#Laryngospasm
Text
Have you ever experienced those moments where your throat closes from a breath and you can’t breathe?
They’re scary, but you get used to them. Something about experiencing panic over and over gets you used to the sensation. Oh it still grips your heart and beads sweat on your brow but it’s familiar now. Like a funhouse ride your mind has memorized even if your body experiences like the first time.
Soon the steps become second nature. Hold your breath, don’t try to breathe. Elbows over the head. Stand up. Wait it out. Don’t worry about trying to breathe. You won’t pass out (you never have).
The new step in the dance you learn is to run.
Run to somewhere they can’t see you. Run to somewhere a good meaning citizen can’t take you by the shoulders and try to “help”. You know how to deal with this, but you know you can’t assure them you’ll be fine as your throat closes.
There’s only so much air in your lungs, you can’t waste it on telling someone to get away.
It’s a good thing they care, but in the moment it’s just another pressure tightening around you. A different fear you’re not as used to, another piece to place into the puzzle while you’re already trying to keep your eyes open.
They can see your body panic but they can’t see your mind roll it’s eyes in boredom. It looks like you’re dying, but you can’t tell them it doesn’t really hurt. Not anymore. Not like the first time.
So you run and you hide and you go through the steps of your dance until your body relaxes and you can breathe. It doesn’t take but a minute or two, but you find yourself wanting to remain hidden. Just for a little longer.
Until you walk back with a smile. Explain. Apologize. Go about your day.
.
.
.
Why doesn’t this feel like it’s not about air anymore?
#freeform#choking tw#complex feelings#these actually have a name btw#Laryngospasm#your vocal chords go FUCK YOU and close up#I’ve had them ever since I was a kid#not often but enough that I’m used to them#happy America for running away from someone so they don’t call an ambulance for something you can handle#but yeah#how are you supposed to tell everyone you’ll be fine when your body thinks it’s dying#complex social situation for sure
23 notes
·
View notes
Text
uh oh!
the red (purple?) onions in the salad were a mistake!
0 notes
Text
Straight Outta Neutrophils
Back in July, when I was dealing with a sick 9 month baby, I had never heard of neutrophils. Three months on, my learner plates have come off, so to speak, as I’ve learned a whole lot more about them.
I’m currently coming to terms with the fact that, Kaydence has got a rare blood disorder called Severe Chronic Neutropenia (SCN). Which is also a rare type of primary immunodeficiency. And what I…

View On WordPress
0 notes
Text
Influenza Persists by Uday Jain in Journal of Clinical and Medical Images, Case Reports (JCMICR)
Introduction
In the US, influenza (flu) causes 9 to 45 million illnesses, leading to 12,000 to 61,000 deaths annually (10.1001/jama.2020.14772). World Health Organization estimates that worldwide annually there are about one billion infections, 3-5 million severe illnesses, and 300,000-500,000 deaths (10.1038/s41572-018-0002-y). Influenza is caused primarily by influenza A and influenza B viruses. Influenza A is the cause of pandemics. A schematic diagram of influenza A virus is presented in (Figure 1). Influenza will continue to be prevalent because its current vaccines are safe but only 30-60% efficacious. In contradistinction, COVID-19 vaccines have an efficacy of about 90%. Additionally, new zoonotic influenza strains intermittently migrate to humans. Influenza is a major part of “The New Normal
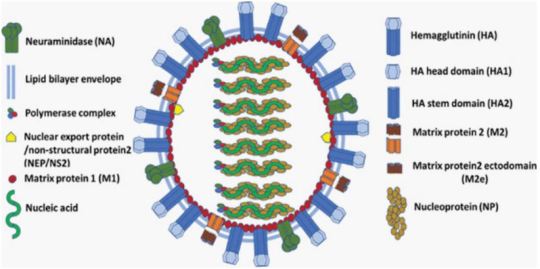
Figure 1: A schematic diagram of influenza A virus.
Coinfection
Since the start of COVID-19 pandemic, influenza is of greater concern. Overlapping spread of both diseases is a major strain on the health care system. Their coinfection is not common but may cause more severe disease. Influenza vaccination and therapy are important in addition to COVID-19 vaccination and therapy, especially in persons at increased risk.
Incubation
Influenza’s median incubation period is 2 days. Patients are infectious for a day before and 5 to 7 days after symptoms. COVID-19 has an incubation period of 4-12 days, a median of about 5 days. Patients are most infectious from 2 days before symptom onset. Influenza symptoms peak in 3-7 days. COVID-19 symptoms peak in second or third week. The spread of both viruses is facilitated by transmission by asymptomatic patients.
Transmission
About one-half of influenza A cases are due to aerosol transmission (10.1038/s41598-019-38825-y). Adequate ventilation can reduce it. Precautions utilized during the COVID-19 pandemic reduced the incidence of influenza in 2020. Used appropriately, surgical masks reduce the concentration of aerosolized influenza virus by about ten-fold and are adequate for prophylaxis against influenza (10.1016/j.jhin.2013.02.007; 10.7326/M20-3213). Transmission by respiratory droplets can also be reduced by masking. Transmission by direct contact can be reduced by hand and general hygiene. COVID-19 is transmitted in a similar manner. Social distancing reduces transmission by all the mechanisms. Influenza is less contagious and causes less severe disease than COVID-19. Quarantine recommended for COVID-19 patients is not necessary for those with influenza. Children play an important role in transmitting influenza. Healthcare providers should take precautions to avoid infecting themselves and others.
Influenza-Like Illness (ILI)
The Centers for Disease Control define ILI as fever 100°F (38°C) or greater and cough or sour throat that is not due to another known cause including streptococcal pharyngitis (strep throat). ILI’s causes can be benign such as common cold (nasopharyngitis caused by rhinovirus or other viruses) or severe including sepsis, meningitis, COVID-19, and SARS. Often there is an abrupt onset. SARS leads to severe disease in most of the infected. Influenza and COVID-19 cause mild disease in most of the infected (10.1016/S1473-3099(20)30484-9). SARS is currently not prevalent. Severe disease due to COVID-19 and SARS occurs primarily in the elderly. Influenza is more evenly distributed across the age groups. ILI can cause immunosuppression, leading to bacterial pneumonia, necessitating antibiotics (10.1097/QCO.0000000000000347).
After general anesthesia, children with influenza have a longer hospital length of stay and increased risk of requiring intensive care (10.1186/1471-2253-11-16). Routine surgery should be postponed for about four weeks in a patient with ILI. Unvaccinated patient should be offered influenza vaccination after the acute phase of ILI has passed and before the surgery. Before performing urgent surgery, severe causes of ILI should be excluded
Upper Respiratory Tract Infection (URI) Excluding ILI
In cold weather URI is common, especially in children. Often it is due to common cold, or noninfectious allergic or vasomotor rhinitis. Less commonly, it can be early presentation of more serious illness including ILI, COVID-19, strep throat, and herpes simplex. Early in infection it is difficult to distinguish between different etiologies of URI.
