#diffusion MRI
Explore tagged Tumblr posts
Text

Recovering from Paralysis
Nerve affected by Bell's palsy – a rapid onset temporary facial paralysis of unknown cause – analysed by MRI reveals not axon damage but myelin sheath injury which can recover thus explaining why the disorder is usually self-limiting
Read the published research paper here
Image from work by Yi Qin and colleagues
Radiology Department, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, XiQing District, Tianjin, China
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Scientific Reports, September 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#biology#neuroscience#bell's palsy#myelin#nerve damage#diffusion mri#mri#brain#facial nerves#nerves
11 notes
·
View notes
Text
I feel very bad and weird. I feel that something bodily is not working, uh. It's really hard to explain. I don't even know how to explain it. What it feels like it:
certain people's "identities" or "profile pictures in my mind" were deleted from my mind, so I still have factual knowledge of those people and I have memories featuring them, but they feel fake. They feel like people from a dream or something, not like they're real people, even though I know they're real.
The emotions associated with these people are still just as strong, but it's like they aren't attached to anything. They surge through me really intensely but find no place to rest. Uh it's like, I know factually who they're about but it doesn't "click", my brain can't find the person in its database or something so the emotion just comes up and then attaches to whatever I'm doing or whoever I happen to be talking to.
This was mostly just distressing and disorienting at first, but now that it's been two months I genuinely feel like I'm factually losing track of which feeling go with which people, because they keep coming up and re-attaching and it's confusing. I'm sad because I feel like I'm losing my sense of who my friends are, and I'm distressed because it feels very violating, like my relationships and memories are being invaded by whatever my brain happens to be thinking about at the time.
I'm scared that if this goes on long enough, I'll totally lose track and not be able to figure out what was what.
I don't know medically what it's happening. Everyone says it sounds like a TLE symptom but the problem is it's too consistent. It's not like I'm getting confused and then getting things a little more straight and then getting more confused, or whatever. It's totally black-and-white: these people's entries in my mental database have just been deleted, they're gone, there's no flux or whatever. That is not how I understand TLE to work, where confusion peaks after a seizure and then your mind kind of sorts things out, there should be an arc to it. Moreover I am not confused about anything else: it is literally just this, and things that feel like a knock-on effect of this. It feels very one-note.
MRI picked up nothing, which means no structural damage (there could still be damage but it would be micro scale). Also I wasn't hit in the head, this happened after anesthesia. So whatever happened had to be diffuse, right, it couldn't have targeted some specific region. And yet it feels like very specific information is fucked, and that's it. Everything else is fine, except for things that rely on this information (which, unfortunately, is a lot, because the people who's identities are messed up are people I think about pretty much daily, and with whom I associate all sorts of familiar activities and so on; there's pretty much no way to not think about it even if I'm trying).
WHAT is going on
37 notes
·
View notes
Note
hi, i was just wondering if you could make a post on apperceptive visual agnosia? love your posts so so much btw
Writing Notes: Apperceptive Visual Agnosia
Agnosia - A rare disease in which a person can’t recognize objects, shapes, or people. Often due to a brain or neurological condition.
Visual Agnosias - Disorders of visual object recognition following brain damage.
Apperceptive Agnosias - According to Lissauer, are those in which recognition fails because of an impairment in visual perception, which is nonetheless above the level of an elementary sensory deficit such as a visual field defect. Patients do not see objects normally, and hence cannot recognize them.
EXAMPLES. Among patients who have been labeled “apperceptive” are those:
who cannot discriminate a circle from a square,
who can recognize any one object but cannot see other objects presented at the same time, and
whose difficulty with object recognition is manifest only with objects presented at unusual orientations.
Apperceptive Visual Agnosias - also known as visual space agnosias, are characterized by the inability to perceive the structure or shape of an object. Persons with apperceptive agnosias have difficulty matching objects of similar form.
This type of agnosia is also classified as an "Object Agnosia". Specifically, the apperceptive type, i.e., the percept is not fully constructed and, therefore, patients are unable to copy drawings.
DIAGNOSIS
Agnosia is diagnosed through:
physical examination,
neuropsychological testing, and
brain imaging.
Examples of neuropsychological tests include:
visual distinction between real and unreal objects,
facial recognition,
verbal and nonverbal sound recognition,
odor recognition, and
tactile form recognition.
Magnetic resonance imaging (MRI) and computerized axial tomography (CAT) scanning may be used to identify brain lesions to aid diagnosis.
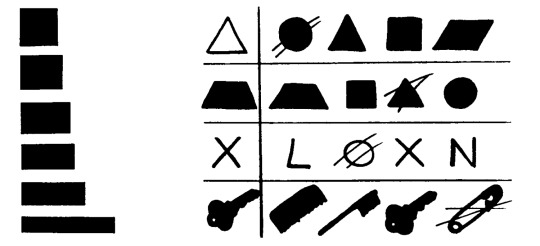
The above image shows the shape-matching ability of an apperceptive agnosic patient. On the left is a set of rectangles matched for overall area, which were presented pairwise to "Mr. S" to be judged same or different in shape. He was unable to discriminate all but the most distinctive, and made errors even with these. On the right are a set of rows containing a target shape (right) and a set of 4 choices to be matched with the target shape. Mr. S’s answers are marked.
CAUSES
It is thought to arise from a breakdown at relatively early stages of visual processing, where the elementary features of the stimulus are processed. Object recognition through verbal description by the examiner is preserved, instead.
These patients have relatively good visual fields, visual acuity, brightness discrimination, color vision, depth, and motion perception. Despite this, shape perception is abnormal in such a way that patients cannot recognize or copy pictures, letters, and even simple geometric shapes.
In most cases of apperceptive agnosia, the brain damage is diffuse, often caused by carbon monoxide poisoning.
In the rare cases with circumscribed brain lesions, the damage primarily affected the ventral occipitotemporal cortex bilaterally.
According to a widely accepted interpretation, apperceptive agnosia can be considered a deficit of shape perception resulting from defective perceptual grouping of object local features into a global percept.
TREATMENT
There is no direct treatment for visual agnosias. However, patients can benefit from rehabilitation to teach them alternative strategies that target specific difficulties.
Few agnosic patients regain sensory function, and most gains in recovery occur within the first few months or year of diagnosis.
Speech therapy and occupational therapy can help agnosic individuals cope with their conditions.
Sources: 1 2 3 4 5 6
Thanks so much for your kind words, hope this helps!
#agnosia#writing reference#writeblr#spilled ink#creative writing#literature#writing notes#writing prompt#writing#writers on tumblr#dark academia#poets on tumblr#light academia#writing resources
45 notes
·
View notes
Text
Reference archived on our website
Highlights • Long-COVID is heterogeneous in its symptoms, severity, and illness duration. • There was no association between long-COVID and cognitive performance. • Cognitive symptoms may represent functional cognitive disorders. • Long-COVID had lower mean diffusivity on diffusion imaging than normal recovery. • Diffusion imaging differences may suggest gliosis as a mechanism of long-COVID.
