#colicky abdominal pain
Text
hour 17 of the same colicky abdominal pain

6 notes
·
View notes
Text
Clinical features – Ulcerative colitis is characterized by recurring episodes of inflammation limited to the mucosal layer of the colon. It commonly involves the rectum and may extend in a proximal and continuous fashion to involve other parts of the colon.
Patients with ulcerative colitis usually present with diarrhea, which is frequently associated with blood. Associated symptoms include colicky abdominal pain, urgency, and tenesmus. Patients with mainly distal disease may have constipation accompanied by frequent discharge of blood and mucus.
Patients may also have fever, fatigue, and weight loss. Ulcerative colitis primarily involves the intestine but may be associated with several extraintestinal manifestations.
●When to suspect ulcerative colitis – Ulcerative colitis should be suspected in patients with chronic diarrhea for more than four weeks. The clinical presentation, including laboratory features, endoscopic appearance, and radiology findings, is not specific for ulcerative colitis, and may be seen in a number of other causes of colitis including Crohn disease, radiation colitis, ischemic colitis, infectious colitis, and colitis related to medications.
●Establishing the diagnosis – The diagnosis of ulcerative colitis is based on the presence of diarrhea for more than four weeks and evidence of chronic colitis on endoscopy and biopsy. Since these features are not specific for ulcerative colitis, establishing the diagnosis also requires the exclusion of other causes of colitis by history, laboratory studies, and by biopsies of the colon.
●Disease course – Patients with ulcerative colitis usually present with attacks of bloody diarrhea that lasts for weeks to months. The course of ulcerative colitis typically consists of intermittent exacerbations alternating with periods of complete symptomatic remission. However, a small percentage of patients have continuing symptoms and are unable to achieve remission. Overall, patients who present initially with proctitis have a more benign disease course and frequently respond to topical therapy, whereas those who present with more extensive disease require systemic therapy and have a higher risk of colectomy.
Extension of colonic disease is seen in up to 20 percent of patients within five years. Approximately 67 percent of patients have at least one relapse within 10 years following the diagnosis. The risk of relapse depends on the age at initial diagnosis. The likelihood and timing of colectomy depends on the extent of the disease and severity at presentation. Mucosal healing in response to treatment is an important predictor of long-term clinical outcomes.
●Complications – Complications associated with ulcerative colitis include severe bleeding, toxic megacolon, perforation, strictures, and the development of dysplasia and colorectal cancer. Patients with ulcerative colitis may have a slightly higher mortality as compared with the general population.
Defining disease severity and risk – Patients with mild to moderate ulcerative colitis (UC) are identified as low risk based on prognostic factors that suggest a nonaggressive form of disease: absence of deep mucosal ulcerations, no extraintestinal manifestations, and diagnosis at age >40 years. These patients usually have mild to moderate symptoms (≤6 stools daily with or without blood) and lack signs of systemic inflammation (ie, normal or minimal elevation in C-reactive protein and/or fecal calprotectin levels).
●Pretreatment evaluation – For patients with UC who present with symptoms of a disease flare (eg, diarrhea, rectal bleeding), some aspects of the initial evaluation (eg, laboratory and stool studies, lower endoscopy) are repeated to exclude other conditions as a cause for symptoms and to assess the extent and severity of disease.
●Goals of therapy – The treatment goal for patients with active UC is to achieve clinical and endoscopic remission by demonstrating complete mucosal healing. Response to therapy can be determined by assessing symptoms and laboratory testing and can be supplemented by endoscopy with biopsies as needed.
●Induction therapy for ulcerative proctitis or proctosigmoiditis – For low-risk patients with ulcerative proctitis or proctosigmoiditis, we suggest topical (rectal) mesalamine rather than oral mesalamine or observation (table 1) (Grade 2B). However, for patients who prefer to avoid the burden of daily topical treatment, it is also reasonable to use oral mesalamine or to observe and initiate treatments if disease progresses.
For patients with mild to moderate disease confined to the rectum, we typically initiate treatment with mesalamine suppository once daily (algorithm 1). For patients with mild to moderate disease extending above 18 cm from anal verge into the sigmoid colon, we treat with mesalamine enema once or twice daily.
For low-risk patients with ulcerative proctitis or proctosigmoiditis who do not have symptom improvement after four weeks of topical mesalamine therapy, subsequent options include adding a topical glucocorticoid (eg, suppository, enema), adding an oral 5-aminosalicylic acid (5-ASA) agent, and/or starting an oral glucocorticoid (eg, budesonide multimatrix). Selection of second-line therapy depends on patient preferences, product availability, clinician preferences, and prior response to therapy.
●Induction therapy for left-sided or extensive UC – For low-risk patients with left-sided or extensive mild to moderate UC, we suggest a combination of an oral 5-ASA agent plus rectal mesalamine for induction therapy rather than oral 5-ASA monotherapy (Grade 2B). We begin high-dose oral mesalamine (ie, >3 grams daily) and mesalamine enemas once daily.
●Maintenance therapy – We suggest long-term maintenance therapy for the following low-risk patients who have achieved clinical remission with medical therapy (Grade 2B):
•Patients with ulcerative proctitis and >1 disease flare per year
•Patients with ulcerative proctosigmoiditis
•Patients with UC proximal to the sigmoid colon (i.e., left-sided colitis and extensive colitis)
The choice of maintenance therapy depends on the specific agent used to induce remission, the distribution of disease, patient preferences, clinician preferences, and insurance coverage/cost. For low-risk patients with mild to moderate UC in remission, the goal of management is to prevent clinical and endoscopic relapse.
●Health maintenance – Routine health maintenance, including screening for and prevention of other diseases as well as monitoring for adverse effects of therapy, is an important aspect of the care of patients with inflammatory bowel disease.
2 notes
·
View notes
Text
Herbal pain oil
TsMadaan Pain Oil useful in the prevention of joint pains, back ache, arthritis, cervical pain, neck & shoulder pain, myositis, fibrositis, sciatica, muscular sprain and strain.
Herbal pain oil
TsMadaan Herbal Pain Oil - 100 ML
Anti-Inflammatory & Muscle Relaxant Massage Oil
The Natural Pain Reliever.
Benefits:
Cures Joints Pain
Relieves Low Back Pain
Cures Swollen Joints
Cures Inflamed Joints
Relieves Sprain.
Relieves Painful Muscles.
Relieves Neck Strain.
Cures Old Age Arthritis.
Cures Rheumatoid Arthritis.
Composition: Hadjod, Datura, Nirgundi, Kaner, Kakjanga Taila, Ashwagandha, Aak, Sounth, Ajwain, Sendha Namak, Vacha, Bachnaag, Kuchla, Ratanjot, Kapur, Boswellia Oil ext., Castor, Turpentine oil, Gandhapura Oil, Sesame Oil, Linseed Oil.
Direction for use: Massage gently on the affected areas. For better results, keep the area covered with a soft, dry cloth for oil to get absorbed. In case of excessive pain, apply twice a day or as directed by physician.
