#abnormal uterine bleeding
Text
PAP is screening only, not indicated in work up of post-menopausal bleeding
General EMStripe <4 is <1% for endometrial cancer
>4mm then EMBiopsy is indicated
Polps with cancer can be missed on EMB
Therefore remove since you can't guarantee it's not cancer
Other special cases
Tamoxifen (1% increased cancer risk). Uterus looks odd on US, need to do a sonohystogram and Hysteroscopy
Recurrent episodes -> Go to biopsy
Risk factors (Consider biopsy)
Risk Factors for early menopause
Smoking #1 risk factor for early menopause
Null parity
Family history
Chemotherapy
Causes of PMB - > generally do the full work up, assess for cancer, don't stop at vaginal atrophy
Uterine Atrophy
Very thin lining, can be unstable (lack of estrogen)
Exacerbated by blood thinners
Most common etiology with "negative" work up
Uterine Atrophy
Loss of rugation, frail skin, dysparenuia, speckled (bursting of blood vessels)
Consider
Uterine track atrophy
Urethral Caruncles, diverticulae
Tx vaginal estrogen (esterase cream preferred), capsules, rings (lasts 90 days, not great if sexually active, but good if already using a Pessary and/or have recurrent UTIs)
4mg imvexxy (Lowest estrogen dose)
Nightly for 2 weeks, then night twice a week
Assess at 2-3 months
Endometrial polyps
Proliferative
Carcinoma/Hyperplasia
Risk- Increasing age, nulliparity, obesity, increased estrogen exposure, tamoxifen
EIN -> Send to GYN/Onc for biopsy on follow up
Simple Hyperplasia
Stop estrogen, weight loss (obesity),
Pre-cancerous
Treat with local progesterone therapy (Merina IUD) /or monitor /or biopsy
"you don't have to do anything, but it sucks to watch someone get cancer"
Fibroid
3-5% chance of malignancy in the post-menopausal women
If US negative, get saline infusion sonohysterogram (In office), saves the women from Hysteroscopy (In OR)(Go right to this if concern for cancer)
Other
HRT
Pessary
Injury
Prolapse/ulceration
Silver nitrate, estrogen, pessary (or surgery)
Non-GYN Causes of PMB
Hematuria
Hemorrhoids
Hematochezia
Excoriations
2 notes
·
View notes
Text

Indications for Hysterectomy:
1. Uterine Fibroids:
• Uterine fibroids, noncancerous growths within the uterus, exhibit a range of symptoms affecting daily life. Hysterectomy is contemplated when these fibroids are substantial, symptomatic, or unresponsive to alternative interventions.
2. Endometriosis:
• The mysterious condition of endometriosis, marked by tissue growth outside the uterus, presents challenges to fertility and daily function. Hysterectomy, often a last resort, can bring relief in severe or recurrent cases, addressing the underlying issue.
3. Uterine Cancer:
• Hysterectomy plays a crucial role in the treatment of uterine cancer, offering a definitive measure by removing cancerous tissue and contributing to improved survival rates.
4. Chronic Pelvic Pain:
• Debilitating chronic pelvic pain prompts consideration of hysterectomy when other interventions prove inadequate. The decision involves a thorough evaluation of the pain's origin and its impact on overall well-being.
5. Uterine Prolapse:
• Uterine prolapse, a result of weakened pelvic floor support, may require hysterectomy when conservative measures fall short. This surgical intervention aims to restore anatomical integrity and alleviate associated discomfort.
6. Abnormal Uterine Bleeding:
• Complex abnormal uterine bleeding brings hysterectomy into focus when other treatments are ineffective or the bleeding poses significant health risks. The decision is tailored to the specific circumstances and health considerations.
7. Pelvic Inflammatory Disease (PID):
• In cases of severe or recurrent PID, where infection and inflammation impact the uterus and surrounding reproductive organs, hysterectomy may be considered as a therapeutic intervention to alleviate chronic symptoms and prevent further complications.
Follow-up care following a hysterectomy includes a regular full body health checkup to check the success of the procedure and its long-term effect on the health of the patient.
