#Incretin Hormones
Text
Comprehensive Guide to Diabetes Medications
Welcome to this comprehensive guide on diabetes medications, where we shall explore the intricacies of various pharmacological agents that aid in effectively managing blood sugar levels and fostering a healthier life with diabetes.
1. Insulin Injections
Insulin, a paramount hormone synthesized by the pancreas, orchestrates the regulation of blood sugar levels, a critical facet for individuals…

View On WordPress
#biguanides#Blood Sugar Control#diabetes medications#DPP-4 inhibitors#edema#fluid retention#genital yeast infections#glucagon-like peptide-1 (GLP-1)#glucose regulation#glucose-dependent insulinotropic polypeptide (GIP)#heart disease#hypoglycemia#Incretin Hormones#injection site reactions#insulin injections#Insulin Sensitivity#intermediate-acting insulin#Liver Glucose Production#long-acting insulin#metformin#nephrons#pancreatic beta cells#Pancreatitis#Potential Side Effects#rapid-acting insulin#SGLT2 Inhibitors#short-acting insulin#sodium-glucose cotransporter 2 (SGLT2)#Sulfonylureas#Type 1 Diabetes
0 notes
Note
can you talk a little about wegovy and muonjaro for weight loss?
The answer is maybe.
If it were just the drugs themselves, I'd say absolutely. But there is a surprising amount of cultural baggage associated with these medications, and I don't really know that I can do them justice.

So first, let's talk about weight. There's a fantastic book called "Fat Talk" by Virginia Sole-Smith, about being overweight or obese in an age that prioritizes thinness, and how diet culture in particular is a threat to young people. Another, called "Intuitive Eating" by Elyse Resch, discusses how calorie restriction- commonly cited as the "way" to lose weight along with exercise- only works once or twice, because our bodies get wise to it and want to hold onto fat.
Humans evolved to gain weight. Fat is how we store energy for times when we might not have enough to eat. And if "not having enough to eat" (whether because of famine or because of calorie restrictive dieting) happens repeatedly, we have evolved to change hormones and metabolism so we a) don't need as much food to stay alive and b) are primed to eat more food than we need when it is available.
Aren't human bodies cool?
In the medical world, there are a lot of things tied to weight. For example, statistically, being overweight or obese means you're more likely to have health conditions like high blood pressure, diabetes, and heart disease. It is unclear, though, if those problems are caused by the weight itself, or other dietary, activity, and behavior patterns that may also happen to contribute to the weight gain. Things like a sedentary lifestyle, frequent consumption of foods with low nutritional value, avoidance of medical care due to stigma, or even chronic calorie restrictive dieting.
Unfortunately, due to this statistical tie, there is a lot of effort made in the medical world to get patients to "lose weight at any cost" instead of recommending dietary, activity, and behavior changes for health reasons alone.
Culturally as well, we prioritize thinness as attractiveness. I remember in high school there was a poster in my health classroom that read "Ideal weight- or it might be hard to get a date!". There are lots of negative associations with people who carry more weight, including that they are lazy or stupid- things that have nothing to do with body size.
Now, that doesn't mean that there aren't things that could be benefits of losing weight. For example, joint and back pain can be improved with weight loss. But weight loss is probably not the end-all be-all cure-all it's touted to be.
Because it is really hard for most people to meet this standard of "lose weight at any cost", there has long been medications that purportedly help people lose weight. Most of these medications have been stimulants, which decrease appetite and make it more comfortable to engage in calorie restrictive dieting. They also increase energy, which can make it easier to exercise or tolerate more exercise than would otherwise be possible.
Before we talk about the drugs, I want to say- there are risks and benefits to all medications, including these! The discussion you should always have is what risks are you and your healthcare provider willing to tolerate for the potential positive outcome. Also, this is a discussion of the drugs when used for weight control. The same drugs used for diabetes are at different dosages and have potentially different risk/benefit comparisons.
Ozempic/Wegovy (semaglutide) and Mounjaro/Zepbound (tirzepatide) are both a type of medication called a GLP-1 agonist. GLP-1 agonists are also called incretin mimics, because they mimic a type of hormone (incretin) that tells the brain and body that it is full. This makes it easier to eat a small amount of high nutrition food and feel satisfied. They also work by increasing metabolism. Between the decreased consumption and the increased metabolism, weight is lost.
Over the course of a year and a half, tirzepatide causes about 15-20% average reduction in body weight with continued use. Over the course of about the same time, semaglutide causes an average of about 15% body weight reduction with continuous use. Say, for example, you weigh 100kg. A year and a half on one of these medications could get you down to 85kg.
The problem is, as soon as that drug is withdrawn, the body realizes it was starving, and tries to compensate. These drugs are good at getting rid of weight, but maintaining a new weight usually means staying on a lower dose of the drug perpetually. Most people regain all weight (and potentially more than they lost) within 5 years of stopping the drugs.
Some studies suggest that repeatedly regaining lost weight may be more detrimental to health than remaining overweight or obese when it comes to statistical risk of type 2 diabetes, heart disease, and other "weight-associated" illnesses.
The main side effects are GI-related. Most of these are nausea, vomiting, diarrhea, gas/bloating, constipation, dizziness, and abdominal pain. More severe side effects include pancreatitis (inflammation of the pancreas) and gasteroparesis (paralysis of the stomach and part of the digestive tract).
41 notes
·
View notes
Text
The Ozempic Face: A Comprehensive Analysis
Ozempic (semaglutide) is a well-known medication used in the treatment of type 2 diabetes. Apart from its efficacy in managing blood sugar levels, it has also been associated with a unique side effect known as the "Ozempic Face." This article sheds some light on the phenomenon of Ozempic Face, exploring its definition, potential causes, symptoms, and management, as well as its relevance in the context of diabetes treatment.
Understanding Ozempic
Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist, a class of drugs that mimics the action of incretin hormones, leading to increased insulin secretion, decreased glucagon release, delayed gastric emptying, and reduced appetite. Semaglutide, the active ingredient in Ozempic, has been shown to be highly effective in improving glycemic control and promoting weight loss in patients with type 2 diabetes.
What is Ozempic Face?
The term "Ozempic Face" is not an official medical term but rather a colloquial expression used by patients and some healthcare professionals to describe a distinct change in facial appearance observed in individuals taking Ozempic. Reports suggest that patients undergoing Ozempic treatment may experience subtle alterations in facial appearance, such as fuller cheeks and a more youthful look. These effects are attributed to the medication's impact on subcutaneous fat and have garnered considerable attention in online diabetes communities and social media platforms.
Potential Causes
The exact mechanism behind Ozempic Face is not yet fully understood, and research in this area is limited. However, it is believed to be related to the medication's impact on adipose tissue, which is the body's fat-storing tissue located beneath the skin. Semaglutide's activation of GLP-1 receptors may affect adipocytes (fat cells) in a way that promotes fat storage and decreases fat breakdown, particularly in facial areas. Nevertheless, more research is needed to elucidate the underlying biological processes responsible for this phenomenon.
Symptoms of Ozempic Face
Patients who experience Ozempic Face typically report changes in facial features that include:
Fuller cheeks: One of the most commonly reported symptoms is a plumper appearance in the cheeks, giving a rounder and more youthful look.
Smoother skin: Some individuals notice a smoother texture to their facial skin, possibly due to increased subcutaneous fat.
Diminished wrinkles: There have been reports of reduced facial wrinkles or lines, contributing to a more rejuvenated appearance.
It is crucial to emphasize that these effects may vary between individuals, and not everyone taking Ozempic will experience Ozempic Face. Additionally, the intensity of these changes may differ from person to person.
