#evidence based medicine
Text






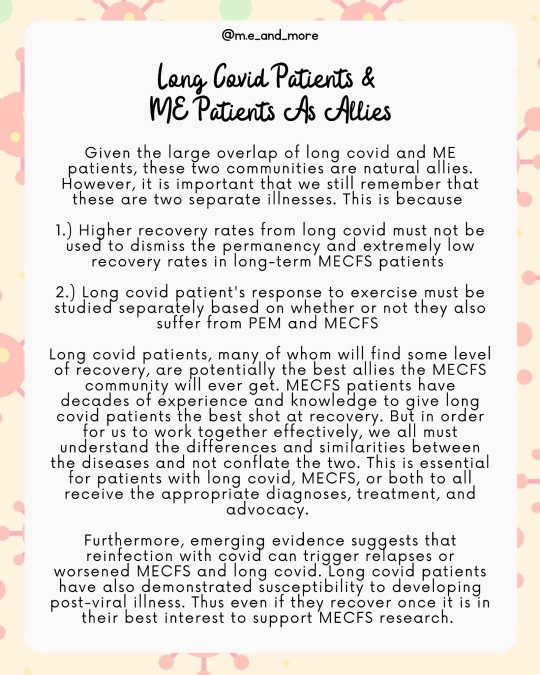
Not all #LongCovid is #myalgicEncephalomyelitis.
While its super important to raise awareness of the simularities of the #millionsMissing with #MECFS and #millionsMore with #LongC it is also essential to recognize that only a subset of #covid #longhaulers meet the criteria for a diagnosis of ME.
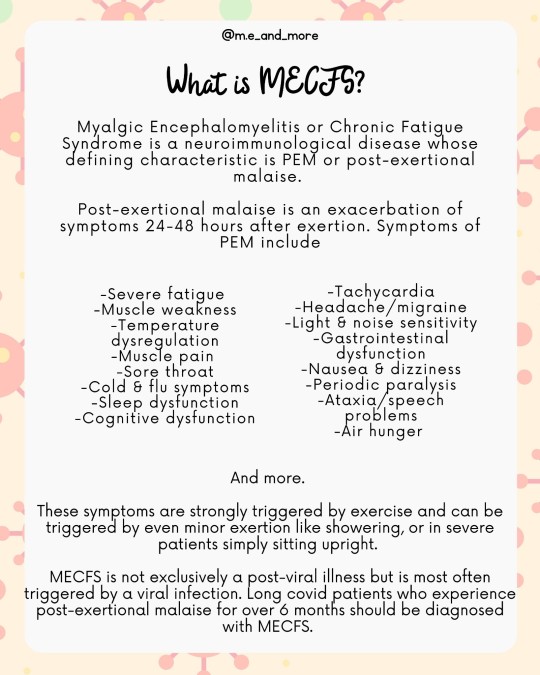
ME aka #ChronicFatigueSydnrome is not the same as #chronicFatigue. The defining symptom of ME / #CFS is #PostExertionalMalaise or an exhasurabtion of metabolic, neurological and immune dysfunction symptoms 24-48 hours after exertion.
When you are talking about long covid patients who experience #PEM you should talk about MECFS because that is what these patients have.
When you are talking about long covid patients be clear that only the subset with PEM have MECFS.
It is important for patients with long covid to receive the correct diagnoses, because while there are no FDA approved treatments for ME, many commorbidities do have effective medication options. Management of ME must also be tailored based on a patients commorbidities.
Patients with MECFS and post viral fatigue syndrome must not be prescribed GET or CBT. This includes all long covid patients with PEM.
Long covid patients who experience PEM should be advised to #StopRestPace and informed about the importance of pacing agressively not just to prevent symptoms from fatigue but to prevent PEM in the following days. This is regardless of whether they have PVFS (less than 6 months post covid) or MECFS (more than 6 months)
Because long covid is a broad category that encompasses patients MECFS #MCAS #fibromyalgia #POTS #dysautonomia #autoimmune and #autoinflammatory diseases in many combinations the prognosis for long covid patients is much more variable than that of ME patients and recovery is more likely in early stages of ME, long covid patients who recover should not generalize their experience onto MECFS patients more broadly and should continue to support MECFS research.
MECFS patients have decades of experience with pacing, medical gaslighting, chronic illness, housebound and bedbound life and more. We hope that #covidLonghaulers will #LearnFromME and ally with us to end #postViralIlness
#mecfs#long covid#long haul#millions missing#millions more#post viral illness#post viral syndrome#post viral fatigue#chronic fatigue#chronic fatigue syndrome#myalgic encephalomyelitis#education#health#evidence based medicine#covid#chronic illness#chronically ill#pots#mcas#dysautonomia#fibromyalgia
310 notes
·
View notes
Text

Doctor Beverly Crusher
@SpaceDocMom
Your immune system is not a muscle. It does not require exercise. Stressing it doesn't make you healthier. That's not how vaccines work. Vaccines are information, disease is stress. You read books, you don't beat your body with them to "get stronger". emojis: black heart, blue heart, masked
2:16 PM · Dec 3, 2023
#star trek#doctor crusher#star trek the next generation#star trek memes#star trek tng#kindness#support#care#compassion#health care#healthcare#medicine#science#evidence based medicine#there is no such thing as immunity debt#spoons#spoonies
31 notes
·
View notes
Text
Student 1: How do you put UpToDate as a reference?
Student 2: UpToDate.
Student 1: Thank you, I don’t know what I’d ever do without you.
