#Mellitus Diabetes.
Text
Know more about Diabetes Nursing at the 13NHPSUCG.

#diabetic distress#concerning diabetes nursing .#Diabetes mellitus (DM) is a metabolic condition marked by unnecessarily high blood glucose levels. Type 1#type 2#maturity-onset diabetes of the young (MODY)#gestational diabetes#neonatal diabetes#and secondary causes resulting from endocrinopathies#steroid use#etc. are some of the different kinds of DM.#Mellitus Diabetes.#Melvin#a 32-year-old#frequently laments his growing thirst. Moreover#he frequently feels the need to urinate and is constantly hungry. His extremities are tingling and are numb. His formerly crystal-clear vis#he already feels exhausted a few hours after getting up. He has a wound on his right knee that has been there for weeks without healing.#Meet Inspiring Speakers and Experts at our CME/CPD accredited 13th World Nursing#Healthcare Management#and Patient Safety Conference#which will take place November 15-18#2023 in Los Angeles#USA. If you are interested to be a part of this Webinar as a speaker then submit your abstract now. Submit here: https://nursing.universeco#visit here#to know more: https://nursing.universeconferences.com/#Description#The gastrointestinal tract's digestion of ingested food and the liver's production of glucose from dietary components are the two main sour#•#Increased blood glucose levels can cause a range of metabolic illnesses known as diabetes mellitus.#Most frequently#diabetes mellitus causes problems with insulin secretion
0 notes
Note
Even with comparatively minor disabilities flying sucks. I have type 1 diabetes and for years my parents were terrified tsa wouldnt let my insulin through. My dad would print out the tsa guidelines saying insulin was ok and bring them with us just in case they tried anything
my father has been type 1 since before I was born (so technically I owe my existence to insulin, god fucking bless), so I feel like you are family already. I have a handful of memories of sitting on one side of TSA with my twin as a child, waiting for him as they tested his pump for explosive residue or whatever and him telling us to board the plane without him (again — as a child!) if he didn’t make it thru before boarding ended
the harassment diabetics have to endure from TSA/security/etc is so frustrating and angering. we should really be teaching people about common medical devices in school. pumps should be so so normal
#anonymous#diabetes#type 1 diabetes#he had adult onset diabetes mellitus. he actually almost died so literally thank insulin for my existence hahahaha
42 notes
·
View notes
Text
Btw i finally found a good diabetic friendly snack! Hippeas nacho and ranch chips. The nachos are like 1% better than the ranch, as in the nacho was closest to nacho doritos while ranch is just like a smidge behind but still really good. good strong flavors, doesnt taste "healthy"