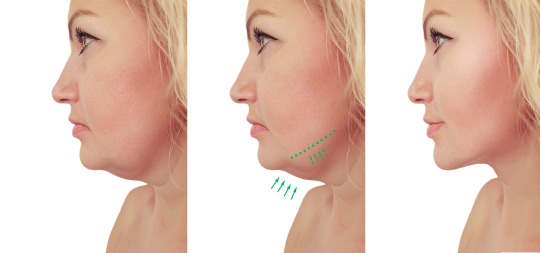
Management and Relevance
There are no specific guidelines or recommendations regarding the management of Ozempic Face. Since it is considered a cosmetic change rather than a medical concern, many individuals do not seek treatment for this side effect. If the changes in facial appearance become bothersome to the patient, they may consider discussing alternative treatment options with their healthcare provider. However, it is essential to weigh the potential benefits of Ozempic's efficacy in managing diabetes and promoting weight loss against any cosmetic side effects.
It's important to note that Ozempic Face is not a reason to discontinue Ozempic treatment, especially if the medication is effectively controlling blood sugar levels and promoting weight loss, which are critical factors in managing type 2 diabetes.
As with any medication, it is essential for patients to be aware of potential side effects and to have open discussions with their healthcare providers about their experiences. If patients are concerned about Ozempic Face or any other side effects, they should seek guidance from their healthcare professionals to make informed decisions about their diabetes treatment plan. Overall, Ozempic remains a valuable option in managing type 2 diabetes, and its potential side effects should be weighed against the benefits it offers in improving patients' quality of life and overall health.
2 notes
·
View notes
Text
Reviewing questions:
Screen Asian-Americans with BMI greater than 23 for DM
I remember hearing in OnlineMedEd or something that you should replace K+ if it's below a certain level before giving insulin to pts with DKA. I told my attending this and he didn't seem to know. It was in a question I just answered:
Restoration of fluid and electrolyte deficits is the first priority when treating patients with hyperglycemic crisis. Regular insulin is usually the next intervention, given while the patient is being hydrated with the first liter of normal saline unless significant hypokalemia (serum potassium less than 3.3 mEq/L) is present. Measured serum potassium increases approximately 0.7 mEq/L for each 0.1-unit decrease in pH. Insulin therapy should be withheld until plasma potassium levels exceed 3.3 mEq/L. If insulin is given it is initially administered as an intravenous bolus of 0.1 U/kg followed by an intravenous infusion at a rate of 0.1 U/kg/hr. Alternatively, it may be given as a continuous infusion at a rate of 0.14 U/kg/hr without an initial bolus.
Restoration of fluid and electrolyte deficits is the first priority when treating patients with hyperglycemic crisis. Regular insulin is usually the next intervention, given while the patient is being hydrated with the first liter of normal saline unless significant hypokalemia (serum potassium less than 3.3 mEq/L) is present. Measured serum potassium increases approximately 0.7 mEq/L for each 0.1-unit decrease in pH. Insulin therapy should be withheld until plasma potassium levels exceed 3.3 mEq/L. If insulin is given it is initially administered as an intravenous bolus of 0.1 U/kg followed by an intravenous infusion at a rate of 0.1 U/kg/hr. Alternatively, it may be given as a continuous infusion at a rate of 0.14 U/kg/hr without an initial bolus.
The American Diabetes Association recommends that patients with type 2 diabetes engage in 150 minutes or more of moderate- to vigorous-intensity aerobic activities spread over at least 3 days each week, in addition to 2–3 sessions of resistance training each week.
Although low-fat diets have traditionally been promoted for weight loss, studies indicate that diets that provide the same caloric restriction but differ in protein, carbohydrate, or fat content are equally effective. Monitoring carbohydrate intake and its impact on blood glucose levels is key for improving postprandial glucose control.
The American Diabetes Association (ADA) has concluded that reducing overall carbohydrate intake for individuals with diabetes has the most evidence for improving glycemia and can be applied in a variety of eating patterns.
Diabetic gastroparesis has generally been attributed to disturbed gastric emptying arising from autonomic neuropathy of the gastrointestinal tract. Associated with uncontrolled and suboptimal glycemic control, it commonly presents with symptoms of nausea, vomiting, abdominal pain, early satiety, postprandial fullness, bloating, and, in severe cases, weight loss. Although upper endoscopy is required to rule out an anatomic cause, the diagnostic gold standard for gastroparesis is the measurement of gastric emptying with scintigraphy of digestible solids at 15-minute intervals for 4 hours after food intake.
Diabetic gastroparesis is generally managed with a low-fat, low-fiber eating plan with small frequent feedings and nutritional drink supplements. Withdrawing drugs with adverse effects on gastrointestinal motility, including opioids, anticholinergics, and tricyclic antidepressants, is also recommended. GLP-1 receptor agonists such as exenatide slow gastric motility and should be avoided. Pramlintide, and possibly DPP-4 inhibitors, can also impact gastric motility and should be avoided.
Incretin hormones, which include GLP-1 and glucose-independent insulinotropic polypeptide (GIP), are released from the gastrointestinal tract after a meal. These hormones are responsible for 70% of postprandial insulin secretion. GLP-1 receptor agonists appear to lower blood glucose levels by potentiating glucose-mediated insulin secretion, suppressing glucagon secretion, slowing gastric motility, and increasing satiety. Insulin glargine should not be mixed with other forms of insulin due to the low pH of its diluent. It is a long-acting, acidic insulin analog soluble only at a pH of 4.0 (as provided in the clear solution in the prescription vial). Its reduced solubility at the physiologic pH it encounters following subcutaneous injection allows for its slow absorption rate.
HbA1c normally represents a weighted average of blood glucose levels during the preceding 120 days, which is the lifespan of a normal red blood cell. Any condition that prolongs the life of the erythrocyte or that is associated with reduced red cell turnover exposes the red cell to glucose for a longer period of time, resulting in higher HbA1c levels. Conditions associated with decreased red blood cell turnover include iron deficiency anemia, vitamin B12 deficiency, folate deficiency, and asplenia. Conversely, any condition that shortens the lifespan of the erythrocyte or that is associated with increased red cell turnover would tend to produce lower HbA1c levels. Examples would include hemolytic anemia, splenomegaly, and acute and chronic blood loss. Vitamin E ingestion has also been associated with lower HbA1c levels, presumably by interfering with glycation.
The GLP-1 receptor agonists such as exenatide and liraglutide are most likely to result in weight reduction.
The estimated prevalence of diabetes mellitus among adults was 7.4% in 1995 and is projected to rise to 9.0% by 2025. Screening every 3 years is recommended in asymptomatic adults beginning at age 45 in the absence of risk factors. Screening should be considered at an earlier age in patients who have a BMI ≥25 kg/m2 and one or more of the following additional risk factors:
• physical inactivity
• a first degree relative with diabetes
• a history of cardiovascular disease
• a Native American, Black, Hispanic, Asian, or South Pacific Islander race/ethnicity
• a blood pressure ≥140/90 mm Hg or receiving drug treatment for hypertension
• an HDL-cholesterol level less than 35 mg/dL
• a serum triglyceride level >250 mg/dL
• a medical condition associated with insulin resistance, including acanthosis nigricans or severe obesity
• a history of polycystic ovary syndrome, gestational diabetes, or delivering an infant weighing more than 4 kg (9 lb)
Insulin resistance is also found in more than half of patients without diabetes who experience an ischemic stroke or TIA. In the IRIS trial, the use of pioglitazone was associated with a 24% reduction in stroke and myocardial infarction and a 52% reduction in the risk of developing type 2 diabetes.
