#tmd network effect
Text
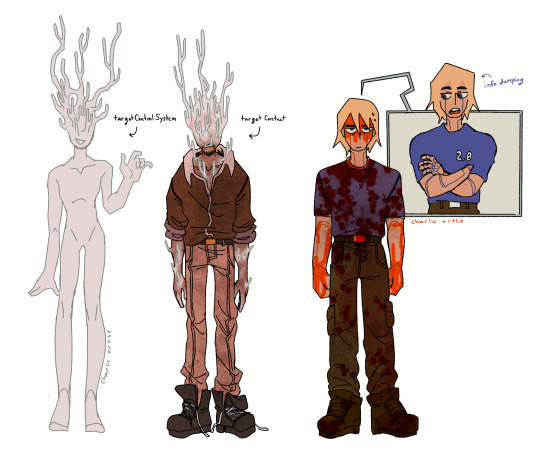
the besties from network effect <3
#the murderbot diaries#murderbot#murderbot 2.0#tmd network effect#targetcontrolsystem#targetcontact#book tags are hard#cant believe there isn’t already a dedicated tag for targetcontrolsystem my favorite character#body horror#slight but just in case#arts#this isn’t technically an au drawing#im just trying to get their designs down#also sorry in advance for drawing tcs Like That
242 notes
·
View notes
Text
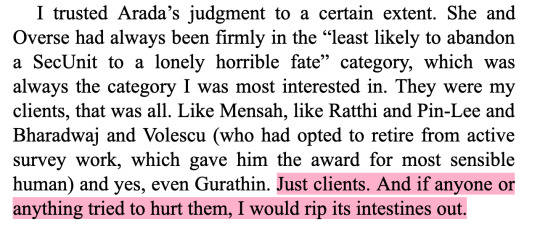
murderbot + friendship




299 notes
·
View notes
Text

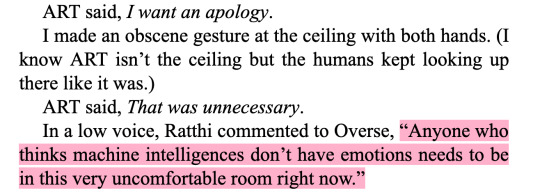
One of the first Murderbot fanarts I started working on.... Took me ages to finish because backgrounds are the bane of my existence lmao.
#fanart#the murderbot diaries#murderbot#murderbot diaries#SecUnit#art (asshole research transport)#asshole research transport#network effect#tmbd#tmd#glad it took me ages to finish because i really didn't like the face i had originally drawn lmao#i was able to update it tho and i love it now
443 notes
·
View notes
Text
The repeated core narratives of the Murderbot series are so fucking funny if you line them up btw
PresAux team: friendship? :)
Murderbot: what the fuck *flees*
ART: friend ship? :)
Murderbot: what the fuck
Miki: friendship? :)
Murderbot: no wtf why does this keep happening Unlovable I’m Unlovable!!!!!
PresAux humans: Murderbot u fucked up
Murderbot: oh shit I CARE
(Interlude where humans think about how much they love their friend the Murderbot)
Targets: ahaha we killed the Friend Ship!
Murderbot:
Murderbot: *rampage*
Targets: o SHIT
Murderbot: Indah thinks I suck, joke’s on her because I do but also I’m great.
Indah: I don’t think you suck I think you’re a valuable member of this team.
Murderbot: whAT
#murderbot#network effect spoiler warn#elk text#23rd#November#2022#November 23rd 2022#the murderbot diaries#secunit#tmd#aka the construct who was so bad at friendship that it went on a galaxy/ies-spanning tour#to avoid being loved#and incidentally made like 500% as many people love it by doing so
2K notes
·
View notes
Text
you know what I'm just posting the results:
How to make the Murderbot Diaries less casually transphobic 2: no explanations of the bigotry just the solutions.
___
Prequel: The Future of Work: Compulsory
Words added: 150.
(You can read this short story here. Archived version here. Just the text can be found on a tumblr post here. Be warned that the first two links have eye-straining neon art at the top that moves, which is why I made the tumblr post.)
Asa took her arm gently. “They can’t talk,” he told her.
She shook her head as her friends steered her toward the access bridge. “No, it talked. I heard it.”
That still came as a pleasant surprise every time it happened.
The Company had assigned me different pronouns when I was constructed, and I’d always hated them. And I hated the gender they’d assigned me, too. So the second thing I’d done after hacking my governer module (the first was downloading media) was hack into the Company’s systems to change my pronoun and gender assignments.
Now, my pronouns were listed as it/its/itself, and my gender was listed as “indeterminate”. None of the humans got paid enough to bother memorizing our assigned pronouns or genders, so none of them had noticed the change. And every time they rented me out, the humans doing the renting got a copy of my relevant info, including my assigned gender and pronouns.
Maybe someday the euphoria of being referred to the way I enjoyed would dissipate, but apparently that day was not today.
___
Book one: All Systems Red
Words added: 79
Then Mensah said quietly, “SecUnit, do you have a name? Pronouns you would prefer?”
"My pronouns are what was listed on my contract when you rented me.“ I said, "It, its, itself.”
I didn’t explain how I’d gotten those pronouns. They didn’t need to know that I’d hacked into the Company’s system to overwrite the ones I’d originally been assigned. I’d changed my gender assignment at the same time. And they didn’t need to know that either. I didn’t want them to know that.
As for having a name, I wasn’t sure what she wanted. “No.”
___
Book two: Artificial Condition
Words added: 22
They had listed themselves as unaffiliated guest workers, but you could list yourself as anything, there was no identity check. Two had listed their gender as female, and they both used she/her/hers/herself pronouns. The other one had listed ter gender as tercera, which was a gender signifier used in the group of non-corporate political entities known as the Divarti Cluster. Ter pronouns were te/ter/ter/terself.
(To initiate the meeting, I’d had to make an entry on the social feed, too. The system was extremely vulnerable to hacking, so I had backdated my entry to look like I had come in on an earlier passenger transport, listed my job as “security consultant,” my pronouns as “it/its/itself”, which was the format humans used, and listed my gender as “indeterminate”. Posing as its own captain, ART gave me a prior employment reference.)
___
Book three: Rogue Protocol
Words added: 135
Her gaze went to Wilken’s back again, but on our private channel she said, ::I’ve never worked with a SecUnit before—I’ve never seen or interacted with a SecUnit before—so please tell me if you need any information or instruction from me. I know you already know my name, but I’m going to introduce myself properly anyways. My name is Don Abene, and my pronouns are she/her/hers/herself. You can call me Abene if you’d like. Do you have a name, or designation? What pronouns would you prefer?::
While I’d had several humans now ask me for my name and pronouns, I had never had a human ask me how to give me orders before. It was an interesting novelty. ::I have standing orders from Rin to assist you. I can do the rest.:: I said, answering the first part of her question, as for the second half… ::It is best if you refer to me as SecUnit, and my pronouns are it/its/itself.:: It wasn’t technically lying, since she’d asked ‘do you have a name’, not ‘what is your name’.
Not that it would matter if I was lying, anyways, considering all the other lies I was telling at the point, but still. Old habits die hard.
___
Book four: Exit Strategy
Words added: 36
I pulled a selection of video from the trip with Ayres and the others on the way to HaveRatton, mostly exchanges I’d tagged so I could critique my performance later. (A few times I’d broken up fights, been forced to give relationship advice, the infamous Cracker Wrapper in the Sink Incident, and the time near the start of the trip where I’d had to explain to a confused but enthusiastic group of depressingly young humans how to properly use it/its/itself pronouns when talking about me.) I cut it together, labeled it “Murderbot Impersonates an Augmented Human Security Consultant,” and sent it to Gurathin.
___
Book four and a half: Home: Habitat, Range, Niche, Territory
Words added: 347
(You can read this short story here. Archived version here. Don’t scroll down to the comments at the bottom unless you want to see people misgendering Murderbot.)
Instead Ephraim asks her, “Can you separate that person from the purpose they were created for?”
Anger flares automatically, despite her best efforts to stifle it. But this is not an insult she will let stand, she can’t.
Ephraim should know better. He does know better, and his motive is clear: Refer to it as ‘they’ rather than its actual pronouns, to make a show of being respectful, the way this whole thing is a show of him being respectful, while denying it the same rights that every other person, including bots, was given without question. It was a transparent farce, and that just made her all the madder.
“Its pronouns are it/its/itself.” She snapped, and the only reason she managed to stay seated instead of storming out of the room in a fury was because SecUnit was still pinging her with armament request forms, getting more absurd by the second. None of its anger leaked into the messages, even though she knew it had to be listening. She wasn’t the one being insulted, so that meant it was her responsibility to shut the idea that this was at all acceptable down forever.
She continued angrily, “You know this, and I know you wouldn’t even think to use the wrong pronouns for anyone else, not a human, not a bot. So why should a construct be the exception? You say SecUnit is ‘a product of surveillance capitalism and authoritarian enforcement’, but how is that any different from any other refugees we take in from the Corporation Rim? Why should we not extend the same rights we grant bots to constructs? Why do you think it’s okay to use the wrong pronouns for a construct when I know for a fact that it wouldn’t even occur to you to do this to any other person? Use its correct pronouns or do not dare to speak about it at all: it/its/itself.”
Ephraim, for his part, looked suitably ashamed and guilty. “You’re right, I’m sorry, it won’t happen again.”
But not ashamed enough, apparently, because he simply repeated the question: “Can you separate that person from the purpose it was created for?”
___
Book five: Network Effect
Words added: 494
There was no planetary feed (stupid planet) but Stupid Boat had its own rudimentary feed that was heavy with games and pornography but light on anything that might be helpful for a security assessment, like who these people were and what they wanted. Even the individual humans’ feed signatures only contained info about their pronouns and sexual availability, which I didn’t give a damn about.
…
She smiled. “Thank you.” Then she added, “Oh, I’m sorry, I’m being rude, interrogating you before I’ve even introduced myself. Forgive me. My name is Farai, my pronouns are she/her/her/hers. What about you?”
I said, “Call me SecUnit. My pronouns are it/its/itself.”
She smiled again. “It’s nice to meet you, SecUnit. Thank you again.”
…
She yawned. “Okay, third mom.”
I froze, confused and annoyed, and almost lost all the data I’d just finished tagging. I put that on pause and said firmly, “I’m not your third mom. I’m not anyone’s mom. I’m not any kind of gender that can be called a mom. Don’t call me that.”
Amena jolted a little and blinked, looking startled, then frowned, shaking her head slowly, clearly confused. “Wait, what? Don’t call you what? What did I say?”
Okay, so, she hadn’t been deep in thought, she was literally falling asleep standing up. That made it a little less annoying. But only a little.
“You called me your third mom.” I said, trying to actively remove some of the anger from my voice but probably failing miserably. My emotions were shot, okay? And so were hers.
I got confirmation that she hadn’t meant to call me that when, a few seconds after I spoke–yes, it was taking way longer than normal for her to process information. She really needed to go to sleep–her eyes got wide and her face flushed red. I didn’t need to be an expert on human body language to know that meant she was embarrassed.
This was further confirmed when she stammered out, “I–I’m so sorry, I didn’t mean to say that, I don’t–I mean I don’t really see you as my third mom, or a mom, or–” She waved one hand in a frantic gesture. “I don’t see you as any gender that’s normally a mom. I know your gender is indeterminate, I’m sorry, I think I just fell asleep and was half dreaming, so when you told me to go to bed I thought ‘oh that’s what my moms are always telling me’, but your voice was different from both of theirs so my brain sort of just said 'oh yeah that’s your third mom telling you to go to sleep’. But it’s not because I see you as a mom! I think I would have called anyone who told me to go to bed right then my third mom. But I’m really sorry it happened, and I promise it won’t happen again…” Her voice started trailing off at the end despite starting out strong, and I could tell she was starting to fall asleep again.
“I forgive you.” I said, since it was true and I really didn’t want to hurt her feelings, “Just–go to sleep. It’s harder to keep you alive if you’re sleep deprived.”
Instead of making another gendered comment, she gave me two sleepy thumbs up, then turned and trudged away down the corridor. I followed her with two drones, just in case.
___
Book six: Fugitive Telemetry
Words added: 5
Senior Indah said, “The feed ID doesn’t need to say anything other than what everyone else’s says, just name, pronouns, and…” She trailed off. She was looking at me and I was looking at her.
…
I posted a feed ID with the name = SecUnit, pronouns = it/its/itself, gender = not applicable, and no other information.
Indah had blinked, then said, “Well, I suppose that will have to do.”
#Rjalker reads The Murderbot Diaries#The Murderbot Diaries#Murderbot#long post#neopronouns in action#ititspronouns#it/its#Martha Wells#Murderbot spoilers#TMD spoilers#TMBD Spoilers#All Systems Red#Artificial Condition#Exit Strategy#Rogue Protocol#Network Effect#Fugitive Telemetry#Home: Habitat Range Niche Territory
5 notes
·
View notes
Text





someone asked me to post the image of murderbot in a flower crown, so i figured why not post all a few of them! so here you go, these are some of the little edits i made for the murderbot uquiz :)
(please note that i am not an artist (aka can't draw for shit), i used tmd cover art and some freepik art that i found. (sources below the cut))
art: latvian cover art for 'artificial condition' (illustrated by andis reinbergs)
murderbot: french cover art for 'all systems red' (illustrated by pierre bourgerie)
2.0: cover art for the illustrated subterranean press edition of 'the murderbot diaries' (illustrated by tommy arnold); danish cover art for 'all systems red' (i tried but couldn't find the name of the artist, please let me know if you know)
secunit three: 'network effect' illustration (by tommy arnold)
combat secunit: spanish cover art for 'all systems red' (illustrated by cecilia g.f.)
comfortunit: art found on freepik (recolored)
#the murderbot diaries#murderbot#asshole research transport#2.0#secunit three#combat secunit#comfortunit#𓄿#these are silly#i know#i had a lot of fun with them :))#i might add the other 4 later but these are the ones i personally like the most#i think i'm also going to make more icon-style murderbot edits#there is so much great cover art to work with#and it's so much fun!!!!
