#Antiretroviral Therapy
Text
Immunomodulators' Power: Widening Applications and Medical Impact
Immunomodulators have emerged as crucial components in the field of medicine, gaining increasing attention for their ability to regulate and modify the immune system’s responses. These agents play a pivotal role in treating a diverse range of conditions, from autoimmune diseases and cancer to infectious diseases and organ transplants. By modulating immune responses, immunomodulators offer…

View On WordPress
#Allergies#Anti-Inflammatory Medications#Antiretroviral Therapy#Autoimmune Diseases#Cancer Treatment#Cytokinesis#Immunomodulators#Immunomodulators Applications#Immunomodulators Market#Infectious Diseases#Organ Transplants#Rheumatoid Arthritis#Vaccines
1 note
·
View note
Text
#The ART Of Life After HIV: HIV & Antiretroviral Therapy (ART)#Antiretroviral Therapy#Antiretroviral Therapy For HIV#Antiretroviral Therapy HIV Treatment
1 note
·
View note
Text
Is HIV treatment possible?
Is HIV treatment possible?
Very few people have been reported to be ‘cured’ of HIV. Read what researchers learn from them.
.

View On WordPress
1 note
·
View note
Text
HIV/AIDs Research and Treatment Breakthroughs
Explore the latest breakthroughs in HIV/AIDS research and treatment, that have the potential to reshape the landscape of HIV/AIDS management.
#"HIV/AIDS Research and Treatment#HIV Care#HIV Cure Research#Antiretroviral therapies#current research on HIV/AIDS#CME Programs#CME Conferences#CME Medical courses#CME credits#doctor conferences#medical CME#Primary Care Conference#Medical CME Online#Emergency Medicine Online CME#Medical Conference Website#Physician Conferences#Medical CME Courses#Doctors CME Conferences#CME training for Physicians#Medical Event Organizer#Organizing Medical Events#Medical Conferences#Medical Speakers#Healthcare Marketplace
1 note
·
View note
Text
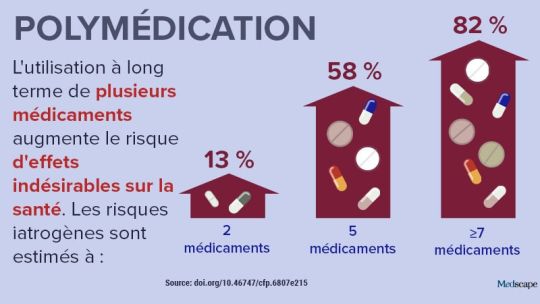
In the news: polypharmacy
In the news: polypharmacy
Polypharmacy, or the daily use of several drugs, is increasingly common and remains associated with significant health risks (see infographic). Recent studies have examined the benefits of interventions to reduce this polypharmacy, as well as the conditions associated with the use of multiple drugs.
Impact of interventions to reduce polypharmacy
A new study showed that strategies aimed at…
View On WordPress
#antiretroviral (HIV) treatment; antiretroviral therapy (ART) for#back pain#HIV#HIV infection#multiple sclerosis (MS); multiple sclerosis; MS (multiple sclerosis)
0 notes
Photo

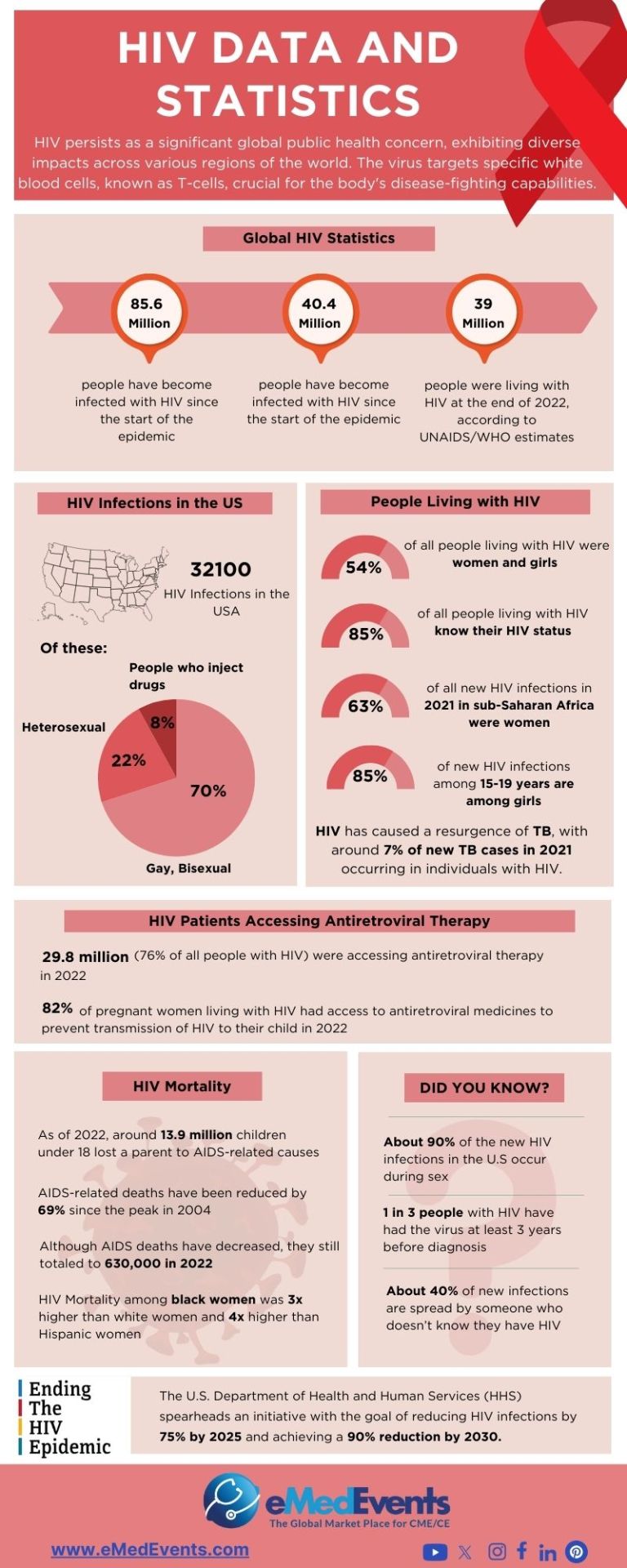
Today marks #WorldAIDSDay, a time to show support for people living with #HIV and those who lost their lives to AIDS.
First commemorated in 1988, World AIDS Day raises awareness to end the spread of HIV and the stigma and discrimination that surrounds it.