URI may cause sneezing, coughing, headache, malaise, rhinorrhea, sore throat, sinusitis, and bronchitis. Subsequently, bronchi may be hyperreactive for about six weeks. Pulmonary complications associated with surgery in a patient with URI are bronchospasm, laryngospasm, coughing, breath holding, postintubation croup, episodes of desaturation, atelectasis, and pneumonia. Anticholinergics and bronchodilators may not be beneficial. Perioperatively, adequate hydration and humidification should be maintained. There are no pediatric or adult anesthesia closed claims that implicate URIs including influenza with serious adverse events. There is a very small incidence of viral myocarditis in patients with URI including ILI. It may lead to serious arrhythmias and refractory heart failure (10.1016/j.jcrc.2018.06.001; 10.1038/s41569-020-00435-x).
Diagnostics Tests
These include nucleic acid amplification via polymerase chain reaction (PCR) and antigen-based immunological assays. A PCR test can be performed even at the point-of-care with results available within an hour (10.1016/S2213-2600(20)30469-0). This can facilitate infection control and utilization of antiviral therapeutics. It is especially useful for patients who have severe symptoms or are hospitalized. Test for COVID-19 may also be performed if indicated.
Influenza Vaccine
It is the best preventive measure. Although not very efficacious, it substantially reduces morbidity and mortality because of high prevalence of influenza. It is recommended for anyone over 6 months of age. It is especially beneficial in the presence of age <2 years or >65 years, pregnancy, and pre-existing conditions (10.1001/jama.2020.14772). Lack of vaccination in pregnancy not only increases the risk to mother but also increases the risk of preterm birth, fetal death, infant respiratory infection and hospital admission. The T cell response vaccines elicit is substantially weaker than the antibody response. Children may need two doses of vaccine, at least four weeks apart. The vaccine should be administered at least one week before surgery. It takes two weeks to develop full effect. As the protection wanes over time, mid-September to mid-October is preferred for vaccination. Influenza and COVID-19 vaccines may be administered together. The vaccine may be administered to surgical inpatients (10.7326/M15-1667).
Available Vaccines
The influenza virus mutates frequently. Quadrivalent vaccines protect against four of the currently most prevalent strains of influenza. The vaccines are altered every year for the predicted prevalent strains. Nine vaccines from four manufacturers are available in the US. Inactivated influenza vaccine is most commonly used. It is approved for persons above 6 months of age. As older individuals have a reduced response, vaccines that have a higher dose or are adjuvanted are recommended for persons above 65 years of age. The vaccine is usually administered intramuscular, but a lower dose intradermal vaccine is non-inferior (10.1001/jamanetworkopen.2020.35693).
Live-attenuated influenza vaccine is administered via nasal spray. It is approved for ages 2-49 years. It may be preferable in some situations such as vaccinating many persons in a community. It should be avoided if the patient or someone nearby has a suppressed immune system. Hence, it is not suitable for inpatients.
Recombinant vaccine and cell culture vaccine do not contain egg products. They are especially suitable for persons who need to avoid eggs because of allergy or dietary preferences.
Available Vaccines
Universal vaccines that provide durable response against all influenza strains are in human trials (10.1038/s41591-020-1118-7). These vaccines generate antibodies against the viral hemagglutinin protein stem (stalk) domain (HA2). Current vaccines generate antibodies against the immunodominant globular head domain (HA1), which is variable and mutates much more frequently. Vaccines utilizing mRNA are also in human trials. They are likely to have greater efficacy but more side effects than current vaccines. A major advantage of the mRNA vaccines is that they can be readily modified to match mutations in the virus.
Benefits of Vaccination for Adults
Influenza vaccine reduces the risk of respiratory and cardiovascular adverse outcomes and mortality among adults, especially in the presence of pre-existing conditions and advanced age. This was confirmed in a meta-analysis of studies on all adults (10.1016/j.arr.2020.101124). Another meta-analysis found that vaccine reduced the risk of adverse cardiac outcomes, especially in sicker patients (10.1001/jama.2013.279206). Preoperative vaccination is beneficial. A large study of elderly patients who had major surgery found preoperative vaccination reduced by about one-half the risk of pneumonia, intensive care admission, and death (10.1093/infdis/jix616). Patients also had shorter hospital stays and reduced resource utilization.
Influenza Therapeutics
These include neuraminidase inhibitors oseltamivir, zanamivir, peramivir, and laninamivir; cap-dependent endonuclease inhibitor baloxavir; and matrix protein M2 ion channel blockers (10.1001/jamanetworkopen.2021.19151). They attenuate viral replication. They provide postexposure prophylaxis. When started within 2 days of symptom onset, they reduce duration and severity of the disease, and complications. They also reduce transmission of influenza virus. However, their efficacy is limited, especially in patients with serious illness. They are expensive and not widely utilized. Although influenza and COVID-19 have similar initial symptoms, their therapeutics are different. Thus, dexamethasone reduces mortality for hospitalized COVID-19 patients on respiratory support but may increase mortality for hospitalized influenza patients (10.1001/jama.2020.15260).
Influenza Pandemics
They are usually caused by zoonotic influenza A virus strains migrating to humans. The 1918 “Spanish flu” pandemic caused by influenza A H1N1 virus led to more than 40 million deaths worldwide. H1 denotes haemagglutinin subtype 1 and N1 denotes neuraminidase subtype 1. The pandemics of 1957, 1968 and 2009 were caused by influenza A H2N2, H3N2, and H1N1 viruses, respectively. The 2009 “swine flu” influenza A H1N1 virus that originated from pigs was antigenically different from previously dominant influenza A H1N1 viruses. It caused 150,000-600,000 deaths worldwide. Avian influenza “bird flu” caused by H5N1 and H7N9 is not prevalent. Overlapping occurrence of influenza pandemic and COVID-19 will be devastating. Vigilance and prompt action are essential to prevent zoonotic influenza A virus strains from migrating to humans.
Conclusion
Influenza is a prevalent respiratory disease that will continue to affect anesthesia practice in the foreseeable future. With appropriate management, the risk of adverse outcomes is low. Vaccination is highly recommended, especially preoperatively.
For more details : https://jcmimagescasereports.org/author-guidelines/
#US#COVID-19#humans#therapy#appropriately#influenza#prophylaxis#ILI#SARS#anesthesia#laryngospasm#arrhythmias#Uday Jain#jcmicr
1 note
·
View note
Text
A Writer's Blueprint for Realistic Drowning Scenes
This guide is designed to help writers depict drowning scenes with authenticity and detail. I’ll walk you through the step-by-step process of drowning, the physical signs to look for and clear up some common misconceptions. With this information, you’ll have the tools to craft vivid, compelling, and believable drowning scenarios that will captivate your readers and add depth to your narrative.
Fair warning; this is a comprehensive and pretty explicit guide, so if you're uncomfortable with those topics, please just scroll away.
The Stages of Drowning
1. Initial Entry
When a person first enters the water, especially unexpectedly, their initial reaction is often one of shock and panic. The sudden change in environment, temperature, and the feeling of being submerged triggers an immediate response from the body.
Shock Response
Cold Water Immersion: Sudden immersion in cold water can cause a cold shock response, which includes involuntary gasping, hyperventilation, and a rapid increase in heart rate and blood pressure.
