Age 36, Trans-Woman:MtF blogging About My Journey Becoming Mira Carleen / 33 months on HRT
Don't wanna be here? Send us removal request.
Text
Vulvoplasty Research Notes
PLEASE NOTE THAT THE RESEARCH NOTES ARE COLLECTED FOR FUTURE OPPERATION AND UNDERSTANDING OF WHAT TO EXPECT BEFORE/DURING/AFTER VULVOPLASTY AT OHSU.
PLEASE NOTE THAT THIS INFORMATION CAN BE ANXIEY-INDUCING TO SOME.
-----------------------------------------------------------------------------------------------------------
WHAT IS VULVOPLASTY?
A vulvoplasty is a gender affirming genital reconstruction surgery that creates a neo-vulva from the existing genitalia. It fashions the external female genitalia but without a vaginal cavity. Depending on a few factors, this kind of surgery can have many different names, but in essence they are all the same:
Vulvoplasty
Vaginoplasty Without Cavity
Shallow / Minimal-Depth / Dimple / Limit-Depth Vaginoplasty
Cosmetic / Aesthetic Vaginoplasty
No-Depth / Zero Depth Vaginoplasty
Personally, I tend to call vulvoplasty - vaginoplasty, as my personal goal is to transition as much into a female without the addition of a uterus and ovaries (as the science hasn’t been developed to add these to the male body at this time). Calling it a vagina is logical in my mind as it affirms my gender as female. Also, most cis-females label their own reproductive organ as a ‘vagina’, including the clitoris and labia into the structure.
The outer characteristics of vulvoplasty are the same as those of vaginoplasty.
A clitoris and inner and outer labia are created, and the testicles and biological male sexual characteristics are removed and discarded.
The difference between a vulvoplasty and vaginoplasty is that a vulvoplasty provides a vaginal entrance that is up to 0 to 2 inches deep (depending on avaiable skin); whereas a vaginoplasty is usually 4-6 inches deep.
A benefit of vulvoplasty include:
1) Shorter Surgery Time (1.5 - 3 hours)
2) Shorter Inpatient Time (1 - 3 days)
3) Shorter Recovery Time (6-8 weeks)
4) No Need For Laser Hair Removal
5) No Dilation
6) Less Chance For Rectal Injury
Those seeking vulvoplasty should be aware that with no real depth, you will not be able to have penetrative sex.
-----------------------------------------------------------------------------------------------------------
HOW A VULVOPLASTY CREATES ‘TRUE’ FEMALE PARTS
This might be something that most people do not consider at first; but your new female parts will be actually true female parts (minus the uterus & ovaries). This is because all life on Earth in its earliest development begins as female.
This is why a vulvoplasty can be performed on a biological male; and why men have nipples on their chests and estrogen in their blood.
When a baby develops, the genitals are all the same; a urogenital slit bounded by periurethral folds and more laterally by labioscrotal swellings. It is only when the male chromosome activates, it causes the genitalia to develop differently. However, every masculine part to be traced to a feminine part. Dihydrotestosterone stimulates growth of the urogenital tubercle and induces fusion of the urethral folds and labial fold swelling during this critical period; it also induces differentiation of the prostate and inhibits growth of the vesicle vaginal septum, thereby preventing the development of the vagina
For example, the structure of the penis and clitoris are pretty much the same. It is an organ designed primarily to promote pleasure and reproduction. Both organs contain a nub or head that is packed with nerves.
The skin from the penis is used to form the area around the clitoris called the ‘hood’. Much of the shaft in a male is external, whereas a female contains the majority of her clitoris structure inside her body. Try to imagine anatomically that the inner labia are made of the penis’s ‘stretched’ skin, forming the foreskin at the end.
Scrotal skin contains a suture line down the center that once was the opening to the outer labia. The vaginal pouch is usually obliterated when the müllerian ducts are reabsorbed, although a vestigial blind vaginal pouch known as the prostatic utricle can sometimes be demonstrated. The prostate gland and the urethral glands of Cowper in the male are outgrowths of the urogenital sinus, in which male differentiation is mediated by dihydrotestosterone and requires the presence of androgen receptors
-----------------------------------------------------------------------------------------------------------
THE PREP / PRE-OP
Both vulvoplasty and vaginoplasty are major surgeries that are usually the last surgeries that MTF individuals have within 2-3 years on HRT.
Be aware of the following:
1) Persistent, well documented gender dysphoria diagnosis.
2) Capacity to make a fully informed decision and to consent for treatment.
3) 12 continuous months of hormone therapy
4) 12 continuous months of living in a gender role that is congruent with their gender identity.
5) Two letters from mental health therapist.
6) Nicotine Free for 10 weeks.
7) Documentation of recent A1C < 6.5% (diabetic patients only)
Pre-Surgery
At OHSU, it is scheduled to have a pre-surgery appointment one month before surgery. At this appointment, you will meet the Physician Assistant and be able to ask any questions before surgery.
You might be tested for nicotine and have blood work. A nicotine test will be performed on the day of surgery.
Stop taking estrogen 4 weeks before surgery. This is to reduce the risk of blood clots. Estrogen can be resumed a week after surgery.
Your surgical team might consist of the following people:
Primary Surgeon
Secondary Surgeon
A PA (physician assistant) Or RN
Medical assistants
Surgery scheduler
Resident physician’s
Physical therapists
Behavioral therapists
Social workers
Inpatient RN & CNA
-----------------------------------------------------------------------------------------------------------
SUPPLIES SUGGESTED
Roll fluff gauze: for surgical site absorption. Having 8-10 rolls be best.
Donut pillow or Hemorrihoid pillow for sitting: this will be important as it is almost a 4-hour drive. You can also use a u-shaped neck pillow or gel seat.
Maxi pads: to help with drainage. Larger is better as you don’t want it too tight.
Lots of toilet paper: You are likely to get messy.
Extra pairs of loose or mesh underwear: With dressing and maxi pads, your regular underwear may be too tight. You also may have some drainage that might ruin your underwear.
Stool softeners: Opioid pain medication and inactivity will likely cause some constipation. Miralax is recommended.
Ice pack: To reduce swelling, inflammation and pain.
Peri bottle: For the first few weeks after surgery, you should shower twice daily with gentle soap and water. Use your hand rather than a washcloth to clean the surgical site. Some patients find a peri bottle, designed for postpartem mothers, to be a gentle way to clean the area after surgery, in addition to showering twice daily.
Items to keep you entertained: computer, books, games, ect.
Snacks: to help ease emotional pain and use as a treat.
Items that make you comfortable: like a blanket, pillow, aromatherapy, eye pillow, ect.
Sore throat remedies: tea, chocolate, medicated spray. The trachea tube can leave behind irritation.
-----------------------------------------------------------------------------------------------------------
THE SURGERY
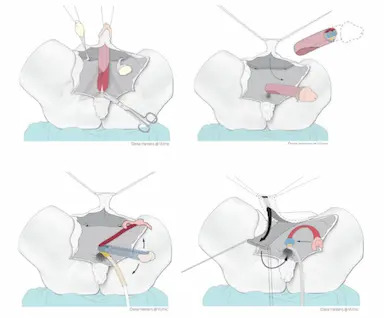
In vulvoplasty, the female genitals are created from the skin and underlying tissue of the penis. No vaginal cavity will be created. In most cases, the testicles are also removed in this operation. Be certain that you have thought about family planning before surgery.
Depending on the technique used, the operation will last anywhere from 2 to 5 hours. The operation will be performed by a plastic surgeon and/or urologist surgeon.
It starts with the insertion of a urinary catheter in the urethra.
The penile skin is removed from the shaft of the penis. The skin is shortened and sutured in order to make it look like a vagina (but without the vaginal cavity).
Then the testicles are removed, and the clitoris and inner labia are made from the glans and the foreskin. The urethra is exposed and shortened up to the new entrance.
The parts of the male genitals that will be incorporated into your new neo-vagina:
Clitoris is made out of the glans of the penis.
The outer labia are made from the scrotum.
The inner labia are made from the skin on the penis and/or urethra.
Urethra shortened and repositioned between the clitoris and vagina.
Introitus (opening of the vagina) is formed from the skin of the penis.
-----------------------------------------------------------------------------------------------------------
IMMEDIATE AFTER SURGERY & DAY 1
In accordance to OHSU Day 1 in Hospital:
After Surgery
Dr. Dy will speak with family after the surgery. Patient will be in post-anesthesia care unit for 2-3 hours for observation. It isn’t uncommon to feel nauseated (I tend to vomit after anesthesia), groggy, irritated, tearful, hungry and especially thirsty for a sore throat.