Despite the progress made, HIV is still a major public health threat globally. In 2021, there were 1.5 million new HIV infections. In particular, girls in sub-Saharan Africa continue to be disproportionately affected by HIV, accounting for 63% of the region's new HIV infections in 2021.
However, it's important to know that in our modern era, people with HIV live long and happy lives thanks to access to antiretroviral therapy (ART). People living with HIV deserve care, not punishment.
To end AIDS, we must look and address underlying inequalities. Solutions include:
Increase availability of HIV testing, treatment and prevention (such as PrEP).
Reform laws and policies that perpetuate the stigma and exclusion of people living with HIV.
Ensure equal access to the best HIV science, between the Global South and North.
Collaboration with UNFPA
[Digital illustration of a Black fem with long curly hair. She’s wearing a white shirt that reads, “Living with HIV doesn't define me.” She’s also wearing gray jeans, a red ribbon and a black choker necklace. Behind her is a sky of gray clouds and a moon.]
#art#feminism#feminist#global health#HIV/AIDS#hiv#sti#sex ed#world aids day#aids#public health#health justice#feminist art
681 notes
·
View notes
Text
"Five people have gone into remission thanks to advancements in medicine — and a sixth patient may also now be free of HIV.
One of the biggest breakthroughs in HIV/AIDS prevention in recent years is the widespread use of PrEP (pre-exposure prophylaxis).
This drug therapy, approved by the Federal Drug Administration in 2012, has been a key player in preventing HIV transmission through sex or injection drug use. Antiretroviral drugs, such as PrEP, also slow the replication of the virus and prevent it from progressing to AIDS.
Although PrEP has become a more accessible treatment for the virus, scientists have been hurriedly working towards cures for HIV for decades — and we’re finally seeing some results.
In February of this year, scientists in Germany confirmed a fifth-ever patient had been cured of HIV after receiving stem cell transplants that include genetic mutations that carry a resistance to HIV.
But it looks like a sixth patient may soon be able to join this very exclusive club.
The man, referred to as the “Geneva patient,” underwent a stem cell transplant after cancer treatment, though these cells did not include the HIV-resistant genetic mutation.
Still, he went off antiretroviral therapy for HIV in November 2021, and his viral load remains undetectable.
Instead, doctors are researching whether a drug called ruxolitinib may be partially responsible for his recovery.
Ruxolitinib decreases inflammation associated with HIV by blocking two proteins, JAK1 and JAK2. This helps kill off “reservoir cells” that lay dormant in the body and have a potential to cause rebounds in patients with HIV.
