Text
The Bin Chronicles
The first thing you need to know about me is that I will not be - in any sense of the word - a reliable narrator.
In fact, being an unreliable narrator is exactly what makes me so uncomfortably authentic. I’m a person who struggles with mental illness writing about having a mentally ill experience in multiple mental facilities with other mentally ill individuals.
If you resonate with what you’re about to hear, I’m deeply sorry and hope you’re getting the care and support you need. If you don’t resonate with my story and are simply reading for entertainment, welcome.
Disclaimer about the word bin*
In case you’re wondering what “bin” means in the title of the book, The Bin Chronicles, let me tell you. It is shorthand for the term “looney bin”. It’s an affectionate joking term that some people use to refer to the psych ward. If anyone asks, I made it up.
Chapter 1 - The Drive
Clutching my bleeding forearm to my chest, I tried to wade through my sandbag heavy thoughts. Were the handfuls of ibuprofen I downed ever going to kick in? Would I get charged extra if I bled out in the Uber I impulsively scheduled? Should I have texted all those friends to see if they were awake enough to convince me to go to the ER? Did I even deserve to go to the hospital for something like this?
The piercing headlights of the approaching white sedan broke through my worrying. It was decided. At 1:39 AM on August 20th, 2023, I was going to head to the Massachusetts General Hospital emergency room for severe self-harm.
I’d like to say something inspiring such as “getting in the backseat of that Uber was one of the bravest choices I’ve ever made”. But I’d be lying. It didn’t feel like a brave choice. I didn’t even really want to get help. I just knew that the voice in my head telling me that I needed to cut deep enough to require stitches needed to be taken seriously.
The only memory my increasingly painkiller sedated brain encoded was the irony of being in this particular car. Never in my life have I had a kinder driver. He went above and beyond and offered me a phone charger and water. That had never happened to me before. Meanwhile, I was having one of the worst nights of my life. His warmth made the hot tears roll down my cheeks even harder, as the juxtaposition of a stranger’s kindness compared to my own deadly self-hatred felt like too much to bear. It would have looked like a completely normal ride had I not been holding my injured arm to my chest.
Now that the anxiety of whether or not I should get into the Uber subsided, a new worry popped up. Was the cut deep enough? If not, would they turn me away? I was determined to finally go inpatient and in my deranged mind I thought the only way to get there was to have a medical emergency. As these thoughts multiplied, I remember trying to take in the city and its beautiful florescent lights. For a split second, I felt true serenity being one of the only cars on the highway. With my arm starting to throb and soak through the gauze, the tranquility didn’t last.
Suddenly, everything looked familiar. I had worked at Massachusetts General Hospital for a year as a research coordinator. I recognized Flour Bakery + Cafe, the little coffee shop with the best butter chicken sandwich around, and the old watering hole where we used to drink after work, Harvard Gardens. I got to retrace my daily commute on Staniford Street passing a Domino’s pizza that made me salivate (yes I like Domino’s, don’t turn your nose up at me!) and a sub shop I never got to try, turning right onto Cambridge Street where I could never resist the Whole Foods next to my work at lunch time. Streets usually jampacked and bustling with cars and pedestrians commuting to and from work were eerily empty. No babies crying, dogs barking, no full hands with lunches and coffee or music blaring while bicyclists rode past. As I finally reached the main entrance of Mass General, a feeling of dread set in. I knew that I wouldn’t be going home that night.
I got out of the car. Part of me thought about getting right back in. I guess in that moment I did two things: I fulfilled my mission of taking myself to the ER and I not only admitted I needed help but brought myself to the place that could keep me safe. Once inside, I talked with the woman at the front desk. Everyone there was incredibly calm and kind and I immediately felt a sense of relief. They asked me some basic demographic intake questions like my age, DOB, the nature of the visit, whether or not I had current suicidal thoughts. Unlike my previous ER visit earlier that week, the first thing they did when they saw me was stitch me up. I’ll never forget that the provider doing them said it was almost too superficial to require stitches. While many people might feel comforted by that fact, I felt discouraged. I felt like I hadn’t made the cut deep enough which in turn made me believe I didn’t deserve to be at the hospital. I didn’t see the psych triage team that morning, but I finally fell asleep in a recliner.
