#pelvic inflammatory diseases
Text

In recent times, the incorporation of CA 125 into comprehensive full-body health examinations has gained popularity as part of a proactive approach to monitoring overall well-being. While CA 125 is well-known for its association with ovarian cancer, its inclusion in broader health assessments extends its usefulness beyond specific cancer screenings.
1. Early Detection of Gynecological Cancers: One of the primary advantages of integrating CA 125 into full-body health checkups is the potential for early identification of gynecological cancers. Elevated CA 125 levels may not only suggest ovarian cancer but also act as an alert for other gynecological malignancies like endometrial or fallopian tube cancers. This holistic approach enhances the likelihood of detecting these cancers in their early stages, enabling timely intervention and improving treatment outcomes.
2. Monitoring Reproductive Health: Beyond cancer detection, CA 125 plays a role in monitoring reproductive health. For women facing conditions such as endometriosis or pelvic inflammatory disease, heightened CA 125 levels could offer valuable insights into the health of reproductive organs. Regular inclusion of CA 125 in health checkups enables a more comprehensive assessment of reproductive well-being, aiding in the early identification of reproductive health issues.
3. Indirect Indications of Inflammation and Other Conditions: CA 125 is not exclusive to gynecological concerns; its elevation can also be linked to inflammatory conditions and other noncancerous health issues. Including CA 125 in full-body health checkups provides a broader perspective on inflammation within the body, potentially indicating underlying health conditions such as liver disease or inflammatory disorders. This indirect insight enhances the diagnostic value of a full-body health assessment.
4. Holistic Approach to Cancer Prevention: Comprehensive health checkups aim to offer a holistic view of an individual's health, and the inclusion of CA 125 aligns with this goal. By monitoring CA 125 levels alongside other health parameters, healthcare professionals can adopt a holistic approach to cancer prevention. Identifying potential risk factors early allows for tailored preventive measures, such as lifestyle modifications and targeted screenings, contributing to an individualized healthcare strategy.
5. Psychological Well-being and Patient Empowerment: The incorporation of CA 125 in full-body health checkups not only serves clinical purposes but also contributes to psychological well-being. For individuals with a family history of ovarian cancer or other gynecological conditions, the regular monitoring of CA 125 levels provides a sense of empowerment and control over their health. Knowledge and early detection empower individuals to actively engage in their healthcare journey.
6. Collaborative Care and Informed Decision-Making: Collaboration between patients and healthcare providers is crucial for effective healthcare. Including CA 125 in full-body health checkups fosters a collaborative approach to care. Informed decision-making becomes possible as patients and healthcare professionals work together to interpret CA 125 results in the context of overall health, allowing for more personalized and targeted healthcare interventions.
7. Research and Advancements: The integration of CA 125 into full-body health checkups contributes to ongoing research and advancements in the field. The data collected from these comprehensive assessments, including CA 125 levels, can inform research on the interplay between biomarkers, overall health, and specific conditions. This continuous feedback loop supports the evolution of healthcare practices and diagnostic strategies.
There are many good hospitals in Bangalore that offer health checkup packages for females and include CA 125 test, such as a full body health checkup at Manipal Hospital Sarjapur Road in Bangalore.
#CA 125#cancer screening#gynecological cancer#reproductive health#ovarian cancer#endometriosis#pelvic inflammatory diseases#cancer prevention#biomarkers#full body health checkups#regular health checkups#health checkup packages
0 notes
Text
A pelvic ache, that lasts six months or more, usually occurs in the space between the hips and beneath the belly button. Pelvic pain, which throbs beneath your belly button, can cause disturbances in your life and leave you in search of solutions. It can range in intensity from a dull aching to a severe stab.