#full body health checkup#regular health checkups#uterine fibroids#uterine cancer#endometriosis#pelvic pain#uterine prolapse#abnormal uterine bleeding#pelvic inflammatory disease
0 notes
Text
How is abnormal uterine bleeding diagnosed?
A menstrual period occurs when the tissue that lines the inside of the uterus, call the endometrium, begins to break down. Most woman find that normal periods are easy to deal other women are not so lucky.
Some women need to use both tampons and pads at the same time, change pads hourly, pass large clots or experiencing flooding, have to change bed sheets, underwear and clothes regularly due to overflow. They may experience extreme fatigue, weakness and shortness of breath. This is not normal.
If your menstrual flow is not easy to control, affecting your quality of life, necessitating you taking time of work or being afraid to leave home it is a problem and worth getting looked at. Learn More
1 note
·
View note
Text
Understanding Dysfunctional Uterine Bleeding: A Guide for Women Aged 20-50
As a woman, experiencing abnormal uterine bleeding can be a distressing and uncomfortable experience. Dysfunctional uterine bleeding (DUB) is a common cause of abnormal uterine bleeding in women of reproductive age. In this blog post, we will provide you with a comprehensive guide to understanding DUB, including its causes, symptoms, and treatment options.
Photo by Pixabay on Pexels.com
What is…

View On WordPress
#abnormal uterine bleeding#DUB#dysfunctional uterine bleeding#Menstrual cramping#Pelvic pain#uterine bleeding#vaginal bleeding
0 notes
Text
sometimes I don’t realise how alarming some of my symptoms are then my flatmate texts me this and I can’t even recollect how I missed cleaning all my blood ; I feel guilty 😔

4 notes
·
View notes
Text
How Stress and Lifestyle Factors Contribute to Abnormal Uterine Bleeding?
Abnormal uterine bleeding (AUB) is a frequent concern experienced by many women. It can be a source of discomfort and concern, particularly when it occurs unexpectedly or more frequently than normal. One surprising yet significant cause of AUB is stress and lifestyle factors, which many overlook. In this article, we will explore how stress and lifestyle choices contribute to abnormal uterine bleeding and what you can do to manage it.
Understanding Abnormal Uterine Bleeding (AUB)
Abnormal uterine bleeding refers to any deviation from a normal menstrual cycle, including unusually heavy periods, spotting between periods, or irregular cycle lengths. A typical menstrual cycle lasts between 24-38 days, with bleeding lasting about 4-7 days. Any pattern that falls outside of this range can be considered abnormal. AUB can occur due to several reasons, including hormonal imbalances, reproductive health issues, and external factors like stress and lifestyle choices.
Common Symptoms of AUB
Heavy or prolonged menstrual bleeding
Bleeding between periods
Irregular menstrual cycles
Spotting after intercourse
Shorter or longer menstrual cycles
The Role of Stress and Lifestyle in AUB
While many factors can contribute to AUB, stress and lifestyle choices play a crucial role. Let’s break down how:
Stress
Chronic stress affects your body in many ways, and one of the systems most impacted is the reproductive system. High levels of stress disrupt the balance of hormones, particularly those responsible for regulating the menstrual cycle (estrogen and progesterone). When your body is under constant stress, it may trigger irregular periods, heavy bleeding, or skipped periods entirely.
Lifestyle Factors
Certain lifestyle habits can also contribute to AUB. These include:
Poor Diet: Diets high in processed foods, sugar, and unhealthy fats can lead to hormonal imbalances.
Lack of Exercise: Physical inactivity can cause weight gain, which in turn affects estrogen levels and menstrual health.
Sleep Deprivation: Not getting enough sleep can lead to stress and hormonal disruptions, affecting your menstrual cycle.
Excessive Alcohol or Caffeine: These substances can have a negative effect on hormonal balance, potentially contributing to irregular bleeding.
How to Identify and Manage AUB Due to Stress and Lifestyle
It is important to note that stress and lifestyle factors alone may not be the only causes of AUB, but they are significant contributors. To effectively manage and treat AUB, it’s crucial to consult with a healthcare professional who specializes in reproductive health. You can easily reach out to abnormal uterine bleeding doctors in India or book an appointment with the best obstetrics gynecologists online consultation services for expert guidance.