Before I explain any further, let me tell you how I put myself in this minacious situation.
…
The weeks leading up to Mass General and eventually McLean Hospital were not pretty. I had been going through a depressive episode for the past 6 months if not longer, but during those last two weeks things had gotten much worse. One of the things I struggle with when I’m depressed is hygiene. Usually that takes the form of not taking my prescribed pills or brushing my teeth. Graphic, I know. Sometimes it involves not brushing my hair or taking showers too infrequently. This time it was all of the above. I felt hopeless consistently and I stopped enjoying things that had otherwise brought me joy.
At that time, I really enjoyed smoking weed and drinking daily. I stopped them both cold turkey. Another source of enjoyment for me was watching TV with my partner every day. During this period, I stopped being able to pay attention to our shows. Instead, I spent most of my time watching myself from outside and above my body. I couldn’t watch TV or hold a conversation without dissociating. Dissociation is a break in how your mind processes information. Dissociation can cause feelings of disconnectedness from your thoughts, feelings, memories, or surroundings. It can also mess with identity and sense of time. It can be a natural response to trauma, a way to cope with stressful experiences, or a symptom of mental illnesses like PTSD, depression, anxiety, bipolar disorder, or borderline personality disorder to name a few. Alternatively, it is sometimes a side effect of alcohol or taking or coming off of medications. For me, I either view myself from outside my body or stare blankly while being bombarded with anxious thoughts or none at all until someone snaps me out of it.
As soon as I lost interest in those aforementioned activities, I couldn’t bring myself to go back to them. I stopped eating. I struggle with a self-diagnosed weed-induced binge eating disorder where most of the time I restrict my food intake except for when I’m high. Once I stopped smoking, I lost my appetite completely. I wasn’t even restricting; I just had no energy to eat. I didn’t see the point in it anymore.
I couldn’t keep myself up past 8:30 at night. I’d blame it on the medications I was taking, but I can’t even do that because my psychiatrist and I took the one medication that was impacting my sleep, Abilify, out of the mix. Abilify is an antipsychotic that treats many different mental health conditions such as schizophrenia, bipolar I, autism spectrum disorder, and Tourette syndrome. What it does is balance the levels of dopamine and serotonin in the brain to help regulate moods, behaviors, and thoughts. We decided to stop the medication because I wasn’t feeling any positive or negative effects and I didn’t feel like it was contributing to our goal of getting me out of my depressed funk.
Now I had nothing to blame for my change in sleep but my depression. I would later learn from McLean how important it is to change the narrative from “my depression made me do this” to “my experience with depression made me feel this way”. It might sound like a small change, but what it does is stop you from making your illness your whole identity. Personifying depression can give it a life of its own, and it can be empowering to separate yourself from it by making these small linguistic changes. Now that I have that information, I can reframe the narrative to recognize that one of the symptoms of depression is sleep disturbance and that I was at the time experiencing that symptom rather than blame my depression as a whole for the situation.
I started moving slowly. I felt like I was wading through water any time I had to stand. My energy was at an all-time low. I couldn’t bring myself to get out of bed on the weekends and went right to bed when I got home from work. My bones ached. I felt tired all the time. I felt worthless. I felt like my life had no meaning, like I was merely a husk of my former self. I didn’t feel like I had any value to offer or bring to the world anymore.
