyer to help me. I tried being a little more aggressive this past summer and collected “documentation” on my fibromyalgia in the hope of preparing to submit it, and literally all of my documentation says “fibromyalgia?” because apparently none of my doctors believe me after years of testing and thousands of dollars of office visits trying to get this diagnosis. To be honest, using fibromyalgia as my reasoning for disability needs was a dead end anyway because lots of doctors still don’t believe it exists, so I doubt the government would find that a good reason either. And I really doubt they would take the Gastroparesis seriously either, even though both of these conditions are dehabilitating at times.
So one of my friends recommended I go through the avenue of my mental health issues. At different points of my life I’ve been diagnosed with depression, anxiety, bipolar, ocd, adhd, etc, and who knows what the real answer is, but she’s a mess. I’ve been realizing over the past couple years that I’m very likely autistic, and that would actually explain a lot of these things, but the past 6 months have been crazy, and even though I’ve been working a bunch, I’m poorer than ever because of the rising cost of everything, so I cannot afford to get a formal diagnosis yet. But I know that I told my most recent psychiatrist all these horror stories about my anxiety, so I decided to get done documentation for her too, and guess what? Generalized depression and mild anxiety. Girl, huh? (Tw: blood and dermatillomania coming up) I showed her evidence of scars on my hands from picking my hands every night til I bleed everywhere, I described how I get overwhelmed and cry at work several times a week and often fight back panic attacks at work and in my private life, I told her than I struggled to fall asleep and stay asleep and only got collectively about a few hours every night, I told her that I literally could not socialize without using alcohol as a crutch but I can no longer do that because of my digestive issues so I self-isolate, I told her that I struggle to maintain eye contact and panic when people give me eye contact… so many stories like these. Mild anxiety smdh
So that comes to my first question cause I guess I decided while writing this that I have a couple:
1) How do you, as a female-presenting person, get a diagnosis for severe anxiety? How wild do my stories have to be without accidentally committing myself?! I have an ex, amab, who basically pulled a john Mulaney and was like, “I get nervous on planes sometimes” and he legit got a prescription for Xanax or one of those other big ones, and another who is on a dose of gabapentin 5x the strength of mine because he gets social anxiety sometimes, so this is especially frustrating that I can’t even get a dang proper diagnosis on anything after ten+ years of therapy, doctors, tests, everything.
2) What is the process like for getting an autism diagnosis and are there cheaper routes you can go that would still be credible? I’ve exhausted my expenses from years of jobs not paying my worth combined with money poured down the drain trying to get any sort of help with my kaleidoscope of issues, and at this point I’m too broke and demotivated and burnt out to figure out a way forward.
3. Has anyone been able to get partial or full disability who would be willing to hold my hand through the steps and keep me motivated? I know it’s a huge ask but I honestly get so anxious even thinking about the process that I completely shut down. At the very least, maybe you could explain what worked for you or how you would approach it better next time? I just moved far away from my support group so I’m feeling alone and even a word of caution or encouragement would help.
I know I’m not really as connected to this community as I used to be, but I’m hoping someone will get to the end of this and even a kind word or a smidge of sympathy/empathy would be nice. And please do reach out if you have fibro because I don’t meet many and it would be nice to have friends who can relate. Thank you for listening! 💜💜💜
12 notes
·
View notes
Text
Because not many people know this, let me add a little info!
First, fibromyalgia is more of a symptom set than a disorder. The entire scope of causes isn’t known yet, but it can be caused by conditions such as mast cell activation syndrome, which is treatable to a degree! Fibromyalgia can also be treated with prescriptions such as gabapentin and supplements such as magnesium malate and fibro response. Of all the things I’ve tried, though, nothing has EVER reduced my pain level to that of a normal person.
Because it is a symptom set, it is nearly impossible to apply for SSI disability for it without being able to also list the root cause — largely because fibromyalgia cannot be tested for and is not considered proven in any given person alone, depending on what state you’re applying in.
Fibromyalgia has been recorded in far more AFAB people than AMAB people. In many cases, it is linked to hormones, and can start with puberty or pregnancy and even end/decrease with menopause. I’m sure it’s no coincidence that these things also have a correlation with MCAS, but studies on both of these conditions aren’t advanced enough yet to say for sure.
Weather can increase fibromyalgia pain, but is not the root cause. Exercise by and large will not help fibromyalgia, and may even cause more damage. The recommended exercise to manage fibromyalgia is aquarobics and water therapy, not running and lifting. It is not dependent on the strength of our muscles.
If you have all of the symptoms listed in the above graphic, I am begging you to check yourself out for mast cell activation syndrome, because every one of those is a symptom of it. You can evaluate yourself for symptoms, see an immunologist or hematologist to get tested, and check out r/MCAS on Reddit for more info.
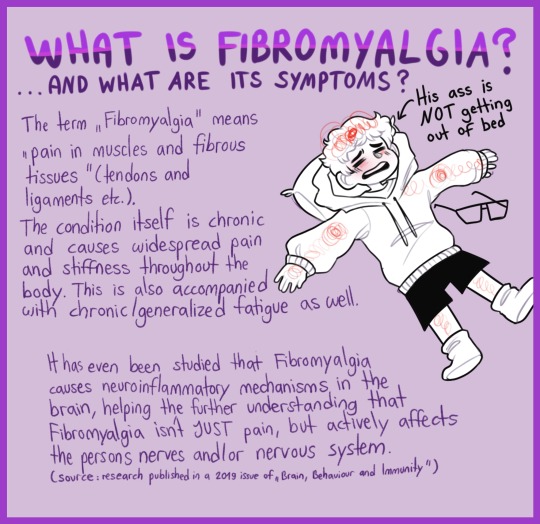





Yesterday the 12th of May was Fibromyalgia awareness day. I'm a little late uploading it, but spreading awareness is being done nonetheless. Lots of love for my chronic pain people!! <3
28K notes
·
View notes
Text
Chat, I am beat.