Panic and Disorientation: The person may become disoriented and panic, struggling to stay afloat and breathe normally.
2. Involuntary Breath-Holding
As the person struggles to keep their head above water, they instinctively hold their breath to prevent water from entering their lungs.
Burning Sensation in Lungs
The buildup of carbon dioxide in the blood creates a burning sensation in the lungs, which intensifies the feeling of panic.
Increased Heart Rate and Blood Pressure
The body's stress response causes an increase in heart rate and blood pressure, further depleting oxygen reserves.
3. Uncontrolled Breathing
When the person can no longer hold their breath, the body's reflexes take over, leading to involuntary attempts to breathe.
Aspiration of Water
Water enters the mouth and is aspirated into the lungs, causing coughing, choking, and a strong gag reflex.
Coughing and Choking
The person may cough and choke as water enters the respiratory tract, leading to more panic and struggle.
Gasping for Air
The body's desperate attempt to get oxygen leads to gasping, but often results in inhaling more water.
4. Laryngospasm
The body's protective reflex to prevent water from entering the lungs can cause the vocal cords to spasm, temporarily sealing the airway.
Temporary Airway Closure
The laryngospasm closes the airway, preventing both water and air from entering the lungs.
Increased CO2 and Decreased O2
As carbon dioxide levels rise and oxygen levels fall, the person becomes increasingly hypoxic.
5. Loss of Consciousness
Due to the lack of oxygen, the person loses consciousness.
Hypoxia and Hypercapnia
Hypoxia (lack of oxygen) and hypercapnia (excess carbon dioxide) cause confusion, dizziness, and loss of motor control.
Fading Senses
Vision blurs, hearing diminishes, and the sense of touch becomes numb.
Blackout
The brain, deprived of oxygen, shuts down, leading to unconsciousness.
6. Cardiac Arrest
Prolonged oxygen deprivation leads to cardiac arrest, where the heart stops beating.
Cessation of Breathing
Respiratory effort ceases as the brain's control over breathing is lost.
Heart Stops Beating
The heart, deprived of oxygen, stops beating, leading to complete circulatory failure.
Brain Damage and Death
Without intervention, brain cells die from lack of oxygen, leading to permanent brain damage and eventually death.
7. Aftermath (if Rescued)
If the person is rescued and resuscitated, there are immediate and long-term consequences to consider.
Immediate Aftermath
CPR and First Aid: Immediate resuscitation efforts, including CPR and the use of a defibrillator if necessary.
Hospitalization: The person will likely need to be hospitalized for further treatment and monitoring.
Long-Term Effects
Lung Damage: Inhalation of water can cause damage to the lung tissues, leading to conditions like pneumonia or acute respiratory distress syndrome (ARDS).
Neurological Damage: Prolonged lack of oxygen can result in brain damage, affecting cognitive and motor functions.
Psychological Impact: Survivors may experience PTSD, anxiety, and a lasting fear of water.
Physical Appearance During Drowning
1. Initial Entry
Shock Response
Wide Eyes and Gasping Mouth: Eyes are wide open, and the mouth is often open in a gasp or scream.
Flailing Limbs: Arms and legs are moving rapidly in an attempt to regain balance and stay afloat.
2. Involuntary Breath-Holding
Tensed Muscles
Rigid Body: Muscles are tensed, and the body may appear stiff as the person tries to maintain control.
Strained Facial Expression: The face may show strain, with furrowed brows and tightly closed eyes.
3. Uncontrolled Breathing
Coughing and Choking
Reddened Face and Eyes: The face may turn red from the effort of coughing and choking.
Foaming at the Mouth: A frothy mixture of saliva and water may be visible around the mouth.
Gasping for Air
Open Mouth and Wide Eyes: The mouth is open wide in an attempt to gasp for air, and the eyes may be bulging with fear.
Erratic Movements: The person’s movements become more erratic and uncoordinated as they struggle to breathe.
4. Laryngospasm
Silent Struggle
Mouth Opening and Closing: The person may appear to be gasping silently as the airway is temporarily sealed.
Clenching Throat: Hands may instinctively clutch at the throat in a futile attempt to open the airway.
5. Loss of Consciousness
Limp Body
Floating Limply: The body becomes limp and may float face down or sink slightly below the surface.
Pale or Blue Skin: Skin may turn pale or blue (cyanosis) due to lack of oxygen.
Relaxed Facial Features
Closed Eyes: Eyes close as the person loses consciousness.
Slack Jaw: The jaw may go slack, and the mouth could be partially open.
6. Cardiac Arrest
Unconsciousness
Still Body: The body is completely still, with no voluntary movements.
Gray or Blue Skin: Skin color becomes ashen, gray, or blue, particularly around the lips and extremities.
7. After Drowning (Post-Rescue Appearance)
If the person is rescued, their appearance post-drowning can indicate the extent of their ordeal and the immediate aftermath.
Immediate Aftermath
Waterlogged Clothing: Clothes may be heavy and waterlogged, clinging to the body.
Coughing and Vomiting: The person may cough up water or vomit as they are resuscitated.
Shivering: If the water was cold, the person might be shivering uncontrollably due to hypothermia.
Long-Term Appearance
Bruising and Cuts: There may be bruises or cuts from the struggle in the water or the rescue process.
Pale or Blue Skin: Skin color might still show signs of cyanosis if oxygen levels are low.
Labored Breathing: Breathing may remain labored and shallow as the lungs recover.
Ways to Drown
Being Tied Down with a Stone
An ancient method where a person is weighted down with a heavy object, preventing them from surfacing.
Pulled Under by a Strong Current
Strong currents or rip tides can overpower a swimmer, pulling them away from safety and making it difficult to stay afloat.
Trapped Under a Capsized Boat
In the event of a boat capsizing, a person can become trapped underneath, unable to reach the surface for air.
Caught in Underwater Vegetation
Dense underwater plants can entangle a swimmer, restricting their movements and preventing them from surfacing.
Unable to Swim in Deep Water
Lack of swimming skills or fatigue in deep water can lead to drowning if the person cannot keep themselves afloat.
Falling Through Ice
Falling through thin ice can trap a person in freezing water, with the ice making it difficult to find an exit.
Getting Caught in a Riptide
A riptide can drag a swimmer out to sea, making it hard to swim back to shore due to the strong current.
Swimming Exhaustion
Overexertion while swimming can lead to exhaustion, making it impossible to continue treading water or swimming to safety.
Diving Accident
A diving mishap, such as hitting one’s head or getting disoriented underwater, can result in drowning.
Shipwreck
In a shipwreck scenario, a person may be stranded in open water, facing potential drowning due to exhaustion, exposure, or lack of flotation devices.
Common Misconceptions About Drowning
1. Drowning is Always Loud and Dramatic
Many people believe that drowning involves a lot of splashing, shouting, and waving for help. In reality, drowning is often a silent and quick event.
Instinctive Drowning Response: When a person is drowning, their body prioritizes breathing over waving or shouting. The struggle to get air means they can’t call for help.
Quiet Struggle: Drowning individuals might be bobbing up and down, with their mouths at water level, making little noise as they gasp for air.