Patient will then be moved to Unit 4A (surgical unit). You will have a foley catheter in urethra, surgical packing, and drains with a collection bag. Your legs will have compression cuffs and an IV will be placed in the arm.
Medicine offered: nausea med, sore throat med, narcotic pain med, and stool softeners.
Diet: Begin with ice for sore throat. Water can be consumed in PACU. Snacks will be offered, like crackers or pudding, before the regular meal on day 2. Yogurt is advised.
Day 1
There is no strict bed rest, move as much as tolerated.
Rolling over in bed is comfortable if you do a ‘log-roll’. The bed should remain at 45 degrees or less.
Medicine Regiment: 650mg Tylenol every 6hrs. 15mg of Toradol IV every 8hrs. 5-15mg Oxycodone every 4hrs. Miralax.
No bathing, you can sponge bathe.
-----------------------------------------------------------------------------------------------------------
DAY 2
Medicine Regiment: 650mg Tylenol every 6hrs. 600mg Ibuprofen every 8hrs. 5-15mg Oxycodone every 4hrs. Miralax.
Encouraged to move around as much as possible. This will help with blood clots, maintaining your muscles, and digestion. Physical therapy suggests you do bed exercises every hour while awake.
Many patients will leave the hospital inpatient floor and go home on Day 2 with a catheter and external dressing in place. These dressings will be removed in the clinic on Day 3 or 4.
-----------------------------------------------------------------------------------------------------------
DAY 3
Medicine Regiment: 650mg Tylenol every 6hrs. 600mg Ibuprofen every 8hrs. 5-15mg Oxycodone every 4hrs. Miralax.
Today, the pressure dressing on the vulva is to be removed. Drains may be taken out today or tomorrow. Foley catheter removed. You need to try to pee without the catheter. 1-5 people find they cannot pee due to swelling, so a catheter will be placed back in. Your bladder will be scanned to see how much urine is left.
Take a shower today. User warm water, not hot! Clean ‘carefully’ all the folds and creases between your legs. Do not scrub! Do not use washcloth here!
Let the water flow over your vulva to wash away soap. Do not rub towel when drying...pat dry if possible.
Prepare for Discharge!
You and the caregivers should ask questions about anything not understood. Caregivers will pick up prescriptions before the patient leaves. Be certain to know the date of the next follow-up visit.
Transfer to the Rood Pavilion for extended stay.
-----------------------------------------------------------------------------------------------------------
RECOVERY AT ROOD
Not all hospitals offer off-campus housing, so your experience might differ. I live out of state, almost 200 miles away (4-hour commute) from OHSU; so, my care will be transferred there, giving me close access to the surgeon.
Medicine Regiment: 625mg Tylenol every 6hrs (end at first follow-up). 600mg Ibuprofen every 8hrs after taking Tylenol (end at first follow-up). 5mg Oxycodone every 6hrs PRN. 1 Lidocaine patch divided on inner tight and groin for 12hrs. Miralax. Resume your estrogen.
There is no diet restriction, however, drinking plenty of fluids is important with narcotics and flushing out the system. Miralax can be used for up to 1 month for constipation.
Try to keep your walking to 2,000 steps a day, for 4 weeks. Do not lift over 10 pounds for 4 weeks. Take stairs one at a time so you do not open sutures. Ice the mons (fatty tissue over public bone) for 20 minutes every 1-2 hours.
Be certain to rest and recover.
You will want to start using sanitary pads to collect blood from wounds.
Shower twice daily for 6 weeks after surgery. No pool or tub for 3 months! Stitches will dissolve on their own.
Appearance: Lots of swelling and bruising. To quote one trans individual, it will look gross, mutilated, or like a Frankenstein. The swelling can take many months to go down. In 6-12 months, you should start to see your vulva settling into form.
-----------------------------------------------------------------------------------------------------------
A CAREGIVER’S DUTY
A certain your caregiver knows their task and is comfortable with what is to be expected.
Surgery Day -- On site to talk to medical staff and to answer questions on the patient's behalf. Caregiver can stay in hospital in an extra bed.
Leaving Hospital -- Carry items, pick up medication, and drive.
At Home -- Help with putting you in comfortable position, give water, food, phone and supplies to patient. Observer and assist in showering and moving. This caregiver needs to be available 24 hours a day for about 14 days. This can be in person or on the phone.
The main goal is to have someone if there is an emergency, call doctors, and provide support and wound care.
Wound Care -- Help with cleaning, dressing, and observing surgical sites for 4 days.
-----------------------------------------------------------------------------------------------------------
FOLLOW-UPS
It might differ from different hospitals.
DAY 3-4 -- First Follow-Up: Remove dressing and catheter. Check surgical site and see how PT is doing with pain, urination, and BM.
4 WEEKS -- Second Follow-Up: 15-minute visit to check on health and answer questions.
3-6 MONTHS -- Third Follow-Up: 15-minute visit to check on health and answer questions. They will access the healing.
1 YEAR -- Fourth Follow-Up: 15-minute visit to check on health and answer questions. Last visit.
-----------------------------------------------------------------------------------------------------------
COMPLICATIONS DURING & AFTER SURGERY
This list is the most common complications seen in GRS patients; however, it does not mean that you will have these complications. It is just best to be aware during your recovery.
Vulvoplasty tends to have less complications as compared to vaginoplasty, but complications can happen depending on your current health.
These complications include:
Bleeding: Bleeding is to be expected after surgery. However, if it does not stop on its own in a few days, a second operation may be necessary to stem the bleeding.
Infection: Although the procedure is done in a clean and sterile way, there is always a chance of bacteria entering the wound. In the period after the operation, there is also a risk of infection. That is why it is so important to take good care of the wound at all times as infection can damage the structure.
Blood suffusion (haematoma): Some blood may accumulate in the surgical area, which may give the area a slightly blue or purple appearance, like a bruise. This will go away by itself after 2 to 4 weeks.
Fluid retention (oedema or seroma): Fluid may also accumulate in the surgical area. If this feels uncomfortable, the fluid can be removed by the physician in a follow-up.
Badly healing wound edges (wound dehiscence): After the operation, the wounds may not heal immediately, and may open up a little. Should this happen, it is recommended that you rinse the wound thoroughly with running water and, if necessary, contact your attending physician.
Hypergranulation: Hypergranulation is a very common problem. It is benign, but does involve a sizeable loss of fluids or blood. It may also have a certain odor and be painful, but it is easy to treat.
Loss of feeling/orgasm: As with any surgery, nerves may be damaged in the operation. Sometimes feeling will not be restored to what they once were. Orgasm can also change after the surgery.
Scarring: The growth in scarring tissue differs per person, skin type and surgical method. People and skin types all heal in their own way. Being overweight or a smoker means that wounds will heal less pretty than in healthy, non-smokers. Sometimes, a scar can be corrected (at least one year after the operation).
Urine spraying: One-third of people in published studies report this complication. Patients often find that it can take more than 6 months before the urine stream is more directed. If you still have bothersome urine spraying after 6 months, it can be often corrected with a second surgery.
Urinary urgency/frequency: This is a feeling of having to pee suddenly and often. This is common soon after surgery because of bladder irritation. This typically resolves on its own.
Urine leakage: This can happen without warning. This usually happens when pressure increases in the abdomen, such as with coughing, laughing or sneezing. This usually gets better on its own as you heal. Pelvic floor physical therapy can help.
-----------------------------------------------------------------------------------------------------------
END RESULTS
The final results will not be visible until after six months with the reduction of swelling. Most who have this operation tend to have an immediate negative experience after seeing their neo-vagina just after surgery.
Remember, this operation takes up to 6-12 months to complete the healing process.
The swelling and discoloration will slowly subside. The vagina will form naturally after the operation and will adapt to your body shape. For example, the color of the scrotum and the amount of fatty tissue will determine what the genitals will look like. The end result is different for everyone.
-----------------------------------------------------------------------------------------------------------
SCAR CARE
Massage is suggested to help loosen scar tissue. This can ease the discomfort and make them less visible over time. It is suggested you begin scar massage, advised by PT, 5-8 weeks after surgery. Daily exercise for 5-10 minutes.
Remember! A Massage Isn’t Meant To Hurt! Go gently to desensitized first.
-----------------------------------------------------------------------------------------------------------
CORRECTIONS
If you are not completely satisfied with the appearance or function of the genitals, you can discuss this with your plastic surgeon or urologist. They will be able to tell you whether an additional operation could lead to improvements.
Some surgeons report that nearly half of their patients will need a second surgery to fix complications or for aesthetics. Some surgeons also tell everyone that two surgeries are always necessary for a final result.
Corrections may, for example, be:
A reduction of the inner labia.