I stopped paying attention at work because I couldn’t focus. I cried constantly and isolated myself from the rest of my coworkers. I had to step away from meetings because I couldn’t stop crying. I wasn’t able to keep up with my social life. I stopped calling my friends and didn’t return their calls when they reached to check in. This may sound like I’m beating a dead horse, and it most definitely is redundant, but I want to highlight what the signs of depression were for me. I hope this helps you to identify it in yourself or in someone else.[MOU1]
I felt like there was no reason for me to live and I fantasized about ending my life. I thought about all the ways in which I could kill myself and how to make it as painless as possible for my loved ones. I had recurring dreams about overdosing on painkillers. To make matters worse, I promised myself that I wouldn’t fail. I knew I didn’t want to end up fucking it up like I did the last time I attempted in 2020. I didn’t want to end up in the hospital or disfigured in some way. I just wanted it all to end.
On August 16th I cut so deeply that I needed stitches. I was on the phone with my partner Beau as he was driving home from work, and I just started cutting and couldn’t stop. The cut was actually a few days old, and it was already relatively deep. I’ve started doing this new thing where I cut in the same spot over and over again. I’m not sure why I switched from hurting myself in multiple places to the same one, but I know that this change is dangerous. It’s dangerous because it deepens the cut which can lead to needing hospital-level care.
Completely on brand, I decided to reopen this old wound and make it deep enough to require stitches. I think the reason I did this was because the other day when I made the initial cut, I called my ex roommate who is studying to be a doctor and she said that it might need stitches. Upon further inspection, she said it should heal on its own. I absolutely hated that she was right, and I wanted to prove her wrong. Welcome to my fucked up brain.
So on August 16th I reopened the wound and slashed at it until my partner came home from work. I couldn’t feel anything while it was happening, and I dissociate[MOU2] d as I watched myself deepen the cut from above my body. Before my partner got home I started rehearsing my smile and my coyness. But as soon as he opened the door, I caved. My cut was bleeding through the gauze, and it was having trouble clotting which was unsurprisingly really hard to hide.
I told him I thought I needed to go to the hospital. So off we went to Newton Wellesley Hospital. It was a surreal experience driving to the emergency room. I wasn’t in an ambulance, just a regular car. And there was that damn irony again, we could have been going anywhere. [MOU3] [MOU4] There I was, bleeding in the passenger seat, but there was no indication to the rest of the world that there was an emergent situation. No one knew I was hurting, inside and out, or that there was a wound acute enough to require stitches.
When we got to the hospital, Beau had me get out of the car so he could park. Upon entering the hospital, I was dismayed at how long the line was. I went all the way to the back and tried not to listen to other people’s conversations. I could smell the hospital: the pungent soapy yet flat geriatric scent that stops you from wanting to take a full deep breath in, the eye-watering bleach that they had used for God knows what, and the stench of stale discomfort and worry. I finally reached the front of the line and it was my turn to tell them why I was there. I strained to get the words out. “I’m here for self-harm”.
Suddenly, I’m treated like VIP. I don’t have to go back to the waiting room like everybody else. I now get to stay at the front of the line, and someone comes to check on me every 5 minutes. Finally, I’m brought back to a different part of the hospital along with a middle aged man who drank too much and took a spill. He keeps insisting that he’s not an alcoholic, and it becomes clear to me why they put us on the same unit: we were both there in a special part of the ER for those who purposefully harmed ourselves in some way. Or maybe it was that we were all dangers to ourselves. [MOU5] I was put on a bed in the hallway but I wasn’t there for long because someone from the psych[MOU6] team came to get me before offering me medical attention. The Psychiatry Triage team at Newton-Wellesley consists of independently licensed social workers. The way it works is people coming through the ER are first evaluated by the Emergency Department clinical team to ensure they are medically cleared. Then the social workers psychiatrically assess the patient to decide what the best level of care is for them. Looking back on this, it’s definitely weird that I wasn’t medically cleared first. Anyways, a nurse came to get me to help me put on scrubs. From there, the social worker and I went into an empty room and I was told to take any seat. I picked one and then was told to find another one, which to delirious me was the first sign that something wasn’t quite right.
