#AntibioticResistance
Text
Did you know that antibiotic resistance is as old as antibiotics themselves?

#TeachingRounds#FOAMed#infectiousdisease#microbiology#bugsanddrugs#antibioticresistance#historyofmedicine#medicalhistory
36 notes
·
View notes
Text
Bacteriophages are viruses that infect and kill bacteria by injecting their genetic material into them. When the bacteriophage DNA or RNA takes over the bacterial cell, it produces more bacteriophages and causes the cell to burst open, releasing the new viruses. This is called lysis.
5 notes
·
View notes
Text
The Dangers of Misusing Antibiotics
Antibiotics are crucial for treating bacterial infections, but their misuse poses serious risks. Taking antibiotics when they aren't needed, such as for viral infections like colds, can lead to antibiotic-resistant bacteria. These resistant bacteria make it harder to treat infections, resulting in longer illnesses and more complicated treatments.
To combat this, healthcare providers, like TGH Urgent Care powered by Fast Track, promote responsible antibiotic use through antibiotic stewardship programs. These programs ensure antibiotics are prescribed only when necessary, reducing the risk of resistance.
Visit: The Dangers Of Misusing Antibiotics
0 notes
Text
A New Era of Healing: Transformative Infectious Disease Therapeutics
Infectious diseases have plagued mankind since antiquity. While public health improvements over the past century have helped control many infectious illnesses, new pathogens continue to emerge and existing ones adapt in the face of globalization and antimicrobial resistance. Researchers have made tremendous progress understanding the biology of infection and developing new therapeutic agents, but more work remains. This article outlines some of the latest advances in infectious disease therapeutics across different disease categories and research areas.
Antibacterial Drug Development
The rise of multidrug-resistant bacteria is a major public health crisis, and the dwindling antibiotic pipeline requires novel solutions. Several new classes of antibacterial agents are under development with activity against resistant pathogens. These include novel ß-lactams that evade extended-spectrum ß-lactamases and novel protein synthesis inhibitors that avoid ribosomal protection mechanisms. Phage therapy is also being revisited, with early clinical studies of engineered phages demonstrating safety and efficacy against difficult-to-treat infections like Pseudomonas aeruginosa and Acinetobacter baumannii. Alternative antibacterial platforms like antimicrobial peptides and small molecule inhibitors of virulence factors also show promise.
Antiviral Drug Discovery
While antibiotics face resistance challenges, antiviral drug development continues making progress against several important viral pathogens. Hepatitis C virus (HCV) represents a major success story, with over 90% cure rates now possible using direct-acting antiviral agents. Research on HIV continues as well, with newer integrase inhibitors and second-generation protease inhibitors demonstrating increased genetic barriers to resistance. Influenza remains a serious threat, but novel cap-dependent endonuclease inhibitors could provide the first truly universal flu drug. For other viruses like herpes simplex, respiratory syncytial virus (RSV)
Pneumococcal Conjugate Vaccines
Streptococcus pneumoniae (pneumococcus) is a leading cause of community-acquired pneumonia as well as invasive pneumococcal disease such as bacteremia and meningitis worldwide. The development of pneumococcal conjugate vaccines (PCVs) targeting the most prevalent disease-causing serotypes has substantially reduced the global burden of pneumococcal disease. PCV7 was first introduced in 2000 and dramatically cut rates of invasive pneumococcal disease in vaccinated children.
Malaria Control Efforts
Malaria remains one of the leading infectious killers globally, with drug and insecticide resistance complicating control efforts. Important infectious disease therapeutics advances include the development of artemisinin-based combination therapies (ACTs) that help delay antimalarial resistance. Novel compounds also aim to complement ACTs through new mechanisms of action. These include the spiroindolone KAE609, which acts on the ATP4 transporter essential for parasite viability, and the Oz439 compound targeting the apicoplast organelle to block isoprenoid biosynthesis. Vaccine progress includes the RTS,S/AS01 candidate demonstrating promising reduction of malaria cases in young children in African clinical trials. Combined with improvements in diagnostics, vector control through insecticide-treated bed nets continues reducing malaria morbidity and mortality worldwide.