For patients with diabetes who are at high cardiovascular risk and whose cholesterol levels are controlled with statin therapy but who have elevated serum triglycerides (135–499 mg/dL), the American Diabetes Association (ADA) recommends the addition of icosapent ethyl (Vascepa) to reduce cardiovascular risk. Icosapent ethyl is highly purified eicosapentaenoic acid (EPA) ethyl ester fish oil. Use of this agent is supported by the REDUCE-IT trial. Use of icosapent ethyl resulted in a 25% reduction in the relative risk of the primary combined endpoint of cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, coronary revascularization, or unstable angina during a mean follow-up period of 4.9 years. This type of benefit has not been demonstrated in trials of other omega-3 fatty acid products and the lack of benefit from these other products may be related either to dosage differences or to their lower ratio of EPA to docosahexaenoic acid (DHA). The ADA has therefore recommended that the benefits of REDUCE-IT not be extrapolated to other omega-3 fatty acid products.
Niacin, which not only reduces serum triglycerides and LDL-cholesterol but raises HDL-cholesterol as well, has also not been shown to reduce cardiovascular risk when used in combination with a statin. Bile acid–binding resins such as cholestyramine and colestipol raise serum triglycerides and are contraindicated in hypertriglyceridemia.
In patients with dyslipidemia, lowering triglycerides with fenofibrate may slow the progression of diabetic retinopathy, particularly in those with very mild nonproliferative diabetic retinopathy at baseline.
For patients of all ages with diabetes mellitus and atherosclerotic cardiovascular disease, the American Diabetes Association (ADA) guidelines recommend that high-intensity statin therapy be added to lifestyle therapy. However, a high risk of myopathy and rhabdomyolysis is associated with high-dose simvastatin, and in 2012 the FDA issued a safety alert advising that the 80-mg dose of simvastatin be used only in patients who have been taking this dosage for 12 months or more without evidence of muscle toxicity. In this patient, simvastatin should be discontinued and another statin such as atorvastatin or rosuvastatin should be prescribed.
A supervised exercise program has been shown to improve functional status, walking distance, and quality of life in patients with peripheral artery disease. Although its use has not been associated with reduced cardiovascular risk or improved quality of life, cilostazol has been shown to improve walking distance. The use of low-dose aspirin (75–162 mg daily) is recommended by the ADA for diabetic patients with existing atherosclerotic vascular disease.
Claudication does not progress to critical limb ischemia in most patients with peripheral artery disease, with reported rates below 10%–15% over a period of 5 years or more. Given the risk of adverse procedural events, such as bleeding, renal failure from contrast-induced nephropathy, and the possibility of adverse limb outcomes, and the lack of proven benefit, the American Heart Association strongly recommends against surgical or endovascular intervention to prevent disease progression.
the choice of medication added to metformin should be based on the clinical characteristics and preferences of the patient. Considerations include cardiovascular risk, the presence of atherosclerotic cardiovascular disease, comorbidities, cost, safety, tolerability, and risk of adverse side effects. Although there is some evidence that metformin may reduce the risk of cardiovascular events and death, the evidence is most robust for SGLT2 inhibitors [-flozins]and GLP-1 receptor agonists [-glutides such as liraglutide, dulaglutide]. Large randomized, controlled trials have demonstrated significant reductions in cardiovascular events in patients with type 2 diabetes treated with an SGLT2 inhibitor such as empagliflozin, canagliflozin, or dapagliflozin, or a GLP-1 receptor agonist such as liraglutide, semaglutide, or dulaglutide.
For patients with type 2 diabetes, the ADA recommends that an SGLT2 inhibitor or a GLP-1 receptor agonist should be strongly considered, independent of baseline hemoglobin A1c or the individualized hemoglobin A1c target, for those with established atherosclerotic cardiovascular disease or indicators of high atherosclerotic cardiovascular risk, established kidney disease, or heart failure.
Indicators of high cardiovascular risk include a patient >55 years of age with left ventricular hypertrophy, or with coronary, carotid, or lower-extremity artery stenosis >50%.
Studies support a link between statin use and the development of diabetes mellitus. Intensive-dose statin therapy was associated with a higher risk of new-onset diabetes compared with moderate-dose statin therapy. In 2012, the FDA modified the package labeling of statins to include the risk of increased blood glucose levels and the development of type 2 diabetes. The benefit of statin therapy, however, outweighs the risk. It has been estimated that although use of statin therapy may cause one additional case of diabetes for every 498 patients treated for 1 year, its use also results in one less patient experiencing a cardiovascular event for every 155 patients treated for 1 year.
Nonalcoholic fatty liver disease (NAFLD) is one of the most common liver disorders and is strongly associated with obesity, insulin resistance, and type 2 diabetes. 20% develop nonalcoholic steatohepatitis (NASH), which by definition includes fibrosis, and 20% of patients with NASH will develop cirrhosis. Patients with steatosis are at higher risk for NASH if they are obese or have glucose intolerance, hypertension, hypertriglyceridemia, or metabolic syndrome.
NAFLD is often suspected on the basis of mildly elevated plasma aminotransferases or vague abdominal symptoms such as right upper quadrant pain. The degree of aminotransferase elevation does not predict the degree of hepatic inflammation or fibrosis, and a normal alanine aminotransferase level does not exclude a clinically important histologic injury or the presence of NASH. The diagnosis of NAFLD is typically based on hepatic steatosis found on liver ultrasonography. Scoring methods such as the FIB-4 can be used to determine if there is a risk of NASH and whether further testing such as a liver biopsy is indicated.
Lifestyle modification, particularly weight loss and exercise, represents the cornerstone of therapy. Weight loss, whether achieved by lifestyle changes or bariatric surgery, has been shown to have the greatest benefit on histologic improvement, with a recommended target weight loss of 7%–10%. Although there is some evidence to suggest that vitamin E and pioglitazone improve liver histology in NASH, there are no FDA-approved agents for treatment of NASH. It is generally recommended that patients with NAFLD avoid alcohol use. The presence of elevated hepatic transaminases in NAFLD does not contraindicate statin use, and guideline-directed medical therapy, which includes statin use, is recommended in patients with NAFLD because of their increased cardiovascular risk.
Resistant hypertension is present when the blood pressure of a hypertensive patient remains elevated above goal despite the concurrent use of three antihypertensive agents of different classes at adequate doses, including a diuretic. For patients with diabetes mellitus diagnosed with resistant hypertension, the American Diabetes Association guidelines recommend considering a mineralocorticoid receptor antagonist such as spironolactone.
Diabetic nephropathy develops in 20%–40% of patients with diabetes mellitus and is the leading cause of end-stage renal disease. Persistent albuminuria in the range of 30–200 mg/24 hr (microalbuminuria) is the earliest sign of nephropathy in patients with type 1 diabetes and is a marker for nephropathy in type 2 diabetes. Patients with microalbuminuria who progress to macroalbuminuria (>300 mg/24 hr) are likely to progress to end-stage renal disease over a period of years.
A random spot urine specimen for measurement of the albumin/creatinine ratio is the preferred method. A minimum of two of three tests showing a urine albumin level >30 µg/mg creatinine over a 6-month period confirms the diagnosis of microalbuminuria.
Intensive diabetic management and the use of ACE inhibitors and angiotensin receptor blockers (ARBs) have been shown to delay the progression from microalbuminuria to macroalbuminuria in patients with type 1 or type 2 diabetes.
current American Diabetes Association (ADA) guidelines recommend the use of either an ACE inhibitor or an ARB for those with a modestly elevated urinary albumin/creatinine ratio (30–299 mg/g creatinine) and strongly recommend them for those with a urinary albumin/creatinine ratio ≥300 mg/g creatinine.
ADA guidelines recommend against the use of these drugs for patients with normal blood pressure and no albuminuria.
The American Diabetes Association (ADA) recommends that patients of all ages with diabetes mellitus and atherosclerotic cardiovascular disease (ASCVD) should have high-intensity statin therapy added to lifestyle therapy
Aspirin at a dosage of 75–162 mg daily is recommended by the ADA as a secondary preventive strategy in patients with diabetes and a history of cardiovascular disease. The ADA also states that low-dose aspirin therapy could be considered as a primary prevention strategy for those with type 1 or type 2 diabetes who are at increased cardiovascular risk and not at increased risk of bleeding.
