#it might be a change in headmates but its happening like everyday at the same time so
Text
Terrible thing that's been happening to me lately: all day, I'm tired all day, feel like I'm gonna fall asleep watching my usual shows, have to almost force myself to be awake. But the minute the sun goes down, I have all the energy in the world, I feel like I could kill God. All the tiredness from the day is suddenly gone and I have trouble getting to sleep. Fuck this gay earth, frfr
2 notes
·
View notes
Text
Dissociative Disorders 101
In this post, I'm going to give an outline of Dissociative identity disorder (DID) and Other Specified Dissociative disorder (OSDD).
These two disorders are terribly misunderstood due to horrible representation in media, a lack of education on the topic. Many people still refer DID as Multiple Personality Disorder (MPD) an outdated term from when DID was classified as a personality disorder, we now know the disorder is better seen as a dissociative disorder. I hope this post will help clear up misunderstandings about these topics.
[CW: Mentions of abuse, medical trauma, war, human tracking, suicide, self-harm, and addiction. All of these are briefly mention and not discussed in detail. Ableism is the only cw discussed in detail]
[Note: This post is not to be used as a diagnostic tool.]
DID & OSDD Glossary:
Alter: Shorthand for alternate personality or alternate identity. The most common language to refer to the multiple identities in the system. You may also see the terms "parts" & "headmates".
Alter jobs: also called “Alter types” or “Alter Roles”. This refers to the common occurrence of certain alters taking on specific roles. This often happens because to some extent DID & OSDD acts as extreme involuntary coping skills. Examples of this are protectors who deal with danger, caretakers who help keep the alters in the system comforted, or trauma holders who retain memories of trauma.
Co-Consciousness: often shortened to co-con. When two or more alter are aware of the outside together. Thoughts of both alters can often blend together. Even at times alters may have split control of the body.
Depersonalization and Derealization: Often shortened to DR/DP. DR/DP disorder is its own diagnosis but those with other dissociative disorders experience it as well. Depersonalization the feeling of oneself is not real or is heavily disconnected from the body. This can even result in one of feeling in control of limbs at all. Derealization is the feeling of the outside world not being real, or a simulation.
Fronting: The act of being the alter conscious at the time and ability to interact with the outside world.
Host: Either the person believed to be the “first” personality (sometimes called the core or original) or the latter who fronts the most.
Splitting: In this case, it refers to when new alters form.
System: A word used to reference all of the alters as a whole. Used like "I am an alter in a system" or sometimes “ I am a system”. Rather someone uses this term is a matter of personal preference, and if they see themselves as part of a system or collectively are a system.
What is Dissociation?
Dissociation refers to the mechanism our brain has to disconnect us from our surroundings sometimes as a benign reaction but severe dissociation is associated with trauma and other mental illnesses.
Every Person has the capacity for dissociation and many experiences some degree of the skill like when you drive home but don’t remember it. However daydreaming in class, spacing out every now again is healthy, there is a huge difference between those experiences and those of people with dissociative disorders.
Dissociation is primarily associated with DID but can also be a symptom of C-PTSD, Borderline Personality Disorder (BPD) and some forms of psychosis. There are also physiological conditions that cause and/or mimic dissociation. Like seizures and migraines.
What are the symptoms of DID & OSDD?
[Disclaimer: I’m aware that the DSM is a flawed way to look at mental health, but it is the best way we have to ensure all parties are working with the same definition of terms]
DID:
DID diagnostic criteria are as follows:
1)Two distinct identity states are present. They have to be separate and able to act autonomy. It isn’t “feeling” like another person.
2)Amnesia must occur, defined as gaps in the recall of everyday events, important personal information and/or traumatic events
3)The person must be distressed by the disorder or have trouble functioning in one or more major life areas because of the disorder. This criterion is common among all serious mental illness diagnoses as a diagnosis is not appropriate where the symptoms do not create distress and/or trouble functioning.
4)The disturbance is not part of normal cultural or religious practices.
This DID criterion is to eliminate diagnosis in cultures or situations where multiplicity is appropriate. An example of this is in children where an imaginary friend is not necessarily indicative of mental illness.