2. People Always Recognize Drowning
It's a common belief that drowning is easily recognizable. However, many drownings go unnoticed until it’s too late.
Subtle Signs: Drowning can look like someone treading water or trying to swim. Signs can be subtle, such as bobbing up and down, head tilted back with mouth open, or eyes glassy and empty.
Misinterpreted Behaviors: Bystanders might mistake a drowning person for someone playing or simply floating.
3. Only Weak Swimmers Drown
Many assume that only those who can’t swim well are at risk of drowning, but even strong swimmers can drown under certain conditions.
Fatigue and Cramps: Strong swimmers can become exhausted, suffer from cramps, or panic, leading to drowning.
Environmental Factors: Strong currents, cold water, and underwater hazards can overwhelm even the best swimmers.
4. Drowning Happens Immediately
There’s a misconception that drowning happens instantly. While it can be quick, it often takes a few minutes for a person to drown.
Struggling Phase: The initial struggle can last for 20-60 seconds, during which the person is trying to stay afloat and breathe.
Silent Submersion: After this, they may silently submerge, often unnoticed.
5. Drowning Only Happens in Deep Water
Many people think that drowning only occurs in deep water. However, shallow water can be just as dangerous.
Shallow Water Drowning: Drowning can occur in as little as a few inches of water, especially with young children or if someone is unconscious.
Bathtubs and Pools: Many drownings occur in bathtubs, kiddie pools, or even buckets.
6. Life Jackets Are Only Needed on Boats
It's commonly believed that life jackets are only necessary when boating, but they are crucial in many other water-related activities.
Swimming and Water Sports: Life jackets provide essential buoyancy and can save lives in swimming pools, lakes, rivers, and during water sports.
Unexpected Situations: Wearing a life jacket can prevent drowning in unexpected situations, like sudden falls into water.
7. People Float After Drowning
A prevalent myth is that drowning victims float on the surface after they die, but this is not always the case.
Initial Sinking: Initially, a drowned body may sink due to the density of the tissues and lack of air in the lungs.
Later Floating: Bodies often float later due to gas buildup from decomposition, but this can take days.
8. Drowning Victims Always Look Distressed
People often think that drowning victims will look distressed or visibly in danger, but many can appear calm and quiet.
Passive Drowning: Drowning individuals may appear to be calmly treading water or just floating.
Lack of Visible Struggle: There may be no visible struggle, making it hard to identify the danger.
9. CPR is Ineffective After Drowning
Some believe that once a person has drowned, CPR cannot help. However, immediate CPR can be life-saving.
Restarting Breathing: CPR can help restart the victim’s breathing and circulation, buying crucial time until emergency services arrive.
Rescue Breathing: Effective rescue breathing can oxygenate the lungs and increase the chances of revival.
Resources
Books
"The Science of Drowning" by Sports Aid Intl
“It offers a significant departure from how drowning is traditionally treated by combining discussions about medical, prevention, and intervention issues.”
Link
"The Perfect Storm: A True Story of Men Against the Sea" by Sebastian Junger
A gripping account of the 1991 storm that hit the North Atlantic and the fishermen caught in its deadly grip, providing insights into the perilous nature of the sea and drowning.
Link
Articles
"Drowning vs Aquatic Distress" by Crunderwood
An article detailing the science of drowning + some interesting points.
Link to article
"Drowning Victim" by SLRG
How to identify a drowning person besides the typical flailing.
Link to article
"Drowning Treatment" by WebMD
Guidelines and tips for healing/treating a drowning person.
Link to article
Websites
American Red Cross: Water Safety Tips
Provides extensive information on water safety, drowning prevention, and emergency response.
Link to website
National Drowning Prevention Alliance
A dedicated organization focused on preventing drowning through education, research, and advocacy.
Link to website
Centers for Disease Control and Prevention (CDC): Drowning Prevention
Offers statistics, prevention strategies, and safety tips to reduce the risk of drowning.
Link to website
Looking For More Writing Tips And Tricks?
Are you an author looking for writing tips and tricks to better your manuscript? Or do you want to learn about how to get a literary agent, get published and properly market your book? Consider checking out the rest of Quillology with Haya Sameer; a blog dedicated to writing and publishing tips for authors! While you’re at it, don’t forget to head over to my TikTok and Instagram profiles @hayatheauthor to learn more about my WIP and writing journey!
#hayatheauthor#haya's book blog#haya blogs#blog masterlist#writing community#writing tools#writer things#writing advice#writer community#writing techniques#writing prompt#writing stuff#creative writing#ya writing advice#writing tips and tricks#writer tools#writers of tumblr#writer blog#writers block#writers on tumblr#writerscommunity#writer stuff#author help#author advice#writing emotions#how to write emotions#emotional writing#writing#author
82 notes
·
View notes
Text
This is kind of a long shot.
I'm wondering if anyone else has had a reaction while under oral anesthesia where they were told that they couldn't breathe/their throat was constricted, something like that? I had this reaction once while under anesthesia, but a previous time I've been under anesthesia, I didn't have this reaction at all.
I was told that this reaction is extremely rare - so rare that the dentist telling me about it said they've only encountered it less then 10 times in their entire years of practice.
I told them I have DID and PTSD (I previously didn't tell them about either. I did not think it was necessary) and they told me that that adds up because every single person who has had that reaction had PTSD.
I'm wondering if anyone else out there has had this ?? Have you had it once, but not other times? I don't know.
I have an upcoming oral surgery next week, but they dismissed my concerns and wouldn't opt for having the surgery at a safer location, at a hospital where they would have the tools necessary to help me and make sure such a reaction doesn't happen again. I'm terrified that this is going to happen again, and I'm terrified that it might result in my actual death.
I guess I wonder if anyone else has had this happen, do you know why?? What it's called??
When I Google, something called laryngospasm comes up, and I have no idea if that could be it.
I'm desperately hoping that maybe there's a chance it won't happen again, I'll just turn out lucky.. I don't know..
I've had a tooth infection for like probably a fucking year now and I've had so many things come up that have forced me to put off getting it treated outside of my control, from being denied insurance, having to be put on insurance again, most places in general not taking my insurance, or insurance denying coverage, and the previous oral surgeon it was GOING to be treated at no longer taking my insurance and so having to find a new place.
I'm sorry about so many tags, I'm trying to reach as wide amount of people as possible.
#My posts#ActuallyDID#ActuallyDissociative#ActuallyTraumatized#PTSD#CPTSD#OSDD System#DID System#ActuallyPTSD#ActuallyOSDD#Trauma Survivor#Dissociative Disorders#DPDR
37 notes
·
View notes
Text
Phantom Thieves react to getting anesthesia: headcanons from a real anesthetist
Ren: wakes up unusually chatty, thinks the recovery room nurse is Sae in the interrogation room, talks about all the stuff he has to do to increase his social stats
Ryuji: won't shut up about being a Phantom Thief and rats out his friends as Phantom Thieves (fortunately none of the OR staff believe him because they chalk it up to post-op delirium)
Ann: confesses her undying love to the recovery room nurse taking care of her (which destroys Morgana)
Yusuke: wakes up reciting a very long list of all the hospital food he wants to eat, ends up not eating for a while due to having the terrible luck of previously undiagnosed post-op nausea and vomiting (PONV sucks, and known history of it in a patient definitely affects the anesthetic plan. A lot of drugs in our disposal have anti-nausea properties: propofol, decadron, zofran being the most common. But a bunch of others can do the exact opposite and cause nausea: opioids, anesthetic gas, etomidate (which I call vomidate) etc. It's a careful balance of what meds to use and which to avoid, and it depends on the patient.)
