#Diabetes Controller
Text

Introduction to Diabetes and Types
Studies have shown that India ranks second after China in the global diabetes epidemic, with 77 million people with diabetes. Of these, 12.1 million are aged >65 years, which is estimated to increase to 27.5 million in the year 2045. There are two most common types of diabetes: Type 1 diabetes and Type 2 diabetes
With Type 1 diabetes, the body stops producing insulin as the insulin-producing cells in the pancreas are destroyed. In this condition, a person must take insulin injections daily to regulate blood glucose levels.
Type 2 diabetes is a serious disease where your body may not respond to insulin, or the body makes insulin but not enough or does not use it well, and thus the sugar levels could go haywire. Thus, sugar steadily builds up in the blood, eventually leading to the blood vessels hardening, causing heart attacks, kidney failure, and stroke.
What are the risk factors for type 2 diabetes?
Risk factors that can increase diabetes include
obesity and a sedentary lifestyle,
uncontrolled blood glucose synthesis in the liver,
hereditary causes
Dysfunctional beta-cell in the pancreas
What are the symptoms of Type 2 diabetes?
You may have diabetes if you have
Blooded vision
Frequent urination
Increased hunger
Slowed healing of wounds, red, swollen, tender gums, and
Tingling hands and feet. If you experience such symptoms, consult your doctor immediately.
What are the complications of Type 2 Diabetes?
Long-term untreated diabetes affects the nerve, kidneys, heart, and eyes.
Nerve damage: Diabetes damages the nerves in the legs and arms. These cause numbness, pain, and tingling that start with the fingers and toes and spread along the legs. If this is left untreated, a person can lose all sense of feeling. Diabetic neuropathy is a family of progressive nerve disorders.
Kidney damage: Long-term uncontrolled blood sugar leads to kidney failure that requires dialysis or a kidney transplant.
Heart and blood vessels: For people with diabetes, who have high blood glucose cause blood vessels in the body to become damaged; when this happens, plaque can form in the blood vessels, making it difficult for the blood to flow.
Eye damage: Diabetes, if left untreated, can damage the retina of the eyes, which may lead to blindness.
Nutrients and vitamins:
Diabetic patients tend to have less nutrient absorption for vitamins like Vit C, D3, calcium, and Vit, herbs. Defective insulin secretion and insulin sensitivity cause metabolic disorders.
Ayurvedic Approach for Type 2 Diabetes
In Ayurveda, diabetes is described as ‘Madhumeha’. Diabetes mellitus is described as Vaat Pramehaand Diabetes insipidus is described as Kaph Prameha
According to Ayurveda, imbalances of kaph dosh, pitt dosh together with vaat dosh are the main cause of Madumeha. Vaat, kaph, and Pitt block the pathways connected to the mamsa (muscle) and meda (fat) tissues.
Eating too much, not exercising, being overweight—all these factors aggravate the vaat dosh of the body, where the body does not make enough insulin or does not use it well, and that leads to diabetes.
Ayurveda suggests Jamun and its seeds are highly effective herbs against diabetes. Known as jamboline and jambosine, the fruit seeds slow down the release of sugar into the bloodstream and increase insulin levels. Diabetes symptoms such as frequent urination and thrusting can be reduced with it since it converts starch into energy. In addition to reducing serum glucose levels and insulin resistance, the herb also reduces dyslipidemia and enhances the function of B cells. As a result, the herb rejuvenates the pancreatic cells at the cellular level.
What is the Treatment for Type 2 Diabetes?
Treatment of type 2 diabetes focus on the combination of diet and lifestyle changes along with medicines.
Lifestyle changes: Yoga has shown to be a great option in the treatment of diabetes. Regularly practising yoga can help to control blood sugar and increase insulin sensitivity in the cells. In addition to helping reduce blood sugar, yoga benefits by reducing stress levels and reducing the risk of heart problems by protecting cardiac health. Regular yoga helps to improve nerve function and boost metabolism, thereby improving nerve health.