Tuberculosis Treatment
Mycobacterium tuberculosis resistance continues complicating tuberculosis (TB) treatment and control globally - about 20% of MDR-TB cases are estimated to further develop extensively drug-resistant TB (XDR-TB). New and repurposed drugs aim to shorten treatment duration for drug-sensitive TB from 6 months to 4 months or less. Regimens including pretomanid, bedaquiline, and delamanid demonstrate potential to treat both drug-sensitive and resistant TB in significantly less time than current guidelines. New anti-TB therapies also target mycobacterial virulence factors and pathways specific to the pathogen. Developing rapid diagnostics to detect drug resistance and evaluating optimized dosing regimens are additionally helping curb the global TB epidemic.
Novel Antifungal Therapies
Life-threatening invasive fungal infections negatively impact public health worldwide, especially in immunocompromised patients. Current antifungal drug classes include azoles, echinocandins, and polyenes, but limitations include toxicities, drug interactions, emerging resistance, and lack of oral options for many serious mycoses. Novel therapies in development aim to overcome these challenges. Novel azoles target the sterol 14α-demethylase enzyme through different binding properties than existing drugs. Echinocandin follow-ups show activity against resistant Candida as well as Aspergillus species.
0 notes
Text
Carmen Leitch - A Tropical Fruit With a Antimicrobial Effects:
BlighiaSapida #Okpu #TropicalFruit #Antimicrobial #AntibioticResistance #Antibiotic #Disease #Pathogenicity #Medicine #PlantBiology #Microbiology #Biology
#blighiasapida#okpu#tropicalfruit#antimicrobial#antibioticresistance#antibiotic#disease#pathogenicity#medicine#plantbiology#microbiology#biology
0 notes
Video
youtube
Understanding Antibiotic Resistance
Antibiotic resistance is a grave concern in healthcare, occurring when bacteria evolve mechanisms to withstand the effects of antibiotics. Overuse and misuse of antibiotics contribute to this phenomenon, leading to the survival and spread of resistant bacteria. Consequently, common infections become more difficult to treat, posing a serious threat to public health. Addressing antibiotic resistance requires a multifaceted approach, including prudent antibiotic use, infection prevention, development of new antibiotics, and global collaboration. It is imperative to act swiftly to preserve the effectiveness of antibiotics and ensure effective treatment for bacterial infections.
#youtube#shorts#short#shortvideo#antibiotics#antibioticresistance#bacteria#superbugs#virus#health#healthcare#awareness#infection#medicine#science#wellbeing
0 notes
Text
#antibioticresistance#guthealth#probiotics#prebiotics#gutmicrobiome#digestivehealth#ibs#constipation#diarrhea#healthygut#healthydigestion#immunesystem#naturalremedies#foodasmedicine#wellness#selfcare#guthealthmatters#probioticsandprebiotics#probioticsforhealth#probioticsforimmunity
0 notes
Text
Dr. Peter Anthony- MBBS
Talking about antibiotic resistance.
Call on our tollfree no + 91 95551 66000 for consulting a doctor
#DrPerteAnthony#raphacure#healthtip#healthcare#wellness#telemedicine#doctoroncall#antibioticresistance#homecollection#IndianHealthCare#covid19#medicine#pharmacy
#DrPerteAnthony#raphacure#healthtip#healthcare#wellness#telemedicine#doctoroncall#antibioticresistance#homecollection#IndianHealthCare#covid19#medicine#pharmacy
0 notes
Text
Scientists Find the Impact of Genes Related to Diseases Such As Autism
#lifestyle#motivation#fitness#health#healthylifestyle#wellness#healthy#antibiotic#antibiotics#antibioticresistance#medicine#microbiology#bacteria#antibioticawareness#Autism
0 notes
Photo

CRE = Carbapenem-Resistant Enterobacteriaceae. Carbapenems are a newer class of beta-lactamase antibiotics; CRE bacteria may also be resistant to unrelated drugs such as fluoroquinolones. Enterobacteriaceae is the name of a family of Gram-negative bacteria (E. coli, Klebsiella, Salmonella, etc.), many of which live in the human gut. Some patients came down with CRE after being scoped with the same endoscope as another patient with CRE in their stomach, intestines, or lungs. This category includes bacteria that have certain resistance factors such as KPC , NDM-1, and VIM. Treat with old and/or toxic drugs such as polymyxins, fosfomycin, and (sometimes) aminoglycosides (susceptibility varies).