To be clear: There was no cognitive difference between people post infection. I can see some people misunderstanding what this says. It says there is some form of brain damage from covid across the board, even if you don't have long covid symptoms or diagnosis.
Abstract
Background
The pathophysiology of protracted symptoms after COVID-19 is unclear. This study aimed to determine if long-COVID is associated with differences in baseline characteristics, markers of white matter diffusivity in the brain, and lower scores on objective cognitive testing.
Methods
Individuals who experienced COVID-19 symptoms for more than 60 days post-infection (long-COVID) (n = 56) were compared to individuals who recovered from COVID-19 within 60 days of infection (normal recovery) (n = 35). Information regarding physical and mental health, and COVID-19 illness was collected. The National Institute of Health Toolbox Cognition Battery was administered. Participants underwent magnetic resonance imaging (MRI) with diffusion tensor imaging (DTI). Tract-based spatial statistics were used to perform a whole-brain voxel-wise analysis on standard DTI metrics (fractional anisotropy, axial diffusivity, mean diffusivity, radial diffusivity), controlling for age and sex. NIH Toolbox Age-Adjusted Fluid Cognition Scores were used to compare long-COVID and normal recovery groups, covarying for Age-Adjusted Crystallized Cognition Scores and years of education. False discovery rate correction was applied for multiple comparisons.
Results
There were no significant differences in age, sex, or history of neurovascular risk factors between the groups. The long-COVID group had significantly (p < 0.05) lower mean diffusivity than the normal recovery group across multiple white matter regions, including the internal capsule, anterior and superior corona radiata, corpus callosum, superior fronto-occiptal fasciculus, and posterior thalamic radiation. However, the effect sizes of these differences were small (all <|0.3|) and no significant differences were found for the other DTI metrics. Fluid cognition composite scores did not differ significantly between the long-COVID and normal recovery groups (p > 0.05).
Conclusions
Differences in diffusivity between long-COVID and normal recovery groups were found on only one DTI metric. This could represent subtle areas of pathology such as gliosis or edema, but the small effect sizes and non-specific nature of the diffusion indices make pathological inference difficult. Although long-COVID patients reported many neuropsychiatric symptoms, significant differences in objective cognitive performance were not found.
#long covid#covid 19#covid#mask up#pandemic#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#covid conscious#covid is not over
44 notes
·
View notes
Text
Neoplasms of the CNS
This is going to be a long one, so I apologize. This topic can be kinda boring and difficult, but it's good to know for anyone in med school. A lot of this stuff is also pretty high-yield for boards, so yay.
I'm going to go over a lot of different types, give you some basic facts, and show (and tell) you what it looks like. Hope you have a fun time reading :D
Glial Tumors
Glial cells are little helper cells in the brain. Gliomas are tumors made of these cells. You have three subtypes: pilocytic astrocytomas, diffuse low-grade gliomas (low grade astrocytomas and oligodendrogliomas), and malignant gliomas (anaplastic astrocytomas and glioblastomas). Glioblastomas are the most aggressive gliomas.
Pilocytic astrocytomas are the most common primary brain tumor in children. They are well-circumscribed and grow very slowly. They prefer the cerebellum and brainstem. Their most distinguishing feature are the Rosenthal fibers (pilocytic means fiber) and red inclusions. These can usually be treated with resection alone. Look how pretty it is:
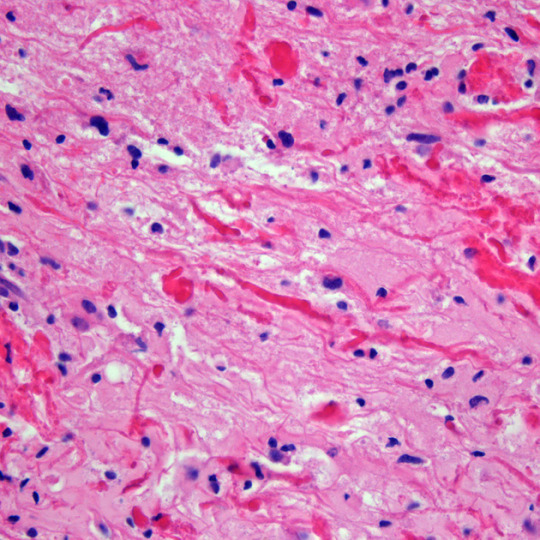
Low grade gliomas are the majority of adult brain tumors. They are infiltrating and are WHO grade 2-4. Both diffuse astrocytomas and oligodendrogliomas are going to be basically in the middle of the brain. Oligodendrogliomas prefer white matter of the cerebral hemispheres and infiltrate to the cortex. Microcalcifications are common. Oligodendrogliomas have a "fried egg" and "chickenwire" appearance, but this is usually stated as uniform cells with clear cytoplasm and branching, delicate blood vessels on board exams.

Diffuse astrocytomas show irregular, angulated, and hyperchromatic nuclei, and have a tendency to recur, spread, and progress to higher stages.
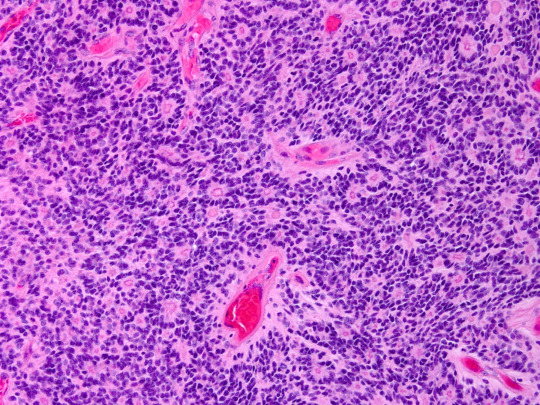
Now to the malignant gliomas. Malignant astrocytomas are the most common primary brain tumor in adults. You'll see a hypercellular glioma with poorly differentiated astrocytes. It tends to recue, and shows significant nuclear atypia and miotic activity (it's dividing!!). These can develop from other types of astrocytomas or de novo. They usually progress to glioblastoma.
Glioblastomas are the most common and most malignant gliomas. They are poorly defined, infiltrating, and will distort the brain. Some people say they look like butterflies on MRI (I say these people are full of shit). You'll see serphintine or psuedopalisading necrosis and microvascular proliferation. The morphology of the cells is highly variable (from giant and bizarre to small and tightly packed). There is about a one year median survival from disgnosis.
