#Gastrojejunostomy
Text
February 6-10 is Feeding Tube Awareness Week!

The beginning of February was selected because of its proximity to Valentine’s Day, because we love our feeding tubes. This is my first year as a tubie and I’m looking forward to learning more about feeding tubes and the conditions that necessitate them! I do love my tube, it saved my life!
I am an adult with a feeding tube, and a lot of the awareness and attention surrounding these medical devices is child focused. A lot of children depend on tube feeding to thrive, but there are plenty of disabled adults that depend on tube feeding as well! In 2017 there were approximately 438,000 people with feeding tubes in the US, and 60% of them are adults.
I have gastroparesis, which directly translates to paralysis of the stomach. My stomach doesn’t grind food the way it’s supposed to, and my pylorus sphincter at the bottom of my stomach doesn’t open well to pass food and liquids through. While gastroparesis has a range of impact and severity, I have a very severe case, and I am no longer able to eat or drink by mouth for nutrition. I am 100% tube fed. I went into starvation ketoacidosis prior to my placement.
Tube feeding, or enteral nutrition, has several different forms. There are nasal tubes and there are surgical tubes. Nasal tubes can go into your stomach (NG), duodenum (ND), or your jejunum (NJ) and are typically for short-term use. They can be used for acute illness and malnutrition, or to trial tolerance of enteral feeding. Surgical tubes go into your stomach (gastrostomy/G) jejunum (jejunostomy/J) or both (gastrojejunostomy/GJ) and they’re for chronic conditions and/or long-term use. I have a GJ tube and it looks like this:
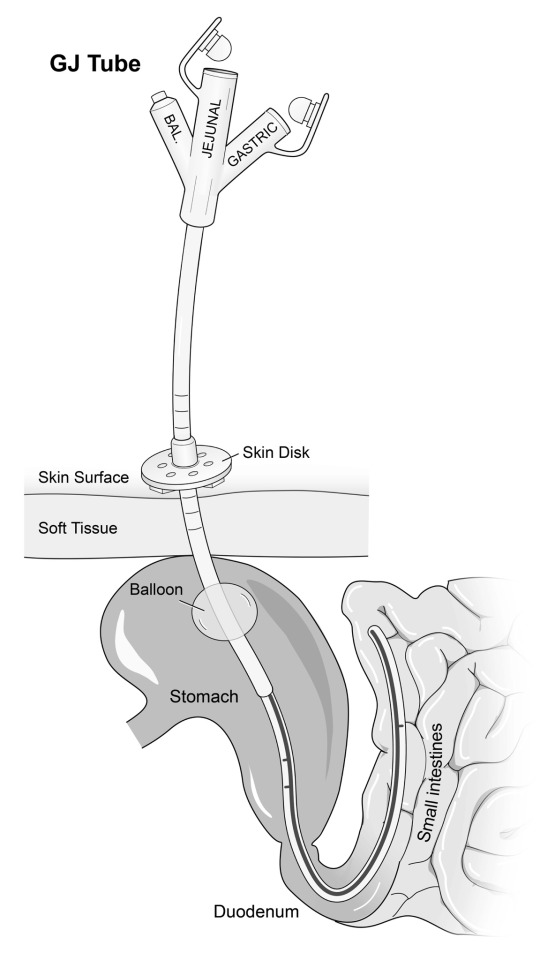
I have a GJ tube so that I can bypass my paralyzed stomach and feed directly into my intestine. I can also drain stomach contents from the gastric port, which allows me to drink liquids and drain them out before they make me sick. Different people will have different tubes depending on their diagnosis and prognosis! Some people have one form of tube, and others have separate G and J tubes.
There are over 400 conditions that can require tube feeding. Some of those include
Gastroparesis
Intestinal dysmotility
Cancer
Intestinal failure
Inflammatory Bowel Disease (Crohn’s disease and Ulcerative Colitis)
Cerebral Palsy
Congenital/chromosomal conditions
Cyclic Vomiting Syndrome
Ehlers-Danlos Syndrome
Several trisomy conditions
Prematurity
Other conditions not mentioned in the link above include
Hyperemesis gravadarium, severe nausea/vomiting during pregnancy to the point of significant weight loss and electrolyte imbalance
Acute trauma requiring bowel rest
Eating disorders
This week, I want to promote visibility for disabled adults with feeding tubes. I didn’t know anything about enteral nutrition until I got sick. Once I had a confirmed diagnosis of gastroparesis, the reality that I was facing forced me to learn and adapt quickly to a completely life changing treatment. I know there are other adults like me, as well as tubie adults that used to be a child with a tube!
4K notes
·
View notes
Text
O Hastanede Yine İlklere Devam Ediliyor;Parkinson Hastası Olan Bir Hastaya Jejunal Tüp Takıldı

Elazığ Fethi Sekin Şehir Hastanesi'nde, ileri evre Parkinson hastaları için endoskopi eşliğinde jejunal tüp ile PEG-J (perkütan endoskopik gastrojejunostomi) işlemi yapılmaya başlandı.
Bu yöntem, Parkinson hastalarının tedavisinde kullanılan ilacın mide asidi tarafından etkilenmesini engelleyerek daha etkili bir tedavi süreci sunmayı amaçlıyor.
Gastroenteroloji Cerrahi Uzmanı Dr. Sadık Keşmer, bu yöntemde ilacın mide asidi ile parçalanmasının önüne geçildiğini belirtti. Dr. Keşmer, “Bugün burada Parkinson hastası olan bir hastamıza jejunal tüp takıldı. Bu işlem endoskopik olarak yapılıyor. Daha önce hastaya endoskopik olarak Perkütan Endoskopik Gastrostomi (PEG) yapılmıştı. PEG işlemi yapılan veya yapılmayan hastalarda, mideden geçirilen tüp ince bağırsağın üst kısmına, yani jejunuma kadar ilerletiliyor. Bu sayede ilacın mide asidi ile parçalanması engelleniyor ve ilaç doğrudan ince bağırsağın jejunum kısmına sürekli infüzyon şeklinde uygulanarak hızla beyne ulaşması sağlanıyor,” dedi.