Diet changes: It is recommended to consume low-fat foods, avoid any dairy-based products, and incorporate certain foods, such as bitter ground, Bengal gram, and fenugreek seeds, to control blood sugar.
Blood sugar monitoring: Regular blood sugar monitoring is beneficial in the treatment of type 2 diabetes.
Medication:
Although it is now one of the most common yet challenging health issues that people face, a rooted approach plus modern technology provide Meta medicine in the form of DiabGavyam, which is effective and consists of some of the best herbs for the treatment of type 2 diabetes.
DiabGavyam activates the pancreas, stimulates the secretion of a balanced amount of insulin, and regulates the metabolism of carbohydrates. The formulation is blended with the herbs Jamun Beej, and Madhunashak that protect the nerve cells in the retina, thus fortifying the blood vessel, and promoting blood circulation, thus lowering the chance of diabetic retinopathy.
While medicine helps in the control of blood sugar; it does not have any side effects after taking a tablet. You can take 1 or 2 tablets twice a day or as directed by your physician.

#Control Blood sugar Medicine#Type 2 Diabetes Medicine#Diabetes Supplement#DiabGavyam#Diabetes Controller#Glucose Controller#Insulin Booster
0 notes
Text
it is not controversial to say that if you cannot finacially, emotionally provide for a child and/or your genetics would lead to them suffering then you should not have said child.
#anti natalism#anti natalist#antinatalism#antinatalist#seriously the amount of people who scream eugenics.#you have no fucking clue what eugenics is#you are screaming your support for children being born into already negelctful and abusive situations just for your own liberalism.#And guess what--animals in the wild who have genetic disorders dont get to pass on their faulty genes either#it isnt rude for me to say it. it's reality#and if you cant accept reality than thats even more reason you should nto be allowed to breed#i myself have endless genetic predisposures. schizophrenia diabetes heart disease arthritis.#even if i had the finances and wanted a child i know it would be COMPLETELY unethical to gamble with their life.#you all have gambling addictions and are control freaks
118 notes
·
View notes
Text


When your horse (Fjara) decides to grab that fun little wire poking out from your pocket and won’t let go despite you begging her to and then manages to damage the infusion tube juuust enough to break down the whole system 🤣
#sort of expected it ngl#it’s not the first time she’s grabbed it#only usually she just fully pulls it from my body#(it’s a taped on infusion clip with a tiny tube that goes just beneath the first layer of skin#the pain really is just the tape being ripped off me)#now she fully had me under control like a puppet on a literal string#while on the phone with my trainer#she got that whoooole interaction lmao#*myhorses#fjara frá skjálg#t1d#actually diabetic#you know what? I’m glad she’s not figured out my CGM set yet#if it were a freestyle Libre it’d be easy enough to avoid her pulling that off#they’re flat and also very easy to get#they’re stingy with Dexcom in the Netherlands for reasons I’ve not yet been able to find out#but they’re bigger and easier to grip with big teeth#and my supply is tight lmao#that too is going to happen some day#mark my words
9 notes
·
View notes
Text
Been on a medically-monitored low carb diet for like a year and a half and my weight did not noticeably change
Doc put me on Ozempic once she finally believed (by the evidence via blood tests) that I was indeed eating as instructed and I've only been on the full dose for a couple of weeks
And suddenly my old jeans fit again
Hmm hmm isn't it funny what happens when my doctor actually fucking listens to me and offers help instead of just telling me I'm not trying hard enough for like, my entire life
#not a huge weight loss so far but definitely some difference#weight loss#weight talk#diet#ask to tag#and fyi i am trying to lose weight to reduce the pain in my knees and back#and the diet is also to control my diabetes (which it has been doing very well)#mod post#i have to go see my doc on wednesday... should i wear my jeans that suddenly fit or the ones that are loose and falling off?
