#cardiac output
Explore tagged Tumblr posts
Text
Normal Range and Factors Affecting Cardiac Output
Introduction: Cardiac Output is the volume of blood pumped out from each ventricle in one minute. Cardiac output is an essential parameter in hemodynamics, the study of blood flow. Its importance is globally accepted. In this article, you will get a definition of cardiac output, standard range, and more. Table of contents: What do you mean by cardiac output?What is the Normal Range of Cardiac…
0 notes
Text
What Is A Nomogram In The Medical World?
Physicians will often use nomograms to get accurate estimations of factors like blood pressure, cardiac output, oxygen saturation levels, and temperature. A nomogram is the graphical representation or diagram of data in two axes (usual y-axis on the left side and x-axis on the bottom) which shows trends of variation over time. The graphical representation of these relationships is done by plotted points with specific coordinates that represent value pairs at given instances in time. A nomogram often consists of three variables (independent variable, parameter or constant; dependent variable; conversion factor), which give functional relations between two variables that are parallel to each other.
#blood pressure#cardiac output#oxygen saturation levels#temperature#age#height#weight#number of pregnancies
0 notes
Text
Cardiac Output (Fick Formula) Calculator
The Fick Formula calculates cardiac output, cardiac index, and stroke volume. Cardiac Output - Fick Cardiology Critical Care Anesthesiology cardiology Cardiac Output Fick catheterization
0 notes
Text
Is real-time heart monitoring the future of saving lives in critical care?
Every second counts when it comes to heart health — especially in critical care units, surgeries, or emergencies. That’s where advanced cardiac output monitoring devices are making waves. These tools provide instant, accurate insights into how well the heart is pumping blood, helping doctors respond faster and with more precision than ever before. So what makes this tech essential, and why is the Cardiac Output Monitoring Device Market expanding so rapidly?
Let’s break down the innovation, growth, and life-saving potential behind these small but powerful machines.
Why is cardiac output such a vital metric in patient care?
Cardiac output is the amount of blood the heart pumps per minute — a direct indicator of how effectively the heart is functioning. It’s especially important during surgeries, in ICU settings, and when managing conditions like heart failure, sepsis, or trauma.
Traditional monitoring relied on invasive methods, often involving catheters and significant risk. But today’s cardiac output monitoring devices are becoming less invasive, more portable, and far more accurate. This means faster decision-making and better outcomes for critically ill patients.
What’s pushing the demand for smarter heart monitoring devices?
Several factors are driving growth in this space. Rising rates of cardiovascular disease, an aging global population, and more surgical procedures are increasing the need for real-time heart function monitoring. Hospitals are also under pressure to improve care quality while cutting costs — and these devices help clinicians act swiftly, reducing complications and ICU stays.
According to a detailed analysis of the Cardiac Output Monitoring Device Market, the industry is seeing massive investment in R&D, with new technologies focusing on minimally invasive and even non-invasive techniques, like pulse contour and bioimpedance monitoring.
How are innovations in this market improving patient outcomes?
Modern cardiac output monitors are combining hardware with intelligent software — think AI-driven algorithms and data integration with electronic health records. These systems don’t just provide raw numbers; they help clinicians interpret trends, predict deterioration, and personalize treatment plans.
For example, during high-risk surgeries, these devices help anesthesiologists adjust fluid and medication levels on the fly. In ICUs, they help manage complex conditions like septic shock, where blood flow must be constantly regulated to avoid organ failure.
Can this technology be scaled to meet global health challenges?
Yes — and that’s a big reason for its market growth. These devices are increasingly being adopted in developing regions where access to specialized cardiac care is limited. Portable and user-friendly devices allow even mid-tier hospitals to deliver better emergency care.
Meanwhile, broader trends in global health, such as the rise of wellness and preventative care, are setting the stage for expanded use. For instance, the South Korea Health Supplements Market reflects a growing population invested in heart health, diet, and preventive measures — all of which increase demand for continuous health monitoring and data-driven care.
Similarly, the surge in the China Health Supplements Market shows how health-conscious consumers and healthcare providers are leaning into solutions that bridge prevention and precision care — a trend that benefits cardiac monitoring adoption.
Are we heading toward at-home cardiac monitoring?
Absolutely. As remote healthcare and telemedicine rise, non-invasive cardiac output monitoring devices are being developed for home use. While hospital-grade monitors remain more complex, compact consumer devices that provide heart function trends are not far behind. This could revolutionize the way chronic cardiac conditions are managed — reducing hospital visits and catching warning signs before they escalate.
Final pulse check
The Cardiac Output Monitoring Device Market is proving that tiny devices can make a massive difference when it comes to saving lives. With smart tech, data integration, and non-invasive options leading the way, the heart of healthcare is beating stronger than ever. Whether in operating rooms or remote villages, real-time cardiac insight is quickly becoming a global standard in modern medicine.
0 notes
Text
Global Cardiac Output Monitoring Devices Market Size: Regional Outlook and Analysis 2024-2036
Research Nester published a report titled “Cardiac Output Monitoring Devices Market: Global Demand Analysis & Opportunity Outlook 2036” which delivers detailed overview of the global cardiac output monitoring devices market in terms of market segmentation by product, type, technology, end-user, and by region.

Further, for the in-depth analysis, the report encompasses the industry growth indicators, restraints, supply and demand risk, along with detailed discussion on current and future market trends that are associated with the growth of the market.
The global cardiac output monitoring devices market is anticipated to grow with a CAGR of ~4% over the forecast period, i.e., 2023 - 2033. The market is supply by type into invasive and non-invasive. Out of these, the invasive segment held the largest market share of 58% in the year 2022 backed by the increasing number of cardiac implant procedures and wide adoption of minimally invasive techniques that involve arterial and venous lines.
Request Free Sample Copy of this Report @ https://www.researchnester.com/sample-request-4217
The global cardiac output monitoring devices market is estimated to garner revenue of ~USD 1.80 Billion by the end of 2033, up from revenue of ~USD 1.19 Billion in the year 2022. The growing occurrences of traumatic injuries, followed by the surge in Chronic Obstructive Pulmonary Disease (COPD) which is a leading reason of disability and death, and escalating geriatric population are some of the major factors anticipated to drive the growth of the market in the coming years.
Regionally, the global cardiac output monitoring devices market is segmented into five major regions comprising of North America, Europe, Asia Pacific, Latin America, and Middle East & Africa. The market in the North America held the largest market share by ~40% in the year 2022 owing to the increasing prevalence of cardiovascular diseases, growing disposable income, favorable medical reimbursement policies and the escalating healthcare spending.
The research is global in nature and covers detailed analysis on the market in North America (U.S., Canada), Europe (U.K., Germany, France, Italy, Spain, Hungary, Belgium, Netherlands & Luxembourg, NORDIC [Finland, Sweden, Norway, Denmark], Poland, Turkey, Russia, Rest of Europe), Latin America (Brazil, Mexico, Argentina, Rest of Latin America), Asia-Pacific (China, India, Japan, South Korea, Indonesia, Singapore, Malaysia, Australia, New Zealand, Rest of Asia-Pacific), Middle East and Africa (Israel, GCC [Saudi Arabia, UAE, Bahrain, Kuwait, Qatar, Oman], North Africa, South Africa, Rest of Middle East and Africa). In addition, analysis comprising market size, Y-O-Y growth & opportunity analysis, market players’ competitive study, investment opportunities, demand for future outlook etc. has also been covered and displayed in the research report.
Escalating Prevalence of Cardiovascular Diseases (CVDs) to Drive the Market Growth
According to the statistics by the World Health Organization (WHO), every year, 17.9 million people worldwide lose their lives from CVDs, accounting for 32% of all deaths.
Request for customization @ https://www.researchnester.com/customized-reports-4217
CVDs encompasses a wide range of conditions. Some of these occur simultaneously or result to certain other conditions or diseases within the group. The heart and blood vessels are mainly affected by cardiovascular diseases (CVDs). Currently, a huge number of people have been dealing with some kind of CVD. In the United States, at least one form of heart disease affects nearly half of all adults. Therefore, the increasing number of CVDs patient is fueling the demand of cardiac output monitoring devices.
However, excessive prices of cardiac output monitoring devices, regulated insurance coverage choices, and the inclination for medicines over surgery are expected to operate as key restraint to the growth of global cardiac output monitoring devices market over the forecast period.
This report also provides the existing competitive scenario of some of the key players of the global cardiac output monitoring devices market which includes company profiling of Schwarzer Cardiotek GmbH, Edward Lifesciences Corporation, ICU Medical, Inc., Masimo Corporation, Baxter International, Inc., Medizintechnik GmbH, Getinge AB, BioTelemetry, Inc., and others. The profiling enfolds key information of the companies which encompasses business overview, products and services, key financials and recent news and developments. On the whole, the report depicts detailed overview of the global cardiac output monitoring devices market that will help industry consultants, equipment manufacturers, existing players searching for expansion opportunities, new players searching possibilities and other stakeholders to align their market centric strategies according to the ongoing and expected trends in the future.
Access our detailed report @
https://www.researchnester.com/reports/cardiac-output-monitoring-devices-market/4217
About Research Nester-
Research Nester is a leading service provider for strategic market research and consulting. We aim to provide unbiased, unparalleled market insights and industry analysis to help industries, conglomerates and executives to take wise decisions for their future marketing strategy, expansion and investment etc. We believe every business can expand to its new horizon, provided a right guidance at a right time is available through strategic minds. Our out of box thinking helps our clients to take wise decision in order to avoid future uncertainties.
Contact for more Info:
AJ Daniel
Email: [email protected]
U.S. Phone: +1 646 586 9123
U.K. Phone: +44 203 608 5919
0 notes
Note
Faaaaa my babyyyy, I'm here as promised. 🥺🥺 We already talked about this in dms and you seemed so interested so can you write the lads men reacting to mc's death, please pretty please
When You Are Gone [All LaDS Men - Angst Headcanons]
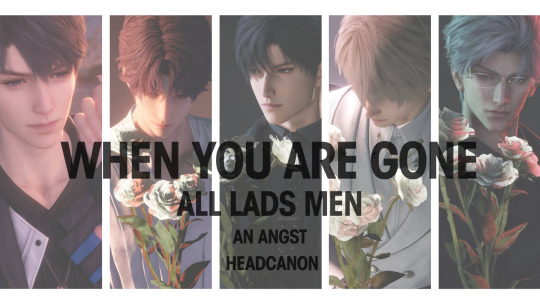
Rated: SFW - Angst Tags: hurt/no comfort, poorly dealing with the death of a loved one
Summary: The LaDS men dealing with the aftermath of your death, in the heartbreaking messages they leave in your voicemail almost regularly even long after you’re gone, in an effort to cope with your loss.