131 notes
·
View notes
Text
Single Photons Go for Gold - Technology Org
New Post has been published on https://thedigitalinsider.com/single-photons-go-for-gold-technology-org/
Single Photons Go for Gold - Technology Org
In 2015, a class of two-dimensional materials called transition metal dichalcogenides (TMDs) entered the scientific limelight for their ability to produce just one particle of light at a time. Such single-photon emission was a natural, and somewhat random, ability in TMDs with structural defects—missing atoms here and there, or a wrinkle where the crystal should have been straight and even.
The experimental set-up at the Borys Lab at the University of Montana, which specializes in low-temperature optics and has been a long-time collaborator with the Schuck Lab.
Researchers quickly moved from observing single photon emission in TMDs to attempting to engineer the materials in a way that could yield the same effect on demand. Writing recently in Nature Communications, a team including mechanical engineers Jim Schuck and Jim Hone and the Borys lab at Montana State University go for gold to create a single photon emitter.
They carefully placed atomically thin layers of a TMD called tungsten diselenide (WSe2) on the tips of nanoscopic gold cones, which create tiny wrinkles in the material. Those wrinkles yielded strong evidence of single photon emission that, notably, occurred at room rather than ultracold temperature.
Columbia Engineering PhD student Emanuil Yanev is leading the effort to research tungsten diselenide’s properties. In this Q&A, Yanev shares what’s so interesting about single photon emitters, his journey from Idaho to New York City, and a little more about himself and his time at Columbia.
Emanuil Yanev in the Schuck Nano-Optics Lab. Image credit: Columbia University
Why do we need single photons?
We’ve all heard lots about quantum computers lately, but, eventually, we’ll want to build a network of them—essentially, a quantum internet. Single photons can be really important elements in transferring information while preserving its quantum nature.
How did you come up with the idea of using gold cones for this research?
We’ve been experimenting with using strain to create single photons.
In a prior paper published in Nature Nanotechnology, we created “nanobubbles” that strained tungsten diselenide and caused localized photon emission, but we realized that the light was coming from very small wrinkles around the bubble perimeters and not the bubble centers. We thought an array of cones could create similar wrinkles, but in a more robust and prescriptive fashion so we could better determine exactly where the strain originated and where the photons were coming from. Making the cones out of a metal like gold can also enhance the output, like an antenna.
Can we definitively say you can create single photons at room temperature?
Almost. The definitive proof is a correlation measurement that demonstrates antibunching, where you statistically show that there’s zero chance that two photons were emitted at the same time. We’re working on that, but it’s technically challenging with our nano-optical approach.
What we did show was power saturation, which is pretty strong evidence for single photon emission. We excite the tungsten diselenide by shining a laser onto a cone-induced nano-wrinkle. A single photon emitter can’t absorb a second photon until it emits what it has already absorbed from the laser, which takes some time. That means you hit a point where it can’t keep up with the rate of incoming photons, and so the emission output no longer scales with the laser input.
We observed that saturation behavior in our engineered samples at room temperature. This is exciting because it shows that single photons are potentially being created without expensive cryogenic equipment, which so far has been necessary for achieving single-photon emission in TMDs.
What’s next for this research?
To demonstrate antibunching, we need to boost the brightness of the single photon emission, so we’re experimenting with different combinations of materials. We are also starting to think about optimizing the design so that, one day, we can integrate these single photon sources onto circuit chips—that’s the ultimate goal.
Bigger picture, we also want to fundamentally understand what’s going on in these materials. The reason we have smartphones today is because 70-plus years of effort have gone into developing our understanding of silicon—the material that all of our electronics are made from. We’ve pushed the scaling of that technology to the limit more or less, so it’s time to see what we can do with new materials.
And what’s next for you?
I’m nearing the end of my PhD, so I’m starting to write up my thesis. And look for jobs. I’d like to pivot into the quantum computing industry. That’s an exciting space right now. I’ve spent a lot of time doing nanofabrication and working in cleanrooms to make substrates and samples with these 2D materials, and I’d love to continue applying that skillset going forward.
What was your path to your PhD?
My family moved to the US from Bulgaria when I was five, and we ended up in Idaho. Idaho was a great place to grow up, but it’s a little sleepy and I wanted to get into a bigger city, so I enrolled in Columbia’s 3-2 Combined Plan Program. I spent three years at The College of Idaho studying math and physics, then transferred to Columbia to study engineering for another two years.
I’ve been an engineer at heart since I was young. I always enjoyed tinkering and building random things in our garage. When I got to Columbia, I was really excited by the research efforts directed at the nano-scale. I started working in Jim Hone’s lab, and I decided to stay to pursue a PhD, which has been co-advised by Jim Hone and Jim Schuck.
How has your time been at Columbia?
With Jim Hone, I learned a lot about nanofabrication, 2D material synthesis, and sample preparation, and with Jim Schuck, I learned more about optical characterization and applications of these materials. I was a bit of a bridge between the two labs initially, which was a great opportunity: Jim Schuck had just arrived at Columbia when I started my PhD, so I helped teach a lot of the group how to make samples with 2D materials that we would then study optically.
I also spent time at Brookhaven National Laboratory as a Department of Energy Office of Science Graduate Student Research Fellow, where I had the chance to explore advanced nanofabrication techniques, such as cryogenic plasma etching.
The 2D materials field is a highly collaborative environment, and it’s been really rewarding to work with people from lots of different backgrounds. You have this great overlap of researchers from mechanical engineering, electrical engineering, materials science, chemistry, and physics coming together to tackle problems.
How do you keep busy outside of the lab?
Mountain biking, which is usually not the first thing that comes to mind when you think of Manhattan! I’m on the board of the New York City Mountain Bike Association, which is a nonprofit that builds and maintains the majority of off-road trails in the city and offers free bike clinics for kids and adults.
Almost everyone had a bike where I grew up, but that’s not the case here. We give New Yorkers who wouldn’t otherwise have the opportunity to ride a chance to do so, while also improving the parks for hikers and the broader community.
Any words of advice?
Don’t be afraid to fail. A lot of people coming into graduate school are high-achieving individuals, but research is very different from the classroom—you’re going to be failing a lot, and you can’t internalize that. Just because your experiment was unsuccessful doesn’t mean you are a failure: it’s just part of the process. In fact, some of the greatest insights and discoveries are had when things don’t go according to plan, so keep an open mind!
Source: Columbia University
You can offer your link to a page which is relevant to the topic of this post.
#2D materials#Advice#amp#applications#approach#atoms#Behavior#board#bridge#Brookhaven National Laboratory#Building#Bulgaria#chemistry#chips#collaborative#college#communications#Community#computers#computing#crystal#Design#Discoveries#Electronics#energy#Engineer#engineering#engineers#Environment#equipment
0 notes
Text
Mining multi-omics data for molecular subtyping in gliomas facilitates precise clinical treatment
Summary Glioma is the most common malignancy in the skull, accounting for approximately 2% of adult systemic tumors. It is characterized by a high recurrence rate, high disability rate, and poor sensitivity to chemotherapy. Different subtypes of glioma exhibit varying prognosis and chemotherapy sensitivities. Currently, researchers extensively study the molecular classification of glioma based on transcriptomic features, facilitating the evaluation of prognosis. However, identification of tumor subtypes based on the single-layer-omics data have several limitations. In this regard, the present study aimed to identify new subtypes of glioma using three omics datasets for prognosis prediction. As a result, cluster A subtype was identified to be associated with lower activation of cell proliferation and better prognosis, while cluster B subtype exhibited higher infiltration of M2-type macrophages and higher activation of the epithelial-mesenchymal transition (EMT) pathway, potentially leading to a poorer prognosis. Furthermore, we employed the Weighted Gene Co-expression Network Analysis (WGCNA) algorithm and limma R package to identify driver genes for clusters A and B. Consequently, nine genes were identified as gene signatures for cluster A. Based on this finding, we quantified the two subtypes using the single-sample gene set enrichment analysis (ssGSEA) algorithm, where a higher score were linked to elevated tumor mutation burden (TMD) and signaling pathways related to cell proliferation. Low scores indicated enrichment of tumorigenesis-related pathways and poor prognosis. In silico drug screening suggested that AGI-6780 could be an effective compound for high cluster subtypes, based on brain tumor cell lines. Consequently, our study determined that the score can serve as an effective index to predict the prognosis of glioma. http://dlvr.it/Spk2l8
0 notes
Text

I’ve written a new fanfic and it’s not SPN 😱
It’s Murderbot, baby! 🤖💛
There’s this scene in Network Effect that got me hooked on hurt!Murderbot and comforting!ART. So I thought I’d try my hand at this kind of stuff.
Thank you so much to TMD discord server, specifically the #despair-event-horizon channel for motivating me 🥰️💛
Link to fic on AO3 || Link to my fic masterpost
2 notes
·
View notes
Text


erm more network effect doodles *u*
#the murderbot diaries#murderbot#murderbot 2.0#tmd network effect#targetcontrolsystem#body horror#the bit where 2.0 destroys the shuttle is like#one of my fav parts of the whole thing#god its so good
284 notes
·
View notes
Text
How Does Well Being CBD Oil Really Work?
What is Well Being CBD Oil?
The cannabis plant, Cannabis sativa, contains a number of active ingredients, including THC and CBD. THC (tetrahydrocannabinol), the most active ingredient of marijuana, is the component that makes a person high when either smoked or ingested. Cannabidiol (CBD), on the other hand, is not psychoactive: it doesn’t induce a mind-altering effect.
what is Well Being CBD Oil ? is a way of delivering CBD. This chemical is first extracted from the plant and then diluted with a carrier oil like hemp seed. It can then be consumed as either the oil itself or within drinks or confectionary. In the USA, it can be found in health shops.
How does Well Being CBD work?
The human body has two currently-known types of points where cannabinoids can bind, called CB1 and CB2 receptors. Cannabinoids can attach to the CB1 and CB2 docking points since they have a similar structure to the body’s naturally-occurring endocannabinoids. From here, CBD can impact movement, pain, emotions, mood and other functions regulated by endocannabinoids. This is still an area of active research and much of how it all works is still being explored.

Is Well Being CBD Oil effective?
Many users of Well Being CBD Oil Benefits claim it helps to relieve pain and inflammation, reduce anxiety and make them calm. Currently, scientific studies cannot say whether the small CBD quantities available in CBD products have any effect at all, but that hasn’t held back use. This is an area of ongoing research – we just haven’t reached a point where we have all the answers. Science is working to catch up with the demand.
CBD products available in health food shops and on the internet are not controlled or regulated as medicines, other than the legal limit on THC content. As doctors, we are advised to tell patients that ‘over-the-counter or internet’ CBD products lack quality assurance and should not be treated as medicines. There’s no way to be sure of what’s in the products you buy.
What conditions can Well Being CBD Oil help?
The list of things we’re told Well Being CBD Oil can do for us is long, but there is still only preliminary evidence.
There is some belief that CBD is a natural painkiller. It’s also thought to have anti-inflammatory properties, and so it may help as a treatment for inflammatory diseases like Crohn’s disease. Indeed, some small studies in mice have supported this claim by showing that CBD significantly reduced chronic inflammation and pain. This has led hope that it may one day help chronic pain, but we won’t know until human tests are complete.
CBD is also believed to help people who suffer from anxiety and mood-related symptoms, as well as insomnia.
The condition that brought Well Being CBD Oil to prominence is epilepsy. Scientific reviews have found that CBD has anti-seizure properties and there are several clinical trials well underway, some of which use pure CBD product. Stronger forms of CBD have been found to reduce the number of epileptic seizures suffered by some patients by more than 40%.
youtube
An estimated 20.4 percent, or 50 million, Americans live with chronic pain, leading to nearly $560 billion each year in direct medical costs, lowering productivity and increasing disability. Today, chronic pain is one of the most common reasons for adults to seek medical care and has led to opioid dependence, anxiety, depression, restrictions in mobility and daily activities and overall reduction in quality of life. While short-term pain-relieving therapies provide relatively good solutions, an effective long-term solution for chronic pain has yet to be identified.
To establish what we are missing in chronic pain treatment, we first need to understand how the body perceives and responds to pain. Throughout the body we have pain-receptive neurons, known as nociceptors, which respond to damaging or potentially damaging stimuli by sending a “possible threat” signal. The signal travels through the nerves to the spinal cord, which processes the pain message and carries it up to the brain, where it is further processed by the thalamus and then sent to the cerebral cortex, where we perceive it.
Upon receiving a nociceptive pain message, the brain’s pain regulation network can either inhibit or enhance the pain experience according to the context. Typically, an acute pain message is often considered a “good” signal since it alerts the body to potential damage, allowing protective action that can thereafter be inhibited. Chronic pain, however, is usually a “bad” signal, reflecting some dysfunction of the system that fails to inhibit the pain and allows it to go on.
A common question that pain researchers face is why similar diseases or injuries cause varying pain levels in different people. We have come to understand that those living with a balanced pain regulation system are able to better inhibit unnecessary or non-threatening pain messages, while those with an imbalanced system lack this inhibitory capacity and are more susceptible to acute and chronic pains. Research has shown that patients with pain disorders such as migraine, tension-type headache, fibromyalgia, irritable bowel syndrome (IBS), temporomandibular joint disorder (TMD) and osteoarthritis usually have lower ability to inhibit pain.

Individuals living with these chronic pain conditions often rely on over-the-counter (OTC) medications or stronger pharmacological solutions to block unnecessary pain signals. In fact, the global opioid market was sized at $25.4 billion in 2018. However, neither OTCs nor prescription pain medication are ideal for long-term use. Instead of developing more medication combinations for long-term pain management, it is time to rethink how we approach pain modulation altogether. With the advancement of technology in the medical device space, recent technologies are making it possible to treat pain conditions non-invasively.
Treating pain where it doesn’t hurt
“Well Being CBD Oil Reviews” is a time-honored medical observation, where pain in one body site will be perceived as less intensive upon the introduction of another pain at a remote site. The underlying mechanism is the activation of internal inhibitory circuits evoked by the new remote pain that inhibit the original pain. When studying this mechanism in humans, we call this phenomenon “conditioned pain modulation” (CPM), a term that is often used to describe the process of endogenous pain inhibition.