An Ayurvedic Proprietary Medicine. Shake well before use.
For external use only.
Benefits of each ingredient of TsMadaan Herbal Pain Oil:
Hadjod
Hadjod can help mend fractures by reducing swelling, relieving pain, and treating allied disorders connected with fractures. Hadjod's anti-inflammatory activities are due to the presence of Beta-sitosterol and luteolin flavonoids.
The phytosterols -sitosterol and -sitosterol glycoside, terpenoids, and phenolic compounds contained in hadjod, such as resveratrol, quercetin, quercitrin, and kaempferol, are thought to be analgesic.
Datura
Datura seeds are analgesic, anthelmintic, and anti-inflammatory, and are used to treat stomach and intestinal pain caused by worm infestation, toothaches, and fever caused by inflammation. Its fruit juice is applied to the scalp to cure dandruff and hair loss.
Nirgundi
Nirgundi root and bark preparations contain the alkaloid nishindine, which has anti-inflammatory and analgesic (pain-relieving) properties. This aids arthritis sufferers in reducing joint pain and muscle spasms.
Kaner
The Kaner plant is one of those plants that has both therapeutic and religious significance. We offer crimson blooms from the Kaner tree to the gods. Kaner's flowers come in a variety of colors, including red, yellow, white, and pink. It's a little tree that's about the same size as the plant. It has very long and thin leaves.
Ashwagandha
Ashwagandha may function as a pain reliever by inhibiting the transmission of pain signals through the central nervous system. It's also possible that it has anti-inflammatory qualities. As a result, some studies has found it to be useful in treating rheumatoid arthritis and other types of arthritis.
Root, Aak
Aak Root helps wounds heal faster and soothes stomach pains, headaches, and sprains.
Sonth
Sonth or Shunthi is also known as vishvabhejhaj (universal medicine) because of its numerous applications. As it balances the vata dosha in the body, it is a natural pain reliever used in Ayurveda to reduce all forms of pain, including abdominal colicky pain, joint pain, headaches, and menstrual pain.
Ajwain
Ajwain, sometimes known as carom or Bishop weeds, is a type of ajwain. It contains essential oil, which is made up of a variety of bioactive chemicals and hence has medical value. Ajwain is available all year round. Ajwain is known for its medicinal and therapeutic properties.
Namak Sendha
A more pure form of sodium chloride is rock salt. It also has a significant amount of potassium. These minerals aid in the correction of electrolyte imbalances in the body, providing relief from muscle cramps. You can also relieve discomfort in the affected area by mixing rock salt with warm water.
Vacha
Vacha is a traditional plant that has a number of health benefits. Because this herb enhances intelligence and expression, it is known as "Vacha" in Sanskrit. Vacha is a revitalizing herb in Ayurveda because of its influence on the neurological system. It has a bitter taste and is available in dried form.
Because of its anti-inflammatory properties, Vacha essential oil may be effective in relieving pain and inflammation when used externally.
Kuchla
Kuchla oil aids in the management of some painful illnesses (such as rheumatism or other joint discomfort) that are caused by a Vata dosha imbalance. Due to its Vata balancing properties, topical application of Kuchla oil on the afflicted area helps to provide pain and inflammation alleviation.
Ratanjot
The origins of Ratanjot's roots are packed with anti-inflammatory, antibacterial, antiviral, anti-aging, and anti-oxidant qualities. This is mostly due to the presence of "beneficial compounds" such as flavonoids, naphthoquinone, alkannin, and shikonin.
Camphor
When applied topically to the skin, camphor activates nerve endings, reducing symptoms such as pain and itching. Camphor is also employed in the treatment of acute pain. When applied to the skin, it de-sensitizes nerve endings and produces a warm sensation. It also aids in the relief of muscular and joint pain.
ext. Boswellia Oil
The plant is employed in Ayurveda, one of the world's oldest traditional medical systems. Boswellic acids are abundant in Boswellia. These acids are thought to have anti-inflammatory properties.
Castor oil
Castor oil has natural anti-inflammatory properties, making it an excellent massage oil for sore muscles and joints.
Turpentine oil
Turpentine oil is used to treat joint pain, muscular discomfort, nerve pain, and toothaches by applying it to the skin. People sometimes inhale the fumes of turpentine oil to relieve chest congestion associated with certain lung conditions.
Sesame seed oil
Sesame oil provides a warming effect, which aids in the relief of muscle pain. It's also great for keeping your feet warm in the winter.
Flaxseed oil
Flaxseed oil, according to study, may aid patients who suffer from pain by reducing inflammation. It's thought that because of the omega-3 fatty acid content, it could be just as helpful as olive oil in this area.
2 notes
·
View notes
Text
The Advantages Of Anti-Colic Feeding Bottles

Welcoming a new baby into the world is an experience filled with love, excitement, and, of course, a bit of anxiety, especially when it comes to feeding. One challenge you might face is dealing with colic—a term that any parent dreads. List of best Baby feeding bottle sippers in India The cries of a colicky baby can tug at your heartstrings, leaving you feeling helpless and searching for solutions. This is where anti-colic feeding bottles become a potential game-changer for you and your little one. Let's explore how these innovative bottles can make feeding time a more serene experience for everyone involved.
Understanding Colic in Infants
In infants, colic is characterised by excessive crying and discomfort, often due to gastrointestinal discomfort. While the exact cause of colic remains a mystery, it's believed that swallowed air during feeding, leading to gas and abdominal pain, plays a significant role. Colic can be stressful for both babies and parents, prompting the search for effective solutions to soothe these tiny tummies.
The Design of Anti-Colic Feeding Bottles
Anti-colic feeding bottles are ingeniously designed to reduce the amount of air a baby ingests during bottle-feeding. They typically feature special vents, valves, or straw-like systems that allow air to bypass the milk or formula, preventing it from being swallowed by the baby. This innovative design mimics more closely the natural process of breastfeeding, where the baby controls the flow and intake of milk, reducing the chances of air ingestion.
Key Benefits of Using Anti-Colic Bottles
1. Reduces Colic Symptoms
Colic can be a distressing condition for babies and parents alike, characterized by prolonged periods of crying and apparent abdominal discomfort. Anti-colic bottles are specifically designed to minimize the amount of air a baby swallows while feeding, which is a common cause of colic. These bottles often feature unique vents, valves, or tube systems that allow air to escape from the bottle before it can be ingested by the baby, leading to a happier, more comfortable feeding experience.
2. Promotes Proper Digestion
By reducing the amount of air swallowed during feeding, anti-colic bottles help promote more efficient digestion. This is crucial in the early stages of a baby's life when its digestive system is still developing. Efficient digestion means less spitting up, gas, and discomfort for your little one, contributing to a smoother, more pleasant feeding routine. baby feeding bottle glass suppliers in Delhi
3. Encourages Natural Latching
Many anti-colic bottles are designed with nipples that mimic the shape and feel of the breast, encouraging a natural latch. This feature particularly benefits breastfeeding moms who alternate between breast and bottle feeding. A natural latch helps in making the transition between the two smoothers, reducing nipple confusion and making it easier for the baby to feed comfortably regardless of the method.