32 notes
·
View notes
Text
How Regular Exercise Reduces the Risk of Diabetes
Diabetes is a significant health concern affecting millions globally, but the good news is that regular exercise can play a pivotal role in reducing the risk of developing this chronic condition. Regular physical activity is beneficial not only for weight management and cardiovascular health but also for blood sugar regulation and insulin sensitivity. In this article, we will explore how regular exercise helps reduce the risk of diabetes and provide tips for incorporating exercise into your daily routine.

Understanding Diabetes and Its Risk Factors
Diabetes, particularly type 2 diabetes, occurs when the body becomes resistant to insulin or when the pancreas is unable to produce enough insulin. This leads to elevated blood sugar levels, which can cause serious health complications over time. Risk factors for type 2 diabetes include obesity, a sedentary lifestyle, poor diet, and a family history of diabetes.
The Role of Exercise in Diabetes Prevention
Improves Insulin Sensitivity: Regular exercise helps improve the body’s sensitivity to insulin. When you exercise, your muscles use more glucose, reducing blood sugar levels. Over time, this increased glucose uptake by muscles makes your body more responsive to insulin, thereby reducing the risk of insulin resistance.
Helps with Weight Management: Maintaining a healthy weight is crucial in preventing diabetes. Exercise helps burn calories, build muscle, and reduce body fat. Even modest weight loss can have a significant impact on reducing diabetes risk. For individuals who are overweight or obese, losing 5-10% of body weight can greatly improve insulin sensitivity and lower blood sugar levels.
Regulates Blood Sugar Levels: Physical activity helps regulate blood sugar levels by promoting the uptake of glucose into muscle cells. Both aerobic exercises, such as walking, running, and swimming, and resistance training, such as weightlifting, are effective in managing blood sugar levels. Regular exercise also helps to stabilize blood sugar levels throughout the day, reducing the risk of spikes and crashes.
Reduces Visceral Fat: Visceral fat, the fat stored around internal organs, is strongly linked to insulin resistance and type 2 diabetes. Regular exercise helps reduce visceral fat, improving overall metabolic health and lowering diabetes risk.
Enhances Cardiovascular Health: People with diabetes are at a higher risk of developing cardiovascular diseases. Regular exercise strengthens the heart and improves circulation, reducing the risk of heart disease, stroke, and other cardiovascular complications.
Types of Exercise for Diabetes Prevention

Aerobic Exercise: Activities like brisk walking, running, cycling, swimming, and dancing increase your heart rate and help burn calories. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week.
Resistance Training: Strength training exercises, such as weightlifting, bodyweight exercises (e.g., push-ups, squats), and resistance band workouts, help build muscle mass and improve insulin sensitivity. Incorporate resistance training at least two days a week.
Flexibility and Balance Exercises: Activities like yoga and tai chi enhance flexibility and balance, reducing the risk of injuries and improving overall physical fitness. These exercises also promote relaxation and stress management, which are important for diabetes prevention.
Tips for Incorporating Exercise into Your Routine
Start Slow: If you’re new to exercise, start with small, manageable goals. Gradually increase the intensity and duration of your workouts as your fitness level improves.
Find Activities You Enjoy: Choose exercises that you enjoy to make it easier to stick with your routine. Whether it’s dancing, hiking, or playing a sport, enjoyment will keep you motivated.
Make It a Habit: Consistency is key. Schedule regular workout sessions and treat them as non-negotiable appointments.
Stay Active Throughout the Day: Incorporate physical activity into your daily routine by taking the stairs, walking during breaks, or cycling to work.
Monitor Progress: Keep track of your workouts and progress. Celebrate milestones to stay motivated.
Conclusion
Regular exercise is a powerful tool in reducing the risk of diabetes. By improving insulin sensitivity, aiding in weight management, regulating blood sugar levels, reducing visceral fat, and enhancing cardiovascular health, physical activity provides a comprehensive approach to diabetes prevention. Start incorporating regular exercise into your daily routine today to enjoy its numerous health benefits and significantly reduce your risk of developing diabetes.
