#PPROM
Explore tagged Tumblr posts
Text
So, maybe it’s not the right mindset, but I can’t get over how unfair it all is. All my life I’ve wanted to be a mom. I had my first kiddo at 34 with a donor and everything was perfect. Got with my husband a year later and had a miscarriage 9 months later. Found out the day before my birthday this year that I was pregnant again. Total surprise this time. Problem after problem from day one, but we finally started to feel like we were going to make it. Did an announcement and even a gender reveal. Then my water broke at 19 weeks and we lost our precious girl. And I just can’t get over how unfair it is. I see kids nobody wanted. I see kids horribly abused. I see moms having 10 successful pregnancies with reasonably healthy babies when they’ve used meth and heroin through the whole pregnancy. I tried so hard to do everything right.
7 notes
·
View notes
Text
Preterm Births and PROM Testing Market Shaping Maternal Health Strategies with Accurate Diagnostics
Preterm birth, defined as childbirth occurring before 37 weeks of gestation, remains a significant global health issue. With more than 15 million babies born prematurely each year, preterm birth is the leading cause of neonatal death and long-term neurological disabilities in children. Among the numerous complications associated with preterm labor, Premature Rupture of Membranes (PROM) — the spontaneous rupture of the amniotic sac before labor begins — plays a critical role. As healthcare systems worldwide strive to reduce the burden of preterm births and PROM testing market has gained significant traction.

PROM testing allows clinicians to determine whether the amniotic sac has ruptured, even when symptoms are subtle or not easily distinguishable from other conditions. Accurate detection is vital for appropriate clinical decisions, ranging from hospital admission to administering steroids for fetal lung development or antibiotics to prevent infection. Traditionally, PROM was diagnosed through methods like nitrazine paper tests, ferning tests, or visual pooling, all of which carried notable limitations in terms of sensitivity and specificity.
In recent years, the PROM testing market has evolved with the development of more sophisticated diagnostic tools. Immunoassay-based tests, such as those detecting placental alpha microglobulin-1 (PAMG-1) and insulin-like growth factor-binding protein 1 (IGFBP-1), have emerged as reliable alternatives to traditional methods. These advanced tests offer higher diagnostic accuracy, faster results, and are easier to administer in both hospital and point-of-care settings. As a result, they have gained widespread adoption across developed healthcare systems.
The global market for PROM testing is projected to experience steady growth in the coming years. This trend is driven by several factors. First, the increasing prevalence of preterm births—linked to lifestyle changes, rising maternal age, multiple pregnancies, and other medical conditions such as diabetes or hypertension—has amplified the demand for early and accurate diagnostics. Second, rising awareness among healthcare providers and patients about the risks associated with delayed or missed PROM diagnosis supports broader usage of testing kits. Third, ongoing technological advancements and the integration of diagnostics into maternal care protocols encourage the growth of the PROM testing market.
North America currently holds the largest share of the PROM testing market, owing to well-established healthcare infrastructure, early adoption of innovative diagnostic tools, and a strong focus on maternal and neonatal health. Europe follows closely, benefiting from government-supported health initiatives and increased spending on perinatal care. However, Asia-Pacific is expected to show the highest growth rate, propelled by large population bases, improving healthcare access, and growing investments in maternal health programs.
Despite its promising outlook, the market also faces certain challenges. The high cost of advanced diagnostic kits, especially in low- and middle-income countries, can limit widespread adoption. Moreover, lack of standardized testing protocols and differences in clinical practice across regions may hinder consistent implementation. Training for proper usage and interpretation of results also remains a concern in resource-limited settings.
However, opportunities continue to emerge. Collaborations between public health organizations and private diagnostic companies aim to expand the reach of PROM testing in underserved areas. Additionally, innovations in point-of-care diagnostics—portable, rapid tests that can be used even in remote clinics—are helping bridge the gap in accessibility. Digital health integration, including electronic health records and AI-assisted diagnostic platforms, further enhances test accuracy and facilitates timely clinical decision-making.