Ways to Manage Stress and Lifestyle-Induced AUB

Why You Should Take Action Now
If you’ve been experiencing irregular menstrual cycles, heavy bleeding, or spotting and think stress or lifestyle factors may be to blame, it’s important to address these issues promptly. Overlooking these symptoms may result in more serious health issues. In many cases, managing stress and making lifestyle changes can significantly reduce AUB. However, it is essential to rule out any underlying medical conditions by consulting with a healthcare professional.
Action Steps:
Consult a DoctorThe first step is to consult with a specialist who can provide you with a diagnosis and personalized treatment plan. You can book the best online doctor consultation or consult with abnormal uterine bleeding doctors in India for expert advice.
Lifestyle AdjustmentsBegin by adding healthy habits to your everyday routine. From regular exercise to a balanced diet, these changes can help manage stress and hormonal imbalances.
Routine CheckupsSchedule routine health checkups to monitor your reproductive health. You can now access the best obstetrics gynecologists online consultation in India to receive 24/7 medical support without leaving your home.
Conclusion
Stress and lifestyle factors play a significant role in abnormal uterine bleeding, and addressing these elements can greatly improve your reproductive health. By understanding the impact of your daily habits and seeking timely medical advice, you can manage AUB effectively.
0 notes
Text
#gynecologist in nyc#best obgyn nyc#nyc gyn#best gynecologist nyc#gynecologist manhattan#obgyn manhattan#abnormal uterine bleeding specialist nyc#abnormal uterine bleeding specialist
0 notes
Text

It’s 740 in the morning and I’m sitting outside, feeling a migraine coming in. I went here so I can drink my ordered coffee from Bo’s because our water boiler is broken. I’m feeling woozy because my patient is co-managed so I don’t have to do anything. She is cared for by OB JIs, currently ongoing blood transfusion, and her case is abnormal uterine bleeding. She will be transferred to ward once BT is done. There’s no thrill, and Doc L is not here teaching, so my body is currently chilling in parasympathetic mode. Currently I’m dreading tomorrow, tonight, where I have to be separated from my family so I can train in RMC.
6 months into clerkship, I feel closer with everyone. I’m not too serious with studying, although of course, I study. Because we need to study so we can save more lives. But being with everyone, staying close with everyone, the daily excitement of being with each other and caring for each other is unparallel. It’s the people I work with, my future colleagues, that make all this bearable.
And tomorrow, we go to the real battle in a public hospital where I expect no less than 10,000 steps a day. A public hospital where we will be having our Christmas together, with our dutymates and patients, not with our family. I’m dreading it but I’m also excited. For the learnings, for the time to pass, for all the funny moments that will happen amidst the battle/storm.
But for now, I’ll continue drinking my cappuccino and monitor the patients now in CCU. Duty during Christmas is challenging because one of our patients wants to go home. He cried saying he wants to go home, but he couldn’t, because he is hypotensive post-op and we need to monitor him closely. It breaks our heart. All we can do is give comfort through words.