Author’s Notes : Hey darling, absolutely! Here you go. Hope you enjoy (?). 😭 This headcanon’s a bit differently formatted because I was inspired by the game’s speech to text function.

Sylus
TW: knowingly putting oneself in danger, mortally wounded Sylus, insomnia, mild spoilers for Razor’s Grip ASMR


Transcript:
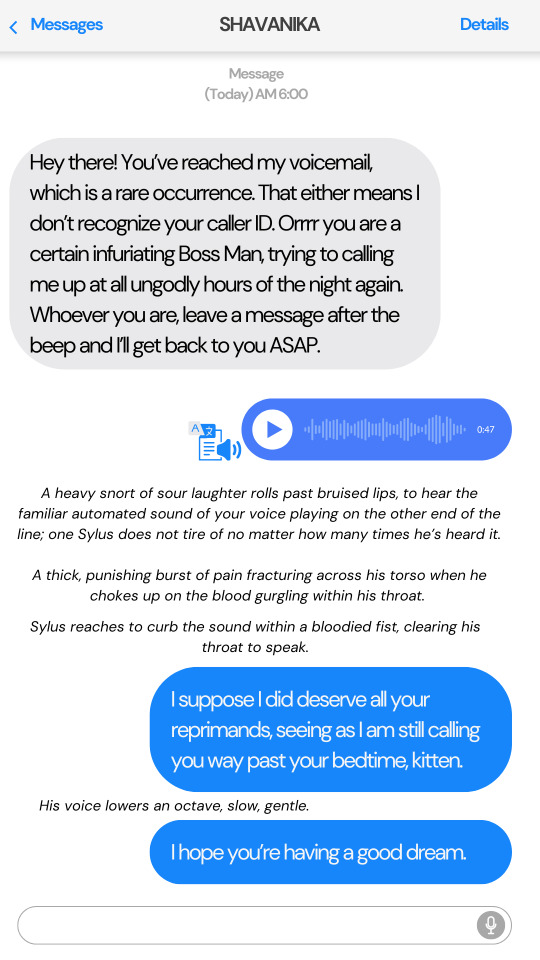
Hey there! You’ve reached my voicemail, which is a rare occurrence. That either means I do not know recognize your caller ID. Orrrr you are a certain infuriating Boss Man, trying to calling me up at all ungodly hours of the night again. Whoever you are, leave a message after the beep and I’ll get back to you ASAP.
A heavy snort of sour laughter rolls past bruised lips, to hear the familiar automated sound of your voice playing on the other end of the line; one Sylus does not tire of no matter how many times he’s heard it. A thick, punishing burst of pain fractures across his torso when he chokes up on the blood gurgling within his throat.
Sylus reaches to curb the sound within a bloodied fist, clearing his throat to speak once more.
I suppose I did deserve all your reprimands, seeing as I am still calling you way past your bedtime, kitten.
His voice lowers an octave, slow, gentle.
I hope you’re having a good dream.
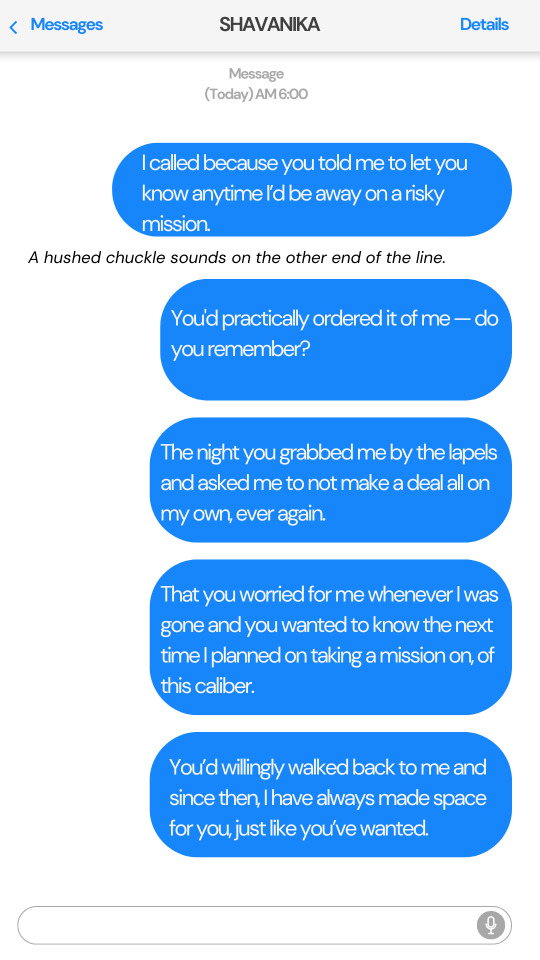
I’m only calling because you told me to let you know anytime I’d be away on a risky mission. A hushed chuckle sounds on the other end of the line.
You'd practically ordered it of me — do you remember?
The night when you grabbed me by the lapels and asked me to not make a deal all on my own, ever again. That you worried for me whenever I was gone and you wanted to know the next time I planned on taking a mission, of this caliber.
You’d willingly walked back to me and since then, I have always made space for you, just like you’ve wanted.
I’ve kept up my end of our bargain.
A guttural moan of pain sounds through the otherwise quiet of the night.
These wounds of mine... functioning without sleep for this long, and a poor decision made on my end, the combination was bound to have consequences.
His chuckles knell throaty, labored.
And now, all I wish to do is sleep.
A lengthy silence follows after, making one believe the user on the other end of the line might’ve cut the call. Or fallen asleep in exhaustion of his wounds, like he said.
Before that gentle burr of his sounds once more.
You know I can’t die, sweetie, unfortunate as that is in this moment.
But I do have a wish for when my body inevitably loses its awareness for the short time it takes to recuperate.
I hope, Sylus’s voice softens. that when I close my eyes this time, I get to see you in my dreams.

Zayne
TW: allusions to embalming a body long after death, mentions of a protocore heart that continues to function even after the host’s death, denial of grief
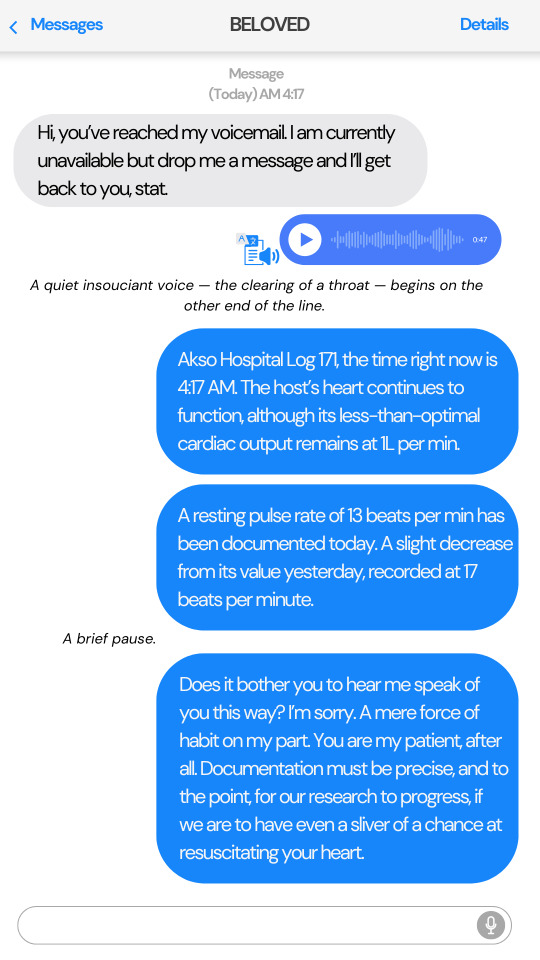
Transcript:
Hi, you’ve reached my voicemail. I am currently unavailable but drop me a message and I’ll get back to you, stat.
A quiet insouciant voice — the clearing of a throat — begins on the other end of the line.
Akso Hospital Log 171, the time right now is 4:17 AM. The host’s heart continues to function, although its less-than-optimal cardiac output remains at 1L per min. A pulse rate of 13 beats per min has been documented today. A slight decrease from its value yesterday, recorded at 17 beats per minute.
A brief pause.
Does it bother you to hear me speak of you this way? I’m sorry. A mere force of habit on my part. You are my patient, after all. Documentation must be precise, and to the point, for our research to progress, if we are to have even a sliver of a chance at resuscitating your heart.
I have hope we will succeed; I will do my utmost as a doctor so that we may save you.
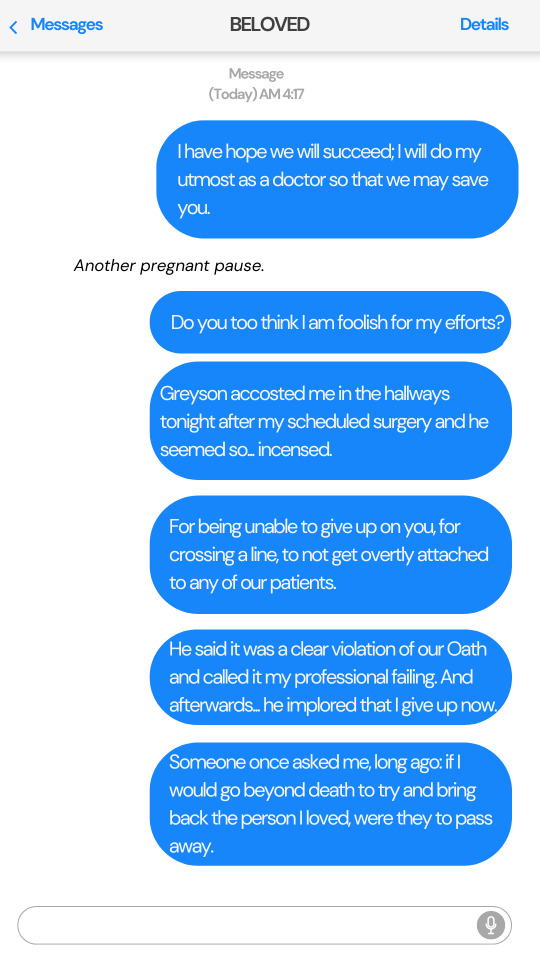
Another pregnant pause.