1 note
·
View note
Text
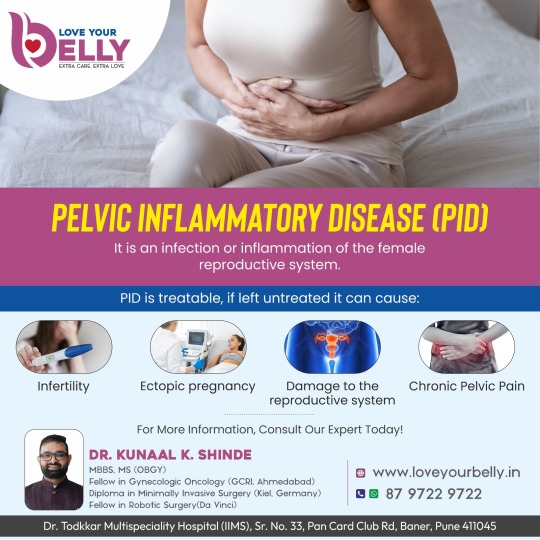
PELVIC INFLAMMATORY DISEASE (PID) - Dr. Kunaal Shinde
Pelvic Inflammatory Disease (PID) is an infection treatable infection of the female reproductive system. Left untreated, PID can cause serious health problems, including infertility, ectopic pregnancy, and chronic pelvic pain. Take control of your health. Get the information you need and talk to an expert today.
For More Information, Consult Our Expert Today!
For more information
☎ Call: 87 9722 9722
✅ Book An Appointment:
#Pelvic Inflammatory Disease#Pelvic Inflammatory Disease treatment Baner#Infertility Specialist in Baner#Pune#Infertility Specialist#Gynecologist in Baner#Best Gynecologist in Baner#Laparoscopic Surgeon in Pune#Laparoscopic specialist in Pune#Gynaec Laparoscopic Surgeon in Pune#Best Gynaec Laparoscopic Surgeon in Pune#Laparoscopic surgeon & Robotic surgeon in Pune
1 note
·
View note
Text
Complications from untreated PID can take many years to develop. The resulting problems can be painful. They can also cause permanent damage to the reproductive organs. Complications can even lead to infertility. The longer a woman has untreated PID, the greater the chance that these problems will occur.
0 notes
Text

Indications for Hysterectomy:
1. Uterine Fibroids:
• Uterine fibroids, noncancerous growths within the uterus, exhibit a range of symptoms affecting daily life. Hysterectomy is contemplated when these fibroids are substantial, symptomatic, or unresponsive to alternative interventions.
2. Endometriosis:
• The mysterious condition of endometriosis, marked by tissue growth outside the uterus, presents challenges to fertility and daily function. Hysterectomy, often a last resort, can bring relief in severe or recurrent cases, addressing the underlying issue.
3. Uterine Cancer:
• Hysterectomy plays a crucial role in the treatment of uterine cancer, offering a definitive measure by removing cancerous tissue and contributing to improved survival rates.
4. Chronic Pelvic Pain:
• Debilitating chronic pelvic pain prompts consideration of hysterectomy when other interventions prove inadequate. The decision involves a thorough evaluation of the pain's origin and its impact on overall well-being.
5. Uterine Prolapse:
• Uterine prolapse, a result of weakened pelvic floor support, may require hysterectomy when conservative measures fall short. This surgical intervention aims to restore anatomical integrity and alleviate associated discomfort.
6. Abnormal Uterine Bleeding:
• Complex abnormal uterine bleeding brings hysterectomy into focus when other treatments are ineffective or the bleeding poses significant health risks. The decision is tailored to the specific circumstances and health considerations.
7. Pelvic Inflammatory Disease (PID):
• In cases of severe or recurrent PID, where infection and inflammation impact the uterus and surrounding reproductive organs, hysterectomy may be considered as a therapeutic intervention to alleviate chronic symptoms and prevent further complications.
Follow-up care following a hysterectomy includes a regular full body health checkup to check the success of the procedure and its long-term effect on the health of the patient.
#full body health checkup#regular health checkups#uterine fibroids#uterine cancer#endometriosis#pelvic pain#uterine prolapse#abnormal uterine bleeding#pelvic inflammatory disease
0 notes
Text
Pelvic Inflammatory Disease

Pelvic inflammatory disease (PID) is an infection that occurs in your uterus, fallopian tubes or ovaries. Sexually transmitted infections typically cause it. Symptoms include stomach, lower abdominal pain and vaginal discharge. Prompt PID treatment, usually antibiotics, helps avoid complications such as infertility. Your partner should get tested and treated, too.
Each year, more than 1 million women and people AFAB in the U.S. get PID. And more than 100,000 people become infertile because of it. PID occurs most frequently in women and people AFAB between 15 and 25 years old.
SYMPTOMS AND CAUSES
Symptoms might be mild or unnoticeable. But symptoms of PID can also start suddenly. They can include:
Pain or tenderness in your stomach or lower abdomen (belly), the most common symptom.
Abnormal vaginal discharge, usually yellow or green with an unusual odour.