Experts say the AIDS crisis can end by 2030 across the globe — as long as leaders prioritize this goal.
A new report from UNAIDS shows a clear, optimistic path to ending the AIDS crisis. (This looks like a 90% reduction in cases by 2030.)
The organization’s report includes data and case studies that show that ending AIDS is a political and financial choice — and that governments that have prioritized a path towards progress are seeing extraordinary results.
By following the data, science, and evidence; tackling inequality; and ensuring sufficient and sustainable funding across communities, the global community could wipe out the AIDS pandemic by the end of the decade.
The report demonstrates that progress has been strongest in the countries and regions that have the most financial investments, like eastern and southern Africa, where new HIV infections have been reduced by 57% since 2010.
Investments in treatments, education, and access to care have also led to a 58% reduction in new HIV infections among children from 2010 to 2022 — the lowest number since the 1980’s.
Plus, the number of people on antiretroviral treatment around the globe has risen from 7.7 million in 2010 to 29.8 million in 2022.
The moral of the story? This goal can be achieved, if world leaders put their minds — and wallets — to it.
A region in Australia might be the first place in the world to reach the United Nations targets for ending HIV transmission.
Researchers believe that the central district of Sydney, Australia is close to becoming the first locality in the world to reach the UN’s target for ending transmission of HIV.
Specifically, new infections among gay men have fallen by 88% between 2010 and 2022. In fact, there were only 11 new HIV cases recorded in central Sydney last year, and almost all HIV-positive Australians are on antiretroviral drugs.
... "These numbers show us that virtual elimination of HIV transmissions is possible. Now, we need to look closely at what has worked in Sydney, and adapt it for other cities and regions across Australia.”
Namibia is ahead of schedule in UN targets to end HIV/AIDS.
Although the virus is still the leading cause of death in Namibia, the country is well on track to hit 95-95-95 UNAIDS targets before its 2030 deadline.
In Namibia, 92% of people know their HIV status, 99% of people living with HIV are on treatment, and 94% of people living with HIV who are on treatment are virally suppressed.
In addition to these exciting statistics, new infections have plummeted. The estimated rate of new HIV infections in Namibia is five times lower than it was in 2002, according to the Centers for Disease Control & Prevention.
These encouraging numbers are thanks to the investment and strategic response of PEPFAR, but also to the willingness of local governmental agencies and organizations to adhere to the UN’s Fast-Track approach.
Breakthroughs are being made in HIV vaccine therapies.
Long before we were all asking each other “Pfizer or Moderna?” about our COVID-19 vaccines, scientists have been researching the potential of mRNA vaccines in treating some of the world’s deadliest diseases — like HIV.
And with the success of our mainstream mRNA vaccines, an HIV inoculation remains a goal for researchers across the globe.
Last year, the National Institutes of Health launched a clinical trial of three mRNA vaccines for HIV, and similar studies are being conducted in Rwanda and South Africa, as well.
CAR T-cell clinical trials are underway to potentially cure HIV.
This spring, UC Davis Health researchers have dosed the second participant in their clinical trial, which poses the use of CAR T-cell therapy as a potential cure for HIV.
The study involves taking a participant’s own white blood cells (called T-cells), and modifying them so they can identify and target HIV cells, ultimately controlling the virus without medication.
The first participant in the study was dosed with anti-HIV T-cells last August, and the trial is the first of its kind to utilize this technology to potentially treat HIV.
Of course, the trials have a long way to go, and the lab is still preparing to dose a third participant for the study, but CAR T-cell treatments have been successful for lupus and forms of cancer in the past...
“So far, there have been no adverse events observed that were related to the treatment, and the two participants are doing fine.”
Guidance on how to reduce stigma and discrimination due to HIV/AIDS is reaching people around the globe.
While the stigma surrounding HIV and AIDS has significantly decreased — especially towards the LGBTQ+ community — with advancements in treatment and prevention, discrimination is certainly not gone.
While most people now understand HIV/AIDS better than they did decades ago, those most impacted by the virus (like gay men and low-income women and children) still face ongoing barriers to care and economic security.
It is vital to maintain awareness and education interventions.
After all, experts suggest that eliminating discrimination and stigma are key factors in reducing disease. And not eliminating stigma impedes HIV services, argues UNAIDS, “limiting access to and acceptance of prevention services, engagement in care, and adherence to antiretroviral therapy.”
Luckily, UNAIDS provides guidance on how to reduce stigma and discrimination in the community, workplace, education, health care, justice, and emergency settings.