5) The symptoms are not due to the direct physiological effects of a substance
So what does that mean? It means that those who have the disorder have at least one alter the hallmark of DID. Alter come in all kinds of varied types and versions. The amnesia criterion does refer to forgetting traumatic events, but also incidents in normal life.
Alters themselves are a complex they aren’t "alter egos or" made up people. Alters can be almost anything, children (younger than the body) adult alters (older than the body), alters based on fiction called Fictional introjects (fictives for short), alters who are angels or spirits, ghost alters, animal alters, alters of varying race and sexualities. This is because alters form to ensure the survival of the child, this includes alters to comfort, protect, soothe and hold trauma away from the wider consciousness. This means that anything that can fill that role can be put into an alter. There is no control over alters, they are not imaginary friends or malleable they are the best way the mind had to survive.
In day to day life DID might look like having missing time, experience dissociation even when in control, a sense of not having an identity, hearing voices within their heads (not auditory hallucinations), meeting people you feel like you should know, having actions you took but have no recollection of, overlapping emotions and trouble focusing.
People with DID have high rates of self-harm, suicidal behaviour, addiction, disordered eating and other behaviours that cause damage to oneself. This is often even more distressing as one might hurt themselves and not remember it because an alter did it.
Those with DID will also often have what is referred to as “Inner worlds” or “headspace” this refers to in the mind of the person there is a mental world within. This is a place where alters have a form, body and voice within the mind. It is often a combination of a coping skill used as a kid to escape and a way to be able to interact with others alters. Headspaces often are where alters feel they are when not fronting. It also provides a way of seeing where alters who are not in communication with others are, and can sometimes serve as a visual connection to understanding the others in the system and understand trauma.
Somatic symptoms are really common, Including: Headaches, nausea and vomiting, Non-epileptic seizure/psychogenic seizures, blurred vision, muscle aches, nerve dysfunction (like dysautonomia), fatigue, other feelings of illness. This is sometimes part of conversion disorder.
People with DID & OSDD almost always also have (C-)PTSD. So symptoms like hypervigilance, nightmares, and flashbacks. As they have DID & OSDD and have experienced trauma they likely have symptoms from that other than dissociation, even if they do not meet PTSD criteria.
BPD has high comorbidity with DID, many people with DID or OSDD are misdiagnosed with BPD. Other common comorbid conditions include Anxiety Disorders, Depression, Eating Disorders, and Conversion Disorder.
OSDD:
So the thing about OSDD is a category of conditions that don’t fit another diagnosis. With this post, we are mostly concerned with OSDD-1a and OSDD-1b because those disorders are most similar to DID and form systems.
The DSM Description is as follows:
This category applies to presentations in which symptoms characteristic of a dissociative disorder that cause clinically significant distress or impairment in social, occupational, or other important areas of functioning predominate but do not meet the full criteria for any of the disorders in the dissociative disorders diagnostic class. The other specified dissociative disorder category is used in situations in which the clinician chooses to specify the reason that the presentation does not meet the criteria for any specific dissociative disorder. This is done by recording "other specified dissociative disorder" followed by the specific reason (e.g., "dissociative trance"). Example presentations that can be specified using the "other specified" designation include the following:
1. Chronic and recurrent syndromes of mixed dissociative symptoms. This category includes identity disturbance associated with less than marked discontinuities in sense of self and agency, or alterations of identity or episodes of possession in an individual who reports no dissociative amnesia.
2. Identity disturbance due to prolonged and intense coercive persuasion: Individuals who have been subjected to intense coercive persuasion (e.g., brainwashing, thought reform, indoctrination while captive, torture, long-term political imprisonment, recruitment by sects/cults or by terror organizations) may present with prolonged changes in, or conscious questions of, their identity.
3. Acute dissociative reactions to stressful events: This category is for acute, transient conditions that typically last less than 1 month, and sometimes only a few hours or days. These conditions are characterized by constriction of consciousness; depersonalization; derealization; perceptual disturbances (e.g., time slowing, macropsia); micro-amnesias; transient stupor; and/or alterations in sensory-motor functioning (e.g., analgesia, paralysis).
4. Dissociative trance: This condition is characterized by an acute narrowing or complete loss of awareness of immediate surroundings that manifest as profound unresponsiveness or insensitivity to environmental stimuli. May be accompanied by minor stereotyped behaviours of which the individual is unaware and/or that he or she cannot control, as well as transient paralysis or loss of consciousness. The dissociative trance is not a normal part of a broadly accepted collective cultural or religious practice.