PEG-J işlemi, ileri evre Parkinson hastalarında kullanılan en etkili tekniklerden biri olarak kabul ediliyor. Özel bir pompa yardımıyla takılan kateterden doğrudan jejunum kısmına sürekli infüzyon yöntemiyle ilaç uygulanabiliyor. Elazığ Fethi Sekin Şehir Hastanesi'nde bu işlem ilk kez gerçekleştirildi ve hastanın bu tedaviden daha fazla fayda görmesi bekleniyor.
Read the full article
0 notes
Text
Partial gastrectomy (Billroth I procedure)
Preoperative situation (left image): resection of the gastric antrum and pylorus (structures depicted as transparent). The C-loop of the duodenum has been mobilized from its peritoneal attachments (red line) to enable a tension-free gastroduodenal anastomosis.
Postoperative situation (right image): the cut end of the duodenum (purple line) is anastomosed to the cut end of the stomach (green line). This gastroduodenal anastomosis may be end-to-end (as depicted here) or end-to-side.
A distal gastrectomy with a gastroduodenostomy is known as a “Billroth I procedure.”

Partial gastrectomy (Billroth II)
Left image: partial gastrectomy (transparent area) and blind-ending duodenal stump (purple line)
Middle image: side-to-end anastomosis between the first jejunal loop and gastric stump (green line = gastrojejunostomy)
Right image: side-to-side anastomosis between the efferent and afferent limbs of the small intestine (blue line = jejunojejunostomy, Brown anastomosis). The Brown anastomosis prevents bile and duodenal secretions from entering the gastric mucosa.
A distal gastrectomy with a gastrojejunal anastomosis and a blind-ending duodenal stump is known as a Billroth II procedure.

Subtotal gastrectomy (with Roux-en-Y anastomosis)
Subtotal gastrectomy:
- Subtotal gastrectomy involves the resection of the body and pyloric channel of the stomach (transparent portion of the stomach in this image).
- The cardia and fundus of the stomach and their blood supply is preserved (opaque portion of the stomach here).
- The duodenal stump (dashed red line) is closed.
Roux-en-Y anastomosis:
- A segment of the proximal jejunum is divided.
- Gastrojejunostomy creation: The distal cut end of the jejunal loop (black I) is anastomosed side-to-side to the gastric stump (purple dashed line; I–I).
- Jejunojejunostomy creation: The proximal jejunal stump (green II) is anastomosed end-to-side to a distal jejunal loop (green dashed line, II–II).