Medulloblastomas
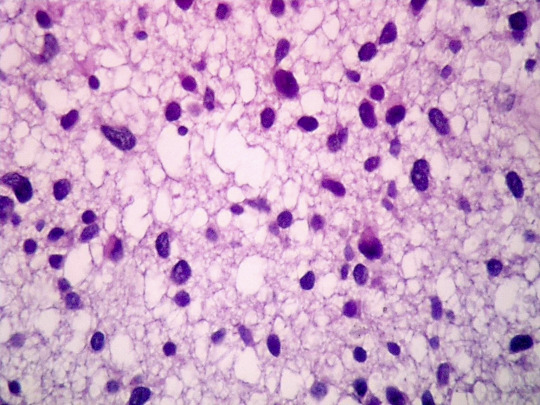
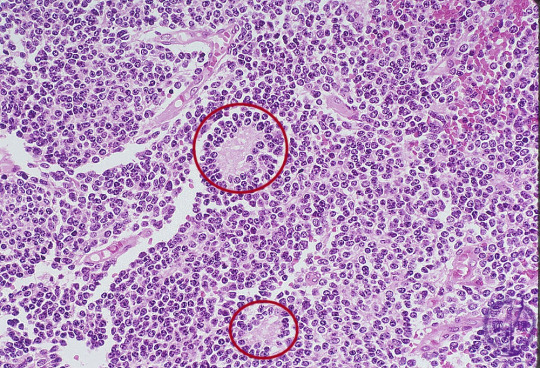
This is the most malignant brain tumor in children, and is only found in the cerebellum (by definition, obviously). All of them are WHO grade IV. The classic (aka the kind on board exams) is composed of sheets of densly packed cells with round to oval nuclei (or sometimes carrot-shaped lol), and little cytoplasm. They are poorly differentiated and primitive. In 40% of them, there are Homer-Wright (neuroblastic) rosettes (circled below).
Sometimes you see spinal drop metastasis of these, which means the tumor has spread to the spinal cord. This will show up as a "sugar coated" spinal cord on MRI. If the tumor compresses the 4th ventricle, you'll also see increased intracranial pressure.
Ependymomas
These are slow-growing tumors that originate from either the walls of the ventricles or the spinal canal. In kids, they're usually in the brain. In adults, they're usually in the spine. There are like nine subtypes, but the most common feature on histology is perivasuclar psuedorosettes. They have a poor prognosis.
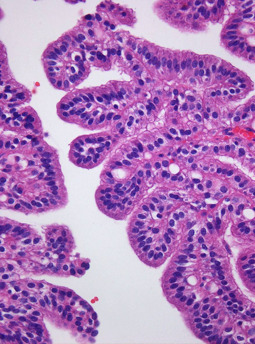
Choroid Plexus Papillomas
These come from the cuboidal cells of the choroid plexus within the ventricles (the things that make CSF). 85% are in kids less than 5 years old, and most are found in the lateral ventricles. They look like cauliflower. Under the microscope, they show papillary structure with delicate fibrovascular cores, with a cuboidal lining. Complete resection is the main treatment.
Neuronal Tumors
We're only gonna talk about gangliocytomas, gangliogliomas, and dysembryoplastic neuroepithelial tumors, but there are other types. Gangliocytomas are the most common tumors associated with chronic temporal lobe epilepsy, but they are rare overall. They show prominent single nucleoli and cytoplasmic basophilic Nissl substance. They also may have pilocytic elements. They may progress to gangliogliomas.
Dysembryoplastic neuroepithelial tumors are low-grade tumors that are seen in kids. Usually they cause seizures. You'll see multinodular lesions in the cortices (usually temporal). Histology looks like prominent clusters of oligodendroglial-like cells, which seem to float in cystic spaces. Resection is the treatment, and usually stops the seizures.
Meningiomas
These are the most common benign tumors in adults, with resection being the primary treatment (unless they're radiation-induced, those fuckers are aggressive). These are attached to the dura mater and compress the brain without invading it. The meningothelial subtype is the only one you need to know the histology of. It has characteristic whorls (can be mineralized) called psammoma bodies. Grossly, they look like an egg yolk.

Primary CNS Lymphomas
PCNSL are usually diffuse large B-call lymphomas. Therefore, they express CD markers. Grossly, they are circumscribed and somewhat necrotic. On histology, they have lymphoid-appearing cells around blood vessels. They're honestly not that interesting in my opinion.
Craniopharyngiomas
These are benign and their origin has to do with some embryology I don't care to explain here. They have neuroendocrine effects, and can usually not be reached for resection, and are therefore considered a lifelong illness. They're usually cystic, solid, and calcified all at once (yum). They are separated into adamantinomatous (kids and adults) and papillary (only in adults). You'll see palisading epithelial cells and wet keratin.

CNS Metastasis
Most common tumor of the CNS, and can occur at any age. Lung cancer is the most common primary tumor. You're going to see edema, and usually they lodge at the gray-white junction. They will be well circumcised and will have histology consistent with the primary lesion.
Peripheral Tumors
We got Schwannomas, Neurofibromas, and Malignant peripheral nerve sheath tumors (MPNSTs). Schwannomas are painless and slow rowing, and just kinda look like a round knot on a nerve. Histologically, they are biphasic, with Antoni A (tight) and Antoni B (loose) areas. You'll also see nuclear palisading with Verocay bodies.
Neurofibromas are either solitary or plexiform. They will present with pain and loss of function. On histology, you'll see myxomatous matric and collagen fibrils leading to intense staining with reticulin.
MPNSTs are highly malignant and aggressive, and are difficult to diagnose. Grossly, you'll see necrosis. Histologically, you'll see hypercellularity, atypia, and pleomorphism.
Neurocutaneous Syndromes
You got neurofibromatosis 1 and 2, tuberous sclerosis, and Von Hippel Lindau disease. With NF1, you have a mutation on chromosome 17, which causes dark skin spots, cutaneous neurofibromas, Lisch nodules on the iris, optic gliomas, seizures, etc.
NF2 is from chromosome 22, and the patient will also sometimes have meningiomas and ependymomas. The biggest thing is bilateral vestibular schwannomas, causing hearing loss, vertigo, and facial weakness. Also common are juvenile cataracts.
Tuberous sclerosis is a disorder of cellular differentiation and proliferation. You'll see ash leaf spots, facial and fingernail angiofibromas, shagreen patches, heart tumors, renal tumor, retinal tumor, lung tumor, epilepsy, etc.
Von Hippel Lindau disease is caused by a deletion on chromosome 3. It is characterized by hemangioblastomas in the retina and CNS. You'll see symptoms from local mass effect and hemorrhage. Patient may also have renal cysts, pheochromocytomas, or pancreatic tumors.
And that's all the ones I want do, I'm not interested in going neuro, so I won't get into the dirty details. They don't really matter unless you want to be a brain surgeon or something.
13 notes
·
View notes
Text
PATIENT NAME: [Redacted] DOB: [Redacted] AGE: 12 years DATE OF ADMISSION: [Redacted] REFERRING PHYSICIAN: Dr. [Redacted] ATTENDING PHYSICIAN: Dr. [Redacted] REASON FOR CONSULTATION: Traumatic Brain Injury (TBI), Memory Impairment
HISTORY OF PRESENT ILLNESS (HPI):
The patient is a 12-year-old male presenting with symptoms secondary to blunt force head trauma sustained approximately [X] days ago. According to reports, the patient was struck on the left temporoparietal region, causing rapid deceleration against a hard surface (counter edge). There was a brief loss of consciousness (~30 seconds) followed by initial confusion and disorientation upon awakening.
Since the injury, the patient has exhibited the following symptoms:
Cognitive impairment: Inconsistent recall of events, with some memories accessible at certain times but absent at others.