The LEADER trial (Liraglutide Effect and Action in Diabetes: Evaluation of cardiovascular outcome Results) was a double-blind trial that compared the use of liraglutide, a GLP-1 analogue, to placebo in 9340 patients with type 2 diabetes at high cardiovascular risk. After a mean follow-up of 3.8 years, liraglutide was found to significantly reduce the rate of death from cardiovascular causes, as well as the first occurrence of nonfatal myocardial infarction and nonfatal stroke
thiazolidinediones are associated with fluid retention, which can lead to weight gain, edema, and heart failure. Their use is contraindicated in patients with New York Heart Association class III or IV heart failure.
a weight reduction as small as 5%–10% was found to lower the risk of developing diabetes.
The American Diabetes Association recommends that patients with prediabetes achieve and maintain a minimum weight loss of 7%–10% and exercise a minimum of 150 minutes per week.
Metabolic syndrome is a constellation of cardiovascular risk factors related to hypertension, abdominal obesity, dyslipidemia, and insulin resistance. Ddiagnostic criteria for metabolic syndrome include the presence of three or more of the following:
• obesity, with a waist circumference exceeding 102 cm (40 inches) in men or 88 cm (35 inches) in women
• blood pressure ≥130 mm Hg systolic and/or 85 mm Hg diastolic
• a fasting glucose level ≥110 mg/dL
• a serum triglyceride level ≥150 mg/dL
• an HDL-cholesterol level less than 40 mg/dL in men or less than 50 mg/dL in women
#diabetes#DKA#gastroparesis#HgbA1c#diabetes management#hypertriglyceridemia#statins#albuminuria#metabolic syndrome
3 notes
·
View notes
Text
High-Purity Peptides for Cutting-Edge Research — Bionexus Technologies
High-Purity Peptides for Cutting-Edge Research — Bionexus Technologies
At Bionexus Technologies, we are committed to the innovation of high-purity peptides, manufactured under strict EU standards. Our products are designed for use in research studies, ensuring the highest levels of purity and effectiveness for research purposes.
What Are High-Purity Peptides?
Peptides are short chains of amino acids that play critical roles in various biological processes. In research, high-purity peptides are essential for consistent and reliable results. At Bionexus Technologies, we offer a wide range of peptides, each crafted to meet the rigorous demands of scientific research.
BPC-157 — High Purity BPC-157 for Regeneration Research
BPC-157 is a synthetic peptide derived from a naturally occurring protein in the stomach. This peptide is widely studied for its potential to accelerate tissue repair, particularly in muscles and tendons. Research indicates that BPC-157 may help reduce inflammation and promote healing in various injuries.
How BPC-157 Supports Muscle Healing
Studies show that BPC-157 enhances the body’s natural healing processes, offering promising results in muscle recovery and injury repair. Researchers are exploring its use in conditions like ligament damage and muscle tears.
DISCLAIMER: NOT FIT FOR HUMAN CONSUMPTION — ANIMAL STUDIES INFORMATION
MOTS-c — High Purity MOTS-c for Metabolic Research
MOTS-c is a mitochondrial peptide that plays a crucial role in regulating metabolic processes, particularly during times of stress. It is being investigated for its potential to improve insulin sensitivity and support weight management.
Benefits of MOTS-c in Metabolic Health Research
Research suggests that MOTS-c can enhance metabolic function, helping regulate glucose levels and promote weight loss. It has also shown promise in studies focusing on anti-aging and mitochondrial function.
DISCLAIMER: NOT FIT FOR HUMAN CONSUMPTION — ANIMAL STUDIES INFORMATION
PT-141 — High Purity PT-141 for Sexual Function Research
PT-141, also known as Bremelanotide, is a peptide primarily studied for its potential to improve sexual function. Unlike traditional treatments, PT-141 works by activating the nervous system, directly influencing sexual arousal rather than affecting the vascular system.
PT-141 in Research for Sexual Health
Early studies suggest that PT-141 may offer benefits in treating sexual dysfunction in both men and women, without the cardiovascular side effects common in other treatments.
DISCLAIMER: NOT FIT FOR HUMAN CONSUMPTION — ANIMAL STUDIES INFORMATION
Semaglutide — High Purity Semaglutide for Weight Loss Research
Semaglutide is a GLP-1 receptor agonist that has been extensively studied for its role in managing blood glucose levels and supporting weight loss. It mimics the action of incretin hormones, helping to regulate appetite and glucose metabolism.
Semaglutide’s Role in Obesity and Diabetes Research
Research shows that Semaglutide may reduce body fat and improve insulin sensitivity, making it a valuable peptide for studies on obesity and Type 2 diabetes.
DISCLAIMER: NOT FIT FOR HUMAN CONSUMPTION — ANIMAL STUDIES INFORMATION
Sermorelin — High Purity Sermorelin for Growth Hormone Research
Sermorelin is a synthetic peptide that stimulates the production of growth hormone by the pituitary gland. It is used in research focused on muscle growth, anti-aging, and recovery enhancement.
How Sermorelin Promotes Longevity Research
By increasing natural growth hormone levels, Sermorelin may support muscle development and recovery, contributing to anti-aging studies and longevity research.
DISCLAIMER: NOT FIT FOR HUMAN CONSUMPTION — ANIMAL STUDIES INFORMATION
TB-500 — High Purity TB-500 for Tissue Repair Research
TB-500, a synthetic version of Thymosin Beta-4, is studied for its ability to promote tissue regeneration. This peptide has shown promise in accelerating the healing process, particularly in muscle and tendon injuries.
TB-500 and Muscle Recovery Research
Research suggests that TB-500 enhances cellular repair and regeneration, making it an important compound in studies focusing on wound healing and muscle recovery.
DISCLAIMER: NOT FIT FOR HUMAN CONSUMPTION — ANIMAL STUDIES INFORMATION
Tirzepatide — Ultra High Purity Tirzepatide for Dual Hormone Research
Tirzepatide is a unique peptide that acts as both a GIP and GLP-1 receptor agonist. This dual-action mechanism is being researched for its potential to manage blood sugar levels and support weight loss.
Tirzepatide in Metabolic Health Research
With its dual-receptor targeting, Tirzepatide offers enhanced control of glucose and may support more effective weight management in obesity and diabetes research.
DISCLAIMER: NOT FIT FOR HUMAN CONSUMPTION — ANIMAL STUDIES INFORMATION
Explore More Peptides for Research at Bionexus Technologies
At Bionexus Technologies, we are dedicated to providing researchers with the highest quality peptides. Our products meet the strictest EU standards, ensuring that your research is supported by the best in peptide science. Visit our full catalog here.
#biotech#biotech and pharmaceuticals#biotechgrowth#biotechequipment#biotechindustry#biotechinnovation#biotechnology#ace attorney#biotechresearch#biotechrevolution#Longevity#Biohacking#AntiAging#HealthOptimization#WellnessJourney#FitnessSupplements#Recovery#MuscleGrowth#PerformanceEnhancement#YouthfulLiving#RegenerativeHealth#CellularHealth#HealthyLifestyle#HolisticHealth#LifeExtension#Vitality#OptimizedLiving#PeptideTherapy#Wellbeing#StrengthAndRecovery
0 notes
Text
Does Ozempic Cause Hair Loss?

Ozempic, a popular medication for type 2 diabetes management, has gained attention for its effectiveness in controlling blood sugar levels and supporting weight loss. However, as with any medication, potential side effects are a concern for patients and healthcare providers. One question that has surfaced among users is whether Ozempic causes hair loss. In this article, we will explore the available evidence, discuss possible mechanisms, and provide insights into managing and preventing hair loss while using Ozempic.
Understanding Ozempic
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist. It works by mimicking the incretin hormones, which stimulate insulin secretion in response to meals, slow gastric emptying, and reduce appetite. These actions help lower blood glucose levels and promote weight loss, making Ozempic an effective treatment for type 2 diabetes and obesity.