• KPC = Klebsiella pneumoniae carbapenemase. A resistance factor that helps bacteria survive carbapenems and other beta-lactamase antibiotics. There was an outbreak in an NIH hospital.
• NDM-1 = New Delhi Metallobeta-lactamase 1. First identified in India and now in 140 countries, this plasmid moves promiscuously among different species of bacteria. Bad news for wound infections, pneumonias, meningitis, and blood infections.
• VIM = Verona Integron-Mediated Metallo-betalactamase. Like NDM-1, makes bugs resistant to beta-lactamase antibiotics such as penicillin or ceftriaxone.
4 notes
·
View notes
Text
Emerging Trends in Veterinary Antibiotics: Europe Market Analysis
The Europe veterinary antibiotics market size is expected to reach USD 1.31 billion by 2030. The rising focus on animal-only antibiotics and ionophores, the launch of new products, and the increasing use of veterinary antibiotics are some of the major factors augmenting the industry's growth. In addition, the rising prevalence and incidence of livestock diseases and concerns regarding zoonoses are further propelling the industry's growth. The COVID-19 pandemic has affected the veterinary antibiotic business operations of key players and resulted in declined financial performance during the initial time.
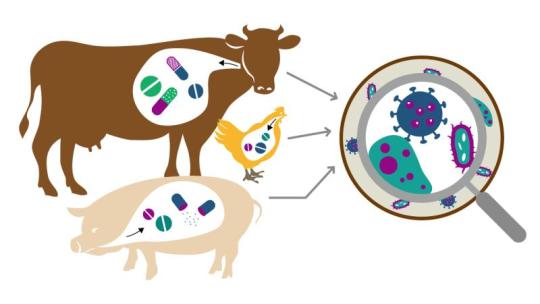
Gain deeper insights on the market and receive your free copy with TOC now @: Europe Veterinary Antibiotics Market Report
The effect of the pandemic with various production and supply chain bottlenecks delayed the delivery of necessary raw materials or active ingredients and postponed certain research & development activities. However, with the easing of restrictions, manufacturers were able to supply antibiotics to meet the necessary veterinary requirements. Few major players have reported significant growth in antibiotic sales despite the pandemic. For instance, Virbac’s bovine antibiotic sales grew from USD 66.98 million in 2020 to USD 79.30 million in 2021. The global concern regarding antibiotic resistance is growing in agriculture and veterinary medicine. Despite the regulatory changes implemented by the European Medicines Agency (EMA) for restriction and ban on routine antibiotic use, the overall sales of veterinary antimicrobial active ingredients have observed significant growth in the past few years.
For instance, according to the EMA, overall veterinary antimicrobial active substance sales grew from 5,282 tonnes in 2019 to 5,562 tonnes in 2020. Furthermore, major players, such as Elanco, have shifted their focus to animal-only antibiotics, as a measure to address antibiotic resistance while also protecting animal health. Key players are implementing various strategic initiatives, such as mergers, partnerships, acquisitions, collaborations, and new product launches, to maintain their competitive edge. For instance, in December 2021, Virbac, in collaboration with Pharmgate, launched Tulissin, an antibiotic solution for swine and cattle with respiratory pathologies. These activities are expected to intensify the competition between major antibiotic manufacturers in the coming years.
