Text
Diseases of the thyroid gland
------------------------
Chapter 2 : Thyroiditis.
-----------------------
Thyroiditis:
Inflammation of the thyroid gland that it can be:
1. Acute : bacterial infection
2. Subacute : ➡ painful : Viral (De Quervain's )
➡ silent (painless) : postpartum. Autoimmune.
3. Chronic: Hashimoto's & Riedel's
4. Other: Amiodarone and thyroiditis
------------------------------
De Quervain's:
🔮 follows a viral illness.
🔮 also called : subacute granulomatous thyroiditis.
🔮 clinical features:
🎯 prodromal phase lasts few weeks : fever, flu-like illness.
🎯Transiet hyperthyroidism ➡ euthyroid state ➡ hypothyroid state.
The transiet hyperthyroidism is due to the leakage of hormones from the inflamed gland.
🎯 Painful, tender thyroid gland. Maybe enlarged
🎯 ⏬⏬ Radioiodine uptake
🎯 ⏫⏫ ESR
🔮 Treatment.
🚨 Mild symptoms : NSAIDs and Aspirin
🚨 More severe: Corticosteroids
🔮 Recovery:
Most patient have recovery within few months to 1 year.
--------------------------------------
Hashimoto thyroiditis:
🔮 Chronic lymphocytic thyroiditis.
🔮 Most common cause of autoimmune thyroid disorder.
🔮 More common in women
🔮Causes:
🔆 Genetic
🔆 Antithyroid antibodies.
🔮 Clinical manifestation:
🎯 Goiter
🎯 Hypothyroidism often later in the disease.
🔮 Normal thyroid lab works unless hypothyroidism is present.
🔮 Antithyroid antibodies:
Antiperoxidase antibodies (in 90% of patients)
Antithyroglobulin antibodies (in 50% of patients)
🔮Treatment : Thyroid hormone
--------------------------------------------
Reidel thyroiditis:
🔮 Fibrous tissue replaces the thyroid tissue ➡ firm thyroid.
🔮 The fibrosis doesn't stop at the thyroid gland but it can destroy nearby tissue.
🔮 in severe cases the parathyoid, trachea and muscles, nerves fuse together into one solid fibrous mass :(
🔮 Symptoms:
🎯 Goiter (hard like a rock) ➡ pressure on surrounding structures ➡ shortness of breath & Dysphagia.
🎯 Voice hoarseness.
🎯Hypothyroidism symptoms :
Lack of energy
Constipation
Dry skin
Cold intolerance.
🔮 Diagnosis:
⏬ thyroid hormones
Enlarged gland on Ultrasound/ CT-scan / MRI
On tissue biopsy : Fibrous tissue & ⏫ T-cells & IgG 4 antibody-producing plasma cells.
🔮Treatment:
Corticosteroids
Thyroid hormone
Surgery
#studyblr#medical student#medicine#notes#Endocrine#endocrinewithmarie#biology#endocrine 2020#usmle#mcat#plab#education#thyroid#science#physiology#clinical#thyroiditis#hypothyroidism
41 notes
·
View notes
Text
Diseases of the thyroid gland
----------------------------------
Chapter 1 : Hyperthyroidism.
-----------------
We're going to discuss:
What is Hyperthyroidism?
Causes of hyperthyroidism?
Clinical manifestation.
Lab works
Other investigations
Treatment
What is a thyroid storm?
----------------------------------------
What is hyperthyroidism?
It is a state where there is ⏫ synthesis of the thyroid hormones : T4 & T3 ➡ ⏫ levels of these hormones in the blood.
-------------------------------
Causes:
Graves' disease (diffuse toxic goiter)
Plummer disease (multinodular toxic goiter)
Toxic thyroid adenoma (single nodule)
Subacute thyroiditis & Hashimoto thyroiditis. (Transient hyperthyroidism)
Fetal thyrotoxicosis
Other rare causes:
- postpartum thyroiditis (transiet)
- Iodine-induced hyperthyroidism.
- Excessive dose of levothyroxine.
------------------
1. Graves' disease:
Autoimmune disorder.
Thyroid-stimulating immunoglobulin TSI (IgG) binds to the TSH receptors on the thyroid cells ➡ triggers the synthesis of excess thyroid hormones.
Younger women >
Goiter : every thyroid cell is hyperfunctioning so it affects ALL parts of the gland >> diffuse. Non tender
2. Plummer disease:
Starts with chronic lack of dietary Iodine ➡ low levels of T4 ➡ triggers high levels of TSH ➡ Thyroid hypertrophy & hyperplasia.
The growth is uneven >> nodules.
These nodules become toxic when a genetic mutation happens and causes TSH recepters to be constantly ON. >> ⏫⏫⏫ T4/T3.
That elevation acts as a negative feed back to the pituitary gland to secrete less TSH >> the rest of the thyroid is not functioning >> atrophy .
3. Adenoma : 2% of all cases.
4. Thyroiditis:
Inflammation of the thyroid gland >> releasing the previously synthesized thyroid hormones ➡ temporary ⏫⏫ in circulating T4/T3.