0 notes
Text

First- Time Ever in Faridabad : A Pioneering Achievement in Digestive Care
EUS Guided Gastrojejunostomy, A minimally Invasive Treatment of benign and malignant gastric outlet obstruction, performed by Dr. Kapil Sharma - Director - Gastroenterology & Head - Endoscopy, Sarvodaya Hospital, Sector-8, Faridabad.
#GastroenterologyEvent
#MinimallyInvasive
#GastroHealth
#Endoscopy
#SwallowingDisorders
#GastroHealth
#EPOEM
#DPOEM
#ZPOEM
#BestMultiSpecialityHospital
#MultispecialityHospital
#SarvodayaHealthcare
#Gastroenterology Treatment Hospital in Faridabad#Gastroenterology Treatment Hospital in Delhi NCR#Gastroenterology Treatment Hospital in Greater Noida#hospital#healthcare#health#sarvodaya hospital
0 notes
Text
EUS Gastrojejunostomy at GASTROPLUS digestive disease centre, Ahmedabad : EUS Gastrojejunostomy is a novel endoscopic technique as an alternative to surgery in high risk candidate.. No scar, No pain.. It’s a surgical procedure done by per oral endoscopy in field of gastroenterology
0 notes
Text
Types of Feeding Tubes
Whether you're preparing to get a tube, to visit someone who you've heard has a tube or need to learn all the types before professional placements starts tomorrow, here's a quick, concise guide!
To ridiculously oversimplify things, lean these 3 now:
NG & PEG
NJ, J-tube
IV line.
Well done!
To be more comprehensive,
The types are:
NG
ND/NI/NJ
PEG/RIG/G-Tube
GJ/PEG-J
PEJ/J-Tube
Then, some intravenous lines can be used for specialised intravenous nutrition:
PICC
Hickman
It's not actually as complicated as it looks, I promise!
Basically:
Nose to stomach or intestine
Or
Hole into stomach or intestine
Or
Veins
Enteral feeding tubes are ones which go into the digestive tract either through the nose or directly through the skin.
Think ENTER as in gastroENTERology
Sometimes, people need parenteral nutrition. This means bypassing the enteral. Parenteral goes straight into veins. That's PAR-enteral, not parental hehe ;) It's often called TPN for short (Total Parenteral Nutrition), especially if the person is dependent on it. Occasionally the term HPN is used if the person uses it at home. The H is for "home"
Ok. Back to Enteral tubes:
Nasoenteric Tubes (any feeding tubes that go in by the nose):
NG = nasogastric. Goes through nose into stomach. Quite common.
ND = nasoduodenal. Through the nose and stomach into the 1st part of the small intestine called the duodenum. Rare because nasojejunal is typically seen as preferable. Some NJs technically end up in the duodenum but may still be simply referred to as an NJ. My NJ often lands right at the juncture where the duodenum becomes the jejunum.
NJ = Nasojejunal. Through the nose , via stomach and duodenum into the second part of the small intestine called the jejunum.
NI = Nasointestinal. Sometimes this word might be used to include NDs and NJs on a product packet or in a medical paper. Nasoenteric may be a term used too
In essence, NG or NJ
Percutaneous (through-the-skin) Enteral Feeding Tubes:
PEG: Percutaneous Endoscopic Gastrostomy tube. Common.
RIG = Radiologically Inserted Gastrostomy. Often these simply get called PEGs anyway.
G-tube = Another word for either PEG or RIG.
PEG-J = PEG with extension tube inside to the Jejunum.
GJ = Gastrojejunostomy. Basically a PEG-J but doesn't necessarily have "percutaneous endoscopic" insertion. It could be radiologically inserted.
J-Tube = Goes directly through a hole made in the skin into the jejunum.
PEJ = A J-tube placed using endoscopy. Like RIGs, sometimes people still call radiologically inserted jejunostomies "PEJ".
So, G, GJ or J
Any feeding or placement into the intestine may also be called "postpyloric", especially in medical academic journals. This means anywhere beyond the stomach. The pylorus is the far part of the stomach before intestine.
BONUS/SIDE NOTE: Most feeding tubes are "single lumen" (lumen = inside channel) but double, even triple lumen tubes exist. Extra channels might be for extra hydration, medicines or "venting" stuff OUT such as painful excess stomach air. Usually medicines and extra water are done through ordinary single lumen tubes and a separate tube is often used if venting is necessary.
Now the Parenteral ones:
These are intravenous lines rather than what's typically classified as a "feeding tube".
PICC = Peripherally Inserted Central Catheter. This is the more common of the parenteral line types and usually short term. It goes into the upper arm. Inside the body the line goes through a vein into the chest, to the heart. Peripheral = opposite of central, so further/outer. (Catheter = tube that goes inside a body channel eg vein, urethra etc)
Hickman Line: This delivers nutrition pretty much the same way but goes in by the chest.
There are other IV line types but usually for medication or hydration rather than feeding. PICCs and Hickmans are often are used for medications too.
Why use gastric enteral feeding (NG, PEG etc)?
Can't or won't eat enough to meet nutritional needs.
Why Postpyloric/intestinal feeding (NJ, GJ, J-tube etc)?
As above but feeding into stomach is ineffective, unhelpful, intolerable or perhaps dangerous.
Why Parenteral (PICC etc)
Last resort if nothing else gives the necessary nutrition and/or balance.
Or if the person is "nil by mouth" but must get the nutrition
Occasionally, people have more than one type.
For example: someone might depend on a line in the veins but spend part of the day on a Nasojejunal feeding as much as they can tolerate, and have an old PEG site used for a tube for venting.
Another example: PEG fed and using PICC every so often to make up for some kind of deficiency.
So you've got the gist of it!
If you have any questions or if I've made any mistakes, feel free to let me know as long as it's nicely! :-)
Now for a pronunciation guide for anyone who needs it:
Nasogastric = NAY-zo-GASS-trick
Duodenum = DYOO-oh-DEE-num. Some might say dyoo-ODD-en-um
Jejunum = JEJ-oo-num or jej-OO-num
Percutaneous = PER-cyu-TAY-nee-us
Endoscopic = END-oh-SCOPP-ic
Gastrostomy = ga-STROSS-tum-ee
Jejunostomy = JEJ-ooNOSS-tum-ee
Parenteral = parENT-er-al
Radiologically = RAY-dee-ol-LOJ-ic-al-ee
Postpyloric = POST-pie-LOR-ic
Intravenous = IN-tra--VEE-nus
Peripherally = per-IF-er-al-ly
#Feedingtubes#Nurseeducation#Typesoffeedingtubes#Feedingtubetypes#Nasogastric#NG#Nasojejunal#NJ#Gastrostomy#Peg#Pej#Gj#Jtube#Gastrojejunostomy#Jejunostomy#Picc#Hickman#tpn#Medicalstudent#Nursingstudent#Healthcare#Gastroenterology#Interventionalradiology#Education#Carers
6 notes
·
View notes
Photo

I kept reading about Billroth procedures and just didn't get it! Now that I answered a question about it, it makes sense. They cut away the antrum of the stomach and connect the body of the stomach to the jejunum in a Billroth II gastrojejunostomy. This is a side to side anastomosis. This procedure can be done for complicated PUD or ulcers that don't respond to treatment. Iron, folate, and B12 are absorbed in the small intestine, so this surgery can lead to deficiency in these vitamins.
1 note
·
View note
Text
I’m creating an informational series on tube feeding on my Instagram @ paralyzedguts and I’d like to get some questions and perceptions from orally fed people on tube feeding! I’d like to create something like a FAQ and a common misconceptions post about enteral nutrition.
Tell me in the tags what you know (or think you know) about feeding tubes! Do you have a feeding tube? If so what kind? You can shoot me an ask as well.
I have a GJ (gastrojejunostomy) tube for gastroparesis. I take all my nutrition through the tube (100% tube fed).