Chills or fever.
Nausea and vomiting.
Pain during sex.
Burning when you pee.
Irregular periods or having spotting or cramping throughout the month.
Causes pelvic inflammatory disease
Sexually transmitted infections (STIs)
The main cause of PID is through a sexually transmitted infection (STI) such as chlamydia, gonorrhoea or mycoplasma genitalium.
These bacteria usually only infect the cervix, where they can be easily treated with antibiotics.
But if they’re not treated there’s a risk the bacteria could travel into the female reproductive organs.
If you have chlamydia and it’s left untreated, it may develop into PID within a year.
Other causes of PID
In many cases, the cause of the infection that leads to PID is unknown.
Sometimes, the usually harmless bacteria found in the vagina can get past the cervix and into the reproductive organs.
Although harmless in the vagina, these types of bacteria can cause infection in other parts of the body.
This is most likely to happen if:
You have had PID before
There’s been damage to the cervix following childbirth or a miscarriage
You have a procedure that involves opening the cervix (such as an abortion, inspection of the womb, or insertion of an intrauterine device.
Which areas can become infected?
If an infection spreads upwards from the vagina and cervix, it can cause inflammation of the:
Womb lining (endometrium)
Fallopian tubes
Tissue around the womb
Ovaries
Lining of the inside of the abdomen (peritoneum)
Pockets of infected fluid called abscesses can also develop in the ovaries and fallopian tubes.
Who’s most at risk?
Anyone with female reproductive organs can get PID, but you’re more likely to get it if you:
Have more than 1 sexual partner
Have a new sexual partner
Have a history of STIs
Have had PID in the past
Are under 25
Started having sex at a young age
1 note
·
View note
Text
What Is Pelvic Inflammatory Disease? - Women Ob-Gyn Associates
PID is an infection of the reproductive organs. Left untreated, it can cause severe damage to the body. PID sometimes causes symptoms bad enough to send you to the emergency room. But in many cases, PID is a "silent" infection with few or no symptoms. Rest assured that the infection can be treated. This can help prevent lasting damage. http://www.womenobgynassociates.com/health-library/diseases-and-conditions/382205/pelvic-inflammatory-disease-what-is
0 notes
Text
Colorectal surgeon is a specially qualified doctor to treat conditions of Colon, rectum and anal
canal. Following general surgery they do 3 year Specialization in surgical gastroenterology. After
that they do fellowship in colorectal surgery.
They study extensively about colon and rectum, so they are very knowledgeable about colorectal
diseases.
Colorectal surgeons practice the full range of endoscopic and surgical techniques for treating your
GI tract. That means they have all the available tools at their disposal to treat complex conditions.
They are very skillful at minimally invasive (Laparoscopic and Robotic) surgeries.
Not all lower GI conditions need surgical treatment, but when they do, it’s helpful to see a specialist
colorectal surgeon.
Colorectal conditions that are likely to require surgery include:
Colon and Rectal Cancers
Inflammatory Bowel Diseases
Pelvic floor disorders
Diverticulitis
Author :- Dr Avadh Patel
MS, DrNB Surgical Gastroenterologist & Colo-Rectal Surgeon
Kaizen Hospital
0 notes
Text
Pelvic inflammatory disease (PID) cause infertility and chronic pelvic pain
Pelvic inflammatory disease (PID) is a medical condition that involves inflammation of the fallopian tubes and ovaries. This condition can be caused by various bacterial infections, with chlamydia and gonorrhea being the most common culprits. However, other bacteria found in the digestive tract or those responsible for bacterial vaginosis may also lead to PID.
The inflammation caused by this…
View On WordPress
0 notes
Text
Female reproductive health terms you should know!
(terfs not welcome)
Dysmenorrhea: Period pain that isn't normal, i.e. any pain more than Mild cramping.
Dyspareunia: painful intercourse
Oligomenorrhea: lighter, shorter menstrual flow.
Menorrhagia: heavier, longer menstrual flow.
Ovarian cysts: a mass on or in one's ovary, can be resolved on its own, or can remain and cause complications such as a rupture.
Polycystic ovary syndrome: a chronic condition causing cysts to reoccur on the ovaries and enlarging them. Symptoms include:
Irregular periods
hormonal imbalance
facial hair
weight gain
painful periods/ ovulation
infertility
People with PCOS are at higher risk for endometrial cancer, type II diabetes heart problems and high blood pressure.