19 notes
·
View notes
Text
By: Sallie Baxendale
Published: Jul 7, 2023
Every medical student should acquaint themselves with the discomfiting history of epilepsy surgery. Regardless of their eventual speciality, they will become better clinicians for it. As a cautionary tale of what happens when we lose sight of primum non nocere as our guiding principle in medicine, the sorry narrative is exemplary, putting well-intentioned doctors on the wrong side of history again and again.
Trepanning (drilling a hole in someone’s skull) has been conducted for millennia, with evidence of the oldest procedure dating back several thousand years. Archaeological finds of skulls with multiple holes in various states of repair indicate that at least some of our ancestors survived these treatments and came back for more. Opening a space to let the demons out of someone’s head makes sense, if you believe the pesky things have taken up residence and are running amok inside. At least this treatment was in the right anatomical ballpark, according to our current understanding of epilepsy as a neurological condition. Less than 130 years ago, surgery for epilepsy had “advanced” (or regressed) to the extent that the head was no longer the sole target of the surgeon’s scalpel.
They had branched out to recommend limb amputation. The rationale was straightforward: if someone’s arm keeps shaking, what more effective cure than to cut it off? Other surgical approaches to epilepsy in the 1890s included clitoridectomy and castration — both attempts to curb the immoral sexual appetites that were “well known” to cause epilepsy at the time. For the squeamish patients who wished to retain their sexual organs, alternative treatments included admonitions to avoid coffee, chocolate and amorous love songs. Late Victorian treatments for epilepsy were nothing if not eclectic.
Into the mid-20th century, people with epilepsy were once again the unwitting participants in a dark era of medical experimentation. In an enterprising spin-off, the radical surgical techniques developed in the Forties’ psychosurgery movement were trialled as treatments for epilepsy. All undergraduate psychology students (and fans of the film Memento) will be aware of Henry Molaison, better known by his initials. In October 1953, Mr Molaison underwent surgical excision of the right and left temporal lobes of his brain. In a short paper delivered six weeks after the surgery, his surgeon reported that the operation had resulted in no real changes, “with the exception of a very grave recent memory loss”; H.M. was unable to remember where his room was in the hospital, or how to find the toilet.
H.M.’s profoundly disabling amnesia persisted for the next 55 years, until his death in 2008. He became the most famous neuropsychological case study in the history of the profession. But he was not the first person to undergo this procedure and suffer this devastating outcome. Scores of others were discovered in a retrospective review, triggered by Mr Molaison’s case. His memory loss could have been anticipated and prevented if the outcome of this procedure had been fully evaluated in his predecessors. More shocking still is that a similar fate was allowed to befall a number of other patients after his amnesia was discovered. Ignorance is one thing, inertia something entirely different.
The lessons from this sobering history are clear. When doctors fundamentally misunderstand the cause of a condition and treat the symptoms instead, and fail to properly monitor outcomes, and modify their practice in response to known adverse outcomes, our patients suffer — often greatly and for the rest of their lives — if indeed they survive. These fundamental errors underpin the depressingly regular scandals that punctuate the history of medicine. (The stakes are particularly high if surgery is involved.)
It is naïve to think that all these scandals are in the past. Our descendants will look back at some aspects of our current medical practice and wonder that we could have been so stupid. They will shudder at how barbaric and crude some of our current treatments are. So where might the next medical scandal be brewing?
The increasing visibility of detransitioners suggests it may lie in wait in gender-affirming medicine. Many detransitioners are young women who underwent treatment for psychological distress that has left them with irreversible, life-long changes to their bodies: a deep voice, a beard, and compromised sexual function. Some have had their breasts surgically removed; some may be infertile. Others are young men who have been castrated.
This is not an argument about the pros and cons of these treatments for trans-identified young people. Nor is it an argument about the percentage of people who may “regret” undergoing these procedures. The existence of just one detransitioner suggests that an individual was not offered the correct treatment for their condition by the doctors charged with their care. It is a clear case where the medical profession caused harm. We are ethically bound to learn, and widely disseminate, the lessons from these cases.
For many detransitioners, the cause of their distress as a teenager was misattributed by their clinicians to the notion that they had been born in the wrong body, and that they would be helped by the surgical creation of the “correct” body. Regardless of the validity of this treatment for some — on which I make no comment — this assumption was incorrect in the case of many detransitioners. Once these fundamental errors of misattribution had been made by the treating clinicians (who in the case of GIDS were primarily psychologists, and not medically qualified), surgeons and endocrinologists embarked on a procedure akin to that of limb amputation for epileptic seizures. The detransitioners’ discomfort with their body was a symptom of psychological distress, not a cause, but their medical team prescribed treatments with an irreversible impact and surgically removed healthy tissue in an effort to cure their symptoms.
In most other fields of surgery, this would be classified as a “never event”, and an exhaustive investigation would be launched. But in the case of many detransitioners, their treating medical team has failed their patient at every stage. They have fundamentally misunderstood the nature of the condition the patient has presented with and have treated the symptom rather than the cause. The astonishing failure of the Tavistock & Portman NHS trust to monitor even primary outcomes were laid bare in the original trial of Bell vs Tavistock, with further shocking details subsequently presented in Hannah Barnes forensic account of the collapse of the service. This failure means there is no opportunity to modify practice in response. It is unsurprising that the results have been catastrophic for some.
However, in the case of detransitioners, there is an additional, darker layer to this cascade of medical errors. The patients themselves are being held responsible, by the very doctors who made them. The term “post-treatment regret” appears to abrogate any responsibility on behalf of the treating clinicians for these outcomes. Some argue that there is some degree of regret associated with every medical procedure. However, there is a fundamental difference between patients who are unhappy with the outcome of elective treatments recommended for their condition, and those who have been misdiagnosed, and have had healthy tissue surgically removed as a result. Many detransitioners were given the wrong treatment for their condition. These people are not experiencing post-treatment regret, they are responding appropriately to the consequences of a grave medical failure.