My 'until at least Thursday' tolerance break was sorely tested when my body decided it was time to start preparing for Shark Week, causing the pre-ovulation ovarian cyst to rupture open so hard that I'm fairly certain my neighbor wonders what the screaming was about.
Part of the tolerance break is to see if I actually can deal with my pain without my green medicine (if you know you know). I didn't realize just how much it was covering.
The Voltaren definitely isn't keeping up with my back.
The Baclofen also isn't keeping up with my back.
The Excedrin is keeping up with my hands, but only barely. It needs the extra benefit of my electrotherapy gloves to really keep up - thanks a lot, hEDS.
The headache and nausea that the Victoza induce? I'm just going to have to deal with it for now, because I need to see how it affects my body on its own first. Which sucks, because now the fibro is acting up again:
The constant "everything is road rash and I just decided to apply bleach to it" pain that is fibromyalgia? Yeah, it was covering that too. Right now the inside of my right arm feels like I spent the day doing arm day at the gym - and on that note can I talk about how much fibro has made me miss going to the gym? I can't do it anymore. The Lyrica, only recently returned to the regimen, needs time to get going before I bring my green medicine back, because it has a stronger enhancing effect on it than even the gabapentin does. Gabapentin was what I was taking to compensate for not having the Lyrica for the last couple weeks, and it barely did anything. It probably doesn't help that it was probably two years or so past the actual prescription date, and being taken at a slightly lower dose than originally prescribed so that it could stretch until I got my Lyrica back.
And to top it off, I just confirmed that another storm system is blowing in with my weather app. I probably didn't need to check, being a human weather vane, but I had to be sure.
And between a fundraiser post and straightening up the house for company on Friday, I have so much to do this week.
0 notes
Text
Menopause Management: What New Treatments Are Available?
Hot flashes. Mood swings. Sleepless nights. Sound familiar?
If you're going through menopause—or getting close—you know it's not always smooth sailing. But here’s the good news: modern medicine has come a long way in helping women manage menopause symptoms with more personalised, effective, and safer treatment options than ever before.

Let’s explore what menopause really means, what symptoms you might expect, and the latest treatments available to help you feel more like yourself again.
First Things First: What Is Menopause?
Menopause marks the end of a woman’s reproductive years. It’s officially diagnosed after 12 months without a menstrual period, usually between the ages of 45 and 55.
But for many women, the transition—called perimenopause—can begin years earlier. During this phase, hormonal fluctuations can trigger a variety of symptoms, both physical and emotional.
Common Menopause Symptoms
Every woman’s experience is different, but here are some of the most common symptoms:
Hot flashes and night sweats
Mood swings and irritability
Sleep disturbances
Low libido and vaginal dryness
Memory lapses or brain fog
Weight gain and joint pain
These changes can impact your quality of life—but they don’t have to.
Why Treatment Matters
Menopause isn’t an illness—it’s a natural life stage. But that doesn’t mean you should suffer through it.
Managing symptoms can help you:
Sleep better
Improve mood and energy
Maintain a healthy sex life
Protect bone and heart health
Thankfully, today’s options go beyond just riding it out.
What's New in Menopause Management?
Here’s a look at some of the most promising and up-to-date treatments available in 2025:
1. Low-Dose Hormone Replacement Therapy (HRT)
HRT has been around for decades, but newer formulations are safer and more tailored. Today, doctors often recommend low-dose estrogen patches, gels, or pills combined with progesterone.
Helps reduce hot flashes, night sweats, and vaginal dryness
Supports bone density and heart health
Must be prescribed based on individual risk factors
Modern HRT is personalised, not one-size-fits-all—and much safer than it used to be.
2. Non-Hormonal Medications
Not a candidate for HRT? No worries. Several non-hormonal options are showing great results:
SSRIs/SNRIs (like paroxetine or venlafaxine) help with mood and hot flashes
Gabapentin is often used for sleep and hot flashes
Clonidine, a blood pressure medication, can also ease flushing
These are prescription medications and should be taken under a doctor's care, but they offer real relief without hormone risks.
3. Vaginal Estrogen Therapy
If vaginal dryness or painful sex is a concern, local estrogen treatments like vaginal creams, rings, or tablets can help—without affecting the rest of your body.
They offer:
Localised relief
Minimal systemic absorption
Long-term comfort with regular use
4. New Generation Supplements
There’s a growing interest in natural, clinically-studied supplements for menopause, such as:
Black cohosh
Red clover
Ashwagandha
Evening primrose oil
Some women find relief using these, especially when paired with healthy lifestyle changes. Just remember: “natural” doesn’t mean risk-free—consult your healthcare provider before starting.
5. Menopause-Friendly Lifestyle Plans
More doctors today are taking a holistic view. That means combining medications or therapy with:
Weight training to protect bones
Anti-inflammatory diets to balance hormones
Yoga and meditation to manage stress
Sleep hygiene techniques to improve rest
These aren’t quick fixes, but they play a vital role in long-term wellness.
6. Digital Health Solutions & Telemedicine
With menopause apps and virtual clinics gaining popularity, women can now:
Track symptoms in real-time
Access expert consultations from home
Join support groups and forums
Receive reminders for medications or screenings
It’s all about putting control back in your hands—and it’s working.
Choosing the Right Treatment for You
Every woman’s journey through menopause is unique. What works for one may not work for another. The best path forward involves:
Honest conversations with your doctor
A personalised treatment plan
Regular reviews and adjustments
Whether you're just entering perimenopause or deep in the throes of it, support is available—and getting better every year.