Do you too think I am foolish for my efforts?
Greyson accosted me in the hallways tonight after my scheduled surgery and he seemed so... incensed. For being unable to give up on you, for crossing a line, to not get overtly attached to any of our patients, he said it was a clear violation of our Oath and called it my professional failing. And afterwards... he implored that I give up now.
Someone once asked me, long ago: if I would go beyond death to try and bring back the person I loved, were they to pass away. And I answered that I would not, a desecration of the dead is not something I’d wish to do. Or wish upon the deceased. I would rather divert all my efforts to ensuring they would live, that their heart would continue to beat healthy.
So, in retrospect, it is Greyson who’s strange in expecting my willing defeat, without having even tried to the best of my capabilities. Not when your heart still continues to beat.
I do, however, miss you... very much, even though hope remains in my heart.
When the day comes that you wake up, I hope you do not have to suffer like this, ever again.

Rafayel
TW: gradual loss of vision, self-blame
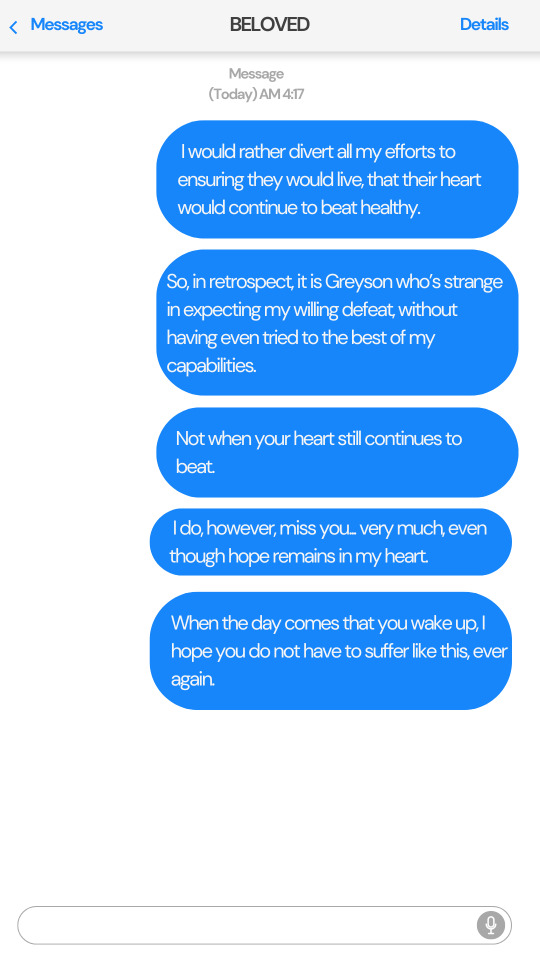
Transcript:
Hi, hello! I’m unable to answer your call at the moment but hey, feel free to drop me a voice message and I’ll get back to you soon. Bye-bye!
A sharp inhale; as if the person on the other end of the line is wracked by sudden, vicious pain.
Before the sound smoothens out, as if it had never been. An airy voice begins, although the nonchalant inflection to his tone sounds odd, all wrong — a fact the recipient of the voicemail would’ve been able to parse instantly, were they still around.
Hey cutie! It’s me again, your favorite person in the entire world.
Sorry about that earlier, I always get a bit startled whenever I hear you say good-bye in that crazy adorable voice.
Since y’know, the very last time we met, you never told me you were leaving.
Silence descends.
It really feels like it’s been another 800 years, I fear the fish will actually start flying and the whales will start walking this time.
Only, I don’t think you’re coming back this time, are you?
My bride can be so cruel sometimes.
A humorless laugh.
Anyyyyway, I’m dropping a voice note today because my eyesight’s been acting up a bit lately so I can’t really leave you a text like I usually do.
And before you scold me about it, I know I’m not supposed to be painting this long but I’m close to completing this new painting of you and I can’t rest until it’s done and dusted.
Don’t hate me for it, pretty?
A pleased, wistful sound.
I really wish you were here so I could show it to you right now.
A strident crash sounds in the background of the caller as paintbrushes overturn along with a color palette; garnet red and deep purple staining his floor a macabre color Rafayel cannot perceive in that moment.
Whoa, now that’s gonna leave a mess from the sounds of it.
Whatever, I’ll clean it up later once I get my sight back.
The point is, cutie, I’ll share a snap of the completed painting with you once it’s done.
Be prepared to be absolutely blown. So dazzled you fall head over heels in love with me.
And then perhaps... return, if you like it and me enough.
His sigh is steeped in mild vexation.
Waiting hurts.
Having you not remember our time together, in every lifetime we meet, hurts. It really is all your fault, you know.
A soft, disgruntled moue you can hear within his words.
But I hope, in our next life, we don’t cross paths.
That way, you won’t be forced to sacrifice yourself for my sake, ever again, you silly girl.
A throttled sound; it almost sounds like a wretched moan of pain.
I don’t want our bond to shackle you down anymore so I think... I’ll let you go now.
A human like you far suits the sun, not being saddled down below within turbulent seas.
So, this will be our final farewell now.
The words nearly scraped free of his throat on a rasped sound.
Goodbye, my beloved bride.
I loved—
Beep. Your message has been recorded and sent.

Caleb

Transcript:
TW: very brief traumatic remembrance of your demise
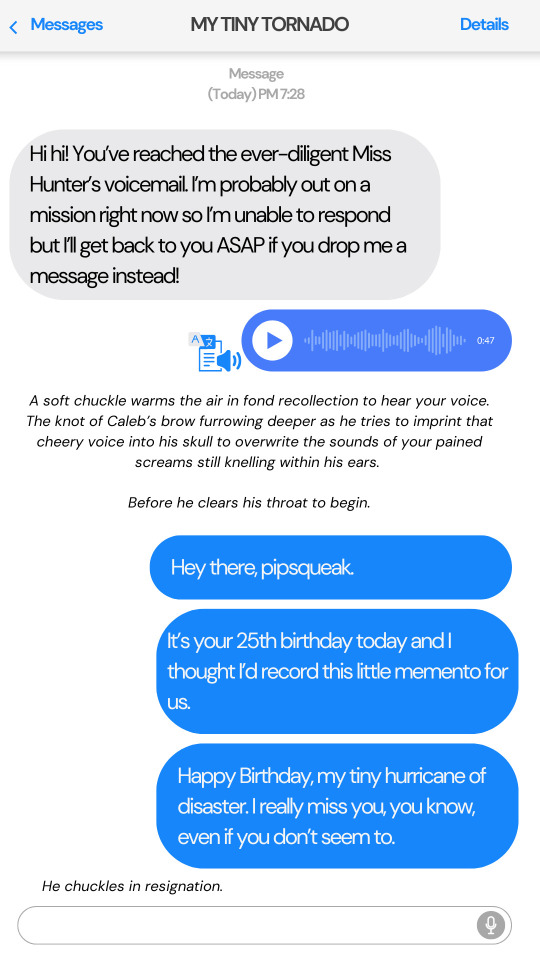
Hi hi! You’ve reached the ever-diligent Miss Hunter’s voicemail. I’m probably out on a mission right now so I’m unable to respond but I’ll get back to you ASAP if you drop me a message instead!
A soft chuckle warms the air in fond recollection to hear your voice. The knot of Caleb’s brow furrowing deeper as he tries to imprint that cheery voice into his skull to overwrite the sounds of your pained screams still knelling within his ears.
Before he clears his throat to begin.
Hello to you too, pipsqueak.
It’s your 25th birthday today and I thought I’d record this little memento for us.
Happy Birthday, my tiny hurricane of disaster. I really miss you, you know, even if you don’t seem to.
He chuckles in resignation.
I should’ve let you bother me more often if I knew you were going to be this terrible at keeping in touch with your best friend later.
We really didn’t have much time together once I returned from my posting abroad. Work kept you so busy.
I should’ve scolded you more often about taking appropriate breaks in between missions. God.
A gentle laugh resounds on the other end of the line.
Reprimanding you like a dad used to be Zayne’s job among us three, not mine.
The tiniest of fractures slip into his voice.
Anyway, I’ve kept to my side of the bargain we made while I was away from Linkon; to leave you regular voice messages about my day and I guess the habit’s just... stuck.
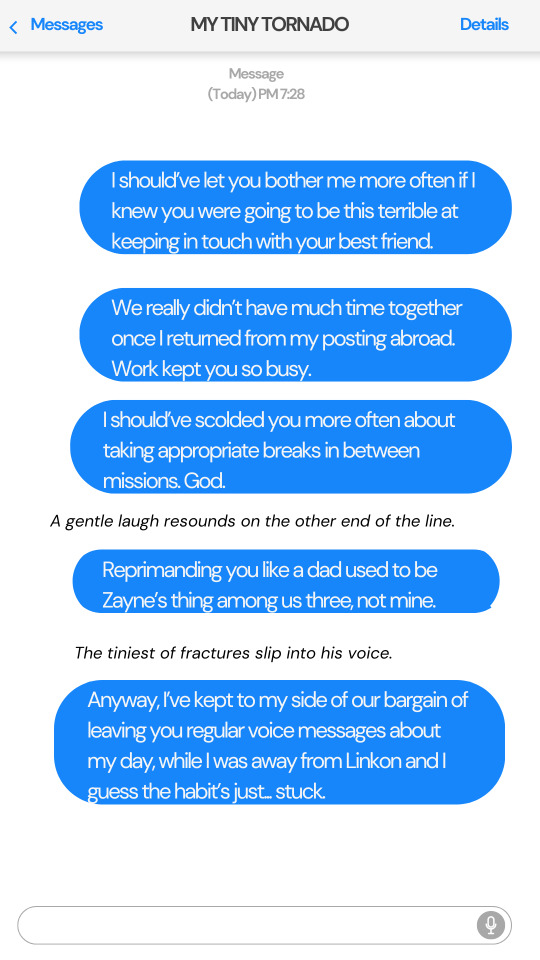
I visited the grocery store earlier to shop for ingredients to whip up your favourite parmesan risotto tonight.