Disorientation: Occasionally misidentifies time and place, particularly under stress or fatigue.
Episodic dissociative states: Rare occurrences where the patient temporarily reverts to earlier behavioral and cognitive states, suggesting a memory retrieval issue rather than psychogenic dissociation.
The patient has no known history of prior neurological conditions, learning disabilities, or psychiatric disorders. No current medication use.
EXAMINATION FINDINGS:
Neurological Examination:
Mental status: Alert but intermittently confused. Inconsistent recall of recent events.
Cranial nerves: No deficits noted.
Motor function: Normal tone and reflexes. No paresis.
Gait & Coordination: Mild postural instability noted.
Speech & Language: Intact, though slightly slowed when recalling specific information.
Neuropsychological Screening:
Impaired episodic memory and executive function.
Fluctuating orientation.
Increased reliance on procedural memory over declarative recall.
Neuroimaging (CT/MRI): Findings consistent with diffuse axonal injury (DAI) localized predominantly in the left temporoparietal region, with evidence of microhemorrages in the subcortical white matter. Minor hippocampal atrophy observed, which may contribute to episodic memory dysfunction and fragmented recall.
IMPRESSION:
The patient sustained a moderate traumatic brain injury (TBI) with clinical findings suggestive of:
Post-Traumatic Amnesia (PTA): Resulting in episodic memory deficits and inconsistent recall.
Post-Concussive Syndrome (PCS): Persistent cognitive disturbances, particularly affecting memory retrieval and orientation.
Possible Retrograde Memory Fragmentation: Periodic retrieval of older memories without full contextual awareness, leading to brief reversions to earlier cognitive states.
RECOMMENDATIONS:
Neurological follow-up: Repeat MRI in 6 months to assess for structural changes.
Cognitive rehabilitation therapy: To improve memory recall and adaptive strategies.
Behavioral assessment: To monitor potential cognitive shifts or further dissociative-like episodes.
Caregiver education: Close observation for worsening cognitive deficits, confusion, or personality changes.
PROGNOSIS & EXPECTED OUTCOME:
The patient’s neurological prognosis is cautiously optimistic. While some memory inconsistencies may improve over time, the presence of hippocampal involvement suggests that episodic memory deficits and occasional cognitive reversion may persist. Memory retrieval may remain context-dependent, with certain recollections accessible only under specific circumstances. Long-term cognitive adaptation is expected, but periodic assessments are recommended to monitor progression.
18 notes
·
View notes
Text
hi everyone :)
i’m a neuroimaging phd student studying in the uk. i’m looking at diffusion mri and how it can be used in assessing paediatric epilepsy. i’m originally from johannebsurg, south africa.
i’m starting a studyblr to post my progress and keep myself accountable. i also want to record the journey, because it’s an important part of my life.
do drop a message and say hi!
#studyblr#study motivation#phd#phdblr#phd life#study blog#studyfulltime#studyspo#study aesthetic#studyinspo#study notes#100 days of productivity
49 notes
·
View notes
Text
University of Florida develops AI-powered MRI tool to improve Parkinson’s diagnosis

- By InnoNurse Staff -
University of Florida researchers have developed Automated Imaging Differentiation for Parkinsonism (AIDP), a machine-learning method using MRI to accurately distinguish Parkinson’s disease (PD) from atypical parkinsonian disorders such as multiple system atrophy (MSA) and progressive supranuclear palsy (PSP).
In a multicenter study involving 249 prospective and 396 retrospective cases, AIDP analyzed diffusion MRI data from 132 brain regions, achieving 96–98% accuracy in differentiating PD, MSA, and PSP.
Compared to traditional clinical methods, AIDP improved diagnostic accuracy by 12.3%, reaching 93.9% accuracy against autopsy-confirmed cases.
Its non-invasive, scalable approach could enhance clinical care and complement existing biomarkers.

Image: Automated Imaging Differentiation for Parkinsonism (AIDP) for the precise classification of parkinsonism subtypes. Credit: JAMA Neurology (2025). DOI: 10.1001/jamaneurol.2025.0112.
Read more at Tech Xplore
///
Other recent news and insights
Researchers urge reproductive health apps to enhance data protection for users (CUNY SPH)
Polish healthtech company Jutro Medical secures €12M to develop its telehealth platform (Tech.EU)
2 notes
·
View notes
Text
Primary dural-based parafalcine diffuse large b-cell lymphoma mimicking meningioma by Amr El Mohamad in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
Background: Primary dural-based diffuse large B-cell lymphoma is very rare. Only few cases were reported in the literature. Case presentation: Herein, we present a case of an immunocompetent patient with primary dural-based diffuse large B-cell lymphomas mimicking meningioma associated with ghost tumor phenomenon without any evidence of a systemic lymphoma. Conclusion: Primary central nervous system lymphomas are rare. Clinicians should always consider this lesion as a differential diagnosis if radiological findings are not indicative of typical one meningiomas.
Key words: Dural-based tumor, diffuse large B-cell lymphoma, ghost tumor, MATRIX regimen, central nervous system.
Introduction
Primary central nervous system lymphomas (CNSLs) (PCNSLs) are rare and account for 2%–5% of all brain tumor cases, whereas secondary CNSLs are more common [1,2]. One study has shown that the most common intraparenchymal histological type is diffuse large B-cell lymphoma, as among 26 patients with PCNSL, 25 had diffuse large B-cell lymphoma [3]. Although primary dural-based lymphomas are rare, the most common area of involvement is the cerebral hemispheres. Most dural-based lymphomas are secondary and present as extra-nodal systemic diffuse large B-cell lymphomas. Primary dural-based lymphomas are usually histologically marginal-zone lymphomas, representing a group of lymphomas that have been historically classified together because they appear to arise from post-germinal center and marginal-zone B cells and share a similar immunophenotype, and few cases were reported to be diffuse large B lymphomas [4]. Here, we present a case of an immunocompetent patient with primary dural-based diffuse large B-cell lymphomas mimicking meningioma associated with ghost tumor phenomenon without any evidence of systemic disease.