WE SUGGEST YOU TO BEST SOLUTION FOR BLOOD SUGAR.CLICK TO KNOW MORE HERE
#blood sugar treatment#diabetes treatment#diabetes#type 2 diabetes#blood sugar control#supplements health#sugar control
7 notes
·
View notes
Text
Me in 2021:

Me now:

I've been on a closed loop system since 2022 and it's the first thing that's actually worked to get my blood glucose down permanently.
(I use the Dexcom/Tandem T:slim system)
I gifted myself an Apple Watch last year to track my health better, but it also allows me to show my blood glucose on the screen. Which is an oddly sentimental element, because when I was 6 and first diagnosed with Type 1 my grandmother said: "One day you'll be able to see your blood glucose on a watch, you mark my words!"
It might not be quite what either of us imagined, but hey gramma, I can see it on my watch now :')
#actually diabetic#t1d#my diabetes behaves like a bouncy ball and reacts to everything an anything#trying to control it manually was exhausting and never actually...rewarding? to give it a name?#you'd get it right and OOP up we go again#this and that from age 6 to 34#December 2022 was when I was super close to actually just...giving up. Truly giving up on ever getting it right.#my diabetes was winning from me at that point#and that same month someone said 'hey. maybe THIS system can help you. Come on. Let's get you started.'#I forget if it was a nurse or my doctor#but that was the turning point I desperately needed before I just let my body go to full ruin#my eyes already aren't well#the rest of me still seems fine though#and now I can hope it'll stay fine for a long time#because MY GOD I don't have to think about my diabetes every second of the day#my CLS does it for me and corrects for me. FIGHTS for me.#I really hope the system can help many others like me#I know in the Netherlands more and more diabetics are getting it#(fully insured)#for some of us it can be a lifesaver#for non-diabetics: 107 iS FUCKING HIGH YO#I WAS NOT FEELING GOOD 24/7#thirsty tired and just blegh
3 notes
·
View notes
Text
I have a bad habit of pulling the tip off of my insulin pen with my mouth. This is now the 4th time in my life that I’ve had someone ask me not to “vape” indoors, before they’ve seen that it is in fact a needle I’m holding
#tbh I use old ass pens that look like those big clunky vapinator 3000s#I’m very outdated with my diabetes tech#but it works for me my control is impeccable#bunny rambles#diabetic type 1#diabetic#chrinic illness#chronically ill#diabetes meme#gut health#meme
9 notes
·
View notes
Text
Apparently hot flashes during periods aren't normal and having that and other pre-menopause symptoms just so happen to be yet another perk of diabetes <3
#personal#diabetes#actually diabetic#hey so um what the fuck???#like what is the specific thing making my hormones angry? is it hyperglycemia?? hypo?? the fact i make 0 insulin???#idk what even triggers it bc the symptoms are not consistent each cycle#sometimes it's normal sometimes it's ''lie on the floor in a puddle of sweat and pray'' and i don't have an early warning system#bet this would make getting on birth control a pain in the ass as well lmfao#anyways good morning everyone
4 notes
·
View notes
Text

DiabGavyam - Diabetes Controller
#Insulin Booster#Glucose Controller#Control Blood sugar Medicine#Type 2 Diabetes Medicine#Diabetes Supplement#Diabetes Controller
0 notes
Text
do any of my diabuddies have tips for keeping blood sugars in check during a longish tattoo appointment?