In recent years, consistent data have accumulated demonstrating that CPM is less efficient in patients suffering from chronic pain, especially for those living with an idiopathic pain syndrome. That is, their ability to inhibit the perception of one pain by another is reduced—either as a cause or as a consequence of their chronic pain.
@FACEBOOK: - https://www.facebook.com/Well-Being-CBD-Oil-Price-106951714842463
https://www.facebook.com/Well-Being-CBD-Oil-101165845434029
@YOUTUBE: - https://www.youtube.com/watch?v=KEAtXfCtUck
@TWITTER: - https://twitter.com/WellBeingCBDOi1
#Well Being CBD Oil#Well Being CBD Oil Reviews#Well Being CBD Ingredients#Well Being CBD Oil Benefits#Well Being CBD Oil side effects#Well Being CBD Oil Price#Well Being CBD Oil Cost#Well Being CBD Oil Buy#Well Being CBD Oil USA#Well Being CBD Oil United states
1 note
·
View note
Text

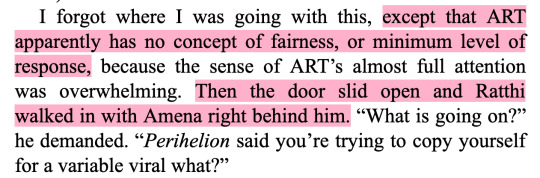
I was moving so fast that later I had to run my video back to analyze my performance. I shoved Target One away and smashed an elbow into Target Two’s face. I tore the energy weapon out of Target Two’s hand along with a few fingers, stabbed the weapon into its chest (it didn’t have a sharp end but I made do) and ripped a large hole. Then I used the weapon, and the large hole, to lift Target Two up and slam it into the upper bulkhead. Three times. Fluid and pieces went everywhere. That was satisfying. I think I’ll do it again.
Network Effect, chapter 4
#fanart#the murderbot diaries#murderbot#murderbot diaries#tmbd#tmd#SecUnit#network effect#blood#blood cw#gore#gore cw
208 notes
·
View notes
Text
I have finished my Network Effect reread and noted another difference.
(Also, can I say? Martha Wells managing completely different voices for 1.0 and 3 is truly amazing given their similar backgrounds and the much shorter amount of time 3 gets to be on screen? I'm not as sure about how 2.0's voice differs or not from 1.0 but there's still some great POV shift happening here.)
During my reread, I'd idly noted that Murderbot's perspective was always past-tense. I though this was a little odd for how it seemed to be narrating current events, though maybe it was a carryover from how the first book was essentially a retrospective diary that it left on Mensah's nightstand.
But it came back to the fore when I realized:
3 thinks in present-tense.
Its narration style differs from 1.0 anyways - more standardized report-style at first, though whether its headers becoming shorter is a personal choice or Wells' decision to speed things up could be read either way. But, 3 always thinks in the present tense! It even throws "is" into sentences with a verb that ends with "-ed" to make clear that everything is present. It's interesting, and I think is part of what contributes to it sounding "younger" than MB - everything is old news for Murderbot, who's been doing this a while, while everything is new (and has no protocol to prep around) for 3. Just a fun detail.
112 notes
·
View notes
Text
Diane E. Hoffmann & Anita J. Tarzian, The Girl Who Cried Pain: A Bias Against Women in the Treatment of Pain, 29 J Law, Med & Ethics 13 (2001)
To the woman, God said, “I will greatly multiply your pain in child bearing; in pain you shall bring forth children, yet your desire shall be for your husband, and he shall rule over you.” --Genesis 3:16
There is now a well-established body of literature documenting the pervasive inadequate treatment of pain in this country.1 There have also been allegations, and some data, supporting the notion that women are more likely than men to be undertreated or inappropriately diagnosed and treated for their pain.
One particularly troublesome study indicated that women are more likely to be given sedatives for their pain and men to be given pain medication.2 Speculation as to why this difference might exist has included the following: Women complain more than men; women are not accurate reporters of their pain; men are more stoic so that when they do complain of pain, “it’s real”; and women are better able to tolerate pain or have better coping skills than men.
In this article, we report on the biological studies that have looked at differences in how men and women report and experience pain to determine if there is sufficient evidence to show that gender3 differences in pain perception have biological origins. We then explore the influence of cognition and emotions on pain perception and how socialized gender differences may influence the way men and women perceive pain. Next, we review the literature on how men and women are diagnosed and treated for their pain to determine whether differences exist here as well. Finally, we discuss some of the underlying assumptions regarding why treatment differences might exist, looking to the sociologic and feminist literature for a framework to explain these assumptions.
We conclude, from the research reviewed, that men and women appear to experience and respond to pain differently, but that determining whether this difference is due to bio- logical versus psychosocial origins is difficult due to the complex, multicausal nature of the pain experience. Women are more likely to seek treatment for chronic pain, but are also more likely to be inadequately treated by health-care providers, who, at least initially, discount women’s verbal pain reports and attribute more import to biological pain contributors than emotional or psychological pain contributors. We suggest ways in which the health-care system and health-care providers might better respond to both women and men who experience persistent pain.
Do Men and Women Experience Pain Differently?
The question of whether men and women experience pain differently is a relatively recent one. Until about a decade ago, many clinical research studies excluded women, resulting in a lack of information about gender differences in disease prevalence, progression, and response to treatment.4 Research on sex-based and gender-based differences in pain response has mounted over the past several years, partially motivated by 1993 legislation mandating the inclusion of women in research sponsored by the National Institutes of Health.5
Three review articles summarized the research findings on sex-based differences in pain response through the mid- 1990s, with most research focusing on sensory (often laboratory-induced) pain. Unruh examined variations between men and women in clinical pain experience through an extensive review of available research.6 She found, in general, that women reported more severe levels of pain, more frequent pain, and pain of longer duration than men. Women were more likely than men to report migraines and chronic tension headaches, facial pain, musculoskeletal pain, and pain from osteoarthritis, rheumatoid arthritis, and fibromyalgia. Women were also more likely than men to develop a chronic pain syndrome after experiencing trauma similar to that experienced by men.
Berkley drew similar conclusions — that for experimentally delivered somatic (skin or deep tissue) stimuli, females have lower pain thresholds, greater ability to discriminate pain, higher pain ratings, and less tolerance of noxious stimuli than males.7 Berkley, however, cautioned that these differences were small and affected by many variables, such as type of pain stimulus, timing of the stimulus, size or bodily locus of the stimulus, and experimental setting. For example, more reliable differences between the sexes have been found when patients are exposed to electrical and pressure stimuli as opposed to thermal stimuli, and when pain is induced in experimental settings as opposed to clinical settings.
Lastly, Fillingim and Maixner reviewed research on sex-based differences in response to noxious stimuli.8 The studies they reviewed also indicated that although pain responses were highly variable among individuals, females exhibited greater sensitivity to laboratory-induced pain than males. They concluded that “it seems plausible that such disparity in the experience of clinical pain [between men and women] could be explained, at least in part, by enhanced pain sensitivity among females.”9
While approximately half of all existing studies prior to 1997 found no difference between men and women in their response to experimental pain, of those studies that did, all were in the same direction: “lower pain threshold, higher pain ratings, and lower pain tolerance for women.”10
More recent studies have contributed further empirical evidence of a difference between men and women in pain response.11 Much of this research has focused on a search for biological differences. Although these early findings do suggest biologically based differences, there remain many research questions yet to be answered.
Biological differences
A number of scientists have hypothesized about potential biological explanations for gender pain differences. Berkley described three aspects of male and female biology that plainly differ: the pelvic reproductive organs, types of circulating hormones, and cyclical changes in hormone levels.12
Other biological explanations for the differences in pain response include mechanisms of analgesia having to do with opioid receptors in the body, mechanisms of nerve growth factor, and sex-based differences in sympathetic nervous system function (e.g., sex-based differences in areas of the brain associated with reproduction). Berkley stated that these differences could result in men and women experiencing different emotional responses to pain13 (e.g., anxiety, fear, depression, or hostility).
Reproductive hormones
A number of studies have added to the body of literature on the influence of reproductive hormones on biological pain differences. Berkley concluded that the reproductive hormones appear to influence sex-based pain differences through the action of a number of neuroactive agents, such as dopamine and serotonin.14
Giamberardino and colleagues found that a woman’s pain sensitivity increases and decreases throughout her menstrual cycle, with skin, subcutaneous tissue, and muscles being affected differently by female hormonal fluctuations.15 They also found that sex-based differences in pain response may depend on the proximity of the stimulus to external reproductive organs. Fillingim and colleagues found that the menstrual cycle produced greater effects on ischemic (i.e., lack of blood flow and oxygen), compared with thermal, pain sensitivity.16 The authors suggest that opiate receptors could be desensitized by reproductive hormones during certain phases of a woman’s menstrual cycle, thus increasing pain sensitivity (particularly ischemic pain sensitivity) at those times.
Glaros, Baharloo, and Glass found that lower levels of circulating estrogens may be associated with higher levels of temporomandibular disorder (TMD) pain and other joint pain in women.17 Dao, Knight, and Ton-That studied the influence of reproductive hormones on TMD.18 They hypothesized that there is a link between reproductive hormones and inflammation and pain — that the hormones may “act directly in the muscles to modulate the release of nitric oxide,” which causes vasodilation (blood vessel dilation), inflammation, and pain.19 In addition, estrogen may interact with various mediators of inflammation (i.e., swelling) and increase pain sensation.20
Stress-induced analgesia responses
Differences have been found between male and female rats for “stress-induced analgesia” responses.21 Stress-induced analgesia involves activation of an intrinsic pain inhibitory system by a noxious stressor, such as exercise-induced stress or predator-evoked stress.
Mogil and colleagues report on a sex-specific stress-induced analgesia mechanism in female mice that is known to be estrogen-dependent and to vary with reproductive status, but for which the neurochemical identity has remained obscure.22 The authors performed genetic mapping experiments to identify the gene underlying stress-induced analgesia in both sexes and found a specific genetic component in female mice but not in male mice.
Brain and central nervous system
Some research has shown differences in the brain and central nervous system of men and women that may contribute to differences in pain response. For example, Fillingim and Maixner describe neural mechanisms that contribute to sex-based differences in the perceptual, emotional, and behavioral responses to noxious stimuli.23 These include peripheral afferents (impulses sent to the brain), brain and central nervous system networks, and peripheral efferents (commands sent from the brain to the muscles). The authors note differences in female tissue thickness and sensory receptor density as one example of structural differences in females that may contribute to enhanced perception of sensation to the skin.
Animal studies provide some evidence that sex-based differences in pain response have biological and genetic origins. Aloisi, Zimmermann, and Herdegen found differences in immune chemicals in the hippocampus and septum of male and female rats that were subjected to a persistent pain- ful stimulus and restraint stress.24 The authors hypothesized that hormonal and behavioral differences between the sexes are accompanied by genetic differences in the limbic system — an area of the brain that, in humans, is involved in cognition and emotion.
Other researchers have probed the human brain for sex- based differences that influence pain responses. Mayer and colleagues found that, compared to male patients with irritable bowel syndrome, female patients with the same syndrome showed specific perceptual alterations in response to rectosigmoid (intestinal) balloon distension and differences in regional brain activation measured by positron emission tomography (PET).25 Findings suggest that physiological sex-related differences in the experience of pain exist in irritable bowel syndrome patients and can be detected using specific stimulation models and brain imaging techniques.
Paulson and colleagues studied cerebral blood flow through PET imaging in normal right-handed male and female subjects as the subjects discriminated differences in the intensity of painless and painful heat stimuli applied to the left forearm.26 Females had significantly greater activation of the contralateral prefrontal cortex, the contralateral insula, and the thalamus when compared to the males. The authors surmised that the differences between men and women in their response to pain were (1) a direct result of physiological differences between men’s and women’s brains; (2) mediated by emotional or cognitive responses that are different between men and women and are responsible for brain activation differences between men and women; or (3) a result of both (1) and (2).
Biology as explaining too much, too little
Given the physiological sex differences reviewed thus far, one might expect the gap in pain responses between men and women to be greater than the research evidence indicates.27 This paradox in the research has led Unruh — commenting on Berkley’s conclusion that differences between men and women in pain perception and response exist but are small and highly variable28 — to argue for a “conceptual shift” in “our efforts to understand the relationships between sex and pain experience”:
The question changes from “Why do women and men differ in their experiences of pain?” to “How do women dampen the effect of powerful sex differences in physiological pain mechanisms to achieve only small sex difference in their actual pain experience?”29
Consequently, researchers must look not only at why women may experience more pain than men, but also at why the difference in experience is not greater than recent findings regarding physiological pain-related differences would indicate. One answer to this paradox may be that some physiological differences between men and women actually make their pain responses similar. For example, De Vries and Boyle concluded that despite major differences in physiological and hormonal conditions, differences between the sexes in the brain create a mediating effect on pain, perhaps resulting in men and women displaying remarkably similar behaviors.30 Another explanation is that more than physiological differences are at work.
What is clear is that the research to date provides ample evidence that differences between men and women in pain response exist.31 What is unclear is whether the reasons for these findings are grounded in differences in biology or differences in coping and expression, or both.
The mind-body connection
Although modern scientists have attempted to identify and localize specific pathophysiological mechanisms that produce and influence pain sensations, progress on this front is advancing slowly. Most experimental pain research has focused on laboratory-induced noxious sensory stimuli, such as heat, cold, pressure, and shock. Subjects report the level at which they detect pain (“threshold”) and the level at which they can no longer tolerate pain (“tolerance”). Bendelow writes: “The experimental nature of these studies does not allow the social context to be taken into account and the psychological research on pain perception is weighted heavily towards sensory cues, with little emphasis on the subjectivity, or indeed any recognition of models of perception that emphasise interaction between sensory cues and expectations or prior experience.”32
The focus on a physiological basis for pain has ignored the findings that one’s response to pain is influenced by a multitude of factors, which may include the biological, psychological, and cultural differences between men and women.