A correction of the clitoral hood.
A correction of the urethra.
In principle, corrections are not performed within 6 months of the first operation. It is advisable to wait at least one year as most issues are due to swelling.
The difficulty with cosmetic corrections is that getting them covered by insurance is difficult without a medical reason.
-----------------------------------------------------------------------------------------------------------
SEXUALITY
Your sex drive (libido) depends on the hormone testosterone. Most patients recovering from GRS report having a low sex drive for a while, as their testicles have been removed.
However, your sexual life depends not only on genital surgery, but also on many psychological and biological factors; so, do not be discouraged if you cannot reach climax at the time.
It can take upwards of 6-9 months for the nerves to heal after surgery. Nerves will not regrow for around 3-4 weeks after surgery. They will then begin to regrow at 1 millimeter a day or 1 inch a month. It seems that younger people will see the most regrowth. This packed regrowth might make sexuality more intense than before.
However, numbness is also a possibility.
It is natural to feel numb in some areas of the surgical site. With nerves regrowing, it will feel like pins and needles, tingling, and or a quick electric shock. Some find their clitoris desensitized, whereas others find it overly sensitive...it varies.
Becoming familiar with your genitals and learning to use them in a pleasurable way are significant challenges after genital surgery. It is important that you discover what gives you sexual pleasure and that you discuss this with your potential partner/partners
Some people have no desire for penetrative vaginal sex, in which case a vulvoplasty can be a good choice.
After vulvoplasty, you can still have orgasms through the stimulation of the clitoris — just like in the case of vaginoplasty. During a vulvoplasty, your surgeon will construct a clitoris from the glans and, if applicable, the foreskin of the penis.
-----------------------------------------------------------------------------------------------------------
RESUMING NORMALCY
Walking: 2000 steps (1 mile) a day for first 4 weeks | Afterwards, gradually increase. The more active you are, the more swelling there will be.
Showering: Twice daily for six weeks.
Bathing & Pools: No bathing or swimming for 3 months.
Lifting: Nothing over 10lbs for 4 weeks. | Afterwards, gradually increase.
Exertion: No workouts, running, or strenuous activities for 6 weeks. No biking for 3 months.
-----------------------------------------------------------------------------------------------------------
RESOURCES
https://genderaid.org/en/feminization/info/vulvoplasty
https://www.ncbi.nlm.nih.gov/books/NBK222286/
https://www.ohsu.edu/sites/default/files/2022-07/OHSU-vulvoplasty-booklet-2022.pdf
#gender transformation#gender#transgender#surgery#change#transformation#trans#tg#gender reassignment#gender reassignment surgery#MtF trans#male to female
21 notes
·
View notes
Text
Gender Reassignment Surgery Finally Scheduled!

It has been almost 17 months since the last time that I visited the OHSU clinic in Portland Oregon to see if I was a candidate for GRS.
There have been many times that my hope had fallen through. Days when I wondered if something outside of my control had ruined my plans to finally feel ‘complete’.
To compound the mental pain during the process, my experience with OHSU has been somewhat ‘complicated’. I am used to medical departments keeping their patients up to date...however, this is just a fantasy that I strongly urge others to avoid.
First off, let me say that my encounter with Dr. Dy, at OHSU was a pleasant experience. Unlike other physicians who only see the physical treatment and outcome, I was greatly appreciative that Dr. Dy also took into consideration my emotions and feelings regarding this sensitive topic that I would rarely speak in public.
It was because of my trust in her, her medical background, and willingness to understand ‘my own’ situation that I committed my care at OHSU. As for the urology department, my experience wasn’t all too great. Hopefully this will change in the following appointments.
One topic that I wish to cover in this blog post is:
Do not be afraid to reach out!
I have reached out three times to OHSU regarding my surgery status, and each time, I have received a different response.
I left OHSU in January 2022 knowing that the surgery would most possibly not occur that calendar year, thanks to COVID. Dr. Dy mentioned in clinic that due to the virus, their patients were backed up. She gave a timeline of ten months upwards to a year.
Yet, as time went on, I never heard a word regarding the status of my surgery. I would check the Portal monthly to see if any messages were sent, but as always, there was nothing to report.
By August of 2022, I finally reached out to the clinic and asked for an update. I was given the timeframe of January 2023 to May 2023 to hear a response for surgery scheduling (but not the offical surgery date).
Yet, by May 1st of 2023, I had yet to hear from them.
So, I sent another message after talking to my PCP and therapist regarding my communication with OHSU. I had expected a prompt reply within 3 days as the Portal promises, yet something ‘anxiety-producing’ had happened that I wish to discuss:
The Portal allows you to see if your messages have been opened, and by May 2nd, my message had been marked as ‘Seen’. Yet, day after day, I recieved no reply from the department of urology.
By May 3rd, I expected to finally have my reply so that I could make plans for the future: like lodging, psychology papers for surgery, saving money, arranging caregivers, and preparing my family to live without me at home
Yet once again, no reply came.
May 4th & 5th, I began to wonder if the clinic was trying to receive an answer to my question...so I gave them the benefit of the doubt.
May 6th & 7th was the weekend, so I did not expect any reply from OHSU. But I was almost certain that a decent person would at least say something by Monday, May 8th.
During the weekend, I wondered what was the reason as to why no one wrote a reply. I came up with many thoughts at night that made me worry and despair. Thoughts like: ‘Are they angry with me?’ | ‘Am I no longer a patient?’ | ‘Did I send the message to the wrong person?’ | ‘Is this something to do with my insurance?’ | ‘Maybe this is a sign that I should not be having surgery!’
By May 8th, my reply had never come.
I began to think that maybe this was a universal sign that I should not be having this surgery after all. And I began wondering if I should wait for an eternity, or look elsewhere for surgery and begin the whole process all over again.
That night, I thought of sending a reminder message to the department: ‘Maybe they forgot?’ Yet, if they cannot answer a simple question regarding scheduling and paperwork...then is it a really good idea to entrust my future care with their department? Especially if I have an urgent question in post-op!
‘Well, the last message did say ‘at the end of Spring’, and Spring officially is over on June 21st. Maybe I should just be patient?”
May 9th -- like before, I waited for a reply -- but no reply came.
Today, my mother brought up my ‘lack’ of swimming and I told her that the last time I went to swim at the YMCA, I had a terrible experience that has kept me away from the pool for almost one year.
Without GRS, my life has been in a painful standstill.
I cannot use any public restroom or locker room because of my strict morals. Everyone is different, but my morals prevent me from using a women’s restroom if I still have a penis. This is because I would never want to encounter a man in a women’s restroom...even if that individual is a transwoman who hasn’t undergone GRS.
I can no longer use a male’s restroom or locker room...because I now ‘appear’ too much as a female. Not to mention that this would create a terrible experience of abuse and even possible sexual harassment.
Even without GRS, I cannot face going to the ER for emergencies due to a bad experience in 2019 when I had to reveal that I was transgender. Even my time in the ocean had suffered because of fear of getting wet and things revealing too much...it is a painful existence!
With a long drive to Bainbridge Island, I had plenty of time to think of my next move. I sent a second message to OHSU...but instead of placing blame...I apologized and asked once more.
I honestly did not expect anything to come out of it.
Around 3:10PST I finally recieved a reply from OHSU. In communications with Mr. Skelton who asked if I would like to have surgery on July 12th 2023 with Dr. Dy being my attending physician.
I was thrilled!
I quickly checked my calandar to see that surgery will be a week after my vacation. Perfect timing!
So, with one step closer to finalizing my new life as a female...I can only dream of returning back to the pool to swim! Play in the ocean and clam dig! Not be afraid to use the restroom when I really need it. No fear in violating my morals bathing amongst other women in onsen and locker rooms.
I can finally focus on my health instead of jeopardizing it. Even possibly enter a relationship without having a panic attack.
For most of my life, I felt neither male or female...but both at the same time. I can only wonder how my future will change after this surgery...for the best and for the worse.
Only time will tell; though the path will be long.
#gender transformation#transgender#gender#surgery#change#gender reassignment#transformation#restroom#trans#MtF trans#mtf#SRS#GRS#gender reassignment surgery#OHSU#Oregon health
8 notes
·
View notes
Text
UPDATE ON GRS/SRS SURGERY DATE
Been about two months since I’ve written anything here. Life has been pretty good; though for the occasional reminder of gender dysphoria.
This topic I wanted to write; as I feel that it could be important to pass on to others who are in the same boat as I am…
So, of all the surgeries I’ve had, the waiting and recovery…so far, my experience in the last major surgery has had its up and downs.
Both breast augmentation and facial feminization took about 6-9 months to schedule and then have surgery.