Image description:
A silhouette of a human demonstrating multiple routes of nutrition.
The person has a pink bottle with a route line going through the mouth, down the esophagus, and into the stomach to represent oral nutrition.
They have a grey feed bag with multiple route lines to represent enteral nutrition. One from the bag in the nose, down the esophagus and into the stomach representing an NG (nasal-gastric) tube. Another from the bag into the stomach, representing a G (gastrostomy) tube. And a third from the bag to the intestine, representing a J (jejunostomy) tube.
They have an orange parenteral bag with two route lines. The first from the bag to the person’s arm, representing total or partial parenteral nutrition via a PICC line. The second one from the bag to the person’s heart, representing TPN/PPN via a port.
End image description
1K notes
·
View notes
Text
O Hastanede Yine İlklere Devam Ediliyor;Parkinson Hastası Olan Bir Hastaya Jejunal Tüp Takıldı

Elazığ Fethi Sekin Şehir Hastanesi'nde, ileri evre Parkinson hastaları için endoskopi eşliğinde jejunal tüp ile PEG-J (perkütan endoskopik gastrojejunostomi) işlemi yapılmaya başlandı.
Bu yöntem, Parkinson hastalarının tedavisinde kullanılan ilacın mide asidi tarafından etkilenmesini engelleyerek daha etkili bir tedavi süreci sunmayı amaçlıyor.
Gastroenteroloji Cerrahi Uzmanı Dr. Sadık Keşmer, bu yöntemde ilacın mide asidi ile parçalanmasının önüne geçildiğini belirtti. Dr. Keşmer, “Bugün burada Parkinson hastası olan bir hastamıza jejunal tüp takıldı. Bu işlem endoskopik olarak yapılıyor. Daha önce hastaya endoskopik olarak Perkütan Endoskopik Gastrostomi (PEG) yapılmıştı. PEG işlemi yapılan veya yapılmayan hastalarda, mideden geçirilen tüp ince bağırsağın üst kısmına, yani jejunuma kadar ilerletiliyor. Bu sayede ilacın mide asidi ile parçalanması engelleniyor ve ilaç doğrudan ince bağırsağın jejunum kısmına sürekli infüzyon şeklinde uygulanarak hızla beyne ulaşması sağlanıyor,” dedi.



PEG-J işlemi, ileri evre Parkinson hastalarında kullanılan en etkili tekniklerden biri olarak kabul ediliyor. Özel bir pompa yardımıyla takılan kateterden doğrudan jejunum kısmına sürekli infüzyon yöntemiyle ilaç uygulanabiliyor. Elazığ Fethi Sekin Şehir Hastanesi'nde bu işlem ilk kez gerçekleştirildi ve hastanın bu tedaviden daha fazla fayda görmesi bekleniyor.
Read the full article
0 notes
Text
Curative Treatment for Morbid Obesity
Obesity is a global health problem. A person with morbid obesity may have difficulty performing daily activities, such as walking and breathing, and is at increased risk for many serious health problems. There are various surgical procedures involve to cure obesity that reduces caloric intake by modifying the anatomy of the gastrointestinal tract, such as :
1) Biliopancreatic diversion: The Biliopancreatic Diversion (BPD) procedure achieves weight loss primarily through malabsorption as a result of an increased gastric emptying rate and accelerated intestinal transit times. The procedure comprises a partial gastrectomy with the closure of the duodenal stump. The small intestine is divided at the midpoint between the ligament of Treitz and the ileocecal valve to create a Roux-en-Y gastroenterostomy.
2) Adjustable gastric banding: This procedure is routinely done
Laparoscopically and is considered the least invasive bariatric surgical procedure due to the lack of disruption of the gastrointestinal tract. The AGB implies the creation of a small virtual gastric pouch by placing a silicone band around the upper stomach 1-2 cm below the gastroesophageal junction, which is connected with a subcutaneous port that allows access. A small retro gastric tunnel is created vast enough for the band to pass through, and stitches are placed anteriorly from the greater curvature to above the band to avoid later slippages. This procedure is entirely reversible but requires close follow-up to perform the adjustments and, by that means, functional outcomes.
3) Sleeve gastrectomy: The procedure involves a vertical gastrectomy performed with linear staplers, which is then oversewn; that excises the most compliant part of the stomach, the fundus and lateral 80% of the body, leaving a narrow gastric tube with preservation of the antrum and the pylorus.
4) Roux-en-Y gastric bypass: This technique involves the creation of a small gastric pouch (less than 30 ml), a small gastrojejunostomy of approximately 12 mm in diameter, and a Roux-en-Y configuration of the alimentary limb that ranges from 60 to 250 cm in length.
For any surgical procedure, one should consider going to some best obesity treatment center.
1 note
·
View note
Text
What is Candy Cane syndrome? | Dr. Sukhvinder Singh Saggu | Best Bariatric Surgeon in Delhi
Abstract. Candy cane syndrome is a rare complication that has been reported in bariatric patients who have undergone Roux-en-Y gastric bypass surgery. It occurs when the roux limb is excessively long proximal to the gastrojejunostomy, allowing food particles to lodge and remain in the blind redundant limb. Call Dr. Sukhvinder Singh Saggu | Best Bariatric Surgeon in Delhi- 9871056324