Endometriosis: A chronic condition in which a tissue similar to, but different than, the endometrial lining grows outside of the uterus instead of inside. During menstruation this tissue sheds and has nowhere to go, thus irritating surrounding organs.
Symptoms include:
Irregular periods
Dysmenorrhea
Widespread pain
Painful ovulation
Vomiting, fainting, chills, sweating, fever and brain fog during menstruation
Infertility
Severe bloating
This also puts people at a higher risk for endometrial and ovarian cancer. There are four stages to Endo as it is a progressive disease, with 3/4 being more severe. The average time it takes to be diagnosed is 7 years.
Adenomyosis: A chronic disease similar and comorbid to endometriosis in which a tissue similar to the endometrial lining grows inside of the uterine wall. Symptoms are nearly identical to endometriosis but more difficult to detect.
Many people are diagnosed post menopause, by fault of the medical system, but it can and does develop much before then.
Ovarian cancer: cancer of the ovary(ies).
Endometrial cancer: cancer of the endometrium, the inner lining of the uterus.
Endometrial cyst, or chocolate cyst: cystic lesions from endometriosis.
Tilted uterus: the uterus is positioned pointing towards the back or severely to the front of the pelvis instead of a slight tilt towards at the cervix. Can cause painful sex and periods.
Pelvic floor dysfunction: inability to control your pelvic muscles. Comorbid with many things and is highly comorbid with endometriosis. Can cause pain and incontinence.
Vulvodynia: chronic and unexplained pain at the opening of the vagina.
Interstitial cystitis: a chronic condition where cysts form on the inside of the bladder and urinary tract and cause symptoms similar to that of a UTI.
Pre-eclampsia: a condition occurring in pregnancy where the blood supply between the fetus and the pregnant person is affected and can cause irregular blood pressure, swelling, and in more severe cases headache, nausea and vomiting, a burning sensation behind the sternum, shortness of breath and potentially death if untreated.
Endometritis: an infection or irritation of the uterine lining. Is not the same as endometriosis and is treatable but can cause pain, bleeding, swelling, general discomfort and fever, and more.
Pelvic inflammatory disease: an infection of the reproductive organs
Ectopic pregnancy: a pregnancy that is attached to the outside of the uterus. Can be fatal if left untreated.
There are many more I could probably add but if you see something missing, please add it!
#reproductive health#endometriosis#adenomyosis#pcos awareness#reproductive health awareness#chronic illness#polycystic ovarian syndrome#ovarian cancer#reproductive rights
219 notes
·
View notes
Note
Hi Sex Witch!
Idk if this is something you would know or not, but when doctors ask about “pain during sex” what does that mean exactly? Because sometimes(not every time, but more than frequent enough to make the connection) when I have sex/use penetration to get off, I get like. Really bad cramping 1-8 hours later. Nothing feels different about the act itself from when it does happen to when it doesn’t, but it happens id say like 70%+ of the time?
I’m just not sure how to even start to talk to someone about it, and all results for searches are showing for pain *during* sex which isn’t a problem for me, unless this counts?
hi anon,
at risk of sounding like a shit, "pain during sex" refers to pain occurring during the act of sex, especially during penetration. cramping up hours after the fact is generally considered something different, and could have a variety of causes.
it's possible that the muscles in your pelvic floor just going a little too bananas with the muscles spasms. very small contractions in the pelvic floor are a normal reaction to sexual stimuli, and are in fact what cause an orgasm. but those muscles are also the same ones that cramp up during menstruation, and sometimes after sex they can go into overdrive and refuse to stop cramping to the point of pain, and if that's the case then I would recommend nothing more complicated than painkillers and a heating pad.
however, there are also a lot of other causes of post-sex pain that are more serious, including ovarian cysts, pelvic inflammatory disease, endometriosis, fibroids, and having a tilted uterus. if the usual care for cramps isn't cutting it, I'd definitely recommend looking into some of those conditions to see if they line up with your experiences and then consulting with a healthcare provider.
25 notes
·
View notes
Note
Question for you. How do you feel about the one CEO saying Endometriosis isn't a gynaecological condition? I mean it technically is, isn't it?
https://news.yahoo.com/trans-ceo-charity-founder-says-210134975.html?.tsrc=daily_mail&uh_test=0_00
Oy vay, what now, lol. Gonna use my psychic powers to say we're entering a world of equality where women can have prostate cancer as well.