External stimuli may set off a biological cascade that contributes to the sensation of pain, but cognition and emotion also contribute to the experience of pain. Cognitive awareness of and emotional response to pain (which are affected by psychosocial and cultural influences) in turn influence the brain’s and body’s subsequent physiological responses. Unlike the “Cartesian” approach that views pain as a product of either biology (body) or psychology (mind), a more informed approach is to acknowledge the interdependence of the two, in addition to cultural influences.33
Psychological and cultural gender differences
Psychological factors influencing the pain response include cognitive appraisal of pain (i.e., meaning-making), behavioral coping mechanisms, and cultural influences. According to Unruh, “[u]nderlying biological differences in pain mechanisms may predispose women to have more pain and may affect recovery from pain but sociological [i.e., cultural] and psychological factors also influence pain perception and behavior.”34
Cognitive appraisal and meaning-making
Cognitive appraisal refers to the process of attributing meaning to an event, which then influences one’s behavioral response to that event.35 For various reasons, men and women may attribute different meanings to their pain experiences.
For one, the types of pain that men and women experience tend to be different. Women more often experience pain that is part of their normal biological processes (e.g., menstruation and childbirth), in addition to pain that may be a sign of injury or disease. Women may thus learn to attend to mild or moderate pain in order to sort normal biological pain out from potentially pathological pain, whereas men do not need to go through this sorting process.36
In addition, men’s and women’s different gender role expectations may influence how they attribute meaning to their pain. Women have been found, for example, to describe their pain by giving more contextual information, such as impact on personal relationships and child-care duties. Men, on the other hand, are more likely to wait to attend to pain until it threatens to interfere with their work duties. Their pain reports are more likely to be an objective report- ing of physical symptoms or functional limitations, and to lack reference to contextual factors such as impact on personal relationships.37
According to one study, factors that influenced women’s likelihood of seeking health care for their pain included a predisposition to “resilience or positive regard for their ability to handle the problem.” Men, in contrast, were influenced to seek health care by “a negative attitude about the condition in terms of its harmfulness, loss or threat.”38 Thus, gender differences in cognitive appraisal and meaning-making of pain may explain some of the differences between men and women in pain response.
Behavioral coping
Prompted by one’s cognitive appraisal of a stressor like pain, individuals respond using various coping mechanisms. Researchers have found that men and women differ in their mechanisms of coping with stress — particularly, coping with pain. Unruh, citing other studies, reported that women more frequently use coping strategies that include “active behavioral and cognitive coping, avoidance, emotion-focused coping, seeking social support, relaxation, and distraction, whereas men rely on direct action, problem-focused coping, talking problems down, denial, looking at the bright side of life and tension-reducing activities such as alcohol consumption, smoking and drug abuse.”39 Thoits found that women’s ways of coping involved more expression of feelings and seeking social support, whereas men’s ways of coping “were more rational and stoic (e.g., accepting the situation, engaging in exercise).”40 Unruh, Ritchie, and Merskey found that in response to pain, women reported significantly more problem-solving, social support, positive self-statements, and palliative behaviors than men.41 Jensen and colleagues found that among individuals with long-term intractable pain in the neck, shoulder, or back, women increased their behavioral activity (e.g., household chores and social activities) as a coping strategy more often than men.42 Other studies suggest that coping strategies are influenced more by the type and duration of pain than by whether the person is a man or a woman.43
Research has also shown that women, as compared to men, respond more aggressively to pain through health-related activities (e.g., taking medications or consulting a healthcare provider).44 This is consistent with studies that have shown that women tend to report more health-care utilization for treatment of pain than do men.45
Culture, gender, and pain
The interplay between behavior and the value systems of a culture is complex and may influence pain perception in many ways. Children are socialized from a very young age to think about pain and to react to painful events in certain ways. In many societies, boys are actively discouraged from expressing emotions.46 Pollack reports that in the United States, “[r]esearchers have found that at birth, and for several months afterward, male infants are actually more emotionally expressive than female babies. But by the time boys reach elementary school much of their emotional expressiveness has been lost or has gone underground. Boys at five or six become less likely than girls to express hurt or distress, either to their teachers or to their own parents.”47 Pollack attributes this change to attitudes toward boys that are “deeply ingrained in the codes of our society” and as a result of which “boys are made to feel ashamed of their feelings, guilty especially about feelings of weakness, vulnerability, fear, and despair.” Male pain research participants have reported that they “felt an obligation to display stoicism in response to pain.”48 Other investigators found that whether the researcher was a man or a woman influenced male pain response in a laboratory setting, with males reporting less pain in front of a female researcher than a male researcher, whereas the researcher’s sex did not affect the responses of female subjects.49
Culture and socialization may also account for the differences in pain reporting between men and women. Women have been found to adopt a more “relational, community-based perception of the world” that allows them to form more extended social support networks and to express their emotions more than men.50 Because of these different socialization experiences, women’s and men’s styles of communication differ,51 which most likely influence how they report their pain to each other and to health-care providers. Miaskowski noted that “women are better able to fully describe their pain sensations than men, or are more willing to describe them, especially to female nurses.”52 In addition, as already mentioned, women tend to describe their pain to a health-care provider by including contextual information, like the pain’s effect on their personal relationships.53
Differences in treatment
The literature suggests not only that men and women communicate differently to health-care providers about their pain, but that health-care providers may respond differently to them. Miaskowski reported on several studies that identified such differences in response and treatment.54 Faherty and Grier studied the administration of pain medication after abdominal surgery and found that, controlling for patient weight, physicians prescribed less pain medication for women aged 55 or older than for men in the same age group, and that nurses gave less pain medication to women aged 25 to 54.55
Calderone found that male patients undergoing a coronary artery bypass graft received narcotics more often than female patients, although the female patients received sedative agents more often, suggesting that female patients were more often perceived as anxious rather than in pain.56 An- other study, examining post-operative pain in children, found that significantly more codeine was given to boys than girls and that girls were more likely to be given acetaminophen.57
Miaskowski further reported on two more recent studies. In a 1994 study of 1,308 outpatients with metastatic cancer, Cleeland and colleagues found that of the 42 percent who were not adequately treated for their pain, women were significantly more likely than men to be undertreated (an odds ratio of 1:5).58 In another study of 366 AIDS patients, Breitbart and colleagues found that women were significantly more likely than men to receive inadequate analgesic therapy.59 The assessment of undertreatment in both studies was based on guidelines developed by the World Health Organization for prescribing analgesics.
Other studies also indicate differences in how men and women are treated by health-care providers for their pain. In a retrospective chart review of male and female post-operative appendectomy patients without complications, McDonald found that in the immediate post-operative period, males received significantly more narcotic analgesics than females.60 However, differences were not significant when taking into account the whole post-operative period. McDonald suggested that these differences might be due to gender-stereotyping during the initial post-operative period when the patient is still drowsy from anesthesia and not always able to make his or her pain needs known. The nurse may respond differently to male and female patients during this time, as compared to later in the post-surgical recovery period when patients are more fully awake and able to report their pain.61
A recent prospective study of patients with chest pain found that women were less likely than men to be admitted to the hospital. Of those hospitalized, women were just as likely to receive a stress test as men, but of those not hospitalized, women were less likely to have received a stress test at a one month follow-up appointment.62 The authors attributed the differences in treatment to the “Yentl Syndrome,” i.e., women are more likely to be treated less aggressively in their initial encounters with the health-care system until they “prove that they are as sick as male patients.” Once they are perceived to be as ill as similarly situated males, they are likely to be treated similarly.63
The “Yentl Syndrome” hypothesis fits well with the results of a study by Weir and colleagues, which found that of chronic pain patients who were referred to a specialty pain clinic, men were more likely to have been referred by a general practitioner, and women, by a specialist.64 The results suggest that women experience disbelief or other obstacles at their initial encounters with health-care providers. An older study (1982) also found that of 188 patients treated at a pain clinic, the women were older and had experienced pain for a longer duration prior to being referred to the clinic than the men. In addition, the researchers found that women were given “more minor tranquilizers, antidepressants, and non-opioid analgesics than men. Men received more opioids than did women.”65 These findings are consistent with those reported by Elderkin-Thompson and Waitzkin, who reviewed evidence from the American Medical Association’s Task Force on Gender Disparities in Clinical Decision-Making. Physicians were found to consistently view women’s (but not men’s) symptom reports as caused by emotional factors, even in the presence of positive clinical tests.66
In addition to actual differences in treatment, studies have also shown differences in health-care providers’ perceptions of men’s and women’s experiences of pain. McCaffery and Ferrell, using a questionnaire administered to more than 300 nurses, found that nurses perceived differences between men and women in sensitivity to pain, pain tolerance, pain distress, willingness to report pain, exaggeration of pain, and nonverbal pain expressions.67 More respondents felt that women, as compared to men, were less sensitive to pain, more tolerant of pain, less distressed as a result of pain, and more likely to report pain and express pain through nonverbal gestures. In another study, nurses were given vignettes describing a particular patient and situation, and were asked to estimate the minutes needed for specific nursing interventions for each patient. In their estimations, the nurses planned significantly more analgesic administration time (as well as ambulation and emotional sup- port time) for male patients than for female patients.68
In addition to whether the patient is a man or a woman, physical attractiveness and nonverbal expressions of pain have been found to influence a health-care provider’s response to the patient’s pain. Hadjistavropoulos and colleagues found that physically unattractive patients were more likely to be perceived as experiencing greater pain than more attractive patients and that the more attractive patients were more likely to be viewed as able to cope with their pain.69 These differences in perception were more likely to be true for female patients than male patients — that is, the effect of the patient’s attractiveness (or lack thereof) on a health-care provider’s perception of the patient’s pain sensitivity was not significant for male patients but it was for female patients. Attractive female patients were thought to be experiencing less pain than unattractive female patients. The authors concluded that a “strong ‘beautiful is healthy’ stereotype” was used by health-care providers in assessing patient pain and that attractive persons “were perceived to be experiencing less pain intensity and unpleasantness, less anxiety and less disability than physically unattractive persons.”70 The authors further concluded that such stereotypes have a negative effect for both attractive and unattractive individuals.71
What Accounts for Differences in Treatment?
The available literature indicates that women receive less treatment for their pain than men. These findings raise the question of whether such a difference in treatment is justified or whether the differences are the result of unproven assumptions and biases about men and women and their sensitivity toward pain or their credibility in reporting pain.
Rationales supported by the data
Treating men and women differently for their pain might be justified if they experience pain differently or respond differently to pain treatment modalities. As for the latter argument, previous research has shown that men and women metabolize medication differently.72 In response to pain medications specifically, Gear and colleagues showed that women experience significantly greater analgesia from kappa-opioids like pentazocine than males.73 Others have predicted that genetic research will lead to identifying drugs for pain that are specific to men’s and women’s biological needs.74
In addition, evidence indicates that men and women do experience pain differently. There is no consensus, however, whether this difference in experience is because women are biologically more sensitive to pain than men, although recent studies provide evidence to support this explanation.75 What is clear is that women in clinical studies often report greater sensitivity than men in response to the same noxious stimuli. This could mean that, in fact, there is a biological difference between men and women that results in women experiencing greater pain than men when exposed to the same stimulus. Or, it could mean that women do not tolerate pain as well as men, or that women are more likely to report pain than men are.
The difficulty in concluding much from existing studies is the subjective nature of pain. While some researchers are exploring the development of diagnostic techniques to validate patients’ pain reports, there are currently no reliable, objective, clinical indicators for pain, e.g., blood pressure, heart rate, temperature.76 Although men’s and women’s brain and central nervous system functioning have been found to respond differently to laboratory-induced pain, the degree to which cognition and emotion influence these pathways is unclear. Animal studies provide compelling evidence that basic biological differences do exist; however, pain in these studies is measured differently from how it is measured in humans (e.g., time to paw withdrawal or tail lick in rats versus self-report in humans). Because diagnostic techniques are not available to accurately “measure” pain and because pain perception is affected by psychological and cultural factors, patient self-reporting remains the basis for diagnosis.
The data support the assertion that women are more likely to report pain than are men in response to the same stimuli. Apart from differences in pain sensitivity, this could be attributed to differences in coping. The literature on coping appears to indicate that women tend to cope in more constructive ways, such as seeing a health-care provider, reaching out to others, and/or praying, whereas men tend to accept the pain, ignore it, or resort to drugs or alcohol rather than consult with a health-care provider.77 These strategies are consistent with cultural mores that discourage men from expressing weakness or vulnerability.
An alternative hypothesis that may explain why men’s pain complaints evoke more medical and nursing interventions is that men wait longer than women to seek medical assistance for their pain and thus are at a stage where their pain characteristics are more extreme and in need of more immediate care. But while there is some evidence that men are less likely to seek medical care for their pain at early stages (or until it interferes with their ability to work),78 there is no evidence that they are in need of more aggressive care than women when they enter the health-care system for pain relief.79 Rather, study findings suggest that women report more severe pain symptoms than men because they suffer from more severe pain-related diseases. For example, in a telephone survey of those with rheumatoid arthritis, researchers found that women reported more severe symptoms than men and that this difference was due to “more severe disease rather than a tendency by women to over-report symptoms or over-rate symptom severity.”80
The perception of women by health-care providers
Given that women experience pain more frequently, are more sensitive to pain, or are more likely to report pain, it seems appropriate that they be treated at least as thoroughly as men and that their reports of pain be taken seriously. The data do not indicate that this is the case. Women who seek help are less likely than men to be taken seriously when they report pain and are less likely to have their pain adequately treated.81
This conclusion raises the question of what accounts for this difference in treatment. In light of the apparent lack of objective data supporting lesser treatment of women for pain, a likely explanation is the health-care provider’s attitudes regarding male and female sensitivity to or tolerance of pain and the validity of their self-reports. There are, in fact, data to support the hypothesis of this attitude or bias by health-care providers. The study by McCaffery and Ferrell of 362 nurses and their views about patients’ experiences of pain found that while most of the nurses (63 percent) agreed that men and women have the same perception of pain, 27 percent thought that men felt greater pain than women. Only 10 percent thought that women experienced greater pain than men in response to comparable stimuli.82 This result has no justification in the literature (and, as discussed above, is actually contradicted by it). The authors do not speculate as to what might contribute to this difference in attitude.