Ready to Find Menopause Relief?
At Medicine Mart, we offer a range of safe, doctor-recommended treatments for menopause symptoms—delivered discreetly and affordably to your door. Explore Menopause Medications Because you deserve to feel balanced, confident, and well—no matter your age.
0 notes
Text
¶ … Label Drug Use USELESS, COSTLY or FATAL Off-Label Drug Use In November, 2003, the Knight-Ridder news service conducted an investigation on a practice called "off-label prescribing (Devitt 2006)." It found that doctors wrote up to 115 million prescriptions per year for drugs for off-label or unapproved uses. The concern has been that 8,000 to 80,000 people could develop serious reactions to these drugs. The May 8th issue of the Archives of Internal Medicine published a report about the practice. It said that more than one in every five prescriptions given out in the United States has been for unapproved or unproven use. One out of seven is intended for purposes with "little or no scientific" basis or support. The drug is either not approved by the Food and Drug Administration or prescribed for another condition. The drug may, for example, be indicated for cancer but prescribed for hypertension. Or the doctor may change the dosage or duration of the treatment or use. These are examples of off-label prescribing (Devitt). When the FDA approves a particular drug for a particular ailment, doctors can legally prescribe it for another ailment (Devitt 2006). Drug manufacturers do not have to get approval for all the conditions for which a particular drug may be useful. Furthermore, doctors do not have to inform patients that the drug being prescribed is for off-label use. The American Medical Association endorses their members' autonomous clinical decision-making authority over off-label drug use as long as it is drawn from "sound medical opinion and strong scientific evidence." This is the provision of AMA policy H. 120-988 (Devitt). A research on the 100 most popularly prescribed drugs in the U.S. And 60 randomly selected medications from the Archives of Internal Medicine (Devitt 2006). These 160 drugs were approximately 56% of all prescribed drugs used in 2001 alone. The purpose of the research was to determine how many of these drugs were FDA-approved, off-label but with sound scientific support, or off-label with limited or without scientific support. Analysis of the findings showed that the majority of the prescribed drugs were FDA-approved but a large number lacked FDA approval for conditions they were used for. In addition, 15% of them lacked the appropriate scientific basis for the use. Off-label prescriptions were most often used for cardiac drugs and anticonvulsants. Findings showed that 46% of all drugs prescribed for these conditions were off-label. As to volume, 35.5 million antimicrobials were prescribed for psychiatric treatment as antidepressants, anxiolytics and anti-psychotics. A third of all off-label prescriptions were cardiac medications and anticonvulsants. The most frequently prescribed off-label at 83% was gabapentin. It is an anticonvulsant medication approved for epileptic seizures but often prescribed for nerve pain caused by the herpes virus. In addition, only 20% of these off-label prescriptions had the required strong scientific support for the alternative use. In 2004, the manufacturer of gabapentin pleaded guilty to two counts of criminal fraud for which it paid more than $430 million for the charges and civil liabilities. Other frequent off-label prescriptions were made for the antidepressant amitriptyline hydrochloride at 81% and the oral steroid dexamethasone (Devitt). The Knight-Ridder study conducted in 2003 found that off-label drugs sold at approximately $12.9 billion or almost a quarter of those on retail (Devitt 2006). Yet the Knight-Ridder examined only 45 of these drugs and did not include those for cancer and pediatric uses. The Archives researched used only 160 of these and only for 2001. Of the thousands of drugs sold in the U.S., one cannot possibly measure the financial and human costs entailed by off-label prescribing as to their wasteful use, insurance billing and paperwork in addition to the incalculable risks to human safety and health (Devitt). Issues on off-label drug use center on effectiveness and safety (Nightingale 2003). In practical terms, these issues relate to the administration, contraindications, warnings, precautions, abuse and dependence of these drugs as they used in ways other than those approved by FDA. Problems arise from the authority and wisdom for their un-approved uses, and the risks incurred in prescribing, reimbursement and coverage, physician liability and the conditions on the manufacturer's dissemination of the literature of these drugs. Effective patient care requires that a physician be authorized and free to use and prescribe drugs as he sees fit. When he uses or prescribes off-label, he assumes the responsibility of being well-informed about the drug and the possession of sound medical evidence and judgment. The lack of approval for off-label use may be the company's lack of interest in acquiring that approval for its own commercial or financial reasons. Or the company may have included off-label use but the FDA did not approve this (Nightingale). A physician who is contemplating on prescribing an off-label drug for a particular patient may be guided by guidelines for pertinent indications, diseases or population groups (Nightingale 2003). He may review the FDA's updated labeling, such as black-box warnings, contraindications, interactions and side effects, especially those relating to off-label use. He may also consider higher doses, use among different groups, use in patients with other medical conditions or taking other medications. It will be an advantage to gather information on how long the particular drug has been in the market and the extent of off-label use and its status in other countries with a modern regulatory system for drugs. The physician has the pivotal role in the matter. If he possesses reliable and detailed knowledge of the medical history and status of the patient, the physician may decide on the appropriateness of an off-label drug for a condition and in that setting. The drug may prove to be more or less effective, safer or less safe, than the drug officially approved for the condition. The drug may otherwise be ineffective and unsafe. Information about off-label prescribing is accessible from medical literature, professional associations, pharmacies and the FDA online. This accessibility will help the physician reach or form appropriate decision on off-label drug use (Nightingale). The consequences of high-profile drug safety controversies have been changing the environment of drugs and marketing of drugs (Business Editors 2005). They also tend to reduce potential profits of companies from the off-label use of these products. The