Case Presentation
A 58-year-old male individual previously healthy and immunocompetent presented with headache, recurrent vomiting, and memory problems lasting for 3 days. No loss of consciousness, seizure, subjective weakness, or fever was observed. On physical examination, the patient’s Glasgow coma scale score was 15; his pupils were 3 mm in diameter, equal, and reactive; and the patient had nominal aphasia without motor and sensory deficit. He had normal cerebellar functions, and cranial nerve exams revealed no deficit. Head computed tomography (CT) (Fig. 1) showed a 2.2 × 3.8 cm (transverse × anteroposterior) iso-dense lesion with internal hypodensity in the left parasagittal frontal region extending to the right frontal region. Extensive perilesional edema was observed with effacement of the sulci and mass effect on bilateral frontal horns, associated with 3-mm midline shift. Head magnetic resonance imaging (MRI) showed an isointense parasagittal lesion on T1 and heterogeneous intense on T2, with redemonstration of perifocal edema (Fig. 2). Head T1-weighted imaging with contrast enhancement (Fig. 3) showed a large, left frontal, parafalcine, irregular-shaped mass located below the superior sagittal sinus level. It measured 4 × 3 × 3.3 cm in anteroposterior, mediolateral, and craniocaudal, respectively. It showed diffusion restriction (Fig. 4). There was central hyperintensity on T2-weighted imaging, without post-contrast enhancement area representing cyst formation. It exerts a mass effect characterized by effacement of the adjacent sulci, compression of the left lateral ventricle, and a 3-mm shift of the midline structures to the right side, and the impression of our neuroradiologist was atypical meningioma. Regarding extensive edema, dexamethasone was started at a dose of 4 mg, thrice a day, and the patient was planned for craniotomy and resection of the tumor. Initially, the patient was reluctant to undergo surgery; however, subsequently, the patient agreed to undergo surgery after approximately 10 days. During surgery, parasagittal craniotomy was performed; however, to our surprise, no definite mass lesion was found at the proposed site, in contrast to the findings described on imaging. The falx was thinned out and partly deficient. A biopsy sample was obtained from this abnormally appearing falx. Moreover, we obtained biopsy samples under neuronavigation guidance from abnormally appearing tissue, which was completely intra-axial, deep down in the lesion visualized on navigation. On postoperative day 1, MRI head with contrast enhancement (Fig. 5) showed that the previously seen lesion had a significant regression in size. Its right frontal extension and adjacent enhanced meningeal tail showed size reduction. Moreover, some regression in the perilesional vasogenic edema was observed. A significant regression in the previously described enhancement was noted at the left-side lentiform nucleus and external capsule. The MR spectroscopy study showed an increased choline/N-acetyl aspartate ratio and elevated lactate level within the lesion.
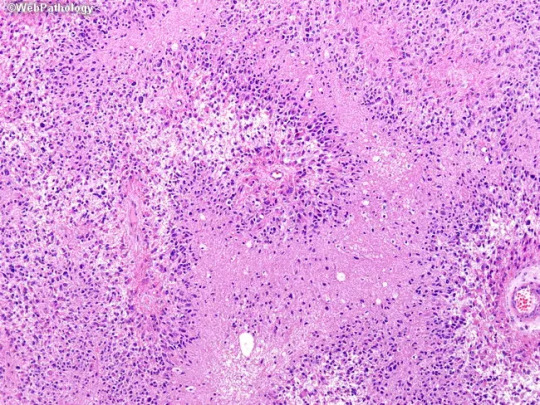
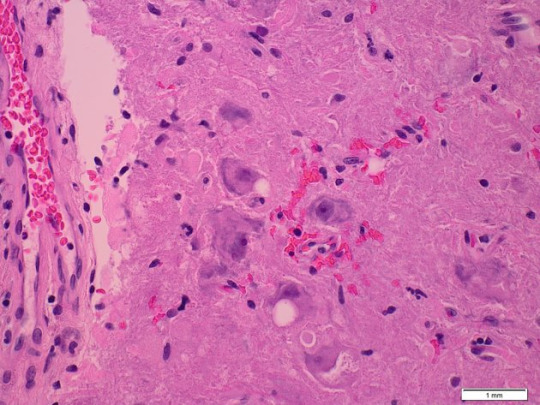
The histopathology results of the first brain biopsy samples (Figs.6–7) obtained from the falx cerebri showed meningothelial hyperplasia with calcification and focal perivascular lymphocytic infiltrate composed of small and large, atypical lymphocytes. Immunohistochemical staining was performed; however, the area of interest disappeared. The pathology team recommended another fresh biopsy to have the final diagnosis and flowmetry studies. So, the patient underwent redo craniotomy using the same incision, and multiple biopsy samples were taken. The second fresh brain biopsy (Figs. 8–9) showed multiple brain fragments with predominant perivascular atypical lymphoid infiltrates. Most cells were medium to large with moderate cytoplasm, atypical irregular nuclei having vesicular chromatin, variably prominent nucleoli, and several mitoses, including atypical one. Necrotic areas were also seen. Immunohistochemistry of the second biopsy (Fig.10 A-D) showed that atypical perivascular cells were positive for CD45, CD20, CD79a, BCl2, BCl6, MUM1, OCT2, and C-MYC, and negative for CD10, CD21, TDT, ALK1, EBV-LMP1, CD3, and CD5; however, few reactive/residual lymphocytes were positive for these enzymes. Moreover, 80% of lymphoid cellular nuclei were positive for Ki67. These findings were consistent with diffuse large B-cell lymphoma, not otherwise specified.
Whole-body positron emission tomography (PET) showed intense fluorodeoxyglucose (FDG) uptake higher than that in the healthy brain cortex, without evidence of coexisting systemic disease. In addition to PET scan, contrast-enhanced chest, abdomen, pelvis CT did not show any other lesions in the body; furthermore, workup for viral markers and autoimmune conditions were all unremarkable, thus confirming the diagnosis of “primary dural-based diffuse large B-cell lymphoma,” distinguishing it from secondary CNSL. The patient was transferred to the Oncology Department and started on three cycles of the methotrexate, cytarabine, thiotepa, and rituximab (MATRIX) protocol, which is the current standard treatment regimen for PCNSLs [5]. Three months after the diagnosis and after receiving two cycles of the MATRIX protocol, brain MRI with contrast enhancement (Fig. 11A, B) showed regression of the lesion, and PET scan showed complete metabolic resolution in terms of decreased FDG activity of the previously seen PCNSL without signs of lymphoma activity elsewhere. Subsequently, the patient received the third cycle of the MATRIX protocol without specific complications. Two weeks later, autologous stem cell transplantation (50 × 106/kg) was performed as part of the consolidation phase of treatment. Six weeks later, conditioning chemotherapy with carmustine–thiotepa was administered, followed by stem cell infusion (CD34 = 12 million/kg). The post-transplant course was complicated with mucositis, folliculitis, diarrhea, febrile neutropenia, and prolonged thrombocytopenia. Two months after transplantation, PET scan was repeated and showed complete metabolic resolution of initially seen PCNSL involvement. Currently, the patient is being followed by the hematology team; the patient is in good health and remission. The last outpatient follow-up was 8 months after the first surgery. The patient was seen by the vascular surgery (for permcath removal) and oncology teams. At this time, the patient was stable with complete remission; then, the patient was lost to follow-up. Another head MRI was performed and showed almost total regression of the lesion.