Makoto: wakes up alternating between yakuza movie quotes and swearing every other word from surgery pain (a bad habit she got from Sae, who swears like a sailor out of work stress when she thinks Makoto can't hear)
Futaba: takes fore-fuckin'-ever to get to sleep, gets slugged with enough medication to knock out a 100 kg 6 foot tall man (redheads are known for needing higher than average anesthetic to go past the threshold of consciousness and awareness. This is actual book knowledge plus my own clinical experience. Futaba would be a real chore to anesthetize.)
Haru: wakes up throwing hands, swinging fists and feet into OR staff, keeps asking for her axe, has to be restrained to the bed until enough sedatives kick in to calm her down (little kids, teenage girls and big healthy guys tend to wake up violently as the anesthetic wears off. The solution and wonder drug for this: precedex.)
Morgana: makes a weepy proposal to Ann, launches into verbal treatises and theories on the psychology of the Metaverse (which just sounds like incoherent meowing and yowling to the vets)
And for the honorary PTs:
Sojiro: the amount of gunk and spit suctioned out of his mouth before removing the airway device is through the roof (suctioning the mouth and throat is super important during emergence of anesthesia, so that stuff doesn't make the vocal cords spaz out and slam shut, which is laryngospasm, an airway emergency. Smokers tend to produce excessive oral secretions, and if they smoke enough, it can even look gray and brown. Lovely huh?)
Sae: has a low heart rate in the 40s that kind of unnerves OR staff, but that's only because she's very athletic (very fit people can have pretty low baseline heart rate, because exercise remodels the heart to optimize blood output for less work/heart rate. Normal heart rate range is 60-100 bpm, but I've seen Ironman type athletes have 30-40 bpm.)
#persona 5#persona 5 headcanons#ren amamiya#ryuji sakamoto#ann takamaki#morgana persona 5#yusuke kitagawa#makoto niijima#futaba sakura#haru okumura#sojiro sakura#sae niijima#this was fun. hope you learned a bit of medical stuff today
73 notes
·
View notes
Text
Waking up and recovery
Masterlist
So you're all stitched up, but you're still asleep? Guess we'd better wake you up then!
This either happens in the operating room or in recovery, but is mostly the same. The anaesthetist turns off the anaesthetic gas and gives a muscle relaxant reverser. Then you just wait.
Usually within 15 minutes the patient will start waking up. Everyone is slightly different. Some people will flap their hands a bit but are still asleep, others wake up all at once.
What you're looking for is that they can follow a basic command - opening their eyes, squeezing a hand, lifting their head up. This is proof that they can protect their airway and it's safe to remove the et tube.
The cuff on the tube gets deflated and the tube is just pulled out. It usually smells a bit gross by the way. An oxygen mask goes on immediately, and if they get laryngospasm (the vocal chords spasm) then we give positive pressure (force oxygen into their lungs with a bag).
If they were woken up in the OR, they'll go to recovery now. The anaesthetist will bugger off really fast once the tube's out, and the recovery practitioner takes over.
Most patients are very very sleepy after anaesthesia. This is generally fine and makes it easier to do all the paperwork. The recovery nurse will take observations every five minutes, and will look at the surgical site to check for bleeding.
If everything's peachy then the patient will go back to the ward after 30 minutes, otherwise we just wait until all their vital signs are stable and there's no signs of deterioration. If the patient's in a lot of pain they'll get some pain relief (usually morphine).
Congrats! The journey's finished! (well, in the surgical department anyway)
34 notes
·
View notes
Text
Aftermath of Drugging
CW: discussions of non-con drugging, spiking food, medical whump, overdosing, drug abuse, addiction, death, brief BBU-mention
Using drugs as a whump method is pretty common, and rightly so! As one of my favorite tropes, it was interesting to think about how they could affect the Whumpee after the act itself, be it physical or mental.
That's why I made a little compilation (for me and you), if you feel like agonizing your Whumpee even further. There are also some examples in between, for your entertainment!
The research is mostly relating to any downers, meaning any drug that makes you calm or fall asleep, so anesthetics, hypnotics or sedatives. Examples include ketamine, Rohypnol, GBL, propofol and heroin.
Uppers on the other hand have the opposite effect in stimulating the human nervous system. Some of the effects that are noted below are applicable to both kinds of drugs, but keep in mind that stimulants are more of an afterthought in this list. I'm going to recap the effects of both at the end.
I'm not a pharmacist by any means, but as far as reliable research for creative writing goes, this should suffice. No one is going to fact-check your whump fic, bestie 🤍
・・・・・・・・・・・・・・・・・・・
By method:
Ingestion (forcing them to take pills, spiking their food)
→ General indigestion, nausea, dry mouth
Injections via syringe or continuous administration through an IV drip (e.g. in medical settings)
-> Swelling/tenderness/infection/bruising of the injection side
-> High fever (even days after the injection)
→ Anaphylaxis: skin rash, chest tightness, dizziness, nausea, facial swelling
Anaphylaxis is an all-body allergic reaction that can cause mild to severe and even deadly symptoms (shock or coma). It can escalate and should be immediately treated with a shot of adrenaline.
This kind of reaction could be detrimental to Whumper's plans, especially if they intend to keep Whumpee alive for the foreseeable future. So it would be helpful for them to always carry an EpiPen, just in case...
Inhalation (gas or liquid)
→ High risk of choking and (sleep) apnea
-> Irritation of throat, nose and eyes
-> Throat spasms (Laryngospasm)
Includes coughing, difficulty breathing/speaking and the feeling of suffocation. Even though this kind of spasm fades away pretty quickly, they cause severe stress and panic to the aggrieved party, even leading up to lose consciousness again.
Physical side effects:
-> Drowsiness/tiredness, headaches/migraines, tinnitus
-> Dry mouth/throat or excessive drooling
-> Dilated pupils (causing Whumpee to be light-sensitive)
-> Slurred speech
-> Skin rash, itching, hives
-> decreased/increased appetite (give them a little snack...or not)
Motor skills:
-> Muscle relaxation, ataxia (lack of movement control), general weakness
-> Poor coordination
-> Tremors, cramps, spasms
-> Numbness, paralysis of the body or extremities (a local anesthetic would also do that trick)
Vegetative effects:
-> PONV: nausea, vomiting, retching
-> Cold shivers or hot flashes, acute sweating
-> Arrhythmia, low blood pressure and heart rate
-> Labored breathing
-> Vertigo
The physical consequences alone can make the wake-up process a living nightmare for Whumpee. Any after-effects that inhibit them from just getting up and escape are probably the worst in such a situation, making them weak and useless even if no restraints are involved.