i was worried they would have a strong chickpea flavor but they dont! not much in the bag, and the price might not be worth for some,
but if youre diabetic and plant based or vegan then these are great as a snack if youve got some heavy cravings
8 notes
·
View notes
Text
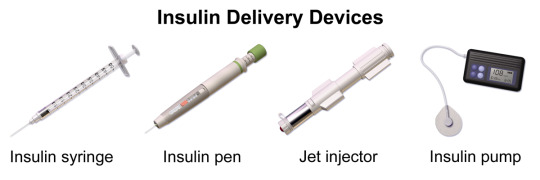
Insulin (medication)
#insulin#insulin delivery devices#wikipedia#wikipedia pictures#medicine#medcore#medicalcore#medicore#medical#tech#technology#techcore#technologycore#medical devices#diabetes mellitus#type 1 diabetes#type 2 diabetes#diabetes#insulin pump#insulin pen#insulin injection#syringe#jet injector
85 notes
·
View notes
Note
Okay! Now it's your turn! Tell me about your DNP project (or any of your dream projects) that you could share at a conference
Loadedddd question, haha!
I technically don't have to land on a project until this coming Spring term (April 2025), but I have been thinking about it. Since my DNP is associated with also becoming an NP, our instructors would like us to focus on how to implement things on the provider side of things versus nursing (though I think that is a bit unfair, considering the majority of my knowledge is nursing, and I'm also here to improve patient lives and outcomes, not just the provider process... but ya know).
So far my ideas include the process of implementing and managing blood glucose in stem cell transplant patients who have acute/chronic graft versus host disease, are in the inpatient setting, and are on high-dose steroids. Steroid-induced DM, or just exacerbate someone's DM! Right now, it is pretty well known that we are okay with blood glucose levels below 180 (typically between 140-180 is tolerated), but steroids make life a lot more tricky, especially when these patients can be on these steroids for *months*. I'm hoping I get to do a rotation on the transplant unit to find out their process (since I don't currently work there). This one is directly tied to how providers order and institute blood glucose management (insulin, sliding scales, etc), and I believe we can always do better when it comes to managing blood glucose.
My second idea (that likely has NO literature on it whatsoever, so it is unlikely to be a process I get to change any time soon, plus it is directly tied to nursing medication administration and not the provider side of medicine) is how we administer Daratumumab (a monoclonal antibody for multiple myeloma). It is frequently given as a subcutaneous injection these days (IV formulation still available), and it is 15 mLs over 5 minutes into the stomach once a week for about 8 weeks, then every two weeks for another 8 weeks, and then once a month until progression of disease. In this case, as someone who has given this drug hundreds of times at two different institutions, I wanted to see if I could implement a new quality improvement on how the drug is administered (a straight needle versus a butterfly needle).
Anecdotally, I have heard from nurses and patients that the butterfly needle is typically preferred. Some patients reported decreased discomfort with the butterfly needle, both during administration and hours after, and others didn't even notice. If you push the med too fast (15 mLs is a lot at once!), there can be discomfort. As for the nurses, we have better control over the syringe and have better ergonomics with a butterfly needle. When using a straight needle, you are holding the needle and syringe up against the skin and are leaning over the patient, which can be uncomfortable for the back and shoulders. You have the ability to sit back more and have more steady control over pushing the syringe when utilizing the butterfly needle. (We typically taped the butterfly needle down, which I think also decreases unnecessary needle movement). At least from what I have seen, there is no standard across the board for administration (just subcutaneous into the abdominal area).
I would love to compile some data on patient and nursing feedback on both administration techniques to get the ball rolling (but it sounds more research-based than quality improvement, and I guess I kind of disagree, but my instructors would argue with me... especially after this summer term. However, it is nursing-focused, not provider-focused, and there is unlikely to be any literature (multiple myeloma is a very small subset of blood cancer, and I pigeon-holed myself on data during my first research course in this program. I ran with it, but it was slim evidence to work with, and it was just around multiple myeloma and stem cell transplantation. I doubt anyone has even considered nursing preference in administration technique for one specific immunotherapy drug *laughs*). I'll get to this one day! Unfortunately, while I talked about it a lot with my fellow nurses in both Denver and here in Portland, I never had a way to implement a change or gather data (though before I left Denver, we changed from the straight technique to the butterfly needle. No idea what data was behind it, but the pharmacy drew up the drug and provided it with the butterfly needle. Daratumumab isn't hazardous, so my Portland job just gave us the bottle, lol)
I am also interested in palliative care (though that might be a project too big to chew for the size we have to limit ourselves to. My mentor Patti literally did her project on the barriers to mass transfusion protocol documentation. All she did was obtain qualitative data from the trauma ICU nurses voluntarily). Our mock project for our quality improvement course this summer was on palliative care in heart failure, and I know my classmate wants to take that and run with it. I also am far more interested in palliative care in oncology. But I couldn't say what I would want to do for a project other than something in palliative care and oncology.
Our instructors (and the class ahead of us, haha) would also love it if we took a previous project and continued it, but none of the current third years have a project I want to continue (no oncology!). I don't want to do a project I am not invested in or interested in.
I may come up with other ideas once we get further into our management courses and start clinicals in February (kajsdlkfjklajsdfl), but I am pretty passionate about DM treatment/management, stem cell transplants, oncology, and palliative care.
(I almost signed up for the elective about submitting abstracts and posters, but I chickened out and went with Institutional Racism. As I said, I have lowered my expectations, lmao. It has been a weird year. I have met some very impressive nursing greats - I effing met the creator of the Tanner's Model of Clinical Judgement. Mind. Blown!)
#pluto#dnp school#nursing#dnp project#dnp project ideas#multiple myeloma#oncology#palliative care#diabetes mellitus#about me#DNP student#insanity
3 notes
·
View notes
Text

#frusemide#hydrochlorothiazide#bronchial#asthma#hyper#coagulopathy#diabetes#mellitus#congestive#heart#science#solutions
3 notes
·
View notes
Text
As someone who has had diabetes for “only” around three years I really don’t understand how dangerous it can be. I have read people’s stories on how they deal with low bloodsugars and their stories about their trips to hospitals, but I am still yet to find people with type 1, who don’t understand the hassle. I know it’s serious, but I don’t know how serious it should be taken as.
See, most often when my bloodsugar goes low, I sort of like it. It makes me feel really light and blissful. I haven’t really told anyone this as everyone says that low bloodsugars are really dangerous. I have never passed out, and for that I am thankful, but maybe I need that scare for me to take this illness seriously. No one has never needed to keep me conscious or feed me when I’ve had hypos, and everyone turns super serious whenever I tell them what to do if, I pass out, and that is something I don’t understand.
I hope that someone else can somehow relate to whatever I’m trying to say here.
Also stay safe and take care of yourselves!
#type one diabetes#type 1 diabetes#diabetes#diabetes mellitus#hypoglycemia#type one diabetic#juvenile diabetes
34 notes
·
View notes
Text
My condition right now 😢