The social worker sat far away from me and constantly had to lean in to hear me better. I told her what was going on, and that I wanted to do an outpatient program for Borderline Personality Disorder at McLean Hospital. This is a diagnosis I received in 2021. She laughed in my face and said it would take way too long to get off that waitlist. She asked me once if I wanted to go inpatient[MOU7] , but didn’t give me any information about the process. I declined, and she asked me why I had come to the hospital in the first place. I gestured toward my arm.
What is inpatient treatment you may ask? Here’s what I wish I knew when I was asked if I wanted to go…inpatient treatment is meant to be a short time in a psychiatric hospital to keep people safe during a mental health crisis. This is the most intensive treatment option for mental health, otherwise known as the highest level of care. What this term describes is different types of mental health treatment. This level of care includes hospitalization, whereas the lowest level of care refers to weekly or less often outpatient therapy sessions. Outpatient refers to a level of care in a non-residential setting where patients can live at home while participating in treatment. There are two main types of inpatient care: hospitalization and residential treatment. Hospitalizations are designed to be short term, often an overnight stay up to a few weeks long, and residential treatment often lasts 30 days or more. The focus of inpatient care is stabilization of the patient and developing a treatment plan for continuing their care once they are discharged. Hospitalizations are often thought of as a necessary safe place for those who are experiencing crisis, while residential treatment can help someone avoid a crisis before it escalates to that level. Inpatient can be voluntary which means you agree to seeking intensive care, or it can be involuntary which is referred to as involuntary or compulsory hospitalization where the person does not want to be at this level of care[MOU8] .
For context, inpatient units often look more like a college dorm than a hospital floor. There are both single and double rooms that often have their own bathroom that is shared with the adjacent room. There are also both group therapy and individual therapy rooms where you meet with psychiatrists, therapists, and group facilitators daily. There are common areas for eating, family visits, relaxing in places such as sensory rooms where there are comfortable chairs, fidget toys, and more, there’s always a nurses station where you take your meds, and there are offices for the staff and clinicians who you meet with on a weekly if not more frequent basis. This depends on if you are in a residential or hospital setting. These units are locked or secured environments, meaning that you cannot leave the unit without supervision. On the floor are a team of professionals including psychiatrists, psychologists, social workers, case workers, nurses, nutritionists, recreational therapists, occupational therapists, and mental health technicians to name a few.
After this awful interaction with the social worker, I was brought back to my hallway bed and was told to sit tight. A doctor came over and questioned if I even needed stitches, so I showed him my arm and he quickly covered it back up and agreed. To give you a visual, puffy fat [MOU9] was visible from my open wound[MOU10] . At first the deep groove filled up with dark red blood and you couldn’t see anything underneath. When they finally removed the rudimentary bandage I had made, that’s when you could see the true damage. According to my boyfriend the cut was about 3 inches long by an inch wide. While the left side of it was thinner, the right side of the wound was gaping. Yellow fat was visible almost in the shape of a bubble drawn flower and it was protruding a tiny bit past the wound. I could see a small black spot that I later learned was a vein. The fat looked bumpy and textured. No butterfly bandage could hold together what I had done to myself.
Hospital staff came over with an EKG and then they finally put me in my own room where x ray came over to look at my arm. Then the doctor entered the room with a huge syringe. He squirted it into my open wound with no regard for my pain tolerance. Then he began sewing the skin on my upper arm back together. Oddly enough, he never asked if the numbing medicine had kicked in. I can’t quite describe the feeling of the needle, but it was strange, dull, and felt far away due to the numbness. It looked exactly like stitching clothing, a long needle with a thin piece of string except there was a hook for the stitch which entered my arm on either side of the wound. This created small holes that filled with blood too. He told me not to look but I couldn’t help myself. I was grotesquely in awe. As he dabbed at the blood flowing from my open wound I thought I might be sick. When he was done, I had 7 blue stitches on my left arm. The doctor left as quickly as he came.