#VetAntibiotics#AnimalHealth#VetMedicine#AntibioticResistance#Vet Care#Animal Welfare#Healthy Animals#Vet Pharmacy#Antibiotic Stewardship#Pet Health#Livestock Care#Vet Science#One Health#Sustainable Farming#Animal Treatment#Veterinary Solutions#Antibiotic Awareness#Farm Animal Health#Vet Research
0 notes
Text
#pharmanews#regulatoryupdates#medicalbreakthroughs#healthcareadvancements#innovationinmedicine#DrugApprovals#VaccineProgress#publichealthmatters#globalhealthcare#patientcare#medicalresearch#healthtech#sciencenews#COVID19Updates#FluVaccine#AlzheimersTreatment#CancerImmunotherapy#HIVtreatment#RareDiseaseTherapy#AntibioticResistance
1 note
·
View note
Text
এন্টিবায়োটিক কি কাজ করে ও এন্টিবায়োটিক এর উপকারিতা
#antibioticerupokaritabangla#antibiotics#AntibioticResistance#antibioticsforearinfection#AntibioticResistant#প্রয়োজনআইটি#proyojonit
1 note
·
View note
Text
The Pros and Cons of Using Medicines for Your Health
Medicines have become an integral part of our lives, as they are used to treat various health conditions and improve our overall well-being. However, there are both pros and cons to using medicines, and it's important to understand them before making a decision to take them.
Pros of using medicines:
Medicines can help alleviate pain and discomfort caused by certain health conditions.
They can help manage chronic illnesses, such as diabetes, hypertension, and asthma, allowing patients to lead a better quality of life.
Some medicines can prevent the progression of certain diseases, such as statins that lower cholesterol levels and reduce the risk of heart disease.
They can also save lives in emergency situations, such as epinephrine injections for severe allergic reactions.
Cons of using medicines:
Medicines can have side effects, ranging from mild to severe, which can impact a person's quality of life and even lead to hospitalization.
Overuse or misuse of medicines can lead to addiction, antibiotic resistance, and other health problems.
Some medicines can interact with other medications, causing adverse effects.
There is also the risk of counterfeit or fake medicines that can be harmful to health.
It's important to weigh the pros and cons of using medicines before making a decision, and to always follow your doctor's advice regarding their use.
For a pharmacy view point: https://bit.ly/3mcBksn
#medicines#health#naturalremedies#wellness#prescriptiondrugs#overthecounter#sideeffects#druginteraction#chronicillness#painmanagement#healthylifestyle#selfcare#mentalhealth#emergencytreatment#fakemedicines#drugabuse#antibioticresistance#alternativehealthcare#acupuncture#meditation#people#cooperpharma#nutrition#healthcare#education#workout#nevergiveup#bodybuilding
0 notes
Video
youtube
Understanding Antibiotic Resistance
In the world of modern medicine, antibiotics have long been heralded as miracle drugs, capable of combating bacterial infections and saving countless lives. However, as their use has become widespread, a new and ominous threat has emerged: antibiotic resistance. This phenomenon occurs when bacteria develop the ability to withstand the effects of antibiotics, rendering these life-saving medications ineffective. Understanding the intricacies of antibiotic resistance is crucial for tackling this growing global health concern.
What are Antibiotics and How Do They Work?
Antibiotics are medications designed to treat bacterial infections by targeting specific components or processes within bacterial cells. They work by either killing bacteria outright (bactericidal) or inhibiting their growth (bacteriostatic). Common targets include bacterial cell walls, protein synthesis machinery, or metabolic pathways. By disrupting these essential bacterial functions, antibiotics weaken or eliminate the bacteria, allowing the body's immune system to effectively clear the infection.