It was almost like you were with me, you know.
With each item I passed by; from the strawberries you love to inhale to your favourite cola displayed, front and center, within their fridge. I almost picked one up for you before I—
He visibly halts himself, his breathing somewhat erratic. Before he resumes once more.
That nice kid you’re friendly with was manning the counter today and he recognized me almost instantly. All thanks to being towed around the Supermart with you, no doubt.
He even gave me a nice discount on the items when I told him I was whipping up a birthday dinner for you.
A short pause.
The risotto was pretty good, if I do say so myself. I wish you could’ve tasted it too.
Sorry I didn’t bake a birthday cake for you this year because it’s just me in the house now.
I don’t have a certain cute girl, with a crazy sweet tooth, to eat it with me and you know I’m not really fond of sweets.
His voice drops into a hushed sound, wrought with emotion.
Time flew by so fast. It seems like only yesterday when we were both kids, huddled around a coffee table with you trying your best to blow out the candles on the cake Grandma baked for us on your birthday.
He laughs softly.
You had a difficult time growing up because of your heart but you were always so brave.
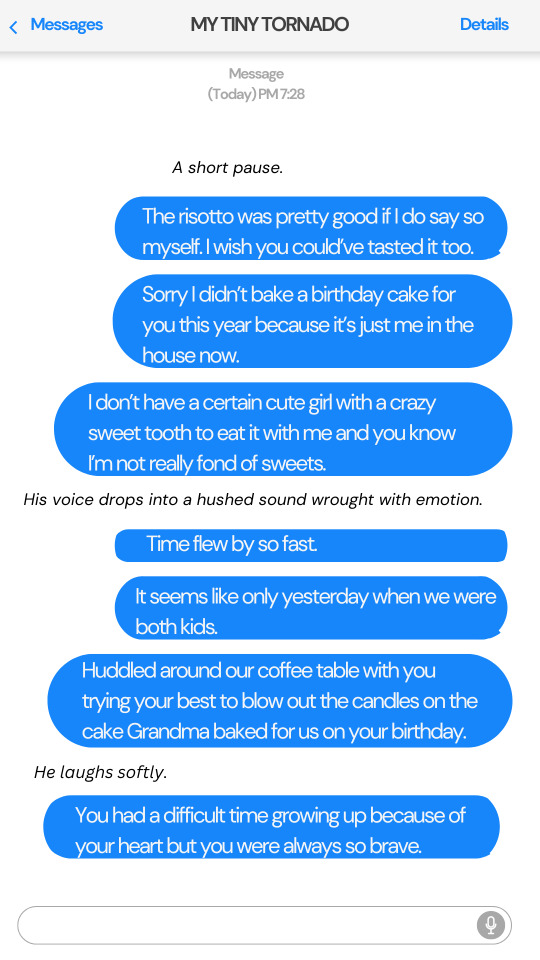
I wish I could’ve spoiled you more often. If only I knew then that our time together would be so short.
His voice breaks into a slight tremor.
Your Caleb really misses you... every day of my excruciating life.
But... I hope that now... wherever you are, you aren’t in pain anymore.
If there is a life after this one, I hope you let me find you in it, too.
I love you, little spitfire.
End of voice message.

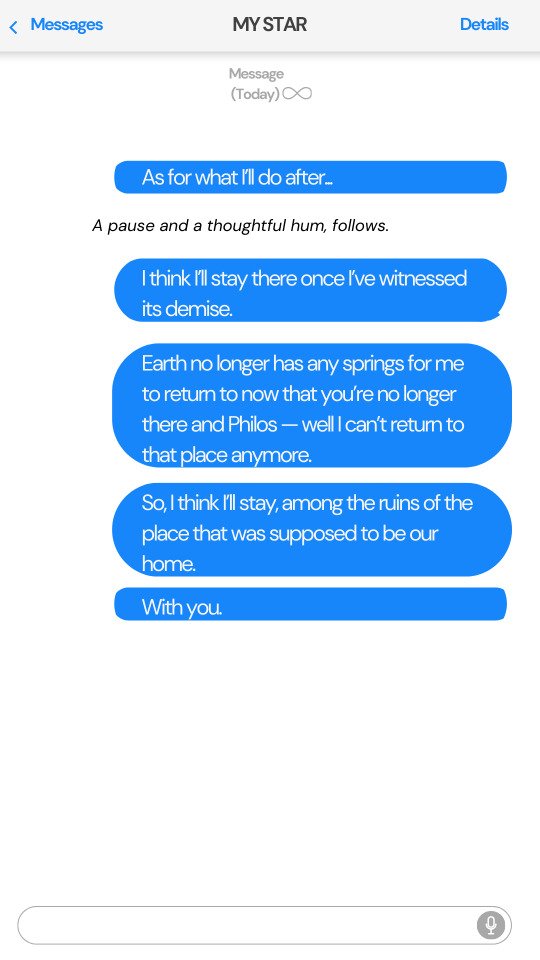
Xavier
TW: space travel, personal logging of a journey, self-imposed isolation and neglect
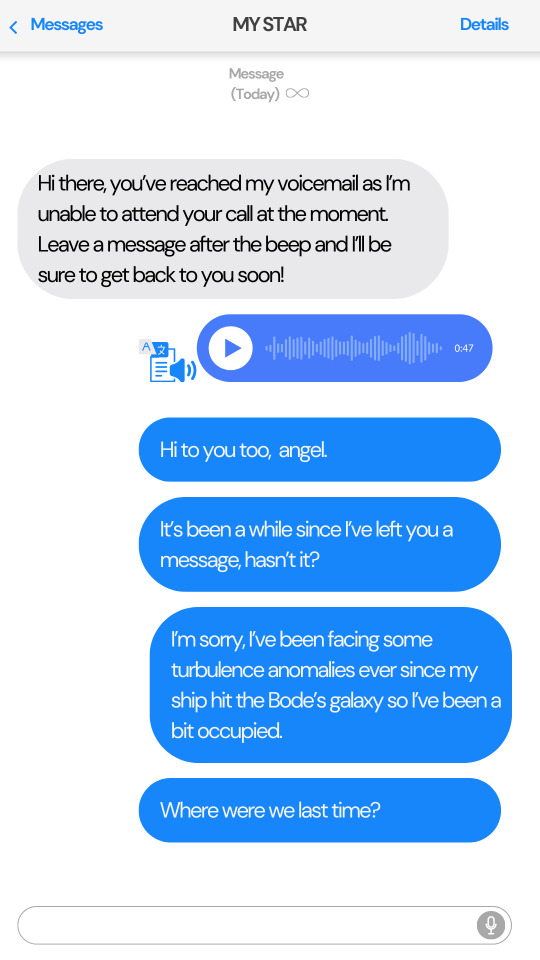
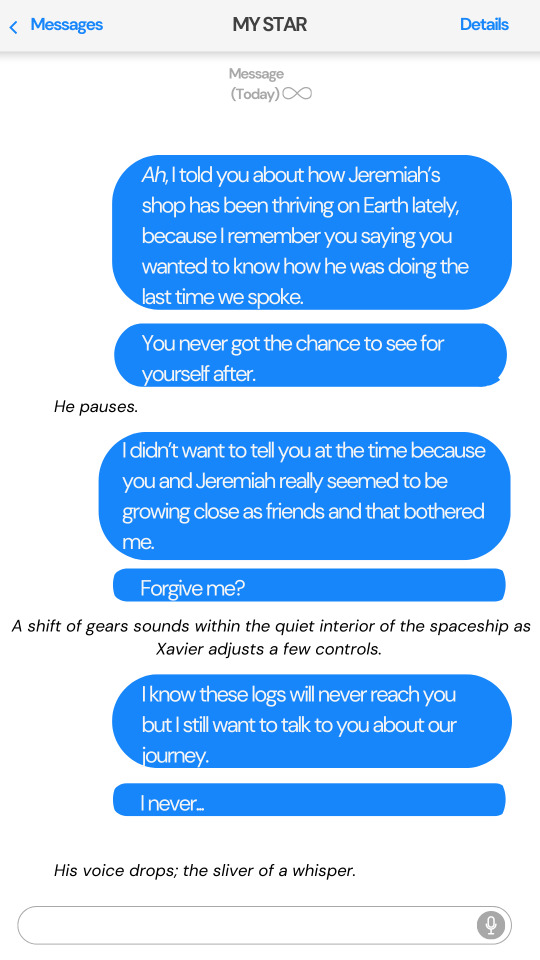
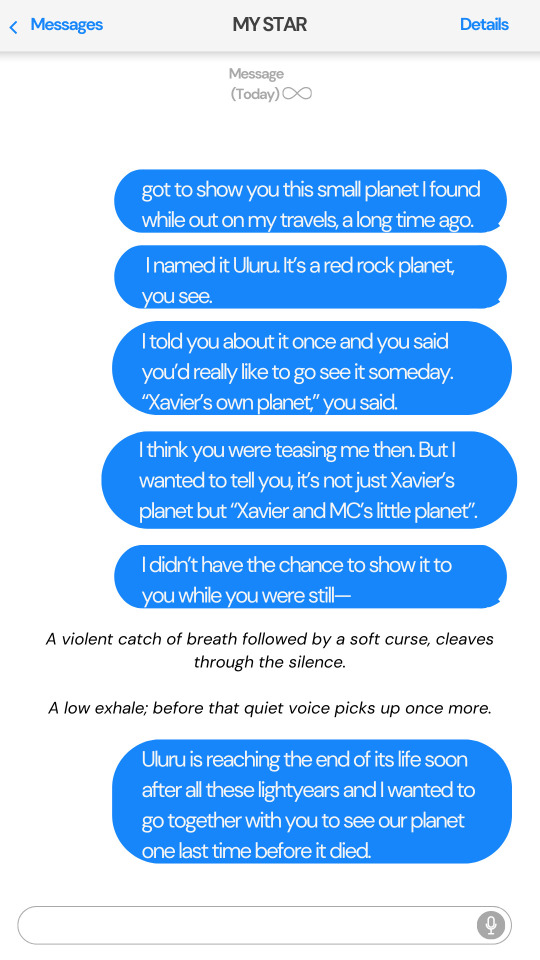
Transcript:
Hi there, you’ve reached my voicemail as I’m unable to attend your call at the moment. Leave a message after the beep and I’ll be sure to get back to you soon!