The goal is to, of course, decrease stigma in order to decrease disease, but also to provide folks with the culturally significant support they need to live safe, integrated lives — with or without disease.
For instance, a 2022 study conducted in Northern Uganda showed that local cultural knowledge passed through Elders was a successful intervention in reducing HIV-related stigma among young people.
“Research in school settings has shown that the use of local cultural stories, songs, myths, riddles, and proverbs increases resilient coping responses among students and strengthens positive and socially accepted morals and values,” the study’s discussion reads.
So, while an uptick in acceptance gives us hope, it also gives us a directive: Keep telling the accurate, full, and human stories behind HIV/AIDS, and we’ll all be better for it. "
-via GoodGoodGood, August 3, 2023
#hiv#hiv/aids#aids crisis#public health#medical research#vaccines#australia#namibia#united nations#queer issues#trans issues#lgbtq issues#lgbtq community#infection prevention#good news#hope
268 notes
·
View notes
Text


World AIDs Day - December 1st.
Global HIV statistics
🎀 38.4 million [33.9 million–43.8 million] people globally were living with HIV in 2021.
🎀 1.5 million [1.1 million–2.0 million] people became newly infected with HIV in 2021.
🎀 650 000 [510 000–860 000] people died from AIDS-related illnesses in 2021.
🎀 28.7 million people were accessing antiretroviral therapy in 2021.
🎀 84.2 million [64.0 million–113.0 million] people have become infected with HIV since the start of the epidemic.
🎀 40.1 million [33.6 million–48.6million] people have died from AIDS-related illnesses since the start of the epidemic.
╔═.✵.══════════╗
🄼🅈 🄻🄸🄽🄺🅂
╚══════════.✵.═╝
50 notes
·
View notes
Text
It is spelt AIDS, which can be stylised to Aids - it is not a plural, it stands for Acquired Immune Deficciency Syndrome. HIV stands for Human Immunodeficiency Virus.
You cannot transmit AIDS to somebody else. HIV is the one which is transmitted; AIDS comes as a result of untreated HIV. We have no cure for HIV, but we do have treatments.
It is very rare for somebody to become diagnosed with AIDS in today's modern world, as HIV treatment has gotten incredibly effective.
PEP (Post-Exposure Prophylaxis) is taken within three days of exposure to the virus, and is an emergency measure which can stop the virus from taking hold. PEP is taken AFTER exposure.
PrEP (Pre-Exposure Prophylaxis) reduces the chance of getting HIV by stopping the virus from replicating before it can take hold; you take it before risk of exposure. PrEP is taken BEFORE exposure.
ART (Antiretroviral therapy) is taken by people living with HIV; it surpresses the virus, which stop the virus from replicating. This is taken every day, to try to make the Viral Load as low as possible - that is to have a low amount of HIV virus in your body. The end goal is for tests to come back negative - Undetectable equals Untransmittable (U=U) - if it cannot be detected by tests, it cannot me transmitted.
Go forth, spell it correctly. And donate to THT, whilst you're at it - THT is a wonderful organisation which offers HIV testing, post-HIV living advice, and does other important work for our wonderful community, such as their incredible non-judgemental chemsex support group.
6 notes
·
View notes
Text
The first time I heard the euro-pop sensation Aqua’s Barbie Girl was in the summer of 1997, at a party We The People organized in Clementon Park, New Jersey. The DJ was mixing bona fide house hits with contemporary jams. I remember this so vividly because I watched someone do “hand performance” to the song that was a newly minted hit. This was also one of those moments that I definitely knew I was gay because I felt like Barbie Girl was composed for LGBTQ folks; not sure how I came to that conclusion, but it just felt gay. I was 13 years old, journeying through puberty and trying to understand myself, but I recognized the subtle ways queer culture could be found in pop music. And now, more than 25 years since I first heard Barbie Girl, it remains a song that resonates and reminds me of what is remembered, who has gone, and the richness of their lives.
We The People was an AIDS service organization in Philadelphia, serving the most vulnerable HIV positive community, and my mother Melody E. Beverly worked there. Most of the organization’s service population was Black and brown people, people who inject drugs, and housing-insecure people with an AIDS diagnosis. It had a brick-and-mortar building at the corner of Broad and Lombard Street. Now a Taqueria with its own controversial history, at the end of the 1990s, it held precious work of caring for the community, with housing units atop, with an industrial-style kitchen. I remember this because I loved volunteering with building residents, preparing and cooking meals. I also had a thing for the biscuits that were often there.