Imagine Whumpee just breathing heavily and quivering with cold shivers on a basement floor, unable to shake this uncomfortable feeling off. Their whole system is just trying to get the drugs out, but doing more damage than intended. Numb to the world around them, not even feeling if they are hurt or wounded.
Or imagine the complete opposite: Them being able to get up and stumble to the exit, only to be overwhelmed by intense dizziness and collapsing back onto their knees.
All the while Whumper watches, of course 👀
Did Whumpee eat beforehand?
Prior to any anesthesia, the person has to fast for at least six hours beforehand. Because Whumpees rarely plan their own kidnapping or non-con high, Whumper should wait for the right moment to get it done.
Otherwise, they're risking aspiration or choking and therefore dangerous lung damage up to death; surely the most undesired outcome. Who would have thought that drug abuse can be dangerous...
Impure compounds? In my illegal drugs!?!
If your Whumper's stash really was cut with popular diluents e.g. other medication or lactose, the risks are surprisingly low. The threat of overdosing still comes from the main drug agent.
However, mixing downers and uppers to cancel each other out can lead to a dangerous cycle, which amplifies the side effects and increases the risk to OD.
Mental side effects:
-> Nightmares, paranoia around food/drinks
-> Depression, anxiety, self-loathing (e.g. for not being careful enough)
-> Psychosis, hallucinations (optic, acoustic, in terms of taste etc.)
-> Dissociation, confusion, disorientation
-> Insomnia
-> Reduced anxiety or inhibitions
Now instead of being afraid, Whumpee could go batshit crazy and make fun of Whumper; spitting, biting and insulting their aggressor. An outburst they will probably regret later, when they're calm again and sober enough to understand the damage they have caused themself.
-> Memory loss/amnesia
Cue intimate Whumper, who just plays the part of a worried friend while keeping their love safe and controlled. Vague recollections of past abuse? No, just take another sip from your tea, it's alright...
One could use drugs as a mean of removing memories altogether, I think in the BBU the "drip" is used to erase the whole personality of the Whumpee, making them a blank slate to train however one would like.
Withdrawal:
-> minutes or even days after the initial drugging
-> extreme anxiety up to paranoia
-> nausea, vomiting, indigestion
-> muscle aches
-> flu symptoms like a runny nose, sweating and fever
Depending on the kind of drug and how often it is used, withdrawal can start after just one dosage. "Not even once"-drugs include meth, heroin and crack cocaine. Also, barbiturates have a high risk of dependence. Speaking of it...⬇
Addiction as a long term effect:
-> Organ damage especially of the brain, liver, kidneys and the diseases that follow (including cancer, short weight, heart failure)
-> Loss of interests, behavior/personality change
-> Selling all valuables and ending up in poverty
-> Aggression/violent behavior
-> Shame and guilt
Isolated, financially and mentally unstable, Whumpee's life had been ruined with just a single act. Even Caretaker turned their back on their former friend. But Whumper would love to help Whumpee become sober again, under just a few conditions.
On the other side of the spectrum: a Whumpee who finally managed to escape and take revenge on their abuser, they slowly but surely make Whumper ruin themself through their newly developed little habit...
To sum up:
Downers (decrease bodily functions and calm you down)
→ Unconsciousness, weakness, distortion of perception, failure of motor functions, coma
-> Common examples: Xanax, ketamine, propofol
Vs.
Uppers (stimulate bodily functions and mood)
-> reduced inhibitions, more prone to hallucinations, psychosis, seizures, serotonin syndrome (high heart rate, sweating, twitching, mania)
-> Common examples: meth, ecstasy, cocaine
Bonus: How to store your Whumpee!
The immediate consequence of drugging someone is to figure out how to keep them. Get them secluded and ready for whumping:
-> In the backseat, foot space or trunk of a car (use an ambulance, it's inconspicuous)
-> You know these roof boxes people strap on top of their car? Stuff ´em in there!
-> Put them in a box and ship them overseas
-> Basements are classics, but try the attic for a change
-> Just use a coffin, combined with an old hearse nobody is going to notice
・・・・・・・・・・・・・・・・・・・
Thanks for reading 🤍 [Masterpost]
#tldr: you will feel pretty shitty afterwards :(#this is organized weirdly sorry for that#please add anything you're missing!#whump#whumpblr#creative writing#whump community#whump drabble#Morris would like this crash course#writing advice#non con drugging#drug abuse#overview#side effects#aftermath#tw addiction#tw death#medical whump#tw overdose#spiking food#anaesthetics#anaesthesiology#sedation#syringe#needles#tw drugs#masterlist#kidnapping#allergic reaction#shock
110 notes
·
View notes
Text
Me: oh I don’t know if I should write a multi chapter fic with Paddy getting rabies. It doesn’t make sense and I don’t know if people would enjoy it.
Google: They cannot tolerate water, not even the sound of it. Then, the patient develops Laryngospasm. We cannot term it as dog bark. Patients make howling sounds due to spasms in throat, which seem like a dog bark,”
Me: this is a sign from god
20 notes
·
View notes
Text
Anaesthetist's Guide to Hospital Superstitions
an expansion of this post.
these are superstitions that i have come across personally! some are common, some not so much but i've seen enough people do it to include it.
don't say the "q" word. it is widely believed that saying it's quiet invites trouble. this goes for "slow", "easy", etc as well. staff will react to this.
we have lucky charms. some people have a lucky scrub cap or pen or shoes, i have lucky compression socks. this is pretty common.
never say anything positive about how a patient handled a procedure until you're away from them. one of my consultants taught me this one, it's just asking for trouble. i don't know how common this is but it's common where i work. i once said, "wow, this patient is amazing, very calm for their first surgery," and then i couldn't extubate for 45 minutes because he wasn't breathing on his own or following commands.
never mention a loved one by name on shift. routinely, i hear people saying, "my partner," or, "my kid," but never their name unless we're off the clock.
when pronouncing a patient, speak as though you are addressing them. i've seen it a few times where people will speak as though they're informing the patient that they have passed.
keeping the emergency or backup equipment nearby wards off bad outcomes. honestly, it's kinda just good practice. i always have a guedel and bougie ready for every intubation as part of this, i probably won't need it but you always need it when it's not prepared in advance.
don't bring patient's out of anaesthesia saying "are you in pain?" this is a complicated concept, there are studies on this and how drawing attention to it can increase pain awareness. instead, i like to say, "are you comfortable?" it's good practice.
the full moon brings chaos, sometimes called the "transylvania effect".
not going straight home after a shift where a patient passed. i tend to go and stop somewhere else then go home. it's so you're not followed home by the spirit, basically. i also do it to just decompress before going home.
never mention a former patient's name, even initials. again, it's good practice not to randomly bring up former patient's by name for confidentiality reasons but it's widely believed that this sort of "summons" them back.
bad luck comes in threes. sometimes people believe death comes in threes, sometimes it's a particular diagnosis or event. it tends to be "oh, i had two of (event), there's another one coming".
the black cloud. sometimes, a "black cloud" will jump from staff member to staff member inviting chaos to their shifts or difficulty for a while. there was a "black cloud" a while back in my workplace where each staff member would fail to cannulate first try for a week before it moved to someone else.