Hair Loss and Its Causes
Hair loss, or alopecia, can result from various factors, including genetics, hormonal changes, medical conditions, and medications. Common types of hair loss include:
Androgenetic Alopecia: A hereditary form of hair loss affecting both men and women.
Telogen Effluvium: Temporary hair thinning due to stress, illness, or medication.
Alopecia Areata: An autoimmune condition causing patchy hair loss.
Investigating the Link Between Ozempic and Hair Loss
Currently, there is limited direct evidence linking Ozempic to hair loss. Clinical trials and post-marketing data for Ozempic have not highlighted hair loss as a common side effect. However, some patients have reported experiencing hair thinning or shedding while using the medication. It’s important to note that individual reactions to medications can vary, and what affects one person may not affect another.
Possible Mechanisms
While Ozempic itself is not known to directly cause hair loss, several indirect factors could contribute to hair shedding in users:
Rapid Weight Loss: Ozempic can aid significant weight loss, which might trigger telogen effluvium, a temporary form of hair shedding often linked to rapid weight reduction.
Nutrient Deficiency: Weight loss, especially when drastic, can lead to deficiencies in essential nutrients such as vitamins and minerals necessary for hair health.
Stress and Health Changes: Managing a chronic condition like diabetes and adapting to new medications can be stressful, potentially impacting hair health.
Managing and Preventing Hair Loss
If you are experiencing hair loss while taking Ozempic, consider the following steps to manage and potentially prevent further hair shedding:
Consult Your Healthcare Provider: Discuss your concerns with your doctor. They can assess your overall health, review your medication regimen, and suggest appropriate interventions.
Maintain a Balanced Diet: Ensure your diet is rich in essential nutrients, including vitamins A, C, D, E, zinc, iron, and omega-3 fatty acids, which support hair health.
Manage Stress: Practice stress-reducing activities such as meditation, yoga, or deep-breathing exercises to support overall well-being.
Monitor Your Weight Loss: Aim for gradual weight loss rather than rapid reduction to minimize the risk of telogen effluvium.
Consider Supplements: If necessary, your healthcare provider may recommend supplements to address any nutritional deficiencies contributing to hair loss.
Conclusion
While there is no concrete evidence directly linking Ozempic to hair loss, individual reactions to the medication can vary. Rapid weight loss, nutrient deficiencies, and stress related to diabetes management and medication changes may contribute to hair shedding. If you are experiencing hair loss while taking Ozempic, consult your healthcare provider to determine the best course of action. By maintaining a balanced diet, managing stress, and monitoring your weight loss, you can support your overall health and potentially reduce the risk of hair loss.
1 note
·
View note
Text
JANUPILL 100MG Tablet
JANUPILL 100MG is primarily used to manage blood sugar levels in individuals with type 2 diabetes mellitus. It works by regulating the levels of insulin your body produces after eating.
How It Works: Sitagliptin, the active ingredient in JANUPILL, is a DPP-4 inhibitor (Dipeptidyl Peptidase-4). It increases the levels of incretins (GLP-1 and GIP), which are hormones that increase insulin release from the pancreas. This helps control blood sugar levels, especially after meals.
#chemist180#genericmedicinesonline#generic medicines#online medicine#side effect#bacterial infections#genericstore#nevlon caloe lotion 100g#genericmedicines
0 notes
Text
TERUJI! (WA) 0812-1440-8050 Terapi Untuk Diabetes Melitus Tipe 2 Ny. Djamilah Najmuddin di Cigending Bandung

Memori diperbarui
Pengobatan Diabetes Tipe 2
Diabetes tipe 2 adalah kondisi kronis yang mempengaruhi cara tubuh memproses gula darah (glukosa). Penderita diabetes tipe 2 mengalami resistensi insulin, di mana tubuh tidak dapat menggunakan insulin dengan efektif. Pengelolaan diabetes tipe 2 memerlukan pendekatan holistik yang mencakup perubahan gaya hidup, terapi obat, dan pemantauan kesehatan secara rutin. Artikel ini akan membahas berbagai aspek pengobatan diabetes tipe 2, termasuk metode terapi, pengobatan alternatif, dan cara mengelola kondisi ini selama kehamilan.
Pengobatan Diabetes Melitus Tipe 2
Diabetes melitus tipe 2 adalah jenis diabetes yang paling umum. Pengobatan untuk kondisi ini melibatkan berbagai pendekatan yang dirancang untuk mengontrol kadar gula darah dan mencegah komplikasi jangka panjang.
Perubahan Gaya Hidup
Mengadopsi gaya hidup sehat adalah langkah pertama dan paling penting dalam pengelolaan diabetes tipe 2. Ini mencakup:
Diet Seimbang: Mengonsumsi makanan yang rendah karbohidrat sederhana, tinggi serat, dan mengandung lemak sehat. Contohnya termasuk sayuran, buah-buahan, biji-bijian utuh, kacang-kacangan, dan ikan.
Olahraga Teratur: Aktivitas fisik seperti berjalan kaki, berlari, berenang, atau yoga dapat membantu meningkatkan sensitivitas insulin dan mengontrol berat badan.
Berat Badan Ideal: Menjaga berat badan yang sehat dapat mengurangi resistensi insulin dan meningkatkan kontrol gula darah.
Terapi Pengobatan Diabetes Melitus
Selain perubahan gaya hidup, banyak penderita diabetes tipe 2 memerlukan obat untuk mengontrol kadar gula darah mereka. Beberapa jenis obat yang umum digunakan termasuk:
Metformin: Obat ini membantu mengurangi produksi glukosa oleh hati dan meningkatkan sensitivitas insulin.
Sulfonilurea: Obat ini merangsang pankreas untuk memproduksi lebih banyak insulin.
Inhibitor DPP-4: Obat ini membantu meningkatkan kadar hormon incretin, yang membantu mengatur insulin dan glukosa.
Terapi Insulin
Meskipun lebih umum digunakan untuk diabetes tipe 1, insulin juga bisa diperlukan untuk diabetes tipe 2 jika kadar gula darah tidak bisa dikendalikan dengan obat oral. Terapi insulin melibatkan suntikan insulin harian atau penggunaan pompa insulin.
Pengobatan Diabetes Melitus Tipe 1
Meskipun artikel ini berfokus pada diabetes tipe 2, penting untuk memahami perbedaan dengan diabetes tipe 1. Diabetes tipe 1 adalah kondisi autoimun di mana tubuh tidak memproduksi insulin sama sekali. Pengobatan utama untuk diabetes tipe 1 adalah pemberian insulin harian, baik melalui suntikan atau pompa insulin.
Pengobatan Diabetes Melitus Tipe 3
Istilah diabetes melitus tipe 3 sering digunakan untuk merujuk pada hubungan antara diabetes dan penyakit Alzheimer. Penderita diabetes tipe 2 memiliki risiko lebih tinggi untuk mengembangkan penyakit Alzheimer. Penelitian menunjukkan bahwa resistensi insulin dan kadar gula darah tinggi dapat mempengaruhi fungsi otak.
Pengelolaan Diabetes Melitus Tipe 3
Pengelolaan diabetes melitus tipe 3 melibatkan kontrol ketat terhadap kadar gula darah, sama seperti pengelolaan diabetes tipe 2. Mengadopsi pola makan sehat, berolahraga teratur, dan menggunakan obat sesuai resep dokter dapat membantu mencegah atau memperlambat perkembangan penyakit Alzheimer.
Pengobatan Diabetes Kering
Diabetes kering adalah istilah yang sering digunakan untuk merujuk pada kondisi di mana kadar gula darah tinggi tetapi tidak ada gejala yang terlihat seperti pada diabetes basah (diabetes dengan komplikasi seperti luka yang sulit sembuh). Pengelolaan diabetes kering melibatkan perubahan gaya hidup dan penggunaan obat untuk menjaga kadar gula darah tetap dalam batas normal.