Advocates of gender-affirming care argue that “no one can know whether post-treatment regret will occur; therefore what matters ethically is whether an individual has a good enough reason for wanting treatment”. This is a remarkable position to take. Surely what matters ethically is that the medical profession offers appropriate, evidence-based treatment to patients who will benefit from them. Others argue that young trans people have “the right to be wrong”. They do indeed; doctors, less so, particularly when they are wielding a scalpel. Just as trans youth deserve access to the very best in evidence-based medicine, so doctors have a fundamental duty not to offer harmful treatments to young people who will not benefit from them. It is not good enough to shrug and say, “no one knows whether this will occur”. We know that poor outcomes do occur, and are duty-bound to find out as much as we can about these in order to predict and prevent them.
Since 2014, there has been a phenomenal increase in young women referred to specialist services for gender dysphoria. There is, therefore, a greater number of people who are at potential risk of receiving inappropriate treatments. To respond by creating a “fast-track” to medical transition is to ignore everything history has to teach us. Meticulous assessment of a young person’s symptoms is not transphobic, nor does it invalidate anyone’s identity. It is good medicine, and ensures that the right treatment is given to the right patient.
No branch of medicine can be exempt from rigour. Exceptionalism lies at the heart of many medical scandals. That way catastrophe lies and, as ever, it will be our patients who suffer. This is not hypothetical: detransitioners stand before us as living, breathing examples of people who have been harmed. To change nothing as the result of their experience — or, even worse, to make changes that mean similar errors could potentially harm even more people — is immoral. Upholding scientific principles is the least we can do to protect our current patients and honour the thousands who have been failed by the medical profession in the past. The history of surgery can teach us that much. It is our responsibility to take note.
==
Here's the thing: it's likely there were people with epilepsy who had holes drilled into their head and swore it was "life-saving." But we're not foolish enough to think that this makes the practice of trepanning ethical, much less evidence-based.
#Sallie Baxendale#detrans#detransition#MTFTM#FTMTF#medical experimentation#sex trait modification#cosmetic surgery#medical scandal#gender epilepsy#medical transition#gender ideology#queer theory#iatrogenic harm#medical malpractice#medical corruption#evidence based medicine#gender affirming care#gender affirming#gender affirming treatment#religion is a mental illness
17 notes
·
View notes
Text
Thanks to @gardening-tea-lesbian for posting about this and bringing it to my attention!
--
The Biden-Harris Administration wants to make substance abuse treatment more accessible for all prisoners in the U.S. Addiction is common among people in prison, and treatment helps fight recidivism and reduce overdose rates.
From Federal Prisons To State Prisons
By this summer, all federal prisons will offer addiction treatment, Dr. Rahul Gupta, director of the White House Office of National Drug Control Policy, said last week.
Federal officials want states to follow suit. Starting this spring, Medicaid funds will be set aside for states to use in their own jails and prisons to provide mental health services, including SUD treatment.
Approximately 25% of all Americans received Medicaid benefits in 2022. For people with low incomes, Medicaid is the largest provider of funds for healthcare services.
The Biden-Harris Administration has shown a commitment to helping underserved communities receive addiction prevention, treatment, and recovery services.
This includes services for rural populations and Tribal populations along with people who are incarcerated.
Addiction In Our Prisons
It’s hard to know precisely how many incarcerated people have an SUD, but the National Institute on Drug Abuse (NIDA) estimates that about 65% of all inmates do.
NIDA estimates that another 20%, who didn’t meet the official criteria for an SUD, were under the influence of drugs or alcohol when they committed a crime.
Overall in America, about 40 million people ages 13 and over are living with addiction, or about 12% of the population, according to the 2020 National Survey on Drug Use and Health.
How Treatment Helps Prison Populations
Drug abuse treatment is effective. For people in prison, receiving treatment can mean the difference between staying out of jail once released or returning behind bars.
It can also provide them with the mental clarity and tools to meet the challenges of life, improve their mental health, and succeed in their relationships and work.
Aids Long-Term Recovery
The Biden-Harris Administration is focusing on evidence-based treatment methods to help people who are incarcerated get and stay on the path to addiction recovery.
This includes medication-assisted treatment (MAT), which combines the use of medications like buprenorphine with behavioral therapy to treat opioid abuse.
Buprenorphine, the first medication that could be prescribed by physicians to treat opioid use disorders, helps people overcome addiction in a few ways.
Using buprenorphine helps with recovery by:
reducing cravings
diminishing opioid withdrawal symptoms, which include flu-like symptoms and severe anxiety
improving safety, if overdose occurs
lessening the chance of misuse
One study in support of buprenorphine’s effectiveness showed that participants receiving the medication were almost twice as likely to remain in treatment and not relapse.
Prevents Overdose Deaths
According to U.S. News and World Report, the leading cause of death among people newly released from prison is drug overdose.
This is partly due to the fact that their tolerance levels decrease while incarcerated, so they aren’t able to tolerate the same amount of the drug as before they were in prison.
The buprenorphine study mentioned above also revealed that people not receiving the treatment had a 20% mortality rate."