#studyspo#studyblr#study#studycommunity#bujo#desk#productivity#bookblr#bullet journal#notebook#tbhstudying#adelinestudiess#myhonestudyblr#notebookist#noodledesk#stuhde#lawyerd
90 notes
·
View notes
Text
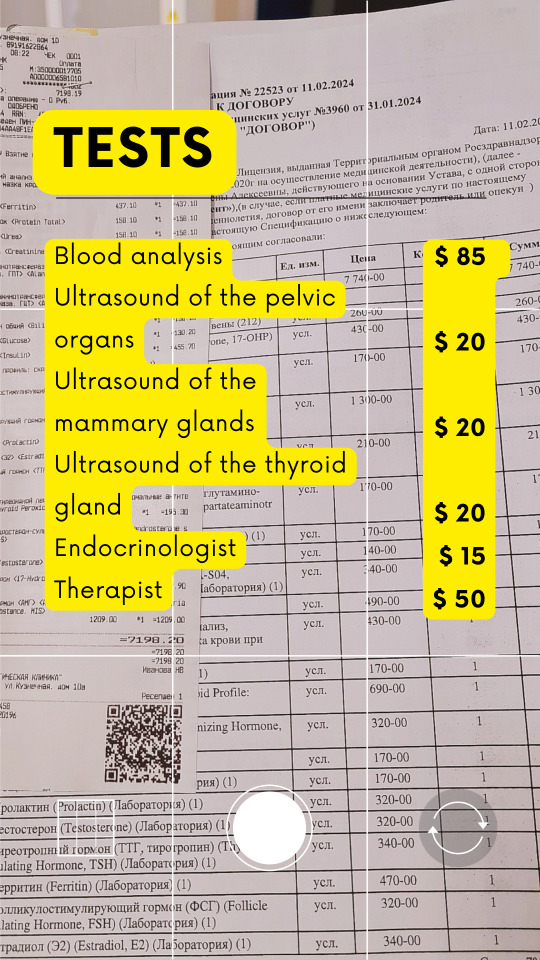
Hello everyone! ˗ˏˋ 🍓 ˎˊ˗ I think, many of you have noticed my absense in art by now. Ever since the last surgery it's been a series of unfortunate events, including a temporary relapse. For the last two months I've been suffering from Abnormal uterine bleeding (AUB)
Loss of blood, pains, nausea, dizziness. These can all point to both something harmless and endometriosis/cancer. I must take lots of tests, but it's been getting harder to work each day, can't meet the ends. Today I made blood tests for about ~$85, no money for food left.
🌡 Anything would help - stories of similar experiences, $5 coffees, even sharing this thread!
If you wish, you may donate to http://ko-fi.com/drekkydrimm Thanks everyone in advance, even if it would be just five people at most. I will be posting more updates as I progress (இ﹏இ`。)
30 notes
·
View notes
Text
Gynecology and Obstetrics Drugs Examples
Drugs for Amenorrhea and Abnormal Uterine Bleeding
-- medroxyprogesterone
-- progesterone
Drugs for Dysmenorrhea
-- ibuprofen
-- mefenamic acid
-- naproxen
Drugs for Endometriosis
-- goserelein
-- leuprolide
Drugs for Premature Labor
-- hydroxyprogesterone
Drugs for Vaginal Yeast Infections
-- clotrimazole
-- miconazole
Drugs Used to Dilate the Cervix
-- dinoprostone
Drugs Used to Induce Labor
-- oxytocin
HRT Drugs
-- conjugated estrogens
-- estradiol
Ovulation-Stimulating Drugs
-- clomiphene
-- human chorionic gonadotropin
.
Patreon
#studyblr#notes#my notes#pharmacology#pharmacology notes#pharma#pharma notes#pharm#pharm notes#pharmacy#pharmacy notes#medical pharmacology#medications#medication notes#pharmacological sciences#biochemistry#chemistry#medical chemistry#medical biochemistry#health science#science#scienceblr#medblr#biological science#common medications#pharmacodynamics#pharmacokinetics#chemical agents#toxicology#med chem
8 notes
·
View notes
Photo

Abnormal uterine bleeding, once called dysfunctional uterine bleeding, is defined as bleeding that is excessive or scanty (abnormal volume), of increased or decreased length of time, has changed in regularity, or occurring outside the patient's normal menstrual cycle. The most common complaints will be of either heavy bleeding which is abnormal or of intermenstrual bleeding. The workup for this disorder is generally designed to evaluate the causes in the diagram.
Bottom Line: Abnormal uterine bleeding in a premenopausal woman should be evaluated with a pregnancy test, CBC, coagulation studies, TSH, and selected other tests based on history and physical examination (e.g., evaluate for Von Willebrand disease if coagulation studies are normal and pt has hx of frequent epistaxis).
Increased frequency and heavy periods--> patient should be evaluated with a complete blood count for hemoglobin and platelets; a serum ferritin should be obtained to evaluate iron stores. Any patient with heavy bleeding or frequent bleeding should be evaluated with a PT/PTT. If there are other signs of bleeding by history, for example, frequent epistaxis, then consideration could be made for von Willebrand disease with measurement of von Willebrand factor assuming her coagulation studies are normal. Additionally, all patients with concern for change in menstrual bleeding should be evaluated for pregnancy with a urine or blood pregnancy test.