#t1d#chronically ill#type 1 diabetes#type 1 diabetic#type one diabetic#diabetic#diabetes#blood sugar#sugar control
3 notes
·
View notes
Text
lying to a kid about if theyre adopted should be classified as abuse and no j am not joking
#abused adoptee#adoption#adoptee voices#to clarify i was never lied to. i knew as early as i can remember#but i work with a kid who was raised thinking her mother was her older sister.#shes seemingly chill about it but you can tell#and even so thats just so fucked up#you hear of people finding out through dna tests#of the adopters waiting till (specific) birthday to tell them -- usually after 18.#im sure even people who arent adopted can sympathize with how awful that would be#to find out your entire life is a lie overnight#especially for medical concerns. all the medical history yourlve come to accept as fact (grandma has diabetes aunt judy has dementia etc)#is suddenly wrong. now you dont know what you are or arent predisposed to. you dont know what tests you shouldve taken#your ancestry and ethnicity could be wrong#i knew i was adopted but they never told me i was hispanic. they kept it from me.#i thought i was pure british like them because im not super tan and have blonde hair#sometimes it's done under the guise of 'keeping peace'or 'saving them from the burden of knowing'#but really--it's all about control#most people dont like to talk about it but a good portion of adoptive situations involve control freaks.#this is from my own personal experience#almost every adopter i know is a control freak.#half of the adopters i know personally adopted just for the manual labor and a scape goat.#this is what my adopters did#to completely take away someones truth and deny them their own history--even after youve taken their legal rights.#oftentimes youve taken their entire names#like that is so vile#it really is#adoptees deserve the right to know theyre adopted. to know their biological familys medica history (if possible)#to be able to contact their biological family if they choose so#to be able to denounce the adopters as their parents or family
8 notes
·
View notes
Text

MO.RDIN MY A1C WENT DOWN ARE YOU PROUD OF ME
#harper has spoken#f: just the thing#im now just barely touching the 'well controlled for diabetics' range
4 notes
·
View notes
Text
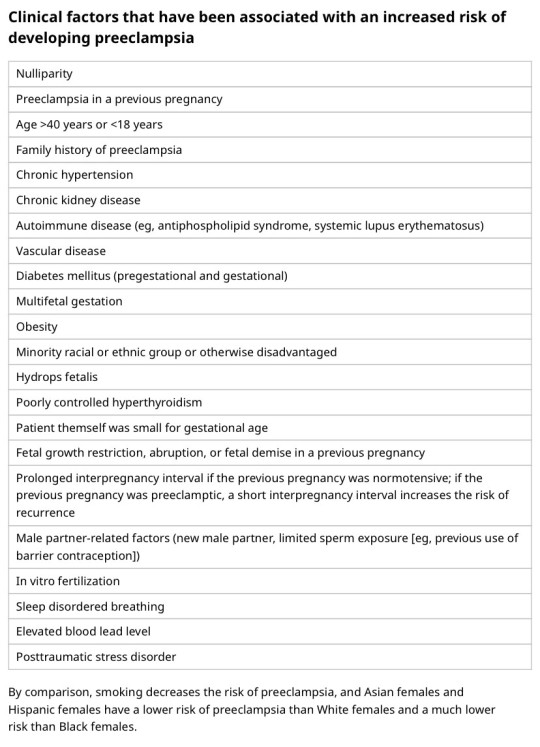
I'm on OB rotation again. I asked the attending what are things the PCP should know about prenatal and postpartum pts. Stuff we discussed:
SSRIs can be continued during pregnancy. I often see patients on Zoloft during pregnancy if they need an antidepressant. In fact, I just started a prenatal patient on Zoloft the other day in clinic. It is safe to continue SSRIs during pregnancy because you should treat the patient's depression. Babies can come out sort of jittery because of the SSRI, but that goes away.
Postpartum patients will have bleeding somewhat similar to a menstrual period right after giving birth. It starts to decrease and becomes like a brownish color and can last up to 6 weeks postpartum. Any bleeding beyond that point is abnormal.
There is some evidence that if you have estrogen-containing birth control, it can decrease milk supply. Actually, I had a patient in clinic recently who was seen by an attending and he started her on a progesterone only birth control so that it would not affect her milk supply. Estrogen decreases the patient's milk supply, so patients who plan to breast-feed should not be started on estrogen-containing birth control. Right after giving birth, your body has increased amounts of estrogen, so you would not start estrogen containing birth control until at least 6 weeks postpartum anyway. Increasing estrogen immediately postpartum increases risk of blood clots. For patients who plan to breastfeed and want to be on an oral contraceptive, use progesterone only oral contraceptives until she stops breastfeeding.