On a hot day in the summer of ‘97, my mother and I arrived to begin boarding a bus to head over to the party at Clementon Park, which also included barbeque. While waiting to board the bus, I overheard Curtis speaking to a Black man who seemed exhausted if he had been taking AZT. This was a year after HAART was established as a standard for HIV care, and people were taking what we now know to be toxic medicine to manage their HIV. The introduction of highly active antiretroviral therapy, or combination therapy, would mean that people who had been living with HIV could live longer lives. I always think about that moment of Curtis checking in with a community member about his health when navigating my own care. I still appreciate the way it was normalized as a communal approach to medicine adherence. Curtis was my mother’s supervisor. He was a charismatic Black gay man with a bald head. Curtis was the sweetest and most sincere person. He was also a drag performer, I had seen him perform for a holiday party and was in awe of him.
youtube
Aqua, a Danish musical group, released their single Barbie Girl in April 1997, from their debut album Aquarium that was released in March of the same year. The track has a synth-pop-house vibe to it, with bubblegum vocals from lead singer Lene, who plays Barbie in the music video for the song. René, another band member, plays Ken, in a campy and hilarious capture of a Barbie world; it does a beautiful job of both bringing humanity to a plastic doll and making the cringey nature of American consumerism visible in a funny way. This is ironic, because during a 2017 interview for Nylon Lene disclaims its politics and sexist overtones by stating that “it was kind of making fun of the Pamela Anderson kind-of girl” and says the song is “super-innocent.” To me, Barbie Girl now appears to be making a statement about bodily autonomy and misogyny. With the incessant lyric, “I’m a Barbie girl, in a Barbie world.” This song makes me think about people who lived with HIV, like Curtis, who were living full and flourishing lives at a tender and promising point in the ongoing AIDS crisis.
Barbie Girl topped global charts and was part of a musical era that included the resurgence of unapologetic bubblegum pop music, led in part by the Spice Girls’ Wannabe, a year earlier. Barbie Girl peaked at number 7 on the US Billboard Hot 100.
youtube
Now the song has a new life in the context of Barbie, the anticipated movie featuring Margot Robbie as the title character original Barbie. Barbie World, a rap track by Nicki Minaj & Ice Spice for the Barbie soundtrack, samples Barbie Girl in a perfect way. I’m most certain Barbie Girl will have a second life on TikTok and a new generation will be embraced by the gummy-gayness of late nineties music, and remember that there were people who existed then, plagued by an epidemic that rendered their stories untold. They too are Barbie Girls, even in their afterworlds, they paved the way for us to live fantastically in the skin we’re in.
Signed, a Barbie Girl from the nineties.
I’m always yours Xx
Abdul-Aily Muhammad ( @mxabdulaliy )
They/Them/Thiers
gran varones Mentor
Philadelphia, PA
#granvarones#gay#queer#storytelling#lgbtqia#non binary#barbie#barbie girl#songs that soundtracked the aids epidemic#Youtube
7 notes
·
View notes
Text
Very early treatment of newborns with HIV could result in medication-free remission for many babies.
An unexpectedly high percentage of children, who were born with HIV and started treatment within 48 hours of life, exhibit biomarkers by 2 years of age that may make them eligible to test for medication-free remission, according to a multinational study published in Lancet HIV.
“Moving away from reliance on daily antiretroviral therapy (ART) to control HIV would be a huge improvement to the…

View On WordPress
2 notes
·
View notes
Text
MMWR Booster #16: HIV Services and Outcomes During the COVID-19 Pandemic — United States, 2019–2021
Top 5 Takeaways
HIV Testing and PrEP Prescriptions Decreased Then Rebounded: In 2020, a decline in HIV testing and preexposure prophylaxis (PrEP) prescriptions was observed in the first half of the year, followed by a rebound.
Stable HIV Care and Treatment: Despite initial disruptions, the number of persons linked to HIV care, prescribed antiretroviral therapy (ART), and achieving viral load suppression remained stable.
Impact of COVID-19 Pandemic: The COVID-19 pandemic, leading to the closure of health care venues and loss of health insurance, significantly impacted HIV services.
Innovative Service Delivery Models Needed: The pandemic highlighted the need for alternative HIV service delivery models, including telehealth and nonclinical settings.
Resilience in HIV Prevention and Care System: Despite early disruptions, the system showed resilience with a return to pre-pandemic trends in PrEP prescriptions and maintenance of ART services.