0 notes
Text
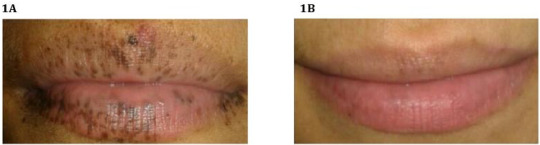
Gastric Outlet Obstruction as an Aggravation of Peutz- Jeghers Syndrome: Case Report - BJSTR Journal
Gastric Outlet Obstruction as an Aggravation of Peutz- Jeghers Syndrome: Case Report by Marcelo Zamorano* in Biomedical Journal of Scientific & Technical Research
https://biomedres.us/fulltexts/BJSTR.MS.ID.006160.php
The Peutz-Jeghers Syndrome (PJS) is a rare autosomal dominant disease characterized by macules of mucocutaneous pigmentation and hamartomatous intestinal polyps. Some signs of the PJS appear in childhood, usually with abdominal pain. In some cases, patients can develop complications. In this article, we report a case of a patient with PJS that reached the emergency room after presenting a concomitant gastric outlet obstruction (GOO). The patient underwent through an endoscopic polypectomy, followed by a laparotomy and an intraoperative enteroscopy. The symptoms were controlled and the extraction of hamartomatous intestinal polyps were achieved, culminating with an intestinal segment resection with muscle atrophy and posterior gastrojejunostomy. There is evidence of PJS cases related to other conditions that developed abnormal scenarios such as biliary obstruction or cecal appendix polyps. However, the association between PJS and GOO and a concomitant delimited intestinal aperistalsis has not been reported. Thus, this case report shows the possible association between the PJS and GOO, whose cause is the intraluminal occupation of the duodenum by polyps and the synergy of the symptoms given by the atrophy of the jejunum muscle.
For more articles on Journals on Biomedical Science please click here
bjstr
Follow on Twitter : https://twitter.com/Biomedres01
Follow on Blogger :https://biomedres01.blogspot.com/
Like Our Pins On : https://www.pinterest.com/biomedres/
#Journals on Medical Drug and Therapeutics#Medical Humanities#Behavioral Medicine Journals#Journals on Emergency Medicine#Nano Medicine
0 notes
Text
A Rare Case Report of Multiple and Large Small Bowel Neuroendocrine Tumours in a 50 Year Old Lady by Harsh M*