If the mother is breastfeeding at least every 4 hours, then this can be used for contraception. It's about 80% effective. Once baby starts sleeping through the night or once baby starts feeding more than every 4 hours, this method won't work! If you go more than 4 hours without breastfeeding, breastfeeding will not protect you from pregnancy! You can also ovulate before your menstrual period returns, so you can't say you can't get pregnant because your period has not returned yet!
I asked the attending I worked with today about how she goes about prescribing birth control. She said she will usually start with Sprintec. It's usually covered by insurance and if it's not covered, it's pretty affordable. She also said Junel is pretty well tolerated. Certain progestins in certain brands of birth control may work better for certain things like acne control, but she didn't have as much knowledge on that. I'll ask another attending again about that. I usually start people on Sprintec as well.
PCP should know that alkaline phosphatase is high in pregnant patients. It comes from the placenta. So don't be freaked out by that.
You should know HTN in pregnancy and preeclampsia workup. High BP is 140/90. Severely high BP is 160/110. Swelling occurs in many pregnant pts, but that should also alert you to start preeclampsia workup.
[Preeclampsia w/u from UpToDate:
Diagnostic evaluation
•Laboratory – Patients with suspected preeclampsia should have a complete blood count with platelets, creatinine level, liver chemistries, and determination of urinary protein excretion.
•Fetal status – Fetal status is assessed concurrently or postdiagnosis, depending on the degree of concern during maternal evaluation. At a minimum, a nonstress test or biophysical profile is performed if appropriate for gestational age. Ultrasound is used to evaluate amniotic fluid volume and estimate fetal weight, given the increased risk for oligohydramnios and growth restriction.
•Consultation with the neurology service is generally indicated in patients with neurologic deficits/abnormal neurologic examination, which may include ocular symptoms or a severe persistent headache that does not respond to initial routine management of preeclampsia.]
An important thing to review is physiology of pregnancy. Blood volume increases during pregnancy, so there are lots of new RBCs and that will throw off a HgbA1c reading, therefore HgbA1c is not measured during pregnancy and will not be accurate! My attending today told me there was a midwife who offered pts either HgbA1c or oral glucose tolerance tests to screen for gestational DM. The HgbA1c is not accurate in pregnancy, so this should not be done. That would be bad to miss a diagnosis of gestational diabetes. You have to wait until 3 months postpartum to measure HgbA1c to get an accurate reading. Had a pt who did not have a PCP prior to getting pregnant, was on insulin during the pregnancy, and after giving birth, still needs to establish with PCP for diabetes f/u. After you give birth, you insulin needs drastically change, so you don't need as much as you did when you were pregnant. So I stopped her insulin and advised that she f/u with her new PCP for diabetes care.
I still need to review fetal heart tracings. The attending today said the first thing to look at is the baseline (the baseline HR should be about 160 beats/min), then the variability, then look for accelerations and decelerations. If more than 32 weeks GA, accelerations are 15 beats/min above the baseline lasting at least 15 seconds. Early decelerations are representative of compression of the fetal head, which is normal during labor as baby moves down the pelvis/birth canal. Variable decelerations look sharper like a "V" and can represent compression of the umbilical cord. Late decelerations represent placental insufficiency.
ACOG has very helpful practice bulletins.
I can't take screen shots on my work laptop, so I'm just going to summarize gestational HTN w/u from UpToDate:
Gestational HTN: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions 4 hours apart after 20 weeks of gestation in a previously normotensive individual
And:
No proteinuria
No signs/symptoms of preeclampsia-related end-organ dysfunction (eg, thrombocytopenia, renal insufficiency, elevated liver transaminases, pulmonary edema, cerebral or visual symptoms)
Preeclampsia: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions at least 4 hours apart after 20 weeks of gestation in a previously normotensive individual. Patients with systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg should have blood pressure confirmed within a short interval (minutes) to facilitate timely administration of antihypertensive therapy.