U.S. And the European Union regulatory reform reduced indication expansion as a protection strategy. Indication expansion will differentiate the new use and prevent off-label use in the new indication. A company needs to identify the best indication management strategy for its brand of drugs. It must discover and understand the impact of regulatory reform and increased drug safety awareness about off-label drug use. It also needs to know the best timing for the launching, competitive position, pricing and what market factors influence the effectiveness of the selected indication expansion strategy (Business Editors). An injectable drug, called Byetta, can now allow diabetics reduce blood sugar to normal levels slowly and steadily (Wilson 2005). Byetta was recently approved by the FDA. These benefits can lower blood pressure and cholesterol and the need to take other medications, according to Dr. Carol Wysham. Dr. Wysham, an endocrinologist at Rockwood Clinic, was a major researcher of a study on the effects of Byetta. She described the drug as the biggest breakthrough in the control of diabetes in the past 10 years. Present FDA-approved medications are injected by the patients themselves before breakfast and before supper. In diabetes, the pancreas does not produce enough insulin to make glucose enter the cells freely. Glucose is the source of body energy. Glucagon-like popypeptide or GLP-1 is produced in the intestines of healthy persons and stimulates the secretion of insulin. Diabetics lack this hormone. Other drugs are administered in the early stages of the disease to raise the level of secretion of insulin or improve sensitivity to insulin. Insulin in injection form is resorted to only when there is no other way the patient can have enough of it as the body needs. It is still unknown why diabetics have less GLP than non-diabetics at 30 to 40%. The new drug, Byetta, fills these needs. It more than supplies the insulin the pancreas cannot secrete. It also does not produce additional insulin when the sugar level reaches the normal range. While current injections are done twice daily, Byetta injections are used only once a week (Wilson). Approximately eight years ago, Dr. John Eng, a hormone researcher in New York, found the chemical composition of the saliva of a Gila monster as almost identical to that of GLP-1 (Wilson 2005). The Gila monster is a poisonous lizard, which lives in the deserts of Southwestern U.S. And Mexico. Amylin Pharmaceuticals took advantage of Dr. Eng's finding and synthesized the Gila monster's saliva. FDA subjected it to prescribed trials and later federally approved it as Byetta. Researchers have been familiar with GLP-1, Byetta's model. But it fades quickly after being introduced into the body. Hence, it could not be used to cure diabetes. There is a steady flow of GLP-1 in non-diabetic bodies, which keeps the pancreas active in secreting insulin at normal levels. The structure of Byetta is similar to that of GLP-1 and performs the same functions. Both promote decreased appetite (Wilson). Dr. Wysham was an observer at a study conducted on 20 Rockwood diabetic patients who were taking conventional diabetic medication for their uncontrolled blood sugar (Wilson 2005). She was not informed about their glucose levels for several months after the tests began. About two-thirds of the respondents were given different injectible doses of Byetta to incorporate into their medication plan, while the rest were given placebos. All of them were instructed and trained to do the injections at certain times twice daily for a month. Then they were subjected to a physical exam. Dr. Wysham closely monitored their liver, kidney, blood counts, and other functions. She observed that the patients consistently lose weight while taking Byetta. The average respondent-patient lost 15 pounds in the duration of the study, 5 lost more than 20 and two, more than 40 (Wilson). The results of the study led Dr. Wysham to believe that Byetta could slow down or even terminate the progression of diabetes before a patient requires insulin therapy (Wilson 2005). Injecting insulin and injecting Byetta had almost the same results. Byetta even made patients lose weight. This was the finding of a recently concluded six-month study. It compared patients who took insulin and patients who took Byetta both as injectibles and twice daily. Dr. Wysham commented that 102-week extension trials confirmed the trend. While she noted that Byetta does not work in all cases. But the results of an 82-week study showed that 62% of the respondents met clinically-established glucose standards, which they previously failed to meet. Dr. Wysham said that 90% of all diabetics are overweight and the benefits deriving from Byetta have understandably drawn diabetics to it. It is expensive yet compares with the price of other conventional diabetic drugs. It is covered by most health insurance plans. She estimated that Byetta costs $150 a month at wholesale (Wilson). Eli Lilly's Byetta, indicated for Type 2 diabetes (Johnsen 2005).Its generic name is exenatide, considered an incretin mimetic agent. It imitates the action of insulin in the intestines in stimulating insulin production without the risk of hypoglycemia. This risk is associated with insulin injections. Byetta is the synthetic exendin-4 hormone from the saliva of the Gila monster. This lizard eats only four times a year. When not eating, its pancreas is inactive. When it does, the exendin-4 found in its saliva reactivates the pancreas. Byetta imitates the mechanisms of insulin, which is similar to extendin-4. Byetta remains in the blood system and works only when blood sugar levels are too high. Observers projected the sales of Byetta to exceed $800 million next year. Its manufacturer, Eli Lilly, was working for the approval of a long-acting release version last year. This new formulation was predicted to reach $1.5 billion in sales (Johnsen). Exenatide injection is indicated only for Type-2 diabetes but not as a substitute for insulin (Ezzo and Ambizas 2006). The biggest clinical test of exenatide therapy investigated 733 patients who used exenatide with metformin and a sulfonylurea for 30 weeks. The most commonly observed adverse reaction was gastrointestinal in nature. The combination of xenatide and metformin did not increase the incidence of hypoglycemia. But there was a 3.3-14.4% increase when sulf0nylurea was added to exenatide (Ezzo and Ambizas). In studies on the tolerability of exenatide when combined with current therapy, 7% of the respondents backed out because of nausea and vomiting (Ezzo and Ambizas 2006). Other common reactions were diarrhea, dizziness, headache and shaking. The patients lost an average of 4.9 pounds in the 30 weeks of study. Another study, which combined exenatide and insulin glargine, 1 in 10 withdrew because of the adverse effects of the combination. These effects