Gonna tl:dr at the end
Endometriosis is not a gynaecological condition, the founder of a charity supporting women with the disease has suggested, after appointing a transgender woman as its chief executive.
Jodie Hughes, the founder of Endometriosis South Coast, recently appointed Steph Richards, a trans woman and activist, as chief executive.
Ms Hughes told BBC Woman’s Hour on Wednesday that referring to the disease as a “gynaecological disorder” may be the reason medical research into the issue has not progressed further.
Endometriosis causes tissue similar to the lining of the uterus to grow outside of the womb, often causing severe pelvic pain. It can also affect fertility.
Another charity, Endometriosis UK, describes it as “the second most common gynaecological condition in the UK”. It affects around 1.5 million women in the country.
Appearing on the BBC programme alongside Ms Richards, Ms Hughes said: “Endometriosis is a systemic inflammatory condition. We need to move away from the gynaecological side of things because you don’t have to be born with a womb to have it.”
She also claimed endometriosis is “not a reproductive disorder”, adding: “It’s being seen as a gynaecological disorder maybe is the reason why the past 200 years research and medicine isn’t progressing.”
Ms Richards, 71, whose appointment drew criticism from some women’s groups, was asked on the programme if she could fully represent women with endometriosis when she previously had not used the word “woman” to describe those suffering from disease.
She said she was “happy” to use the word but did not want to ignore how endometriosis could also affect trans men and non-binary people.
Men diagnosed
Ms Richards also claimed that endometriosis was not only seen in women because 29 men had been recorded as being diagnosed with the disease.
“I look at women but I also look at the issue of trans men and non-binary people. There’s something like 5,500 trans men who had endometriosis who probably feel rather left out and also non-binary people,” Ms Hughes said.
The charity faced a backlash this week after appointing Ms Richards to the role.
Helen Joyce, director of advocacy at Sex Matters, told The Telegraph: “Endometriosis is a disorder that involves cells from the womb lining finding their way to other parts of a woman’s anatomy, and it can cause infertility.
“So, of course, it’s a women’s reproductive issue; it’s absurd and offensive to the many female sufferers of this debilitating condition to say otherwise. Yes, women who identify as men or non-binary can have the disease – how you identify obviously doesn’t change your biology. And, yes, there are a handful of cases in the literature where biological men suffer from something similar, but these are ultra-rare exceptions.”
Ms Joyce said that Ms Hughes’ remarks suggesting endometriosis should not be framed as a gynaecological issue were “offensive”.
“Endometriosis is poorly understood and researched precisely because it only affects women and our reproductive systems. This is part of the systemic lack of research and funding for “women’s issues”.
“The answer is for the medical profession to step up and do more for women – not to rebrand women’s disease by pretending they also affect men. People can’t in reality change sex, and men won’t start suffering from endometriosis even if we pretend people can change sex (and no man should want this disease; it’s horrific).”
_________________________________
This entire article is lunacy.
For the first bit it's a gynecological condition because it's people with uterus's that get it
Endometriosis causes tissue similar to the lining of the uterus to grow outside of the womb, often causing severe pelvic pain. It can also affect fertility.
until they get the uterus transplant thing down this is something that will hit AFAB people and telling transmen this also almost sounds like telling them they don't need to go to a gynecologist to me.
It's not sexist or transphobic to say you need a gynocoligist if you have, vulva, vagina, uterus, cervex, fallopian tubes, ovaries and any bits I didn't mention, they're the doctors that specialize in those body parts
I'm very trans positive and supportive, this woman is an idiot however, and people are going to get hurt as a result of her being an idiot if she keeps going with this shit.
If you have a uterus you can get endometriosis.
If you have a uterus you go to a gynecologist to get those bits looked at, you can pull the gender away and be fine with it, gynecologist is a doctor that works on parts that 50% (or so) of the human population have.
Issues dealing with those bits are gynecological issues, make it gender neutral in your head if you need to.
We're getting dangerously close to a trans woman threatening to sue an oncologist because he said she has prostate cancer.