A hypothyoid phase may follow.
5. Fetal thyrotoxicosis:
Classically in an infant born to a mother with Graves disease. TSI are IgG and can cross the placenta.
--------------------------------------------
Clinical manifestations : Symptoms
Nervousness.
Irritability
Insomnia.
Fine tremor
Hyperactivity
Heat intolerance & excessive sweating.
Weight loss despite increased appetite.
Proximal muscle weakness.
Palpitations.
Signs:
On the thyroid glad:
Graves' : diffusely enlarged. symmetric . Nontender gland. Bruit may be present.
Subacute thyroiditis: exquisitely tender. Diffusely enlarged (viral illness)
Plummer: bump. Irregular . Asymmetric gland.
Toxic adenoma: single nodule with atrophic gland.
Extrathyroidal:
Eyes: - Edema of the extraocular muscles ➡ proptosis (hallmark of Graves') - lid lag - lid retraction
- corneal exposure ➡ excessive tearing.
Cardiovascular effects: ⏫ Blood pressure.
- Arrhythmias : Sinus tachycardia - Atrial fibrillation
Skin: Warm & moist - pretibial myxedema (specific to Graves')
Neurologic: Hyperreflexia - fine tremor.
-----------------------------------
Lab works:
⏬⏬ TSH
⏫⏫ free T4 & FT3
Other investigations:
1. RAIU:
Radioactive iodine uptake scan.
Useful to differentiate the causes of hyperthyroidisim.
If the uptake is ⏫look for the findings (forms):
Diffuse ( homogeneous) ➡ Graves'
Heterogeneous (multiple nodules of ⏫uptake) ➡ plummer
Focal (one area of ⏫ uptake w/suppression of rest of the gland) ➡ adenoma (hot nodule)
No RAIU findings (⏬⏬uptake) we look at serum thyroglobulin:
⏫ ➡ Thyroiditis /iodine exposure / extraglandular production
⏬ ➡ Exogenous thyroid hormone.
2. Radioactive T3 uptake:
Gives information about the status of TBG
We give resin to the patient + radioactive T3.
Radioactive T3 will bind to resin only when there is no space left on TBG.
SO WHEN THERE IS ⏫T4 ➡ no available seats on TBG ➡ more radioactive T3 will bind to resin ➡ ⏫ radioactive uptake.
The importance of this is to know if there is true hyperthyroidism or increased TBG
High TBG production ➡ low radioactive T3 uptake.
3. Free thyroxine index (FTI) :
Proportional for FREE T4 concentration.
Calculated to correct for the changes in the thyroid binding proteins.
FTI : ( Radioactive T3 uptake × serum total T4) /100
FTI : (patient's radioactive T3 uptake / normal radioactive T3 uptake) × total T4
Normal : 4-11
--------------------------------------------
Treatment :
1. Pharmacologic:
🎐Immediate control of adrenergic symptoms:
B-blockers (propanolol)
🎐 Anti-thyroid drugs: Thionamides
Methimazole:
1- Inhibits thyroid peroxidase ➡ stops the oxidation of Iodide into Iodine
2- Inhibits the coupling of DIT and MIT to form T3 & T4.
PTU (propylthiouracil) :
Shares the same mechanism with Methimazole except that PTU works on the peripheral tissue by
- Inhibiting the converting of T4 into T3.
⚠ Watch for side effects⚠
⚠Agranulocytosis
⚠Skin rash
⚠Arthralgias
Specific ⚠ for PTU is:
Hepatotoxicity.
During pregnancy:
Both can cross the placenta but it is preferred to give:
PTU at the first trimester
Methimazole at the 2nd and 3rd trimester.
Sodium ipodate or iopanoic:
Lowers serum T3 & T4 levels and causes rapid improvement of hyperthyroidism.
Appropriate for acute management of severe hyperthyroidism that's not responding to conventional therapy.
2. RAI ; Radioactive iodine:
Causes destruction of thyroid follicular cells.
Uses IODINE 131
Most common for: Graves' disease & multi-nodular goiter.
If the first dose doesn't control the hyperthyroidism within 6 to 12 months then administer another dose.
✔ Selected pations ✔
✔ Elderly patients w/Graves disease.
✔ Solitary toxic nodule
✔ Patients w/graves disease in whom therapy w/antithyroid drugs fails.
⚠ Warning ⚠
⚠ Hypothyroidism over time in the majority patients. ⚠
Note :
Ophthalmopathy can worsen after RAI prevent that by prophylactic therapy w/prednisone in high-risk patients.
3. Surgery:
Very effective
Only 1% of patients are treated by it.
Often reserved w/patients that have large goiters ; more common in toxic multinodular goiter.