As governments and global health agencies intensify efforts to reduce neonatal morbidity and mortality, early intervention strategies, including effective PROM testing, are receiving stronger emphasis. Investments in maternal health education, clinical training, and technology will be essential in ensuring broader adoption and market growth.
In conclusion, the Preterm Births and PROM Testing Market is poised for sustained expansion due to increasing clinical need, rising awareness, and technological advancement. While challenges persist, strategic innovations and healthcare collaborations are paving the way for more accurate, accessible, and life-saving diagnostic solutions in maternal care. Ensuring early diagnosis through reliable PROM testing will remain a cornerstone in the global fight against preterm birth complications.
0 notes
Text
The short version of a very sad story.
I just had to say goodbye to my son, who was only 19 weeks into development. My wife suffered a preterm premature rupture of membranes (PPROM) at just the 12+3 mark. The amniotic sack ruptured, leaving the fetus in a precarious spot, but as long as the vitals checked out things had a chance of going okay, a small one. On Saturday (18+5), the umbilical cord fell out of her cervix, six centimeters, and we were promptly transferred to a women's hospital. Our son was medically aborted by induced delivered on Monday, and we said our final goodbyes to his remains on Tuesday. This kid fought like hell for his survival, and held on for nearly seven weeks. It's a shame it ended like this.
I might post the long version of this in the near future.
#tw death#tw child death#pregnancy#personal#tragedy#announcement#pprom#preterm premature rupture of membranes
0 notes
Text
[150] The Sims
Last prenatal check-up, this time it was friends/family and Sabo had PPROM again (like with Roule) so it is best to be alert that the delivery may come early or the date may change.
Everyone thinks Sabo's new haircut is cute, I still don't like it, but since Sabo and Law like it, I'll leave it longer.
In another universe, Koala is the alpha who impregnated Sabo, just look at her reaction... I love her, that little girl is alpha *chuckle*
55 notes
·
View notes
Text
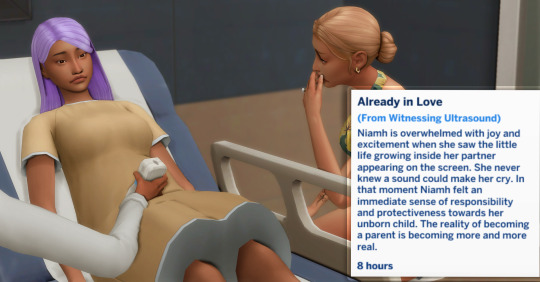
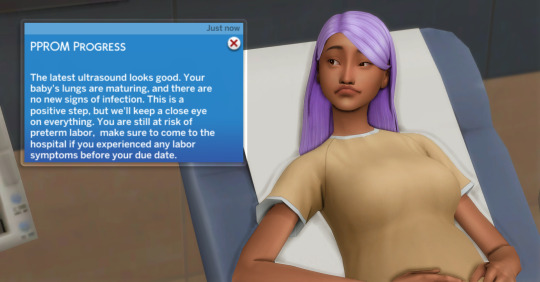
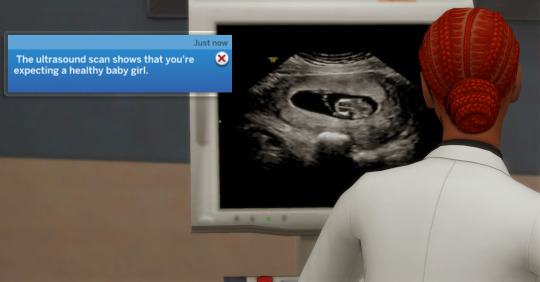
Zelda got some good news- her PPROM is improving. Even more exciting, Zelda and Niamh found out they're having a little girl!🎀This family has a streak of having firstborn girls😂
9 notes
·
View notes
Text


30 weeks 1 day
We have been in the hospital for a week now due to PPROM at 29 weeks. It was touch and go for a while but as long as we remain stable then we will be here for 4 more weeks where we will then deliver at 34 weeks. I have good days and bad days. I’ve mostly come to terms with everything for now but I know that when the time comes to deliver and our NICU journey begins I will have to go through all of the emotions again. Right now I feel guilty that she’ll be a premie and will have to spend time in NICU and I also feel guilty for Aubrey and Hazel because it is summer time and I’m stuck in the hospital and they miss and need me. I also feel sorry for Alex, this is his first baby and I am so sad for the moments that we will miss out on. One thing that I haven’t admitted out loud is how angry (jealous) of others around me who are carrying to full term, delivering their babies and getting to hold them, getting those sweet, quiet first few hours, getting to take them home with them and I won’t have any of that. It’s just hard right now but I am thankful for my support system and that this didn’t happen earlier
3 notes
·
View notes
Text
I don't know that I like third year. It's an adjustment. I'm sure it will be fine, eventually. But it's hard, and it's a different vibe, and it's struggling to find my place.