And:
Proteinuria (≥300 mg per 24-hour urine collection [or this amount extrapolated from a timed collection], or protein:creatinine ratio ≥0.3, or urine dipstick reading ≥2+ [if other quantitative methods are not available]).
In a patient with new-onset hypertension without proteinuria, the diagnosis of preeclampsia can still be made if any features of severe disease are present.
Preeclampsia with severe features: In a patient with preeclampsia, presence of any of the following findings are features of severe disease:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg on 2 occasions at least 4 hours apart (unless antihypertensive therapy is initiated before this time)
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
Progressive renal insufficiency (serum creatinine concentration >1.1 mg/dL [97 micromol/L] or doubling of the serum creatinine concentration in the absence of other renal disease)
Pulmonary edema
Persistent cerebral or visual disturbances
Eclampsia: A generalized seizure in a pt with preeclampsia that cannot be attributed to other causes.
HELLP syndrome: hemolysis, elevated liver enzymes, low platelets. Hypertension may be present (HELLP in such cases is often considered a variant of preeclampsia).
Chronic (pre-existing) hypertension: hypertension diagnosed or present before pregnancy or on at least 2 occasions before 20 weeks of gestation. Hypertension that is first diagnosed during pregnancy and persists for at least 12 weeks postpartum is also consider chronic hypertension.
Blood pressure criteria during pregnancy are:
Systolic ≥140 mmHg and/or diastolic ≥90 mmHg
Prepregnancy and 12 weeks postpartum blood pressure criteria are:
Stage 1 – Systolic 130 to 139 mmHg or diastolic 80 to 89 mmHg
Stage 2 – Systolic ≥140 mmHg or diastolic ≥90 mmHg
Chronic HTN with superimposed preeclampsia*:
Any of these findings in a patient with chronic hypertension:
A sudden increase in blood pressure that was previously well-controlled or an escalation of antihypertensive therapy to control blood pressure
New onset of proteinuria or a sudden increase in proteinuria in a patient with known proteinuria before or early in pregnancy
Significant new end-organ dysfunction consistent with preeclampsia after 20 weeks of gestation or postpartum
*Precise diagnosis is often challenging. High clinical suspicion is warranted given the increase in maternal and fetal-neonatal risks associated with superimposed preeclampsia.
Chronic hypertension with superimposed preeclampsia with severe features:
Any of these findings in a patient with chronic hypertension and superimposed preeclampsia:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg despite escalation of antihypertensive therapy
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
New-onset or worsening renal insufficiency
Pulmonary edema
Persistent cerebral or visual disturbances
A reduction in blood pressure early in pregnancy is a normal physiologic occurrence. For this reason, women with chronic hypertension may be normotensive at their first few prenatal visits. Later in pregnancy, when their blood pressure returns to its prepregnancy baseline, they may appear to be developing preeclampsia or gestational hypertension if there are no documented prepregnancy blood pressure measurements.
BP: blood pressure.
* Blood pressure should be elevated on at least two occasions at least four hours apart. However, if systolic pressure is ≥160 mmHg or diastolic pressure is ≥110 mmHg, confirmation after a short interval, even within a few minutes, is acceptable to facilitate timely initiation of antihypertensive therapy.
¶ The onset of preeclampsia and gestational hypertension is almost always after 20 weeks of gestation. Preeclampsia before 20 weeks of gestation may be associated with a complete or partial molar pregnancy or fetal hydrops. Postpartum preeclampsia usually presents within two days of delivery. The term "delayed postpartum preeclampsia" is used for signs and symptoms of the disease leading to readmission more than two days but less than six weeks after delivery.
Δ Significant proteinuria is defined as ≥0.3 g in a 24-hour urine specimen or protein/creatinine ratio ≥0.3 (mg/mg) (34 mg/mmol) in a random urine specimen or dipstick ≥1+ if a quantitative measurement is unavailable.