TL:DR; whole thing is insanity and will wind up killing people if they don't knock it off, you can call it whatever you want to call it but don't tell the professionals they're wrong on this one.
if it's a job for a OBGYN then it's a gynecological issue
36 notes
·
View notes
Text
“Regina Roe,” 23 (USA 1972–1978)
“Regina” had multiple pre-existing risk factors before the legal abortion that took her life. She was obese and had recently suffered PID (pelvic inflammatory disease). In addition, the study that recorded Regina’s death noted that based on the data they were able to collect, Black women like her were over three times more likely to die from a second-trimester surgical abortion than a white woman.
Regina underwent the D&E abortion (colloquially known as a dismemberment abortion) at 13 weeks pregnant in a hospital. In theory, the hospital was supposed to have the equipment to save her life. However, even the resources of the hospital wouldn’t save her once the abortionist perforated her uterus and left parts of her baby and/or the placenta rotting inside of her body.
Because of the uterine perforation and incomplete abortion, Regina developed peritonitis and went into septic shock. The infection and injuries killed her. A “safe and legal” abortion made her oldest child an only child, and then took away their mother.
(Regina Roe is Case 2)
#tw abortion#pro life#unsafe yet legal#tw ab*rtion#tw murder#unidentified victim#victims of roe#black lives matter#abortion#abortion debate#death from legal abortion#tw malpractice#tw negligence#tw death
6 notes
·
View notes
Text
𝘼-𝙕 𝙇𝙄𝙎𝙏 𝙊𝙁 𝘿𝙄𝙎𝙀𝘼𝙎𝙀𝙎/𝙄𝙇𝙇𝙉𝙀𝙎𝙎𝙀𝙎 𝙁𝙊𝙍 𝙎𝙄𝘾𝙆𝙁𝙄𝘾/𝙒𝙃𝙐𝙈𝙋
— A
Anemia.
Adenomyosis.
Asthma.
Arterial thrombosis.
Allergies.
Anxiety.
Angel toxicosis ( fictional ).
Acne.
Anorexia nervosa.
Anthrax.
Atma virus ( fictional ).
ADHD.
Agoraphobia.
Astrocytoma.
AIDS.
— B
Breast cancer.
Bunions.
Borderline personality disorder.
Botulism.
Barrett's esophagus.
Bowel polyps.
Brucellosis.
Bipolar disorder.
Bronchitis.
Bacterial vaginosis.
Binge eating disorder.
— C
Crohn's disease.
Conjunctivitis.
Coronavirus disease.
Coeliac disease.
Chronic migranes.
Coup.
Cushing syndrome.
Cystic fibrosis.
Cellulitis.
Coma.
Cooties ( fictional ).
COPD.
Chickenpox.
Cholera.
Cerebral palsy.
Chlamydia.
Constipation.
Cancer.
Common cold.
Chronic pain.
— D
Diabetes.
Dyslexia.
Dissociative identify disorder.
Dengue fever.
Delirium.
Deep vein thrombosis.
Dementia.
Dysthimia.
Diphtheria.
Diarrhoea.
Disruptive mood dysregulation disorder.
Dyspraxia.
Dehydration.
— E
Ebola.
Endometriosis.
Epilepsy.
E-coli.
Ectopic pregnancy.
Enuresis.
Erectile dysfunction.
Exzema.
— F
Fusobacterium infection.
Filariasis.
Fibromyalgia.
Fascioliasis.
Fever.
Food poisoning.
Fatal familial insomnia.
— G
Gonorrhoea.
Ganser syndrome.
Gas gangrene.
Giardiasis.
Gastroesophageal reflux disease.
Gall stones.
Glandular fever.
Greyscale ( fictional ).
Glanders.
— H
Hookworm infection.
Hand, foot and mouth disease.
Hypoglycaemia.
Herpes.
Headache.
Hanahaki disease ( fictional ).
Hyperhidrosis.
Heat stroke.
Heat exhaustion.
Heart failure.
High blood pressure.
Human papillomavirus infection.
Hypersomnia.
HIV.
Heart failure.
Hay fever.
Hepatitis.
Hemorrhoids.
— I
Influenza.
Iron deficiency anemia.
Indigestion.
Inflammatory bowel disease.
Insomnia.
Irritable bowel syndrome.
Intercranial hypertension.
Impetigo.
— K
Keratitis.
Kidney stones.
Kidney infection.
Kawasaki disease.
Kaposi's sarcoma.
— L
Lyme disease.
Lassa fever.
Low blood pressure.
Lupus.
Lactose intolerance.
Lymphatic filariasis.
Leprosy.
— M
Measles.
Mad cow disease.