Hormonal changes are a frequent cause of changes in menstrual bleeding and should be evaluated with a TSH at a minimum. Obesity--> consideration should be made for checking HgbA1c.
Acne, signs of terminal hair growth, and obesity--> a total testosterone should be checked as a diagnosis of hyperandrogenism could also be considered.
In most women with oligomenorrhea, a serum prolactin should be checked. If the woman is older and there is concern for premature ovarian insufficiency, then a serum FSH can be sent as well.
Imaging is not immediately necessary in a premenopausal woman with no structural abnormalities detected on exam but should be considered if the workup is otherwise unremarkable and the bleeding is not able to be controlled or corrected with appropriate therapy. Transvaginal ultrasound is generally considered the first line imaging test. If some kind of intracavitary pathology is suspected such as a uterine polyp, then hysteroscopy or saline ultrasonography may be required.
1 note
·
View note
Text
I've not been able to figure out why I've just not felt well enough to do very much (except to binge-play Fallout 76 and now Once Human, but I swear to fuck it's because I get to build bases/houses, which is the most fun thing ever--and we can blame The Sims for getting me into that obsession, thank you very much!!).
But, now I have answers at last.
And that answer is.... endometrial carcinoma. Which is a fancy way of saying uterine cancer.
Fuck cancer.
But, BUT, despite the abnormal bleeding events lasting 3 years, and then becoming especially bad in the past few months, I am very, very, very fucking fortunate that it is 'low grade' and that the surgeons believe it's most likely limited to the uterine lining!
So what's next? First, an MRI to do official "staging" and plotting the best path for the hysterectomy to follow. I knew a hysterectomy would happen anyway based on what they found, but I only found out today the "what" is cancer (again, fuck you cancer).
If all goes as expected (currently), then it will be: MRI, hysterectomy, and finally no more cancer.
Obviously things could change when they get in there. But, I am being optimistic and hopeful that the surgery will be the whole of it, and then I can get on with recovery and feeling more human than I've felt in recent times.
Anyway, I'm going to busy myself with my slow-but-in-progress plans of tidying up some fanfics I want to repost, and doing the equally as slow work on figuring what the fuck I'm doing with my original stories because a lot are blending together and I continually get myself confused - which is no help whatsoever lol
Also I really, really want to get back into gif making as I've been thinking of so many that I want to redo, and others that I've never done and figured could be fun. Mostly it's Sanrion AU's, Rachel/Joey and Rumbelle. And I'm fine with that, as they're my happy space right now!
4 notes
·
View notes
Text
I'm just kind of dreading this hysterectomy. Which I know is usually standard for surgeries but it's not really the surgery itself. I mean, I'm really dreading the pain afterwards, of course because I know people who have had it and it's apparently agony. But it's just that I don't really care about what this surgery is doing all that much.
I know for a fact the abnormal uterine bleeding is another symptom of the same thing that causes my fatigue, not the cause. Which just means getting rid of it makes the real issue that much harder to get treated. I'm not even bothered by the bleeding that much. It's a mild inconvenience amid a bunch of life destroying debilitations that this surgery is more likely to make worse than improve.
And I really think if I was just on levothyroxine again, the abnormal bleeding would go away. Because that's what happened last time I started on levothyroxine. Now the effects of any treatment are going to be less apparent and the only symptom anyone cared enough to do anything about will go away and the rest will all be invisible, for the most part.
I know it's good to get this surgery because it means I won't be able to get cervical cancer. But without being sexually active and never planning to become so, the chances of me getting that was next to nothing anyway.
It just feels like so many possible complications and weeks and weeks of painful recovery for a surgery I wouldn't need if I just got back on the medicine I've been begging to be put back on.
And I know there's so many people who would kill to be able to get this surgery but it just feels like so much suffering for a reward I don't even care about.