⚠ Side Effects ⚠
⚠ permanent hypothyroidism 30%
⚠Recurrent laryngeal nerve palsy 1%
⚠Permanent hypoparathyroidism 1%
⚠ watch for hypocalcemia (due to inflammation/removal of the parathyroid glands)
------------------------------------------
Treatment plan :
Immediate control of adrenergic symptoms (of any cause) ➡ (beta-blocker) propanolol
Non-pregnant patients w/Graves' disease: beta blocker + Methimazole Taper B-blocker after 4-8 weeks (once methimazole takes effect) give methimazole for 1-2 years then measure TSI at 12 months : ✔ Absent ➡ discontinue therapy. ✔ Relapse ➡ Resume methimazole for 1 more year or radioactive therapy.
Pregnant patients w/Graves' disease : Endocrinology consult is indicated before starting treatment.
Toxic multinodular goiter or Toxic adenoma: RAI or surgery Methimazole pretherapy for surgery and before RAI in selected patients.
------------------------------------
What is a thyroid storm?
Rare, life-threatening complication of thyrotoxicosis.
Characterized by an acute exacerbation of the manifestations of hyperthyroidism.
There's usually a precipitating factor: infection, DKA, stress (Surgery, illness, childbirth)
High mortality rate
Clinical manifestations:
✔ Marked fever
✔ Tachycardia
✔ agitation
✔ Confusion
✔ GI symptoms (nausea , vomiting , diarrhea)
Treatment:
Provide supportive therapy : IV fluids , cooling blankets and glucose
Give antithyroid agents (PTU preferred due to its peripheral effects) followed w/iodine.
B-blockers
Dexamethazone (steroids) to impair peripheral generation of T3 from T4 and to provide adrenal support.
-------------------------
Wow that was a long one XD
I tried to include all the important stuff :)
Resources:
First-aid
Kaplan lecture notes 2019
Medscape
Pocket medicine
Step-up to medicine.
#studyblr#study motivation#medicine#biology#medicinewithmarie#endocrinewithmarie#hyperthyroidism#notes#usmle#usmle step 2#medical student#medblr#notes 2020#thyroid#education#endocrine notes#nedicine
28 notes
·
View notes
Text
I think I am going to re-do all of these notes
66 notes
·
View notes
Text
hi!!! if your blog is medical/science related could you please reblog this i want to follow more stem students thank you!!!
75 notes
·
View notes
Text
Factors that increase TBG :
Pregnancy
Liver disease
Oral contraceptives
Aspirin.
4 notes
·
View notes
Text
Thank you so much! I am really glad you liked them and I know right? I'd say memorizing physiology is a great way to make the best out of diseases comprehension! Snd ty again! Your feedback means a lot🌸
The endocrine system physiology

Part 4 (last part)
In this chapter we're going to talk about:
1. Thyroid Hormones.
2. Insulin & Glucagon.
Thyroid Hormones:
T4 or Thyroxine
T3 or Triiodothyronine
Calcitonin.
T4 & T3 :
T4 and T3 are tyrosine based hormones. Produced by the follicular cells (thyrocytes).
Synthesis:
Iodide (I-) is taken from the bloodstream by follicular cells to the colloid where it gets oxidized to iodine (I) then it combines with thyroglobulin to form MIT (monoiodotyrosine) and DIT (diiodotyrosine) .
Two DIT molecules combine to form T4 while MIT & DIT combine to form T3.
Iodinated thyroglobulin is transported back to the follicular cells and is cleaved by lysosomes.
T4 & T3 are then released into the circulation through MCT transporter.
Regulation:
TRH ➡ TSH ➡ THYROID ➡T4 & T3
➡ By:
⏫Iodide pumping
⏫ Iodination
⏫Thyroglobulin synthesis.
⏫ release of thyroid hormone.
T4 & T3 bind in the plasma to plasma proteins such as:
TBG or Thyroxine binding globulin
Albumin
Transthyretin.
The bound form is the inactive form. While free T3 & T4 form the active form that works on cells.
Note that inside the cell T4 is coverted to T3 by 5-Iodinase.
Effects:
⏫ Basal metabolic rate.
⏫Activation of sympathetic nervous system.
⏫long bone growth
⏫Hair follicle growth
Regulation of body temperature & weight.
Brain development.
Insulin:
Is a peptide hormone produced and secreted by Beta cells which are cells in the islets of langerhans
Synthesis:
Single polypeptide (preproinsulin) ➡ proinsulin (which has 3 chains : peptide A, peptide B and peptide C in between.
Proinsulin gets cleaved on two positions leaving the C chain alone (AWW :-( )
Two disulfide bonds connect The B chain and the A chain to form INSULIN
Effects:
⏬⏬ Blood sugar levels.
How :
In the liver:
Activates the formation of glycogen
(glucose ➡ glycogen)
In adipose tissue:
Activates glycolysis
In skeletal muscles :
stimulates amino acids and glucose uptake into muscle cells ➡ protein production and muscle growth.
Inhibites:
▶ Gluconeogenesis
▶ lipolysis.
Glucagon:
A hormone produced by alpha cells which are cells in the islets of langerhans.
Works by ⏫⏫ blood suger ▶ in situations like: fasting.