-via Addiction Resources.net, 3/9/23
#addiction#cw drug use#cw addiction#addiction treatment#mass incarceration#medicaid#united states#us politics#prison reform#prison industrial complex#biden#kamala harris#evidence based medicine#healthcare access#opiod crisis#opiod epidemic#buprenorphine#drug treatment#good news#hope#voting matters
53 notes
·
View notes
Text
youtube
Is Your Evidence Really Based? Behaviourist Capture, Autistic Self-Advocacy, and Librarianship
In the history of science and medicine there are numerous examples of how the “best available evidence” promoted by professional societies was profoundly, destructively wrong. This can be seen in the widespread support of scientific racism and eugenics as well as the pathologization of “sexual inversion” and gender variance. When, as librarians, we talk about the nature of authority and hold up peer review as an example of a methodological gold standard in academic and medical research, we must always ask ourselves: whose peers are we talking about? For that matter, whose interests are we talking about? It is becoming increasingly evident even to those outside the autistic community that despite claims of being grounded in evidence-based practices, most studies on the effectiveness of Applied Behavioral Analysis (ABA) are poorly designed, do not disclose conflicts of interest, display a strategic disregard of the harmful outcomes of interventions, and do not reflect the interests of the majority of autistic people. At best, ABA is expensive, intensive, and ineffective at improving life outcomes. At worst, it is actively traumatic and makes us more susceptible to further victimization.
This discussion will examine recent challenges to the evidence-based nature of ABA and how ABA practitioners have historically taken advantage of the internalist nature of the peer-review system. These challenges reinforce what autistic activists have been saying for over twenty years and have consequences for how librarians deliver information literacy instruction. Information literacy and librarianship are not neutral activities and must include a place for own voice narratives, patient, and survivor accounts if we are to avoid perpetuating harmful industry standards with a shrug and a gesture to how “well, everyone’s doing it.”
7 notes
·
View notes
Text
In concluding their piece, Lahl and Fell said: 'The authors' suggestion that medical providers should deviate from the principle of 'do no harm' to follow paths where the evidence indicates harm is quite shocking.""This perspective, driven more by ideology, emotions, and personal desires than by evidence, conflicts with the foundations of evidence-based medicine.'
MSU sociology professor Dr. Carla Pfeffer is slammed over scientific journal article saying trans men should be allowed to take testosterone while pregnant, despite warnings hormones may trigger severe health issues in fetuses
Dr. Carla Pfeffer published a paper alongside five other academics concerning the use of testosterone therapy during transgender pregnancy
The sociology professor and her cohorts have since been slammed by two nurses for disregarding the safety of a fetus 'in the name of trans inclusion'
Jennifer Lahl and Kallie Fell hit back at the study, deeming one portion of it 'quite frankly, insane'
By JOE HUTCHISON FOR DAILYMAIL.COM
PUBLISHED: 10:37 EDT, 20 October 2023
A professor has been slammed over a scientific journal in which she said trans man should be allowed to take testosterone while pregnant, despite warnings it could trigger severe health issues.
Dr. Carla Pfeffer, who is not a medical doctor, penned a new paper alongside five other academics titled 'Medical uncertainty and reproduction of the 'normal': Decision-making around testosterone therapy in transgender pregnancy.
Pfeffer, who is a sociology professor at Michigan State University, argues that pregnancy care is too focused on helping women have healthy babies, and that trans men might be fine to take testosterone while pregnant.
The authors , who are sociologists, have since been accused of choosing to disregard the safety of a developing fetus 'in the name of trans inclusion'.
In a scathing response to the paper, two nurses have criticized the article saying if abiding by their take 'would land us in a vacuum devoid of medical ethics'.

Dr Carla Pfeffer, pictured here, published a paper alongside five other academics concerning the use of testosterone therapy during transgender pregnancy

The sociology professor and her cohorts have since been slammed by two nurses for disregarding the safety of a fetus 'in the name of trans inclusion'
Authors Jennifer Lahl and Kallie Fell, who is the Executive Director at The Center for Bioethics and Culture, published a response to the paper titled: 'Is There a Doctor in the House?'
In it, they said: 'The authors argue that 'gendered' pregnancy care is too focused on helping women have healthy babies, and that it might be okay for transmen to continue taking testosterone during pregnancy despite the known health risks to the fetus and effects on its normal development.
'This is, quite frankly, insane.'
In the paper, Pfeffer and her fellow colleagues had studied 70 international trans individuals and 22 health care providers who focus on trans people.
Their paper says: 'We argue that in the context of lacking and uncertain medical evidence (HRT with testosterone during pregnancy and chest feeding) in a highly gendered treatment context (pregnancy and lactation care), both patients and providers tend to pursue precautionary, offspring-focused treatment approaches.'
In response, Lahl and Fell say the findings are flawed as only biologically fertile human females possess the attributes for pregnancy and childbirth.
The two label this 'a simple biological reality', saying that pregnancy care isn't 'gendered' at all.
According to the Mayo Clinic, testosterone may cause birth defects if a pregnant woman comes into contact with it.
Lahl and Fell also added: 'The concerns raised by Pfeffer and colleagues focus on the modern treatment approach physicians take, which they deem excessively 'precautionary' and 'offspring-focused.'

Kal Fell, front, and Jennifer Lahl, background, published a response to the paper titled: 'Is There a Doctor in the House?'
'Fortunately, caring for the child and the mother are neither mutually exclusive nor zero-sum.
'In situations where a woman aspires to become pregnant and commits to motherhood, physicians can provide care that optimizes outcomes for both parties while minimizing potential harm.
'If a woman chooses to continue a pregnancy, doesn't the developing fetus also have a right to the four principles of medical ethics?'
'In such cases, the physician is duty-bound to care for both the child and the mother.'
One health care provider also told researchers: 'I think if you choose to have a pregnancy and your female hormone levels would be already so high that testosterone probably wouldn't even mentally help.
'If you're producing breast milk and you couldn't be without testosterone for mental health, if you couldn't deal without testosterone, then you probably shouldn't be pregnant.'