4. Supports Healthy Feeding Habits
Anti-colic bottles can also promote healthy feeding habits by allowing babies to control the flow of milk based on their sucking strength. This closely replicates the natural flow of breast milk, which can prevent overfeeding and reduce the likelihood of feeding-related issues. When babies feed at their own pace, they learn to listen to their bodies' hunger and fullness cues, fostering a healthy relationship with feeding from an early age.
5. Facilitates Easy Cleaning
To be effective, anti-colic baby feeding bottles come with a somewhat more complex design than standard bottles, featuring parts like vents or tubes. However, manufacturers are keenly aware of the need for easy cleaning and often design these bottles to be easily disassembled and cleaned, ensuring that hygiene is not compromised. Many anti-colic bottles are also made to be dishwasher safe, adding an extra layer of convenience for busy parents.
Things to consider while Choosing Anti-Colic Bottles
When choosing an anti-colic bottle for your baby, several factors merit careful consideration to ensure you're selecting the best option for your infant's needs. First and foremost, material safety is paramount; look for bottles made from BPA-free plastic, glass, or silicone to ensure that your baby is not exposed to harmful chemicals during feeding. Ease of cleaning is another crucial aspect, as anti-colic bottles often come with extra parts—choose a design that can be easily disassembled and cleaned to maintain hygiene and prevent the buildup of milk residues.
The nipple design plays a significant role in how well your baby will adapt to the bottle; look for nipples that mimic the natural shape of the breast to facilitate a smooth transition between breast and bottle feeding and reduce nipple confusion. Additionally, consider the ventilation system of the bottle, which is the core feature that helps prevent air ingestion; opt for a system that effectively channels air away from the milk to minimize gas and colic symptoms. Finally, take into account the size and flow rate of the bottle to match your baby's growing appetite and feeding rhythm. By keeping these considerations in mind, you can choose an anti-colic bottle that offers comfort, convenience, and a peaceful feeding experience for both you and your baby.
Anti-colic feeding bottles offer a range of benefits that not only ensure a more comfortable and enjoyable feeding experience for your baby but also provide peace of mind and convenience for you as a parent. From reducing colic symptoms and promoting proper digestion to encouraging natural latching and supporting healthy feeding habits, these bottles are designed with both the baby's and parent's best interests in mind. Baby feeding bottle with spoon in Delhi
#Baby feeding bottle sippers in India#Baby feeding bottle glass suppliers in Delhi#Baby Feeding bottle with spoon in delhi#baby feeding bottle#feeding bottle#babyfeedingbottle#feedingbottle#babyfeeding#babybottle#bottlefeeding
0 notes
Text
Homeopathic Relief for Colicky Abdominal Pain - Safe & Natural Remedies
Explore safe, natural remedies for colicky abdominal pain treatment. Find immediate relief with our specially formulated remedies
Introduction
Colicky abdominal pain is a common but distressing condition characterized by sudden, severe spasms in the abdomen. This pain often stems from intestinal gas or obstructions. Homeopathy offers effective, gentle relief for this pain, utilizing natural…

View On WordPress
0 notes
Text
Urgent Management Is Necessary For Intestinal Obstruction - Surgical Expert in Chandigarh
Intestinal obstruction is a serious medical condition characterized by the partial or complete blockage of the normal flow of digestive contents through the intestines. This condition can be caused by various factors and can lead to severe complications if not promptly diagnosed and managed. Let’s explore the causes, clinical presentation, diagnostic methods, and treatment options for intestinal obstruction.
Causes of Intestinal Obstruction
Intestinal obstruction can occur in both the small intestine and the large intestine (colon) and may be caused by various factors, including:
Mechanical Obstruction
This is the most common cause and is often due to physical blockages, such as:
Adhesions: Scar tissue that forms after abdominal surgery.
Hernias: When a portion of the intestine pushes through a weak spot in the abdominal wall.
Tumors: Benign or malignant growths that obstruct the intestinal lumen.
Intussusception: Telescoping of one segment of the intestine into another.
Volvulus: Twisting of the intestine upon itself.
Functional Obstruction: This occurs when there is no physical blockage but the intestines fail to function properly due to issues like muscle or nerve problems.
Clinical Presentation
The presentation of Intestinal obstruction can vary depending on the location, severity, and underlying cause. Common symptoms and signs include:
Abdominal Pain: Crampy, colicky pain that comes and goes, often in waves, as the intestine tries to overcome the obstruction.
Vomiting: Frequent and forceful vomiting, which may become feculent (containing feces) in complete obstruction.
Abdominal Distension: Swelling and bloating of the abdomen due to trapped gas and fluids.
Constipation: Inability to pass stool or gas, especially in cases of large intestine obstruction.
Dehydration: Due to vomiting and fluid loss, patients may become dehydrated, leading to dry mouth, decreased urine output, and electrolyte imbalances.
Fever: In cases of strangulated obstruction where blood supply to the affected segment is compromised.
Diagnosis
Diagnosing Intestinal obstruction typically involves a combination of clinical assessment and imaging studies:
Physical Examination: The healthcare provider will perform a physical examination, including palpating the abdomen for tenderness, distension, and abnormal bowel sounds.
X-rays: Abdominal X-rays can reveal signs of obstruction, such as dilated loops of bowel and air-fluid levels.
CT Scan: A computed tomography (CT) scan of the abdomen can provide detailed images and help determine the cause and location of the obstruction.
Blood Tests: These are conducted to assess for electrolyte imbalances and signs of infection in cases of strangulated obstruction.
Visit Our Website For More Details: https://drrajeevkapoor.com/
0 notes
Text
gastro doctors in pattaravakkam
GI Tract Disease Symptoms and Process of Diagnosis
We all experience stomach pain, upset stomach, and abdominal pain from time to time, but these are usually not serious. However, especially if you have severe or stabbing abdominal pain, these may indicate that something in your body is not working properly. Causes can range from bloating and muscle strain to something more serious likes an internal infection or heart attack. In such circumstances, you need to consult gastro doctors in Pattaravakkam Chennai.