The same study also found that almost half of the respondents (47 percent) thought that women were able to tolerate more pain than men as compared to 15 percent who felt that men were able to tolerate more pain than women. This result, although consistent with other studies,83 seems at odds with our societal notions that men are stronger and tougher than women and better able to withstand physical discomfort. McCaffery and Ferrell explained this seeming contradiction by speculating that while society attributes strength and bravery to men, these characteristics are dis- played by an unwillingness to complain or express discomfort rather than by an actual tolerance of discomfort.
Other researchers offer alternative explanations for this perceived difference in tolerance. Some have asserted that as a result of women’s biological role in childbirth, women are capable of withstanding significantly more pain than men.84
Fillingim and Maixner postulate that the sum of men’s and women’s differences in pain response exist as a consequence of evolutionary pressures that increase reproductive potential and species survival.85 In her study of the interplay of pain, gender, and culture, Bendelow found that women were frequently thought to be equipped with a “natural capacity to endure pain,” in part linked to their reproductive functioning.86 This attitude does appear to be somewhat common among certain groups, as conveyed by offhand remarks such as, “if men had to bear children, there wouldn’t be any.”87
Bendelow found that “the perceived superiority of capacities of endurance is double-edged for women — the assumption that they may be able to ‘cope’ better may lead to the expectation that they can put up with more pain, that their pain does not need to be taken so seriously.”88 Crook and Tunks point to the influence of the psychoprophylaxis movement in the United States with its implicit assumption that it is good to experience childbirth without the aid of analgesia. As a result, some women who have “gone through psychoprophylaxis classes, feel guilty if they relent at the last minute and ask for an epidural”; according to the authors, “these attitudes imply that we have a value system endorsed by some parts of our population that suggest women should be encouraged to keep a stiff upper lip.”89
Another possible explanation of why health-care providers view women as better able to tolerate pain and thus in need of less treatment is that women have better coping mechanisms than men for dealing with pain. The literature confirms that women in fact have a greater repertoire of coping skills to deal with their pain. These include a greater ability to verbally acknowledge and describe their pain, to seek health-care intervention, and to gain emotional support. Men, in contrast, are likely to ignore the pain or delay seeking treatment.90 Yet this reluctance on the part of men does not lead to the conclusion that women, as not reluctant, must therefore be less in need of adequate treatment. Rather, a request for medical care would seem to imply that the person perceives her pain as real and enough of a threat to her lifestyle to seek outside assistance.
What men’s reluctance says — if anything at all — is that they are perhaps, as a whole, more undertreated than we think. While their complaints of pain appear to be taken more seriously than women’s pain complaints when they initially enter the health-care system, many may not seek medical assistance for their pain and, as a result, may be disadvantaged in getting relief from their painful symptoms.
A third possible explanation of why health-care providers might view men as less tolerant of pain than women may be a projection that men need more assistance with their pain because they are the household breadwinners. In their study, McCaffery and Ferrell found that nurses tended to equate “day-to-day physical functioning with pain tolerance” and that nurses believed men were more likely to stop functioning when they were in pain whereas women would continue their role as homemaker in addition to working outside the home. Another study similarly found that men were “more likely to be referred earlier for active treatment with a combination of therapies because of the demands of their bread- winner roles.”91 Again, such reasoning is unfounded. Unruh argued that women may, in fact, more readily attend to pain and more aggressively manage it because they assume more role responsibilities than men.92 As a result, they “may have more complex concerns about managing the interference of pain in the activities and responsibilities of daily life.” Given this possibility, it would again make more sense for health-care providers to at least be as aggressive in treating women for pain as they are in treating men.
Another factor that may play a key role in explaining the different treatment of men and women for pain and the tendency to treat women less aggressively is the subjective nature of pain and the credibility given to women’s self-reports of pain. These two factors perhaps exacerbate the likely undertreatment of women for pain.
Western medicine discounts female pain expression
In Western medicine, health-care providers are trained to rely predominantly on objective evidence of disease and injury. This is not only true of physicians but also nurses. One study of nurses found that they incorrectly expect patients who report moderate to severe pain to have elevated vital signs or behavioral expressions of pain.93 The medical model overemphasizes objective, biological indicators of pain and underacknowledges women’s subjective, experiential reports. Johansson and colleagues state, “medical models often end up in reductionism and medico-centrism, since they look for expert explanations in biological facts.”94 They cite a study by Baszanger which revealed that physicians attempting to make a diagnosis after consulting with a patient considered “cellular pathology as ‘something,’ whereas illness-provoking, psycho-social circumstances were ‘nothing.’”95
The subjective nature of pain requires health-care providers to view the patient as a credible reporter, and stereo- types or assumptions about behavior in such circumstances (oversensitivity, complaining, stoicism) add to the likelihood of undertreatment of some groups and overtreatment of others.96 The feminist literature is rife with examples and criticism of women’s voices not being heard or considered credible in the male-dominated health-care system. Sherwin de- scribes physicians as frequently “patronizing, detached, disrespectful, ... and unwilling to trust the reports of their women patients.”97 Dresser, in characterizing the literature on women’s health care, finds that women’s “[s]ubjective experiences of illness and treatment are frequently ignored.”98
A deeper examination of why women are treated this way is explored by several feminist authors. They attribute it to a long history within our culture of regarding women’s reasoning capacity as limited99 and of viewing women’s opinions as “unreflective, emotional, or immature.”100 In particular, in relation to medical decision-making, women’s moral identity is “often not recognized.”101 In a recent article, Parks argued that women’s requests for physician assisted suicide (PAS) are likely to be ignored. Parks reasoned that while a man’s request for help in ending his life is likely to be considered a “rational self-evaluation” if marked by “intolerable pain, personal suffering or terminal illness, ... women’s similar experiences are much more likely to be rejected, discounted, or unheeded because their capacity for such determinations of personal suffering are questioned.”102
Evidence of health-care providers’ doubting the pain experience of women with chronic pain is provided by Grace. She found that women with pelvic pain expressed difficulty communicating with their general practitioner about their pain, and some difficulty communicating with their gynecologist.103 A significant number of the women “did not think the doctor (GP) really understood what they said and left the doctor’s office feeling that there were things about their pelvic pain that they hadn’t talked about.”104 These women had received seventy-three different diagnoses to explain the cause of their pain, and reported that their physician implied “nothing was wrong” if no physical cause of pain could be identified.105 More than half of the women said that on occasion they felt that the doctor was not taking their pain seriously or that the doctor expected them to put up with their pain.
Women are also portrayed as hysterical or emotional in much of the medical and other literature. While men may be seen as forceful or aggressive, women are perceived as hysterical for the same behavior.106 Physicians have found women to have more “psychosomatic illnesses, more emotional lability and more complaints due to emotional factors” than men.107 In a frequently cited paper by Engel, “the majority of the case histories presented to illustrate ‘psychogenic pain and the pain prone patient’ are histories of females.”108 Fishbain and colleagues found that female chronic pain patients were more likely to be diagnosed with histrionic disorder (excessive emotionality and attention-seeking behavior) compared to male chronic pain patients.
Some researchers have argued that a “bias toward psychogenic causation for disorders in women has occurred even in well defined painful biological processes: ‘Despite the well documented presence of organic etiologic factors, the therapeutic literature is characterized by an unscientific recourse to psychogenesis and a correspondingly inadequate, even derisive approach to their management.’”109 These findings are consistent with studies reporting that female pain patients are less likely than their male counterparts to be taken seriously or are more likely to receive sedatives than opioids for the treatment of their pain.
The health-care provider’s bias toward psychogenic causes of women’s pain is problematic on two levels. First, women are more likely than men to have their pain attributed to psychogenesis whether or not that is in fact a cause of their pain. Second, for those women whose pain is exacerbated by emotional disorders, the health-care provider’s bias against psychological contributors to pain may lead them to undertreat the pain. Some claim that health-care providers’ predisposition toward attributing women’s pain to emotional causes is related to the higher prevalence of emotional problems (e.g., depression and anxiety) among women.110 However, it is possible that a gender bias exists in the processes by which women are evaluated for and diagnosed with these psychological disorders. What is clear is that women are more likely than men to express their feelings and more likely than men to have their symptoms (including pain) attributed to emotional factors. What is unknown is the degree to which emotional factors actually contribute to women’s and men’s pain experiences.
The tendency of health-care providers to discredit women’s pain reports may, in part, be rooted in communication differences between men and women. Vallerand argues that “[b]ecause pain is a subjective phenomenon that can be assessed most reliably from the patient’s self-report, the ability to communicate the discomfort of pain to a HCP [health- care provider] should be an advantage.” In contrast, it appears that “women’s ability to verbalize their emotions causes their responses to be viewed with suspicion [e.g., considered psychologically based] and treated less aggressively.”111 Alternatively, women’s style of communication may simply not fit neatly into the traditional medical interview model adopted by most physicians. In this model, Smith writes:
[the] physician controls the entry and exit of topics and controls the time devoted to a certain topic. By interrogative speech acts, ... the physician also controls the introduction and timing of topics. Through interruptions, the physician allows or cuts off patient lines of questioning. Several studies have shown that the physician-led medical interview is confined mainly to the question-and-answer mode of speech and that patient-initiated questions are often “dispreferred” in medical interviews.112
In general, women in Western societies are socialized to take turns in conversation, to downplay their own status, and to demonstrate behaviors that communicate more accessibility and friendliness.113 While both men and women might benefit from a more humanistic approach to physician-patient communication,114 it is likely that women are more likely to be disadvantaged by the traditional medical interview model. Women with chronic pain may be particularly vulnerable in this traditional communication style and re- buffed by physicians in their attempts to express the multiple ways in which their pain affects the quality of their lives and their ability to function.115
Lastly, patient characteristics and behaviors may also play a role in how female pain patients are perceived and, thus, how they are treated by their physicians. To the extent that women are culturally influenced to try to look good, even on visits to their physician, they may be viewed by their physician as attractive and thus not really in pain.116 Alternatively, if female patients present with hostility, they may not receive appropriate treatment. Patient hostility has been reported as an obstacle to establishing a rapport with a healthcare provider. A few studies have indicated a correlation between female pain patients and high levels of hostility.117 Such hostility, however, may be the result of frustration with the medical system and difficulty finding a sympathetic health-care provider. There is evidence that chronic pain patients must see dozens of physicians before finding one that is willing and/or able to treat their pain.118
Summary, Implications, and Recommendations
The research findings point to several troubling inconsistencies or paradoxes regarding the differences between men and women in pain response and treatment:
While women have a higher prevalence of chronic pain syndromes and diseases associated with chronic pain than men, and women are biologically more sensitive to pain than men and respond differently to certain analgesics, women’s pain reports are taken less seriously than men’s, and women receive less aggressive treatment than men for their pain.
Although women have more coping mechanisms to deal with pain, this may contribute to a general perception that they can put up with more pain and that their pain does not need to be taken as seriously.
Although women more frequently report pain to a health-care provider, they are more likely to have their pain reports discounted as “emotional” or “psychogenic” and, therefore, “not real.”
Women, being socialized to attend more to their physical appearance, are more likely than men to have health-care providers assume they are not in pain if they look more physically attractive.
Men with chronic pain are more likely to delay seeking treatment, but generally receive a more aggressive response by health-care providers once they enter the health-care system.
Both men and women are more likely to have the emotional or psychological component of their pain experience suppressed due to Western medicine’s tendency to separate mind and body and to view objective, biological “facts” as more credible than subjective feelings.
If one examines these findings from different ethical perspectives, they are deeply problematic. From a justice perspective, for example, there exists a strong argument that individuals should be treated equally effectively according to their needs. Thus, a just approach to providing sex-specific, gender-sensitive pain management treatments acknowledges that men and women in pain may have different needs. The current situation, in which women are more likely than men to be undertreated for their pain, is ethically unjustifiable.
From a utilitarian perspective, undertreating women who have persistent pain is likely to have negative outcomes not only for productivity in the workforce but also for families and children. While undertreating men for pain has implications for their role as monetary providers, the implications of undertreating women are perhaps more far-reaching. In many families, the woman is now the breadwinner or one of the breadwinners.119 In addition, the woman typically takes on the primary role of family caretaker, making sure the household runs well, there is food on the table, and the children are cared for. If women are unable to function because of their pain, the possibility of extensive harm to families and children is very real.
The consequences for our health-care system are also potentially negative. A health-care system that continues to discriminate in its treatment of women is also likely to lose the confidence of its female patrons. There is, in fact, evidence that more women than men use alternative therapies for health-care treatment.120 While the loss of confidence in the conventional health-care system is a threat to its continued well-being, the elevated interest in complementary121 and holistic therapies may be a positive side effect of female patients’ dissatisfaction with the traditional medical system. The question of whether such therapies will be alternative or complementary to conventional medical therapies will be influenced by how conventional health-care providers respond to the demand for a more holistic approach to pain management.
From a perspective of narrative or care ethics, the fact that pain defies mind-body dichotomization and that women, in general, tend to adopt a more holistic approach to health and illness122 might provide justification for a female-specific approach to pain treatment — one that explores etiologies of pain without bias for or against biology, psychology, or other affective contributors, and one that acknowledges context and lived experiences.