Pengobatan Diabetes Awal
Deteksi dini dan pengobatan diabetes sangat penting untuk mencegah komplikasi serius. Pengobatan diabetes pada tahap awal melibatkan:
Pemeriksaan Rutin: Melakukan tes gula darah secara rutin untuk memantau kadar gula darah.
Perubahan Gaya Hidup: Mengadopsi pola makan sehat dan berolahraga teratur.
Obat: Menggunakan obat yang diresepkan oleh dokter untuk mengontrol kadar gula darah.
Pengobatan Alternatif dan Terapi Refleksi
Selain metode pengobatan konvensional, beberapa penderita diabetes di Indonesia menggunakan pengobatan alternatif dan terapi refleksi untuk mengelola kondisi mereka.
Pengobatan Alternatif
Beberapa bentuk pengobatan alternatif yang populer termasuk penggunaan herbal seperti daun jambu biji, yang dipercaya dapat membantu menurunkan kadar gula darah. Namun, penting untuk berkonsultasi dengan dokter sebelum mencoba pengobatan alternatif untuk memastikan keamanannya.
Terapi Refleksi
Terapi refleksi melibatkan pijatan pada titik-titik tertentu di kaki yang diyakini dapat mempengaruhi organ-organ dalam tubuh, termasuk pankreas. Meskipun ada klaim bahwa terapi refleksi dapat membantu mengontrol diabetes, bukti ilmiah yang mendukung efektivitasnya masih terbatas.
Mengelola Diabetes Selama Kehamilan
Diabetes selama kehamilan, dikenal sebagai diabetes gestasional, memerlukan perhatian khusus untuk memastikan kesehatan ibu dan bayi.
Diet Seimbang
Mengonsumsi makanan sehat dengan indeks glikemik rendah dan menjaga asupan karbohidrat dapat membantu mengontrol kadar gula darah selama kehamilan.
Aktivitas Fisik
Olahraga ringan seperti berjalan kaki dapat membantu mengontrol kadar gula darah selama kehamilan. Konsultasikan dengan dokter sebelum memulai program olahraga.
Pemantauan Gula Darah
Pemantauan gula darah secara rutin sangat penting selama kehamilan untuk memastikan kadar gula darah tetap dalam batas yang aman.
FAQ (Pertanyaan yang Sering Diajukan)
Apa yang perlu diketahui tentang sindrom PCOS dan diabetes?
Sindrom Polikistik Ovarium (PCOS) adalah kondisi yang mempengaruhi hormon wanita dan dapat meningkatkan risiko mengembangkan diabetes tipe 2. Wanita dengan PCOS sering mengalami resistensi insulin, yang dapat menyebabkan peningkatan kadar gula darah.
Bagaimana cara mengelola diabetes selama kehamilan?
Mengelola diabetes selama kehamilan melibatkan diet seimbang, olahraga ringan, dan pemantauan gula darah secara rutin. Konsultasi dengan dokter sangat penting untuk memastikan kesehatan ibu dan bayi.
Apa yang perlu diketahui tentang hipoglikemia (rendahnya gula darah)?
Hipoglikemia adalah kondisi di mana kadar gula darah turun terlalu rendah. Gejala hipoglikemia termasuk keringat dingin, pusing, dan kebingungan. Penting untuk mengenali gejala ini dan mengonsumsi makanan atau minuman yang mengandung gula segera jika terjadi.
Bagaimana diabetes memengaruhi kesehatan mata?
Diabetes dapat menyebabkan berbagai masalah mata, termasuk retinopati diabetik, katarak, dan glaukoma. Kadar gula darah yang tinggi dapat merusak pembuluh darah di retina, menyebabkan penglihatan kabur atau bahkan kebutaan.
Apakah ada pengobatan alternatif atau terapi refleksi yang digunakan untuk mengobati diabetes di Indonesia?
Ya, beberapa penderita diabetes di Indonesia menggunakan pengobatan alternatif seperti herbal dan terapi refleksi. Namun, penting untuk berkonsultasi dengan dokter sebelum mencoba pengobatan alternatif untuk memastikan keamanannya.
Kesimpulan
Pengobatan diabetes tipe 2 memerlukan pendekatan yang komprehensif dan holistik, mencakup perubahan gaya hidup, penggunaan obat, dan pemantauan kesehatan secara rutin. Mengadopsi pola makan sehat, berolahraga teratur, dan menggunakan obat sesuai resep dokter adalah langkah-langkah penting dalam mengelola diabetes tipe 2. Selain itu, memahami dan mengelola komplikasi yang terkait dengan diabetes, seperti masalah mata dan hipoglikemia, juga sangat penting. Dengan pendekatan yang tepat, penderita diabetes tipe 2 dapat menjalani kehidupan yang sehat dan aktif.
Kontak dan Janji Temu Hubungi 0812 1440 8050 Balai Pengobatan Tradisional Ny. Djamilah Najmuddin merupakan sebuah klinik pengobatan tradisional yang sudah berdiri sejak tahun 1985 hingga sekarang dan bertempat di kota Bandung. menyembuhkan diabetes tipe 1,pengobatan penyakit diabetes insipidus,terapi farmakologi diabetes melitus tipe 2,terapi farmakologi dm tipe 2,gejala diabetes dan pengobatannya
Kontak dan Janji Temu Hubungi
Jl Guntur Madu No. 03
Kel. Turangga, Kec. Lengkong, Kota Bandung
0812 1440 8050
https://wa.me/6281214408050
Kunjungi website
https://djamilah-najmuddin.com
Baca juga :
#pengobatanpadadiabetesgestasional#pengobatandiabetestipe2#pengobatandiabetestipe1dan2#pengobatanuntukdiabetesmellitus#pengobatandiabetesyangbagus#tempatpengobatandiabetesmelitus#terapipengobatandiabetesmelitus#pengobatandiabetesdenganterapi#pengobatantradisionaldiabetes#pengobatanalternatifdiabetes
0 notes
Text
Choose Semaglutide for Effective Diabetes Management!

We offer Semaglutide, an innovative treatment for diabetes. It's a once-weekly injectable medication for managing type 2 diabetes, enhancing blood sugar control, and aiding weight loss. This GLP-1 receptor agonist mimics the natural hormone incretin to regulate insulin levels after meals while reducing appetite. For more details, contact Infinite30 at 984-777-8446.
0 notes
Text
Exploring Tirzepatide for Weight Loss: Mechanisms and Benefits
In the ongoing battle against the global obesity epidemic, the healthcare community has eagerly awaited the emergence of novel, effective, and safe treatment options. One such promising development is the dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, Tirzepatide for weight loss. This innovative drug has garnered significant attention for its potential to facilitate substantial and sustainable weight loss, revolutionizing the approach to managing obesity and associated metabolic conditions.
Tirzepatide, a synthetic peptide, represents a unique class of medications that simultaneously target two key incretin hormones – GIP and GLP-1. These hormones play pivotal roles in regulating glucose homeostasis, insulin secretion, and appetite control, making them attractive targets for obesity management.

Mechanisms of Action
The dual mechanism of action of tirzepatide is at the heart of its remarkable weight loss capabilities. By simultaneously activating both the GIP and GLP-1 receptors, tirzepatide elicits a synergistic effect that amplifies the beneficial metabolic responses.
Glucose Homeostasis and Insulin Sensitivity
GIP and GLP-1 are incretin hormones that stimulate insulin secretion in a glucose-dependent manner, helping to maintain optimal blood glucose levels. Tirzepatide's ability to activate both receptors enhances insulin secretion and improves insulin sensitivity, leading to better glycemic control.