Those with OSDD-1a&b meet most but not all of DID criterion. They are considered Complex Dissociative Disorders along with DID.
OSDD-1a is either identity disturbance with less distinct alters than DID (they cannot physically take executive control over the person's body, but strongly influence the person's thoughts and actions with this type there is amnesia.
OSDD-1b does have distinct alter do exist and can take executive control with the type there is no amnesia.
How does DID or OSDD Develop?
DID & OSDD comes from long term childhood trauma. When a child is exposed to long term trauma and the identity of the child cannot properly integrate. This means your brain put up amnesic barriers to memories and perception forming the separate identity states.
DID is highly correlated with sexual abuse, physical abuse, medical trauma, living in a war zone, child trafficking, and Ritual abuse. Another key factor in a child developing these disorder is the lack of healthy attachment (more info here) You can not develop this disorder after age 9, you can't develop it from a single trauma.
The most current theory used to understand how these disorders works are Structural Dissociation. It refers to the way our brain changes the usual structure to compensate for traumatic experiences. It also posits that a child is not born with an integrated personality, to begin with, and this what allows the extreme dissociative symptoms of DID to manifest.
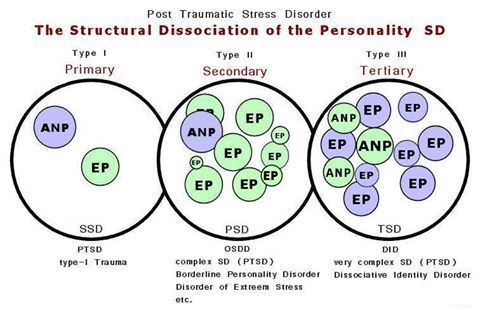
(Image Source)
ANP refers to “Apparently Normal Part” (someone who takes care of daily life)
EP refers to “Emotional part” (someone who holds trauma memories, reactions, and/or sensations).
Primary SD: is found among those with PTSD. The EP holds all trauma associated things such as fight or flight, feelings, sensations, etc, and is not a fully differentiated being (such as alters are/can be in DID and OSDD-1)
Secondary SD is OSDD, complex PTSD, and BPD. OSDD-1 has the most developed EPs out of the secondary SD disorders. BPD and C-PTSD EPs are less developed than OSDD-1 and are fragments (less fragmented than fragments found in OSDD-1 and DID). Secondary SD emotional parts hold less trauma-related material than the single EP found in PTSD. While the EP in PTSD will hold all of the trauma, there may be an EP in the secondary SD category for an emotion related to the traumas, another for body memories, another for visual memories and auditory memories in some of the traumas, and so on.
Secondary SD is OSDD, PTSD, and BPD. OSDD-1 has the most developed EPs out of the secondary SD disorders. BPD and C-PTSD EPs are less developed than OSDD-1 and are fragments (less fragmented than fragments found in OSDD-1 and DID). Secondary SD emotional parts hold less trauma-related material than the single EP found in PTSD. While the EP in PTSD will hold all of the trauma, there may be an EP in the secondary SD category for an emotion related to the traumas, another for body memories, another for visual memories and auditory memories in some of the traumas, and so on.
Tertiary SD refers to DID. There are multiple ANP and multiple EP. They are more developed than the ANP and the EPs in Secondary structural dissociation (though DID parts can have the same degree of development as OSDD-1 parts and vice versa). EPs can be “small”, as in less developed and would be considered fragments, as they hold limited trauma material such as a single feeling or one or two of the senses in a few trauma memories (or just one or two of the senses in one trauma memory). EPs can also be a fully developed part, such as an ANP would be, but hold trauma material. Multiple ANPs exist and can have various jobs associated with daily life such as a school part, a work part, a caretaker part, etc.
This theory is one of the most widely accepted concepts of how alters form and best matches most people's experience. It does contradict the idea that alters are split pieces of one cohesive identity being split the old model.
Another thing to keep in mind about this theory is it shows the structure and function of the brain are altered from a young age. Brains conditioned to dissociate during stress and trauma will continue to split during stress. This means alters can continue to form in those with DID & OSDD past age 9.