Symptoms associated with abdominal pain
Chest pain (see your doctor immediately)
Bloating or swelling lasting for several days
An injury or recent accident
Blood or dark stools
Vomiting blood or dark matter
Changes in bowel habits
Unexpected weight loss
Difficulty swallowing
Repeated diarrhea going on more than 5 days
Persistent vaginal bleeding
Fever greater than 100 degrees
Burning sensation during urination or frequent urination
Digestive disorders or Indigestion is a group of disorders that occur when the digestive system does not function properly. Health experts have divided GI complications into two categories: organic gastrointestinal diseases and functional gastrointestinal diseases. Organic gastrointestinal disorders occur when the digestive system has a structural abnormality and does not function properly. In functional gastrointestinal diseases, the gastrointestinal tract appears structurally normal but is still not fully functional. Some of the common GI disorders include -
Gallstones
Celiac disease
Crohn’s disease
Ulcerative colitis (uc)
Irritable bowel syndrome (ibs)
Small intestinal bacterial overgrowth (sibo)
Gastroesophageal reflux disease (gerd)
Abdominal Pain Diagnosis
When it comes to treating GI tract complications, your doctor will first physical exam and will ask about the symptoms and medical history. There are several types of stomach pains. The gastro doctors in Pattaravakkam could ask you whether such stomach pain is mild or severe, burning or achy, dull or sharp, crampy or colicky, whether it appears in one place or all over, constant or in waves. All such data will help the doctor to diagnosis the actual cause of pain and determine what to do about it.
0 notes
Text
Emergency Abdominal Pain Management

Due to the vast range of probable causes, which can range from minor and self-limiting diseases to life-threatening situations, abdominal pain is a common presenting symptom in emergency medical departments. Severe abdominal pain requires immediate medical concern which includes optimum assessment, treatment, and results.
This article will delve into the complex and often challenging world of emergency abdominal pain management, focusing on causes, assessment techniques, and treatment strategies. Meanwhile, references taken from Dr. Dipty Mangla a Pain Management Physician renowned for abdominal pain treatment in New Jersey have made the article a guide to consider while learning about abdominal pain management.
Causes of Abdominal Pain
Abdominal pain has various reasons. It may be caused by gastrointestinal issues to problems with other organs and systems within the body. Some common causes of abdominal are as follows:
1. Gastrointestinal Disorders
a. Gastritis and Peptic Ulcers: Inflammation of the stomach lining or the presence of ulcers can lead to sharp, burning pain in the upper abdomen.
b. Gastroenteritis: It often caused by viral or bacterial infections, this condition leads to stomach cramps and diarrhea.
c. Inflammatory Bowel Disease (IBD): Conditions like Crohn's disease and ulcerative colitis can cause severe abdominal pain. It typically accompanied by diarrhoea, weight loss, and other gastrointestinal symptoms.
d. Appendicitis: Inflammation of the appendix, located in the lower right abdomen, results in sharp, worsening pain that usually requires surgical intervention.
2. Gallbladder and Liver Disorders
a. Gallstones: The presence of gallstones in the gallbladder can lead to intense pain, usually in the upper right abdomen.
b. Hepatitis: Inflammation of the liver due to viral infections or other factors can cause abdominal discomfort, particularly in the right upper quadrant.
3. Kidney and Urinary Tract Problems
a. Kidney Stones: These small, hard mineral deposits can cause severe, colicky pain in the lower back and lower abdomen.
b. Urinary Tract Infections (UTIs): Infections in the urinary tract can lead to lower abdominal pain, frequent urination, and a burning sensation while urinating.
4. Reproductive System Issues
a. Ectopic Pregnancy: When a fertilized egg implants outside the uterus, it can cause sharp, severe pain, typically on one side of the lower abdomen.
b. Ovarian Cysts: The growth or rupture of cysts on the ovaries can result in lower abdominal discomfort.
5. Vascular Problems
a. Aortic Aneurysm: A ballooning or rupture of the aorta can lead to sudden, intense pain in the abdomen and requires immediate medical attention.
6. Trauma
a. Blunt Abdominal Trauma: Injuries resulting from accidents or physical assaults can lead to abdominal pain and require prompt assessment.
7. Miscellaneous
a. Hernias: The protrusion of organs through a weakened abdominal wall can cause discomfort and may require surgical repair.
b. Pancreatitis: Inflammation of the pancreas can lead to severe abdominal pain, often radiating to the back.
c. Cancer: Abdominal pain may be a symptom of various types of cancer, including stomach, liver, pancreatic, or ovarian cancer.
Assessing Abdominal Pain
A careful and systematic approach to assessing abdominal pain is essential in the emergency department. The primary goal is to differentiate between benign conditions that may require simple symptom relief and potentially life-threatening conditions that demand immediate intervention.
Evaluation of The History Taking
A detailed history of the patient's abdominal pain is the first step in the assessment process. Clinicians should inquire about the onset, duration, location, quality, and severity of the pain. They should also explore any associated symptoms, such as nausea, vomiting, fever, changes in bowel habits, or urinary symptoms. Understanding the patient's medical history, including any pre-existing conditions, recent surgeries, or medication use, is crucial for identifying potential risk factors.
Physical Examination
A thorough physical examination follows the history taking. The focus should be on:
a. Abdominal Examination: Palpation of the abdomen can help identify areas of tenderness, guarding, or rebound tenderness, which may suggest peritoneal irritation. Percussion and auscultation can provide additional diagnostic clues.
b. Vital Signs: Monitoring vital signs, including blood pressure, heart rate, respiratory rate, and temperature, is vital for assessing the patient's overall condition and identifying signs of potential sepsis or shock.
c. Signs of Dehydration: Clues such as dry mucous membranes, sunken eyes, and poor skin turgor can suggest dehydration, which may result from vomiting, diarrhea, or inadequate fluid intake.
Laboratory and Radiological Tests
Appropriate laboratory and imaging studies can aid in the diagnosis and risk stratification of abdominal pain.
a. Blood Tests: Complete blood counts, basic metabolic panels, liver function tests, amylase, and lipase levels can help assess for infection, inflammation, or organ dysfunction.
b. Urinalysis: A urinalysis can detect urinary tract infections or hematuria.
c. Imaging: Depending on the clinical suspicion and findings, imaging studies such as abdominal X-rays, ultrasonography, computed tomography (CT) scans, or magnetic resonance imaging (MRI) may be necessary to identify structural abnormalities or acute conditions like appendicitis or kidney stones.
Specialized Tests
In some cases, more specific tests, such as endoscopy for gastrointestinal evaluation or a pregnancy test for women of childbearing age, may be required for a precise diagnosis.
Treatment Strategies
The treatment of abdominal pain in the emergency department varies widely based on the underlying cause and the patient's condition. Here are some key strategies:
Pain Management
Managing pain is a crucial aspect of treatment. Non-prescription analgesics, such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs), can provide relief for mild cases. For more severe pain, especially in acute conditions like appendicitis, intravenous opioids may be necessary. However, opioid use should be judicious, given the risk of addiction and potential side effects.
Fluid Resuscitation
Dehydrated patients, often due to conditions like vomiting and diarrhea, may require intravenous (IV) fluid resuscitation to correct fluid and electrolyte imbalances.
Antiemetics
Nausea and vomiting are common accompanying symptoms of abdominal pain. Antiemetic medications can help relieve these symptoms and improve the patient's overall comfort.
Antibiotics
In cases where infection is suspected, empiric antibiotic therapy may be initiated while waiting for test results or before definitive treatment, such as surgical intervention.
Surgical Intervention
For conditions like appendicitis, bowel obstruction, or acute cholecystitis, surgical intervention may be necessary to address the underlying problem. In these cases, prompt consultation with a surgeon is vital.