I don't think I really *need* this surgery. I'm just getting it because I want it. But I don't even really want it. So why am I getting it? Just because I don't *not* want it? I'm sure I'll come around to it once I don't have to deal with my period anymore. But it just feels so pointless.
13 notes
·
View notes
Text
What are the Causes of Late Periods?
A period is a natural part of a woman's life, and its arrival, or lack thereof, can be a source of curiosity or concern. While a late period might send your mind racing to pregnancy tests, there are numerous reasons why your period might be behind schedule. Let's discuss the world of menstrual cycles and explore the top causes of late periods.
Pregnancy: The Obvious One
We can't ignore the most common reason for a missed period – pregnancy. If you're sexually active and haven't used contraception, a late period could be the first sign of a bun in the oven. However, it's important to note that pregnancy tests might not be conclusive in the very early stages. For accurate results, wait at least a week after a missed period before taking a test. You can also visit or take an online consultation with our specialist doctor Geetanjali Thakur , the best Gynecologist in Karnal.

Hormonal Harmony: When Things Get Out of Sync
Our bodies are like intricate orchestras, and hormones play the lead role in regulating our menstrual cycles. When these hormones get out of sync, it can lead to a late period or even missed periods altogether. Here are some common hormonal culprits:
● Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal imbalance that affects ovulation, leading to irregular periods or their absence.
● Thyroid Issues: An overactive or underactive thyroid can disrupt hormone production, impacting your cycle.
● Birth Control: Starting, stopping, or switching birth control methods can disrupt your cycle for a few months as your body adjusts to the hormonal changes.
● Perimenopause: As you approach menopause, your estrogen levels naturally decline, leading to irregular periods or their absence.
Lifestyle Choices: Big Impact on Small Cycles
Our daily habits can significantly impact our menstrual health. Here's how some lifestyle choices can cause a late period:
● Stress: Chronic stress wreaks havoc on our hormones, including those regulating periods.
● Weight Fluctuations: Dramatic weight loss or gain can disrupt ovulation and lead to irregular periods.
● Excessive Exercise: While exercise is great for overall health, excessive workouts can put stress on your body and cause missed periods.
● Diet: Crash diets or restrictive eating habits can deprive your body of essential nutrients needed for a regular cycle.
Medical Conditions: When Other Factors Come into Play
Certain medical conditions can also affect your menstrual cycle and you should search Gynecologist dr near me and get the best solution, here are a few examples:
● Chronic illnesses: Conditions like diabetes, celiac disease, and autoimmune diseases can disrupt hormone regulation and lead to irregular periods.
● Pelvic inflammatory disease (PID): This infection of the reproductive organs can cause irregular periods.
● Uterine fibroids: These benign tumors in the uterus can sometimes cause heavy or irregular periods.
When to See a Doctor
While a late period is sometimes nothing to worry about, there are situations where it's best to consult a Gynecologist near you. Here are some red flags:
● You miss multiple periods in a row (especially if you're not pregnant or breastfeeding).
● Your periods are unusually heavy or painful.
● You experience abnormal vaginal bleeding.
● You have sudden weight loss or gain.
● You suspect you might have an underlying medical condition.
Taking Charge of Your Cycle
Understanding your menstrual cycle and its potential disruptions empowers you to make informed choices about your health. Here are some tips for keeping your cycle on track:
● Maintain a healthy weight.
● Eat a balanced diet.
● Manage stress effectively.
● Exercise regularly, but don't overdo it.
● Track your periods using a calendar or app.
● Talk openly with your doctor about any concerns.
Remember, a late period doesn't necessarily mean something is wrong. However, if you're concerned, don't hesitate to consult a Gynecologist near me. They can help you determine the cause and recommend the best course of action.
Additional Considerations
This blog post provides a general overview of common causes for late periods. It is not a substitute for professional medical advice. If you have any specific concerns about your menstrual cycle, consult your doctor for personalized guidance.
Concerned about your late period? Don't wait!
Schedule an appointment with the expert gynecologists Karnal. Our team can provide personalized guidance and address any questions you might have. Visit our website to book an appointment today!