Looking at the interns, I do see how far I've come. I was in their shoes, once: struggling to find a cervix, falling behind with inductions/mag notes/strip notes/postpartum calls, scared of decelerations, unsure how to piece the clinical picture of labor together. I'm efficient with things I know how to do. Keep me to ante/gyne and I'm ON TOP of blood pressures, blood sugars, consults, antepartum calls etc. I feel pretty good about up-titrating blood pressure medications, deducing superimposed preeclampsia from chronic hypertension exacerbations, managing PPROM +/- PTL. I've read a lot. I think my signouts are decent.
But now as a third year, the antepartum "chief", I am really, really struggling. Now I have to delegate. I need to figure out what things I do, what things I have the second year do. When my actual R4 L&D chief is off the floor, I'm then in charge of everything (including training the day 3 intern). What's REALLY hard is the power dynamics. I'm in charge of the antepartum service, but my R4 is still in charge of me. And then on top of that, different R4s have different opinions, and then I get caught in the middle!!! A patient came into triage today, ruptured with twins, concern for preterm labor. I was told to let the R2 see her. I did, then sent the R2 home. Then the night team told me I should have seen her instead. And the R2 should be doing XYZ. And my signout wasn't well-prepared enough about her (even though I thought it was decent). Which to the first point, like, fair. I tried to have my R2 doing the XYZ. But I was also told to have her see the triage patient. So then it's like I'm in charge, but actually I'm in "charge", and the different people who are ACTUALLY in charge have different ideas about how to do things, but then it's either I take the blame or throw someone else under the bus.
And obviously, there are learning points. I can always know more about the patients. I think I did a fine job, especially since I've been on MFM/antepartum for TWO MONTHS STRAIGHT, but I do need to know the patients I don't admit a little better. And when my R4 can't come to signout, I really should know the floor better. These are things that will come with time, I'm sure. I am three days into my first time being a senior. I'm learning not only how to cover an ENTIRE service, but also how to manage an intern who needs to learn, well, literally everything. And can't do anything by herself yet. (Like I said, it's fine, we were all there at some point.)
But it's really, really hard to be told to do your job different ways from different people, and then you have to take responsibility for it anyway, and also you're supposed to be in charge of a service but you're not really.
And also, I have tomorrow off, but there's still hot as fuck drying equipment all over my apartment, and it's ninety degrees in here, and I can't play PC games without tripping the breaker. So I guess I'll just sit alone in the heat and be miserable.
Oh well. I ranted to like. Three of my friends. And here. I'll feel better eventually. Residency is really hard, and in really unexpected ways.
7 notes
·
View notes
Text
34+6
I got an ultrasound when I was admitted on Tuesday and apparently they found a placental lake which they believe, in this case, is the start of an abruption. I slid and fell on ice at 33+4 and was in the hospital overnight for monitoring, which is when they assume it happened. They said it very well could've been what weakened my membranes causing the PPROM. They also have said that baby boy looks incredible, not a single sign of distress and I haven't been contracting and we have lots of hope he'll stay in until 36 weeks and hopefully avoid most of the NICU stay.