However, SRS/GRS is proving to be a game of patience.
It has been about 8 months since I’ve had my consultation and I have not heard a word. So many questions go through my head:
What if I missed a phone call?
What if my insurance denied it?
What if they forgot?
What if my consultation went bad?
What if I offended the surgeon?
What if this isn’t meant to be?
What if…
For eight months I thought about the what if’s and it only made the dysphoria much worse!
So, for anyone asking the what-ifs; please do not hesitate or expect the clinic to call you! This will only make things much worse.
Message Them!
I’ve played the what if game for almost 8 months; thinking:
‘They are busy…I must be patient!’
‘It’s only been eight months, I’ll wait for ten months—or until January of next year’
‘They’ll email me. They’ll tell me when to expect a scheduling date soon.’
Wait and wait…and nothing.
Waiting on a scheduling day, and then a surgery date. Knowing it will pass into the day of surgery and the long recovery.
I’ve prepared my family for this surgery, which was hard…and I wonder what will break first: my family unable to be there, my health, my nerves, my insurance, or my dysphoria crippling me!
Please Do Wait! Ask For A Status Update!
If the uncertain is making it hard to cope, just ask the clinics urology department! And if you live far from your clinic; don’t hesitate to ask for a means of contacting the clinic for questions and concerns.
Luckily, OHSU has a online portal that allows me to contact my surgeon, the urology department, and transgender team.
Do not be afraid to use these resources!
Please don’t allow yourselves to suffer of processed blindly. Always ask!
8 notes
·
View notes
Text




#transgender#lgbtq#transformation#gender#trans#lgbt#lgbtqa#lgbtq community#male to female#mtf hrt#maletofemale#mtf#gender transformation#mtf trans#lgbtpride
93 notes
·
View notes
Text




Happy LGBT 🏳️⚧️ 🏳️🌈 Day!
#transgender#lgbtq#transformation#gender#trans#lgbt#lgbtqa#lgbtq community#male to female#mtf hrt#maletofemale#mtf#gender transformation#gender bender#mtf trans#gender nonconforming#nonconforming#lgbtpride#body dysphoria#mermazing#mermaid#transgender mermaid#hormone replacement therapy
12 notes
·
View notes
Text
A Review Of My GRS (SRS) Consultation At OHSU.

So, it’s been almost five months since my consultation at Oregon Health & Sciences University (OHSU) regarding Sex Reassignment Surgery (SRS)/Gender Reassignment Surgery (GRS).
The appointment was on Wed 26th of January (2022) with Dr. Geolani Dy (MD).
I’ve been postponing writing about my experience as it was rather a traumatic experience that has taken many months to get over.
I wish to first state the Dr. Dy was very professional in her approach to my care. She explained everything so throughly and listened to my expectations I had for myself.
I only wish that if we have surgery, that she is my appointed physician as she was the only one I met.
So, let’s talk about the OHSU/Transgender Services regarding ‘bottom surgery’!
THE CLINIC—

OHSU is a large campus — I’ve never been to the clinic prior to my visit; and luckily the clinic was located in Downtown Portland’s Waterfront district that also has the Roods Family Pavilion. The parking was easy to access and secured.
The main hospital is located about a mile away, on the hill, just west of the clinic.
Be certain that you are aware that you are visiting the Clinic and avoid the main hospital.
FOR out of staters — I live up north, near Tacoma…so the drive is about 3.5 hours coming and going. The appointment was about 45 minutes.
I’ve driven in Seattle before and believe the Portland can be overwhelming to some.
I elected to stay in the community overnight, for two days to calm my nerves. If you are driving alone, this might be a good idea; as I was very jumpy and emotionally compromised after my appointment that I accidentally went the wrong way down a one-way street. Luckily the people help guided me out of the area with very rude words.
I stayed at the Park Lane Suites & Inn which was a very nice and reasonable place to stay. A bonus was that it was near the Japanese Gardens.
I spoke to Dr. Dy about lodging during and after surgery; as it is too far for my family to drive back-and-forward.
She stated that the hospital had a 30 mile radius that was considered local; all others are available to stay at the Rood Family Pavilion for the duration of the surgery.
I talked about being discharged and going home; only to return a week later.
She sympathized, offering to put myself and my family in the RFP for almost 3 weeks (20 days) after discharge.
This would allow me to have immediate access to her clinic if there are any situations or trouble. I was in full agreement and loved this plan as I didn’t know what I was going to do if I had an emergency.
For those wishing to add RFP to your stay, be aware that they have limited rooms for children and adults and this could affect your surgery date.
THE STAFF —
My arrival to the clinic was met with both friendly and unfriendly staff. This can be very stressful when you are anxious.
The receptionists at the front were very brash and I waited for them to talk talking to one another for almost ten minutes.
I should have said something, but I was so scared that I just wanted to disappear.
Once back; I found the CNA to be very sweet and friendly. She helped to ease my tension.
And Dr. Dy was amazing! She was very patient with me and didn’t try to push me into having something which I didn’t want.
When it came to physical exam; I was so terrified that I was moved to crying. She was very understanding and offered to skip that part of the exam; but after a moment, I allowed (for precaution reasons).
THE EXAM —
There will be an exam at your appointment that will require inspection and physical touching of the genitalia. For someone with terrible dysphoria, this part of the test is very painful to endure…but here is why you should do it:
First off, you can ask for no examination of the genitalia. This is your right as a patient!
Dr. Dy was very polite and offered not to do the exam if I wasn’t ready. But mentioned the importance to scheduling for an appointment all pended on a physical examination.
Basically, she is looking for lumps or growths that might signify cancer or tumors. If these are present at your scheduling; your appointment could be postponed for diagnostic care to rule out cancer.
Even though it is a terrible experience; it is best to get comfortable with having people looking and touching down there—as it will happen a lot after surgery.
THE EXPECTATIONS—
As the patient, you have the right to have vaginoplasty or vulvoplasty.
Understand that certain requirements will influence your decision (from weight, prior surgeries, health, smoking & drug use, and especially hair removal).
Since I am not sexually attracted to men; and have no desire for penetrative sex, I elected to have a vulvoplasty with 1” depth neo-vaginal canal.
This is a new concept being offered to new transgender patients, by some doctors. I asked Dr. Dy if she could perform a vulvoplasty with a max 1” depth vagina and she said it was possible. Most depth is around 1” with the skin of the shaft…the skin from the testicles are added to create the maximum depth in vaginoplasty.
This isn’t a guarantee; but a plan.
After surgery; the expectations are lesser with a vulvoplasty (as compared to a vaginoplasty) as there is no (or very little) dilation.
I will be expected to come to all appointments for up to a year; and maintain a weight and non-smoking regimen for my life. These are all doable as I don’t smoke, drink, or do drugs.
3 notes
·
View notes
Note
What makes Shinto allign with your personal beliefs?
Thank you for your question.
I practice Shinto (alignment mainly with Omiya Nome no Okami and Uka no Mitama no Okami / Inari) and am an active member of the Shinto Shrine of Shusse Inari of America.
As a student of Japanese dance, culture and etiquette; I pray to Omiya Nome no Okami (Ame no Uzume no Mikoto) for guidance, happiness, and success in the performing arts; as she is the goddess of performing arts, like kagura.
I also pray and enshrine Uka no Mitama no Okami for good productivity and harvest of my crops, success in my business and thanks for my life aligned to a spiritual nurturing and growth.
As for my personal beliefs; I was raised to believe that everything has a divine spirit residing within. As a steward of this Earth; I am to honor, protect, and abide by the laws of nature.
My belief in family oriented living, assisting my community, and honoring my ancestors are concepts reflected in Shinto that I find most agreeable. Unlike most traditional religions, Shinto (though once considered strictly a Japanese only faith) is inclusive to all backgrounds of culture and faith.
As a spiritualist, the concept of monthly purification, and bi-annual in-depth purification allows one to release attachments, negative energy, and toxins while elevating the mind, body, and spirit to living a life in sync with nature; as we too have Kami residing within us.
Douzo yoroshiku onegaishimasu!
5 notes
·
View notes
Text
(2021) A Yearly Gender Dysphoria Review
December, 2021
BASELINE QUESTIONS
Given Name: David Joseph
Desired Name: Mira
Legal Name: Mira Carleen
Desired Gender: Female
Legal Gender: Female
LGBT Status: Transgender Woman
Relationship Status: Single
1) How Long Have You’ve Been On HRT (Without stopping more than a week)?
A: 39 Months (Enrolled In The Program) and 37 Months of compliance with HRT.
2) How Long Have You Been Going By The Name Mira?