The Mechanisms of Antibiotic Resistance
Antibiotic resistance is a natural evolutionary process that occurs when bacteria develop mechanisms to resist the effects of antibiotics. These mechanisms can vary widely depending on the type of antibiotic and the specific bacteria involved. One common mechanism involves the modification of antibiotic targets, rendering them ineffective. For example, bacteria may alter the structure of the protein targeted by the antibiotic, preventing the drug from binding and exerting its effects. Another mechanism involves the production of enzymes that degrade or modify the antibiotic, rendering it harmless to the bacteria. Additionally, bacteria can develop efflux pumps that actively remove antibiotics from the cell, reducing their concentration to subtherapeutic levels.
Causes of Antibiotic Resistance
The rise of antibiotic resistance can be attributed to a multitude of factors, but one of the primary drivers is the overuse and misuse of antibiotics. In human medicine, antibiotics are often prescribed unnecessarily for viral infections, against which they are ineffective. Patients may also fail to complete their prescribed antibiotic courses, leading to incomplete eradication of the infection and potential development of resistance. Furthermore, antibiotics are extensively used in agriculture to promote growth and prevent disease in livestock. This agricultural use of antibiotics creates selective pressure, favoring the emergence of resistant bacteria that can spread to humans through food, water, or direct contact.
Consequences of Antibiotic Resistance
The consequences of antibiotic resistance are far-reaching and profound. Infections caused by resistant bacteria are associated with increased morbidity, mortality, and healthcare costs. Common infections, such as urinary tract infections, pneumonia, and skin infections, are becoming increasingly difficult to treat due to antibiotic resistance. In severe cases, infections may become untreatable, leading to prolonged illness, disability, and death. Moreover, the emergence of multidrug-resistant bacteria complicates treatment options, leaving healthcare providers with limited or no effective antibiotics to combat infections.
Global Impact of Antibiotic Resistance
Antibiotic resistance is a global health crisis that transcends geographical boundaries. It affects people of all ages, genders, and socio-economic backgrounds. Low and middle-income countries are particularly vulnerable due to limited access to healthcare, inadequate sanitation, and over-the-counter availability of antibiotics. However, antibiotic resistance knows no borders, with resistant bacteria capable of spreading rapidly through international travel and trade. The interconnected nature of our world necessitates coordinated efforts at the global level to address this urgent threat.
Addressing Antibiotic Resistance
Combatting antibiotic resistance requires a multifaceted and coordinated approach involving various stakeholders, including healthcare professionals, policymakers, researchers, and the public. Key strategies include promoting responsible antibiotic use through education and stewardship programs, implementing infection prevention and control measures in healthcare settings, investing in research and development of new antibiotics and alternative therapies, and fostering global collaboration to share data, resources, and best practices. Additionally, raising public awareness about the importance of prudent antibiotic use and the consequences of resistance can empower individuals to take action in their communities.
Conclusion
Antibiotic resistance poses a significant threat to public health, requiring urgent and concerted action from all sectors of society. By understanding the mechanisms, causes, and consequences of antibiotic resistance, we can work together to preserve the effectiveness of antibiotics for future generations. Through responsible antibiotic use, infection prevention, research, and global collaboration, we can mitigate the impact of antibiotic resistance and safeguard the effectiveness of these life-saving medications. The time to act is now, for the sake of our health and the health of generations to come. Let us join forces to combat antibiotic resistance and ensure a healthier, safer future for all.
#youtube#antibiotics#antibioticresistance#bacteria#superbugs#virus#health#healthcare#awareness#infection#medicine#science#wellbeing#publichealth#wellness#bactericidal
0 notes
Text
"Shigella on the rise: Antibiotic-resistant diarrhea poses a growing threat to public health" #AntibioticResistance #PublicHealth #ShigellaOutbreak
“Shigella on the rise: Antibiotic-resistant diarrhea poses a growing threat to public health” #AntibioticResistance #PublicHealth #ShigellaOutbreak
The NPR article discusses a growing concern regarding the spread of antibiotic-resistant Shigella bacteria. Shigella is a bacteria that causes diarrhea, and the article explains that it is becoming increasingly difficult to treat due to its ability to…

View On WordPress
0 notes