Mumps.
Major depressive disorder.
Malaria.
Malnutrition.
Motor neurone disease.
Mutism.
Mouth ulcer.
Monkeypox.
Multiple sclerosis.
Meningitis.
Menopause.
Mycetoma.
— N
Norovirus.
Nipah virus infection.
Narcolepsy.
Nosebleed.
Nocardiosis.
— O
Obsessive-compulsive disorder.
Osteoporosis.
Ovarian cyst.
Overactive thyroid.
Oral thrush.
Otitis externa.
— P
Pancreatic cancer.
Pneumonia.
Pelvic inflammatory disease.
PICA.
Premenstrual dysphoric disorder.
Psoriasis.
Parkinson's disease.
Panic disorder.
Polycystic ovarian syndrome.
Plague.
Postpartum depression.
Pediculosis capitis.
Psychosis.
Post-traumatic stress disorder.
— Q
Q fever.
Quintan fever.
— R
Rubella.
Rabbit fever.
Rotavirus infection.
Ringworm.
Restless legs syndrome.
Rhinovirus infection.
Rosacea.
Relapsing fever.
Rheumatoid arthritis.
Rabies.
— S
Shingles.
Sore throat.
Stutter.
Separation anxiety disorder.
Smallpox.
Scoliosis.
Septic shock.
Shigellosis.
Sepsis.
Social anxiety disorder.
Stroke.
Scarlet fever.
Schizophrenia.
Sleep apnea.
Sun burn.
Syphilis.
Sickle cell disease.
Scabies.
Selective mutism.
Salmonella.
Sensory processing disorder.
— T
Thyroid cancer.
Tuberculosis.
Thirst.
Trichuriasis.
Tinea pedis.
Tourette's syndrome.
Trachoma.
Tetanus.
Toxic shock syndrome.
Tinnitus.
Thyroid disease.
Typhus fever.
Tonsillitis.
Thrush.
— U
Urinary tract infection.
Underactive thyroid.
— V
Valley fever.
Vertigo.
Vomiting.
— W
White piedra.
Withdrawal.
Whooping cough.
West nile fever.
— X
Xerophthalmia.
— Y
Yersiniosis.
Yellow fever.
— Z
Zygomycosis.
Zika fever.
Zeaspora.
19 notes
·
View notes
Text

Embracing Self-Love: The Health Benefits of Female Self-Pleasure
In a world where open conversations about sexuality are increasingly encouraged, it's essential to recognize that self-love and self-pleasure play a significant role in a woman's overall well-being. While societal taboos have often shrouded the topic, it's time to shed light on the numerous health benefits of female self-pleasure.
Stress Relief
One of the most immediate and noticeable benefits of self-pleasure is stress relief. Engaging in self-pleasure triggers the release of endorphins and oxytocin, commonly known as "feel-good" hormones. These chemicals promote relaxation and reduce stress, helping women unwind after a long day.
Improved Sleep
For those struggling with sleep disorders or insomnia, self-pleasure can be a natural remedy. The release of endorphins during orgasm can induce a sense of calm and relaxation, making it easier to fall asleep and enjoy a restful night.
Enhanced Mood
Regular self-pleasure can help balance mood swings by regulating hormones. It's an effective way to combat anxiety and depression, fostering a sense of well-being and happiness.
Improved Pelvic Health
Engaging in self-pleasure helps strengthen the pelvic floor muscles, which can contribute to better bladder control and sexual satisfaction. lt can also reduce the risk of pelvic inflammatory diseases and urinary tract infections.
Increased Libido
Exploring one's body through self-pleasure can lead to a better understanding of one's desires and preferences. This increased self-awareness often translates into a higher libido
and more fulfilling sexual experiences with a partner.
Better Body lmage
Self-pleasure can promote a positive body image by fostering self-acceptance and self-love. It encourages women to embrace their bodies, which can lead to improved self-confidence in all aspects of life.
Hormonal Balance
Regular self-pleasure can help regulate hormonal fluctuations, particularly during the menstrual cycle. lt may reduce the severity of PMS (Premenstrual Syndrome) symptoms and create a smoother transition through the ups and downs of hormonal changes. By engaging in self-pleasure, women can potentially mitigate mood swings, irritability, and discomfort associated with hormonal fluctuations, allowing for a more harmonious and balanced emotional state throughout the month.
23 notes
·
View notes