Appetite Regulation and Satiety
One of the primary mechanisms by which tirzepatide facilitates weight loss is through its impact on appetite regulation and satiety. GLP-1 receptor activation is known to suppress appetite and promote feelings of fullness, leading to reduced caloric intake. GIP, on the other hand, has been shown to enhance meal-induced satiety. The dual activation of these receptors by tirzepatide results in a powerful synergistic effect, effectively curbing appetite and enhancing the sensation of satiety, making it easier for individuals to adhere to a calorie-controlled diet.
Energy Expenditure and Metabolism
In addition to its effects on appetite and satiety, tirzepatide has also been observed to influence energy expenditure and metabolism. GLP-1 receptor agonism has been linked to increased thermogenesis and fat oxidation, while GIP signaling has been associated with improved glucose and lipid metabolism. The combinatorial action of tirzepatide on these pathways may contribute to an overall increase in energy expenditure and a favorable shift in substrate utilization, potentially leading to greater weight loss.
Gut Microbiome Modulation
Emerging evidence suggests that tirzepatide may also have a positive impact on the gut microbiome, which plays a crucial role in metabolic health. GLP-1 receptor agonists have been shown to modulate the composition and diversity of the gut microbiome, potentially enhancing the production of beneficial metabolites and promoting overall gut health. This gut-mediated effect may further contribute to the weight loss and metabolic benefits associated with tirzepatide.
Clinical Evidence and Potential Benefits
The clinical evidence surrounding tirzepatide's efficacy in weight loss and metabolic improvements has been remarkably promising. Several large-scale clinical trials have been conducted, demonstrating the drug's ability to facilitate significant and sustained weight loss in individuals with obesity and overweight.
Substantial and Sustained Weight Loss
In the SURPASS-1 trial, individuals with type 2 diabetes who received tirzepatide experienced mean weight reductions of up to 15% from baseline, significantly outperforming the placebo and standard-of-care treatment groups. Importantly, the weight loss achieved with tirzepatide was found to be well-maintained over the long-term, highlighting its potential for sustained weight management.
Cardiometabolic Benefits
Beyond weight loss, tirzepatide has also been shown to confer important cardiometabolic benefits. Clinical studies have reported improvements in glycemic control, lipid profiles, and markers of insulin resistance in individuals treated with tirzepatide. These findings suggest that the drug may not only facilitate weight loss but also have a positive impact on overall metabolic health, potentially reducing the risk of cardiovascular complications associated with obesity and type 2 diabetes.
Improved Quality of Life
The substantial weight loss and metabolic improvements observed with tirzepatide have been accompanied by improvements in various aspects of quality of life, including physical function, self-esteem, and overall well-being. This holistic approach to obesity management is crucial, as it addresses not only the physical but also the psychological and emotional aspects of the condition.
Safety and Tolerability
One of the critical factors in the adoption of any new obesity treatment is its safety and tolerability profile. Tirzepatide has generally been well-tolerated in clinical trials, with the most commonly reported adverse events being gastrointestinal in nature, such as nausea, vomiting, and diarrhea. These side effects are often transient and tend to subside as the body adapts to the medication.
Importantly, tirzepatide has not been associated with an increased risk of serious adverse events, including cardiovascular events or pancreatitis, which have been a concern with some previous weight loss medications. This favorable safety profile, combined with its impressive efficacy, makes tirzepatide a promising addition to the arsenal of obesity management tools.
Conclusion
The emergence of tirzepatide as a novel dual GIP and GLP-1 receptor agonist represents a significant advancement in the field of obesity treatment. Its unique mechanism of action, targeting two key incretin hormones simultaneously, has demonstrated the ability to facilitate substantial and sustained weight loss, as well as meaningful improvements in cardiometabolic health.
The clinical evidence supporting tirzepatide's efficacy and safety profile has generated considerable excitement within the healthcare community, offering new hope for individuals struggling with obesity and its associated comorbidities. As research continues to elucidate the full breadth of tirzepatide's benefits, its potential to transform the management of obesity and contribute to improved overall health outcomes becomes increasingly apparent.
Ultimately, the emergence of tirzepatide as a therapeutic option for weight loss represents a significant step forward in the ongoing battle against the global obesity epidemic. By leveraging the synergistic effects of dual GIP and GLP-1 receptor activation, this innovative drug holds the promise of delivering meaningful and lasting weight loss, while also addressing the broader metabolic and cardiovascular implications of obesity. As healthcare providers and patients alike eagerly await the wider availability of tirzepatide, the future of obesity management appears to be taking a transformative leap forward.
0 notes
Text
Semaglutide: A Breakthrough in Diabetes and Weight Management
Semaglutide is a medication that has garnered significant attention in recent years for its dual role in managing type 2 diabetes and aiding in weight loss. Developed by Novo Nordisk, semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics the incretin hormones the body naturally produces to stimulate insulin secretion in response to meals. This article explores the mechanism, benefits, and growing applications of semaglutide in both diabetes management and obesity treatment.
Mechanism of Action
Semaglutide works by binding to GLP-1 receptors, which are located on pancreatic beta cells. This binding stimulates the release of insulin when glucose levels are high, thereby lowering blood sugar. Additionally, semaglutide inhibits glucagon release, reduces hepatic glucose production, and slows gastric emptying, all contributing to its glucose-lowering effects. This comprehensive approach helps maintain better glycemic control and has proven to be highly effective for patients with type 2 diabetes.
Benefits for Diabetes Management
Clinical trials have shown that semaglutide is highly effective in lowering HbA1c levels, a key marker of long-term blood glucose control. In several studies, patients treated with semaglutide achieved significant reductions in HbA1c compared to those treated with other GLP-1 agonists or placebo. This reduction translates into a lower risk of diabetes-related complications such as neuropathy, nephropathy, and cardiovascular diseases.
Moreover, semaglutide offers the convenience of once-weekly administration, improving adherence among patients who may find daily medications burdensome. Its ability to promote weight loss, a common challenge for individuals with type 2 diabetes, adds an additional layer of benefit, addressing both blood sugar control and obesity-related health risks.
Weight Loss Benefits
Beyond its efficacy in managing type 2 diabetes, semaglutide has gained recognition for its substantial weight loss benefits. In clinical trials, participants using semaglutide for weight management lost significantly more weight compared to those on placebo. The weight loss effects are attributed to its impact on appetite regulation and satiety, making it easier for individuals to reduce caloric intake and adhere to healthier eating patterns.
The STEP (Semaglutide Treatment Effect in People with Obesity) trials have highlighted these benefits, showing that higher doses of semaglutide (2.4 mg weekly) can lead to an average weight loss of around 15% of body weight over 68 weeks. This makes semaglutide one of the most effective pharmacological treatments for obesity available today.
Broader Health Implications
The benefits of semaglutide extend beyond diabetes and weight loss. Obesity is a major risk factor for numerous conditions, including cardiovascular disease, hypertension, and certain cancers. By effectively promoting weight loss, semaglutide can potentially reduce the incidence and severity of these conditions, offering a broader public health benefit.
Safety and Side Effects
While semaglutide is generally well-tolerated, some patients may experience side effects. The most common include gastrointestinal issues such as nausea, vomiting, and diarrhea, which tend to diminish over time. There is also a potential risk of thyroid C-cell tumors, as observed in rodent studies, though this has not been confirmed in humans. As with any medication, it is crucial for patients to discuss their medical history and any potential risks with their healthcare provider.
Also read about buy semaglutide online
Conclusion
Semaglutide represents a significant advancement in the treatment of type 2 diabetes and obesity. Its multifaceted mechanism of action, coupled with its effectiveness in both glycemic control and weight loss, makes it a valuable tool for managing two of the most pressing health issues today. As research continues and real-world experience grows, semaglutide's role in improving health outcomes is likely to expand, offering hope to millions of individuals struggling with diabetes and obesity.