A: 30 Years (Personally)
3) How Long Have You Been ‘Mira’ Legally?
A: 3 Years
4) How Long Have You Identified As Female?
A: About 30 Years (Personally)
5) How long have you’ve been legally Female?
A: 3 Years Now
6) Do You Regret Your Decision To Transition?
A: Never! I’ve been quite happy with my transition to female. I have found that appearing and identifying as female has released my stress and tension that I once felt as David.
7) How Long Have You Known That You Were Transgender (LGBT)?
A: I never learned about the transgender community, until my late years in collage (2004). Before then, I thought my dysphoria was a disease that I should be ashamed of. I didn’t start considering that I might have been transgender until the year 2016. I legally had to sign documents, labeling I was transgender in 2018 (Cedar River Clinics).
The diagnosis of ‘Male-to-Female Transgender’ and ‘Gender Dysphoria’ were not established until 2019.
LGBT QUESTIONS
1) On The LGBT Spectrum, Where Do You Fall; Gender-Wise?
A: Female
2) On The LGBT Spectrum, Where Do You Fall; Sexual-Wise?
A: Lesbian / Interested In Women
3) When Did You Realize That The Term Transgender-Woman Referred To You?
A: At the beginning of 2019 when I began considering legally changing my name from David to Mira. The catalysis that solidified the term was when I decided to make a full gender transition from male to female and began considering surgical intervention to make this a possibility.
Because of these changes, I feel that I can no longer label myself neither as ‘gender-fluid’ or ‘non-conforming’; which were my first labels (2018).
4) When Did You Realize That The Term Lesbian Referred To You?
A: Around February 2019 when I rekindled my relationship with my girlfriend. We considered the aspect of our relationship, and because I yearn to become female legally, physically, and sexually…it would transform our relationship status from male & female to female & female.
July 2020, I tried to solidify my sexuality as a Lesbian, but I don’t think my girlfriend is comfortable with my decision.
In 2021, I consider myself Lesbian, only privately. As I am not sexually active, and the term really doesn’t apply until I have my vulvoplasty. Even then, I would be Lesbian in a relationship, but not sexually.
5) Are You Comfortable Using The Term ‘LGBT’, Or Calling Yourself A Transgender-Woman; And / Or A Lesbian?
A: Personally, I don’t like labels. I will use the term LGBT when writing on forums or speaking to my physicians. But it isn’t a term I use openly in public.
As for the label of Lesbian, I avoid that word. I don’t like it as it implies that I am sexually active with another woman. I am not even in a relationship!
6) Are You Currently Active In The Trans Community Or LGBT Community?
A: Not physically, but I want to become active in the future. COVID has blocked all community meetings at this time, in my area. I do however still post to my Transgender blog about my research and updates.
7) Have You Reached Out To A LGBT Center For Help?
A: No. I have not needed the assistance of a LGBT Center since 2017. My last communication was to the main LGBT Center in Seattle, but they were not helpful. Personally, LGBT Centers are pointless.
8) Who Was The First Person You Talked To, About Being Transgender?
A: Unofficially, that would have been my girlfriend, Ruth.
Before I started HRT, I mentioned to her that I thought that I might be gender-fluid or gender nonconforming. She replied that she had suspicions that I might be transgender as I always associated as female in our relationship. She also thought I might be asexual due to my displeasure in intimacy.
9) What Is Something Positive About Being Transgender?
A: It isn’t the same for every person, but being Trans has allowed me to accept my feminine nature without apology for my physical sexual appearance. Before transitioning, I was very unhappy with my life. I believe my displeasure had a negative effect on my overall mental and physical health.
With the aid of being male-to-female transgender, I’ve been allowed to conform to the mental image in my mind, and not be afraid to my empathic and intuitive.
10) What Are Some Fears About Being Transgender?
A: There are many fears that come along with not being transgender, but with dysphoria. My greatest fear that I have dealt with in 2021 was the fear of someone finding out that I am not completely female. It has driven my need to finalize my metamorphosis.
I feel this fear amplified if I wear tight fitting pants or go swimming. I am almost certain that nothing would happen, but I don’t want to risk it.
11) How Do You Manage Your Dysphoria?
A: In 2021, I’ve managed my dysphoria with committing to the program, having my regular medical checkups, seeing a psychologist monthly (since July), writing stories and blog posts, and being truthful of my feminine nature.
12) What Steps Have You’ve Done To Further Your Compliance And Develop Your Feminine Identity?
A: In Jan 2021, I was still healing from my Facial Feminization (10-2020) and was preparing for my Breast Augmentation (1-4-2021). I’ve been complying with my healing regiments by exercising the tissue in both breasts to reduce scar tissue (capsular contracture) from forming around the implants, and to help encourage blood flow to give the breasts a soft and flexible nature.
By 4-2021, my implants finally fluffed out and settled by 7-2021.
I did a month of vocal feminization, but discontinued due to poor quality of service.
I also began the application work to have my consultation with Dr. Dy at OHSU to discuss vulvoplasty. In preparations for this possible surgery (up to a year away, possible, due to COVID); I have hired a psychologist to review my mental health every month.
It is my hopes that after building a trust with her, I can depend on her greatly, after my post-opts. I have read many reports on the psychological aftermath of GRS(SRS) and want to have all my bases covered.
Lastly, in 10-2021, I enrolled in a Japanese Dance Academy that teaches me feminine manners, body movement, and etiquette.
13) How Have You’ve Embraced Your Transgender Identity?
A: I’ve embraced my transgender identity by embracing my feminine identity. I’ve pushed my past aside and look to the future. I understand that I have a male physiology, but I don’t let that interfere with my happiness as being emotionally and chemically female.
14) How Do You Feel About The LGBT Laws Where You Live?
A: Washington is quite friendly to the LGBT. According to a 2019 Gallup Poll, roughly 5.2% (342,000) people are on the spectrum. We have Nondiscrimination laws for both sexual orientation and gender identity. It is also unlawful to discriminate against a person who is trans; which is nice.
By law, healthcare cannot deny or discriminate against a person’s gender identity (but sexual orientation is only protected under private insurance laws). Overall, my experience with healthcare is about 50/50.
In June of 2021, Gov. Inslee signed the LGBT Pride Month proclamation, giving the month of June as Pride Month to the LGBT.
Starting Jan 2022, health insurance companies operating in Washington will be required by law to cover gender affirming surgeries and care (SB 5313). This will be a great relief to many, as I’ve experienced denial-of-care by the insurance for both FFS and BAS. I privately fought each denial and overturned them with my methodology, gaining full coverage for the procedure.
15) What Are Your Views On The Cis-Gendered Community?
A: Unchanged. Cis-gendered individuals, like myself before 2017, can also be transgender without showing it. And actually, most people will experience some form of gender dysphoria in their lifetime.
I prefer to look at the Trans and Cis communities as equal; but different when it comes to dysphoria.
BODY-TYPE (DYSPHORIA) QUESTIONS
1) Facial Features (Desired)
A: Completely feminine.
In 2020, I finally was able to have my masculine traits reduced. Dr. Nuara wasn’t all to thrilled to do everything in one surgery, but to my shock at the moment of pre-opts, he did everything (plus more) to give me the face that I wanted.
The surgery took over eight hours to complete!
The areas worked on, were the areas that I was most concerned about:
A) The brow was shaved down. The sinus plate was removed and shaved down too, and fused back to the skill with titanium fasteners.
B) The orbital rims were reduced to open up my eyes; but I am unsatisfied with the results on the right eye.
C) My hairline was brough down to undo male pattern baldness.
D) My lips were brought out to give them a fuller appearance. The philtrum was reduced, bringing my upper lip closer to my nose.
E) My chin was shaved to cut down the sharp angle.
2) Hair Features (Desired)
A: I am trying to grow my hair to the point that it covers beyond my nipples. That will be a perfect length that I would like to achieve.
I prefer straight hair, but mine is naturally wavy and does not straighten well. I have been blonde for almost 18 months. I have decided to returned to a darker color in December of 2021. I plan to return to blonde in June of 2022.
3) Neck Features (Desired)
A: I prefer a neck that is slender and feminine in appearance.
I had my neck tightened during my facial feminization, removing the second chin below. Slender and feminine.
4) Shoulders Features (Desired)
A: Shoulders typically are not one of my areas that trigger my dysphoria. I have a wide width to my chest, and thus, my shoulders are around 17 inches apart.
I prefer to keep them toned and with no long hairs (which really isn’t a problem either, as hair doesn’t grow there).
5) Upper Arms (Desired)
A: The upper arms are not typically one of my dysphoria areas.
With the use of hormones, my upper arm width went from 16 inches (muscular) to 14 inches (toned). I’ve certainly noticed that lifting things isn’t as easy as it was before!