Discussion
Lymphomas in CNS are classified as primary, arising de novo from brain parenchyma, leptomeninges, eye, and spinal cord and as secondary to systemic lymphoma, which can be dural-based lesions. Secondary CNSLs are more common than PCNSLs. Most PCNSLs are intraparenchymal diffuse large B-cell lymphomas with a predilection to occur in the frontal lobe and then deep nucleic and periventricular locations; the infratentorial cerebellum is the most common location. However, primary dural-based lymphomas are rare, and even when found, they are histologically marginal-zone lymphomas. Few cases of primary dural-based diffuse large B-cell lymphoma have been reported in the literature [4,6]. Furthermore, PCNSLs are more common in immunocompromised patients with a mean age of 34 years, and they occur in immunocompetent individuals at an older age with a mean of 52 years [7]. The patient in this case report was 58 years old and immunocompetent without significant previous medical conditions. The latest review of the literature on primary dural-based lymphoma has been conducted by Quinn et al., who have found only 24 reported cases of primary dural-based diffuse large B-cell lymphoma, which confirms the rarity of the disease and subsequently the limited knowledge regarding this disease entity [8]. CNSLs have rapid response to steroids with shrinkage in size and initial remission [9]. Moreover, the initial response to steroids is associated with a better response to chemoradiotherapy and good prognosis [9]. In the patient in this case report, there was an unintentional delay of surgery for approximately 10 days, and the patient was on steroids (dexamethasone). In this case report, the failure to identify a discrete lesion of the size expected as perceived on initial imaging, despite proper surgical planning using neuronavigation, was probably due to the rapid regression of the tumor in response to steroids. This phenomenon agrees with the scientific literature reporting about the disappearance of lymphomas in response to steroids (ghost tumors) [10,11]. The pathogenesis of primary dural-based lymphoma remains unknown as there is no lymphoid tissue in the dura. It is hypothesized that it is related to chronic infection, autoimmune disease, or chronic inflammatory condition, which recruits polyclonal lymphocytes resulting in monoclonal lymphomas [6]. In contrast, the patient in this case report did not have any chronic conditions. All workups were negative, including the entire viral panel and autoimmune markers. Basic research is needed to determine the etiology of PCNSL, especially dural-based lymphomas. In the patient in this case report, the initial radiological findings were mimicking those of a meningioma: dural-based and uniformly enhanced. There was significant surrounding edema, significant diffusion restriction, and blooming in susceptibility-weighted image, which goes more with higher-grade meningioma or another high-grade lesion. One review has shown that primary dural-based lymphomas can display the “dural tail “sign, further confusing the preoperative diagnosis with meningioma [12], which did happen in the patient in this case report. Therefore, we suggest that in case of a dural-based lesion that has non-typical features of grade 1 meningioma, clinicians should consider lymphoma in the differential diagnosis and avoid steroids unless necessary due to edema and mass effect keeping in mind the ghost tumor phenomena of lymphoma.
The role of surgery in PCNSLs is limited mainly to histological diagnosis through biopsy or tumor debulking in case of increased intracranial pressure or impending brain herniation. Some studies have shown no benefit of complete surgical resection of PCNSLs; however, a recent systematic review of 244 articles has shown evidence in support of cytoreductive surgery [13]. Previously, whole-brain radiotherapy (WBRT) was the recommended treatment; however, this treatment modality resulted in a high rate of relapse and a decrease in performance status and cognitive impairment, and with the improvement in survival with high-dose methotrexate, WBRT is no longer recommended. Currently, newly diagnosed PCNSLs are initially treated with induction chemotherapy until complete radiological response, followed by consolidation therapy, to prolong the overall survival [14]. The International Extra Nodal Lymphoma Study Group-32 trial has shown that a methotrexate-based MATRIX regimen results in a good outcome and control rate in PCNSL [5], and it is the standard induction chemotherapy. Ferreri AJM, in his article “The role of autologous stem cell transplantation in PCNSL” has compared various consolidation phase treatment modalities, including beam radiation, carmustine–thiotepa regimens, and autologous stem cell transplantation, and the results showed that autologous stem cell transplantation resulted in good outcomes [15]. The patient in this case report showed a good response to treatment with almost total resolution of PCNSL with three cycles of MATRIX chemotherapy, followed by conditioning chemotherapy with stem cell infusion.
Conclusion
PCNSL is a rare entity. Clinicians should always consider it in differential diagnosis of meningioma if the radiological findings are not typical for meningioma. When there is a high index of suspicion of lymphoma, repeating neuroimaging, particularly MRI, before surgery, especially if the surgery is delayed while the patient is on steroids, may help develop a better management plan while dealing with this rare lesion. In case of lesion disappearance, falx biopsy can be an option. The aim of surgery in PCNSL is mainly biopsy or debulking to decrease intracranial pressure in case of significant mass effect.
List of abbreviation:
Primary central nervous system lymphomas (PCNSLs)
Central nervous system lymphomas (CNSLs)
Head computed tomography (CT)
magnetic resonance imaging (MRI)
positron emission tomography (PET)
fluorodeoxyglucose (FDG)
whole-brain radiotherapy (WBRT)
#Dural-based tumor#diffuse large B-cell lymphoma#ghost tumor#MATRIX regimen#central nervous system#jcrmhs#Clinical decision making#Is Journal of Clinical Case Reports Medical Images and Health Sciences PubMed indexed
2 notes
·
View notes
Text
Incantation [咒] (2022)
Talk about a kitchen sink approach to found footage horror. We get a little bit of everything in this tale of shared loss and familial tragedy. Spooky possessed kids, sad suffering kids, creepy arms, folk horror imagery, consults with experts, meta elements… the lot of it. As the narrative unspools its nonlinear tale, we are drawn into a web of spiritual intrigue as Ronan tries to save her daughter Dodo, whom she has recently retrieved from foster care after being discharged from psychiatric treatment. What exactly provoked the need for that treatment is carrot-on-a-sticked along, teased and hinted at, until the movie is finally ready for a big reveal. As is common for this sort of movie, Incantation uses a variety of different forms of recording to tell its story: handheld camcorders serve as the heavy lifters, but we also get MRI scans, security camera footage, and the dreaded iPhone vertical video. There’s just one problem: how do they have so many damn angles? The question of “why are they still recording” often plagues these movies, but more importantly here, how can a scene that’s established to have only one person with a camera in it still have at least two perspectives? This murkiness happens frequently enough that it raises the question as to why this was found footage format to begin with and not simply a conventional horror movie. There’s enough here to deal with: Rohan’s conflicted relationship to motherhood, the intricacies of the ancestral rituals performed by the family, that the gimmick wasn’t really needed. Aside from some well-constructed scares along the way, it seems to feed almost solely to build up to the final twist, diffusing the curse out into every viewer in a gambit to save Dodo.
THE RULES
SIP
Dodo says 'baddie'.
Direct camera address.
Time jump!
A caterpillar appears onscreen.
BIG DRINK
The curse symbol appears.
Mom crimes.
Someone is painted up Kwaidan style.
#drinking games#incantation#zhòu#horror#horror & thriller#taiwanese cinema#kevin ko#found footage horror#found footage
2 notes
·
View notes
Text
Interesting Reviews for Week 26, 2023
All the brain’s a stage for serotonin: the forgotten story of serotonin diffusion across cell membranes. Andrews, P. W., Bosyj, C., Brenton, L., Green, L., Gasser, P. J., Lowry, C. A., & Pickel, V. M. (2022). Proceedings of the Royal Society B: Biological Sciences, 289(1986).
Imagination as a fundamental function of the hippocampus. Comrie, A. E., Frank, L. M., & Kay, K. (2022). Philosophical Transactions of the Royal Society B: Biological Sciences, 377(1866).