Symptomatic Relief
Patients with less severe conditions, such as gastritis or mild gastroenteritis, may benefit from symptom relief measures, including dietary modifications, antacids, or anti-diarrheal medications.
Disposition
The decision to admit or discharge a patient depends on the diagnosis, severity of the condition, and the patient's response to initial treatment. Patients with life-threatening conditions, such as aortic aneurysm, will require immediate admission and potentially surgery, while those with mild gastroenteritis may be sent home with instructions for self-care and follow-up.
Special Considerations
Pediatric Patients
Abdominal pain in children can be challenging to assess, as young children may not effectively communicate their symptoms. Special consideration must be given to pediatric patients, with a focus on the child's overall appearance, pain assessment, and a cautious approach to imaging.
Geriatric Patients
In older adults, abdominal pain can be atypical and may be associated with underlying comorbidities. Careful evaluation, especially for potentially life-threatening conditions like aortic aneurysm, is essential.
Conclusion
Emergency abdominal pain management is a multifaceted process that demands a systematic approach, beginning with a thorough history and physical examination. It is imperative for healthcare providers to be aware of the wide array of potential causes, from benign conditions to life-threatening emergencies. The successful management of abdominal pain hinges on prompt and accurate diagnosis, followed by appropriate treatment strategies.
In cases where surgery is required, timely consultation with a surgeon is vital. In order to find one pain management physician in New Jersey you can visit MainLand Pain Management and schedule a consultation with Dr. Dipty Mangla. She is a leading expert in addressing and treating various types of chronic and acute pain. Some of the pain management treatments she is known for include Kyphoplasty, Radiofrequency Ablation, Spinal Cord Stimulator, and Peripheral Nerve Stimulator.
#Abdominal Pain Treatment#Pain Treatment#Abdominal Pain Treatment in New Jersey#pain management physician in New Jersey
0 notes
Text
Abdominal pain – Causes, Types & Best Treatment for It
Abdominal discomfort can occur anywhere between your ribs and pelvis in the midsection. Abdominal discomfort is usually referred to as "stomach pain" or a "stomachache". Although organs other than the stomach can also produce abdominal pain, medications like Etadol 100mg and Aspadol 100mg can be used to treat this sort of discomfort.
Your stomach resides in your abdomen.
Liver.
The gallbladder.
The pancreas.
Small intestines.
A very large gut.
These are all components of the digestive system. However, the muscles, skin, and abdominal wall that make up the outside of your abdomen can also cause discomfort. Your back, pelvis, or chest may also occasionally be to fault for the abdominal pain you feel.
Abdominal pain may have a wide range of signs and causes:
• Gentle or severe.
• Sharp or boring.
• Burning or aching.
· A cramp or colicky.
• Regular or sporadic; either limited (in one place) or universal (all over).
In the end, abdominal discomfort is a condition that only you can diagnose. Since your doctor is unable to measure it, it is what you say it is. Your doctor will always treat your stomach discomfort carefully.
What are the four types of abdominal pain?
Since your abdomen contains several organs, your doctor may want to focus on a specific area of your abdomen to determine what sort of discomfort you're experiencing. The abdomen is frequently divided into four quadrants by medical professionals. If your pain is in the: they might inquire.
Upper and lower halves. Pain in the upper abdomen occurs above the belly button. It is below lower abdominal ache.
Left side/right side. Your belly button and sternum form the midline of your abdomen.
What causes stomach discomfort most frequently?
Abdominal discomfort often has transient, non-serious causes. They might be caused by digestion, menstruation, or a short-term illness. For instance:
Intestinal problems:
After eating, abdominal discomfort may result from:
Indigestion.
Discomfort from gas.
Constipation.
Diarrhea.
Food intolerances and allergies.
Foodborne illness.
Inflammation
Temporary inflammation can be brought on by irritation or infection in your organs, including:
Gastroenteritis caused by a virus.
Stomach ulcer illness.
Acid reflux disease (gerd) that is persistent.
Uti, or urinary tract infection.
Cycle of female reproduction
You may occasionally feel discomfort if you have a uterus from:
Period cramps.
A painful ovulation.
How is abdominal pain diagnosed?
You will be questioned in-depth by your healthcare practitioner regarding your stomach discomfort. They will inquire as to:
Whatever place you feel it.
Exactly how it feels.
How long have you had it?
If it arrives and departs.
If it is deteriorating.
If it moves or if it remains still.
What improves or worsens it.
What further signs you may have.
Your healthcare professional will try to establish if you require emergency treatment based on your responses. Your healthcare professional might be able to detect straight away whether your belly discomfort is transient and not significant in some cases.
They might wish to do certain tests if they detect a more serious problem sometimes. Additionally, on their first visit, they might not always be able to solve the puzzle. You could experience less discomfort or need to go back for more testing.
How can stomach discomfort be treated?
There are many different reasons and therapies for abdominal discomfort. Surgery could be necessary for some illnesses, such gallstones or appendicitis. Others, including infections or ulcers, may be treated with medication. Additionally, there are occasions when you simply have to endure a kidney stone or a case of stomach sickness until it passes.
Finding out the source of your stomach discomfort is crucial, especially if it doesn't go away on its own. Keep in mind that even minor conditions might develop into serious ones. But if you're quite certain that your stomachache is caused by digestion, you can start by treating it with:
Stomach rest. Eat nothing, or just simple things like crackers or bananas that are easy to digest.
Hydration. Take in a lot of water or a hydration drink.
Heat treatment. Consider using a warm water bottle or taking a bath.
Domestic remedies. Licorice can aid with gas, ginger can help with indigestion, and peppermint can help your digestive muscles relax.

0 notes
Text
Abdominal Pain (Causes, Remedies, Treatment)

Abdominal pain definition and facts
Abdominal pain refers to pain or discomfort felt in the region between the chest and the groin. It can be acute or chronic and can range from mild to severe.Here are some important facts about abdominal pain:- Gastrointestinal issues: Conditions like acid reflux, gastroenteritis, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), constipation, and diarrhea can cause abdominal pain.
- Reproductive system issues: Women may experience abdominal pain due to menstrual cramps, endometriosis, ovarian cysts, or fibroids.
- Urinary tract issues: Conditions like urinary tract infections (UTIs) and kidney stones can cause abdominal pain.
- Pancreatic and liver issues: Conditions like pancreatitis and hepatitis can cause abdominal pain.
- Abdominal wall issues: Conditions like hernias, strains, and sprains can cause abdominal pain.
- Vascular issues: Aortic aneurysm, mesenteric ischemia, and ischemic bowel disease can cause abdominal pain.
- Medications: Some medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), can cause abdominal pain as a side effect.
- Psychological issues: Anxiety, depression, and stress can cause abdominal pain.
- Gastrointestinal issues: Conditions like acid reflux, gastroenteritis, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), constipation, and diarrhea can cause abdominal pain.