6) Lower Arms (Desired)
A: Again, not one of the areas that I am overly concerned with. I keep my hands and lower arms shaved, as I don’t like body hair. I use to paint my nails, but only done so, about three times this year.
7) Back (Desired)
A: One of the worst places for body hair was my back! It was so embarrassing! Yes, after hormones, the hair had thinned, shorted to around .5cm and turned blonde. It was one of the greatest, welcomed surprises of my HRT.
8) Chest & Breasts (Desired)
A: Like my back, my chest was heavily influenced by male hormones, becoming quite hairy in the process. Hormones only reduced the hair by about 30%, the thickest is still over the sternum. The darkest is around the areolas. Hair growth on the breasts has dramatically slowed down to maybe .3cm per two weeks.
In Jan 2021, I grew to around a full B-cup (46/48), but fit comfortably in a C-Cup during the growth cycles.
After surgery, I was raised to a DD/DDD-Cup (46/51) with an implant of 640cc, each.
About five months after my surgery, I underwent a sudden a quite painful growth period that swelled my breasts from 51 inches to 54 inches. Since December of 2021, my breasts have not shrunken down, remaining around 54 inches (full bust measurement). This was actually glandular development, as I’m develop ‘atop’ the implants, making them hard to feel during daily massages.
At this moment, my new D-bras that I bought (and fit nicely) now are too small, as I overflow. It is likely that I will need to find a bra that is G/H Size.
at 46/53.
I will be returning to see Dr. Schmitt in 2024 for a checkup on the implants.
9) Belly And Waist (Desired)
A: The belly and waist are not triggers of my dysphoria, only annoyances from poor diet choices. Only thing that I desire to modify is the removal of any hair that grows on my belly.
10) Buttock (Desired)
A: The buttock wasn’t something that I was overly concerned about. Yet, hormones caused some amusing and feminine transformations to take hold.
At the beginning, my hips/buttock measurement were around 49.5/50 inches. Today, around 54.5 inches. I can certainly tell that my buttock has nearly doubled in size; as I had a rather diminished subcutaneous fat layer, but very wide feminine-like hips.
Since then, my buttock has toned with a lovely upside-down heart shape.
11) Upper Thighs (Desired)
A: Upper thighs are not really a concern of mine. Due to my build, height and abnormally larger hips (in cis-males), I will always carry a little extra weight in this region. Oddly though, I’ve lost inches here; from 30-inch diameter to 26.5 inches in diameter
12) Lower Legs (Desired)
A: No changes are desired here; I am pretty happy with them. I only wish to keep them shaved for wearing skirts.
13) Feet (Desired)
A: Feet are ugly, no matter what you do with them. I have no desire to change them though.
14) Hands (Desired)
A: No desired physical change.
In July of 2021, I stopped having my nails painted due to COVID restrictions and contracting a painful infection in my left big toe, just after having my toenails painted. It took one year to defeat that infection!
15) Genitalia (Desired)
A: Of all the parts that I don’t like talking about, or writing about; it would certainly be the genitalia.
Ever since I was nine years old, I’ve always had a disconnect with the genitalia that I was forced to have. It was gross having a penis on my body—it just felt that it didn’t belong there!
The best way I can describe it: Imagine waking every morning to the wrong genitalia that makes you want to vomit with the idea that you might have to use it. Even talking about it, on my own body is like undergoing shock therapy—makes my stomach clinch so badly that it screws up my digestive system for a week!
My main dysphoria is my penis—I will not allow myself to become intimate with another, choosing isolation and loneliness to hide my shame. I wear clothing that especially covers this region; careful every day to be certain that its imprint does not show.
Using the restroom, showering, undressing—it is a nightmare. I’ve trained myself never to look or look in reflective surfaces as I can’t take the blasphemy that I was cursed to carry! This is what I deal with when it comes to my sexuality, and why I’ve became asexual in nature.
Mentally, I expect to see female genitalia when I wake. It is hard to put in words, but it seems natural to me to have a vagina, clitoris, and labia. In my mind, it is perfect symmetry—perfect balance. It is the only form that I feel comfortable revealing if I am in a serious relationship or at the hospital.
With my surgical consultation coming up in less then a month, I have rather detailed results that I wish to see in post-opts.
Since I am not sexually attracted to men, I feel that having a full vaginoplasty is like buying a yacht on Mars, pointless and useless. The upkeep for a transgender woman with a vaginoplasty is really taxing and exhaustive with a higher risk for infection.
Secondly, my choice against a vaginoplasty is the painful requirement of having hair removal in the genitalia. This would absolutely devastate me! First, I am not comfortable with my own genitalia, so why would I wish to expose them to a stranger for them to touch! Secondly, the pain! I’ve had laser on my face, neck, and chest—and even with numbing cream, it is barely tolerable!
It is because of these reasons that I’ve decided to only have a vulvoplasty; though I am open to doing a minimal-depth vaginoplasty for dysphoric reasons. (Also, having the title ‘vaginoplasty’ might help with the mental adjustment of actually having a vagina, and not just a flat void).
Appearance is very important to me. I am my biggest critic, and if I think that it looks fake, or mutilated; I fear this would only lead to future problems.
I have no need for a deep canal, but I would like my pseudo-vagina to be between 1.5-2 inches in depth. This will be big enough to maintain the illusion and use in stimulation.
I plan to ask for a vulvoplasty with the maximum possible depth possible for the pseudo-vagina without the full depth as seen in a vaginoplasty. I will be seeing Dr. Dy at OHSU on January 26th 2022 to discuss these questions.
MENTAL/PHYSICAN EVALUATION QUESTIONS
Aspects Of The Feminized Brain
1) Have You’ve Grown Fond Of The Color Pink?
A: Yes. I now have two pink shirts that I wear many times a year. I find that the color pink is very useful in emphasizing my feminine nature when I am having a difficult day with my dysphoria.
2) Have You’ve Noticed Any New Scents Coming Off Your Body?
A: Not recently. I’ve adjusted to the new scents of my pheromones.
3) Have You’ve Notice Any Scent Sensitivities Since Transitioning? (New Question For 2021)
A: Oh yes! My tolerances for scents have dramatically changed! Before, I could tolerate some of the worst scents possible: like sewage, rotten eggs, or mold. Now, these same scents cause me to nearly vomit.
4) Have You Subconsciously Used ‘Female Pronouns’ In Describing Yourself?
A: Yes. It is weird to think of myself as ‘he’, ‘him’, or ‘male’. I first noticed this new way of thinking when I tried to describe my past during therapy. I stumbled over the pronouns, wanting to use female pronouns instead of male. I paused thinking: ‘Well, that was weird!’
I also have noticed that my dreams have begun to change too! I see myself now mainly as female with female pronouns. It was very weird, as I am not in control of my subconscious thoughts.
5) Have You Started ‘Mentally Seeing’ Yourself Only As A Female?
A: Yes. It isn’t something that I dwell on; but one day, I was looking at photos and when I saw my old self, it was like looking at a stranger. Typically, I have always mentally saw myself as female, long before HRT. It is this female personality that has taken over.
6) Has Your Demeanor Become ‘Feminine?’
A: Yes! I notice that I still walk masculine from time to time; but I’ve taken up Japanese ‘feminine’ dance to enforce a feminine demeanor. My sensei is really nice in helping me behave like a proper female (Japanese temper). I’ve noticed that 1.5 months into the program, my walk and demeanor has changed to a more graceful gait.
7) Have You Expressed A More Feminine Approach When Talking? (New Question For 2021)
A: Yes, I find that when I am relaxed, I will slip into an in-between state where I emphasize my words with a feminine manner, with an androgynous vocal tone. However, when I am out in public; I am more tense and very careful with my voice.
8) Have You Been Drawn To Appreciate Cute-Looking Things, With An Emotional/Empathic Attachment? (New Question For 2021)
A: I added this question, as this is something new that I’ve discovered about myself this year. I found that when seeing cute stuff animals, cute anime characters, baby animals, baby children, or cute moment on TV; I feel overly emotional about it, sometimes acting a bit ‘girly’.
I believe that this behavior is tied to my once buried feminine nature. I did some research and found that many transwomen experience this also.
9 Have You’ve Experienced PMS-Like Symptoms? (New Question For 2021)
A: I believe so.
I notice that my body seems to cycle with the lunar cycle. Since being on hormones, it has become apparent that something odd has changed.
It is almost like clockwork, five days of misery. Usually, my first warning of the cycle is tender breasts, followed by stomach pain, feeling tired, bloated, and moody.