4 notes
·
View notes
Text
Highlights of the internship - Week 7:
• Identifying aortic dissection on CT and the attending being so proud that he talks about it even in the OR. “Do you know what she has recognised today??”
• Had to hold and protect intestines from any possible damage for such a long time that I am glad my spine does not have a new distorted shape now because of my wrong and bad position.
• I could close the half of the subcutaneous tissue and skin on a midline incision simultaneously with a resident, I can feel that I gain speed and it does make me content.
• The fact that all the C-sections I have attended in this week came across with the same doctor feels like I am part of his team now haha.
• I didn’t do surgery like my attending said but I assisted him at one, there was only one nurse so I was more active.
I was melt by his words when I opened the topic of residency during this surgery; “I would love to have you as a resident here and work with you. If you choose this hospital, I will provide you all the opportunities to equip you as best as I can for this job.
“Either way, I know that you will be a known and respected doctor in the OB/GYN community.” 🥹
• During a conversation about some kids’ relationship with their doctor father, a nurse insinuated that I must have chosen medicine because of money after my attending mentioned that my father is doctor too. How all this ended after she was not convinced by me that it is not right was my attending trying to defend me with saying that I chose it because I must have emulated my father’s job. That is right but she didn’t believe.
• While watching an operation which was getting done by some residents, my shoulder has been poked behind my back by my attending. I turned my head only to hear him saying, “look, you are going to be doing these operations if you come here.” Way to steal my heart and mind.
• An OB/GYN doctor has talked to me for about 30 minutes about why I should not choose this specialty. I can see his points about it being really demanding and requiring sacrifice from your social life, etc. However, one point of him was rather disturbing, I don’t even call it a point; at surgery, it is like testosterone in women increases because they lose femininity. Will your husband put up with your testosterone? There will be more femininity at others.”
The way, some of them wants me to plan my life on a non-existent husband 🤦🏻♀️
And I did definitely mentioned about this to my attending, how nobody around ever says OB/GYN is good. “Okay, fine, let’s say it is bad. But you obviously do love bad, you can choose it.
“There has got to be some people who will choose it. If people like you or me don’t it, then who will?”
• Found fetal heart on ultrasound by myself!!
• After my first time doing it at 4th year, I again did curettage for abortion with the same doctor. Memoriesss!!
• I had my first weekend shift of OB/GYN at this week. What are the odds of two women who were pregnant with twins coming in for PPROM at about the same gestation weeks and getting admitted for urgent C/S in the same day? Also to the same doctor of whose C/S operations I have been attending in the previous days? We really are about to become a team haha
#ob/gyn#internship#6th year#medical student#medical stuff#medical school#medblr#night shift memories
2 notes
·
View notes
Text
Legacy Stories
Update #27
Settling in and new additions!












When Luna went to Uni she had to leave Kitana at home with her parents. While at Uni, Kitana had a couple of litters of kittens. When they moved, Luna and Ty took Kitana and her youngest kitten Bobie with them. The family spent a while getting settled in to the new house and then one day Luna discovered that she was pregnant. Both her and Ty were very happy. At her first scan, however, she was diagnosed with PPROM and this along with the previous miscarriage made Luna nervous.
0 notes
Text


Millie went for her checkup...things don't look good, amongst finding out that she's having TRIPLETS, she been diagnosed with PPROM. She worried for her and her unborn babies' health, but her obstetrician helped soothe her worries by giving her a shot that'll help with her diagnosis.