In concluding their piece, Lahl and Fell said: 'The authors' suggestion that medical providers should deviate from the principle of 'do no harm' to follow paths where the evidence indicates harm is quite shocking.
'This perspective, driven more by ideology, emotions, and personal desires than by evidence, conflicts with the foundations of evidence-based medicine.'
#Dr Carla Pfeffer is a sociology professor#Why is she writing papers on maternal and fetal health?#Jennifer Lahl is speaking the truth#Kallie Fell is speaking the truth#Medical uncertainty and reproduction of the 'normal': Decision-making around testosterone therapy in transgender pregnancy#michigan state university#Pregnancy care is too focused on helping women have healthy babies#statement showing transcult brain rot#The transcult and medical ethics#disregard the safety of a developing fetus in the name of trans inclusion'#Is there a Doctor in the house?#Pregnancy care isn't gendered it's sex based#evidence based medicine
4 notes
·
View notes
Note
How do you feel about probiotic and prebiotics supplement use (or just in a source like a bit of yogurt, etc) in a health animal?
I have heard of these being used and was interested because I know gut health and diversity is important. I read VCA's website and it has a few brands listed, but I just wanted to know if there would be possible harm of using it in a healthy animal, more.so as a preventative care sort of deal.
Same with joint supplements. I know you shouldn't give too many extras to avoid ruining the balance of the kibble, but I was wondering if starting an animal on a vet recommended joint supplement/chew would be a bad idea in an animal who is healthy as well?
I plan to ask my personal vet those questions, but I know my other pets have got arthritis and I'd love to prevent or lessen the harm from that.
Thank you so much! Just wanting to hear a few more opinions :)
gettingvetted here.
At best, evidence for probiotic use in animals is iffy. The best evidence for their use is with acute GI disease caused by dysbiosis or antibiotics. So, it won’t hurt anything to have a dog on it long term, but probably won’t help prevent anything either. (source)
As for joint supplements, about the same is true. There are potential benefits, unlikely to harm, but if there is joint disease, it is best to use alongside other treatment methods. (source)
33 notes
·
View notes
Text
The Extreme Nutritional Benefits of Mushrooms: Varieties and Mechanisms of Anti-Cancer, Anti-Death, Nootropic Effects
The Extreme Nutritional Benefits of Mushrooms: Varieties and Mechanisms of Anti-Cancer, Anti-Death, Nootropic Effects
Mushrooms have been part of the human diet for up to 18,000 years, since the Upper Paleolithic’s Magdalenian phase, possibly beginning with bolete (porcini) variety mushrooms, which are still popular in Italian cuisine today.
Delicious and an ample quality-protein source, mushrooms are also extremely beneficial to health in important ways. Generally, they are nootropic brain-protectants,…

View On WordPress
#autoimmune disease diet#bart kay#biohacker#biohacking#carnivore diet#danny roddy#delicious healthy foods keto#diet to fight cancer#Dominic D’Agostino#eat to live#epidemiology#ergo-log#evidence based medicine#fight cancer naturally#fight chronic inflammation diet#functional medicine#fungi medicine#grimhood#holistic health#ketogenic diet#leaky gut#low carb high fat diet#mark hyman#mark sisson#michael gregor#microbiome#mikhaela peterson diet#mushrooms fight cancer#mushrooms miracle health benefits#natural herbal medicine
19 notes
·
View notes
Text
Send This Open Letter to The Alberta Medical Association - They defend the quackery that is "Gender Affirming Care"
Thank you to Our Duty Canada for composing this letter.
An Open Letter to the Alberta Medical Association (AMA)
Regarding the February 1st Statement from the AMA
Section of Pediatrics on gender-affirming treatments March 2024
On February 1, 2024 your association released a statement in response to
Alberta Premiere Danielle Smith’s proposed changes to the treatment of
trans-identified children…
View On WordPress
#Evidence Based Medicine#Gender Affirming Care is based on Poor quality evidence#Quackery#The Alberta Medical Association
0 notes
Video
youtube
Is Evidence Based Medicine now impossible?
0 notes
Text
Chiropractic Misconceptions
This is gonna be a doozy.
Chiropractic was started by D.D. Palmer who got his idea from a seance.
I think this one is really funny. Honestly, no amount of googling got me anywhere with this besides the Reddit posts that claim this is a fact. What I do know, however, is that around 1890, the U.S. midwest was rife with spirtualism and the foundation of two health professions, osteopathic medicine (then osteopathy) and chiropractic. I'm not going to defend D.D. Palmer. The guy was a bit nuts, but he never claimed to have received information from a seance. The leftover religious subtext in chiropractic philosophy is due to the backup plan for chiropractic to follow "Christian Science" which, if B.J. and David Palmer (child and grandchild to D.D.) had not gotten the profession legally established, would have resulted in chiropractic protected as a religion. Thankfully, the practice medical (and legal).
2. Chiropractic is dangerous.
No, it's really not. A meta-analysis completed by the Spine Journal in May 2023 reported that while studies are still limited, the benefits of chiropractic/manual manipulation are present and the risks are rare, but further studies will need to be reported. An older analysis from 2008 also identified risks and benefits of cervical manipulation noting that these risks were negligible given the associated benefits.
3. Chiropractic care does not "do anything."
This one always bothers me. Does it do anything for ADHD or autism as some chiros, unfortunately, claim? No, goodness no. Does it help with back pain, neck pain, and other musculoskeletal elements? Heck yeah!
Here's a few studies for that. I will add more as I find them.