2 notes
·
View notes
Text
0 notes
Text
Alyona Dixon, 24 (USA 2022)

Alyona with her only surviving son
On September 22, 2022, LA resident Alyona Dixon went to Planned Parenthood and was told she was 8 weeks and 5 days pregnant.
Alyona loved children and hoped one day to operate a play center, but she felt that she wasn’t ready to add another child to her family. If she had been given support and assurance, maybe she and her baby would still be alive. But according to a medical officer who later reviewed Alyona’s case, Planned Parenthood gave Alyona what they considered “appropriate counseling”, which led to her undergoing a chemical abortion. The abortionist administered mifepristone and then misoprostol as a vaginal suppository. Although it was still legal, no method involving the vaginal administration of the abortion pill has ever been approved by the FDA. The drug itself has a Black Box warning.
Only four days after her visit to Planned Parenthood, Alyona had to go the ER at Dignity Health’s Blue Diamond Hospital. She reported suffering from “sharp tower abdominal pain since yesterday.”
Blue Diamond observed that Alyona was bleeding vaginally and that she was experiencing tenderness in the right lower quadrant. Despite the recent abortion, no pelvic exam was performed. Alyona’s ultrasound was interpreted by Dr. Justin J. Puopolo, who detected ‘abnormal vascular flow between the endometrium and the myometrium at the uterine fundus could represent retained products of conception and should be correlated with the patient’s serial beta-hcg levels. Complex material within the endocervical canal could reflect an abortion in progress or blood products.”
A pelvic exam would have given Alyona’s doctors a better chance for faster intervention. Instead, after receiving pain medication, a CT scan with abnormal results and an ultrasound that showed her dead child could be rotting inside of her, Alyona was discharged and told to arrange a follow-up appointment with a gynecologist. Blue Diamond employee Dr. Maag documented “a low suspicion for septic process/systemic infection.” This was a fatal mistake.
The next day, Alyona’s symptoms were even worse. She was seen at Desert View Hospital, where Dr. Clark “documented his clinical impression as abdominal pain, vomiting and diarrhea, severe dehydration, acute renal failure, leukocytosis, sepsis, lactic acidosis, hypokalemia, sinus tachycardia, metabolic acidosis, pulseless electrical activity, respiratory failure.” She never should have been discharged from Dignity Health in such a condition.
Despite all of Desert View’s attempts to save her life, Alyona continued to deteriorate. She was transferred to Summerlin Hospital, where she spent her last hours of life.
By 3:10 AM of September 28, Alyona acutely worsened. She had to be sedated and intubated, but vomited during the intubation. After about 5 minutes, she went into “a rhythm of pulseless ventricular tachycardia then asystole then pulseless electrical activity with bradycardia.”

All attempts at resuscitation failed. Alyona Dixon was pronounced dead at 5:32 AM.
The Clark County Coroner’s Office gave her cause of death as “complications from septic abortion.” (While the term “septic abortion” has historically been used to describe sepsis after a miscarriage (such as in the infamous and typically misrepresented case of Becky Bell, who miscarried and then died of pneumonia), it can also be used to describe an abortion death such as Alyona’s.)
A lawsuit was filed on behalf of Alyona’s husband Michael and her little son Walter. The The complaint alleges that the Emergency Department physician “negligently failed to conduct a pelvic exam”… “failed to order a consult with an OB/GYN despite ALYONA’S abnormal lab results, her clinical history, and her abnormal diagnostic imaging…” “…negligently discharged ALYONA without preforming a pelvic exam and without ordering an immediate consult with an OB/GYN…” and “negligently did not have a credentialed OB/GYN on-call at the facility,” all of which were categorized as substantial factors in Alyona’s death.

Oddly enough, Planned Parenthood was not named in the lawsuit for Alyona’s wrongful death despite being the cause of the entire incident.
Alyona Dixon should still be alive today.
#justice for alyona#planned parenthood#planned parenthood kills women#abortion pill#tw abortion#unsafe yet legal#tw murder#tw ab*rtion#abortion#abortion debate#death from legal abortion#tw malpractice#tw negligence#this is chemical abortion
12 notes
·
View notes