- Reproductive system issues: Women may experience abdominal pain due to menstrual cramps, endometriosis, ovarian cysts, or fibroids.
- Urinary tract issues: Conditions like urinary tract infections (UTIs) and kidney stones can cause abdominal pain.
- Pancreatic and liver issues: Conditions like pancreatitis and hepatitis can cause abdominal pain.
- Abdominal wall issues: Conditions like hernias, strains, and sprains can cause abdominal pain.
- Vascular issues: Aortic aneurysm, mesenteric ischemia, and ischemic bowel disease can cause abdominal pain.
- Medications: Some medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), can cause abdominal pain as a side effect.
- Psychological issues: Anxiety, depression, and stress can cause abdominal pain.
- Nausea and vomiting
- Loss of appetite
- Fever
- Diarrhea or constipation
- Bloating or gas
- Fatigue
- Dehydration
- Jaundice
- Upper abdomen
- Lower abdomen
- Right upper quadrant
- Left upper quadrant
- Right lower quadrant
- Left lower quadrant
- Generalized abdominal pain (pain in the entire abdomen)
- Localized abdominal pain (pain in a specific area of the abdomen)
- Colicky pain (intermittent pain that comes and goes in waves)
- Cramping pain (pain that feels like cramps)
- Sharp pain (pain that feels sharp or stabbing)
- Dull pain (pain that feels achy or sore)
- Mild abdominal pain (pain that is tolerable and does not interfere with daily activities)
- Moderate abdominal pain (pain that is uncomfortable and may interfere with daily activities)
- Severe abdominal pain (pain that is intense and may require immediate medical attention)
- Sudden onset: Abdominal pain can sometimes come on suddenly and may be severe, such as in the case of a ruptured organ or a blockage in the digestive tract.
- Gradual onset: Abdominal pain may also develop gradually over time, such as in the case of a chronic condition like inflammatory bowel disease (IBD).
- After a meal: Abdominal pain that occurs after eating may be caused by conditions like acid reflux or gallbladder disease.
- During menstrual cycle: Women may experience abdominal pain during their menstrual cycle due to menstrual cramps or other reproductive system issues.
- After physical activity: Abdominal pain that occurs after physical activity may be caused by muscle strain or injury.
- Upper abdominal pain: This type of pain is felt in the area above the belly button and below the ribs. It may be caused by conditions affecting the stomach, pancreas, liver, gallbladder, or upper part of the small intestine.
- Lower abdominal pain: This type of pain is felt below the belly button and may be caused by conditions affecting the large intestine, bladder, uterus or ovaries (in women), or the lower part of the small intestine.
- Right upper quadrant pain: This type of pain is felt in the upper right side of the abdomen and may be caused by conditions affecting the liver, gallbladder, or right kidney.
- Left upper quadrant pain: This type of pain is felt in the upper left side of the abdomen and may be caused by conditions affecting the spleen, stomach, or left kidney.
- Right lower quadrant pain: This type of pain is felt in the lower right side of the abdomen and may be caused by conditions affecting the appendix, cecum, or right ovary (in women).
- Left lower quadrant pain: This type of pain is felt in the lower left side of the abdomen and may be caused by conditions affecting the sigmoid colon, left ovary (in women), or left ureter.
- Cramping: Abdominal pain that is crampy or colicky in nature may be caused by conditions such as irritable bowel syndrome (IBS), gastroenteritis, or menstrual cramps.
- Sharp: Abdominal pain that is sharp or stabbing may be caused by conditions such as pancreatitis, gallstones, or a perforated organ.
- Dull: Abdominal pain that is dull or achy in nature may be caused by conditions such as constipation, a urinary tract infection (UTI), or endometriosis (in women).
- Burning: Abdominal pain that feels like a burning sensation may be caused by conditions such as gastroesophageal reflux disease (GERD) or gastritis.
- Intermittent: Abdominal pain that comes and goes may be caused by conditions such as IBS or inflammatory bowel disease.
- Constant: Abdominal pain that is constant and unrelenting may be caused by conditions such as appendicitis, pancreatitis, or a ruptured organ.
- Acute pain: Abdominal pain that comes on suddenly and lasts for a few hours to a few days may be caused by conditions such as gastroenteritis, appendicitis, or a urinary tract infection.
- Chronic pain: Abdominal pain that lasts for weeks or months may be caused by conditions such as inflammatory bowel disease, endometriosis, or chronic pancreatitis.
- Intermittent pain: Abdominal pain that comes and goes over a period of time may be caused by conditions such as irritable bowel syndrome or intermittent gastritis.
- Colicky pain: Abdominal pain that occurs in waves or spasms may be caused by conditions such as gallstones or renal colic (kidney stones).
- Eating: Pain that worsens after eating may be caused by conditions such as gastritis, peptic ulcer disease, or gastroesophageal reflux disease (GERD).
- Movement: Pain that worsens with movement may be caused by conditions such as appendicitis, peritonitis, or a ruptured organ.
- Bowel movements: Pain that worsens during or after bowel movements may be caused by conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease, or anal fissures.
- Menstruation: Pain that worsens during menstruation may be caused by conditions such as endometriosis or uterine fibroids.
- Stress: Pain that worsens with stress may be caused by conditions such as functional dyspepsia or irritable bowel syndrome (IBS).
- Certain foods: Pain that worsens after consuming certain foods or beverages may be caused by food intolerances or sensitivities, such as lactose intolerance or celiac disease.
- Rest and relaxation: Taking a break and resting can help relieve abdominal pain caused by stress, anxiety, or tension.
- Heat therapy: Applying a heating pad or warm compress to the affected area can help relieve abdominal pain caused by muscle tension, menstrual cramps, or gas.
- Over-the-counter medication: Pain relievers such as acetaminophen or ibuprofen can help relieve mild to moderate abdominal pain caused by inflammation, menstrual cramps, or other conditions.
- Hydration: Drinking plenty of water can help relieve abdominal pain caused by constipation or dehydration.
- Dietary changes: Avoiding spicy, fatty, or high-fiber foods can help relieve abdominal pain caused by indigestion or gastrointestinal issues.
- Physical exam: The healthcare provider will perform a physical exam, checking for any signs of tenderness, swelling, or abnormalities in the abdomen.
- Medical history: The healthcare provider will ask about the nature and duration of the pain, as well as any other symptoms that may be present.
- Imaging tests: Imaging tests such as X-rays, ultrasound, CT scan, or MRI can help identify any abnormalities or damage to the organs in the abdomen.
- Blood tests: Blood tests can help identify any signs of infection, inflammation, or organ damage.
- Endoscopy: Endoscopy involves inserting a thin, flexible tube with a camera into the digestive tract to view the organs directly and take tissue samples for further testing.
- Stool analysis: Stool analysis can help identify any signs of infection or inflammation in the digestive tract.
- Blood tests: A blood test can help identify any signs of infection, inflammation, organ damage, or other abnormalities that may be causing the abdominal pain.