we never say "oh, it's just (procedure)". it invites trouble. e.g. "it's just an LMA case," then that patient goes into laryngospasm or you can't secure an airway. i also think it's good practice not to encourage complacency with "simple" procedures.
working with a specific coworker means you are in for a chaotic shift. similar to the "black cloud" but a bit more specific. these coworkers might be amazing at their job and have good shifts with everyone else but, for some reason, when you work with them everything seems to go wrong. i have a coworker that i adore but we refuse to work together because a black cloud seems to follow us when we're teamed up.
don't plan your free time during your shift. you'll get called back in or extend your shift.
stand your pager up or lay your phone face-up when you're on-call. it's a weird one but leaving a pager flat or phone face-down "tells the pager/phone" that you're resting and invites chaos. some people also face their pager or phone away from them when they're making coffee or having lunch.
some staff members are "shit magnets". no matter how good they are at their job, trouble seems to follow them.
eat/drink something and/or go to the bathroom before every case. if you don't, it'll go longer than expected.
don't listen to music with themes of death or suffering on your way to work. another one bites the dust came on the radio before my shift once and never again. this one, in part, i think it's also so you're not going into work with that in the back of your mind.
if a patient says, "i'm going to die," believe them.
some places will not have a room 13. i once saw a theatre department that went 12, 12a then 14.
don't look back at the theatres or the board while going on break or to the bathroom.
below the cut i'm just going to be a nerd so if you want to see that, go for it.
a lot of superstitions circle back to patient outcomes and care, i believe they call it "magical thinking" where somehow a factor is effected by an unrelated element, e.g. knocking on wood.
i also think the idea of "jinxing" is fairly common, not just in medicine.
there was an article in 2020 that reviewed 295 studies of specific superstitions and then organised them by specialty and subject while also assessing a specific superstition (patient age = chance of admittance), the evidence for this was compiled from 250,000 charts. the superstition was ultimately not supported by the data.
out of the 295 studies, psychiatry was identified as having the most articles at 74, OB/GYN was second with 44, and anaesthesia was 7th with 14. it also looked at the common themes, some of these were more diagnostic or relating to anatomy so i haven't included them as they're not relevant to the concept of superstitions in my opinion.
it did list a common anaesthesia "superstition" that people with red hair have an increased anaesthetic requirement, there are actually quite a few articles on this with varied results and a lot of them are outdated now so the research isn't conclusive but experience is a form of evidence.
there are actually some really interesting medical journals on the topic of superstitions where, as mentioned above, they measure the validity of certain superstitions and there is a peer-reviewed article from 2019 specifically on using the "q" word. it was a "randomised controlled non-inferiority trial" where we're basically testing whether the new treatment, or in this case simply saying "quiet", is worse than the alternative, refraining from saying "quiet".
this is that article if anyone is interested:
Brookfield, C. R., Phillips, P. P. J., & Shorten, R. J. (2019). Q fever—the superstition of avoiding the word “quiet” as a coping mechanism: randomised controlled non-inferiority trial. BMJ (Online), 367, l6446–l6446. https://doi.org/10.1136/bmj.l6446
and here's another peer-reviewed article on the same topic if anyone wants something a bit beefier. this was an assessment of literature, including the one above:
Umar, T. P., & Jain, N. (2022). Debunking the myth of using “quiet” in clinical departments: an integrative overview of available literature. Annals of Medicine and Surgery, 82, 104792–104792. https://doi.org/10.1016/j.amsu.2022.104792
i don't know if anyone will find this stuff interesting but i do.
#anaesthetist#anaesthesia#healthcare#writing tips#writing help#writing advice#ao3 fanfic#fanfic help#medical#surgery#superstition#superstitious beliefs#medicine
6 notes
·
View notes
Text
Autopsy report on subject ******
Name: Amy Olivia *Classified*
Age: 19
Sex: Female
Ethnicity: Caucasian
Hair colour: Black
Eye colour: Teal/Blue
Height: 5"4
Weight: 125.10lbs
Build: Slim
Physical description: Miss *Classified* arrived in a black bodybag at the mortuary wearing Black platform 'New Rock' brand platforms. White woolen knee height leg warmers pushed down towards the middle section of the calves. Standard undergarments and brassiere. A pair of semi-opaque black tights (slight holes were observed to be cut into some areas of the thigh and calves by an unknown tool or object). A black leather spiked choker fastened around her neck with a buckle. A black and white pleated mid-thigh length Scots skirt. A tightly fitting black tank top with a picture of a skeletal hand performing a rude gesture with the text above it reading 'F**k off'. On top of the shirt she wore a thick black hoodie with electric blue stars decorating each of the shoulders. A stain was spotted on the front of the hoodie just above the left breast (Later identified as Monster Energy drink). A black substance was observed presant on both upper eyelids and a black coating adorned the lashes(later identified as eyeshadow and mascara). On her head were a pair of Letscom rose gold Bluetooth headphones.
Upon inspection, the body of Amy *Classified* showed no sign of struggle or homicide, ruling out the possibility of a physical attack and/or assault which lead to death. Slight redness to the chest and clavicle implies a period of prolonged coughing. Autopsy reports shows no sign of damage or malfunction to Amy's brain or spinal cord. Amy's internal organs were in standard condition for a woman of her age and weight, although her lungs showed signs of nicotine and smoke damage (implications towards her being a heavy smoker are high).
He windpipe was swollen and narrow with evidence of a sugary liquid substance entering through the mouth and entering the lungs (most likely from either drinking too quickly or taking large gulps possibly resulting in the liquid traveling into the wrong tract). Amy's larynx and vocal folds had closed up, implying a laryngospasm had taken place moments before death.
From this we can conclude that Amy *Classified*'s death was an accident and no other persons were at fault. It is my professional opinion that Miss Amy Olivia *Classified* died of Dry Drowning, a phenomenon that can occur outside of being submerged in water of any kind, exacerbated by the affects of a laryngospasm. Following the request filled by the mother of the late Amy Olivia *Classified*, her body shall be cremated and returned in an urn to Miss Ruth *Classified*.
3 notes
·
View notes
Text
Envy
Envy is defined as a feeling of discount or resentful longing aroused by someone else’s possessions, qualities or luck. Aristotle defined Envy as pain at the sight of another’s good fortune. The Bible states Envy is a sin. As one evangelical dictionary puts it, envy is the “sin of jealousy over the blessings and achievements of others. The words Envy and Jealousy are interchangeable.
So it seems pretty straight forward that Envy is a bad thing, hard to see Envy as anything but a bad thing. So I hope that you won’t think less of me when I share with you that I am a very envious person these days. I envy so much, I spend so much of my day feeling envious of so many of those around me. Don’t get me wrong, I don’t want for those around me to be pulled down to my level of struggle, I just wish that I was still able to live at my former level of living, the level that most around me still live at.
So what do I envy….where do I start…….
I envy those who get to sleep in their own bed, with the love of their life. I sleep in a borrowed hospital bed where I can grab onto the bed rail to help me roll over, since I can’t do that anymore on my own. I look over at my wife sleeping quietly in the next bed missing the comfort received from reaching out and feeling her beside me in the depths of the night. When a caress, embrace or soft kiss was all that was needed to chase away the demons and ease us back into a restful slumber.