Hi to you too, angel.
It’s been a while since I’ve left you a message, hasn’t it?
I’m sorry, I’ve been facing some turbulence anomalies ever since my ship hit the Bode’s galaxy so I’ve been a bit occupied.
Where were we last time?
Ah, I told you how Jeremiah’s shop has been thriving on Earth lately, because I remembered you saying you wanted to know how he was doing the last time we spoke.
You never got the chance to see for yourself after.
He pauses.
I didn’t want to tell you at the time because you and Jeremiah really seemed to be growing close as friends and that bothered me.
Forgive me?
A shift of gears sounds within the quiet interior of the spaceship as Xavier adjusts a few controls.
I know these logs will never reach you but I still want to talk to you about our journey.
I never...
His voice drops; the sliver of a whisper.
got to show you this small planet I found while out on my travels, a long time ago. I named it Uluru. It’s a red rock planet, you see.
I told you about it once and you said you’d really like to go see it someday. “Xavier’s own planet,” you said.
I think you were teasing me then. But I wanted to tell you, it’s not just Xavier’s planet but “Xavier and MC’s little planet”.
I didn’t have the chance to show it to you while you were still—
A violent catch of breath followed by a soft curse, cleaves through the quiet.
A low exhale before that quiet voice picks up once more.
Uluru is reaching the end of its life soon after all these lightyears and I wanted to go together with you to see our planet one last time before it died.
As for what I’ll do after...
A pause and a thoughtful hum, follows.
I think I’ll stay there once I’ve witnessed its demise.
Earth no longer has any springs for me to return to now that you’re gone and Philos — well I can’t return to that place anymore.
So, I think I’ll stay, among the ruins of the place that was supposed to be our home.
With you.

End Notes: Thank you for reading! I know many of us wept about how we wished for God to take all of Zayne’s pain and give it to us instead so here I am, happy to do exactly that. 😇 Happy Zayne story branch release, y’all.
Likes, comments and reblogs are always appreciated if you are so inclined, lovelies!
Tagging as requested: @samanthagnicole , @catboi-anon , @bitches4lifebro , @beebumbo , @hellinistical
If you have not been tagged, it’s because I can’t tag you due to tagging permissions turned off on your end.
If you’d like to be tagged in my future stories, you can fill this short form here. If you’d like to be removed, shoot me a DM!
You can also find me on Ao3 and twitter, if you’d like to chat or just squeal with me about hot characters, in general.
#sylus x reader#rafayel x reader#zayne x reader#xavier x reader#caleb x reader#love and deepspace x reader#lads x reader#lads x you#lads x y/n#lads x mc#lads sylus#love and deepspace sylus#rafayel love and deepspace#xavier love and deepspace#caleb love and deepspace#sylus x you#rafayel x you#zayne x you#lnds x reader#lnds x you#l&ds x reader#l&ds x you
509 notes
·
View notes
Text
Also preserved in our archive
In patients with long COVID, lower pulmonary gas exchange may be associated with impaired cognitive function, according to a study being presented next week at the annual meeting of the Radiological Society of North America (RSNA).
According to the National Center for Health Statistics, approximately 17.6% of adults in the U.S. have experienced a post-COVID condition commonly referred to as long COVID. People with long COVID may exhibit a wide variety of symptoms, including difficulty concentrating ("brain fog"), change in sense of smell or taste, fatigue, joint or muscle pain, dyspnea (shortness of breath), digestive symptoms, and more. These symptoms may persist for weeks, months, or even years after COVID-19 infection.
Researchers from the University of Iowa in Iowa City set out to assess associations between pulmonary MRI gas exchange, structural and functional brain MRI, and cognition in long COVID patients. In pulmonary gas exchange, oxygen moves from the lungs to the bloodstream, while carbon dioxide moves from the bloodstream to the lungs.
"This is the first time that MRI has been used to jointly assess lung and brain function to investigate their relationship in long COVID," said the study's lead author Keegan Staab, B.S., graduate research assistant in the Department of Radiology at the University of Iowa in Iowa City. "This research is new in that it combines multiple unique imaging types to study a multiorgan relationship in a disease population."
Senior study author Sean B. Fain, Ph.D., professor and vice chair for research in the Department of Radiology at the University of Iowa, added, "If these findings can be generalized to the long COVID population, the study suggests that there may be a causative relationship between cognitive dysfunction and lung dysfunction, suggesting a potential treatment strategy using methods that target improved gas exchange."
For the study, 10 female and 2 male patients (median age: 59 years) who had persistent dyspnea and/or fatigue following the resolution of acute COVID-19 infection were recruited from a post-COVID-19 clinic. Hyperpolarized Xe pulmonary MRI, structural and functional brain MRI, pulmonary function tests and cognitive tests were acquired.
"129Xe MRI allows for advanced measurements of ventilation and gas exchange," Staab said. "The literature also indicates that 129Xe may be more sensitive to pulmonary injury compared to standard breathing tests, making it better suited to study long COVID in which patients typically have normal breathing tests."
Perceived cognitive difficulties were measured using Patient-Reported Outcomes Measurement Information System, and objective cognitive performance was assessed using the National Institutes of Health Toolbox V3 Cognition Battery.
"There was a range of cognitive difficulties among the patients in the study," Staab said. "Some were mild and indicated slight dysfunction, while others were more serious and indicated that some patients have slow thinking and trouble concentrating several times per day."
The results showed that lower pulmonary gas exchange may be associated with cognitive dysfunction, as well as lower gray matter and white matter volumes in patients with long COVID. In addition, the researchers observed significant relationships suggesting that increased cerebral blood flow is associated with decreased gas exchange in long COVID patients.
Staab said larger studies are needed to investigate the association between gas exchange and cerebral blood flow in long COVID.
"This relationship could be a compensatory mechanism where lower lung function is compensated by higher cardiac output and higher brain perfusion," he said. "It's also a possibility that the disease mechanism that impairs pulmonary gas exchange also leads to higher brain perfusion through downstream vascular injury in both lung and brain."
Based on the findings of this study, gas exchange abnormalities may help identify long COVID patients who require additional treatment or long-term management.
Other co-authors are Marrissa J. McIntosh, Ph.DDD., Jonathan L. Percy, B.S., Andrew D. Hahn, Ph.DDD., Natally AlArab, M.D., Conner J. Wharff, B.S. B.A. RT(R)(MR), Eric Bruening, M.S., Alejandro P. Comellas, M.D., Eric A. Hoffman, Ph.DDD., Carinda Linkenmeyer, M.A.E., Tara Lanning, B.S., and Karin F. Hoth, Ph.DDD.
Note: Copies of RSNA 2024 news releases and electronic images will be available online at RSNA.org/press24.
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
#mask up#wear a mask#public health#pandemic#covid#wear a respirator#covid 19#still coviding#coronavirus#sars cov 2#long covid#covid conscious#covid19#covid is airborne
102 notes
·
View notes
Text
"My uh...whiff...is very faint thank you. Nothing a little bergamont, rosemary, and a hint of fine aged brandy can't hide. It's the perfect olfactory disguise for a corpse. Honestly, I think I missed my calling as a perfumer!" - Astarion to Shadowheart I don't know if anybody has analysed Astarion's perfume or if the ingredients were even thought of this hard by Stephen Rooney (I am kicking myself for not asking when I met him at MCM 2 weeks ago). I, however, have read about them and thought about them quite hard.
So, my findings and ramblings about Astarion's perfume:
Bergamot - From the bergamot orange. Ironically, it's phototoxic - it makes skin more sensitive to sunlight/UV damage so I guess you could say it's associated with the sun? I dunno if Astarion should be wearing it tbh...
I also saw the fruit called 'Aphrodite's apple' and 'the most beautiful fruit' but the source was kind of flimsy.
Rosemary - Used in funeral rites throughout history, it symbolises death and remembrance but also fidelity in love.
The Ancient Egyptians used it in their embalming process to mask the scent of death (makes sense that Astarion uses it to mask his faint whiff of undeath), and it used to be (and still is?) placed on or in graves.
It's also mentioned a bunch in Shakespeare's works, specifically in scenes to do with death, which is quite appropriate and ironic for this silver-tongued, theatrical vampire who hates poets.
FRIAR LAWRENCE:
Dry up your tears, and stick your rosemary
On this fair corse
- Romeo and Juliet
OPHELIA:
There's rosemary, that's for remembrance. Pray you, love,
remember.
- Hamlet
Aphrodite pops up again here because in some versions of her creation myth, she arises from the sea adorned with rosemary.
Brandy - A biiit of a stretch maybe but there is a category of brandy known as eau-de-vie - water of life - so-called because medieval alchemists would ascribe miraculous properties to alcohol such as immortality.
In the late 19th and early 20th century, brandy was also used as a cardiac stimulant (so an association with life?) because it seemingly increased cardiac output and blood pressure. Which doesn't really help Astarion in any way but hey he is wearing it, not drinking it or getting it injected up his butt (that was one way it was used to resuscitate patients apparently yeah idk).
SO basically, his perfume ingredients are associated with life, death, the sun, immortality, devotion in love, and maybe the Greek goddess of passion, pleasure, beauty, and sex.
It also smells amazing.
#thank u for coming to my ted talk#astarion#bg3#bg3 astarion#baldur's gate#added in the quote bcos idk if everybody knows about the dialogue#sparrow's stuff
103 notes
·
View notes
Text
Heart Rates in MotoGP 🫀
There’s this post about the doctor in the movie Faster (2003) comparing Valentino Rossi's and Max Biaggi’s heart rates, and Vale’s maximum being only 125 bpm while Max’s was 170 bpm was a bit unbelievable to me so I’ve decided to do some research because those who know me know this is one of my favorite topics.