- Imaging tests: Imaging tests such as X-rays, ultrasound, CT scan, or MRI can help identify any abnormalities or damage to the organs in the abdomen.
- Endoscopy: Endoscopy involves inserting a thin, flexible tube with a camera into the digestive tract to view the organs directly and take tissue samples for further testing.
- Stool analysis: Stool analysis can help identify any signs of infection or inflammation in the digestive tract.
- Urine tests: Urine tests can help identify any signs of infection or inflammation in the urinary tract or kidneys, which can cause abdominal pain.
- Pregnancy test: A pregnancy test may be performed if the abdominal pain is accompanied by other symptoms such as missed periods or vaginal bleeding.
- An elevated white count suggests inflammation or infection (as with appendicitis, pancreatitis, diverticulitis, or colitis).
- A low red blood cell count may indicate a bleed in the intestines.
- Amylase and lipase (enzymes produced by the pancreas) commonly are elevated in pancreatitis.
- Liver enzymes may be elevated with gallstone attacks or acute hepatitis.
- Blood in the urine suggests kidney stones.
- When there is diarrhea, white blood cells in the stool suggest intestinal inflammation or infection.
- Esophagogastroduodenoscopy (EGD): This procedure allows doctors to examine the lining of the esophagus, stomach, and small intestine.
- Colonoscopy: This procedure is used to examine the large intestine and rectum for signs of inflammation, bleeding, or other abnormalities.
- Endoscopic retrograde cholangiopancreatography (ERCP): This procedure combines endoscopy and X-ray imaging to examine the bile ducts and pancreas for blockages or other issues.
- Endoscopic ultrasound (EUS): This procedure uses ultrasound technology to examine the digestive tract and surrounding organs for signs of abnormalities or tumors.
- Foods to eat: ginger, peppermint tea, fennel, chamomile tea, probiotics (such as yogurt)
- Foods to avoid: carbonated drinks, beans, broccoli, cabbage, onions, dairy products
- OTC treatments: simethicone, activated charcoal tablets
- Foods to eat: high-fiber foods (such as fruits, vegetables, whole grains), prunes, kiwi, flaxseeds
- Foods to avoid: processed foods, dairy products, red meat
- Natural remedies: drinking plenty of water, exercise, avoiding holding in bowel movements
- OTC treatments: fiber supplements, stool softeners, laxatives (use with caution and follow package instructions)
- Foods to eat: oatmeal, ginger, melons, bananas, lean protein sources (such as fish and poultry), vegetables (except for those high in acid, such as tomatoes)
- Foods to avoid: citrus fruits, tomatoes, chocolate, caffeine, spicy foods, fatty foods, alcohol
- Natural remedies: chewing gum, elevating the head of the bed, avoiding lying down after meals
- OTC treatments: antacids, H2 blockers, proton pump inhibitors (use with caution and follow package instructions)
- Foods to eat: magnesium-rich foods (such as leafy greens, nuts, and seeds), fruits, whole grains, lean protein sources
- Foods to avoid: caffeine, alcohol, salty foods, processed foods
- Natural remedies: heat therapy, massage, exercise, relaxation techniques
- OTC treatments: nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (use with caution and follow package instructions)
- For instance, the pain associated with appendicitis may sometimes be felt in the upper right abdomen, while diverticulitis can cause pain on the right side. Elderly patients and those taking corticosteroids may experience minimal or no pain and tenderness even when there is inflammation, as in the case of cholecystitis or diverticulitis. This is because corticosteroids reduce inflammation.
- Gallstones, especially small ones, may not be detected by ultrasound examinations.
- Pancreatic cancer, particularly small ones, may not be visible on CT scans.
- Intestinal obstruction or stomach perforation signs may not be detected by a KUB.
- Appendicitis or even abscesses, especially small ones, may not be demonstrated by ultrasounds and CT scans.
- Blood tests like CBC and others may appear normal despite severe infection or inflammation, especially in individuals taking corticosteroids or other immune system-suppressing drugs.
- Symptoms of IBS may imitate bowel obstruction, cancer, ulcers, gallbladder attacks, or even appendicitis.
- Crohn's disease can imitate appendicitis.
- Infection of the right kidney can imitate acute cholecystitis.
- A ruptured right ovarian cyst can imitate appendicitis, whereas a ruptured left ovarian cyst can mimic diverticulitis.
- Kidney stones can mimic appendicitis or diverticulitis.
- Examples of this include the spreading of pancreatitis inflammation to involve the whole abdomen and the progression of biliary colic to cholecystitis, as discussed earlier.
Read the full article
0 notes
Text
How To Extract The Sunthi Powder

Individuals who want to purchase sunthi powder can get it through the nutrapharm platform. Through our platform, we provide herbs and extracts for customers. Sunthi powder is a pure herb extracted from pure ginger; its supplement is used in ayurvedic medicines. It has numerous benefits, such as relieving pain that includes abdominal colicky, joint, headaches, and menstrual. Sunthi powder is a herbal medicine used to treat digestive disorders.
0 notes
Text

𝐑𝐚𝐬𝐚 𝐒𝐢𝐧𝐝𝐨𝐨𝐫𝐚 𝐂𝐚𝐩𝐬𝐮𝐥𝐞: 𝑯𝒆𝒍𝒑𝒔 𝒕𝒐 𝒃𝒐𝒐𝒔𝒕 𝒊𝒎𝒎𝒖𝒏𝒆 𝒔𝒚𝒔𝒕𝒆𝒎, 𝒕𝒐 𝒊𝒎𝒑𝒓𝒐𝒗𝒆 𝒔𝒕𝒓𝒆𝒏𝒈𝒕𝒉.
0 notes
Text
What Is Abdominal Pain? Symptoms, Causes, Treatment, and Prevention
What Is Abdominal Pain? Symptoms, Causes, Treatment, and Prevention
Signs and Symptoms of Abdominal Pain
Abdominal ache may additionally take numerous unique forms. In addition to how extreme it is, stomach ache can be described in the following ways:
Generalized Pain This refers to ache felt in greater than half of of your belly area, and is standard of belly viruses, indigestion, or gasoline as the purpose of your pain.