were 57% nausea and 17% vomiting. As to effectiveness, studies showed that a combination of exenatide would result in 7% or less of A1C in 24 to 46% of patients with an initial A1C of more than 7%. Exenatide reduced fasting plasma glucose levels by 5 to 10 mg per dL. This did not increase weight. A pre-filled pen containing 60 doses of exenatide for a month would cost approximately $191 to 223. A vial of 10 ml of insulin glargine would cost approximately $69 for a month's use. And exenatide is sold as a sterile solution for subcutaneous injection at 250 mcg per mL. It is available in 1.2-mL prefilled pen and in 2.4-ml prefilled pen forms. This should be injected into the thigh, abdomen or upper arm. It should be refrigerated and protected from light. It should be disposed of 30 days after the first use. The first dosage must be injected subcutaneously two times daily within 60 minutes before the morning and evening meals, not after. The dose may be increased to 10 mcg twice daily after a month of treatment. When added to metformin, exenatide may be continued. When added to a sulfonylurea, the dose of sulfonylurea should be reduced to avoid or reduce the risk of hypoglycemia (Ezzo and Ambizas). Exenatide injectible for Type-2 diabetes requires that the patient be educated in its use (Ezzo and Ambizas 2006). Glucose levels should be strictly monitored because of the difficulty of use. Exenatide is costly and inconvenient. It is still believed not to have proven benefits over other drugs used to treat diabetes, such as insulin (Ezzo and Ambizas). The other off-label drug used in the treatment of Type-2 diabetes is Januvia, a product of Merck & Co., Inc. (Business Editors 2007). It was the first and only depeptidyl peptidase-4 inhibitor or DPP-4 to be accepted and used by the European Commission. It is said to enhance the body's ability to reduce blood sugar levels when it goes higher than normal. In treating Type 2 diabetes, Januvia improves glycemic control when combined with metformin. This is the recourse when diet, exercise and metformin have not effected sufficient glycemic control. Patients with Type-2 diabetes and using a PPAR gamma agonist may find it useful. All 27 countries of the EU have adopted its use. The drug was to be launched in the 42 EU countries, including Mexico, the U.S. And the Philippines (Business Editors). The U.S. FDA approved Januvia in October 2006 as a monotherapy as well as an adjunct therapy to metformin or thiazolidinediones or TZDs (Business Editors 2007). These are intended to improve blood sugar control in Type-2 patients when diet and exercise alone would not work. The recommended dose is 100 mg once a day. It should not be used for Type-1 diabetes or diabetic ketoacidosis because it would not be effective in these cases. Common side effects were stuffy or runny nose and sore throat, upper respiratory infection and headache. The common and adverse gastrointestinal reactions include abdominal pain, nausea and diarrhea. Januvia is an oral and selective DPP04 inhibitor, which is taken once a day. It enhances the body's process of lowering blood sugar. It belongs to the incretin class of drugs. When the blood sugar level goes up, an incretin either helps the body regulate the high levels by stimulating the pancreas to increase the release of insulin. At the same time, it stimulates the liver to reduce the volume of glucose it produces. DPP-4 inhibitors promoted the body's natural ability to control blood sugar levels by activating these hormones. The drug has been approved in at least one country in the major regions of the world. These include Asia Pacific, Europe, the United States and Latin America. The recommended dose is also 100 mg per day with or without food. Patients with Type-2 diabetes who responded to clinical studies showed significant improvements in their hemoglobin A1C, fasting plasma glucose and the two-hour post prandial glucose (Business Editors). A study was presented to the American Diabetic Association, which found that Januvia, in combination with metformin, significantly improved glycemic control (Business Editors 2007). It was also well-tolerated for 54 weeks by patients with Type-2 diabetes. Additional data also showed that Januvia also performed at high levels when added to a sulfonylurea, glimepiride or when added to a combination of sulfonylurea and metformin. There are no contraindications to Januvia. It is a component of Janumet, the first and only synthetic tablet. It puts a DPP-4 inhibitor and metformin for the treatment of Type-2 diabetes. It may also be used as an adjunct to diet and exercise. Janumet is contraindicated to renal disease, renal dysfunction, abnormal creatinine clearance, and acute or chronic metabolic acidosis. Like Byetta, it should not be used for Type-1 diabetes. An investigational study revealed that Januvia substantially improved blood sugar control when added to sulfonylurea or a combination of sylfonylurea and metformin as against sulfonylurea or sulfonylurea and metformin alone. It is generally well-tolerated as monotherapy, as an initial combination therapy or as an additional therapy. It should be given twice daily with meals at 100 mg. Merck $ Co. continues to experiment on the siragliptin family for its other potential uses (Business Editors). Bibliography Business Editors (2005). Understand the impact of regulatory reform and raised drug Safety awareness on off-label drug use. 2 pages. Business Wire: Gale Group 2007). Januvia approved in the European Union for the treatment of type-2 diabetes. 4 pages. 2007). Late breaking data released at ADA showed that the investigational use of Januvia and Metformin as initial combination therapy provided significant glucose lowering efficacy over 54 weeks in patients with type 2 diabetes. 8 Devitt, M. (2006). A prescription for disaster. 3 pages. Dynamic Chiropractic: ProQuest Information and Learning Company Ezzo, D.C. And a.M. Ambizas (2006). Exenatide injection: adjunctive therapy for glycemic control. 3 pages. American Family Physician: American Academy of Family Physicians Johnsen, M. (2005). Diabetes drug evolving with first-in-class therapies. 3 pages. Drug Store News: Gale Group Nightingale, S.L. (2003). Off-label use of prescription drugs. 4 pages. Read the full article
0 notes
Text
Understanding Pain Management Options in Elmhurst

Pain is a universal experience that can significantly impact a person's quality of life. Whether it’s chronic, acute, or somewhere in between, managing pain effectively is crucial to maintaining daily function and well-being. Elmhurst, a vibrant city located in DuPage County, Illinois, offers a range of pain management elmhurst services for individuals suffering from various types of pain. This blog post aims to explore the various pain management options available in Elmhurst, covering everything from traditional treatments to cutting-edge therapies.