I’ve tried to mend the pain with Tylenol and home remedies, but nothing had helped. I might want to try something like Midol to see if it helps. Usually, I just use hot showers and lots of rest.
As much as I hate feeling this way monthly, I take solace in the idea that I am being empathetic with the females of my family. Considering empathy as being a dominate feminine trait: being empathic could be a link that aligns all the females of my family to syncing up their cycles, one after the other.
10) Have You’ve Experienced Crying At Any Sad Moment? For Example, TV, Movie, Music, etc. (New Question For 2021)
A: Oh my gosh, yes!
Before my transition, I hardly shed a tear—for it was forbidden! I remember that I was so emotionless that I didn’t even weep at my grandfather’s funeral until later that night.
Now, it seems that anything with a sad, or emotional moment will have me in tears. I’ve even tried not to cry, but usually never win that game. I find that the hardest cries come when I am feeling someone else’s pain, even if they are not real.
Some media that I avoid in public (as they are instant crying) is Johnny Cash’s song ‘Hurt’. Movies likes: Your Voice, Weathering With You, Only The Brave, A Silent Voice, When Marnie Was There, Archive.
11) Have You’ve Been Looking At The Other Sex, After Two Years Being On Hormones? (New Question For 2021)
A: Yes. I notice that just prior to my cycle; I seem to become infatuated with men. It is a weird emotional feeling, as I am not sexually attracted to men; I just feel connected to them emotionally. Wanting to be held and protected.
12) Have You’ve Noticed Any Cravings For Certain Salty Foods? (New Question For 2021)
A: Yes. I had to do some deep research to learn of a cause.
I always have craved salt, but recently, it’s been an obsession! Like I can’t get enough!
If I am not controlling what I consume, I can eat an entire jar of pickles. This is possibly due to spironolactone.
These food changes have reached new levels of ‘weirdness’ as I never liked vinegar; but spilled tarragon white vinegar on my hand and licked it, finding it actually good.
Feminized Aspects Of Social Influence
1) What Cup Size Do You ‘Want’ Your Breasts To Be?
A: D-cup is my ideal size.
I am already between D and DD(E)-cup size. It is a quite large size; resulting in many of my shirts not fitting well.
Secondly, I’ve found that D-cup puts a great deal of stress on the back. It is also difficult to sleep as they are large (but not impossible to cope with).
My ideal size would be between D-E as C-cup is disproportionate to my frame; and anything over E-cup just sounds absolutely uncomfortable!
My main goal that I had, before surgery was:
1) If laying down, I don’t want my breasts to simply disappear like they use to
2) If without a bra, I can still wear a dress and look ‘full’
3) Natural appearance!
2) Has Your Sexuality Changed?
A: I don’t think so.
I know that something hormonally has made me acceptive of having a FTM or MTF mate. However, I am not interested in cis-men. I prefer a female relationship, both sexually and intimate.
3) Do You Feel Sexually-Active As A Woman Right Now?
A: No…I still have my penis.
I know that I want to experience feeling sexual, as a woman…and my body seems to be changing the thresholds of pleasure from the groin to the breasts. They seem to be my new drive. I know that I have been asked if I want to experience sex as a man, just before losing my penis in surgery; but that thought makes me want to vomit!
4) Has Your Attention To Beauty Changed From The Time You Were A Cis-Male?
A: Yes.
I seem obsessed about my hair! I am also very observant to what I am wearing and how I appear to other people. I have not needed makeup much this year, thanks to the mask laws here in Washington.
5) Do You Desire Fuller Lips?
A: Yep…and have them!
6) Has Transitioning Enhanced Your Desire To Be A Parent?
A: Yes. Mainly to nurture a new generation! But I am turned away from the society that we are experiencing right now. Considering that I am sterile (before HRT), if I was in a relationship where my partner and I want a child, I’d probably adopt.
7) How Do You Navigate The Concept Of Sex While Being Dysphoric?
A: I don’t. I tried to open a consensual relationship with Ruth in 2020; but it was a terrible experience! I would like a deep consensual experience after my genital surgery.
8) Do You Believe That Your Brain Has Been Feminized?
A: I know science is still out on debating regarding this topic; but I have to say yes. As a scientist, I observe my transition from an emotional side and a logical side. I’ve noticed that my empathy and emotions are almost 100% heightened from when I was a male! I cry at the silliest of sad moments, and find that I am becoming attracted to ‘cute’ things.
I find enjoyment in watching romantic movies, as it is an emotional rollercoaster. I also notice that my speech and behavior has changed, becoming feminine.
My mental cognition really hasn’t changed much from before to now—I’ve always had a dominate creative empathic side, and a dominate (yet weakened) logical side (as reflected in my grades).
CULTURAL CHALLENGES (FOR TRANS-WOMEN)
1) Have You Been Outed For Being Transgender This Year?
A: Not this year.
2) Have You Been Misgendered This Year?
A: Yes, but only by my grandmother. I think she does it on purpose.
3) Have You Been Physically Harmed Or Abused, Because You Are Transgender?
A: No.
4) Have You Been Mentally Harmed Or Abused Because You Are Transgender?
A: Yes. Sometime the words unspoken to cut like a thousand knives. Actually, went writing this report for the end of the year assessment, I had to deal with the psychological harm that came from my grandmother. She heard about my appointment and was very rude and disrespectful, behind my back.
5) Have Your Family Fully Accepted Who You Are?
A: Mostly. They respect me for being female and calling me by my name. Many members of my family either don’t understand, are arrogant, or hurtful.
6) How Do You Deal With Being Misgendered By Cis-People?
A: I brush it aside. Confrontation isn’t what I feel comfortable doing. I prefer to live by the saying: ‘You cannot respect me; I don’t have to acknowledge that you exist.’
7) How Has Been Your Experience With Public Restrooms?
A: I avoid them at all cost! I personally believe that only females with vaginas use female locker rooms and restrooms. And males with penises use male locker rooms and restrooms. As a female with still a penis, I disqualify myself from using a public restroom (unless it is an unavoidable emergency). And because of my male sexual organ, I have completely stopped swimming because of the locker rooms to reach the pool.
8) If You Are Religious; Has Being Transgender Conflicted With Your Spiritual Care?
A: I use to be Lutheran; but I’ve denounced my faith and became a spiritualist. I have been considering following the Shinto faith, as it aligns with my personal beliefs.
9) Do You Feel Comfortable Answering Simple Questions About Being Transgender By:
A) Family: Yes, as long as it isn’t about SRS(GRS)
B) Friends: Yes, if they are trusted.
C) Strangers: No…they must become my friend.
D) Online: Yes…but very limited on personal information.
10) What Is Something You Loved To Do That You Are Unable To Do Now As A Transgender Woman?
A: Swim! I miss swimming. I am terrified that someone might see something and cause me harm in my community’s only pool. So, I will wait until SRS(GRS) is complete.
LIFESTYLE CHANGES QUESTIONS
1) Have You Grown Your Hair Longer And / Or Modified It In The Last Year?
A: Yes, it is almost three inches longer than last year! 16-17 inches long right now. Measuring shows that at 23 inches, I would achieve my desirable length.
2) Have You Worn Makeup In The Past Year? Or Stopped Wearing Makeup?
A: I’ve only worn makeup four times this year. COVID has made wearing makeup obsolete. I still like to dress up for holidays.
3) Have You Worn High Heels In The Past Year? Or Not Worn High Heels?
A: I want to…I just can’t find a pair the fits a size 15!
4) Have You Worn A Skirt In The Past Year?
A: So many times! I probably wear a skirt over 100 times a year. I’m bought five new skirts just this year!
5) Have You Worn A Dress In The Past Year?
A: A few times. Dresses just don’t work on a farm. I like to wear a dress when going out on the town.
6) Have You Worn A Blouse In The Past Year?
A: Nearly every day!
7) Have You Worn Any Form Of A Bra In The Past Year?
A: Every day! I don’t feel right without having one on. It isn’t proper. I am thinking of buying a sports bra when I am dancing. I bought my first cotton bra this year.
8) Have You Worn Any Feminine Undergarments In The Past Year?
A: Just panties.
9) Have You Gotten Your Ears Pierced? Body Piercings?
A: No, but my family keeps suggesting getting my ears pierced.
10) Have You Started Wearing ‘Feminine’ Jewelry?
A: Yes, I continue to wears rings and necklaces.
11) If You Had Some ‘Passing Tips’ To Offer Other Transgendered Individuals, What Are Some Things That You Learnt This Year, To Help You Pass?
A: Don’t be afraid to take a leap of faith. Sometimes learning from a different culture can help enrich your etiquette and feminine identity.
12) Have Being Transgender Held You Back From Your Career Choice?
A: No, I am still medically discharged.