Abstract
Small intestinal neuroendocrine tumors are the most common type of neuroendocrine tumors and small bowel neoplasms. The clinical presentation varies from asymptomatic incidentally detected localized lesions to lethal metastatic disease with carcinoid syndrome [2].
A 50 year old lady presented with chief complaints of lump in upper abdomen associated with dull aching pain since 3 months. Cect scan was suggestive of a probable gastrointestinal stromal tumour for which patient underwent elective laparotomy. Postoperatively on the basis of histopathology a diagnosis of neuroendocrine tumor was made and confirmed with immunohistochemistry. Approximately 90% of duodenal NET’s are not associated with clinical syndrome. It is a rare diagnosis with incidence of 0.5/100,000.
Patients with well differentiated tumours diagnosed in early stage have a good prognosis with an 85% overall 5year survival rate.
Keywords: Neuroendocrine; Gastrointestinal; Stromal; Duodenum
Introduction
Neuroendocrine tumors are a heterogeneous group of neoplasms arising from various anatomical sites with the majority originating from small intestine and pancreas. They originate in the enterochromaffin cells of the aerodigestive tract. The underlying pathogenic mechanisms have been poorly characterised due to relative rarity.1
Small intestinal neuroendocrine tumors are the most common type of neuroendocrine tumors and small bowel neoplasms. The clinical presentation varies from asymptomatic incidentally detected localized lesions to lethal metastatic disease with carcinoid syndrome [2].
Functional neuroendocrine tumors are characterised by a clinical syndrome caused by excess hormonal secretion while non-functional neuroendocrine tumors are hormonally silent [3]. Intestinal neuroendocrine tumors have distinct features depending on their site of origin. Neuroendocrine tumors originating in the duodenum are not well characterized. Many are discovered incidentally during endoscopy [4]. Unlike other midgut neuroendocrine tumors, they are not commonly associated with the typical carcinoid syndrome. NET’s usually have an indolent clinical course, but tumor behavior varies widely depending on 2017 WHO (World Health Organization) grading, based on Ki-67 proliferation index and mitotic count [5].
Case Report
A 50 year old lady presented with chief complaints of lump in upper abdomen associated with dull aching pain since 3 months. There were no associated complaints of pain, fever, vomiting, constipation, diarrhoea, passage of blood in urine or stools, breathlessness, loss of weight or appetite and no complaint of other swellings in the body.
Patient was not a known case of diabetes mellitus, hypertension, heart disease, asthma or any other major illnesses. Patient is not a known alcoholic, smoker or drug addict. There is history of attaining menopause 5 years ago. Presently patient bears two children. On physical examination, patient was vitally stable. Per abdomen examination was soft to touch, non-tender with no guarding or rigidity felt. A lump of 15x8cm was felt in left hypochondriac and epigastric region, firm in consistency, immobile, non-tender with no local rise in temperature and with a smooth overlying surface. Per vaginal and per rectal examination had no abnormal findings. Routine lab investigations were within normal limits.
Patient was referred with a contrast enhanced computed tomography scan of abdomen and pelvis which was suggestive of:
1) A large well-defined solid heterogenously enhancing exophytic mass lesion of size 12x8cm containing non enhancing necrotic areas, arising from third part of duodenum.
2) Two well defined nodular enhancing lesions of approximate size 2x1 cm and 3x1cm from second part of duodenum.
Following above findings, CT was suggestive of a probable gastrointestinal stromal tumour with paraduodenal nodes.
An upper gastrointestinal endoscopy was performed which was within normal limits. Usg guided biopsy or fnac was not done due to high vascularity of tumour.
Following investigations and anesthesia fitness, patient was posted for an elective exploratory laparotomy. Intraoperatively:
There was evidence of a large 15x8x6cm exophytic growth from third and fourth part of duodenum, duodenojejunal flexure and proximal jejunal segment.
Another 4x2cm and 3x2cm growths were seen arising from second part of duodenum.
Intraoperative decision was taken to perform whipple’s procedure. Resection of the large tumor with associated jejunal segment was done with primary closure of proximal and distal duodenum. Cholecystectomy was done with resection of pylorus, duodenum and part of pancreas followed by sequential pancreaticojejunostomy, choledochojejunostomy, gastrojejunostomy and feeding jejunostomy.
Postoperatively patient was managed aggressively and closely monitored. Multiple blood transfusions and parenteral nutrition were supplied consecutively. Feeding jejunostomy feeds were started on fifth day postoperatively. Abdominal drain in subhepatic space was removed on the sixth day while the pelvic drain was removed on the tenth day postoperatively.
Histopathology report was as follows:
Grade 1 neuroendocrine tumour of duodenum with low mitotic activity and lack of necrosis.
Multiple neuroendocrine tumours of mesentery.
Resected ends of duodenum and jejunum were free of tumour.
Gall bladder, pancreas and pylorus were free of tumour
Further histopathology block were sent for Immunohistochemistry and KI 67 to enable exact grading that showed mitotic index less than 1, that was suggestive of a low grade, well differentiated tumour, following which patient was discharged on feeding jejunostomy and oral feeds and followed up after two and four weeks respectively.
At follow up, ultrasonography of abdomen and pelvis was done which showed no evidence of any anastomotic leak. Feeding jejunostomy was removed and patient was continued on complete oral feeds.
Discussion
The annual incidence of small intestinal carcinoids is nearly 0.5/100,000, they account for a small proportion of intestinal neoplasms while colorectal adenocarcinomas are 60 times more frequent [6]. Duodenal NETs comprise 1%-3% of all primary duodenal tumors and 2.8% of all carcinoid tumors [6]. The age-adjusted annual incidence of NETs arising from jejunum and ileum is 0.67 per 100000. Being a rare malignancy, investigation regarding its pathophysiology and information on classification of these tumors has been limited till recent times. Duodenal NETs are usually diagnosed in the sixth decade with a male predominance [7,8].
There are five types of duodenal NET’s: Duodenal gastrinoma [the most common type] duodenal somatostatinoma, non-functioning duodenal NETs, duodenal gangliocytic paraganglioma and poorly differentiated neuroendocrine duodenal carcinomas.
Majority of duodenal NET’s are small, single lesions, usually limited to the mucosa and submucosa. Regional lymph node metastases may be found in up to 60% of cases, while liver metastasis usually occur in less than 10% [7]. Approximately 90% of duodenal NET’s are not associated with clinical syndrome, as majority of diagnosis are made accidentally during a routine workup or if the patient develops symptoms attributable to the mass itself [7]. Most frequently reported presenting symptoms include pain, jaundice (more frequent in peri-ampullary NET’s), nausea, vomiting, diarrhea, obstruction, active bleeding or anemia. In the minority of duodenal NET’s that cause a functional syndrome the two main presentations are Zollinger-Ellison syndrome and carcinoid syndrome.
NET’s of jejunum and ileum are usually diagnosed in the sixth or seventh decade but as opposed to duodenal NET’s, have no gender preference. Most of them are nonfunctioning tumors but about 20% of patients show liver metastases and may present with carcinoid syndrome. At diagnosis, lesions are commonly > 2 cm, with invasion of muscularis propria and metastasis to regional lymph nodes. Multiple lesions may be found in up to 40% of cases [9].
USG plays a limited role in the imaging of small bowel NETs. The most common imaging study obtained for the diagnosis of small bowel NETs is a multiphase CT scan. Gastrointestinal NET’s are graded according to the 2010 WHO classification of tumours of the digestive system based on the proliferative index, which is assessed by the percentage of cells that stain positively for Ki-67 and mitotic rate. The accepted surgical approach for resection of small bowel NET’s is an open abdominal operation, to achieve the goals of careful palpation of the entire small bowel and adequate resection of mesenteric lymph nodes while preserving vascular inflow and outflow to the remainder of the intestine. The need for resecting the primary tumour is to treat or avoid the situations that lead to symptoms, that is, bowel obstruction, bleeding, mesenteric fibrosis, peritoneal dissemination and reducing the risk of further metastasis.
In our case there was a vague clinical presentation of an abdominal lump with only dull aching pain for which a preoperative diagnosis of gastrointestinal stromal tumour was made on cect scan. The tumour proved to be a neuroendocrine tumour on histopathology of the operative specimen which was a rare incidental finding.
Conclusion
Small intestinal NET’s are highly prone to metastasize, are fairly slow growing and associated with relatively favourable survival durations compared to other metastatic cancers. Regarding prognosis, patients with well-differentiated duodenal NET’s have an average global 5-year survival rate of nearly 85% [10]. It is 65% for patients with localized disease and only 36% for those with distant metastasis [11]. The stage of disease at diagnosis highly influence prognosis, with a 10-year survival of 95% for patients with local disease and 10% for those with distant metastases [11]. The prognosis of these NETs is generally unfavourable when compared with other location of tumours of comparable size since they have a higher tendency to grow and spread before the diagnosis is confirmed [12,13]. The diagnosed incidence of SINETs has tripled over the last three decades, likely from frequent use of abdominal radiologic imaging and endoscopic procedures [14,15].
For more information about Journal : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00058.pdf
https://ijclinmedcasereports.com/ijcmcr-cr-id-00058/
0 notes
Text
Fight Against GI Cancer: Why A Surgical Gastroenterologist is Necessary for GI Surgeries?