1 note
·
View note
Text
Glucagon-like Peptide 1 / GLP-1 (7-36)
Glucagon-like Peptide 1 / GLP-1 (7-36)
Catalog number: B2016848
Lot number: Batch Dependent
Expiration Date: Batch dependent
Amount: 1 mg
Molecular Weight or Concentration: 3297.7 Dalton (30 aa) monomer
Supplied as: Powder
Applications: a molecular tool for various biochemical applications
Storage: -20°C
Keywords: Glucagon-like peptide 1, GLP-1, Incretin hormone
Grade: Biotechnology grade. All…

View On WordPress
0 notes
Text

At the heart of Mounjaro's efficacy lies its unique composition and mechanism of action. Known scientifically as tirzepatide, Mounjaro belongs to a class of weight loss injections designed to target not only weight reduction but also the amelioration of type 2 diabetes severity. Drawing inspiration from its predecessor, Wegovy (semaglutide), Mounjaro leverages the properties of incretins, natural hormones pivotal in regulating hunger, appetite, and blood sugar levels. However, what sets Mounjaro apart is its designation as a 'Twincretin,' which means it mimics the effects of two crucial incretin hormones: GLP1 and GIP. This dual action proves to be a game-changer, yielding an impressive average weight loss of 21%, surpassing the 15% achieved by Wegovy. https://semapen.co.uk/
0 notes
Text
Semaglutide Simplified: Where to Buy and How It Can Benefit You
In recent years, Semaglutide has emerged as a significant breakthrough in the treatment of type 2 diabetes and obesity. As its popularity grows, individuals are seeking reliable sources to purchase Semaglutide for personal use. This comprehensive guide aims to simplify buy semaglutide, detailing its benefits, considerations, and tips for making informed purchases, empowering individuals to understand its potential and make informed decisions about their health.

Understanding Semaglutide: A Brief Overview
Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA), a class of medications used to treat type 2 diabetes. It works by mimicking the action of the incretin hormone GLP-1, which stimulates insulin secretion, inhibits glucagon release, and slows gastric emptying, leading to improved blood sugar control. Semaglutide is also effective in promoting weight loss and reducing the risk of cardiovascular events in individuals with type 2 diabetes and obesity.
The Benefits of Semaglutide
Semaglutide offers a range of benefits for individuals with type 2 diabetes and obesity:
Improved Blood Sugar Control: Semaglutide helps regulate blood sugar levels by increasing insulin secretion and decreasing glucagon release. This leads to better glycemic control, reducing the risk of hyperglycemia and its associated complications.
Weight Loss: Semaglutide has been shown to promote weight loss by reducing appetite and food intake. Clinical trials have demonstrated significant weight loss outcomes in individuals with obesity or overweight who were treated with Semaglutide.
Cardiovascular Risk Reduction: In addition to its effects on blood sugar and weight, Semaglutide has demonstrated cardiovascular benefits, including reductions in the risk of major adverse cardiovascular events (MACE) such as heart attack, stroke, and cardiovascular death.
Convenience of Use: Semaglutide is available in injectable form, administered once weekly, which offers convenience for individuals who prefer less frequent dosing compared to daily medications.
Considerations for Purchasing Semaglutide
Before purchasing Semaglutide, consider the following factors:
Quality and Purity: Ensure that you purchase Semaglutide from reputable sources that provide third-party lab testing results to verify the authenticity and purity of their products. High-quality Semaglutide should be free from contaminants and meet pharmaceutical-grade standards.
Dosage and Administration: Follow dosage recommendations provided by healthcare professionals or the manufacturer. It is essential to consult with a healthcare provider to determine the appropriate dosage based on your individual health needs and goals.
Legal and Regulatory Considerations: Be aware of the laws and regulations regarding Semaglutide in your country or region. Semaglutide is a prescription medication and may be regulated or restricted in some jurisdictions.
Consultation with a Healthcare Professional: Before starting Semaglutide, consult with a healthcare professional, especially if you have underlying medical conditions or are taking other medications. They can provide personalized advice based on your individual health needs and goals.
Tips for Making Informed Purchases
To ensure a safe and satisfactory buying experience, consider the following tips when purchasing Semaglutide:
Research and Comparison: Research different brands and suppliers of Semaglutide. Compare product reviews, prices, and customer satisfaction ratings to find a reputable supplier that meets your needs.
Customer Reviews and Testimonials: Read customer reviews and testimonials to gauge the reputation and reliability of the supplier. Look for feedback from verified customers regarding product quality, effectiveness, and customer service.
Shipping and Return Policies: Familiarize yourself with the supplier's shipping and return policies before making a purchase. Ensure that they offer secure shipping methods and have a hassle-free return policy in case you are not satisfied with your purchase.
Customer Support: Choose a supplier that provides excellent customer support and is responsive to inquiries and concerns. A reliable supplier should be accessible via email, phone, or live chat to address any questions or issues promptly.
Conclusion: Harnessing the Benefits of Semaglutide
In conclusion, Semaglutide offers significant benefits for individuals with type 2 diabetes and obesity, including improved blood sugar control, weight loss, and cardiovascular risk reduction. However, it is essential to purchase Semaglutide from reputable sources, follow dosage recommendations, and consult with a healthcare professional before starting treatment. By following the guidelines outlined in this guide, individuals can harness the benefits of Semaglutide safely and effectively, empowering them to take control of their health and well-being.
0 notes
Text
https://youtu.be/iTeq9ijLKu8
youtube
Roux En Y Gastric Bypass Part 2 - Why is weight loss long lasting after 'Roux En Y Gastric
Bypass' while lifestyle modifications fail in long run? - Dr. Amar Vennapusa, +91 9676675646
In roux y gastric bypass, a small gastric pouch is created. Jejunum (Second part of small intestine) is divided and connected to the gastric pouch. In short, we are creating a short cut
between stomach pouch and small intestine.
Because of gastric pouch there is food restriction. Since part of the small intestine is
bypassed, there is malabsorption. But the main causes of weight loss or diabetes remission are not food restriction or malabsorption, these are due to physiological and genetic changes. Because of rapid emptying of stomach, undigested food reaches end of small intestine faster leading to increased hunger suppressing hormones, GLP1 and Peptide YY. Bypassing part of small intestine reduces anti incretins, further reducing fat set point. GLP1 and Peptide YY increase insulin production and reduce insulin resistance. So blood sugars are normalised.
Like this there are more than 200 hormonal changes and more than 5000 genetic changes. Fat set point is reset to a lower level leading to long lasting weight loss. Insulin production increases and insulin resistance comes down leading to long term diabetes remission.
For regular updates on bariatric and metabolic surgeries and healthy life style, please subscribe to my youtube channel @drVamar and follow my instagram page @drVamar
-
Dr. AMAR VENNAPUSA
Chief Consultant Bariatric & Metabolic Surgeon
Dr. Amar Bariatric & Metabolic Center
🌏 www.drvamar.com
📱 +91 9676675646
#obesity
#diabetes
#type2diabetes
#weightloss
#weightlossjourney
#weightlossmotivation
#weightlosstips
#bariatriccommunity
#bariatriclife
#bariatricsleeve
#drvamar
#obesitysurgery
#rouxenygastricbypass
#minigastrikbypass
#gastricsleevesurgery
#gastricsleevecommunity #gastricsleevebeforeandafter
#hyderabad
#healthylifestyle
#healthy
#healthyfood
#nutrition
#nutritionfacts
#overweight
#life
#health
#fitness
#fitnessmotivation
#fitnessmodel
0 notes
Text

Linagliptin, the primary ingredient in Trajenta, functions by inhibiting the DPP-4 enzyme. This enzyme plays a crucial role in breaking down incretin hormones, essential for blood sugar regulation. By blocking DPP-4, linagliptin elevates the levels of these hormones, leading to more effective control of blood sugar.
Click Here ::: https://bestgenericmedicine.com/product/trajenta-5-mg
0 notes