Full summary link: BroadlyEpi.com
Enjoying these summaries? Check back every day at 8am and 4pm Pacific Time (UTC - 8) for a new MMWR Booster. A reblog would also be greatly appreciated, and thanks to everyone who already has! BroadlyEpi hopes to make Epidemiology and Public Health more approachable to anyone who's interested.
2 notes
·
View notes
Text
Antiretroviral Drugs and Benefits

What are Antiretroviral Drugs?
The antiretroviral drugs are used in the treatment of HIV infection. Combination of various HIV drugs are used to treat individuals infected with the human immunodeficiency virus (HIV). These medications can inhibit HIV replication with conventional treatment, commonly referred to as "highly active antiretroviral therapy" or HAART. The purpose of the medicine combination is to boost efficiency and lower the risk of resistance development in the virus. HIV-positive individuals who receive Antiretroviral Treatment (ART) have lower rates of death and morbidity and a higher quality of life. As it suppresses HIV replication in infected individuals and also prevents HIV from spreading.
Start Medication Immediately After a Diagnosis Is Best
The first big step in treating HIV is to begin antiretroviral therapy. Initially, it could be frightening or annoying to have to take medicine every day for the rest of your life.
However, patients with HIV can anticipate living long lives after starting antiretroviral drugs. This is due to ART's ability to halt the virus's replication.
ART is not a treatment. However, it dramatically reduces the chance of contracting potentially fatal opportunistic infections.
Antiretroviral drugs can actually reduce the viral load to the point where it is no longer observable in the blood. You can keep your viral load undetectable with ongoing treatment. As a result, sexual activity is not a means of spreading the infection.
Importance of Examination and Test
It is possible to become infected and not feel at all. You won't experience the virus spreading. However, in the first six months, the viral load might increase significantly if treatment is not received. We refer to this as "acute infection."
This increases your susceptibility to more infections and ailments. You run the risk of spreading HIV if you engage in sexual activity.
Take an immediate HIV test if you think you may have been exposed to the virus. Initiating therapy during the acute phase can assist in reducing the viral load prior to illness or transmission of the infection to others.
Advantages of Early Treatment
According to studies, three-drug therapy has reduced the rates of AIDS, hospitalization, and death by 60% to 80%. The CDC wants to be 90-90-90 by 2030 (i.e., 90% on medication, 90% suppressed, 90% diagnosed with HIV). Stopping HIV from spreading is the aim of HIV medications.
Antiretroviral drugs can significantly lower your body's viral load. However, it may take up to six months for ART to reduce the viral load to an undetectable level.
An HIV viral load that is low or undetectable enhances the ability of your immune system to defend itself against disease.
According to research, individuals living with HIV can improve their health by beginning antiretroviral treatment (ART) as soon as they are diagnosed.
ART users who maintain an undetectable viral load are unable to sexually transfer the virus to other people.
Conclusion
The discovery of HIV can change your life. However, antiretroviral treatment (ART) has greatly enhanced expectancy and enabled a long, healthy life with HIV.
So, experts recommend starting ART as soon as possible after diagnosis. Antiretroviral treatment has the ability to reduce the viral load to an undetectable level, so rendering it non-transmittable. Your immune system will be more capable of fighting off other infections and diseases if your viral load is undetectable.
Get tested if you believe you may have been exposed to HIV. Also, think about beginning treatment straight away if your test results are positive. See your doctor about any worries you may have. You can decide on the most effective HIV treatment plan together.
Title- The Benefit of Antiretroviral Drugs
Meta Description- The antiretroviral drugs are used in the treatment of HIV infection. They are combination of highly effective medications. We are going to analysis more about these drugs in this blog
2 notes
·
View notes
Text
Can you breastfeed if you have HIV?
Can you breastfeed if you have HIV?
Baby food is recommended for mothers with HIV in the US because of the small chance that babies will contract HIV through breast milk.
Women with HIV who are on antiretroviral therapy and who have an undetectable viral load can have HIV-free babies. They may see ‘breast is best’ posters in their doctor’s office and want to breastfeed their babies. But they may not think it’s an option for…
View On WordPress
0 notes
Text
Since the start of Russia’s full-scale invasion of Ukraine, more than 62,000 Russians and 20,000 Ukrainians have relocated to Georgia. Meanwhile, Georgia itself has seen a rise in HIV infections, with almost 400 new cases reported in the first eight months of 2023, despite having been lauded among European countries for its effective HIV and AIDS policies in recent years. This has led some Georgian doctors and media outlets to attribute the worsening HIV situation to the wartime influx of Russian and Ukrainian migrants — the latest iteration of a theory that’s found resonance in a number of countries, particularly among conservative politicians. Meduza takes a look at the reasons behind the widespread popularity of this dubious hypothesis.