What I found when searching for this topic was a gold mine for people who are interested in hearts, so I thought I’d write a post about it because I think it could be interesting for everybody, especially for new fans (like me) who don’t already know about these heart-related things in MotoGP.
Important information: I don’t have a medical background, I’m just a cardiophile/someone who’s interested in hearts so this post isn’t about the medical side of this topic, it’s only to share the interesting stuff I found.
So, according to this article (which is basically the copy of this but I found the other one earlier), the riders’ highest heart rate is typically around 160-170 beats per minute. But what makes this really interesting is that I’ve discovered that there are a few riders that are an exception because of their extreme cardiac output like Maverick Viñales, whose highest heart rate barely exceeds 130 bpm, or like Jorge Martín, who’s the opposite extreme with his heart rate reaching 200 bpm during the highest points of qualifyings and races. Both of their resting heart rates are around 40 bpm, which is surprising because I expected Jorge's to be higher.
instagram
MotoGP began broadcasting the live heart rates of riders in 2019 with Maverick’s being shown first (as he writes it in the caption of the post above) and that was when his heart became a sensation because of it beating significantly slower than the hearts of other riders. The video above is him doing a hot lap at the 2019 Japanese GP weekend. That was when they discovered that his heart was different from the other riders’ hearts and in this video, they asked him about it because some people doubted if the monitor was accurate. (After seeing this, Vale's 125 bpm from the beginning of the post doesn't seem that unbelievable anymore.)

As you can see above, in 2020, during the Austrian GP weekend, they compared Maverick and Jack Miller’s heart rates, to which Jack’s reaction was, “I don’t know what Vinales is, a snake or something, or his heart is not working!” (jokingly) “I just saw they did a comparison and I am sitting at 160 and Vinales on 120-something. I’m sure mine wasn’t even at the highest point when I was doing those laps.”
And then Jack talked about his heart rate a bit more:
“I’ve never been in the 200s, I think the most I had in a test – and this was 3 years ago – was 199. If I’m training on the bicycle it’s 175-180. I think the best I have had on the bicycle has been 188. I think the start of the race, the lights, would be the highest point for me. And if you're in a fight especially in the first couple of laps it’ll be through the roof. Then you can sort of stabilize it around 160. I know with the motocross bike it stays around 172. That’s my normal average for a 25-minute training moto. Like I say, it’s not like I'm blowing out of my arse or anything like that, it’s just that Vinales is a bit of a ‘snake’! His just doesn’t work in the same way as mine… He’s got a bigger stroke, less rpm!”
And something worth mentioning here is that Maverick posted about his pre-season medical check-up and someone in the comments asked about his VO2 Max result and he answered the question in a video posted in his Instagram story (you can see it below), which was really surprising to me because I don’t usually see people openly sharing information like that.
(For reference, the average for people his age is 31-41.9, good is 42-49.9 and >50 is excellent. So his results of 64-70 are incredible.)
And some other things I found while doing some more research for this post:
Jorge talking about having an overheating problem and a heart rate of 230 bpm during the 2023 Indian GP.
Álex Rins racing with an average of 190 bpm (remember, the maximum is 160-170 bpm usually) during the 2024 Japanese GP (and finishing last despite trying really hard to get a good result).
And here is a video of Marc’s start in the 2012 Moto2 Valencia GP where his heart rate goes above 200 bpm. In this interview, he said he usually doesn’t monitor his heart rate during a race, but he did during this one. I think it was a good idea because it shows us how his heart behaves during the start, which is one of the most stressful moments of the race.
-
I really enjoyed writing this post and getting to know the incredible hearts these riders have. I hope I could show something new and interesting to those who didn't know about this. Thank you for reading it! ❤
#i started writing this almost a week ago but uni's killing me so i could only finish it at 3 am today#i didn't expect hearts to be this big of a thing here but i'm definitely not complaining 😏#motogp#maverick viñales#jorge martin#jack miller#alex rins#valentino rossi#max biaggi#heart things#i had to try really hard not to fangirl my way through this because holy shit guys this is incredible#also i'm a shipper at heart so i can't not mention this but from a cardiophile's point of view people being on two sides of extremes is so#fun because with two hearts this different there's so many possiblities when it comes to writing fanfics where hearts are in the focus#me and my friend mostly talk about maverick and jorge in connection with this but it could work with rosquez too 👀#(and with a lot of other pairings too)
56 notes
·
View notes
Text
Nerd time! I rediscovered this old article I read about an experiment that's just too fuckin hot. They tested elite athletes to determine their heart's maximal capacity: how fast it can beat, how much blood it can deliver, how much oxygen it can deliver. Then the next day they threaded wires into their beating hearts and sent their hearts into overdrive, forcing them to beat up to 26 bpm higher than they could naturally achieve.
Especially enticing to me as a guy who loves feeling his heart race but can't get it to go super fast. These athletes' hearts would not go much past 184bpm but then they got to exercise maximally with their hearts as fast as 209bpm. Literal dream of mine. Super jealous lol.
Fascinating result nerd-wise btw. Tl;dr is basically that at overdrive pacing their stroke volumes decreased in such a way that their overall cardiopulmonary performance (blood delivered i.e. cardiac output and oxygen delivered i.e. vo2max) were equivalent to their natural maximum heart rates. So, the body seems to naturally cap the heart's fastest rate around when it has "mini-maxed" its cardiac output (rate x stroke volume, so fastest it can deliver blood without dropping the stroke volume, at least too dramatically). I wonder if this is kind of naturally preventative, like if it went faster while dropping stroke volume would it lead to hemodynamic collapse? I'm kinda shocked this study cleared ethical boards and I guarantee you testing my lil idea never would lol.
I gotta find me one of these studies to participate in. I wonder if we could augment some other aspect of my heart to maintain/improve stroke volume while increasing the rate. Someone find me a cardiac researcher!
54 notes
·
View notes
Note
Hello! Currently im working on my story and I need to write my character Fainting/falling unconscious and I need help with writing that. General things I would like to know is how long would someone be out cold in which situations and what are some aftermaths. You can (and please do) add extra info. I dont see alot of posts covering this topic so I would request this :>
Hi! I have these previous posts: On Fainting ⚜ Some Reactions
Some Additional Notes
Faintness
‘Light- headedness’.
Seen in anaemia, low BP, postural hypotension, hypoglycaemia, carotid sinus hypersensitivity, epilepsy
Syncope
This is sudden loss of consciousness over seconds.
Another word for fainting or passing out.
Think of abnormal ‘electrical’ activity in the central nervous system or a temporary drop in cardiac output and BP that improves as soon as the patient is in a prone position.
Fits can occur due to a profound fall in BP so they are not specific of epilepsy.
Someone is considered to have syncope if they become unconscious and go limp, then soon recover.
For most people, syncope occurs once in a great while, if ever, and is not a sign of serious illness.
However in others, syncope can be the first and only warning sign prior to an episode of sudden cardiac death.
Syncope can also lead to serious injury.
Talk to your physician if syncope happens more often.
Pre-syncope - is the feeling that you are about to faint.
Someone with pre-syncope may be:
lightheaded (dizzy) or nauseated,
have a visual "gray out" or trouble hearing,
have palpitations, or
feel weak or suddenly sweaty.
When discussing syncope with your doctor, you should note episodes of pre-syncope as well.
Becoming unconscious due to a seizure, heart attack, head injury, stroke, intoxication, blow to the head, diabetic hypoglycemia or other emergency condition is not considered syncope.
WHAT TO DO
Someone who faints should be moved so they are lying down to allow blood to flow to the brain.
If they do not regain consciousness promptly, start CPR.
Reflex syncope - the result of a reflex response to some trigger, in which the heart slows or blood vessels dilate (widen).
This causes blood pressure to drop, so less blood flows to the brain and fainting (syncope) or near-fainting (pre-syncope) occurs.
Reflex syncope is the most frequent cause of fainting.
Vasovagal syncope — the common faint — occurs in one third of the population.
It is by far the most common form of reflex syncope.
Often triggered by a combination of dehydration and upright posture.
But it can also have an emotional trigger such as seeing blood ("fainting at the sight of blood").
Some Vasovagal Syncope Triggers
Seeing blood (not considered a serious symptom)
Getting an injection or having blood drawn (not considered serious)
Standing up quickly (a "head rush" is considered pre-syncope)
Standing upright for a long time
Sudden and unexpected trauma, stress or pain, such as being hit
Blood donation
Other types of reflex syncope include:
Situational syncope - a sudden reflex response to a trigger other than those listed above. Triggers include:
Coughing, sneezing, laughing, swallowing
Pressure on the chest after exertion or exercise
Defecating
Urinating (post-micturition syncope: occurs in men while standing to urinate)
Eating a meal
Sudden abdominal pain
Blowing a brass instrument or lifting weights
Carotid Sinus Syncope - a response in older adults that occurs when pressure is applied to the carotid artery in the neck. A hard twist of the neck, wearing a tight collar and pressing on the artery are triggers for carotid sinus syncope.
How is syncope treated? The treatment for syncope will depend upon the underlying condition but may include:
Catheter ablation: procedure to cauterize the specific heart cells that cause abnormal heart rhythms
Pacemakers: device inserted under the skin below the collarbone to deliver regular electrical pulses through thin, highly durable wires attached to the heart; used to treat bradycardia, heart block and some types of heart failure
Implantable cardioverter-defibrillators (ICDs): a small implanted device that delivers an electrical pulse to the heart to reset a dangerously irregular heartbeat; often used to treat ventricular tachycardia or heart failure
Avoiding known triggers
Vasovagal Attack
Simple faint precipated by emotion, pain, fear, prolonged standing, etc.
Suggested by: syncope within seconds or minutes of preceding precipitant.
Nausea,
sweating, and
darkening of vision.
Recovery within minutes.
No incontinence.
Confirmed by: history. No abnormal physical signs.
Finalized by: the predictable outcome of management, e.g. reassurance and advice regarding avoidance of preciptating causes.
Cough Syncope
Suggested by: sudden loss of consciousness after severe bout of coughing.
Confirmed by: history. Normal examination.
Finalized by: the predictable outcome of management, e.g. treating cause of cough.
Panic Disorder
Suggested by: Intense feeling of apprehension or impending disaster.