I have led a good life and had some adventures along the way, there were times when what I was doing in my career was quite dangerous. You know what the most dangerous thing I do now is? The most dangerous thing that I do everyday is I go to the bathroom, struggling to get in and out, legs quivering under the strain and exhaustion of standing, praying that I won’t fall and require rescue, or even worse break something. I worry about the day when my legs stop working totally, and I know that is only days or weeks away. I envy people who can easily and discretely take care of their bathroom needs.
I envy those who have the ability to be independent, I was once independent but now I’m totally dependant on others for my survival. It is one thing to accept another’s help, it is another thing to require someones help for almost everything. It is a hard lesson to learn, how to accept the constant help of others, not sure that there is anything more humbling.
I envy those who are able to dress themselves. My wife picks out my clothes, although she does accept my input. I wait for her to have a break in her busy morning so she has the time to help me get dressed. Something that used to be done so easily and quickly is now a major ordeal.
I envy those who can quickly jump in the shower, wash, dry off and get dressed. I feel like I have run a marathon by the time I just make it to the bathroom, then I need my wife to lift my legs into the tub as I sit on the shower bench. I then do my best to shower myself while sitting. I miss standing there under the shower head letting the hot water run over my body, it just felt so good. Now I shut the water off, dry myself as best I can before Robin helps me get my legs out of the tub and helps me to my feet again. I stand there on my unreliable legs while Robin drys the rest of me and I struggle out into the other room where Robin helps me get dressed, by which time I’m physically spent.
Your odds of getting ALS in Canada is .25%, or one out of every 400. About 4% of people with ALS have something called Laryngospasms, basically where your vocal chords spasm and close off your windpipe so you can’t breath. Yes I have hit the long odds twice, and I envy those who don’t know the panic off suddenly having their windpipe close off while you wonder if this is your time to die.
Connected to the Laryngospasms, is the weakened throat and mouth muscles I now live in constant fear whenever I eat or drink that I will choke. We were out to a restaurant with another couple recently and I spent the entire time extremely stressed that I would choke and make a big scene, embarrassing me and everyone with me. I ate slowly with small bites and was still eating when everyone else's plates were empty and had been taken away. I envy those who can eat and drink without giving a thought to the risk of choking.
I envy those who can go out, get in and out of a vehicle easily, can climb those stairs into that really nice restaurant, just walk through that door without struggling to hold the door open and maneuver a wheel chair through the opening. I envy those who can go out and just use the washroom, that don’t live in fear that maybe they drank too much and won’t make it home before needing a washroom. Very soon my wife and I will not be able to go out in the van anymore because I won’t be able to transfer between the wheelchair and the van. I will be trapped in my Condo, only able to go where my wheelchair will take me.
I envy my friends who are living their best life, travelling or living their dream, friends that have a world full of possibilities in front of them. I envy people who don’t have a major struggle to make it through every single day.
I envy people who can communicate easily. You see my arms and hands are becoming non-compliant to the directions my brain is sending them. Most of my writing on my laptop is now done with either one or two fingers. Everything takes longer, and I don’t know that I will ever get the writing done that I wanted to get done before I die.
I envy people who can talk clearly. You see for years I spoke very well, I had great diction, spoke clearly and intelligently during many Press Conferences. I also felt I had a great voice, I used to joke that when I turned it on that I had that Late Night Radio Talk Show Host Voice. Now I mumble because of the muscle degeneration, I dislike the sound of my voice, I don’t like talking on the phone now because I am hard to understand. Now at Social Events I am more inclined to just sit quietly hoping no one tries to converse with me. It’s not worth having to repeat myself two or three times and even then still not be understood. No one wants to be a spectacle, yet that is what I have become.
Now that I have confessed my sin of Envy I hope you will forgive me this continuing transgression. Despite all these challenges I continue to consider myself a very fortunate person, Robin and I will continue to do our best until….well until we can’t anymore. I don’t want your pity, or you feeling sad for me but what I do want is for you to realize just how fortunate you are. Perhaps my situation can help make your more mindful, to be aware and grateful for all the little things that you do without giving them a second thought. Savour every minute because one day the sand in your hourglass will run out, perhaps when you’re not looking, or perhaps when you are upset over some trivial matter, or perhaps when you least expect it. Strive instead to be in a happy, content and mindful state when your time runs out, after all isn’t that how all great journeys should end?
9 notes
·
View notes
Text
Thanks to dysautonomia I choke on my own spit a lot and always have, and likewise have always been kinda shit at breathing. but I had my first full blown laryngospasm today and actually honest to God thought I was about to die. I started to pass out bc I couldn't breathe. And now everything hurts! My throat, my head, my neck and shoulders, my chest, my legs??? Everything seized up bc I was panicking! Now I'm scared of *checks notes* fucking breathing! so that's cool
#me#pots#medical stuff#disability stuff#wild how pots can literally just make you flatline and/or stop breathing.#and thats just. a Thing That Happens sometimes.
3 notes
·
View notes
Text
Donna Heim, 20 (USA 1986)

California resident Donna Heim was 20 years old. She was perfectly healthy other than a history of asthma. In 1986, she found out that she was pregnant and ended up going to Her Medical Clinic (which was actually an abortion facility) when she was in the second trimester.
On August 11, 1986, an unspecified HMC employee inserted laminaria dilators and told Donna to come back the next day. Donna was not warned about the risks of abortion and had no idea that she was going to die.
The next day, Donna underwent the abortion at the hands of abortionist Mahlon Douglas Cannon. HMC had not bothered to check Donna’s medical history other than a brief record of the past two weeks. It was already documented that Donna had asthma, but HMC didn’t bother to make sure that Donna was receiving any oxygen or that the drugs administered were safe for her. Donna was also not given a pre-op exam.
During the abortion, Donna suffered bronchospasms and/or laryngospasms. A nurse anesthetist started trying to get Donna to breathe normally, but did not check her medical records or administer any treatment that could have actually helped. Cannon was aware of the situation, but he didn’t help try to save Donna or call 911. Instead he just continued the abortion.
4 or 5 minutes later, Cannon actually tried to do something about his dying client— in a completely incompetent way. Instead of giving any medicine that might have had a chance at saving her, he attempted the Heimlich maneuver. It is unclear why he thought this would do anything. When Donna still couldn’t breathe, Cannon laid her down flat and put his fingers in her mouth. It didn’t help.
By the time someone finally called an ambulance, it was too late. Paramedics arrived to find Donna in full cardio-respiratory arrest. They desperately tried to save her, but she was declared dead shortly after.
The next month, another young client named Liliana Cortez who was perfectly healthy other than having asthma was killed by HMC in strikingly similar circumstances.
(Medical Board Documents)
#pro life#tw ab*rtion#tw abortion#abortion#tw murder#pro choice#abortion debate#unsafe yet legal#tw death#death from legal abortion
23 notes
·
View notes
Text
Dissociative dose of ketamine is 1 mg/kg. That's the dose used for conscious sedation. Ketamine can cause laryngospasm.
6 notes
·
View notes