#ts4#sims 4#the sims 4#simblr#the sims community#ts4 simblr#black simblr#ts4 screenshots#sims 4 gameplay#sims 4 screenshots#the sims 4 growing together#the sims 4 legacy#The James Family
0 notes
Text
[20] The Sims
I knew something bad was happening, being a 14-year-old teenager it was obvious that Sabo would have problems with the pregnancy, but it makes me sad to see my sims sad...
Sabo has not gained weight because he has anemia, he does not assimilate food well and he is depressed, but the ultrasound showed that he has PPROM (Premature Rupture of Membranes) just when he is three months old.
Now I'll have to take extra care of Sabo, and Law still has to take the final exams and send his letters to apply for a place at the Universities. There's also the prom and graduation... Omg, first time playing a game Sabo gets pregnant so young and has so many difficulties. I'll blame Law, hormonal sim *lol*
Same in the tiktok poll, everyone supports the pregnancy -as Law asked-, so there was no abortion -as Sabo wanted- And now it's my turn to save that baby who will be Roule, obviously.
57 notes
·
View notes
Text



Zelda woke up feeling a bit off. Her second trimester appointment wasn't for a few more days but she decided to go early in case there was a problem. She found out that, in addition to her PPROM, she also has preeclampsia😅
5 notes
·
View notes
Text
Here is the actual Jezebel article and since it's Jezebel you know they're going to be totally honest.
The woman was almost 16 weeks pregnant and experienced PPROM (preterm pre-mature rupture of the membranes) and this article claims that the treatment is either induced labor or abortion and further claims that the ER doctor told the woman they couldn't induce her because of the abortion ban but I call bullshit.
First of all, nowhere is abortion described at the treatment for PPROM. Since it was preterm PROM she should have been admitted to the hospital. Not sent home.
Generally, patients with preterm PROM should be admitted to hospital with periodic assessment for infection, placental abruption, umbilical cord compression, fetal well-being, and labor. Periodic ultrasound evaluation should be performed to monitor fetal growth as well as periodic fetal heart rate monitoring. Vital signs should be monitored and a rise in maternal temperature should raise suspicion for an intrauterine infection. Serial monitoring of leukocytes and inflammatory markers have not proved to be useful in diagnosing infection as they are found to be nonspecific if there is no clinical evidence of infection. Administration of corticosteroids will also cause a transient leukocytosis.
The treatment for PPROM is either to induce labor or be admitted to the hospital on bed rest while doctors monitor the woman and her baby and to try and progress the pregnancy to at least 34 weeks before delivering the baby. It is not ever abortion.
Abortion laws absolutely do not prevent either inducing labor or admitting and treating a woman who is experiencing PPROM.
If the doctor truly did say that they "couldn't induce" her because of abortion laws and just sent her home that was a lie and serious malpractice and that doctor should lose their medical license.
Please stop spreading disinformation.


1K notes
·
View notes
Text
Premature Birth: Signs, Causes, Complications, and Treatment

Premature birth, or preterm birth, is when a baby is born before 37 weeks of pregnancy, whereas a full-term pregnancy lasts around 40 weeks. This early delivery can lead to various health problems, making it crucial for expectant mothers to understand the signs, causes, and treatment options.
What is Premature Birth?
Premature birth happens when delivery occurs before 37 weeks of pregnancy. It is the leading cause of death in children under five and can result in lifelong disabilities. Premature births are categorized based on gestational age:
Extremely Preterm: Born before 28 weeks
Very Preterm: Born between 28 and less than 32 weeks
Moderate to Late Preterm: Born between 32 and 37 weeks
Signs and Symptoms of Premature Birth
Call your doctor immediately if you notice any of these signs before 37 weeks of pregnancy:
Regular Contractions: Tightenings or cramps that come at regular intervals, sharp backache, or persistent pelvic pressure.
Fluid Leakage: Gushing or trickling of fluid from the vagina, especially if the fluid is discoloured.
Vaginal Bleeding: Any bleeding during pregnancy.
Decreased Fetal Movement: A noticeable reduction in your baby’s movements.