A lack of evidence
In late June, Professor Maya Butsashvili, an infectious disease specialist who works at Tbilisi’s NEOLAB clinic, expressed concern on Facebook regarding the large number of Russians entering the country. Arguing that Russia was grappling with an HIV epidemic and that unprotected sexual encounters between local residents and migrants could lead to an increase in HIV infections in Georgia, she urged officials to remind citizens about safe practices to avoid sexually transmitted infections.
Shortly after, Tengiz Tsertsvadze, the director of Georgia's main infectious disease hospital, said that Butsashvili's theory “had some truth to it” but suggested that the increase in cases might have “less to do with the influx of migrants and more to do with the end of the COVID-19 pandemic, the lifting of restrictions, and an increase in testing.” He noted that since the wartime migration of Russian and Ukrainian citizens had begun, Georgia’s HIV and AIDS Control Service had intensified its surveillance and implemented measures for prevention and treatment. Tsertsvadze also emphasized the importance of only using sterile medical instruments and avoiding unprotected sexual contact, encouraging those with suspected infections to seek medical assistance.
Nonetheless, Butsashvili remained firm in her stance, insisting that migrants were a “high-risk group.” In August, she recommended a policy of mandatory HIV testing for people entering the country and urged local residents to “abstain from unprotected sexual contact.”
Butsashvili, whose Facebook page has some 7,000 followers, has been widely quoted in the Georgian media for her statements, especially during the COVID-19 pandemic. Her opinions on the role of migrants in HIV transmission have sparked huge debates across social media platforms. According to her profile, she studied epidemiology at the State University of New York and is currently a faculty member at the University of Georgia.
Skewed by the pandemic
Georgia was seeing record spikes in HIV rates well before the recent influx of migrants from Russia began. In 2018, for instance, the country identified 672 new HIV cases, while it saw 719 in 2016, which remains the highest year on record. In 2022, 617 new cases were recorded, and in the first eight months of this year, 393 cases were confirmed.
In August 2023, the total number of HIV infections in Georgia reached 10,170, with the majority of cases in Tbilisi (3,830). According to the Georgian Center for Research of Infectious Diseases and AIDS, the virus is transmitted primarily through heterosexual contact (51.4%) and intravenous drug use (32.6%). HIV prevalence in Georgia, at 0.27% of the total population, is substantially lower than in Russia (0.8%) and Ukraine (approximately 0.55%).
Georgia's HIV and AIDS policy, according to WHO estimates, has been one of the most effective in Europe. The country introduced antiretroviral therapy (ARV therapy) in the 1990s and ensured universal access in the 2000s, significantly reducing AIDS-related mortality. In 2011, Georgia established a national AIDS information system, creating a comprehensive database of demographic, epidemiological, clinical and laboratory data on all AIDS patients. The government also actively promotes ARV therapy and health services for all, regardless of gender, ethnicity, or viral load.
Despite these efforts, Georgia fell short of its goal to provide ARV therapy to 90% of the infected population by 2020, with only 76% of virus carriers knowing their status and only 65% receiving ARV therapy. Even fewer individuals (65% of those on therapy) have managed to suppress the virus's activity.
A more plausible explanation
One epidemiologist, who asked to remain anonymous for security reasons, acknowledged that Russia and Ukraine have significant HIV epidemics and that migrants are a particularly vulnerable group. But at the same time, he said, Georgia’s rise in infections cannot be unequivocally attributed to the influx in migrants without a comprehensive analysis of the epidemiological data.
The Georgian Center for Infectious Diseases and AIDS Research reported more HIV cases in 2022 than in 2020 and 2021. However, this increase could be attributed at least in part to reduced testing during the COVID-19 pandemic, when resources were diverted to coronavirus prevention efforts.
The epidemiologist further explained that there’s little to no evidence that compulsory testing, entry restrictions, or deportation are effective public health measures. In fact, such measures may even hinder HIV prevention and treatment as they make individuals more likely to hide their status, avoid seeking help, and then propagate the virus as a result.
The U.N.’s note on HIV/AIDS and the Protection of Refugees states:
Detention or restrictions on the freedom of movement of persons living with HIV and AIDS would be in violation of the fundamental rights to liberty and security of the person, as well as the right to freedom of movement, if carried out solely on the basis of a person’s actual or suspected HIV status. There is no public health justification for restrictions of these rights due to a person’s HIV status alone. Moreover such restrictions would be discriminatory.