The Importance of Pain Management
Before diving into the specifics of pain management options in Elmhurst, it’s important to understand why pain management is so critical. Pain can come from many sources, including injury, illness, surgery, or underlying conditions such as arthritis, cancer, or neurological disorders. Chronic pain, in particular, can lead to long-term physical and emotional stress, impairing mobility, sleep, and overall health.
In fact, the American Academy of Pain Medicine reports that approximately 20% of adults in the U.S. suffer from chronic pain. Without effective treatment, pain can result in decreased productivity, a lower quality of life, and even mental health challenges like depression and anxiety. Pain management is not just about alleviating discomfort; it’s about restoring function and improving one’s overall well-being.
Elmhurst is fortunate to have access to a variety of pain management specialists and clinics, offering patients multiple options for addressing their pain and getting back to living a fulfilling life.
Types of Pain
Understanding the different types of pain is essential for determining the most effective treatment approach. Pain can broadly be categorized into the following types:
Acute Pain: This is short-term pain that arises suddenly, usually due to injury or illness. Acute pain serves as a warning system to the body that something is wrong. It typically resolves as the body heals.
Chronic Pain: Pain that persists for a longer period—typically more than three months—despite treatment and healing. Conditions like arthritis, fibromyalgia, or back pain often lead to chronic pain.
Neuropathic Pain: Caused by damage to the nerves, neuropathic pain can result from conditions like diabetes, multiple sclerosis, or shingles.
Cancer Pain: Pain associated with cancer can arise from the tumor pressing against tissues or nerves or as a side effect of treatment.
Post-Surgical Pain: After surgery, pain may occur due to healing tissues, inflammation, or nerve injury.
Each type of pain requires a unique approach to treatment. As a result, Elmhurst has a wide range of specialists, clinics, and methods to tailor pain management strategies to individual needs.
Traditional Pain Management Approaches
1. Medication Management
Medications are often the first line of defense for managing pain. Different types of medications target different types of pain, and they can range from over-the-counter options to more advanced prescriptions.
Over-the-counter (OTC) Medications: These are non-prescription drugs like acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin). They are often used for mild pain such as headaches or muscle strains.
Prescription Medications: For more severe pain, doctors may prescribe stronger medications. Opioids (e.g., morphine, oxycodone) have been used to manage acute and severe pain, but they come with risks such as dependency, overdose, and side effects. Due to the opioid epidemic, doctors are increasingly cautious about prescribing opioids for chronic pain.
Antidepressants and Anticonvulsants: These are often used for managing neuropathic pain, such as from diabetes or shingles. Drugs like amitriptyline (Elavil) or gabapentin (Neurontin) can help relieve nerve-related pain.
Topical Analgesics: These include creams, patches, and sprays applied directly to the skin to relieve localized pain, such as arthritis pain in the knees or hands.
2. Physical Therapy
Physical therapy is a cornerstone of pain management in Elmhurst. A licensed physical therapist (PT) works with the patient to improve movement, flexibility, and strength through targeted exercises and stretches. For many patients, physical therapy can help alleviate chronic pain associated with musculoskeletal issues like back pain, neck pain, or joint problems.
The main benefits of physical therapy include:
Pain Reduction: By improving posture and muscle function, physical therapy can reduce strain on affected areas and minimize pain.
Restoration of Function: PT can help restore mobility and function, reducing the need for long-term pain medication.
Education and Prevention: Physical therapists educate patients on proper body mechanics and ergonomics to avoid future injury and pain.
Elmhurst is home to a number of physical therapy clinics that specialize in treating various types of pain, from sports injuries to post-surgical recovery.
3. Chiropractic Care
Chiropractors in Elmhurst focus on diagnosing and treating musculoskeletal disorders, particularly those involving the spine. Chiropractic adjustments involve hands-on manipulation of the spine and other joints to reduce pain and improve function. This approach can be effective for conditions like:
Lower back pain
Neck pain
Headaches
Sciatica
Chiropractic care often complements other treatments like physical therapy and medication, providing a holistic approach to pain management.
4. Interventional Pain Management
For individuals experiencing persistent pain, particularly chronic or neuropathic pain, interventional pain management elmhurst techniques may be recommended. These minimally invasive procedures are typically performed by specialists such as anesthesiologists, pain management physicians, or orthopedic surgeons. Some common procedures include:
Epidural Steroid Injections: Often used to treat conditions like sciatica or herniated discs, these injections deliver steroids directly to the inflamed area of the spine to reduce pain and inflammation.
Facet Joint Injections: These are used to treat pain in the joints of the spine, commonly due to arthritis or injury. The injection delivers medication directly to the joint to reduce inflammation and pain.
Nerve Blocks: These injections target specific nerves to block pain signals from reaching the brain, often used for neuropathic pain or after surgery.
Radiofrequency Ablation: This procedure uses heat to destroy nerve fibers that are transmitting pain signals. It can be especially helpful for conditions like chronic back pain or arthritis.
Advanced Pain Management Techniques
1. Regenerative Medicine
Regenerative medicine is an innovative field that uses the body’s own healing mechanisms to repair damaged tissues and relieve pain. This includes treatments like:
Platelet-Rich Plasma (PRP) Therapy: This involves drawing a patient’s blood, concentrating the platelets, and injecting them into the painful area to promote healing. It is often used for joint pain, tendon injuries, and osteoarthritis.
Stem Cell Therapy: Stem cells have the ability to regenerate damaged tissues. In pain management, stem cell therapy can help repair cartilage in the joints, alleviate degenerative diseases, and promote healing in areas like the spine or knees.