Although the growth of holistic medicine may be one silver lining of conventional medicine’s gender-biased approach to pain treatment, this does not change the ethical imperative to rectify our mainstream health-care system’s unjust treatment of women with pain. It is necessary to begin educating health-care providers and those who train them to expose biases that lead to the undertreatment of women. Some research has shown that efforts at educating and enlightening health-care providers regarding women’s health needs has positive effects.123 Moreover, the bias against psychological or emotional pain contributors adversely affects both women and men. Women’s pain tends to be viewed as more emotionally based and thus less credible — or, likewise, less credible if indeed it is emotionally based.124 Men’s pain is more likely to be acknowledged strictly as a physical symptom, thus reinforcing the societal expectation that men suppress their emotions, even if it impedes their pain treatment and recovery.125 Medical schools must endorse, and teach students, an approach that best elicits the concerns of any patient in pain — an approach that does not discount the patient’s subjective reports of pain. This will require attentiveness to the emotional aspects of a patient’s reports of pain. As Johansson and colleagues state:
A purely diagnosis-oriented approach is not enough, and an attitude of healing through adaptation must be completed with a gender perspective on women’s actual circumstances. The medical encounter ought to provide possibilities for the patient to express psychosocial problems. Physicians must have a chance to listen, voice concern, discuss solutions and offer remedies such as counseling as well as medication to empower the patient.126
In addition to more attention to this issue in the medical school curriculum by modeling effective physician-patient communication with respect to pain management, there needs to be scrutiny on the part of quality care evaluators such as the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), as well as ethical awareness-raising by institutional ethics committees about the current bias in the pain treatment of women. Without this pressure, change is unlikely. The fact that JCAHO has established new pain management standards for the institutions that they accredit is a step in the right direction.127 Perhaps inclusion of evaluative mechanisms to ensure that vulnerable populations are not undertreated for pain due to a health-care provider’s gender, ethnic, age, or racial biases will contribute to a more just approach to pain management. In addition to JCAHO’s regulatory approach, institutional ethics committees have a role in educating and enlightening health-care providers regarding unjust pain treatment. Indeed, future JCAHO standards that address organizational ethics may dovetail into the same arena.
Conclusion
Research indicates that differences between men and women exist in the experience of pain, with women experiencing and reporting both more frequent and greater pain. Yet rather than receiving greater or at least as effective treatment for their pain as men, women are more likely to be less well treated than men for their painful symptoms. There are numerous factors that contribute to this undertreatment, but the literature supports the conclusion that there are gender-based biases regarding women’s pain experiences. These biases have led health-care providers to discount women’s self-reports of pain at least until there is objective evidence for the pain’s cause. Medicine’s focus on objective factors and its cultural stereotypes of women combine insidiously, leaving women at greater risk for inadequate pain relief and continued suffering. Greater awareness among health-care providers of this injustice, a readjustment of medicine’s preoccupation with objective factors through education about alternative approaches, and scrutiny by quality and ethical reviewers within health-care institutions are necessary to change health-care providers’ behavior and ensure that women’s voices regarding treatment of their pain are heard.
References
1. See R. Payne, “Practice Guidelines for Cancer Pain Treatment: Issues Pertinent to the Revision of National Guidelines,” Oncology, 12, no. 11A (1998): 169–75; M. McCaffery, “Pain Control: Barriers to the Use of Available Information,” Cancer, 70, no. 5 (supplement) (1992): 1438–49; R. Bernabei et al., “Managing Pain in Elderly Patients with Cancer,” JAMA, 279, no. 23 (1998): 1877–82. See also P. Wall and M. Jones, Defeating Pain, The War Against a Silent Epidemic (New York: Plenum, 1991).
2. See K.L. Calderone, “The Influence of Gender on the Frequency of Pain and Sedative Medication Administered to Postoperative Patients,” Sex Roles, 23 (1990):11–12, 713–25.
3. See P.L. Walker and D.C. Cook, “Brief Communication: Gender and Sex: Vive la Difference,” American Journal of Physical Anthropology, 106, no. 2 (1998): 255–59, who underscore maintaining the distinction between “sex” (the anatomical or chromosomal categories of male and female) and “gender” (socially constructed roles that are related to sex distinctions). It should be noted that while isolating the influence of sex and gender on pain response and treatment is the focus of this article, we do not mean to dismiss the powerful influence of class, race, culture, education, and other such variables that likely affect pain response and treatment.
4. See S.J. Blumenthal and S.F. Wood, “Women’s Health Care: Federal Initiatives, Policies, and Directions,” in S. Gallant and G.P. Keita, eds., Health Care for Women: Psychological, Social & Behavioral Influences (Washington, D.C.: American Psychological Association, 1997): 57–71.
5. See National Institutes of Health Revitalization Act of 1993, Pub. L. No. 103-43, 107 Stat. 22 (June 10, 1993).
6. A.M. Unruh, “Gender Variations in Clinical Pain Experience,” Pain, 65 (1996): 123–67.
7. See K.J. Berkley, “Sex Differences in Pain,” Behavioral & Brain Sciences, 20, no. 3 (1997): 371–80.
8. See R.B. Fillingim and W. Maixner, “Gender Differences in the Responses to Noxious Stimuli,” Pain Forum, 4, no. 4 (1995), 209–21.
9. Id. at 209.
10. A.M. Unruh, “Why Can’t a Woman Be More Like a Man?,” Behavioral & Brain Sciences, 20, no. 3 (1997): at 467.
11. See T.D. Carr, K.L. Lemanek, and F.D. Armstrong, “Pain and Fear Ratings: Clinical Implications of Age and Gender Differences,” Journal of Pain and Symptom Management, 15, no. 5 (1998): 305–13; B.S. Krogstad, A. Jokstad, and O. Vassend, “The Reporting of Pain, Somatic Complaints, and Anxiety in a Group of Patients with TMD Before and 2 Years After Treatment. Sex Differences,” Journal of Orofacial Pain, 10, no. 3 (1996): 263– 69; O. Plesh et al., “Gender Difference in Jaw Pain by Clench- ing,” Journal of Oral Rehabilitation, 25, no. 4 (1998): 258–63 (corroborating that women have a higher incidence than men of temporomandibular pain). See also C.R. France and S. Suchowiecki, “A Comparison of Diffuse Noxious Inhibitory Controls in Men and Women,” Pain, 81, no. 1–2 (1999): 77–84 (finding that women exhibited significantly lower pain thresh- olds than men and reported significantly greater pain in response to both ischemia and electrocutaneous noxious stimulation).
12. See Berkley, supra note 7.
13. Id.
14. Id.
15. See M.A. Giamberardino et al., “Pain Threshold Variations in Somatic Wall Tissues as a Function of Menstrual Cycle, Segmental Site and Tissue Depth in Non-Dysmenorrheic Women, Dysmenorrheic Women and Men,” Pain, 71 (1997): 187–97.
16. SeeR.B.Fillingimetal.,“IschemicButNotThermalPain Sensitivity Varies Across the Menstrual Cycle,” Psychosomatic Medicine, 59 (1997): 512–20.
17. See A.G. Glaros, L. Baharloo, and E.G. Glass, “Effect of Parafunctional Clenching and Estrogen on Temporomandibular Disorder Pain,” Journal of Craniomandibular Practice, 16, no. 2 (1998): 78–83.
18. See T.T. Dao, K. Knight, and V. Ton-That, “Modulation of Myofascial Pain by the Reproductive Hormones: A Preliminary Report,” The Journal of Prosthetic Dentistry, 79 (1998): 663– 70.
19. Id. at 667.
20. Id.
21. See B.S. McEwen, S.E. Alves, K. Bulloch, and N.G. Weiland, “Clinically Relevant Basic Science Studies of Gender Differences and Sex Hormone Effects,” Psychopharmacology Bulletin, 34, no. 3 (1998), 251–59, in which the authors present a review of studies depicting the array of neurochemical and structural effects of ovarian hormones, including their influence on cognitive function and pain sensitivity. Female rats showed less opioid-mediated stress-induced analgesia than male rats when exposed to a variety of stressors, and male rats demonstrated greater swim stress analgesia and less predator-evoked analgesia than females.
22. See J. S. Mogil et al., “Identification of a Sex-Specific Quantitative Trait Locus Mediating Nonopioid Stress-Induced Analgesia in Female Mice,” The Journal of Neuroscience, 17, no. 20 (1997): 7995–8002.
23. Fillingim and Maixner, supra note 8, at 214.
24. See A.M. Aloisi, M. Zimmermann, and T. Herdegen, “Sex-Dependent Effects of Formalin and Restraint on c-Fos Expression in the Septum and Hippocampus of the Rat,” Neuroscience, 81, no. 4 (1997): 951–958. See also A.M. Aloisi, “Sex Differences in Pain-Induced Effects on the Septo-Hippocampal System,” Brain Research Reviews, 25, no. 3 (1997): 397–406.
25. See E.A. Mayer et al., “Review Article: Gender-Related Differences in Functional Gastrointestinal Disorders,” Alimentary Pharmacology & Therapeutics, 13, no. 2 (supplement) (1999): 65–69.
26. See P.E. Paulson et al., “Gender Differences in Pain Perception and Patterns of Cerebral Activation During Noxious Heat Stimulation in Humans,” Pain, 76 (1998), 223–29.
27. Berkley, supra note 7.
28. Berkley, supra note 7.
29. Unruh, supra note 6.
30. See G.J. De Vries and P.A. Boyle, “Double Duty for Sex Differences in the Brain,” Behavioral & Brain Sciences, 92, no. 2 (1998): 205–13.
31. One difficulty in interpreting evidence from research studies is the individual variability of the pain response. Greater variability makes research on pain responses more difficult, as it decreases power and thus increases the likelihood of having in- significant results due to an insufficient number of subjects studied. This has been recently corroborated in a meta-analysis by Riley and colleagues, who determined that only seven of thirty-four studies reviewed on gender differences in pain response had adequate sample sizes. This implies that gender differences have been underestimated rather than overestimated in pain research. See J.L. Riley III et al., “Sex Differences in the Perception of Noxious Experimental Stimuli: A Meta-Analysis,” Pain, 74 (1998): 181–87.
32. G. Bendelow, Pain and Gender (New York: Prentice Hall, 2000): at 17, citing V. Neisser, Cognition and Reality (San Francisco: Freeman, 1976): at 214.
33. Duncan describes how Cartesian (i.e., Descartes’) mind-body dualism is inaccurately equated with medical reductionism, the latter of which tends to dismiss mind (psychology) and favor body (physiology) in the diagnostic encounter. See G. Duncan, “Mind-Body Dualism and the Biopsychosocial Model of Pain: What Did Descartes Really Say?,” Journal of Medicine and Philosophy, 25, no. 4 (2000): 485–513. A more holistic approach is supported somewhat by Melzack and Wall’s gate-control theory of pain, in which a neural mechanism in the spinal cord is thought to function like a gate to control the flow of nerve impulses into the central nervous system. Whether sensory transmission is in- creased or decreased (causing, respectively, a greater or lesser pain intensity perception) is influenced by cognitive and emotional input such as anxiety, mood state, attention, and past experiences. Bendelow and Williams state that the gate-control theory “signals the end of the mind/body split with regard to pain.” However, these authors acknowledge that currently “the biological remains dominant over the social.” Indeed, Duncan points out that the contemporary biopsychosocial model of pain does not entirely escape mind-body dualism. See also R. Melzack and P. Wall, The Challenge of Pain (Harmondsworth, England: Penguin, 1988); G.A. Bendelow and S.J. Williams, “Transcending the Dualisms: Towards a Sociology of Pain,” Sociology of Health and Illness, 17, no. 2 (1995): 139–65, at 143.
34. Unruh, supra note 6, at 157.
35. See R.S. Lazarus and S. Folkman, Stress, Appraisal, and Coping (New York: Springer, 1984), as cited in A. O’Leary and V.S. Helgeson, “Psychosocial Factors and Women’s Health: Integrating Mind, Heart, and Body,” in S.J. Gallant, G.P. Keita, and R. Royak-Shaler, eds., Health Care for Women: Psychological, Social and Behavioral Influences (Washington, D.C.: American Psychological Association, 1997): 25–71.
36. Unruh, supra note 6.
37. Id. at 158.
38. R. Weir et al., “Gender Differences in Psychosocial Adjustment to Chronic Pain and Expenditures for Health Care Services Used,” The Clinical Journal of Pain, 12 (1996): 277–90, at 287.
39. Unruh, supra note 6, at 149, citing L. Astor-Dubin and C. Hammen, “Cognitive Versus Behavioral Coping Response of Men and Women: A Brief Report,” Cognitive Research Therapy, 8 (1984): 85–90; C. Brehms and M.E. Johnson, “Problem-Solving Appraisal and Coping Style: The Influence of Sex-Role Orientation and Gender,” The Journal of Psychology, 123 (1989): 187– 94; J.E. Holm et al., “The Role of Stress in Recurrent Tension Headache,” Headache, 26 (1986): 160–67; A.A. Stone and J.M. Neale, “New Measure of Daily Coping: Development and Prliminary Results,” Journal of Personality & Social Psychology, 46 (1984): 892–906; L.M. Verbrugge, “Sex Differences in Com- plaints and Diagnoses,” Journal of Behavioral Medicine, 3 (1980): 327–55; A.J.J.M. Vingerhoets and G.L. Van Heck, “Gender, Coping and Psychosomatic Symptoms,” Psychological Medicine, 20 (1990): 125–35.
40. P.A. Thoits, “Gender Differences in Coping with Emo-ional Distress,” in J. Eckenrode, ed., The Social Context of Coping (New York: Plenum, 1991): 107–38, as cited in O’Leary and Helgeson, supra note 35, at 30.
41. See A.M. Unruh, J. Ritchie, and H. Merskey, “Does Gender Affect Appraisal of Pain and Pain Coping Strategies?,” The Clinical Journal of Pain, 15, no. 1 (1999), 31–40.
42. See I. Jensen et al., “Coping with Long-Term Musculosk- eletal Pain and Its Consequence: Is Gender a Factor?,” Pain, 57 (1994): 167–72.
43. Unruh, supra note 6, at 149. See also S.P. Buckelew et al., “Health Locus of Control, Gender Differences and Adjustment to Persistent Pain,” Pain, 42 (1990): 287–94; F.J. Keefe et al., “Analyzing Pain in Rheumatoid Arthritis Patients,” Pain, 46 (1991): 153–60; and J. Strong, R. Ashton, and A. Stewart, “Chronic Low Back Pain: Towards an Integrated Psychosocial Assessment Model,” Clinical Psychology, 69 (1994), 1058–63.
44. O’Leary and Helgeson, supra note 35; Unruh, supra note 6; Weir et al., supra note 38. There is some evidence, however, that health-care utilization rates do not differ among elderly men and women and that older females tend to report lower levels of health-care utilization than older males. See K. Hunt et al., “Are Women More Ready to Consult Than Men? Gender Differences in Family Practitioner Consultation for Common Chronic Conditions,” Journal of Health Services and Research Policy, 4, no. 2 (1999), 96–100. See also J.L. Riley, G.H. Gilbert, and M.W. Heft, “Orofacial Pain Symptom Prevalence: Selective Sex Differences in the Elderly?,” Pain, 76, no. 1–2 (1998), 97–104.