13) How Is Your Relationship With Your Doctor(s)?
A: Very nice! Dr. Worth is quite professional and tends to my care quite well. Mrs. Mulligan is very through with my mental health, being certain that I am ready for my really uncomfortable conversation in January.
13) Since Transitioning, Have You’ve Noticed Your Physical Health Improving? (New Question For 2021)
A: Yes. Before my use of hormones in 2018; I was very sick from 2014-2017. My asthma and cystic fibrosis had severely damaged my lungs and caused inflammation in my bronchus. At one point, I was given two years to live.
After starting HRT, I noticed that my weekly asthma attacks that usually placed me in the hospital has weaken in severity. The swelling wasn’t as severe.
With decreased stress, and estrogen (an anti-inflammatory) in my blood; my hospitalizations dropped dramatically to the point of only three ER visits in 2021!
Here is a chart of Inpatient Stays prior to HRT and on HRT:
PRE-HRT 2015—167 Days Hospitalized | 2016—121 Days Hospitalized | 2017—97 Days Hospitalized | HRT BEGINS | 2018—67 Days Hospitalized | 2019—24 Days Hospitalized | 2020—12 Days Hospitalized | 2021—0 Days Hospitalized
COMPLIANCE QUESTIONS
1) Right Now, Are You Complying To A Feminine Attire? If So, What Is It?
A: Yes, I am in compliance.
This is New Year’s Eve and I am wearing a new blouse that I received for Christmas from mother. It is a silvery metallic sheen blouse with a belt, tried in a nice musubi knot. I am wearing my feminine undergarments with a vermillion-colored pleated skirt. My hair is brushed back with a single red band to hold it in place.
2) Right Now, Are You In A Serious Relationship?
A: Not really. I no longer feel that Ruth and I are compatible. The event happened two years ago, on the 4th of July (2020); when I learned that Ruth didn’t consider me as a serious partner. She revealed her true feeling for some other girl; saying she’s even slept with her. This goes against my morals.
I continue to maintain on my Facebook account that she and I are dating, as we officially have not called it off. But I feel it is just a means to protect us both from harassment of pervy guys on the internet. It is complicated. My social media site says that I am in a relationship, but I don’t feel that I am in one. I just allow the social media illusion to continue so I don’t receive many gross messages.
Overall, I hold out hope for a relationship with her, but I just don’t think it will happen anytime soon.
3) Right Now (Without Using Goggle), Write Out Something Positive About Yourself Using The Letters Of Your First Name:
A: M: Miracle I: Intelligent R: Romantic A: Admire
4) Please Explain In Your Own Opinion, Your Transition Process And What You Have Gone Through To Transition Into A Transgender Individual.
A: I began transitioning in June of 2018, but didn’t take my pills religiously, as I was scared of changing too fast. In 2019, I transferred my care to Dr. Worth and in June, I changed my name from David to Mira. In 2020, I underwent facial feminization. By 2021, I took vocal feminization lessons and then underwent breast augmentation.
I hope in 2022 that my meeting with Dr. Dy will go well and have surgery sometime in 2022 or 2023. Afterwards, I can focus on relationships, swimming, and proper female etiquette.
5) Which Feature Of Your Body Do You Like The Most Since HRT?
A: Respectfully, I would have to say my breasts. There is something more then having breasts to look sexually attractive, or self-gratification. Since January of this year, I have not needed to worry about forms, or if I will look ridiculous trying to wear a strapless dress. Just having them is a major step in balancing the spirit and the body as one.
6) Which Feature Of Your Body Do You Dislike The Most Since HRT?
A: Certainly, would have to say my male genitalia. I can write a list of things I dislike about it; but I have to be honest, I have two things that make having a penis ‘useful’: Outdoor urination & lower chance of UTI’s.
However, I’d trade convince any day to feel ‘balanced’.
I’ve already mentioned how having male genitalia makes me feel; and in reflection, I am afraid that if I fail to convert to female genitalia; it could lead to serious consequences!
For example, in my whole life, I’ve only had one physical, back in 1999. That experience with Dr. Anderson still bothers me to this day. To make matters worse, I have a family history of male reproductive issues that might have affect me too. Considering that I am aware that something doesn’t feel right when self-checking, but I will do nothing to bring it to awareness to my physician as the experience would probably lead to suicide.
Romantically, I ‘cannot’ form relationships with males or females; as I won’t let anyone near me, or go to bed with me. No intimacy whatsoever, so I feel grossed out over the anatomical reactions of love.
I know that my adoptive father wishes that I’d at least try once, having sex with a woman, to be certain that this is what I really want to do; but I can’t imagine ever doing that, as I only desire intimacy and sexual stimulation as a female, not a male.
HRT has been a blessing and a curse, when it comes to my top dysphoria.
With hormones, I hardly get aroused (masculine); though this doesn’t mean I don’t have libido—it is just in different places. I am blessed with some shrinkage, and not having to deal with those sexual testosterone urges that use to hit me so hard, I’d be sick.
However, due to my morals and feminine identity and outward appearance; I am more aware of my male genitalia and find it now only a nuisance that I wish to be rid of, for once and for all.
7) With A New Year Coming Soon In A Few Hours; What Is Something You’d Like To Change For 2022?
A: I like to finalize my transition from male to female. I feel that once I am as close as possible to being female; I will begin the long process of healing both physically and spiritually.
8) With A New Year Coming Soon; What Is Your Focus For 2022 Regarding Your Ongoing Battle With Gender Dysphoria?
A: To continued looking towards the future and be happy. It has been a long road since I made my decision to transition. I must prepare for the knowledge that having GRS will probably be the hardest thing that I will ever endure!
#gender identity#gender reassignment#estrogen#transgender#transition#transgender pride#mtf woman#mtf lesbian#MtF trans#mtf#mtf hormones#male to female#maletofemale#new year#transgender assessment#gender assessment#assessment
18 notes
·
View notes
Text



Preparing for Kagura lessons
12 notes
·
View notes
Text



New Kimono for Sakura-Sakura
5 notes
·
View notes
Text

Getting ready for dance class!
#transgender#transformation#lgbtq#gender#trans#trans woman#mtf positivity#mtf woman#halloween#lgbt#actually mtf
13 notes
·
View notes
Text
I had a terrific Halloween!
Such amazing chance to be with wonderful people!








25 notes
·
View notes
Text
Stepping Back Into Public Volunteering
It hasn’t been since 2014 since I truly dedicated a whole week to volunteering in a public venue.
Before my transition, I had to learn to balance my skills, expectations, & dysphoria all at once.
I worked at a summer camp as a Outdoor Specialist, yet, when it came to expressing myself or acting as who I truly am…I was under so much stress.
This didn’t affect my production or quality of work…it actually increased productivity…but at a emotional cost and its aftermath was expressed in my outward physical discomfort.
Now, seven years later, I am returning to the same place where I worked as an employee; but this time as a volunteer.
This will be a great test to see if I truly am passing as female. And what other corrections I need to fine tune.
Will not lie, I am apprehensive!
I have thoughts of all the ways I could be emotionally compromised, but I tell myself:
“I am who I am meant to be! The opinions of others is not my concern. I am the best version of myself…as it is my true version.”
“I shall be fine.”
In reflection, I was thinking of how odd it will feel returning to a place that knew me as Radagast (our camp ID)(the no nonsense, strictly professional specialist); now to take on a new identity as Sirena (the —?).
And though I’ve worked and volunteered for this organization for over 9 years…this year is like starting on Year 1!
It is a complete new experience and view of the person I had to pretend to be…and the person I was born to be.
#transgender#transformation#lgbtq#gender#trans#lgbt#lgbtqa#lgbtq community#male to female#mtf hrt#gender dysphoria#dysphoria
2 notes
·
View notes
Text










PRIDE MONTH - Merfolk style!
Have a blessed Pride Month
#transgender#transformation#lgbtq#gender#trans#lgbt#lgbtqa#lgbtq community#male to female#mtf pride#ftm pride#transgender pride#trans pride#lesbian pride#pride month#pride love is love#love is love
28 notes
·
View notes
Text

Absolutely love this! It’s ‘mermazing’!
As a woman who loves mermaids and is trans! It’s perfect!
Please note, this isn’t my art. If anyone knows the artist, please identify them in the comments as people can like it too and purchase it (if desired).
They deserve all the credit!
Cheers!
#transgender#transformation#lgbtq#gender#lgbt#trans#lgbtqa#lgbtq community#male to female#mtf hrt#mermazing#mermaid art#mermaid
3 notes
·
View notes
Text

21 notes
·
View notes