How reliable are amygdala findings in psychopathy? A systematic review of MRI studies. Deming, P., Heilicher, M., & Koenigs, M. (2022). Neuroscience & Biobehavioral Reviews, 142, 104875.
The role of aberrant neural oscillations in the hippocampal-medial prefrontal cortex circuit in neurodevelopmental and neurological disorders. Shing, N., Walker, M. C., & Chang, P. (2022). Neurobiology of Learning and Memory, 195, 107683.
#science#Neuroscience#computational neuroscience#Brain science#research#reviews#scientific publications#cognition
3 notes
·
View notes
Text
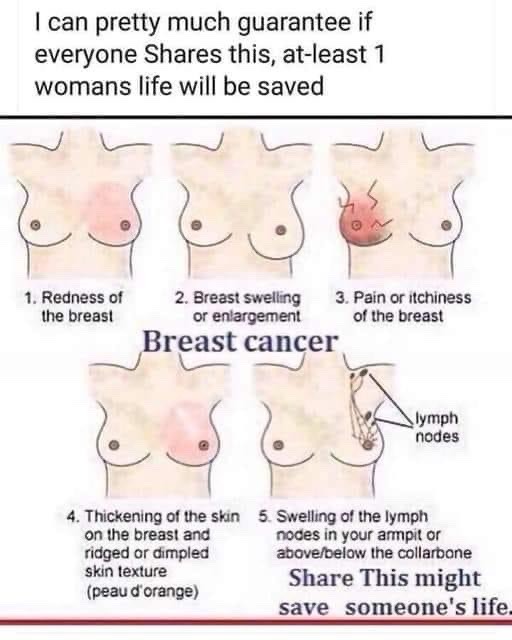
Reblogging to save a life.
Here's a little personal story. 16 years ago I had an 8-month old, was breast feeding (so boobs were a mess) and was dealing with helping my Mum out after Dad died. Part of that helping out involved hauling coal out of the coal bunker every evening - as I leaned over the metal edge of the bunker, night after night I noticed a sore spot. I thought it was just a bruise but I fiddled with it, obsessively, until I was able to get home six weeks later and go see my obgyn. She sent me for a mammogram. I had a <1cm tumour. I had to emergency wean the wean (a reference only my fellow Scots will get) and then had a lumpectomy, a lymphectomy and a course of radiation. All has been well since, but I get checked out twice a year (mammogram and MRI). At the beginning of February they noticed a diffuse calcification at the old tumour site. It is officially Stage 0 and I will be having a bilateral mastectomy within the next few weeks. The chances of recurrence are virtually zero.
The moral of this story is - check your boobs regularly and if you have ANY doubt at all about an irregularity, get it checked out. If you catch it in time, the chances are you will be just fine.
And yes, this post acknowledges the inherent privilege in having half way decent medical coverage if you are in the US.
98K notes
·
View notes
Text
Reference Archived on our website
Introduction: There is a growing interest in the effect of Long-COVID (LC) on cognition, and neuroimaging allows us to gain insight into the structural and functional changes underlying cognitive impairment in LC. We used multimodal neuroimaging data in combination with neuropsychological evaluations to study cognitive complaints in a cohort of LC patients with mild to moderate severity symptoms.
Methods: We conducted a 3T brain magnetic resonance imaging (MRI) study with diffusion tensor imaging (DTI) and functional MRI (fMRI) sequences on 53 LC patients 1.8 years after acute COVID-19 onset. We administered neuropsychological tests to evaluate cognitive domains and examined correlations with Tract-Based Spatial Statistics (TBSS) and resting state.
Results: We included 53 participants with LC (mean age, 48.23 years; 88.7% females). According to the Frascati criteria, more than half of the participants had deficits in the executive (59%) and attentional (55%) domains, while 40% had impairments in the memory domain. Only one participant (1.89%) showed problems in the visuospatial and visuoconstructive domain. We observed that increased radial diffusivity in different white matter tracts was negatively correlated with the memory domain. Our results showed that higher resting state activity in the fronto-parietal network was associated with lower memory performance. Moreover, we detected increased functional connectivity among the bilateral hippocampus, the right hippocampus and the left amygdala, and the right hippocampus and the left middle temporal gyrus. These connectivity patterns were inversely related to memory and did not survive false discovery rate (FDR) correction.
Discussion: People with LC exhibit cognitive impairments linked to long-lasting changes in brain structure and function, which justify the cognitive alterations detected.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#long covid#covid conscious#covid is airborne
14 notes
·
View notes
Text
Head injury Treatment in India | Dr. Vikas Kathuria
Comprehensive Guide to Head Injury Treatment in Gurgaon
Head injuries can occur in the blink of an eye—whether from road accidents, falls, sports, or workplace mishaps. While some may appear minor at first glance, others can have life-threatening consequences. Timely and expert head injury treatment is crucial to ensure full recovery and to prevent long-term complications.
If you're searching for the best care in Gurgaon, Skin Aura Hair Transplant, Brain and Spine Neuro Centre offers world-class neuro care services led by highly qualified specialists. This blog will walk you through the causes, symptoms, and the best approach to head injury treatment in Gurgaon.
What Is a Head Injury?
A head injury refers to any trauma to the scalp, skull, or brain. It can range from a mild bump or bruise to a serious traumatic brain injury (TBI). The impact can be open (with a visible wound) or closed (with no break in the skull), but both types can be dangerous.
Common types of head injuries include:
Concussions
Skull fractures
Intracranial hematomas (bleeding in the brain)
Contusions (bruising of brain tissue)
Diffuse axonal injury (severe brain trauma due to shaking or rotation)
Causes of Head Injuries
Head injuries are alarmingly common and can result from:
Road traffic accidents (a leading cause in urban areas like Gurgaon)
Falls, especially in children and elderly people
Physical assaults or violence
Sports injuries
Industrial or construction site mishaps
Each of these scenarios requires a different approach to head injury treatment, which should always be handled by trained professionals.
Symptoms That Demand Immediate Medical Attention
It’s important to recognize the warning signs of a serious head injury. Seek urgent medical care if any of the following symptoms are present:
Loss of consciousness (even briefly)
Persistent headache or increasing pain
Vomiting or nausea
Confusion, dizziness, or disorientation
Slurred speech or difficulty speaking
Seizures
Fluid leakage from nose or ears
Unequal pupil size
Weakness or numbness in limbs
Memory loss or changes in behavior
Ignoring these symptoms can worsen the condition and may lead to permanent damage or even death.
Why Choose Skin Aura Hair Transplant, Brain and Spine Neuro Centre for Head Injury Treatment?
At Skin Aura Hair Transplant, Brain and Spine Neuro Centre in Gurgaon, patients receive advanced and compassionate care for all types of neurological trauma. Here's why this center stands out:
1. Experienced Neurosurgeons and Specialists
Led by top-tier neurosurgeons, the clinic has a dedicated team experienced in handling emergency and critical neurological cases. They use evidence-based protocols and individualized treatment plans to ensure optimal recovery.