#chronic illness#chronic pancreatitis#health blog#pancreas#pancreas support supplement#pancreatitis#diabetes mellitus#diabetes care#insulin#diabetic#diabetes management#enzymes#creon
3 notes
·
View notes
Text
TYPE 1 DIABETIC PRIDE FLAG


Flags: Type 1 Diabetic with diabetes circle symbol | Ditto without symbols
T1D: Type 1 diabetes is a serious condition where your blood glucose (sugar) level is too high because your body can’t make a hormone called insulin. This happens because your body attacks the cells in your pancreas that make the insulin, meaning you can’t produce any at all.
#VIVOPOSTING#mad pride#mad flag#mad pride flag#diabetes#diabetic#type 1#type 1 diabetes#diabetes mellitus#diabetes flag#diabetic flag
22 notes
·
View notes
Text

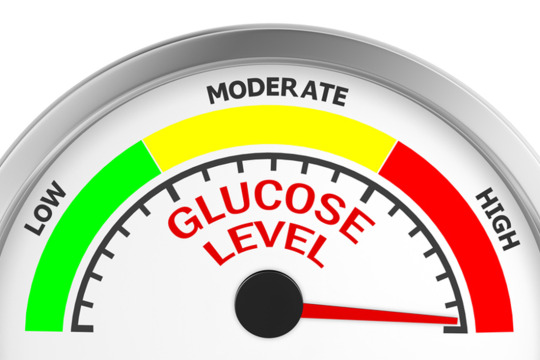
VITAMINS THAT CAN LOWER BLOOD SUGAR QUICKLY
Balancing blood sugar levels is crucial for maintaining overall health, especially for individuals with diabetes or those at risk of developing the condition. While diet, exercise, and medication play primary roles in managing blood sugar, certain vitamins and supplements can also significantly impact glucose control. This article explores vitamins known for their potential to lower blood sugar levels quickly and efficiently.
Vitamin D
Vitamin D plays a pivotal role in blood sugar regulation by enhancing the body's sensitivity to insulin, the hormone responsible for managing blood glucose levels. Insulin resistance is a common issue in individuals with type 2 diabetes, where the body fails to use insulin effectively, leading to elevated blood sugar levels. Studies suggest that maintaining adequate levels of vitamin D can improve insulin sensitivity and lower blood sugar, thus aiding in diabetes management.
Sources of Vitamin D:
Sunlight exposure
Fatty fish (salmon, mackerel, and sardines)
Fortified foods (milk, orange juice, and cereals)
Vitamin D supplements
Vitamin B1 (Thiamine)
Thiamine is essential for glucose metabolism, helping convert carbohydrates into energy. People with diabetes often have low levels of thiamine, which can contribute to higher blood sugar levels and complications. Thiamine supplements, particularly in the form of benfotiamine (a lipid-soluble derivative of thiamine), have been shown to improve glucose metabolism and reduce the risk of developing diabetes-related complications.
Sources of Vitamin B1:
Whole grains
Pork
Nuts and seeds
Legumes
Thiamine supplements, including benfotiamine
Vitamin B3 (Niacin)
Niacin, or vitamin B3, influences blood sugar control indirectly through its role in converting food into energy. However, high doses of niacin can increase blood sugar levels, making it necessary for individuals with diabetes or those at risk to consult a healthcare provider before taking niacin supplements.
Sources of Vitamin B3:
Turkey
Chicken breast
Peanuts
Mushrooms
Supplements, with medical guidance
Vitamin C
Vitamin C, an antioxidant, can lower blood sugar levels and help manage diabetes by improving glucose metabolism and protecting cells from damage caused by excess sugar in the blood. Research indicates that vitamin C supplementation can help reduce fasting blood sugar levels and improve blood sugar control in people with type 2 diabetes.
Sources of Vitamin C:
Citrus fruits (oranges, lemons, and grapefruits)
Kiwi
Strawberries
Bell peppers
Supplements
Magnesium
Though not a vitamin, magnesium is a crucial mineral that aids in blood sugar control. It plays a significant role in glucose metabolism and insulin action. Low levels of magnesium are linked to insulin resistance, a condition often preceding type 2 diabetes. Increasing magnesium intake through diet or supplements can improve insulin sensitivity and lower blood sugar levels.
Sources of Magnesium:
Spinach
Pumpkin seeds
Almonds
Avocado
Supplements
Chromium
Another essential mineral for blood sugar regulation is chromium. It enhances the action of insulin and is involved in carbohydrate, fat, and protein metabolism. Some studies suggest that chromium supplementation can have a beneficial effect on blood sugar levels, especially for those with diabetes.
Sources of Chromium:
Broccoli
Whole grains
Green beans
Nuts
Supplements
Conclusion
While vitamins and minerals can support blood sugar management, they should complement, not replace, standard treatments such as medication, a balanced diet, and regular physical activity. Always consult a healthcare provider before starting any new supplement, especially if you have diabetes or other health conditions, to ensure it's safe and appropriate for your specific health needs. By integrating these vitamins and minerals into a holistic approach to health, individuals can achieve better blood sugar control and improve their overall well-being.
#usascriphelpersofficial#diabetes care#diabetes treatment#diabetes mellitus#diabetes management#diabetes symptoms#insulin#diabetic#doctors#type 1 diabetic#type 2 diabetes
4 notes
·
View notes
Text
can someone explain why a meal that usually is low glycemic for me and gives off low readings, suddenly gives of a really high blood sugar readings?
its usually like 160 on average but now its 235??
i didnt eat much today, this was my main meal, and so is that a thing? if you dont eat much at all, and then eat a proper meal can that make your blood sugar spike?
ive been sitting for a while, and then got up and took my blood sugar, is that something?
kind of worried bc i was doing so well with keeping my blood sugar under 200, and on average at 160, but then why is it SO high?
edit: just got test results in from today