Although several cancers are one of the main reasons for deaths globally, GI cancers are the most common cause of death. GI cancer is the collective term of different types of cancerous diseases that affect the digestive tract. So, if you have a cancerous tumor in the esophagus, stomach, liver, colon, or other parts of the digestive system, the doctors will categorize it as GI cancer.
Gastrointestinal cancers begin in the lining of the cells of one or more organs of the GI tract. Cancer may metastasize to the digestive organs and spread to lymph nodes and other surrounding tissues.
A Surgical Gastroenterologist is Important for the treatment of GI Cancers
Whenever we think of a GI surgeon, we think of problems with the stomach and intestine. However, a surgical gastroenterologist does much more than tackle heartburn, indigestion, and acidity issues.
Surgical gastroenterology is a sub-specialty field of medicine dealing with diseases related to the entire human gastrointestinal tract. It means that a GI surgeon has received formal training in treating disorders related to several GI tract organs such as the esophagus, stomach, pancreas, liver, gall bladder, and biliary tract, small and large intestine, rectum, and anus.
As diseases of the gastrointestinal system are far common in India today, surgical gastroenterology is a well-recognized field, especially by the National Board of Examinations. A surgical gastroenterologist or a GI surgeon has received training to provide tertiary care for patients. They have experience in complicated GI surgeries, including the treatment of different types of gastrointestinal cancers.
With the advancement in medical technology, the profession of a GI surgeon has evolved from a pure diagnostician to an essential member of the oncology team. They hold a crucial place towards ensuring optimum patient care. As a GI cancer surgeon, the medical professional is equipped in:
a. Accurate risk assessment and early detection of GI cancers.
b. Interpretation of laboratory tests and investigations to arrive at a logical diagnosis.
c. Emergency GI surgeries such as gastrointestinal bleeding, trauma, etc.
d. Carrying out endoscopic procedures, laparoscopy, and other minimally-invasive surgical procedures.
e. Proficient pre-operative and post-operative care.
f. Pain management techniques and palliative surgeries.
Whether caused by a lifestyle issue or congenital anomalies, surgical gastroenterologists advise regular medical screenings and immediate medical attention to treat cancer. So, do not miss out on routine medical checkups at the GI surgeon's clinic.
How are GI Cancer Surgeries different than Other Surgeries?
The digestive system is one of the most crucial systems of our body. It does the function of breaking down food into nutrients that the body can assimilate for energy, cell growth, and repair. Without the efficient working of the digestive system, it becomes difficult for the patient to survive. Let’s understand how GI cancer surgeries are more complicated:
1. Esophageal Cancer Surgery
With the help of an esophagectomy, the GI surgeon will remove the cancerous tumor and the affected part of the esophagus. The procedure also includes a resection to connect the healthy section of the esophagus to the stomach so that the patient can swallow food easily.
2. Stomach Cancer Surgery
If a patient has stomach cancer and a total gastrectomy is necessary, the GI surgeon will remove the stomach and connect the esophagus to the small intestine. This way, the doctor can ensure the passage of food and absorption of nutrients.
3. Colon Cancer Surgery
If the GI surgeon is undertaking a colectomy, the doctor will remove a part of the colon affected by cancer. The surgical procedure also involves attaching the remaining of the colon to the digestive tract to ensure efficient functioning. For example, during the right hemicolectomy, the doctor will remove the ascending colon and attach the end of the small intestine to the transverse colon.
4. Liver and Biliary Tract Cancer Surgery
If the patient is suffering from liver and biliary tract cancer, the GI surgeon has to undertake a complicated biliary tract surgery to remove the tumor. The surgery will depend on the size and location of the tumor. For example, in cases of Intrahepatic bile duct cancers, the surgeon may have to cut out a piece of the liver as well. It is essential to work with an experienced surgical gastroenterologist because, after the resection of tumor, the doctor will have to undertake a reconstruction of the biliary tract for the optimum digestive function of the body.
5. Whipple’s Procedure for Pancreatic Cancer
The procedure to remove the cancerous tumors from the head of the pancreas, duodenum, gall bladder and bile duct is called Whipple’s procedure or Pancreaticoduodenectomy. Usually, the surgery involves removing tumors. It is a proven surgical procedure to treat pancreatic cancer in the head of the organ. After the surgery, the GI surgeon will reconstruct/reconnect the remaining organs for effective digestion. The medical professional may undertake: 1) Pancreatojejunostomy for pancreatic juices 2) Hepaticojejunostomy for biliary juices 3) Gastrojejunostomy for food and gastric juices.
And, so when it comes to GI cancer surgeries, surgical gastroenterologists take special care in removing the tumor & the affected tissues and ensure accurate reconstruction of the remaining of the GI tract.
So, whether you undergo surgery for diagnosing cancer, staging cancer, removing the cancerous tumor and surrounding tissues to prevent the spread of the disease, or as a preventative measure, choose a reputed and experienced GI surgeon as a part of your oncology team.
For the best GI cancer treatment, consult Surat’s first National Board Certified HPB and GI cancer surgeon.
0 notes
Photo



From Wikipedia:
Billroth II, more formally Billroth's operation II, is an operation in which a partial gastrectomy (removal of the stomach) is performed and the cut end of the stomach is closed. The greater curvature of the stomach (not involved with the previous closure of the stomach) is then connected to the first part of the jejunum in end-to-side anastomosis. The Billroth II always follows resection of the lower part of the stomach (antrum). The surgical procedure is called a partial gastrectomy and gastrojejunostomy. The Billroth II is often indicated in refractory peptic ulcer disease and gastric adenocarcinoma.
Over the years, the Billroth II operation has been colloquially referred to as any partial removal of the stomach with an end to side connection to the stomach as shown in the picture; however, technically, this picture is a modification of Billroth's operation called a partial gastrectomy with a Kronelein anastomosis where the divided end of the stomach is directly anastomosed to the side of the jejunal loop.
Von Hacker was the first person to refer to the Billroth II partial gastrectomy operation writing from Billroth's clinic in 1885.
So a Billroth II is basically removal of the antrum of the stomach and connecting it to the jejunum (the second part of the small intestine).
Billroth I, more formally Billroth's operation I, is an operation in which the pylorus is removed and the distal stomach is anastomosed directly to the duodenum.
The operation is most closely associated with Theodor Billroth, but was first described by Polish surgeon Ludwik Rydygier.
The surgical procedure is called a gastroduodenostomy.
Second and third pictures are from Grant's Atlas.
1 note
·
View note
Text
Enteral Feeding Devices Market: Facts, Figures And Analytical Insights, 2021 To 2027