Both PRP therapy and stem cell treatments are available in Elmhurst through specialized pain clinics and orthopedic practices.
2. TENS (Transcutaneous Electrical Nerve Stimulation)
TENS is a non-invasive method of pain relief that involves using electrical impulses to stimulate the nerves. This can help block pain signals from reaching the brain and stimulate the release of endorphins, the body’s natural painkillers. TENS units are available for at-home use, and many patients find them effective for managing chronic pain, especially for conditions like arthritis and muscle pain.
3. Cognitive Behavioral Therapy (CBT) for Pain
Pain management isn’t only about treating the physical aspect; the emotional and psychological factors also play a significant role. Cognitive Behavioral Therapy (CBT) is a form of psychotherapy that helps patients change their negative thought patterns and behaviors related to pain. This can improve coping strategies, reduce anxiety, and help patients manage chronic pain more effectively.
In Elmhurst, several mental health professionals specialize in CBT for pain management. By addressing the psychological components of pain, CBT can lead to a more comprehensive and effective treatment plan.
Complementary and Alternative Therapies
Alongside conventional treatments, many Elmhurst residents also seek complementary and alternative therapies to manage pain. These therapies often focus on holistic approaches to healing.
1. Acupuncture
Acupuncture is an ancient Chinese practice that involves inserting thin needles into specific points on the body to stimulate the flow of energy (or "qi"). It is often used to manage chronic pain, particularly for conditions like headaches, back pain, and osteoarthritis. Many patients in Elmhurst turn to acupuncture as an adjunct to other treatments.
2. Massage Therapy
Massage therapy can provide relief for muscle tension, stress, and certain types of chronic pain. Whether it’s a deep tissue massage for back pain or a soothing Swedish massage for relaxation, Elmhurst has a variety of licensed massage therapists who specialize in pain relief.
3. Yoga and Meditation
Mind-body practices such as yoga and meditation can also be effective for managing pain. Yoga promotes flexibility, strength, and relaxation, while meditation helps individuals cope with the emotional aspects of chronic pain. Many local wellness centers in Elmhurst offer yoga classes specifically designed for pain management.
Conclusion
Living with pain mangement elmhurst can be challenging, but Elmhurst offers a wide range of options to help individuals manage and alleviate their discomfort. From traditional methods like medication, physical therapy, and chiropractic care to advanced treatments such as regenerative medicine and interventional procedures, residents of Elmhurst have access to comprehensive pain management solutions.
By working with healthcare professionals to tailor a treatment plan that meets individual needs, patients can significantly improve their quality of life, manage their pain effectively, and get back to doing the things they love. Whether you're dealing with acute pain from an injury or chronic pain from a long-term condition, Elmhurst has the resources and expertise to help you on your journey to recovery.
If you or a loved one are experiencing pain, consider reaching out to one of the many specialists or clinics in Elmhurst to explore the best pain management options for your specific situation.
Let's Connected Name: Orthopedic Specialists Address: 360 W Butterfield Rd # 160, Elmhurst, IL 60126, United States Phone No: +1 6307829600 Map: https://maps.app.goo.gl/zVGiG6Qcvryrokkp8
1 note
·
View note
Text
Buy Gabapentin 800 mg Online (oe 800 pill) Without Prescription
Buy Gabapentin 800mg Online (oe 800 pill) This anticonvulsant drug is used to treat nerve injury as well as other disorders causing nerve pain, such as herpes zoster nerve pain and restless legs syndrome.
https://twb.nz/buy-gabapentin-online-curecog
1 note
·
View note
Text
Gabapentin: A Calming Companion for Canine Concerns

Gabapentin, often referred to by its brand name Neurontin, is a medication that has found a valuable place in veterinary medicine. While not specifically designed for dogs, its effectiveness in managing various conditions has made it a go-to for many veterinarians. Let's dive into the world of Gabapentin, understanding its uses, side effects, and how it can benefit your furry friend.
What is Gabapentin, and How Does it Work?
Gabapentin is primarily an anticonvulsant medication, originally developed to treat seizures in humans. However, its uses have expanded, and it's now commonly prescribed for dogs to manage a range of conditions. While the exact mechanism isn't fully understood, it's believed to work by blocking certain nerve signals in the brain, which can help alleviate pain, anxiety, and seizures.
Why Do Dogs Take Gabapentin?
Gabapentin has become a versatile tool in a veterinarian's arsenal. Here are some common reasons why it might be prescribed for your dog:
Seizure Management: For dogs with epilepsy or seizure disorders, Gabapentin can help reduce the frequency and severity of seizures when used in conjunction with other medications.
Pain Relief: Gabapentin can be effective in managing chronic pain, particularly nerve pain associated with conditions like arthritis, intervertebral disc disease (IVDD), and cancer.
Anxiety Reduction: Whether it's fear of thunderstorms, separation anxiety, or general nervousness, Gabapentin can help calm anxious dogs and reduce their stress levels.
Post-Operative Pain: After surgeries, Gabapentin can be used to help manage pain and discomfort, allowing your dog a smoother recovery.
Common Side Effects and Considerations:
Like any medication, Gabapentin can have side effects. The most common ones include drowsiness, loss of appetite, and vomiting. While these side effects are usually mild and temporary, it's essential to monitor your dog closely for any unusual changes in behavior or health.
It's crucial to remember that Gabapentin is a prescription medication. Never administer it to your dog without consulting your veterinarian. They will determine the appropriate dosage, frequency, and duration of treatment based on your dog's specific condition and needs.