In Russia, however, it remains legally permissible to deport migrants based solely on their HIV status. In 2021, Fedot Tumusov, a deputy from the political party “A Just Russia — For Truth,” proposed a bill to abolish these measures due to their lack of effectiveness, but the State Duma ignored his proposal. According to the head of one public organization that works with individuals affected by HIV in Eastern Europe and Central Asia, who asked to remain anonymous, there’s no reasonable basis for a country to deport foreigners with HIV. Many developed countries have already repealed such laws.
An easy scapegoat
One human rights activist who specialises in HIV issues and wished to maintain anonymity told Meduza that the practice of blaming migrants, a vulnerable group, for various societal problems is not unique to Georgia; it’s a common rhetorical move employed by conservative political figures worldwide. In Georgia, she argued, negative sentiments regarding migrants may have been exacerbated by the strain on public health and the surge in migration caused by the war, leading to concerns and frustrations among local residents that politicians can exploit for political gain.
Georgian political scientist Gela Vasadze has also suggested that accusing migrants of spreading HIV may be an element of the political campaigns of right-wing opposition parties in the upcoming 2024 elections. He told the outlet Paper Kartuli that the Georgian authorities should address the migration crisis by reducing the stay period of visitors with uncertain legal status and making it easier for migrants to obtain residence permits.
According to the anonymous human rights activist, migrants are a vulnerable group with limited political and civil rights, which makes them easy scapegoats for various social problems. This phenomenon is not unique to Georgia but is a broader issue tied to policies and levels of tension within countries.
Russia is no exception: it, too, has a long history of public figures making public health-related xenophobic statements. In 2009, for example, the country’s then-Chief Health Inspector, Gennady Onishchenko, alleged that migrants “contribute significantly to the HIV and AIDS epidemic.” Similar sentiments were echoed in 2012, when the chairman of the Moscow City Duma’s healthcare commission, Lyudmila Stebenkova, proposed putting out public service announcements to warn Muscovites about the risk of contracting HIV from migrants.
Over the past two decades, however, Georgia has been decidedly receptive to international recommendations, focusing on testing and treatment while avoiding discriminatory policies. Anyone who’s in the country legally has the right to receive assistance, including refugees, who can access ARV treatment while their asylum requests are being processed.
At the same time, the activist said, there’s no question that the Georgian healthcare system was unprepared for the influx of migrants. While Georgia has been proactive in HIV prevention, migrants have encountered difficulties in accessing HIV treatment.
According to the experts who spoke to Meduza, effectively addressing Georgia’s HIV problem will require ensuring equal access to healthcare, repealing discriminatory laws, and prioritizing prevention programs and HIV awareness campaigns. Providing free counselling, testing, and treatment to all individuals living with HIV, regardless of their legal status, is paramount.
2 notes
·
View notes
Text
Man Cured of HIV After Stem Cell Treatment
A 66 year old man suffering from leukemia and HIV has been cured of HIV after receiving stem cell treatment for leukemia, 34 years after his initial diagnosis. The patient, who wishes to remain anonymous, is the oldest person to undergo the treatment and enter long term remission.
In March 1987, the FDA approved the first antiretroviral drug for HIV (azidothymidine). In the 1990's, a mixture of therapies designed to boost the efficacy of treatment and prevent natural development of resistance to drugs was used. This particular patient took antiretrovirals for 31 years, however, his condition did progress to AIDS.
In 2018, he was diagnosed with leukemia (blood and bone marrow cancer). He received a blood stem cell transplant from a donor who was resistant to HIV due to a rare genetic mutation called homozygous CCR5 delta 32, which results in the typical entryway that the HIV virus utilises being altered, preventing HIV from entering the white blood cells.
Throughout March 2021, the patient stopped taking antiretrovirals, and up till now, there have been no signs of HIV present in his body. After a certain period of time, the patient can be officially declared "cured", however, continuous monitoring is required.
This patient shares a similar story with The Berlin Patient, The Dusseldorf Patient, and The London Patient, all of whom review similar treatment, and were similarly provisionally cured. However, it's important to note that transplant of blood stem cells is not a viable option for every person who has HIV/AIDS due to the risks associated with transplants. There is still hope for them though, research is constantly carried out into the potential cures and treatments for HIV, including gene editing techniques.
This story is an incredible one, spreading hope for all those who's lives have been impacted by this disease, and may prove to be the beginning of a world where HIV/AIDS are eradicated.
Source: LiveScience, written by Nicoletta Lanese
23 notes
·
View notes