And it does that by:
▶ activation of gluconeogenesis & glycogenolysis
▶ activation of lipolysis.
Glucagon is a catabolic hormone which means it promotes the breaking down of large storage molecules inside certain tissues into small energy molecules in the blood.
Glucagon stimulators:
▶ low blood suger
▶ adrenaline
▶ cholecystokinin
Glucagon inhibitors:
▶ high blood sugar
▶ somatostatin
▶GH
Part 1
Part 2
Part 3
💒- 💒-💒-💒-💒-💒-💒-💒
Hello 🌸🍃
With this we're done with a good part of endocrine physiology!Next, we're going to start with clinical cases and diseases related to the endocrine system (aka we're gonna get serious SERIOUS xD) I hope you find this helpful in reviewing or studying ☺
Thank you so much🌸🍃
Marie🌸
53 notes
·
View notes
Text
https://mariesstudycorner.tumblr.com/post/633082331131002880/the-endocrine-system-physiology
The Endocrine system - physiology
https://mariesstudycorner.tumblr.com/post/632263039373213696/the-endocrine-physiology-overview
#endocrine#studyblr#med blr#medical student#notes#medicinewithmarie#biology#endocrinewithmarie#medicine#med school#medical school#clinical#human science#human body#education#hormones
33 notes
·
View notes
Text
https://mariesstudycorner.tumblr.com/post/632801959869595648/the-endocrine-system-physiology
The Endocrine system - physiology
https://mariesstudycorner.tumblr.com/post/632263039373213696/the-endocrine-physiology-overview
33 notes
·
View notes
Text
https://mariesstudycorner.tumblr.com/post/632722640607526912/the-endocrine-system-physiology
The Endocrine system - physiology
https://mariesstudycorner.tumblr.com/post/632263039373213696/the-endocrine-physiology-overview
33 notes
·
View notes
Text
The Endocrine system - physiology
https://mariesstudycorner.tumblr.com/post/632263039373213696/the-endocrine-physiology-overview
33 notes
·
View notes
Text
The endocrine system physiology

Part 4 (last part)
In this chapter we're going to talk about:
1. Thyroid Hormones.
2. Insulin & Glucagon.
Thyroid Hormones:
T4 or Thyroxine
T3 or Triiodothyronine
Calcitonin.
T4 & T3 :
T4 and T3 are tyrosine based hormones. Produced by the follicular cells (thyrocytes).
Synthesis:
Iodide (I-) is taken from the bloodstream by follicular cells to the colloid where it gets oxidized to iodine (I) then it combines with thyroglobulin to form MIT (monoiodotyrosine) and DIT (diiodotyrosine) .
Two DIT molecules combine to form T4 while MIT & DIT combine to form T3.
Iodinated thyroglobulin is transported back to the follicular cells and is cleaved by lysosomes.
T4 & T3 are then released into the circulation through MCT transporter.
Regulation:
TRH ➡ TSH ➡ THYROID ➡T4 & T3
➡ By:
⏫Iodide pumping
⏫ Iodination
⏫Thyroglobulin synthesis.
⏫ release of thyroid hormone.
T4 & T3 bind in the plasma to plasma proteins such as:
TBG or Thyroxine binding globulin
Albumin
Transthyretin.
The bound form is the inactive form. While free T3 & T4 form the active form that works on cells.
Note that inside the cell T4 is coverted to T3 by 5-Iodinase.
Effects:
⏫ Basal metabolic rate.
⏫Activation of sympathetic nervous system.
⏫long bone growth
⏫Hair follicle growth
Regulation of body temperature & weight.
Brain development.
Insulin:
Is a peptide hormone produced and secreted by Beta cells which are cells in the islets of langerhans
Synthesis:
Single polypeptide (preproinsulin) ➡ proinsulin (which has 3 chains : peptide A, peptide B and peptide C in between.
Proinsulin gets cleaved on two positions leaving the C chain alone (AWW :-( )
Two disulfide bonds connect The B chain and the A chain to form INSULIN
Effects:
⏬⏬ Blood sugar levels.
How :
In the liver:
Activates the formation of glycogen
(glucose ➡ glycogen)
In adipose tissue:
Activates glycolysis
In skeletal muscles :
stimulates amino acids and glucose uptake into muscle cells ➡ protein production and muscle growth.
Inhibites:
▶ Gluconeogenesis
▶ lipolysis.
Glucagon:
A hormone produced by alpha cells which are cells in the islets of langerhans.
Works by ⏫⏫ blood suger ▶ in situations like: fasting.
And it does that by:
▶ activation of gluconeogenesis & glycogenolysis
▶ activation of lipolysis.
Glucagon is a catabolic hormone which means it promotes the breaking down of large storage molecules inside certain tissues into small energy molecules in the blood.