Evidence-Based Guidelines for the Chiropractic Treatment of Adults With Headache
Clinical Practice Guideline: Chiropractic Care for Low Back Pain
Evidence-Based Practice and Chiropractic Care
4. Chiropractors believe they can "cure" anything.
I don't have a lot for this one. Unfortunately, the scope of our practice is ill-defined. Efforts are being made to secure the title of "musculoskeletal primary care," but this is slow-going. Far too many of the old-brass refuses to acknowledge what we are and what we aren't.
5. Chiropractic doesn't believe in germ-theory (i.e. we don't have proper education.)
Chiropractic education is 173 credits and 310 contact hours in clinic. Covering biochemistry, pathology, physiology, anatomy, and technique practice. It is comparable to medical education, minus a focus on pharmacology and the clinical rotations. Chiropractic students either rotate through the clinic attached to their school or through local preceptorships.
And yes, we believe in germ-theory AND vaccinations.
I might add more, but these are the ones I have information on/opinions on at this moment. I want to point out that while our founder was a bit weird, so was medicine at the time.
4 notes
·
View notes
Text
“Finally, Evidence-Based partying.”
When all the budget is calculated and spent according to the trend in previous parties.
17 notes
·
View notes
Text
By: Leor Sapir
Published: Jun 28, 2023
A growing number of countries, including some of the most progressive in Europe, are rejecting the U.S. “gender-affirming” model of care for transgender-identified youth. These countries have adopted a far more restrictive and cautious approach, one that prioritizes psychotherapy and reserves hormonal interventions for extreme cases.
In stark contrast to groups like the American Academy of Pediatrics (AAP), which urges clinicians to “affirm” their patient’s identity irrespective of circumstance and regards alternatives to an affirm-early/affirm-only approach “conversion therapy,” European health authorities are recommending exploratory therapy to discern why teens are rejecting their bodies and whether less invasive treatments may help.
If implemented in American clinics, the European approach would effectively deny puberty blockers and cross-sex hormones to most adolescents who are receiving these drugs today. Unlike in the U.S., in Europe surgeries are generally off the table before adulthood.
Why are more countries turning their backs on what American medical associations, most Democrats and the American Civil Liberties Union call “medically necessary” and “life-saving” care? The answer is that Europeans are following principles of evidence-based medicine (EBM), while Americans are not.
A bedrock principle of EBM is that medical recommendations should be grounded in the best available research. EBM recognizes a hierarchy of information. The expert opinion of doctors, for example, even when based on extensive clinical experience, furnishes the lowest quality — meaning, least reliable — information. Slightly higher on the information pyramid are observational studies. Systematic reviews of evidence, meanwhile, furnish the highest quality evidence. They follow a rigorously developed, reproducible methodology. They do not cherry-pick studies with convenient results, but instead consider all the available research.
Most importantly, systematic reviews don’t merely summarize the conclusions of available studies on a question of interest. Instead, they assess the strengths and weaknesses of these studies to determine the reliability of their findings. To do this, systematic reviews typically use the GRADE system (Grading of Recommendations, Assessment, Development and Evaluations) and rank the quality of evidence as “high,” “moderate,” “low” or “very low.”
Systematic reviews by EBM experts in Scandinavia and the United Kingdom have concluded that there are serious gaps in the evidence base for sex modification in minors. The U.K. systematic reviews found the available research to be of “very low” quality — meaning that there is very low certainty that an observed effect, like reduced suicidality, is due to the intervention, and therefore the studies’ claimed results are unlikely to represent the truth.
Importantly, even the famous Dutch study that is said to be the “gold standard” of research in this area received a rating of “very low” due to serious methodological problems. Sweden’s National Board of Health and Welfare has said that the risks of treating gender dysphoric minors with hormonal interventions “currently outweigh the possible benefits.”
Last year, Florida’s health authorities commissioned what is known as an “umbrella review,” or a systematic overview of systematic reviews, from independent experts at McMaster University, home of EBM. Unsurprisingly, that overview came to the same conclusion: There is no reliable evidence that youth transition improves mental health outcomes.
Because U.S. medical groups don’t always use EBM, their conclusions can be based on studies whose fatal flaws are overlooked or ignored. Consider, as an example, a study done at Seattle Children’s Hospital and published last year. The study’s authors reported that use of puberty blockers and cross-sex hormones was associated with 60 percent lower odds of depression and 73 percent lower odds of suicidality. Leading mainstream publications, including Scientific American and Psychology Today, celebrated the findings. More recently, major U.S. medical associations cited the study in federal court proceedings.
But a careful look at the study’s data shows that the kids who received hormonal interventions did no better by the end of the study than at the beginning. The researchers’ claim about improvement was based on the fact that the kids in the control group, who received psychotherapy but not hormones, got worse relative to the hormone group. But even this isn’t accurate, as 80 percent of the control group dropped out by the end of the study, and a likely reason for this dramatic loss to follow-up is that many or perhaps all of the non-hormone-treated kids improved without “gender-affirming” drugs. It’s quite possible that if the researchers had followed up with all the participants, we’d see this study become Exhibit A in the case against pediatric sex changes.
Similar problems exist in studies purporting to show a rate of transition regret of less than 1 percent. The true rate of regret is not known and won’t be known for years to come. The claim that gender dysphoric teens are at high risk of suicide if not given access to “gender-affirming” drugs and surgeries is likewise baseless and irresponsible. In February, Finland’s top expert in gender medicine emphasized this point to the country’s liberal newspaper of record.
The American Academy of Pediatrics’ main statement on gender medicine, authored by a single doctor while still in his residency, is not a systematic review. The author himself has conceded as much. A later published peer-reviewed fact check found the AAP statement to be a textbook example of cherry-picking and mischaracterization of evidence.