Developing quickly and unexpectedly without a recognizable trigger.
Shortness of breath and
sensation of smothering, nausea, abdominal pain, depersonalization and derealization,
choking,
numbness,
tingling,
palpitations,
flushes,
trembling,
shaking, chest discomfort,
fear of dying,
sweating,
dizziness,
faintness.
Confirmed by: recognized criteria, e.g. the ICD.
Finalized by: the predictable outcome of management, e.g. reassurance about nature of symptoms, cognitive behaviour therapy, anxiolytics (e.g. diazepam), or antidepressants (e.g. SSRIs).
Sources: 1 2 3 ⚜ More: Notes & References ⚜ On Hemophobia
Hope this helps with your writing!
#fainting#writing reference#writeblr#dark academia#spilled ink#writers on tumblr#literature#writing inspiration#writing notes#writing prompt#poets on tumblr#writing ideas#creative writing#fiction#medicine#pietro longhi#writing resources
78 notes
·
View notes
Text

The Cardiac Output–Cerebral Blood Flow Relationship Is Abnormal in Most Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients with a Normal Heart Rate and Blood Pressure Response During a Tilt Test
https://www.mdpi.com/2227-9032/12/24/2566
Screenshot from the AMMES May email newsletter
--- Somebody wrote this summary for laypeople when I shared it on Facebook: Summary - 91% of people with ME/CFS had insufficient heart output and hence insufficient blood flow to the brain despite normal heart rate and blood pressure during a tilt test. Ie even though they may not meet criteria for POTS 91% of ME/CFS sufferes have reduced blood flow to brain when body changes position.
24 notes
·
View notes
Text
⚕️Gallifreyan Healing Coma Management
Your Gallifreyan is sleeping and not dead.
This guide is for use on Gallifreyans and Time Lords only. Always seek your human advice from human health providers.
✨ What is a Healing Coma?
A healing coma is a physiological state unique to Gallifreyans wherein the body enters full stasis to direct all metabolic and regenerative resources toward healing. It's an evolved response to catastrophic injury, post-regenerative instability, or systemic failure. While it can appear life-threatening to outsiders, it's an entirely natural part of Gallifreyan biology.
🧠 When to Suspect a Healing Coma
A healing coma should be suspected only when multiple signs align, and never presumed lightly. These patients often appear dead to the untrained eye, with reduced or absent vital signs.
Key Indicators:
Recent severe injury, illness, or regeneration.
No visible glow (regenerative energy not active).
Extremely low vital signs, including: - Respiration <3/min - Combined hearts rate <10 bpm - Body temperature <5°C / 41°F - Systolic BP <20 mmHg
Unresponsiveness to all stimuli except occasional involuntary responses to high pain or telepathic signals.
Brain electrical activity is present but minimal.
TARDIS link unaffected (if applicable).
Refer to the Healing Coma Checklist in GASS. If 8 or more criteria are met, proceed with coma care.
📋 Initial Assessment
🔎 Clinical Differentiation
Before declaring a healing coma, rule out the following:
Respiratory bypass
Psionic shutdown
Induced stasis (voluntary)
Cardiac arrest (refer to CPR guide)
Anaphylaxis, toxic shock, or sepsis (see SER protocol)
If in doubt, initiate full GASS and ABCDE-P assessments.
🛑 Do Not Intervene If Healing Coma is Confirmed
Once a healing coma is confirmed:
🚫 Do not initiate CPR. 🚫 Do not forcefully rouse the patient. 🚫 Do not stimulate them verbally, telepathically, or physically.
Premature arousal can cause:
Cerebral damage
Systemic collapse
🛠️ Supportive Management
While the patient is in a healing coma, your job is to stabilise the environment, monitor, and prevent external harm.
1. 🌡️ Environment
Keep ambient temperature stable at 17°C (±0.5°C).
Reduce noise/light stimuli.
Do not allow contact with strong psionic fields.
2. 🛏️ Positioning
Flat or semi-recumbent.
Maintain cervical spine neutrality if trauma suspected.
Use a padded surface to avoid pressure injury.
3. 🧪 Ongoing Monitoring
GASS scores every 30 minutes for the first 6 hours, then hourly.
Monitor for: - Returning vital signs - Early signs of waking (twitches, murmuring) - Glitches in psionic output (may indicate instability or pain)
4. 🧬 Psionic Stability
If linked to a TARDIS, monitor the ship's response; it often reflects patient status.
Avoid telepathic interference unless absolutely necessary.
If psionic storm or uncontrolled feedback occurs, apply psychic dampening fields.
💊 Pain Management Considerations
While healing comas reduce pain perception significantly, residual pain may trigger premature arousal.
Do not use aspirin under any circumstances.
If pre-coma pain was extreme, ensure: - Environmental calm - Symbiotic contact (if possible) - Low-dose sedatives if awakening occurs in distress (Gallifreyan-only)
🚨 When to Escalate
Immediate intervention is required if:
Vitals drop below even healing coma thresholds (i.e., no BP or respiration at all)
Signs of regenerative instability appear (glow misfires)
The coma persists beyond 72 hours without improvement or explanation
New trauma or infection is introduced
📍Key Takeaways
✔️ Healing comas are normal (if dramatic) Gallifreyan responses to severe physiological strain.
✔️ Do not intervene once confirmed. Provide supportive care only.
✔️ Environmental control, GASS reassessments, and TARDIS monitoring are your best tools.
✔️ If you're ever in doubt—call a hospitaller. Or get the TARDIS. Or, ideally, both.
Medical Guides
These are all practical guides to assessing and treating a Gallifreyan in an emergency.
⚕️💕Gallifreyan CPR
⚕️👽Gallifreyan Assessment Scoring System (GASS)
⚕️👽ABCDE Assessment
⚕️⚠️Sepsis Emergency Response (SER)
⚕️⚠️Severe Trauma Protocol
⚕️🌡️Gallifreyan Thermoregulation and Emergency Response
⚕️🔮Psionic Emergency Pathways
⚕️✨Post-Regeneration Management
⚕️💤Gallifreyan Healing Coma Management
⚕️🩸Interpreting Gallifreyan Bloodwork
⚕️👶Gallifreyan Paediatric Emergencies
⚕️🧠Managing Gallifreyan Neurological Trauma
Any orange text is educated guesswork or theoretical. More content ... →📫Got a question? | 📚Complete list of Q+A and factoids →📢Announcements |🩻Biology |🗨️Language |🕰️Throwbacks |🤓Facts → Features:⭐Guest Posts | 🍜Chomp Chomp with Myishu →🫀Gallifreyan Anatomy and Physiology Guide (pending) →⚕️Gallifreyan Emergency Medicine Guides →📝Source list (WIP) →📜Masterpost If you're finding your happy place in this part of the internet, feel free to buy a coffee to help keep our exhausted human conscious. She works full-time in medicine and is so very tired 😴
#doctor who#dr who#dw eu#gallifreyans#gallifrey institute for learning#Time Lord biology#GAP Quick Guides#whoniverse#GIL: Biology#gallifreyan biology#GIL: Species/Gallifreyans#GIL#GIL: Biology/Medical
29 notes
·
View notes
Text


The crocodile icefish or white-blooded fish comprise a family (Channichthyidae) of notothenioidfish found in the Southern Ocean around Antarctica. They are the only known vertebrates to lack hemoglobin in their blood as adults.[2]
Although they do not manufacture hemoglobin, remnants of hemoglobin genes can be found in their genome. The hemoglobin protein is made of two subunits (alpha and beta). In 15 of the 16 icefish species, the beta subunit gene has been completely deleted and the alpha subunit gene has been partially deleted.[13] One icefish species, Neopagetopsis ionah, has a more complete, but still nonfunctional, hemoglobin gene.[14]
Red blood cells (RBCs) are usually absent, and if present, are rare and defunct.[15] Oxygen is dissolved in the plasma and transported throughout the body without the hemoglobin protein. The fish can live without hemoglobin via low metabolic rates and the high solubility of oxygen in water at the low temperatures of their environment (the solubility of a gas tends to increase as temperature decreases).[2] However, the oxygen-carrying capacity of icefish blood is less than 10% that of their relatives with hemoglobin.[16]
Myoglobin, the oxygen-binding protein used in muscles, is absent from all icefish skeletal muscles. In 10 species, myoglobin is found in the heart muscle, specifically ventricles.[17] Loss of myoglobin gene expression in icefish heart ventricles has occurred at least four separate times.[2][18]
To compensate for the absence of hemoglobin, icefish have larger blood vessels (including capillaries), greater blood volumes (four-fold those of other fish), larger hearts, and greater cardiac outputs (five-fold greater) compared to other fish.[2] Their hearts lack coronary arteries, and the ventricle muscles are very spongy, enabling them to absorb oxygen directly from the blood they pump.[19] Their hearts, large blood vessels and low-viscosity (RBC-free) blood are specialized to carry out very high flow rates at low pressures.[20] This helps to reduce the problems caused by the lack of hemoglobin.
The Southern Ocean is an atypical environment. To begin with, the Southern Ocean has been characterized by extremely cold but stable temperatures for the past 10-14 million years.[26] These cold temperatures, which allow for higher water oxygen content, combined with a high degree of vertical mixing in these waters, means oxygen availability in Antarctic waters is unusually high. The loss of hemoglobin and myoglobin would have negative consequences in warmer environments.[12] The stability in temperature is also "lucky", as strong fluctuations in temperature would create a more stressful environment that would likely weed out individuals with deleterious mutations. Although most research suggests that the loss of hemoglobin in icefish was a neutral or maladaptive trait that arose due to a random evolutionary event,[27] some researchers have also suggested that the loss of hemoglobin might be tied to a necessary adaptation for the icefish.[27] Most animals require iron for hemoglobin production, and iron is often limited in ocean environments.[28] Through hemoglobin loss, icefish may minimize their iron requirements. This minimization could have aided the icefish survival 8.5 million years ago when Arctic diversity plummeted dramatically.[27]
???
170 notes
·
View notes
Text
Mother's Month Recap, Part 3: How Do You Measure Up?