Glucagon stimulators:
▶ low blood suger
▶ adrenaline
▶ cholecystokinin
Glucagon inhibitors:
▶ high blood sugar
▶ somatostatin
▶GH
Part 1
Part 2
Part 3
🌸- 🌸-🌸-🌸-🌸-🌸-🌸-🌸-🌸
Hello 🌸🍃
With this we're done with a good part of endocrine physiology!Next, we're going to start with clinical cases and diseases related to the endocrine system (aka we're gonna get serious SERIOUS xD) I hope you find this helpful in reviewing or studying ☺
Thank you so much🌸🍃
Marie🌸
#studyblr#medicine#physiology#notes#endocrine notes#insulin#thyroid gland#T4#thyroid hormones#glucagon#biology#biochem#pathology#medblr#study#study motivation#study inspo#notes 2020#endorinewithmarie#medical student#usmle#education
53 notes
·
View notes
Text
Nothing is more worthy than to fight for your dreams.💎
6 notes
·
View notes
Text
The Endocrine System physiology
Part 3

ACTH & Adrenocortical hormones.
ACTH :
Polypeptide hormone produced and secreted by the anterior pituitary gland in the brain. ACTH regulates the levels of the hormones produced by the adrenal glands.
ACTH synthesis:
Preproopiomelanocortin -(cleaved)-> POMC -> (splits into many peptides one of them is ACTH)
ACTH release:
Pulsatile manner
Peaks in the morning.
ACTH role:
ACTH binds to its receptors and activates the release of cortico-steroid hormones:
Glucocorticoids : anti-inflammatory & metabolic effects
Mineralocarticoids: Electrolyte and water balance.
Adrenocortical Hormones:
Once ACTH binds to its receptors on the cells of the layers of the adrenal cortex it stimulates these cells to take cholesterol from the blood which is essential for adrenocortical hormones synthesis.
ACTH stimulates cholesterol desmolase enzyme inside these cells.
cholesterol desmolase converts:
Cholesterol -> pregnenolone
The adrenal cortex has 3 layers (as we mentioned in part 1)
Zona glomerulosa -> Aldosterone.
Zona fasciculata -> Cortisol
Zona reticularis -> Androgens.
The synthesis of Aldosterone: {image}
Aldosterone ⬆⬆ blood volume & ⬆⬆ blood pressure.
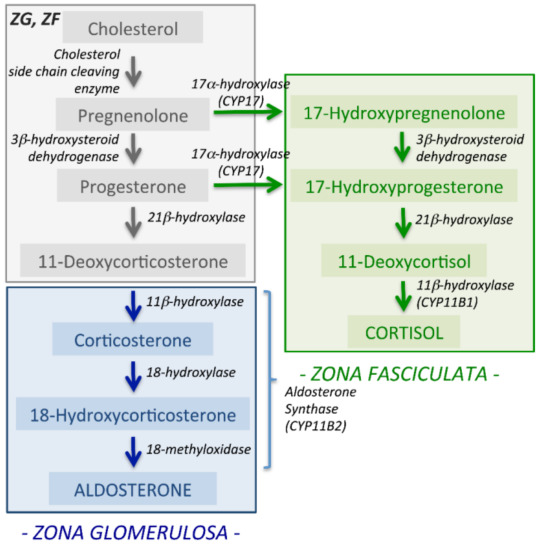
Pregnenolone --(3beta-HSD) → progesterone --(21beta-hydroxylase)
→ 11-DOC --(11 beta- hydroxylase)→ corticosterone -- (18 hydroxylase)
→ 18-hydroxy-corticosterone → ALDOSTERONE.
3beta-HSD= 3 Beta- hydroxysteroid dehydrogenase
11- DOC = 11- deoxycorticosterone
Aldosterone function:
Regulation of sodium concentration
⬆Blood volume → ⬆ blood pressure.
How?
Binds to receptors on the cells lining the distal tubule and collecting ducts → ⬆⬆ sodium/potassium pumps → ⬆⬆ sodium reabsorption into the blood → ⬆⬆ blood volume → ⬆⬆ blood pressure.
The synthesis of cortisol : {image }
1. Pregnenolone & progesterone -(17 alpha-hydroxylase)→
17 alpha- hydroxy-pregnenolone & 17 alpha-hydroxy -progesterone.
2. 17 alpha-hydroxy pregnenolone -(3beta-HSD) → 17 alpha-hydroxy -progesterone -(21beta-hydroxylase) → 11-Deoxycortisol → CORTISOL.
Cortisol function:
Cortisol is not stored but secreted once produced.
Pulsatile manner & peaks in the morning.
It is also secreted in stressful situations like - infections - caffeine - hypoglycemia (low blood sugar levels)
Cortisol is anti-inflammatory hormone and it inhibites: prostaglandin & leukotrienes.
Cortisol effects on the body:
Cortisol ⬆⬆ blood glucose & blood pressure
Fat → activates lipolysis → breaking down of fat in adipose tissue.
Liver → activates gluconeogenesis & glycogenolysis
⬆⬆ insulin resistance → diabetogenic
Muscles → activates proteolysis
⬆⬆Blood pressure
⬇⬇ bone formation
Poor wound healing.
What is cortisone?