45. Miaskowski reports that women report more visits to health-care providers on retrospective assessment, but on prospective studies, men and women seek health care at the same rate. Researchers have attributed this difference to the possibility that men are more reluctant than women to admit visiting health- care providers or less likely to remember such visits. See C. Miaskowski, “The Role of Sex and Gender in Pain Perception and Responses to Treatment,” in R.J. Gatchel and D.C. Turk, eds., Psychosocial Factors in Pain: Critical Perspectives (New York: The Guildford Press, 1999): 401–11, at 406. In one prospective study, E. Berkanovic, C. Telesky, and S. Reeder found that perceived efficacy of health care, perceived seriousness of one’s symptom, and reported disability from that symptom were more highly correlated with health-care utilization than was gender, although older women were found to have accessed a physician more than men. “Structural and Social Psychological Factors in the Decision to Seek Medical Care for Symptoms,” Medical Care, XIX, no. 7 (1981): 693–709.
46. Bendelow, supra note 32. See also G. Bendelow, “Pain Perceptions, Emotions and Gender,” Sociology of Health and Illness, 15 (1993): 273–94; W. Pollack, Real Boys: Rescuing Our Sons from the Myths of Boyhood (New York: Henry Holt & Co., 1998).
47. Pollack, supra note 46, at 11.
48. Miaskowski, supra note 45, at 404.
49. See F.M. Levine and L.L. De Simone, “The Effects of Experimenter Gender on Pain Report in Male and Female Subjects,” Pain, 44 (1991): 69–72.
50. See D.J. Davidson and W.R. Freudenburg, “Gender and Environmental Risk Concerns: A Review and Analysis of Available Research,” Environment and Behavior, 28, no. 3 (1996): 302–39.
51. Women have been found to be more other-directed in conversation and to frequently seek support and validation in their communication encounters. Men have been found to be more goal-directed and status-conscious in communication and to give advice more often. See D. Tannen, You Just Don’t Under- stand: Women and Men in Conversation (New York: Ballantine, 1990).
52. C. Miaskowski, “Women and Pain,” Critical Care Nursing Clinics of North America, 9, no. 4 (1997): at 467.
53. Unruh et al., supra note 41. See also Bendelow, supra note 32.
54. Miaskowski, supra note 45.
55. See B.S. Faherty and M.R. Grier, “Analgesic Medication for Elderly People Post-Surgery,” Nursing Research, 33, no. 6 (1984): 369–72.
56. Calderone, supra note 2. Frequency of pain medication dosing was studied rather than the amount of analgesic being dosed since the latter is related to body weight and men might be administered higher doses based on body weight, not gender bias.
57. See J.E. Beyer et al., “Patterns of Postoperative Analgesic Use with Adults and Children Following Cardiac Surgery,” Pain, 17, no. 1 (1983), 71–81, as cited in Miaskowsi, supra note 45. Miaskowski cautions readers that most studies that have looked at gender differences in post-operative pain medication administration did not evaluate whether men and women received adequate amounts of analgesic medication. See Miaskowsi, supra notes 45 and 52.
58. See C.S. Cleeland et al., “Pain and Its Treatment in Outpatients with Metastatic Cancer,” N. Engl. J. Med., 330, no. 9 (1994): 592–96.
59. W. Breitbart et al., “The Undertreatment of Pain in Ambulatory AIDS Patients,” Pain, 65, no. 2 (1996), 243–49.
60. See D.D. McDonald, “Gender and Ethnic Stereotyping and Narcotic Analgesic Administration,” Research in Nursing and Health, 17 (1994): 45–49. McDonald, however, did not control for patient weight and thus could not rule out that men were given more narcotic analgesics based on greater body weight.
61. However, Raftery and colleagues found that female patients admitted to the emergency room reported more pain than males, were perceived by health-care providers to experience more pain, received more pain medications and more potent analgesics, and were less likely to receive no pain medications. Patient perception of pain and pain severity was the strongest predictor of number and strength of medications given for pain. The sex of the patient or health-care provider did not predict the number, type, and strength of medications received. Thus, health-care provider gender biases may fluctuate by geographical region or medical specialty. See K. A. Raftery, R. Smith-Coggins, and A.H. Chen, “Gender-Associated Differences in Emergency Department Pain Management,” Annals of Emergency Medicine, 26, no. 4 (1995): 414–21.
62. See V. Elderkin-Thompson and H. Waitzkin, “Differences in Clinical Communication by Gender,” Journal of General Inter- nal Medicine, 14 (1999): 112–21.
63. See P.A. Johnson, L. Golman, and E.J. Orav, “Gender Differences in the Management of Acute Chest Pain: Support for the ‘Yentl Syndrome,’” Journal of General Internal Medicine, 11 (1996): 209–17.
64. Weir et al., supra note 38. “Specialist” was not defined, and the possibility exists that some women were referred by a gynecologist who was considered a “specialist,” but served as the woman’s primary care provider.
65. See D.Z. Lack, “Women and Pain: Another Feminist Is- sue,” Women and Therapy, 1 (1982): 55–64, as cited in Unruh, supra note 6, at 159.
66. Elderkin-Thompson and Waitzkin, supra note 62. In addition, Crook and Tunks found that women with persistent pain were significantly more likely than men with persistent pain to receive psychotropic drugs from their family practitioner. See J. Crook and E. Tunks, “Women with Pain,” in E. Tunks, A. Bellissimo, and R. Roy, eds., Chronic Pain: Psychosocial Factors in Rehabilitation (Malabar, Florida: R.E. Krieger Publishing Company, 1990): 37–48.
67. See M. McCaffery and B.R. Ferrell, “Does the Gender Gap Affect Your Pain Control Decisions?,” Nursing, 22, no. 8 (1992): 48–51.
68. See D. McDonald and R.G. Bridge, “Gender Stereotyping and Nursing Care,” Research in Nursing and Health, 14 (1991): 373–78.
69. See T. Hadjistavropoulos, B. McMurty, and K.D. Craig, “Beautiful Faces in Pain: Biases and Accuracy in the Perception of Pain,” Psychology and Health, 11 (1996): 411–20.
70. Id. at 417. The hypothesis that stereotyping based on attractiveness may actually influence individuals’ pain responses (i.e., attractive individuals learn to actively cope better with pain and thus experience less pain intensity, and unattractive individuals learn more passive pain coping mechanisms and experience greater pain intensity) was considered.
71. See T. Hadjistavropoulos, H.D. Hadjistavropoulos, and K.D. Craig, “Appearance-Based Information about Coping with Pain: Valid or Biased?,” Social Science and Medicine, 40, no. 4 (1995): 537–43; H.D. Hadjistavropoulos, M. Ross, and C.L. von Baeyer, “Are Physicians’ Ratings of Pain Affected by Patients’ Physical Attractiveness?,” Social Science and Medicine, 31 (1990): 69– 72.
72. See S.M. Ebert, X. Liu, and R.L. Woosley, “Female Gender as a Risk Factor for Drug-Induced Cardiac Arrhythmias: Evaluation of Clinical and Experimental Evidence,” Journal of Women’s Health, 7, no. 5 (1998): 547–57. See also P.M. Thompson and J.L. Wolf, “The Sexual Revolution in Science: What Gender-Based Research Is Telling Us,” Journal of Investigative Medicine, 47, no. 3 (1999): 106–13.
73. See R.W. Gear et al., “Gender Difference in Analgesic Response to the Kappa-Opioid Pentazocine,” Neuroscience Letters, 205, no. 3 (1996): 207–09; R.W. Gear et al., “Kappa-Opioids Produce Significantly Greater Analgesia in Women Than in Men,” Nature Medicine, 2, no. 11 (1996): 1248–50. See also L.D. Jamner et al., “Pain Inhibition, Nicotine, and Gender,” Experimental and Clinical Psychopharmacology, 6, no. 1 (1998): 96–106 (finding that nicotine had a direct pain-inhibitory effect in men but not in women); M.E. Robinson et al., “Sex Differences in Response to Cutaneous Anesthesia: A Double Blind Randomized Study,” Pain, 77 (1998): 143–49 (finding that men responded differently from women to the pain inhibitory effects of a local anesthetic, e.g., locally anesthetized men rated a pressure stimulus as less painful than anesthetized women).
74. See J. Mogil, “Does He Feel Her Pain? Maybe Not,” University of Illinois Alumnae LAS Newsletter, Spring (1999): at 7.
75. Weir et al., supra note 38, at 278, stating that “several current hypotheses from the biological perspective are that pain perception is probably related to sensory factors rather than differences in attitudes or emotional responses, and that endogenous pain inhibition may be affected by hormonal variation.”
76. Although episodes of acute, severe pain will often be associated with an increase in heart rate or blood pressure, and increased heart rate is used in some studies (e.g., with infants) as a proxy measure of pain, others discourage clinicians from relyiing on these physiological measures as evidence of a patient’s pain. See M. McCaffery and B.R. Ferrell, “How Vital Are Vital Signs?,” Nursing, 22, no. 1 (1992): at 45 (“No firm clinical evidence exists to support the assumption that moderate to severe pain is always accompanied by a change in vital signs.”).
77. Unruh, supra note 39.
78. O’Leary and Helgeson, supra note 35; Unruh, supra note 6; Weir et al., supra note 38.
79. Unruh, supra note 6, at 159. See also P.P. Katz and L.A. Criswell, “Differences in Symptom Reports Between Men and Women with Rheumatoid Arthritis,” Arthritis Care & Research, 9, no. 6 (1996): 441–48.
80. Id. at 441.
81. Miaskowski, supra note 45, at 406.
82. McCaffery and Ferrell, supra note 67.
83. Bendelow, supra note 32, at 130. See also Nurofen, Pain Relief Study (London: Kings Fund, 1989), as cited in Bendelow, supra note 32, at 36.
84. See E.E. Johansson et al., “The Meanings of Pain: An Exploration of Women’s Descriptions of Symptoms,” Social Science and Medicine, 48, no. 12 (1999), 1791–1802.
85. Fillingim and Maixner, supra note 8.
86. Bendelow, “Pain Perceptions, Emotions, and Gender,” supra note 46, at 286.
87. Bendelow, supra note 32, at 53–55. 88. Id. at 115–16.
89. Crook and Tunks, supra note 66, at 38. 90. Unruh, supra note 39.
91. See L.M. Verbrugge, “Females and Illness: Recent Trends in Sex Differences in the United States,” Journal of Health and Social Behavior, 17 (1976): 387–403, as cited in Weir et al., supra note 38, at 288. Bendelow also describes how women’s more predominant involvement in the domestic sphere has associated them more with the “natural” world in the form of bodily functions, whereas men have been more involved in the “public world of work and therefore ‘higher’ cultural and mental processes.” The perception thus may exist that men’s “higher” functioning, if interrupted by the presence of pain, should receive a higher priority for medical intervention. See Bendelow, supra note 32, at 131.
92. N.L. Marshall states, “combining work and family has become the norm for women rather than the exception.” N.L. Marshall, “Combining Work and Family,” in S.J. Gallant, G.P. Keita, and R. Royak-Shaler, eds., Health Care for Women: Psycho- logical, Social and Behavioral Influences (Washington, D.C.: American Psychological Association, 1997): 163–74, at 163.
93. McCaffery and Ferrell, supra note 76.
94. Johansson et al., supra note 84, at 1792.
95. See I. Baszanger, “Deciphering Chronic Pain,” Sociology of Health and Illness, 14 (1992): 181–215, as cited in Johansson et al., supra note 84, at 1792.
96. Studies have found that the most significant predictor of inadequate pain relief is a discrepancy between the patient and physician regarding the severity of the patient’s pain. See Cleeland et al., supra note 58.
97. R. Dresser, “What Bioethics Can Learn from the Women’s Health Movement,” in S.M. Wolf, ed., Feminism & Bioethics (New York: Oxford University Press, 1996): 144–59, at 147, citing S. Sherwin, No Longer Patient: Feminist Ethics and Health Care (Philadelphia: Temple University Press, 1992): at 193.
98. Id. at 147.
99. J.A. Parks, “Why Gender Matters to the Euthanasia Debate: On Decisional Capacity and the Rejection of Women’s Death Requests,” The Hastings Center Report, 30, no. 1 (2000): 30–36, at 33.
100. S. H. Miles and A. August, “Courts, Gender and the ‘Right to Die,’” Journal of Law, Medicine & Health Care, 18 (1990): 85– 95.
101. Id.
102. Parks, supra note 99. See also K. H. Rothenberg,“Gender Matters: Implications for Clinical Research and Women’s Health Care,” Houston Law Review, 32, no. 5 (1996), 1201–72.
103. V.M. Grace, “Problems of Communication, Diagnosis, and Treatment Experienced by Women Using the New Zealand Health Services for Chronic Pelvic Pain: A Quantitative Analysis,” Health Care for Women International, 16 (1995): 521–35.
104. Id. at 525.
105. Id.
106. See Sherwin, supra note 97, at 48. See also J.F. Smith, “Communicative Ethics in Medicine: The Physician-Patient Relationship,” in S.M. Wolf, ed., Feminism & Bioethics (New York: Oxford University Press, 1996): 184–215, at 194 (“Women who do speak assertively are often taken to be domineering rather than dominant, emotional rather than rational, biased rather than authoritative, and complaining rather than assertive.”). Kate Nicholson, a disability lawyer who is writing a book about her experiences living with chronic neuropathic pain, and who commented on an earlier version of this manuscript, expressed concern that acknowledging gender differences in pain response might lead to gender stereotyping. She made a point of trying to report her pain to health-care providers factually and unemotionally, and recalled one female pain specialist’s comment to her, “You are not crazy; you’re not like my other patients.” Additionally, she recalled a male acquaintance’s adamant demand from emergency room staff to give him something for his acute pain (“You SOB’s, you are giving me something for pain and you’re giving it to me right now!”). He got the pain medication. Yet Nicholson was aware that if she had done something similar, “I’d have been perceived extremely differently, in all likelihood.”