The World Professional Association of Transgender Health (WPATH) says in its latest “standards of care” that a systematic review of evidence is “not possible.” Instead, WPATH used a “narrative review,” which has a high risk of bias according to EBM because it doesn’t utilize a reproducible methodology. England has broken from WPATH, and the director of Belgium’s Center for Evidence-Based Medicine has said he would “toss them [WPATH’s guidelines] in the bin.” In the U.S., WPATH’s standards are widely accepted as authoritative.
The U.S. Endocrine Society has relied on two systematic reviews in developing its own guideline. But these reviews were not for mental health benefits, and in any case the Endocrine Society ranks the quality of evidence behind its own recommendations as “low” or “very low.”
All other U.S. medical groups cite these three sources when assuring the public about “gender-affirming care,” thus creating an illusion of consensus around “settled science.”
Earlier this year, an investigative report in the prestigious British Medical Journal concluded that although pediatric gender medicine in the U.S. is “consensus-based,” it is not “evidence-based.” Gordon Guyatt, distinguished professor in the Department of Health Research Methods, Evidence, and Impact at McMaster University, Ontario, and one of the founders of EBM, recently called American guidelines for managing youth gender dysphoria “untrustworthy.”
Consensus can be produced by misguided empathy, ideological capture or political pressures. Consensus can also be manufactured. The new president of the American Medical Association (AMA) has said there should be “no debate” when it comes to offering kids “gender-affirming” drugs and surgeries.
Yale School of Medicine’s Dr. Meredithe McNamara calls the questioning of the evidence behind pediatric sex changes “science denialism.” Her protest is ironic. Science is a process of ongoing inquiry and debate, not a set of predetermined conclusions. Science depends on skepticism, especially about sensitive subjects. True science denialism means restricting rational, evidence-based debate — exactly what McNamara and the AMA’s new president want to do.
Their calls are bearing fruit. Just this month, gender activists successfully pressured a medical journal to retract a paper whose conclusions they found inconvenient. The ongoing campaign to suppress scientific debate allows a pseudo-consensus to emerge around “gender-affirming care.”
Put simply, pediatric gender medicine in the U.S. is out of control. Medicalization of gender diversity in children is a fast-growing industry that shows no signs of self-correction. Doctors and therapists who practice “affirmative” medicine consistently demonstrate ignorance about EBM principles and deceive the public about the grim realities behind the euphemism “gender-affirming care.”
A Reuters investigation last year interviewed providers at 18 pediatric gender clinics and found that none were doing comprehensive mental health assessments and differential diagnosis. Those who promote and practice “gender-affirming care” themselves tell us that their approach is child-led. “Gatekeeping” of medical transition, they insist, is pointless, even “dehumanizing.”
The author of the AAP’s position paper on gender medicine has said that a “child’s sense of reality” is the “navigational beacon to orient treatment around.” The director of the gender clinic at Boston Children’s Hospital has admitted that they give out puberty blockers “like candy.” Even the founding psychologist of that clinic has warned that kids are being inappropriately “rushed toward the medical model.”
Why the U.S. has become an outlier on pediatric transgender medicine is a complicated question, but at least part of the answer is that European welfare states have centralized health bureaucracies and public health insurance. Before medicines can be approved for state funding, their evidence base needs to be evaluated. The American health care system is more vulnerable to profit motives, activist doctors and political pressures. Medical associations claim to advocate for patient health but can have other motives as well.
The situation is so dire that when pediatric gender medicine experts in other countries want to defend their practices before a skeptical public, they sometimes say that at least they are not as bad as the Americans. That is one kind of American exceptionalism we can do without.
==
[A] “child’s sense of reality” is the “navigational beacon to orient treatment around.”
Holy shit.
How can you claim that it's "settled science" and "consensus," and then leave everything up to the most immature, most depressed, most anxious, least experienced person in the room?
There are no grown ups in charge.
#Leor Sapir#gender ideology#genderwang#queer theory#medical corruption#medical scandal#gender affirming#sex trait modification#gender affirming care#affirmation model#affirmation#weak evidence#poor evidence#evidence based medicine#settled science#religion is a mental illness
27 notes
·
View notes
Text
Spread awareness !

0 notes
Text
Palantir’s NHS-stealing Big Lie

I'm on tour with my new, nationally bestselling novel The Bezzle! Catch me in TUCSON (Mar 9-10), then SAN FRANCISCO (Mar 13), Anaheim, and more!

Capitalism's Big Lie in four words: "There is no alternative." Looters use this lie for cover, insisting that they're hard-nosed grownups living in the reality of human nature, incentives, and facts (which don't care about your feelings).
The point of "there is no alternative" is to extinguish the innovative imagination. "There is no alternative" is really "stop trying to think of alternatives, dammit." But there are always alternatives, and the only reason to demand that they be excluded from consideration is that these alternatives are manifestly superior to the looter's supposed inevitability.
Right now, there's an attempt underway to loot the NHS, the UK's single most beloved institution. The NHS has been under sustained assault for decades – budget cuts, overt and stealth privatisation, etc. But one of its crown jewels has been stubbournly resistant to being auctioned off: patient data. Not that HMG hasn't repeatedly tried to flog patient data – it's just that the public won't stand for it:
https://www.theguardian.com/society/2023/nov/21/nhs-data-platform-may-be-undermined-by-lack-of-public-trust-warn-campaigners
Patients – quite reasonably – do not trust the private sector to handle their sensitive medical records.
Now, this presents a real conundrum, because NHS patient data, taken as a whole, holds untold medical insights. The UK is a large and diverse country and those records in aggregate can help researchers understand the efficacy of various medicines and other interventions. Leaving that data inert and unanalysed will cost lives: in the UK, and all over the world.