Some tissues can convert cortisol to cortisone by the enzyme 11 beta- hydroxysteroid-dehydrogenase 2.
Cortisone has marginally reduced glucocorticoid activity compared to cortisol (80-90%), and thus, cortisone can be considered an active metabolite of cortisol.
Androgens : {image}

17 alpha-hydroxypregnenolone → DHEA → Androstenediol → Testosterone.
DHEA → Androstenedione → Testosterone
17 alpha hydroxyprogesterone → Androstenedione → Testosterone.
Testosterone → Estrogen by the enzyme Aromatase.
Note:
The amount of testosterone secreted by the adrenal glands is very small compared to the one produced by the testes.
Part 1 { here}
Part 2 { here}
#studyblr#study motivation#2020 quarantine challenge#medicine#endocrine notes#endocrinewithmarie#medicinewithmarie#medical student#med school#ACTH#adrenal glands#aldosterone#cortisol#androgen#education#study inspo#biology#physiology#biochem#medblr#science#high yield#usmle#usmle endicrine#mcat
16 notes
·
View notes
Photo



271217 | 🎧 : jazzclub - BoA
the week this spread was made in was one of the worst weeks this month :c [open for better quality xx]
girl almighty sticker from @studyrose
ig: ttstudys
4K notes
·
View notes
Text
The Endocrine System physiology.
Part 2

Calcium and phosphate hormonal regulation
Extracellular calcium can be found in three forms:
As the free cation (Ca2+)
Complexed calcium -> linked to tiny negatively-charged ions like: phosphate & Oxalate
Bound to proteins like: Albumin
Only the free-ionized calcium (Ca2+) is involved with the cellular processes.
Calcium levels in the blood are regulated by three major hormones:
PTH = Parathyroid hormone
Active vitamin D
Calcitonin
Normal calcium level : 8.5 - 10 mg/dl
PTH :
PTH synthesis:
PreproPTH (synthesized by the chief cells in the parathyroid glands) -> proPTH (after the prepropth is cleaved by an enzyme called: signal peptidase) -> moves to the Golgi Apparatus -> PTH (After proPTH is being cleaved by trypsin-like enzyme)
How does PTH help in regulating calcium levels?
PTH increases calcium extracellular levels
When Ca2+ is normal/ ⬆⬆:
When Ca2+ levels are normal or⬆⬆ then more Ca2+ bind to calcium sensing receptors on the chief cells. These receptors are bound to an enzyme called: Phospholipase c by G protein. This phospholipase c gets activated then it splits PIP2 to DAG & IP3 that gets into the Endoplasmic reticulum (ER) and binds to Ins3PR -> ⬆⬆ intracellular calcium -> stops the secretion of PTH.
When Ca2+ levels are ⬇⬇:
1. PTH ⬆ bone resorption -> ⬆ Ca2+ & phosphate.
PTH binds to receptors on the osteoblasts -> producing cytokines like RANL & M-csf -> causes few macrophages to fuse together forming an osteoclast -> breaks down bone -> ⬆⬆Ca2+ and phosphate
2. ⬆⬆ Ca2+ reabsorption in the Distal convoluted tubule
By binding to the principle cells and stimulating the making of more sodium/calcium channels -> ⬆⬆Calcium reabsorption from the urine.
3. Blocks phosphate reabsorption in the proximal tubule.
Why ?
Because in the blood calcium binds to phosphate and forms complexed calcium that is not active. So to prevent that PTH works on getting rid of phosphate or (phosphaturia)
4. Acts on the cells in the proximal tubule to increase the synthesis of 1-alpha-hydroxylase that converts vitamin D to its active form = [ Calcitriol]
Active vitamin D :
Vitamin D has two inactive forms:
D2 or Ergocalciferol
D3 or Cholecalciferol
D2 comes from the plants in our food while D3 comes from animal products/ sunlight and they are both inactive.
Inactive vit D to active vit D:
D2 & D3 from the diet -> small intestine -> packed with bile salts -> absorbed by the enterocytes -> chylomicrons -> lymph-> lymphatic system-> blood -> liver [carried by vitamin D-binding proteins ]
In the liver:
25- hydroxylase converts : D2 -> Ercalcidiol and D3 -> calcifediol -> kidney -> proximal tubule
In the proximal tubule:
1- alpha- hydroxylaze converts: Ercalcidiol -> ercalcitriol & calcifediol -> calcitriol
Calcitriol & ercalcitriol are active vitamin D forms
In the skin: The keratinocytes produces
7-dehydrocholesterol that absorbs UV radiation and gets converted to previtamin D3 then isomerizes into vitamin D3 -> blood etc.
How does vitamin D help with calcium regulation?
Vitamin D ⬆⬆⬆ calcium levels in the blood
1. On the bone : It has the same effects as PTH
2. In enterocytes: ⬆ calcium & phosphate absorption from the food.
Stimulates the synthesis of cal-bindin D-28k -> ⬆ calcium absorption from the food.
Stimulates the synthesis of sodium / phosphate co-transporters -> ⬆ phosphate absorption.