◊ Almost all women with the new onset of hypertension and proteinuria at this gestational age or postpartum have preeclampsia, but a rare patient may have occult renal disease exacerbated by the physiologic changes of pregnancy. An active urine sediment (red and white cells and/or cellular casts) is consistent with a proliferative glomerular disorder but not a feature of preeclampsia. Women with chronic hypertension who had proteinuria prior to or in early pregnancy may develop superimposed preeclampsia. This can be difficult to diagnose definitively, but should be suspected when blood pressure increases significantly (especially acutely) in the last half of pregnancy/postpartum or signs/symptoms associated with the severe end of the disease spectrum develop.
§ Photopsia (flashes of light), scotomata (dark areas or gaps in the visual field), blurred vision, or temporary blindness (rare); severe headache (ie, incapacitating, "the worst headache I've ever had") or headache that persists and progresses despite analgesic therapy; altered mental status. Seizure occurrence upgrades the diagnosis to eclampsia.¥ The differential diagnosis of preeclampsia with severe features includes but is not limited to:
Antiphospholipid syndrome
Acute fatty liver of pregnancy
Thrombotic thrombocytopenic purpura (TTP)
Hemolytic uremic syndrome (HUS)
The laboratory findings in these disorders overlap with those in preeclampsia with severe features. (Refer to table in the UpToDate topic on the clinical manifestations and diagnosis of preeclampsia.) The prepregnancy history, magnitude and spectrum of laboratory abnormalities, and additional presence of signs and symptoms not typically associated with preeclampsia help in making the correct diagnosis, which is not always possible during pregnancy.
In addition, a variety of medical disorders may be associated with hypertension and one or more of the signs and symptoms that occur in women with preeclampsia with severe features. These patients can usually be distinguished from patients with preeclampsia by taking a detailed history, performing a thorough physical examination, and obtaining relevant laboratory studies.‡ In contrast to preeclampsia, gestational hypertension is not associated with end-organ involvement, so neither proteinuria nor the symptoms or laboratory findings of preeclampsia are present.
#OB#OBGYN#birth control#gestational HTN#preeclampsia#eclampsia#breastfeeding#gestational diabetes#fetal heart tracing#FHT
2 notes
·
View notes
Text
If I had a pound for everytime I got treated like I don't have diabetes by a health professional who is supposed to have looked at my medical history I'd have £2
Which isn't a lot in the grand scheme of things but it's weird it's happened twice.
#ive had type 1 for 20 years and have complications from it but lmfao#twice in the space of 15 days i fucking cant#one of the things im being seen for is literally a side effect from badly controlled diabetes like mate
6 notes
·
View notes
Text
I have a specific kind of autism that upon getting a new ‘mild’ but extremely miserable health condition I decided “that’s fine I always wanted to learn herbalism anyways” and just decided to manage it myself
#I can’t take birth control I have few options#and I (hopefully???) won’t die if it’s unsuccessful#no one should do this for like cancer or anything that can easily kill you#don’t treat diabetes with just herbs
2 notes
·
View notes
Text
Every time o research things to learn abt my brothers new type one diabetes diagnosis I have vivid flashbacks to how he looked when we were loading him into the car to go to the er and I start having a panic attack
#mark says#t1d#t1diabetic#and then i feel guilty bc i need to learn to help as much as i can#but i wanna puke bc my brains telling me hes gonna go into dka and almost die again#and wtf do you do overnight?? do yiu just load up on insulin and hope nothing crazy happens?#why cant he be type two like my grandmas.#like its still diabetes yes but its at least pill controlled (sometimes)#im literally on a t2d medication for my pcos (metformin) and it makes me shit my brains out. my grandma is too. also makes her shit her#brains out#but at least it isnt insulin#chop chop find a cure docs and sciences#hope he can get a pump#did expensive reserch on pancreatic transplant bc before i knew it was dead donors only i was fully abt to#give him half lf mine like a kidney 💀#but yeah hes in the icu.
4 notes
·
View notes