Gabapentin and Your Dog's Overall Health
While Gabapentin can be a valuable tool in managing various conditions, it's essential to view it as part of a comprehensive healthcare plan. Your veterinarian will likely recommend additional treatments or lifestyle adjustments to address the underlying cause of your dog's discomfort or anxiety. Regular check-ups and open communication with your vet are key to ensuring your dog's overall well-being.
A Note on Caution:
It's important to emphasize that Gabapentin is not a magic cure-all. While it can be effective in managing certain conditions, it's not suitable for every dog or every situation. Always consult your veterinarian to determine if Gabapentin is the right choice for your furry friend.
The Bottom Line
Gabapentin has proven to be a valuable asset in veterinary medicine, offering relief for a range of canine ailments. By understanding its uses, potential side effects, and proper administration, you can work with your veterinarian to determine if it's the right choice for your dog's specific needs. Remember, open communication and regular check-ups are key to ensuring your furry friend's health and happiness.
Doxycycline: A Canine Cure-All?

Doxycycline, often referred to by its brand names like Vibramycin or Monodox, is an antibiotic that's become a staple in the veterinary world. It's like a versatile tool in a vet's kit, tackling a wide range of bacterial infections in our furry friends. Let's dive into the world of doxycycline, understanding its uses, potential side effects, and why it's become a go-to for many canine ailments.
What is Doxycycline and How Does it Work?
Doxycycline belongs to a family of antibiotics called tetracyclines. It works by stopping the growth of bacteria, giving your dog's immune system a chance to fight off the infection. It's like calling in reinforcements to help your pup's body win the battle against pesky bugs.
Why Would My Dog Need Doxycycline?
Your vet might prescribe doxycycline for a variety of reasons. Here are some common uses:
Tick-Borne Illnesses: It's a go-to treatment for tick-borne diseases like Lyme disease, ehrlichiosis, and anaplasmosis.
Urinary Tract Infections: Doxycycline can help clear up those pesky UTIs that can make your pup uncomfortable.
Skin Infections: Whether it's a hot spot or a general skin infection, doxycycline can help target the bacteria causing the problem.
Dental Disease: It's often used to treat periodontal disease, helping to manage the bacteria that cause gum inflammation.
Other Infections: Doxycycline can also be used to treat a variety of other bacterial infections, such as respiratory infections and those affecting the reproductive system.
Side Effects and Cautions
Like most medications, doxycycline can have side effects. The most common include upset stomach, vomiting, and diarrhea. While these are usually mild, it's important to monitor your dog closely.
Doxycycline can also interact with other medications, so it's crucial to inform your vet about any other drugs your dog is taking. Additionally, it can cause sensitivity to sunlight, so limiting prolonged sun exposure might be a good idea.
It's important to remember that doxycycline should only be used under the guidance of a veterinarian. Never administer medication without consulting your vet first.
Doxycycline and Your Dog's Overall Health
While doxycycline is a powerful tool in fighting bacterial infections, it's not a magic cure-all. It's essential to address the underlying cause of the infection, whether it's a tick-infested environment or poor dental hygiene. Your vet will work with you to create a comprehensive treatment plan.
Remember, antibiotics can disrupt the natural balance of bacteria in your dog's body. This can sometimes lead to secondary infections like yeast infections. Always consult with your vet if you notice any unusual symptoms after your dog finishes the medication.
A Final Note
Doxycycline is a valuable tool in your pet's healthcare arsenal. When used correctly and under veterinary guidance, it can effectively treat a range of bacterial infections. However, it's not a substitute for preventive care, such as regular vet check-ups, vaccinations, and flea and tick prevention. By partnering with your vet and providing your furry friend with a healthy environment, you can help keep them happy and healthy.
Tramadol: A Pain Reliever for Our Pawed Pals

Tramadol, a medication often used to manage moderate to moderately severe pain in humans, has found its place in veterinary medicine as well. While not specifically designed for dogs, its pain-relieving properties have made it a valuable tool in managing discomfort in our furry friends. Let's dive into the world of Tramadol, understanding its uses, potential side effects, and how it can benefit your dog.
What is Tramadol, and How Does it Work?
Tramadol is classified as an opioid analgesic, meaning it works on the central nervous system to reduce pain perception. It's different from traditional opioids like morphine because it also affects the levels of serotonin and norepinephrine, neurotransmitters that influence mood and pain sensation. This dual action contributes to its effectiveness in managing pain.
Why Would My Dog Need Tramadol?
Your vet might prescribe Tramadol for a variety of reasons, including:
Post-Surgical Pain: After surgeries, Tramadol can help manage discomfort and promote a smoother recovery.
Chronic Pain: Conditions like arthritis or hip dysplasia can cause persistent pain. Tramadol can provide relief and improve your dog's quality of life.
Acute Pain: Injuries like broken bones or soft tissue damage might require short-term pain management with Tramadol.
Side Effects and Cautions
Like any medication, Tramadol can have side effects. Common ones include nausea, vomiting, constipation, and drowsiness. While these are usually mild, it's important to monitor your dog closely.
In some dogs, Tramadol can cause excitement or agitation instead of sedation. This is less common but worth watching out for.
It's crucial to remember that Tramadol should only be administered under the guidance of a veterinarian. Never give your dog any medication without consulting your vet first.
Tramadol and Your Dog's Overall Health
While Tramadol can be a valuable tool in managing pain, it's essential to address the underlying cause. Your vet will likely recommend additional treatments or lifestyle changes to improve your dog's overall health and reduce discomfort.
Also, keep in mind that Tramadol can interact with other medications, so it's crucial to inform your vet about any other drugs your dog is taking.
The Bottom Line
Tramadol can be a helpful medication for managing pain in dogs when used appropriately. It's essential to work closely with your veterinarian to determine if it's the right choice for your furry friend. Remember, it's not a miracle cure, and addressing the underlying cause of pain is crucial for long-term relief.
0 notes