For years, the stock answer to "how do we do science on NHS records without violating patient privacy?" has been "just anonymise the data." The claim is that if you replace patient names with random numbers, you can release the data to research partners without compromising patient privacy, because no one will be able to turn those numbers back into names.
It would be great if this were true, but it isn't. In theory and in practice, it is surprisingly easy to "re-identify" individuals in anonymous data-sets. To take an obvious example: we know which two dates former PM Tony Blair was given a specific treatment for a cardiac emergency, because this happened while he was in office. We also know Blair's date of birth. Check any trove of NHS data that records a person who matches those three facts and you've found Tony Blair – and all the private data contained alongside those public facts is now in the public domain, forever.
Not everyone has Tony Blair's reidentification hooks, but everyone has data in some kind of database, and those databases are continually being breached, leaked or intentionally released. A breach from a taxi service like Addison-Lee or Uber, or from Transport for London, will reveal the journeys that immediately preceded each prescription at each clinic or hospital in an "anonymous" NHS dataset, which can then be cross-referenced to databases of home addresses and workplaces. In an eyeblink, millions of Britons' records of receiving treatment for STIs or cancer can be connected with named individuals – again, forever.
Re-identification attacks are now considered inevitable; security researchers have made a sport out of seeing how little additional information they need to re-identify individuals in anonymised data-sets. A surprising number of people in any large data-set can be re-identified based on a single characteristic in the data-set.
Given all this, anonymous NHS data releases should have been ruled out years ago. Instead, NHS records are to be handed over to the US military surveillance company Palantir, a notorious human-rights abuser and supplier to the world's most disgusting authoritarian regimes. Palantir – founded by the far-right Trump bagman Peter Thiel – takes its name from the evil wizard Sauron's all-seeing orb in Lord of the Rings ("Sauron, are we the baddies?"):
https://pluralistic.net/2022/10/01/the-palantir-will-see-you-now/#public-private-partnership
The argument for turning over Britons' most sensitive personal data to an offshore war-crimes company is "there is no alternative." The UK needs the medical insights in those NHS records, and this is the only way to get at them.
As with every instance of "there is no alternative," this turns out to be a lie. What's more, the alternative is vastly superior to this chumocratic sell-out, was Made in Britain, and is the envy of medical researchers the world 'round. That alternative is "trusted research environments." In a new article for the Good Law Project, I describe these nigh-miraculous tools for privacy-preserving, best-of-breed medical research:
https://goodlawproject.org/cory-doctorow-health-data-it-isnt-just-palantir-or-bust/
At the outset of the covid pandemic Oxford's Ben Goldacre and his colleagues set out to perform realtime analysis of the data flooding into NHS trusts up and down the country, in order to learn more about this new disease. To do so, they created Opensafely, an open-source database that was tied into each NHS trust's own patient record systems:
https://timharford.com/2022/07/how-to-save-more-lives-and-avoid-a-privacy-apocalypse/
Opensafely has its own database query language, built on SQL, but tailored to medical research. Researchers write programs in this language to extract aggregate data from each NHS trust's servers, posing medical questions of the data without ever directly touching it. These programs are published in advance on a git server, and are preflighted on synthetic NHS data on a test server. Once the program is approved, it is sent to the main Opensafely server, which then farms out parts of the query to each NHS trust, packages up the results, and publishes them to a public repository.
This is better than "the best of both worlds." This public scientific process, with peer review and disclosure built in, allows for frequent, complex analysis of NHS data without giving a single third party access to a a single patient record, ever. Opensafely was wildly successful: in just months, Opensafely collaborators published sixty blockbuster papers in Nature – science that shaped the world's response to the pandemic.
Opensafely was so successful that the Secretary of State for Health and Social Care commissioned a review of the programme with an eye to expanding it to serve as the nation's default way of conducting research on medical data:
https://www.gov.uk/government/publications/better-broader-safer-using-health-data-for-research-and-analysis/better-broader-safer-using-health-data-for-research-and-analysis
This approach is cheaper, safer, and more effective than handing hundreds of millions of pounds to Palantir and hoping they will manage the impossible: anonymising data well enough that it is never re-identified. Trusted Research Environments have been endorsed by national associations of doctors and researchers as the superior alternative to giving the NHS's data to Peter Thiel or any other sharp operator seeking a public contract.
As a lifelong privacy campaigner, I find this approach nothing short of inspiring. I would love for there to be a way for publishers and researchers to glean privacy-preserving insights from public library checkouts (such a system would prove an important counter to Amazon's proprietary god's-eye view of reading habits); or BBC podcasts or streaming video viewership.
You see, there is an alternative. We don't have to choose between science and privacy, or the public interest and private gain. There's always an alternative – if there wasn't, the other side wouldn't have to continuously repeat the lie that no alternative is possible.
Name your price for 18 of my DRM-free ebooks and support the Electronic Frontier Foundation with the Humble Cory Doctorow Bundle.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/03/08/the-fire-of-orodruin/#are-we-the-baddies

Image:
Gage Skidmore (modified)
https://commons.m.wikimedia.org/wiki/File:Peter_Thiel_(51876933345).jpg
CC BY-SA 2.0
https://creativecommons.org/licenses/by-sa/2.0/deed.en
#pluralistic#peter thiel#trusted research environment#opensafely#medical data#floss#privacy#reidentification#anonymization#anonymisation#nhs#ukpoli#uk#ben goldacre#goldacre report#science#evidence-based medicine#goldacre review#interoperability#transparency
520 notes
·
View notes