The global enteral feeding devices market was valued at US$ xx million in the year 2019. This market is estimated to be valued at US$ xx million in the year 2020, and is expected to reach US$ xx million by the year 2025, with an estimated CAGR of 6.10% during the forecast period (2020−2025). Enteral feeding is a process of delivering nutrition or medications directly in the stomach or intestine. Enteral feeding devices are used to feed specialized diets to elderly or bedridden patients suffering from chronic ailments. Enteral feeding is the preferred route of nutrition delivery as compared to parenteral feeding because enteral feeding avoids complications, such as infection, sepsis, liver & gallbladder disorders, etc.
Key Insights:
Latest Updates
Analyst Views
Future Outllook og the Market
Get Free PDF Brochure of this Report @ https://www.fostermarketresearch.com/product/industry/medical-devices/global-enteral-feeding-devices-market/Pdf%20Brochure/
Competitive Landscape:
Key players in the global enteral feeding devices market include: Fresenius Kabi, Nestlé S.A., Danone, B. Braun Melsungen Ag, Avanos Medical, Cardinal Health, Inc., Moog, Inc., CONMED Corporation, Cook Medical, Becton, Dickinson and Company, Abbott Laboratories, Boston Scientific, Vygon Group, Applied Medical Technology, and Amsino International, Inc, among others.
In December 2018, Nestlé Health Science opened the new Nestlé Product Technology Center in New Jersey with an investment of US$ 70 million, with the aim of establishing a global R&D hub to upgrade the company’s offerings in the nutrition division.
Market Dynamics:
Factors such as growing demand from home care sector, prevalence of chronic diseases, incidence of preterm birth, and growing geriatric population are driving the enteral feeding devices market growth. Soaring number of malnutrition patients across the globe is another significant factor propelling the market growth. For instance, according to a World Health Organization (WHO) report, from 2017, around 2 billion people across the globe lack key micronutrients like vitamins and iron. Thus, enteral feeding is the first line of choice to serve suitable amount of nutrients in malnourished patients and those who are unable to take nutrients orally.
Geriatric population suffering from neurological conditions such as multiple sclerosis, stroke, and dementia that impact swallowing is the biggest target population for this market. Therefore, facility of nutritional support in the form of oral nutrition supplements and enteral nutrition feeding tube mitigate the challenges of nutrition deficit among these diagnosed population.
For More Information of this Report @ https://www.fostermarketresearch.com/medical-devices/global-enteral-feeding-devices-market/
Market Taxonomy:
By Product Type
Enteral Feeding Tubes
Enterostomy Feeding Tubes
Standard TubesStandard Gastrostomy Tubes
Standard Gastrojejunostomy Tubes
Standard Jejunostomy Tubes
Low-Profile Gastrostomy TubesLow-Profile Gastrostomy Tubes
Low-Profile Gastrojejunostomy Tubes
Low-Profile Jejunostomy Tubes
Nasoenteric Feeding TubesNasogastric Feeding Tubes
Nasojejunal Feeding Tubes
Nasoduodenal Feeding Tubes
Oroenteric Feeding Tube
Enteral Syringes
Enteral Feeding Pumps
Administration Sets
Consumable
By Age Group
Adult
Pediatrics
By Application
Gastrointestinal Disease
CancerHead & Neck Cancer
Gastrointestinal Cancer
Liver Cancer
Pancreatic Cancer
Esophageal Cancer
Others
Malnutrition
Hypermetabolism
Neurological Disorder
Others
By End User
Hospital
Ambulatory Surgical Center (ASCs)
Home Care Settings
By Region
North America
Europe
Asia-Pacific
Latin America
Middle East and Africa
Request for Customization of this Report @ https://www.fostermarketresearch.com/product/industry/medical-devices/global-enteral-feeding-devices-market/Customization/
Benefits You Gain With Our Research Methodology:
Develop your Business strategies to refine the profits in near team.
Grow your Business profit ratio through our analytics report.
Acquire the valuable insights on different products, services and technology along with their obsolescence nature in the foreseen period.
Gain and upper hand on competition by having competitive financial, growth and economic data.
Identity future threats by our accurate forecasting strategies.
Obtain Go-To market strategy to increase your chances in the existing market.
Buy Now This Business Strategic Report to Improve Your Profits @ https://www.fostermarketresearch.com/product/buy/medical-devices/282/
About Foster Market Research:
Foster Market Research is a global market intelligence and advisory firm engaged in providing data-driven research extract from rigorous analysis, to the clients to make critical business decisions and execute them successfully. Foster connects over various distribution channels and numerous markets for great understanding of the trends and market to deliver our clients with accurate data.
Our focus is on providing market research that delivers a positive impact on your business. We work continuously to provide our clients with the most accurate analytics data and research reports without any delay so as to improve their business strategies and provide them with rich customer experience.
Contact Us:
1701 Royal Lane,
#1306, Dallas
Tx-75229
Phone: +1 469 4981929
Email: [email protected]
0 notes