is this anything?
3 notes
·
View notes
Text

Insulin (medication)
#insulin#insulin injection#insulin pen#wikipedia#wikipedia pictures#medicine#medical#meds#med#medcore#medicalcore#medicore#tech#technology#pharmacore#diabetes#diabetes mellitus#type 1 diabetes#type 2 diabetes#gestational diabetes#medical care#injection#needles
23 notes
·
View notes
Text
Diabetes Mellitus Type 1
-- the pancreas secretes insulin
-- insulin is released from beta cells
-- these beta cells are also called islets of Langerhans
-- insulin secretion increases in response to elevated blood glucose levels
-- in diabetes mellitus type 1, beta cells are destroyed
-- an autoimmune response destroys the beta cells
-- secondary diabetes mellitus type 1 results in beta cells damaged by cancer or other diseases of the pancreas
#medblr#studyblr#notes#my notes#medical notes#med notes#medblr notes#anatomy and physiology#anatomy#physiology#anatomy notes#physiology notes#diabetes mellitus#diabetes
3 notes
·
View notes
Text
youtube
𝗖𝗢𝗠𝗢 𝗚𝗔𝗡𝗔𝗥𝗟𝗘 𝗔 𝗟𝗔 𝗗𝗜𝗔𝗕𝗘𝗧𝗘𝗦, te lo contamos en 𝙈𝙀𝙉𝙊𝙎 𝘿𝙀 𝟮 𝙈𝙄𝙉𝙐𝙏𝙊𝙎
#como ganarle a la diabetes#salud en armonia#diabetes#diabetes tipo 2#diabetes tipo 1#como curar la diabetes#diabetes mellitus#como evitar la diabetes#como controlar la diabetes#resistencia a la insulina#control de la diabetes#como solucionar la diabetes#como curar la diabetes tipo 2#Ejercicio para diabéticos#REVIERTE LA DIABETES TIPO 2 EN 5 PASOS#CODIGO DE LA DIABETES PARTE 2#CODIGO DE LA DIABETES PARTE 1#por que adelgaza un diabetico#como controlar mi azucar#Youtube
2 notes
·
View notes
Text
6 Long Term Complications of Diabetes Mellitus
Living with Diabetes Mellitus comes with many complications which can occur even if your diabetes is well controlled. Back then diabetes was known as an endocrine disorder but these days it is widely accepted that diabetes is a vascular-metabolic disorder. This is because most of the damage done by diabetes is primarily on the small blood vessels of many organs.
Complications of Diabetes are…
View On WordPress
2 notes
·
View notes
Text
Ever woke up unable to move, very nauseous, shaky, and just all in all feeling like shit but unable to check your blood sugar because you are out of test strips and monitors and your sensor failed?
Yeah. That's what happened to me this morning
#my grandma lent me hers.#i was 64#💫🌌. lilith talks#it wasnt fun#type 1 diabetes#actually diabetic#diabetes mellitus type 1#5 year diabetic#(almost 6 that tag is gonna change soon!)
2 notes
·
View notes