2. Advanced Diagnostic Tools
Proper head injury treatment starts with accurate diagnosis. The clinic is equipped with advanced imaging tools like CT scans, MRIs, and digital X-rays to assess the extent of damage quickly and precisely.
3. 24/7 Emergency Services
Head injuries are unpredictable and time-sensitive. The center offers round-the-clock emergency services to handle urgent cases without delay.
4. Comprehensive Rehabilitation
Recovery doesn’t end with surgery or medication. The clinic provides holistic rehabilitation, including physiotherapy, occupational therapy, and counseling, to support full recovery after a head injury.
5. Patient-Centered Approach
Each patient is unique. The team at Skin Aura Brain and Spine Centre prioritizes patient comfort and well-being, making the entire treatment journey as stress-free as possible for both the patient and their family.
Step-by-Step Process of Head Injury Treatment
Understanding what happens after a head injury can ease anxiety and encourage prompt action. Here’s what to expect during head injury treatment at the center:
Step 1: Emergency Stabilization
The first priority is to stabilize the patient’s vital signs—breathing, heartbeat, and consciousness level. If the injury is severe, life-saving interventions are initiated immediately.
Step 2: Diagnostic Evaluation
A thorough neurological exam is performed. Imaging scans like CT or MRI help identify fractures, bleeding, swelling, or brain damage.
Step 3: Treatment Plan
Depending on the diagnosis, treatment may include:
Observation and monitoring (for mild cases)
Medication to reduce swelling or prevent seizures
Surgery to remove clots, repair skull fractures, or relieve pressure
Step 4: Post-Treatment Monitoring
After treatment, patients are closely monitored in the ICU or neuro ward. Any changes in behavior or vital signs are addressed promptly.
Step 5: Rehabilitation and Follow-Up
Rehabilitation may include physical therapy, speech therapy, and psychological support. Follow-up appointments ensure recovery is on track and prevent complications.
Long-Term Effects of Untreated Head Injuries
Delaying or avoiding proper head injury treatment can lead to:
Memory problems
Personality changes
Depression and anxiety
Seizures
Motor function impairment
Loss of speech or vision
Permanent disability or death
This is why it’s critical to get expert care from a reputed center like Skin Aura Brain and Spine Neuro Centre in Gurgaon, where every step is managed with clinical precision and care.

Tips to Prevent Head Injuries
While accidents aren’t always avoidable, here are some precautions:
Always wear helmets while riding two-wheelers or during sports
Use seat belts in cars and follow traffic rules
Make your home fall-proof, especially for elderly family members
Use proper safety gear at work
Supervise children during risky activities
Final Thoughts
A head injury is never something to take lightly. Whether it's a small fall or a major accident, timely diagnosis and expert care are the keys to a successful recovery. If you or a loved one ever needs head injury treatment in Gurgaon, trust the dedicated team at Skin Aura Hair Transplant, Brain and Spine Neuro Centre.
Their specialized care, advanced technology, and commitment to patient health make them a trusted name in neurological treatment across the region. Don’t wait for symptoms to worsen—early intervention can save lives.
For consultations or emergency care, contact Skin Aura Brain and Spine Centre today and take the first step toward healing and recovery.
0 notes
Text
The Science Behind Organic Essential Oil Blends: Why Purity Matters
I still remember the first time I brought a diffuser home after a nail-biting week at work. I had ordered a couple of Essential Oil Blends Online, eager to see whether all the hype about “true purity” was real or just good marketing. One deep, eucalyptus-mint breath later, I felt like my shoulders had slid down from my ears to where they belong. That pleasant surprise kicked off my quest to understand what exactly makes organic essential oil blends so special—and why purity genuinely matters.
I Start With the Plant, Not the Bottle
When I shop for Essential Oil Blends Online, I always check where the plants were grown. Organically farmed lavender, for example, is cultivated without synthetic pesticides or herbicides. That matters because aromatic compounds are “lipophilic”—they love to bind to oils and fats. If any chemical residues cling to the plant, they can hitchhike right into the finished oil. Keeping the crop chemical-free from seed to seal means I’m inhaling the plant’s own therapeutic molecules—not a cocktail of extras I didn’t sign up for.
Steam, Pressure, and Tiny Molecules
Most of the blends I purchase are produced through steam distillation. In this method, pressurized steam ruptures plant cell walls, releasing volatile molecules like linalool (calming) or 1,8-cineole (clearing). Because these compounds are fragile, even slight contamination or over-heating can distort their natural chemical profile. Certified organic producers must follow strict temperature and pressure guidelines, preserving the exact mix that nature designed. When I compare lab reports for organic and non-organic oils, the organic batch almost always shows a cleaner chromatogram—science-speak for “nothing extra hiding in there.”
Why “Synergy” Isn’t Just Buzzword Bingo
Blending oils isn’t as simple as splashing equal parts into a bottle. Each compound in a blend can amplify or buffer its neighbors. Think of it like a symphony: one violin is lovely, but an entire string section gives me goosebumps. Purity ensures that each “instrument” in the blend plays its intended note. When I diffuse a certified-organic Stress-Away blend, for instance, the limonene from sweet orange sharpens my focus while the chamomile’s bisabolol calms my nerves—no synthetic off-notes muddying the harmony.
The Nose-to-Brain Express Lane
Inhaling essential oils fast-tracks active molecules to my limbic system—the brain’s emotional command center. Research using functional MRI shows that compounds such as menthol or linalyl acetate can alter neural activity within seconds. If those molecules arrive tainted with impurities, my body still absorbs them; I’m just not getting the clean therapeutic signal I paid for. Pure, organic blends give my gray matter the undiluted message to relax, uplift, or energize—whatever I need in that moment.
Safety First, Especially for Daily Users
Because I lean on aromatherapy every single day, cumulative exposure matters. Repeated inhalation of minute pesticide residues might not cause an immediate disaster, but over months or years it can tax my liver’s detox pathways. By sticking with organic Essential Oil Blends Online, I simply remove that variable from the equation. It’s one less layer of stress—exactly what I’m trying to avoid in the first place.
How I Vet My Bottles Before They Hit the Cart
Third-Party Testing I look for GC/MS (gas chromatography/mass spectrometry) reports posted right on the retailer’s product page.
Clear Lot Numbers Traceability means I can track a bottle back to its harvest date and farm.
Transparent Sourcing Stories Brands eager to show me photos of their distilleries and fields usually have nothing to hide.
Organic Certification Seals USDA, ACO (in Australia), or ECOCERT logos are my quick visual cues.
The Bottom Line for Fellow Stress-Prone Professionals
Investing in pure, organic essential oil blends isn’t just greenwashing; it’s grounded in chemistry, physiology, and long-term wellness. When I unwind after a marathon of Zoom calls, I want every inhalation to count. That’s why I keep ordering my Essential Oil Blends Online from companies that treat purity like a promise.
So the next time you spot two similar-looking bottles but one costs a few dollars more, ask yourself: “Is my peace of mind worth the upgrade?” I already know my answer—my diffuser is humming beside me as I type this.
0 notes