Then the nurse who had helped me undress and put on scrubs came back in. I told her that I had had an awful experience talking to the social worker. She said, “I’m sorry” and then walked out. Anothernurse overheard the conversation and said she could talk to the social worker for me. I almost let her advocate for me, but I was too scared that the social worker would come in and try to talk to me again, so I said no. She said she could look in the nurses station to see if another social worker was available. I thanked her. She came back with a list of crisis hotline numbers. I left disappointed with no aftercare plan in place. I texted my therapist about it, and she said that particular social worker was known to be a bitch. It’s still insane to me that the last thing I got that night was stitches when that’s all I went in for. It would be understandable to delay my stitches if they had properly gotten me set up with inpatient or outpatient care, but as you can tell that was not the case. I vowed to not go back to Newton Wellesley in the event of another mental health crisis.
…
When I returned home, my therapist made it clear that if I self-harmed again I needed to go directly to the hospital. Her and my psychiatrist both thought I needed to go back to the hospital regardless, but I didn’t want to leave work. I thought that leaving work for a medical emergency meant I wasn’t a good employee. That I wasn’t dedicated enough. To this day, I still feel that way.
Alas, I hung in there. For those of you who don’t go to therapy, therapists often use the phrase “hang in there” when the session is over and you’ve just unloaded five years’ worth of trauma into a fifty-five minute slot. I have always hated the phrase because I feel like it is minimizing. You’re contemplating ending your life? Just hang in there[MOU11] . Anyways, I “hung in there” for three more days.
I don’t remember what time it was on August 19th that I made my decision. In my head I suddenly had a plan. I would pretend for the rest of the day that everything was fine, that I was in a positive mood, and then at night I would cut to the degree of needing stitches again and take myself to the ER. I was actually really nice and generous that day. I bought my roommate and partner dinner and drinks. I kept up appearances. My partner commented on how good of a mood I was in and I cheerily agreed, suggesting that my depression must have finally gone away. On the inside, I was on a mission. All I wanted was for my boyfriend to go to sleep that night. I didn’t want him to take me to the ER because he had already helped me get to the ER for self-harm three days prior. It didn’t feel fair to have him take me for a second time in the matter of one week.
Somehow, I forced myself to watch part of a movie with him. As soon as he started to doze off, I got to work on my plan. I located my scissors. I went into the bathroom. I normally cut horizontally on my left arm. In perfect dissonance, I decided to cut vertically on my right arm. The pair of scissors I was using had gotten dull from years of use. I could barely cut my skin. It was also awkward because I’m a righty, so using my left hand to cut vertically was a challenge. I was listening to Call Your Mom by Noah Kahan [MOU12] on repeat. The pre chorus and chorus really haunt me.
“Stayed on the line with you the entire night
‘Til you let it out and let it in
Don’t let this darkness fool you
All lights turned off can be turned on
I’ll drive, I’ll drive all night
I’ll call your mom”
At the time I didn’t realize how much I was contemplating suicide. The idea of having someone on the phone with me who I could talk to about these feelings rather than acton them would have changed the course of my life. Having someone remind me that the darkness that I was feeling was temporary might have made me make a different decision. That night, I really needed someone to call my mom.
I took one earbud out of my ear so I could hear if my partner woke up. In the bathroom I felt too far away from my room, so I moved to the couch. I used my flashlight on my phone to see what I was doing. He stirred. I freaked out. He got up to use the bathroom and I quickly shut off the flashlight and put a blanket over the bloody scissors and blood-soaked napkins. Somehow he didn’t get suspicious and went back to bed. I started thinking about what I would take with me to the ER. Underwear is a must. Computer, computer charger. Piece of paper from work about FMLA resources. Phone charger. Scrub pants. Comfy clothes.