3. On the kidney:
⬆ Ca2+ reabsorption from the urine -> ⬆ Ca2+ in the blood
⬆ phosphate in the urine
Calcitonin :
Poly-peptid hormone secreted by the C-cells or parafollicular cells of the thyroid gland.
Calcitonin lowers calcium levels in the blood
But
When there is no calcitonin it was noticed that the regulation of blood calcium does not get affected!!
Mechanism of action:
Major effect on the bones
Minor effect on the kidney.
On the bones:
Binds to its receptors on osteoclasts -> activates adenylate cyclase that converts ATP -> cAMP which decreases the arms of osteoclasts (the one they use to eat bones XD) -> ⬇bone resorption and ⬇ blood calcium.
On the kidney: (distal convoluted tubule)
Binds on its receptors on the principal cells -> ⬇ calcium & phosphate reabsorption : Calciuria & phosphaturia.
Part 1 {here}
#studyblr#study motivation#medical student#2020 quarantine challenge#notes#education#medicine#biology#endocrine#endocrinewithmarie#medicinewithmarie#med school#physiology#calcium regulation#calcium and phosphate#bone#glands#thyroid gland#pth#parathyroid glands#vitamin D#health#high yield#endocrine high yield#endocrine notes#science
17 notes
·
View notes
Text
German A1
Part 1
The alphabet : [here]
The personal pronouns:
Notice that in german we have the formal way which is what you use with people that you don't know/boss/teacher etc! And the informal which you use with friends/family/kids..etc.
ich = I wir = we
du = You (informal) ihr= you guys (informal)
Sie = You (formal) sie = They.
er = He
sie = she
The verb to be in german: Sein
I am -> ich bin we are -> wir sind
You are -> du bist You guys are -> ihr seid
He/she/it is -> er/sie/es ist They are -> sie sind.
Sie (formal) sind.
Ex: Ich bin Marie -> I am Marie!
The verb to have in german: Haben
I have -> ich habe we have -> wir haben
You have -> du hast you guys have -> ihr habt
He/she/it has -> er/sie/es hat they have -> sie haben
Sie (formal) haben.
Ex: Er hat ein Auto -> He has a car.
Articles :
Definite articles:
In English we have only one definite article which is 'the' we use it to all nouns whether if the noun is masculine or feminine, singular or plural. But in german we have 3 definite articles for the singular nouns : Der, die and das and one definite article for the plural: die
Der :
Definite article used for singular masculine people and professions.
Ex: Der Mann (the man) , Der Arzt (the doctor)
Some tips to figure out when the word is singular masculine:
1. Months of the year are masculine.
2. Days of the week
3. Seasons
4. Directions
5. Most words that have the following endings:
-el -ich -ig -us -eich -ant -or -ner -ling -er
Ex: Der
6. Words that have the ending -ismus.
7. The following countries: Lebanon, Irak , Iran, suden
Note: The previous endings are just a way to help you memorize the article BUT there are always exceptions so the best way to know the article is to learn each word along with its right article by heart.
So instead of memorizing that 'Elefant' means elephant you can go like this: Der Elefant = the elephant
Die :
Definite article for singular feminine people and professions.
Ex: Die Mutter (the mother)
Some tips to figure out when the word is S.F:
1. Cardinal numbers : Die zwie
2. The words that have the following endings:
-heit -keit -schaft -ung
3. New words that entered the german language and end with :
-ur -ade -age -anz -enz -ik -ion -tät
4. Most words that end with: -e -ei -ie -in
5. The following countries: Türkei, Schweiz, Slowakai.
Das :
When the word is neutral we use DAS!
Das Gold (the gold)
Tips to figure out when the word is neutral:
1. Names of hotels and restaurants.
2. Most nouns starting with -Ge
3. When an infinitive used as a noun: Das Essen (The food)
4. Colors!
5. Words ending with:
-chen -lein -um -ment -nis

#studyblr#study motivation#2020 quarantine challenge#notes#education#germannwithmarie#lesson 1#language#grammar#german#new language#learning german#uni#good vibes#study inspo#study vibes#student#german grammar
5 notes
·
View notes
Text
The Endocrine physiology overview

Part 1
Endocrine glands = Glands that secretes hormones directly into the blood stream= No canal.
Hormones = chemical substances that act on certain cells and guide processes such as: metabolism, growth etc.
The endocrine system in our body has :
Hypothalamus & the pituitary gland
Pineal gland
Thyroid gland
Parathyroid glands
Pancreas
Adreal glands
And the gonads (testes and ovaries)
The hypothalamus:
Nuclei [ supraoptic & paraventricular]
The ceo of the whole system! It senses the information from the body and then reacts by secreting CEO hormones!