We hope you've been enjoying our look back on our Mother's Month campaign, during which our staff photographers and documentarians did their best to capture every moment for posterity. Today we continue with additional glimpses into Phase I of our Pre-Conception Readiness Protocol (PCRP), where we focus on anthropometry - i.e., the measurement of the body. Properly speaking, we should call this gynopometry for the purposes of the PCRP program.
Following the recording of the candidate's weight, meticulous measurements are made of her body - height, waist, buttocks, breasts, etc. This knowledge allows a fine-tuned assessment of critical health parameters to be formulated. For example, by incorporating weight we know body mass index (BMI), and with further fitness testing we will be able to measure cardiac output and effort. All of these, and more, are essential to knowing a PCRP candidate's potential for conception and maternity. In these photos, we also see a couple of candidates undergoing additional measurements for the more demanding Protomom program. And, as always, close blood pressure monitoring is vital. One of the Protomoms gives us a glimpse into the more demanding and intimate mammometry protocol - the assessment of the breasts. More on this in the future. Coming soon, we'll see our candidates have their labs performed and their vitals assessed. Thanks for your continued interest in Mother's Month!
===== All our info in one place: https://specialmedicalcentre.myflodesk.com/
#medicalerotica#medicalfetish#medfetish#medfet#blood pressure#cardiophilia#hospital#female patient#bouffant cap#specialmedicalcentre#thebestcareanywhere#tbca#female nurse#realrotica#SMCrealrotica#prepregnant#protomom#breast size#waist size
21 notes
·
View notes
Note
I don’t know if the prompts can be asking for more in stories you’ve already started, but I would love to see more of the Hero of Shadow and Wild Link interacting, or more on Abel’s heart attack in the HC AU, or more interactions with Zelda and Link after they had to get married (Golden Mercy? The Imprisoning War? Not sure what that one’s called). … Or basically anything involving hurt/comfort or Hyrule, honestly. 😂
I love your writing so much, thank you for sharing it with us! < 3
Hyrule snapped his fingers in front of his friend. “Wild!”
Wild blinked, flinching and taking a step back. “S-sorry—”
“You good? Was that another—I thought the meds—”
“No,” Wild shook his head. “I—it was—sorry, I just—he—”
Wild continued to stammer, at a loss for words. What was he supposed to say? He hadn't spaced out, he'd honed in, his mind had snapped with clarity, screaming at him and wanting nothing more than to run towards the stretcher.
That man—he was—
And he was having a—
"I-I just... need to sit down for a bit," Wild finally said, walking out of the ED.
Wild had yet to fully explain everything that had happened in his past. Everyone knew he had gaps in his memory, that he'd sustained a head injury, that it made him have absence seizures, but the cause of it... the people he'd left behind because of the aftermath...
How could Wild possibly ever explain? He'd failed in his mission, and it had gotten his entire team killed. He could never face anyone from his past, let alone his—
Castle Town had promised a new life, a new beginning, especially as memories had tried to piece themselves back together and make him want to run and hide all the more. If he told everyone... then there was no more running from it.
Wild buried his face in his hands, resting on an empty stretcher in the basement. His mind screamed with anxiety as his past caught up to the present, and his heart screamed with worry over his father.
This was a nightmare.
XXX
Fable looked over her room one more time. Ambu bag? Check. Suction? Check. Defibrillator? Check. She had her maintenance IV fluid set up, the plasmolyte liter set up, the wires for the cardiac monitoring system ready to go, chest tube suction at the ready, and her little trays had all the syringes, saline flushes, blunt tips, alcohol swabs, caps, lab tubes, and everything else she could think of prepared.
She'd chart stalked the patient while he was in the OR, and she'd already gotten report from the nurse. Forty-year-old male (oh he's young, Fable thought, used to seeing far older patients) presented to the ED via EMS with chest pain and shortness of breath, STEMI confirmed with EKG, and he was sent to the cath lab. There they found multiple severe occlusions and opted for an open heart bypass surgery rather than using stents, and off to the OR he'd gone.
The surgery had gone fairly straightforward from what she could see - he'd been on bypass for about an hour, and the surgery itself had been going on for about four. He'd gotten about 500 of cell saver, 2L crystalloid, and 1 RBC, and he'd only been defibrillated once.
Just as she looked over the chart again, roll call was sent out to the unit, and she gathered her thoughts as she went to the room, awaiting the patient. He arrived a minute or so later, and the room quickly filled with Fable, the charge nurse, the tech, another nurse, the anesthesiologist, the attending surgeon, the fellow surgeon, the respiratory therapist, the ICU attending, and the nurse practitioner.
Everyone slipped into different roles and tasks fairly easily and quickly. Anesthesia handed off to the RT, who attached the ET tube to his ventilator, the tech worked on putting chest tubes to suction and getting outputs, Fable assessed her patient and looked at what drips they were on (2 of epi, 4 of levo, 0.02 of vaso, 1.5 of Dex, 1.2 of insulin), charge took the admission note while the surgeons gave report and Fable listened vaguely, her other nurse was attaching the safe set to the arterial line to collect blood for labs and an ABG, and the ICU providers listened to the report.
Vasoplegia, not too much bleeding but enough to merit product, chest tube output was a little high but not alarming, and he was cold at 35.8. Fable asked her tech to get a bear hugger, and x-ray arrived to check ET placement as the surgeons finished report. Fable stripped the chest tubes alongside the surgical fellow before they all stepped out for x-ray. ABG resulted pH 7.33, pO2 107, CO2 38, bicarb 24, and lactate 3.1. Fable opened the extra plasmolyte fluid bolus up to try and help with the lactate, which was likely indicative that the patient was dry.
The surgery team left, and Fable remained to stabilize the patient. She and her charge nurse worked on detangling the lines while the tech covered him in a warm blanket. His blood pressure was within parameters, with a mean arterial pressure greater than 65, though his systolics were in the 120s, which was right at his upper limit, so she tried weaning the levo a little, going to 3 to see what would happen, before continuing to detangle lines, get a blood sugar for the glucommander that was determining the insulin levels to give him, and obtaining cardiac output indeces. His cardiac index was 2.8, and his systemic vascular resistance indexed for his body weight was around 2600. Good CI, a little higher on the SVRI end. Perhaps she should wean the epi too, assuming his MAP tolerated it.
After about an hour, Fable felt a little less overwhelmed, and she called her charge nurse, who had left the room a good while ago alongside the rest of the team. "Have we heard anything about family?"
"He has a wife and daughter," she replied. "But they're a fair distance from here, out in Hateno. I think last we heard they were making arrangements to get here, but it wouldn't be until tomorrow morning."
Fable glanced at the clock. It was almost shift change, so night shift would have to be the ones to wake the man up, get a neuro assessment, and then hopefully extubate him.
Nodding, she went back to work. She wasn't going to wean sedation until he was warm enough, so all she had to focus on right now was stabilizing him. His labs came back and his hemoglobin was a little low, and his two mediastinal and one pleural chest tubes collectively put out about 280mL of blood. It was still a fairly high amount, mostly evenly distributed (the meds were bleeding more, but neither exceeded 100mL for the hour), but not enough to think there was an active bleed that needed surgical intervention. Not yet, at least.
Overall, he looked pretty decent.
After another hour, one blood product later, Fable finally felt like she was starting to get everything settled. Her patient's temperature was normalizing, but she was twenty minutes from shift change, so she figured it was safer to let him sleep through report and then night shift could try to figure out weaning and bathing. His lactic on his repeat ABG was improving at 2.4, so they were likely addressing all the problems.
When a transporter walked by, IV pumps in hand, she noticed him pause in front of her room. She walked over to him. "Hey. Can I help you?"
The transporter, a young man with long blonde hair tied out of his face, jumped, a little startled. "Uh, hi. Yeah. Sorry. I just..."
"What room are you looking for?" she asked helpfully. "I don't need extra channels."
"Uh, these are for 4301."
"You passed it, it's back that way."
"Right," the man nodded, looking back in the room. "Right."
Fable waited a moment, and then asked, "Can I help you with anything else?"
"Is he doing okay?" the man immediately asked.
Fable smiled. "Yeah, he's looking pretty good, I think."
"Can..." the transporter swallowed, shifting anxiously. "Can I talk to him?"
"He's pretty sedated right now," Fable answered cautiously. "Why do you want to talk to him?"
The transporter sighed in defeat. "I... he's my dad. I... haven't seen him in a long time."
His dad? Her charge nurse had said he had a daughter, not a son. Though... looking between her patient and the transporter in front of her, the family resemblance was striking.
Well, she hadn't heard of any visitor restrictions for him. "Yeah. You're not on his chart, though - can I get your name?"
The transporter sighed, putting the supplies he'd been carrying on the counter of the nurse's station. "I wouldn't be on it. My family thinks I'm dead. It's complicated."
He—uh... what?
"My name's Link," he answered her nonetheless before entering her patient's room.
Link? Huh. That was...
Wait a second.
"Hey, are you one of my brother's friends?" Fable asked as she followed him into the room.
"Your brother?"
"Link. Likes to call himself Legend to differentiate," she replied with an amused roll of her eyes.
Link gawked at her. "You're Legend's sister? He never even said he had a sister!"
"You two are alike," Fable huffed. "He doesn't particularly want a bunch of people to know he's related to me. But never mind that. Go talk to your dad."
Link stood there a moment, processing the words, before he exhaled shakily and nodded. Fable moved to the computer, working on catching up on charting to give him some privacy but also keep an eye on things. This patient's safety was her responsibility, after all.
Link seemed almost timid to approach the patient, even though he knew he was sedated. He slowly slid his hand into the older man's, shakily and quietly saying, "Hey, Papa. I... I, uh... I-I..."
Fable glanced out of the corner of her eye, seeing the young man getting tearful, and she tried to focus on her work once more.
"I missed you," Link whispered. "I'm s-sorry... about... about everything."
She heard a sniffle, and then the transporter moved quickly out of the room, offering her a brief but quick thanks before disappearing.
Fable turned towards the doorway, and then looked at her patient uncertainly. That was... odd.
Sighing, she walked up to the man, brushing hair out of his face. "Buddy, your family drama sounds almost as crazy as mine."
#you ask skye answers#lovely webhead#don't worry Abel's doing fine lol#Wild on the other hand...#writing#lu in healthcare#lu wild#abel#lu fable
99 notes
·
View notes