I got a plastic bag for my dirty supplies. While cutting didn’t hurt on the 16th, it hurt every second on the early morning of the 20th. I couldn’t stand it anymore. I packed my bag, took one last look at my room, and left my apartment. As soon as I got outside I started hyperventilating. In a very unlike me fashion, I proceeded to text a bunch of my friends to ask if they were up. 2 responded, 1 was busy. I called my friend from home and told her I needed to go to the hospital. She stayed on the phone with me until I got in the Uber.
#bipolor#borderline personality disorder#actually borderline#depressing shit#tw depressing stuff#self h@rm#suicide squad#mental health#mental illness#actually mentally ill#mental instability#mental institution#inpatient
2 notes
·
View notes
Text
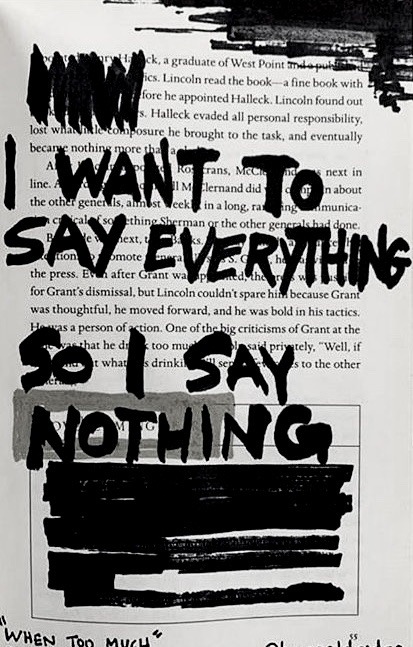
𝐈 𝐡𝐚𝐭𝐞 𝐰𝐡𝐞𝐧 𝐩𝐞𝐨𝐩𝐥𝐞 𝐚𝐬𝐤 𝐦𝐞 𝐡𝐨𝐰 𝐈 𝐟𝐞𝐞𝐥 𝐛𝐞𝐜𝐚𝐮𝐬𝐞 𝐭𝐡𝐞𝐧 𝐦𝐲 𝐦𝐢𝐧𝐝 𝐠𝐨𝐞𝐬 𝐭𝐡𝐫𝐨𝐮𝐠𝐡 𝐭𝐡𝐢𝐬 𝐞𝐧𝐝𝐥𝐞𝐬𝐬 𝐯𝐨𝐢𝐝 𝐨𝐟 𝐞𝐦𝐨𝐭𝐢𝐨𝐧𝐬 𝐚𝐧𝐝 𝐈'𝐦 𝐞𝐢𝐭𝐡𝐞𝐫 𝐟𝐞𝐞𝐥𝐢𝐧𝐠 𝐞𝐯𝐞𝐫𝐲𝐭𝐡𝐢𝐧𝐠 𝐚𝐭 𝐨𝐧𝐜𝐞 𝐨𝐫 𝐧𝐨𝐭𝐡𝐢𝐧𝐠 𝐚𝐭 𝐚𝐥𝐥 𝐬𝐨 𝐭𝐡𝐞𝐧 𝐈 𝐣𝐮𝐬𝐭 𝐞𝐧𝐝 𝐮𝐩 𝐬𝐡𝐫𝐮𝐠𝐠𝐢𝐧𝐠 𝐚𝐧𝐝 𝐬𝐚𝐲𝐢𝐧𝐠
“𝐈 𝐝𝐨𝐧'𝐭 𝐤𝐧𝐨𝐰“
7K notes
·
View notes
Text
if you can’t eat a whole meal, eat half. you ate, that’s what is important.
if you can’t get out of bed, try and sit up instead of lying down. it’ll be better for your back and your blood pressure.
if you can’t shower or have a bath today, try and brush your teeth and clean your ears. it’ll keep you a little cleaner, and we often forget those areas.
if you can’t get dressed today, change underwear and use some deoderant. it’ll leave you a little fresher until you have the strength to change fully.
and remember, i’m very proud of you. your best will look different every day, and that’s okay.
44K notes
·
View notes