The romantic relationship between the hypo and the pituitary:
Between the hypo and the anterior lobe of the pituitary ->
The hypothalamic-hypophyseal portal system (which is a system of blood vessels)
Between the hypo and the posterior lobe of the pituitary ->
The pituitary stalk (which is made by the axons coming from the nuclei in the hypo)
The hypothalamus hormones:
Hormones that affect the cells in the anterior lobe of the pituitary to trigger the secretion of certain hormones :
•- Stimulatory:
TRH = Thyrotropin Releasing Hormone
CRH = corticotropin Releasing Hormone
GNRH = Gonadotropin Releasing Hormone
GHRH= Growth hormone Releasing Hormone.
•- Inhibitory:
GHIH = Growth Hormone Inhibiting Hormone (Somatostatin)
Prolactin Inhibiting Hormone (Dopamine)
Hormones that are secreted by the hypo and stored in the posterior lobe of the pituitary (in Herring bodies) :
ADH (Vasopressin)
Oxytocin
The pituitary gland:
The co-ceo of the endocrine system. Lies in the sella turcica near the hypothalamuc underneath the optic chiasm.
Has two lobes: Anterior and posterior.
The posterior works as a storage for the hypo's two hormones (ADH & oxytocin) that secretes them when needed.
The anterior is made of glandular tissue = is able to produce hormones.
The Pituitary hormones:
ACTH = Adrenocorticotrophic hormone
TSH = Thyroid-stimulating hormone
LH = Luteinising hormone
FSH = Follicle-stimulating hormone.
PRL = Prolactin
GH = Growth hormone
MSH = Melanocyte- stimulating hormone.
Now how do these hormones work?
Now it is a great chance to learn 3 things:
Why the hypothalamus is the ceo?
What is the romantic relationship between it and the pituitary?
And the Endocrine /axes/
So, basically we can recap that like this:
TRH-> TSH-> Thyroid gland -> T4 & T3
CRH-> ACTH-> Adrenal cortex -> Cortisol & androgen
GNRH-> FSH/LH -> Gonads -> sex hormones
GHRH-> GH-> Liver-> IGF-1 / IGF-BP3
Example explained:
TRH stimulates the pituitary to secrete TSH in response to certain conditions and TSH works on certain cells in the thyroid gland (the follicular cells) to activate the producing of T3 & T4 .
What about ADH and oxytocin?
⬇ Blood volume -> ADH -> Distal nephron -> water balance.
Oxytocin = the hormone of motherhood and cuddle!
Motherhood:
- Uterus during delivery = stimulates uterine contractions.
- Breast = During breastfeeding
Cuddle:
Such as social interactions (snuggles~ ) and orgasms!!
The Thyroid Gland:
Butterfly-shaped gland located in the anterior neck just below the laryngeal prominence (adam's apple) . It has left and right lobe wrapping around the trachea and connected in the middle by an isthmus.
Thyroid hormones:
The thyroid gland has many follicles which walls are lined by follicular cells (thyrocytes) that produce:
T4: Triiodothyronine
T3: Thyroxine
Both affect metabolism.
Parafollicular cells (C-cells) produce: Calcitonin
-> calcium and phosphate -> bone metabolism.
Parathyroid glands:
Tiny, round structures found embedded in the posterior surface of the thyroid gland. Most people have 4 parathyroid glands.
Hormones:
PTH = parathyroid hormone -> calcium regulation.
Pineal gland:
Endocrine structure of the diencephalon of the brain . Inferior and posterior to the thalamus. Made of pinealocytes.
Hormones:
Melatonin -> circadian rhythm.
Pancreas:
Located in the abdomen behind the stomach. Has endocrine and a digestive exocrine function.
The endocrine part is called 'Langerhans islets' constitutes about 1-2% of the pancreas volume.
There are five types of cells in these islets:
Beta-> insulin -> ⬇Blood sugar
Alpha -> Glucagon -> ⬆ Blood sugar
PP cells -> pancreatic polypeptide
Delta -> somatostatin -> inhibits the secretion of other pancreatic hormones.
Epsilon -> ghrelin -> 'the hunger hormone'
The Adrenal Glands:
Two small glands located on top of each kidney
Has two parts :
Cortex:
3 Zones:
Zona glomerulosa -> Aldosterone -> ⬆ Blood pressure
Zona Fasciculata -> Cortisol -> Stress & diabetogenic
Zona reticularis -> Androgens.
Medulla:
Epinephrine & norepinephrine -> flight or fight response.
The Gonads:
Ovaries:
Located along the lateral wall of the uterus under the external iliac artery and in front of the internal iliac artery. The region that has the ovaries is called 'the ovarian fossa'
Hormones:
Estrogen : Estradiol, Estrone & Estriol.
Progesterone
Testes :
Oval-shaped organs, contained in the scrotum that hangs outside the body in front of the pelvic region.
Hormones :
Testosterone.
#studyblr#study motivation#medical student#2020 quarantine challenge#medical school#medicine#education#student#notes#biology#endocrinewithmarie#medicinewithmarie#physiology#pathology#the endocrine system#science#endocrine notes#study inspo#human biology#pituitary#medblr#med school#biomedicine#thyroid#human body#usmle#usmle endocrine#med
86 notes
·
View notes