This Video explains further how this relates to alters splitting
Treatment:
DID & OSDD can be treated and worked on so the person is no longer experiencing the adverse effects or usually lessen them. Treating DID works mostly the same way as any other trauma survivor. Most kinds of trauma therapy can be used, EMDR being the exception. Certain kinds of meditation and visualisation also prove to be not as effective.
Medication can be used to treat comorbid disorders like depression or anxiety but there are no pharmacological treatments for DID on its own.
What is unique about DID is there is the aspect of how the alters affect you. With DID & OSDD time spent with, alters is crucial. Helping alters who are struggling with trauma becomes deeply important in healing.
The two main options with alters are integration or communication.
Integration refers to a process of when two identity states fuse together. This means you have less altered consciousness states, it also relates to them both being able to handle their trauma. The goal here is to end up with the patient having a singular integrated identity.
The other treatment focuses on forming functional working relationships with the altar and helping them process trauma individually, integration might still happen but a singular identity is not the end goal.
Mythbusting:
“People with DID are just psychotic or delusional” False, psychosis is not a feature of DID or OSDD and has been shown to act completely differently for the person and in the brain than psychosis. This is also offensive as it denigrates people with psychosis.
“DID is fake/made up by a therapist/ social contagion/the person only believes they have alters” False: DID has been observed in multiple studies and social contagion, malingering and therapist coercion are no longer prime theories. People saying this often bring up the false memory scare and Sybil. Both of those have been proven to be wildly overstated and are not the only evidence we have. There are cases dating back to the 1500s with the first psychiatric observations in the 1800s.
“Aren’t they dangerous?” or “they're so scary and crazy!” or “Don’t they need to be locked up” False, The real facts are people with dissociative disorders don’t commit violence at a higher rate than anyone else. They are much more likely to be the victims of violence. Starting with the fact they faced violence as a child to even have the disorder.
“Isn't that possession?” or any other spiritual concepts. False, There is nothing supernatural reasons for DID. Some people have spiritual or religious beliefs that change how they personally perceive their condition, but there is nothing supernatural about DID or OSDD.
“It’s super rare” Not actually the estimate for DID is about 1% of the population. Might sound small but with the number of people in the US alone who have, it means you're likely to meet someone with it.
“I would know if you had it” Not likely. Most people with DID present with covert DID. These people do not have alters who act wildly different from the host. Generally alters will attempt to not show obvious signs as well as being n the same mind with similar physiological aspects and upbringing influence things like mannerisms. Only 5-6% of people with DID have an overt presentation. Even these people are unlikely to be able to wildly change the way they dress and the like as it’s impractical.
“Bad alters/evil alters/violent alters/murder alters” False. There are often alters who might feel aggressive or be persecutors who hurt the other alters. But they are not going to commit murder or rape. They are usually more dangerous to the person with the disorder than anyone outside. And this anger usually stems from trauma.
“You can’t have the disorder you wouldn’t know” and other variations on “Crazy people don't know their cray”. False usually people with DID reach out to help themselves they don’t get forced into it. Because the symptoms of DID disrupt life and the usual comorbid PTSD or other mental health conditions. People with DID are also often aware to some extent of their alters. Rather this is voices, time gaps, or passive influence. And people who have known about the disorder and are in treatment often have good communication between alters in the mind, they are definitely aware of their health.
I Hope this is helpful for those with and without the disorder to better understand these conditions. My personal experience with DID does mean I’m particularly passionate about education on this topic even more as it intersects with education about trauma in general. I hope this didn’t come off as adversarial and helps people learn.
-Admin 1
{Resources: Structural Dissociation Explained, OSDD Diagnostic Material, The Fantasy Theory of DID, New Models of DID, DID Literature Review, DID Research.org, DSM Library, Webermann, A. R. & Brand, B. L. (2017). Mental illness and violent behaviour: The role of dissociation. Borderline Personality Disorder and Emotion Dysregulation}
#blog post#mental illness#mental health resources#mental health education#mental illness education#dissociative identity disorder#did#other specified dissociative disorder#osdd#osdd1#multiple personality disorder#mpd#dissociative disorder#dissociatvie disorders#dissociation#childhood trauma#structural dissociation#bpd#cptsd#ptsd#disordered eating#long post
39 notes
·
View notes