Localized Pain This refers to ache felt…

View On WordPress
#Abdominal Pain#abdominal pain after eating#abdominal pain and bloating#abdominal pain and diarrhea#abdominal pain before period#abdominal pain bloating#Abdominal Pain Causes#abdominal pain constipation#Abdominal Pain Diagnosis#Abdominal Pain Prevention#Abdominal Pain Symptoms#Abdominal Pain Treatment#acute abdominal pain#after eating lower abdominal pain#are cramps abdominal pain#back and abdominal pain#blood in stool and abdominal pain#burning abdominal pain#chronic abdominal pain#colicky abdominal pain#crampy abdominal pain#lower abdominal pain#lower left abdominal pain#severe abdominal pain#upper abdominal pain
0 notes
Text
gastrointestinal system studies
case study – 43 yo female, dyspepsia and fatigue
» physical examination
abdominal pain
pale skin, looks ill
» laboratory testing and assays
macrocytic anemia (large red blood cells, few in number) | possibly arrest in early stages of differentiation in bone marrow
(microcytic anemia is a small RBC size, having to do with iron deficiency)
low Vitamin B12 levels | B12 is important for RBC differentiation and development
elevated serum gastrin levels (marker of abnormal GI activity)
» endoscopy / colonoscopy
run a probe with attached light down esophagus (can also grab biopsy samples) | colonoscopy is from rectum
healthy stomach has folds with glands in it
patient’s stomach has atrophic folds - it’s smooth, regressed folds
presence of cyst / tumor / polyp
pH = 6, low gastric acid aka hypochlorhydria
» biopsy procedure
cardia → body → antrum of stomach, which all have different linings
general: stomach lumen → lumen lining cells → (area-specific linings)
(body = pink and mitochondria-heavy, mutinous and oxyntic glands with gastric acid secretions, as well as ECL) specifically pink, mitochondria, and presence of oxyntic glands in histology
(antrum = mutinous glands and G-neuroendocrine hormonal cells, secreting gastrin)
G-cell gastrin from antrum binds ECL → ECL secretes histamine → histamine stimulates acid from oxyntic glands
patient biopsy from antrum has glands spaced far apart, and spatial extension causes stomach folds to pull out and become smooth
patient biopsy from antrum has lymphocytes (increased purple nucleus stains) – chronic gastritis | acute is neutrophils
patient’s body has “antralized” → metaplasia, or a change in tissue to look like another organ’s tissue after injury and bodily adaptations
verdict from biopsy: atrophic metaplasia chronic lymphatic gastritis
» assessing the cyst / tumor mass
carcinoid - neuroendocrine cells form malignant tumor
cancer cells have bypassed stroma
» summary
pale skin = anemic = bleeding or low RBC count
fold atrophy = chronic inflammation stretches lamina of stomach = high pH because glands ≠ making acid
biopsy = metaplastic, atrophic, lymphocyte proliferations, tumor mass
» AMAG diagnosis: autoimmune metaplastic atrophic gastritis
auto-antibodies are made against oxyntic gland’s parietal cells
antibodies recruit lymphocytes, which begin destroying oxyntic glands
body becomes “antralized” because pink oxyntic glands are destroyed
stomach grows back cells, but they are mucin-secreting cells and pH stays low because gastrin ≠ responded to
gastrin over-secretion to compensate → gastrin becomes a growth factor and NE cells in antrum begin to proliferate
NE cells acquire some cancerous mutation → and the tumor forms
case study – 40 yo female, episodic abdominal pain, jaundice, fever
» physical examination
colicky upper right quadrant – pain occurs intermittently
especially after a meal or when contact is made to area
painful jaundice
» laboratory assays
WBC, bilirubin, amylase and lipase build-up | possible pancreatic injury
alkaline phosphatase – made by cells in bile ducts
» imaging – abdominal ultrasound and ERCP
ultrasound: gallbladder is enlarged, contains gallstones
ERCP: analyze tiny bile and pancreatic ducts, as well as gallbladder, via injection of dye through esophageal line to duodenum
imaging of dye from bile, cystic, and pancreatic ducts and can see all three organs
filling defect - dye cannot get to pancreatic duct or gallbladder
slow transit - dye takes a long time to get to liver from bile ducts
bile duct injury, pancreatic injury, gallbladder blockage
bile stops moving and grows infected → fever and inflammation, WBC up
» verdict from the ERCP: gallstone pancreatitis
gallbladder stones exit the gallbladder alongside bile after a fatty meal, and stone blocks pancreatic duct
another stone blocks the cystic duct and causes pain
stones - commonly cholesterol, or other types and compositions
digestive enzymes spill out into pancreas and auto-digest it causing more pain
can inject stone-dissolving substances, or elective cholecystectomy (gallbladder removal, voluntary) if needed
any GI surgical procedure → adhesin tissue builds up and pins parts of bowel, blocks it → need to re-operate when things build up and infection occurs
case study – 45 yo male, rectal bleeding
» physical examination:
medical history: HIV+
otherwise normal
» laboratory testing and assays
undetectable HIV viral load (i.e., taking anti-retroviral medications well)
normal T-cell counts (visit is not due to HIV flare-up)
RPR+ (IgG) against syphilis | IgM is recent infection, IgG is long-time infection, high sensitivity
rectal bleeding could be due to gonorrhea, HPV
» colonoscopy findings
flat, barely raised polyp on right, sessile → removed for biopsy
glands of the area are crowded, overgrown and hypertrophic
lumens are irregular, branched and serrated instead of round in healthy patients
diagnosis: sessile serrated adenoma, pre-cancerous so removed
large, raised polyp on left, pedunculated → removed
overgrown, hypertrophic lining - cancerous epithelial cells
pre-cancerous polyp, mushroom-like → has not yet invaded stroma
diagnosis: tubular adenoma, where the growth looks like a tube
upper colon is spotted with white plaques (ulcers - fibrin and inflammatory cells), and inflamed, eroded → biopsy
» rectal biopsy to find source of bleeding
abundance of inflammatory cells, lamina expanded as a result of overcrowding
neutrophils from acute inflammation; plasma cells from chronic inflammation
acute inflammation turned chronic, essentially → silver staining reveals syphilis organisms in rectum
» verdict: syphilis in rectum causing rectal bleeding
4 notes
·
View notes
Text
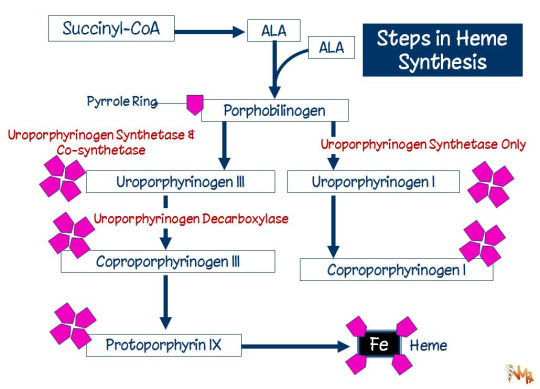

Acute Intermittent Porphyria (AIP) is due to deficiency of uroporphyrinogen (I) synthase (aka porphobilinogen deaminase). Porphobilinogen and ALA accumulate in urine. It is the most severe hepatic (abdominal) form of porphyria and more common in women. It is precipitated by drugs (barbiturates, estrogen, alcohol, sulfa, etc.), and sun exposure. Patients present with colicky pain, vomiting, fever, and leukocytosis. As opposed to other porphyrias, patients characteristically lack photosensitivity. For this reason, excessive sun exposure quite often is associated with initiation of porphyric symptoms in these patients.
Note that variegate porphyria (also known as mixed hepatic porphyria and South African genetic porphyria) is an autosomal dominant porphyria that presents with acute symptoms like AIP, but in contrast to AIP it presents with photosensitivity.
4 notes
·
View notes