Early detection and treatment can help prevent complications and improve outcomes for both mother and baby.
Causes of Premature Birth
Premature birth can occur spontaneously or be medically induced. Common causes include:
Previous premature birth increases the risk.
Placental problems, such as placental abruption or placenta previa.
Abnormal amounts of amniotic fluid.
Preterm premature rupture of membranes (PPROM).
Uterine abnormalities or a short cervix.
Multiple pregnancies (twins, triplets).
Chronic maternal health conditions like high blood pressure or diabetes.
Pregnancy-related conditions such as preeclampsia or gestational diabetes.
Infections and fetal growth restrictions.
Risk Factors
Being very young (under 18) or older (over 40).
Higher incidence in Black women compared to other ethnicities.
Being underweight or overweight before pregnancy.
Smoking, alcohol use, or illicit drug abuse.
High levels of stress or depression.
Diagnosis
Doctors diagnose premature birth through:
Pelvic Assessment: Checking cervix dilation and uterus firmness.
Ultrasound: Measuring cervical length and assessing fetal and placental issues.
Uterine Monitoring: Measuring contraction duration and spacing.
Urine Test: Checking for bacterial presence.
Treatment
For preterm labour or risk of premature birth, treatments may include:
Antenatal Steroids: To help mature the baby’s lungs faster.
Tocolytic Medications: To delay labour temporarily.
Antibiotics: To prevent infections if water breaks early.
After birth, premature babies often need specialized care in the NICU, including:
Incubator Care: To maintain body temperature.
Respiratory Support: Using ventilators or CPAP machines.
Feeding Assistance: Initially through IV or feeding tubes.
Phototherapy: To treat jaundice.
Complications
Premature birth can lead to:
Short-term complications: Breathing problems, heart issues, brain problems, digestive issues, blood problems, metabolism problems, and immune system problems.
Long-Term Complications: Cerebral palsy, learning disabilities, retinopathy of prematurity, hearing loss, enamel defects, and increased risk of conditions like autism spectrum disorder.
When to See a Doctor
Contact your doctor if you experience:
Regular contractions or tightenings.
Excess fluid leakage.
Vaginal bleeding.
Reduced fetal movements.
Persistent pelvic pressure.
Prevention
To reduce the risk of premature birth:
Maintain a Healthy Weight: Through a balanced diet and exercise.
Stay Active: To reduce risks of complications.
Manage Stress and Depression: Seek help if needed.
Quit Smoking and Avoid Alcohol: For a healthier pregnancy.
Check Medication Safety: Ensure medications are safe for pregnancy
Prevent Infections: Practice good hygiene.
Even with no identifiable risk factors, regular prenatal care is essential.
Conclusion
Premature birth is a complex issue with significant implications. Understanding the signs, causes, and potential complications can help expectant parents manage this challenging situation. With advances in medical care, many premature babies lead healthy lives. For comprehensive care, choose the best hospital in Varanasi.
For personalized care and support, visit Arvachin Hospital, a leading medical facility dedicated to providing top-notch healthcare.
0 notes
Text
34+5
We were admitted with PPROM yesterday. I was actually thinking of making a post about how we set our induction to be on the 7th of February and baby boy just could not wait. My water broke yesterday around 2pm. So almost 13 hours ago. No contractions currently and baby boy sounds great on monitors. He was measuring just under 6lbs when we did a growth last night. They want me to get to 36 weeks and we'd induce that day but they won't stop my labor if it starts before that since I'm already passed 34 weeks.
I got steroids at 28 weeks due to knowing we were inducing at 37. And I got a rescue dose last night. I'm on antibiotics every 6 hours currently and nsts twice daily. Praying for little to no NICU time but these next 9 days are gunna be long. If anyone has any recommendations for stuff to keep occupied? I can barely sleep in a hospital and I'm on bed rest in hopes to avoid contracting. I'm sure I'll be updating lots out of pure boredom
4 notes
·
View notes