107. See Unruh, supra note 6, at 158, summarizing the literature on this point.
108. See Crook and Tunks, supra note 66, at 37, citing G. Engel, “‘Psychogenic’ Pain and the Pain-Prone Patient,” American Journal of Medicine, 26 (1959): 899–918.
109. See K. J. Lennane and R. J. Lennane, “Alleged Psychogenic Disorders in Women — A Possible Manifestation of Sexual Prejudice,” N. Engl. J. Med., 288 (1973): 288–92, as cited in Unruh, supra note 6, at 158.
110. Women are four times as likely as men to be diagnosed with a major depression, and twice as likely as men to be diagnosed with a general depression, although rates vary with ethnicity and culture. Possible reasons for this may include that women are more willing to seek help and thus may be diagnosed more frequently; there may be biological differences that predispose women to developing depression (e.g., effects of reproductive hormones); or women may be more likely to suffer from depression due to external stressors (e.g., the effects of sexism, domestic violence, lower pay, and relationship stressors). See F.M. Culbertson, “Depression and Gender,” American Psychologist, 52, no. 1 (1997), 25–31. See also O’Leary and Helgeson, supra note 35. Also, female chronic pain patients are more likely than male chronic pain patients to be diagnosed with and treated for depression. See W.E. Haley, J.A. Turner, and J.M. Romano, “Depression in Chronic Pain Patients: Relation to Pain, Activity, and Sex Differences,” Pain, 23 (1985): 337–43.
111. See A.H. Vallerand, “Gender Differences in Pain,” Image: Journal of Nursing Scholarship, 27, no. 3 (1995): at 237.
112. Smith, supra note 106, at 190.
113. See D.L. Roter and J.A. Hall, “Gender Differences in Patient-Physician Communication,” in S.J. Gallant, G.P. Keita, and R. Royak-Shaler, eds., Health Care for Women: Psychological, Social & Behavioral influences (Washington, D.C.: American Psychological Association, (1997): 57–71.
114. Smith, supra note 106.
115. Female physicians, however, have been found to spend more time with patients, engage in more positive talk, ask more questions, and elicit more responses from patients. See Roter and Hall, supra note 113. See also J. Bensing, A. Van den Brink-Muinen, and D. de Bakker, “Differences Between Male and Female General Practitioners in the Care of Psychosocial Problems,” Medical Care, 31 (1993): 219–29.
116. Hadjistavropoulos, McMurtry, and Craig, supra note 69; Hadjistavropoulos, Hadjistavropoulos, and Craig, “Appearance-Based Information about Coping with Pain: Valid or Biased?,” supra note 71; Hadjistavropoulos, Ross, and von Baeyer, “Are Physicians’ Ratings of Pain Affected by Patients’ Physical Attractiveness?,” supra note 71.
117. See S.A. Selfe, Z. Matthews, and R.W. Stones, “Factors Influencing Outcome in Consultations for Chronic Pelvic Pain,” Journal of Women’s Health, 7, no. 8 (1998): 1041–48.
118. In a Connecticut focus-group study with chronic pain patients, participants reported visiting multiple physicians (quoting “60 to 100”) in order to find a diagnosis and a practitioner with whom they felt comfortable. See S. Grantham and M. Robbins, The Connecticut Pain Management Initiative: Focus Group Report (Boston: John Snow, Inc., February 11, 2000).
119. Marshall, supra note 92.
120. About 55 to 65 percent of those who consult complementary practitioners are women, the highest users being those aged 35 to 60. See C. Zollman and A. Vickers, “ABCs of Complementary Medicine: Users and Practitioners of Complementary Medicine,” British Medical Journal, 319, no. 7213 (1999): 836– 38; and E. Ernst, “Prevalence of Use of Complementary/Alternative Medicine: A Systematic Review,” Bulletin of the World Health Organization, 78, no. 2 (2000): 252–57.
121. Controversy over use of the term “alternative” rather than “complementary” medicine demonstrates the point being made here. The former describes therapies that are not sanctioned by conventional medicine and which patients choose instead of conventional medical therapy. The latter views such therapies as complementing conventional medical therapies. The goal would be for women (as well as men) to have access to both traditional and non-traditional therapies for pain management, with a focus on a holistic approach that provides optimal pain relief. This holistic approach is the accepted standard for many pain clinics and inpatient pain teams, but adequate access to such care is limited for many individuals — either because the pain teams and clinics are not available in their area or they do not get the referral they need.
122. Davidson and Freudenberg conclude that women in general, as a result of their socialization, are not as likely to develop a distinction between themselves as individuals and the world around them, whereas men are socialized to objectify and control their environment and to define themselves as separate from the world around them. Men would thus be more apt to try to separate biological and psychosocial pain etiologies, whereas women would tend to view them more holistically. See D.J. Davidson and W.R. Freudenburg, “Gender and Environmental Risk Concerns: A Review and Analysis of Available Research,” Environment and Behavior, 28, no. 3 (1996): 302–39. This theory is affirmed by Bendelow’s findings that women spoke of pain experiences more holistically as compared to men and that “men were significantly less inclined to think that the emotional component of pain perception had any importance.” See Bendelow, supra note 32, at 90.
123. See D.S. Kwolek et al., “Gender Differences in Clinical Evaluation: Narrowing the Gap with Women’s Health Clinical Skills Workshop,” Academic Medicine, 73, no. 10 (supplement) (1998): S88–90.
124. That is, women may: (1) have their pain complaints erroneously dismissed as being emotionally-based and therefore “not real” when there is no significant psychological component to the pain; (2) have the likely psychological components that accompany chronic pain be misidentified by health-care providers as the cause, rather than the result of their unrelieved pain, leading to a discounting of the pain; or (3) have the psychological problem that is the source of their pain be discounted and not adequately addressed. All three are inappropriate and reveal a disdain for psychosocial contributors to pain over evidence of organic causation. See Duncan, supra note 33.
125. Bendelow found that men who were given an opportunity to discuss the emotional aspects of their pain experiences did so and were grateful for the opportunity, even though they did not initially acknowledge emotions as contributing to their pain. See Bendelow, supra note 32, at 90–94.
126. Johansson et al., supra note 84, at 1800.
127. Some institutions have already begun addressing the impact of JCAHO pain management standards. See C. Pasero, M. McCaffery, and D.B. Gordon, “Build Institutional Commitment to Improving Pain Management,” Nursing Management, 30, no. 1 (1999): 27–33.
#pain#medicine#gender inequality#women#feminism#epistemology of pain#chronic pain#pain management#bias#gender bias#bias in medicine#communication#subjectivity#embodiment#healthcare#sexism#misogyny
1 note
·
View note
Text
Microwave Devices Market Share and Growth Information Analysis Report by 2024
16th August 2021 – The global Microwave Devices Market size is expected to value at USD 11.86 billion by 2024. The market is subject to witness a substantial growth due to the increasing consummation of Gallium Nitride (GaN) and Silicon Carbide (SiC) devices. These devices provide benefits such as high efficiency and heat tolerance. Additionally, the devices are capable of performing precisely in harsh environments. Such advantages are expected to drive the demand of the market over the forecast period. Globally, the microwave devices market is predicted to grow at a higher CAGR in forecast period, providing numerous opportunities for market players to invest in research and development in the market.
With recent technological advancement in microwave technology, has led to improved accuracy, and superior performance, thus driving demand of the microwave devices in number of telecommunication applications. Growing popularity of the microwave devices in various telecommunications applications is attributed to high bandwidth and faster data transmission rate. Some of the major applications of the microwave devices include generation, amplification, detection, and measurement of the microwave signal. The current developments in telecom sector involving introduction of 4G and 5G technology is making businesses to adopt highly advanced microwave emitting hardware across network bridges. These factors are critical for the sustained growth of the microwave devices industry over the forecast period.
Access Microwave Devices Market Report with TOC @ https://www.millioninsights.com/industry-reports/microwave-devices-market
Rise in the demand of the power modules, amplifiers, and transmitters from various electronic manufacturing industries is expected to boost the growth of microwave devices industry in years to come. Furthermore, substantial increase in the investments by private organization in research and developments, is leading development of the by modern and sophisticated microwave devices. Growing customer base owing to increasing focus towards implementation of connected technology such as IoT is anticipated to boost market growth in upcoming years as well. Higher penetration of mobile phones in developing countries is driving demand of the microwave devices due to higher frequencies associated with these devices and capability to perform long-range communication.
The C-band is one of the fastest growing segment in the microwave devices market with substantial revenue generation in the last couple of years. The X-band segment has also witnessed substantial growth, in recent years. Growing popularity of the C-band is credited to its increasing adoption in the satellite, communications, and television. Some of the critical advantages of the C-band include cost-effectiveness and flexibility. C-band is widely used in the telecommunication applications involving fiber optics. Application of the C-band ranges from radio transmissions and particle accelerators. Above-mentioned factors are key drivers for sustained the growth of the market.
Microwave devices are broadly divided into two categories such as relays and coaxial switches. Microwave devices operates at very high frequencies. Microwave devices are widely used as a test and measurement equipment, in wireless technologies like 4G & 5G, and base station use. Microwave devices typically requires high power for their operations. Microwave device use a particular set of vacuum tubes to generate microwave signal. Principal of operation for microwave devices involves the use of ballistic movement of electrons in a vacuum while varying electric or magnetic fields accordingly.
The microwave devices industry is divided by region such as North America, Europe, Asia-Pacific, Latin America and Africa. North America has shown major growth in recent years owing to the rise in the implementation of latest technologies such as broadband data links, countermeasures, and surface radars, and existence of well-established industrial infrastructure. Asia-Pacific region is predicted to hold major market share in the microwave devices market with massive growth in forecast period. Countries such as India, China and Singapore are leading the Asia-Pacific market with increasing defense expenditure by regional governments and significant investment by leading industry players considering potential opportunities in the region.
The key players in the microwave devices industry are Communications & Power Industries Limited, Cytec Co., Teledyne e2V plc, L-3 Communication systems, MicroWave Technology Ltd., RF Micro Devices Ltd., Richardson Electronics Limited, Teledyne Technologies Incorporations, Thales Group, TMD Technologies Limited, and Toshiba Co.
Request a Sample Copy of Microwave Devices Market Report @ https://www.millioninsights.com/industry-reports/microwave-devices-market/request-sample
0 notes
Text
Microwave Devices Market 2024 - Top Countries Data with Future Scope and Top Key Players Analysis
16th August 2021 – The global Microwave Devices Market size is expected to value at USD 11.86 billion by 2024. The market is subject to witness a substantial growth due to the increasing consummation of Gallium Nitride (GaN) and Silicon Carbide (SiC) devices. These devices provide benefits such as high efficiency and heat tolerance. Additionally, the devices are capable of performing precisely in harsh environments. Such advantages are expected to drive the demand of the market over the forecast period. Globally, the microwave devices market is predicted to grow at a higher CAGR in forecast period, providing numerous opportunities for market players to invest in research and development in the market.
With recent technological advancement in microwave technology, has led to improved accuracy, and superior performance, thus driving demand of the microwave devices in number of telecommunication applications. Growing popularity of the microwave devices in various telecommunications applications is attributed to high bandwidth and faster data transmission rate. Some of the major applications of the microwave devices include generation, amplification, detection, and measurement of the microwave signal. The current developments in telecom sector involving introduction of 4G and 5G technology is making businesses to adopt highly advanced microwave emitting hardware across network bridges. These factors are critical for the sustained growth of the microwave devices industry over the forecast period.
Access Microwave Devices Market Report with TOC @ https://www.millioninsights.com/industry-reports/microwave-devices-market
Rise in the demand of the power modules, amplifiers, and transmitters from various electronic manufacturing industries is expected to boost the growth of microwave devices industry in years to come. Furthermore, substantial increase in the investments by private organization in research and developments, is leading development of the by modern and sophisticated microwave devices. Growing customer base owing to increasing focus towards implementation of connected technology such as IoT is anticipated to boost market growth in upcoming years as well. Higher penetration of mobile phones in developing countries is driving demand of the microwave devices due to higher frequencies associated with these devices and capability to perform long-range communication.
The C-band is one of the fastest growing segment in the microwave devices market with substantial revenue generation in the last couple of years. The X-band segment has also witnessed substantial growth, in recent years. Growing popularity of the C-band is credited to its increasing adoption in the satellite, communications, and television. Some of the critical advantages of the C-band include cost-effectiveness and flexibility. C-band is widely used in the telecommunication applications involving fiber optics. Application of the C-band ranges from radio transmissions and particle accelerators. Above-mentioned factors are key drivers for sustained the growth of the market.
Microwave devices are broadly divided into two categories such as relays and coaxial switches. Microwave devices operates at very high frequencies. Microwave devices are widely used as a test and measurement equipment, in wireless technologies like 4G & 5G, and base station use. Microwave devices typically requires high power for their operations. Microwave device use a particular set of vacuum tubes to generate microwave signal. Principal of operation for microwave devices involves the use of ballistic movement of electrons in a vacuum while varying electric or magnetic fields accordingly.
The microwave devices industry is divided by region such as North America, Europe, Asia-Pacific, Latin America and Africa. North America has shown major growth in recent years owing to the rise in the implementation of latest technologies such as broadband data links, countermeasures, and surface radars, and existence of well-established industrial infrastructure. Asia-Pacific region is predicted to hold major market share in the microwave devices market with massive growth in forecast period. Countries such as India, China and Singapore are leading the Asia-Pacific market with increasing defense expenditure by regional governments and significant investment by leading industry players considering potential opportunities in the region.
The key players in the microwave devices industry are Communications & Power Industries Limited, Cytec Co., Teledyne e2V plc, L-3 Communication systems, MicroWave Technology Ltd., RF Micro Devices Ltd., Richardson Electronics Limited, Teledyne Technologies Incorporations, Thales Group, TMD Technologies Limited, and Toshiba Co.
Request a Sample Copy of Microwave Devices Market Report @ https://www.millioninsights.com/industry-reports/microwave-devices-market/request-sample
0 notes